Professional Documents
Culture Documents
Psychiatry Study Guide For Shelf
Uploaded by
appoliniaOriginal Title
Copyright
Available Formats
Share this document
Read this document in other languages
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Psychiatry Study Guide For Shelf
Uploaded by
appoliniaCopyright:
Available Formats
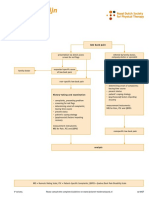
PSYCHIATRY General Principles 5% - 10% Organ Systems 90% - 95% - Mental Disorders 75% - 85% o Promoting Health and
Health Maintenance 1% - 5% o Understanding Mechanisms of Disease 10% - 15% o Establishing a Diagnosis 55% - 65% Mental disorders usually 1st diagnosed in infancy, childhood, or adolescence (5-10%) Substance-related disorders (5-10%) Schizophrenia and other psychotic disorders (5-10%) Mood disorders (5-10%) Anxiety disorders (5-10%) Somatoform disorders (1-5%) Other disorders/conditions (5-10%) o Applying Principles of Management 20-25% - Diseases of the Nervous System and Special Senses 10%-15%
Review Session: - LOTS of questions of substance abuse - Depression, mood, anxiety o Suicide risk factors When the pt can name something that has changed you are in a better postion than when they cant Acute change in job, worthlessness hopelessness, substance abuse, suicide ideation, attempt, plan, older Caucasian males, poor family support, prior history of suicide, family members with suicide history - Body dysmorphic disorder is a 1 question topic - Child questions about 25% are child/adolescent as patient. (does not mean child disorders could be MDD, anorexia) - No theorists - There will be psychotherapy stuff there wont be freud or theories, no defense mechanisms - Everything will be tested on DSM diagnoses. - Schizophrenia progression brief, schizophreniform, schizophrenia Neuro: - dementias - MR and childhood presentations of MR, prognosis One question disorders: - Somatoform - somatization disorder, conversion d/o o Conversion with OC people loss of fxn tx with appropriate therapy (PT for poor movement of arm, speech therapist for poor talking, etc) o Hypochondriasis with feelers reassurance (anxiety based and can treat with SSRIs in real life. o Somatization o Body Dysmorphic disorders - Eating Disorders - Bulimia can be tx with ssri, anorexia tx behavioral - Sleep disorders - Pain disorder - dissociative disorders
Key Points: - Adjustment disorder vs. MDD vs. GAD vs. Acute Stress disorder vs. PTSD - Medications, ESPECIALLY side effects - Medical Disorders with psychiatric manifestations o Depression and pancreatic cancer, addisons disease o Pheochromocytoma or carcinoid looking like panic disorder - Depression vs. bereavement vs. somatization disorder - Physical features of common MR presentations (down syndrome, fragile X) - Look for delirium and psychosis - Medication Side effects o At receptor level - Neurotransmitters o Affected in psychiatric disease Anxiety increased NE, decreased GABA and serotonin Schizophrenia elevated serotonin, elevated NE, decreased GABA, excess dopamine in prefrontal cortex = negative sx. Dopamine in mesolimbic pathway = positive symptoms Blocking dopamine in Tubuloinfundibular hyperprolactinemia; Nigrostriatal EPS Depression decreased serotonin, NE, dopamine; high cortisol, abnormal thyroid axis Panic Disorder increased NE, decreased GABA, serotonin Alzheimers dementia decreased Ach due to loss of cholinergic neurons in basal nucleus of meynert in midbrain and decreased NE due to loss of noradrenergic neurons in locus ceruleus of brainstem. Parkinson Disease loss of cells in substantia nigre of basal ganglia which leads to decreased dopamine and loss of dopaminergic tracts Tourettes/Tics impaired regularion of dopamine in the caudate nucleus and possible upregularion of endogenous opiates and the noradrenergic system o Site of NT release Locus ceruleus NE Raphe nucleus serotonin - Intoxication and Withdrawal Section from first aid
PSYCHOTIC DISORDERS Schizophrenia To make the diagnosis of schizophrenia, a pt must have symptoms of the disease for at least _____. - 6 months Name the 5 subtypes of schizophrenia. - Paranoid - Disorganzied - Catatonic - Undifferentiated - residual What are 5 characteristics of catatonic schizophrenia? - Motor immobility - excessive purposeless motor activity - extreme negativism or mutism - peculiar voluntary movements or posturing - echolalia/echopraxia What are the "5 A's" of schizophrenia, which describe the negative symptoms of the disease? - Anhedonia - Affect (flat) - Alogia (poverty of speech) - Avolition (apathy) - Attention (poor)
2 or more of what 5 symptoms must be present for at least 1 month to diagnose schizophrenia? - Delusions - Hallucinations - disorganized speech - grossly disorganized or catatonic behavior - negative symptoms Differentiate between brief psychotic disorder, schizophreniform disorder, and schizophrenia based on duration of symptoms. - Brief psychotic disorder: < 1 month - schizophreniform disorder: 1 - 6 months - schizophrenia: > 6 months What are 'ideas of reference'? - Belief that cues in the external environment are uniquely related to the individual What is the downward drift hypothesis regarding schizophrenics? - People suffering from schizophrenia are unable to function well in society and hence enter lower socioeconomic groups What are 2 theorized dopamine pathways affected in schizophrenia? - Prefrontal cortical: inadequate dopaminergic activity responsible for negative symptoms - mesolimbic: excessive dopaminergic activity responsible for positive symptoms What are 4 components of the mesolimbic pathway responsible for positive schizophrenia sx? - Nucleus accumbens - Fornix - Amygdala - hippocampus The negative sx of schizophrenia are thought to occur due to dopamine action in the _____ pathway. - Mesocortical Describe the relative levels of serotonin, norepinephrine, GABA, and glutamate receptors in schizophrenic pts. - Elevated: serotonin, norepinephrine - decreased: GABA, glutamate receptors Name 4 first-generation antipsychotic medications used to treat schizophrenia. - Chlorpromazine - Thioridazine - Trifluoperazine - haloperidol First-generation antipsychotic medications are all _____ antagonists. - Dopamine (mostly D2) What are 4 second-generation antipsychotic medications used to treat schizophrenia? - Risperidone; clozapine; olanzapine; quetiapine; aripiprazole; ziprosidone Second-generation antipsychotic medications antagonize _____ receptors as well as dopamine receptors. - Serotonin What are the hallmark side effects for first and second-generation antipsychotics? - First-generation: EPS; second-generation: metabolic syndrome What 2 antiparkinsonian medications can be used to treat EPS? - Benztropine - diphenhydramine Blockage of what dopamine pathway by neuroleptic medication results in extrapyramidal side effects? - Nigrostriatal In what 3 situations is only one psychotic sx necessary for a diagnosis of schizophrenia? - Bizarre delusions - auditory hallucinations commenting on the patient - two or more voices speaking to each other Schizoaffective Disorder What criteria is used to distinguish schizoaffective disorder from mood disorder w/ psychotic features? - Delusions or hallucinations for 2 weeks in the absence of mood disorder symptoms
Schizophreniform Disorder Brief Reactive Psychosis MOOD DISORDERS Bipolar Disorder Mania: Describe the DIG FAST mnemonic for symptoms of mania. - Distractibility - Insomnia/Impulsive behavior - Grandiosity - Flight of ideas/racing thoughts - Activity/agitation - Speech (pressured) - Thoughtlessness What criterion is required for diagnosis of a manic episode? - Presence of an abnormally elevated, expansive, or irritable mood and 3 of the above symptoms lasting at least 1 week What 3 drugs are approved for the acute treatment of mania? - Lithium - Valproate - carbamazepine What drug is used as maintenance treatment for bipolar disorder? - Lamotrigine All second-generation anti-psychotic medications are approved to treat acute mania except _____. - Clozapine What is the rapid-cycling specifier? - At least 4 major depressive, manic, hypomanic, or mixed episodes within the past 12 months What time period is required for diagnosis of mania vs. hypomania? - Mania: 7 days - hypomania: 4 days What is the definition of rapid cycling? - The occurrence of 4 or more mood episodes in 1 year (major depressive, manic, mixed, etc.) (T/F) Bipolar I has the highest genetic link of all major psychiatric disorders. - True What is the best treatment for a manic woman in pregnancy? - ECT What 2 anticonvulsants are especially useful for rapid cycling bipolar disorder? - Carbamazepine; valproic acid Bipolar depression Mood stabilizer. Cyclothymia Depressive Disorders Bereavement/Grief What time period signifies transition from normal to complicated/prolonged grief? - 6 months (T/F) Normal bereavement may include gross disorganization or suicidality. - False PostPartum Depression Describe the postpartum onset specifier. - Depressive, manic, or mixed episode within the first 4 weeks postpartum (T/F) Postpartum depression usually resolves w/o medication. - True What time of onset is required for the postpartum specifier for depression?
Onset within 4 weeks of delivery
Seasonal Affective Disorder What is the triad for seasonal affective disorder? - Irritability - carbohydrate craving - hypersomnia Major Depressive Disorder What is the response rate of patients w/ major depression to antidepressants? - 70% will respond; 30% of this response is a placebo effect - take 4-8 weeks to work (up to 3 months in elderly patients) What 2 characteristics define major depression? - Depressed mood; loss of interest or pleasure Most depressive episodes clear spontaneously within _____. - 6 months Name 4 unique subcategories of depressive disorders. - Melancholic anhedonia, early AM awakenings, PMR, excessive guilt, anorexia - Atypical hypersomnia, hyperphagia, reactive mood, leaden paralysis, hypersensitive to interpersonal rejection - Catatonic catalepsy (immobility), purposeless motor activity, extreme negativism or mutism, bizarre postures, echolalia; tx with antidepressants and antipsychotics concurrently psychotic - delusions/hallucinations Name the 2 characteristics required for the diagnosis of melancholia? - Pervasive loss of interest or pleasure; inability to respond to pleasurable stimuli What are 2 unique descriptive features of melancholia? - Diurnal variation; terminal insomnia What are 5 characteristics of atypical depression? - Hypersomnia - Hyperphagia - reactive mood - leaden paralysis - hypersensitivity to interpersonal rejection What category of antidepressant medication has been shown to be particularly effective in treating atypical depression? - Monoamine oxidase inhibitors (MAOIs) Name 3 sleep changes a/w depression. - Decreased delta sleep; decreased REM latency; increased REM density Describe the progression of anti-depressant drug trials. - Drug trials should last from 4-8 weeks; if the pt fails to respond within 4 weeks of treatment, the dosage should be increased or the pt should be switched to another drug, preferably from another class Augmentation of anti-depressant drugs w/ _____ is the best-researched option. - Lithium carbonate What second-generation anti-psychotic medication is often used as anti-depressant augmentation? - Aripiprazole _____ has the highest rate of suicide of any psychiatric disorder. - MDD What scale is used as the standard measure of depression severity in research to assess the effectiveness of therapies? - Hamilton Rating Score What cancer has a high association w/ depression? - Pancreatic cancer Use of MAOIs is a/w what 2 adverse conditions? - Hypertensive crisis - serotonin syndrome (T/F) Treatment of MDD w/ psychotic features may be treated w/ an anti-depressant alone.
- False; treatment should include an anti-depressant as well as either an antipsychotic medication or ECT What is the protocol for medication changes in a child w/ major depression w/ psychotic features who responds to the combination of an antidepressant and an antipsychotic? - Atypical antipsychotic should be continued for 3 months and then tapered off; the antidepressant should be continued for 6 - 9 months and then tapered over 2 - 3 months at 33% per month Describe results of a PET scan in a patient w/ depression. - Reduced metabolic activity and blood flow in both frontal lobes Use of tetracycline, nifedipine, and verapamil is a/w _____. - Depression Treatment of major depression in older adults is most successful with a combination of antidepressant medications plus interpersonal supportive psychotherapy. Interpersonal psychotherapy is suitable for individuals having experienced recent interpersonal conflicts or difficult role transitions. Dysthymic Disorder How does the diagnosis of dysthymic disorder differ between children and adults? - Dysthymic disorder can be diagnosed in children if they are symptomatic over a 1 year time period (instead of the 2 years required for adults) Electroconvulsive Therapy Name 4 indications for electroconvulsive therapy (ECT). - Very severe depression - high potential for suicide - cardiovascular disease - pregnancy - unresponsive to pharmacotherapy Describe 2 characteristics of MDD in which ECT treatment would be indicated. - MDD w/ psychotic features - MDD where rapid response is required The effectiveness of ECT is based on _____, not _____. - Length of postictal suppression; seizure duration Method: - premedication with atropine generalized anesthesia muscle relaxant generalized seizure by current across brain (bilateral/unilateral) seizure < 1 minute. - 8 tx over 2-3 week period. - Retrograde amnesia common SE but disappears within 6 months. NO true contraindications increased intracranial pressure is the most detrimental/associated. Recent MI is not an absolute contraindication.
ANXIETY DISORDERS Panic Disorder with and without agoraphobia What is the hallmark of panic disorder? - Unexpected panic attacks not provoked by any particular stimulus The treatment regimen for panic disorder should contain what 2 items? - Antidepressant; CBT What other disorder is commonly seen in pts w/ panic disorder? - MDD Name 5 medical conditions a/w panic attacks. - Mitral valve prolapse - Asthma - pulmonary embolus - angina - anaphylaxis Name 3 characteristics a/w panic disorder. - Persistent concern about having additional attacks
- worry about the implications of the attack - significant change in behavior related to the attacks What specifier is required w/ the diagnosis of panic disorder? - W/ or w/o agoraphobia What 2 SSRIs are commonly used to treat panic disorder? - Paroxetine - sertraline Nothing treats a panic attack like a BZD but dont start person who gets addicted to benzos or not? Specific and Social Phobias What qualifier is required for diagnosis of phobias in pts under age 18? - Duration > 6 months What SSRI is FDA approved for the treatment of social phobia? - Paroxetine Social phobia gradual desensitization; propranolol for physical manifestations; does not take care of actual anxiety School phobia in children - flooding Four most common mental disorders: 1. phobias 2. substance induced disorders 3. major depression 4. OCD Obsessive Compulsive Disorders What TCA has been shown to be effective in treating OCD? - Clomipramine Differentiate between an obsession and a compulsion. - Obsession: recurrent and intrusive thought, feeling, or idea that is egodystonic - compulsion: conscious repetitive behavior linked to an obsession that, when performed, functions to relieve anxiety caused by the obsession The rate of OCD is higher in pts w/ first-degree relatives who have _____. - Tourette syndrome Post Traumatic Stress Disorder What 2 classes of medications should be used to treat PTSD? - SSRIs; alpha-2 agonists (e.g. prazosin, clonidine) Nightmares, flashbacks, startle responses Treatment is TALKING - psychoanalytic psychotherapy pays particular attention to the role of trauma and sexual experiences in shaping both unconscious content and unconscious processing. Generalized Anxiety Disorder What atypical antidepressant is used for treatment of generalized anxiety disorder? - Buspirone Describe the indication and mechanism of buspirone. - Non-sedating non-benzodiazepine anxiolytic approved by the FDA for the treatment of anxiety disorders - acts as an agonist on 5HT-1A receptors What 4 medications/medication classes are used in the treatment of GAD? - SSRIs; venlafaxine; buspirone; benzodiazepines (T/F) Buspirone is not as effective in pts already exposed to benzodiazepines. - true Describe the anxiolytic action of buspirone. - 5HT-1A receptor partial agonist What is the advantage of buspirone over benzodiazepines? - Does not potentiate the CNS depression of alcohol (useful in alcoholics) and has a low potential for abuse/addiction
What medication is useful for patients who want a quick-acting, short-term medication but cannot tolerate benzodiazepines for various reasons? - Hydroxyzine (antihistamine) Treatment: - Psychotherapy
CHILD PSYCHIATRY Mental Retardation/Intelligence/Cognition What is the most commonly used IQ test for pts 16 - 75 years of age? - Wechsler Adult Intelligence Scale (WAIS) What IQ test is used in pts 2 - 18 years of age? - Stanford-Binet Test What 2 intelligence tests are used for children and adolescents? - Ages 2-12: Kaufman Assessment Battery for Children (K-ABC) - ages 6-16: Wechsler Intelligence Scale for Children-Revised (WISC-R) What 3 characteristics are required for diagnosis of mental retardation? - IQ < 70 - deficits in adaptive skills appropriate for the age group - onset before the age of 18 Name and describe the IQ levels which correspond to the 4 categories of mental retardation. - Mild: 70-55 - moderate: 55-40 - severe: 40-25 - profound: < 25 What is the most common inherited form of mental retardation? What is its cause? - Fragile X syndrome, caused by a defect in the FMR-1 gene What is the most common learning disorder? - Reading disorder, affecting up to 10% of school-age children Name 4 pervasive developmental disorders (PDDs). - Autistic disorder - Asperger disorder - Rett disorder - childhood disintegrative disorder Noonan Syndrome - An 8-year-old girl is brought to your office after her mother noticed that she was not growing well. The mother states that the girl gets poor grades at school, catches cold and cough infections very often, and bruises very easily. You note that the girl has a triangular face, hypertelorism, deeply grooved philtrum, and downslanting eyes. You also note the presence of webbed neck and low-set ears. The girl has scoliosis and an IQ of 65. You then order a complete work up, including CBC, coagulation profile, and cardiac evaluation. Echocardiography detects pulmonary valve stenosis. Suspecting a congenital disorder, you order karyotyping and mutation analysis. The diagnosis in this girl is Noonan syndrome (NS). PTPN11 gene mutations are seen in 50% of individuals with NS. SOS1 and KRAS mutations are other causes, although absence of a mutation does not rule out NS. NS is a sporadic or autosomal dominant congenital disorder with typical phenotypic features, which may not be visible to the casual onlooker. The most common facial features include hypertelorism and low-set and backward rotated ears, along with a thick helix. The philtrum is deeply grooved in more than 90% of cases. Congenital cardiac defects, bleeding disorders, mental retardation, webbed neck, and short stature are other features. Pulmonary valve stenosis is the most common cardiac defect and is seen in 50% of those affected. Other cardiac findings include atrial and/or ventricular septal defects and cardiomyopathies. Mowat-Wilson syndrome refers to an autosomal dominant condition resulting from mutation or deletion of ZEB2 gene on chromosome 22. Characteristic features include: narrow chin; deep, widely set eyes; open mouth; uplifted ear lobes; wide nasal bridges; and a shortened philtrum. Mental retardation, delayed growth and motor development, heart disease, and Hirschsprung disease are also seen.
Mutation in the fragile mental retardation 1 (FMR1) gene causes fragile X syndrome (FXS). FXS is the most common cause of inherited mental retardation and is characterized by cognitive, neuropsychological, and behavioral problems. Autistic-like behavior, speech and language delays, anxiety, mental retardation (IQ 35-70), shyness, attention deficit disorder with or without hyperactivity, and typical facies are observed. The FBN1 gene codes for the fibrillin-1 protein, and mutation in this gene causes Marfan syndrome. Other conditions that may arise from the mutation are isolated ectopia lentis, MASS syndrome, etc. Mutation in the KAL gene on chromosome 22 is the most common cause of Kalmann syndrome. It results in gonadotropin releasing hormone deficiency along with anosmia or severe hyposomia due to olfactory bulb hypoplasia or agenesis. Findings include absence of secondary sexual development, anosmia, sensorineural deafness, seizure disorders, decreased bone density, short metacarpals, and infertility. Fragile X The correct answer is fragile X syndrome (FXS). FXS is the most common cause of inherited mental retardation and is characterized by cognitive, neuropsychological, and behavioral problems. Autistic-like behavior, speech and language delays, anxiety, mental retardation (IQ 35-70), shyness, attention deficit disorder with or without hyperactivity, and typical facies are observed. The syndrome results from an expanded CGG repeat (> 200 repeats) at the 5' untranslated portion of the fragile mental retardation 1 gene ( FMR1). This causes a deficiency (or absence) of the FMR protein. The FMR protein controls the translation of several genes that regulate synaptic plasticity and development. Marfan syndrome is a genetic disorder affecting the bodys connective tissue and is caused by mutations in the FBN1 gene on chromosome 15. Affected individuals are above average height and may have lens subluxation, aortic dissection, and pneumothorax, apart from other abnormalities. Williams syndrome is a rare genetic condition with characteristic elflike features, cardiovascular defects, hypercalcemia, and neurodevelopmental defects. Mental retardation is typically mild to moderate. Language acquisition is generally delayed; and although quality of language is somewhat normal, language impairment is present throughout life. Other characteristic features are visuospatial deficits and hypersociability. Hypothyroidism, growth retardation, and feeding difficulties are additional features. Most cases are sporadic, and inherited cases are mostly autosomal dominant. XYY syndrome is a condition in which males have an extra Y chromosome; it is characterized by increased height, speech delays, and learning difficulties. Noonan syndrome is a sporadic or autosomal dominant congenital disorder with typical phenotypic features, which may not be visible to the casual onlooker. The most common facial features include hypertelorism and low-set and backward rotated ears, along with a thick helix. The philtrum is deeply grooved in more than 90% of cases. Congenital cardiac defects, bleeding disorders, mental retardation, webbed neck, and short stature are other features.
Autistic Disorder Describe the 3 categories of symptoms used to diagnose autism. - Problems w/ social interaction; impairments in communication; repetitive/stereotyped patterns of behavior or activities What is the age requirement a/w autism? - Age 3 (T/F) 70% of individuals w/ autism meet criteria for mental retardation. - True Aspergers Disorder Rett Disorder What are the characteristics of Rett disorder? - Normal physical and psychomotor development during the first 5 months after birth, followed by a decreasing rate of head growth and loss of previously learned purposeful hand skills between ages 5 and 30 months
children then develop stereotyped hand movements (hand wringing/washing), impaired language and psychomotor retardation, and problems w/ gait or trunk movements With what gene mutation is Rett disorder associated? - MECP2 gene mutation on X chromosome Attention Deficit Hyperactivity Disorder (ADHD) What are the 3 subcategories of ADHD? - Predominantly inattentive - predominantly hyperactive-impulsive - combined type Children w/ ADHD have a _____ chance of developing antisocial personality disorder. - 25% What are 3 clinical indications for use of atomoxetine in the treatment of ADHD? - Individuals or families w/ substance abuse problems; individuals w/ tics; patients w/ comorbid anxiety disorders Intoxication w/ what heavy metal may lead to hyperactivity which masquerades as ADHD? - Lead Name 3 medications used to treat ADHD. - Dextroamphetamine; methylphenidate; atomoxetine What is atomoxetine? (Strattera) - A non-stimulant that has been approved by the FDA for the treatment of ADHD What drug class is used to treat ADHD should CNS stimulants fail? - Alpha-2 agonists (clonidine, guanfacine) Childhood Disintegrative Disorder What is the age range for development of childhood disintegrative disorder? - Ages 2-10 Elimination What are 2 criteria for the diagnosis of encoporesis? - Greater than 5 years old - have already been toilet trained Define enuresis. - Involuntary voiding of urine (bed-wetting) after age 5 (at least twice a week for at least 3 consecutive months or w/ marked impairment) What TCA may be used to treat enuresis? - Imipramine Oppositional Defiant Disorder vs. Conduct Disorder How does oppositional defiant disorder (ODD) differ from conduct disorder? - ODD does not involve physical aggression or violation of the basic rights of others Describe the 4 categories of behaviors described by conduct disorder. - Aggression towards people or animals - destruction of property - deceitfulness/theft - serious violation of rules What is the diagnostic time period a/w ODD and conduct disorder? - ODD: 6 months - conduct disorder: 12 months Tourettes Disorder Describe the temporal component of tics required for the diagnosis of Tourette disorder. - Tics occur may times per day, almost every day for > 1 year (no tic-free period > 3 months) (T/F) Only motor or vocal tics are required for the diagnosis of Tourette disorder. - False; both motor and vocal tics must be present to diagnose Tourette disorder Describe the neurochemical basis of Tourette syndrome. - Impaired regulation of dopamine in the caudate nucleus
Describe the PANDAS mnemonic and the associated disorder. - Pediatric Autoimmune Neuropsychiatric Disorders Associated w/ Streptococcal infections - rapid onset of OCD and/or tic disorders such as Tourette syndrome following group A beta-hemolytic streptococcal infections What 2 classes of medications are used to treat Tourette disorder? - Atypical neuroleptics (e.g. risperidone) - alpha-2 agonists (e.g. clonidine, guanfacine) What 2 disorders are often present in patients w/ Tourette syndrome? - ADHD; OCD Separation Anxiety Disorder In what age range is separation anxiety age-appropriate? - 7 months to 6 years of age
EATING DISORDERS Anorexia Nervosa Name the 2 categories of anorexia nervosa. - Restrictive type - binge-eating/purging type Describe the weight requirement(s) listed by DSM-IV for the diagnosis of anorexia nervosa. - < 85% ideal body weight or BMI < 17.5 kg/m2 What acid-base disturbance is often found in anorexic binge-eating/purging type patients? - Hypochloremic, hypokalemic alkalosis What specific characteristic must be present in order to diagnose anorexia nervosa in females? - Amenorrhea (absence of at least 3 consecutive menstrual cycles) Bulimia Nervosa One-fourth of patients w/ bulimia nervosa have comorbid _____. - Kleptomania What temporal component is required for diagnosis of bulimia nervosa? - Binge eating and compensatory behaviors occur at least twice a week for 3 months According to DSM-IV, what is the most diagnostic feature of bulimia nervosa? - Recurrent episodes of binge eating What is the mechanism of sibutramine in the treatment of binge-eating disorder? - Inhibits reuptake of norepinephrine, serotonin, and dopamine Describe the required temporal component to bulimia nervosa. - Binge eating and inappropriate compensatory behaviors both occur, on average, at least twice a week for 3 months What is the only SSRI approved by the FDA for the treatment of bulimia nervosa? - Fluoxetine
SOMATOFORM DISORDERS Name 5 types of somatoform disorders. - Somatization disorder - conversion disorder - pain disorder - body dysmorphic disorder - hypochondriasis Describe the 8 required symptoms for diagnosis of somatoform disorder. - 4 pain; 2 gastrointestinal; 1 sexual; 1 pseudo-neurological Somatoform disorder typically presents prior to _____ years of age. - 30 Somatization Disorder
What age of onset is required for diagnosis of somatization disorder? - Onset prior to age 30 What 8 symptoms are required for somatization disorder? - 4 pain symptoms; 2 gastrointestinal symptoms; 1 sexual/reproductive symptom; 1 pseudoneurological symptom, not limited to pain Conversion Disorder Define globus hystericus. - The sensation of a lump in the throat experienced by many patients w/ conversion disorder Pain Disorder What are 2 subtypes of pain disorder? - Pain a/w psychological factors - pain a/w both psychological factors an a general medical condition Body Dysmorphic Diosrder Hypochondriasis One particular form of hypochondriasis, illness phobia, has been reported to respond to _____. - Imipramine What is the treatment of choice for body dysmorphic disorder and hypochondriasis? - SSRIs (T/F) Hypochondriasis is the only somatoform disorder that does not have a higher frequency in women. - True Factitious Disorder vs. Malingering What distinguishes factitious disorder from malingering? - Factitious disorder lacks secondary gain
PERSONALITY DISORDERS Personality disorders cannot be diagnosed before _____ years of age. - 18.0 Cluster A = Weird; Acusatory, Aloof, Awkward - Paranoid What is the treatment of choice for paranoid personality disorder? - Psychotherapy - Schizoid (T/F) There is no increase in incidence of schizoid personality disorder in families w/ history of schizophrenia. - True - Schizotypal Cluster B = wild; bad to the bone - Antisocial What form of psychotherapy has been singularly unhelpful in patients w/ antisocial personality disorder? - Psychodynamic psychotherapy This will never be the right answer on the test would fit in dysthymia or personality disorders, adjustment disorders, GAD. This is the insight oriented therapy; once in a while MDD. Development of a _____ disorder becomes more common in patients w/ antisocial personality disorder as they grow older. - Somatization What 2 age-related criteria must be met for the diagnosis of antisocial personality disorder? - Pattern of disregard for others and violations of the rights of others since age 15; patients must be at least 18 years old for the diagnosis
What type of therapy is recommended to treat both antisocial and borderline personality disorders? - Dialectical behavior therapy (DBT) Borderline What personality disorder is found in up to 70% of patients w/ dissociative identity disorder? - Borderline personality disorder What personality disorder presents w/ transient, stress-related psychotic experiences? - Borderline personality disorder Histrionic What defense mechanism is often employed by histrionic patients? - Regression Narcissistic
Cluster C = worried; cowardly, compulsive, clingy - Avoidant - Dependent - Obsessive compulsive personality disorder - Passive Aggressive
COGNITIVE DISORDERS Name 3 major cognitive disorders. - Delirium - Dementia o Alzheimer Disease o Vascular Dementia o AIDS Dementia Complex - amnestic disorder o Wernicke-Korsakoff Delirium Describe the AEIOU TIPSS mnemonic for causes of delirium. - Alcohol/drug toxicity - Electrolyte abnormality - Iatrogenic - Oxygen hypoxia - Uremia/hepatic encephalopathy - Trauma - Infection - Poisons - Seizures - Stroke What condition is described by delirium, tachycardia, tremor, and thyromegaly? - Thyrotoxicosis Along w/ delirium, what other 2 symptoms are often present in hypertensive encephalopathy? - Elevated blood pressure - papilledema What class of medications should be avoided in delirious patients? - Benzodiazepines What medication can be used to treat anticholingeric delirium caused by TCAs and some neuroleptic drugs? - Bethanechol (T/F) As a general rule, olfactory and tactile hallucinations are more common w/ medical conditions rather than psychosis. - True What are the 3 characteristics of Wernicke encephalopathy?
- Delirium; ophthalmoplegia; ataxia What test is sensitive in determining the etiology of delirium? - Electroencephalogram (EEG) What antibiotic is a/w psychosis? - Isoniazid Differentiate between hallucinations and illusions. - Hallucinations: sensory perception that occur in the absence of actual stimulus - illusions: inaccurate perception of existing sensory stimuli What 2 drugs should be considered to calm agitated delirious patients? - Haloperidol IM, PO, IV - second-generation antipsychotic (e.g. risperidone) Dementia What are the "4 A's" of dementia? - Aphasia - Amnesia - Apraxia - Agnosia Differentiate between agnosia and apraxia. - Agnosia: failure to recognize or identify objects despite intact sensory function - apraxia: impaired ability to carry out motor activities despite intact motor function Mild memory changes that occur w/ normal aging are called _____. - Benign senescent forgetfulness What type of imaging is used to distinguish Alzheimer's from other forms of dementia? - Fluorodeoxyglucose PET imaging, which shows characteristic temporal and parietal hypometabolism What is mild cognitive impairment (MCI)? - Prodromal state in which 12% of patients each year progress to dementia Name 4 characteristics of Wernicke's encephalopathy. - Ophthalmoplegia - ataxic gait - nystagmus - mental confusion What 2 forms of dementia present w/ cogwheel rigidity and resting tremor? - Lewy body dementia - Parkinson disease What endocrinologic disorder can cause reversible dementia? - Hypothyroidism Alzheimers Disease What are 3 genes considered linked to Alzheimer's disease? - Presenelin I; presenelin II; amyloid precursor protein (APP) What is the major Alzheimer's susceptibility gene? - Apolipoprotein e4 (APOe4) Name 3 cholinesterase inhibitors used to treat Alzheimer's disease. - Donepezil; rivastigmine; galantamine _____ is an NMDA antagonist approved for the treatment of moderate-to-severe Alzheimer's disease. - Memantine What are 3 anticholinesterase inhibitors used in the treatment of dementia? - Rivastigmine; galantamine; donepezil Lewy Body Dementia What are 4 characteristics of Lewy body dementia? - Waxing/waning - Parkinsonism - visual hallucinations - sensitivity to neuroleptics
How can Lewy body dementia be differentiated from Parkinson disease dementia? - Lewy body dementia: onset of dementia within 12 months of parkinsonism symptoms - Parkinson disease dementia: dementia that begins more than 12 months after the parkinsonism symptoms What medication is used to treat the REM sleep behavior disorder a/w Lewy body dementia? - Clonazepam (Klonopin) Frontotemporal Dementia Frontotemporal dementia is also known as _____. - Pick disease Huntingtons Disease Describe the pathology of Huntington's disease. - Trinucleotide repeat (CAG) on short arm of chromosome 4 What MRI finding is characteristic of Huntington's disease? - Caudate atrophy (T/F) Dementia due to Parkinson disease is exacerbated by antipsychotic medications. - True Describe the pathology a/w Parkinson disease. - Loss of cells in the substantia nigra of the basal ganglia, causing a decrease in dopamine and loss of the dopaminergic tracts Cruetzfeldt Jakob Disease What symptom is present in over 90% of pts w/ Creutzfeldt-Jakob disease (CJD)? - Myoclonus (sudden spasms of muscles) What EEG finding is consistent w/ Creutzfeldt-Jakob disease? - Triphasic complexes Normal Pressure Hydrocephalus Name 3 characteristic symptoms of normal pressure hydrocephalus. - Ataxia; urinary incontinence; dementia
SUBSTANCE ABUSE AND DEPENDENCE Substance Abuse/Withdrawal What 4 criteria define substance abuse? - Failure to fulfill obligations at work, school, or home - use in dangerous situations - recurrent substance-related legal problems - continued use despite social or interpersonal problems due to the substance use Opioids What 2 opioids will not be detected on a standard drug screen? - Methadone - oxycodone What drug combinations are present in Vicodin and Percocet? - Vicodin: hydrocodone/acetaminophen - Percocet: oxycodone/acetaminophen How does meperidine intoxication differ from that of other opioids? - Meperidine produces mydriasis in contrast to other opioids, which produce miosis Meperidine and MAOIs taken in combination may cause _____. - Serotonin syndrome o Sweating, muscle contractions, shivering, CNS symptoms (confusion, disorientation, hypomania, apprehension, agitation, seizures) What is the danger of administering naloxone/naltrexone in opioid overdose? - May cause severe withdrawal in opioid-dependent patients What drug can be used to treat the autonomic symptoms experienced during opioid withdrawal?
- Clonidine Alcohol Describe the effect of alcohol on GABA and glutamate receptors. - Alcohol activates GABA receptors (inhibitory) and inhibits glutamate receptors (excitatory) What class of drugs is used to treat acute alcohol withdrawal? - Benzodiazepines (often chlordiazepoxide) What electrolyte abnormality may predispose to development of delirium tremens (DTs)? - Hypomagnesemia What is the time window for development of DTs? - 48 - 72 hours What defines "at-risk" or "heavy" drinking? - Men: > 4 drinks per day or > 14 drinks per week - women: > 3 drinks day or > 7 drinks per week Name 4 medications used to treat alcohol dependence. - Disulfiram; naltrexone; acamprosate; topiramate What is the function of topiramate? - Anticonvulsant that potentiates GABA and inhibits glutamate receptors, reducing the craving for alcohol What is the major advantage of acamprosate? - Can be used in patients w/ liver disease Name 3 characteristics of Wernicke's encephalopathy. - Broad-based ataxia; confusion; nystagmus PCP Describe the pharmacologic effect of PCP. - Antagonizes NMDA glutamate receptors and activates dopaminergic neurons What symptom is pathognomonic for PCP intoxication? - Rotary nystagmus Name 2 serum markers often elevated during PCP use. - Creatine phosphokinase (CPK) - aspartate aminotransferase (AST) What 3 benzodiazepines are indicated in the treatment of PCP intoxication? - Diazepam; midazolam; lorazepam Why should typical antipsychotics and benzodiazepines be avoided in PCP intoxication pts? - Antipsychotics: anticholinergic side effects can worsen side effects - benzodiazepines: may delay excretion of the drug BZD/Barbiturates Differentiate between the effects of benzodiazepines and barbiturates on chloride channel opening. - Barbiturates: increases the duration of chloride channel opening - benzodiazepines: increases the frequency of chloride channel opening What type of drug withdrawal has the highest mortality rate? - Barbiturate What short-acting benzodiazepine antagonist can be used to treat benzodiazepine overdose? - Flumazenil What is the treatment of choice for opioid overdose? - Naloxone Describe the treatment for barbiturate overdose. - Alkalinize the urine w/ sodium bicarbonate to promote renal excretion Name 3 benzodiazepines that are not cleared by the liver and may be used in pts w/ chronic alcoholism or liver disease. - Lorazepam, oxazepam, temazepam; LOT Name 2 long-acting (> 20 hrs) benzodiazepines. - Diazepam; clonazepam Avoid clonazepam in pts w/ _____. - Renal dysfunction
What are 4 intermediate-acting (6 - 20 hrs) benzodiazepines? - Alprazolam; lorazepam; oxazepam; temazepam Name 2 short-acting (< 6 hrs) benzodiazepines. Triazolam; midazolam Marijuana What is the physiological effect of THC in the brain? - Activation of cannabinoid receptors, which inhibit adenylate cyclase Stimulants What is the pharmacologic effect of cocaine? - Block dopamine re-uptake from the synaptic cleft, causing a stimulant effect Describe the pharmacologic effect of amphetamines. - Block re-uptake and facilitate release of dopamine and norepinephrine from nerve endings, causing a stimulant effect Describe the physiologic effect of caffeine. - Adenosine antagonist, causing an increase in cAMP and a stimulant effect via the dopaminergic system Name 2 medications used to treat nicotine dependence. - Varenicline (Chantix) - buproprion (Zyban) What is the mechanism of varenicline? - Alpha-4-beta-2 nicotinic cholinergic receptor (nAChR) partial agonist that mimics the action of nicotine and prevents withdrawal symptoms Define formication. - A hallucinated sensation that insects or snakes are crawling over the skin - common side effect of extensive use of cocaine and amphetamines SLEEP Describe the changes in REM and non-REM sleep seen in the elderly. - Decreased REM latency and decreased total REM; increased amounts of stage 1/2 sleep and decreased amounts of stage 3/4 sleep Describe the half-lives of the non-benzodiazepine hypnotics. - Zaleplon < zolpidem < eszopiclone What is the mechanism of the non-benzodiazepine hypnotics? - Selective receptor binding to benzodiazepine receptor 1 What is ramelteon? - Selective melatonin MT1/MT2 agonist Differentiate between dyssomnias and parasomnias. - Dyssomnias: insufficient, excessive, or altered timing of sleep - parasomnias: unusual sleep-related behavior What is the temporal distinction between acute and chronic insomnia? - Acute: 1 month What is considered first-line treatment for chronic insomnia? - CBT Name the 3 "Z drugs" used to treat primary insomnia. - Zolpidem (Ambien); eszopiclone (Lunesta); zaleplon (Sonata) Name 3 antidepressants used to treat primary insomnia. - Trazodone (most common); amitriptyline; doxepin What are 3 risk factors for obstructive sleep apnea? - Obesity - increased neck circumference - airway narrowing Describe the classic tetrad a/w narcolepsy. - Excessive daytime sleepiness ("sleep attacks") - REM-related sleep phenomenon including inability to move during the transition from sleep to wakefulness - hypnagogic/hypnopompic hallucinations
- cataplexy What is cataplexy? - Sudden loss of muscle tone evoked by strong emotion w/o LOC What is the drug of choice to treat cataplexy in narcoleptic pts? - Sodium oxybate Define Kleine-Levin syndrome. - Rare disorder characterized by recurrent hypersomnia w/ episodes of daytime sleepiness w/ hyperphagia, hypersexuality, and aggression Name 4 circadian rhythm sleep disorders. - Delayed sleep phase disorder - advanced sleep phase disorder - shift-work disorder - jet lag disorder Describe image rehearsal training (IRT). - Involves the use of mental imagery to modify the outcome of a recurrent nightmare, writing down the improved outcome, and then mentally rehearsing it in a relaxed state REM Sleep Disorder Characterize REM sleep behavior disorder. - Characterized by muscle atonia during REM sleep and complex motor activity a/w dream mentation (dream enactment) What 2 types of dementia are a/w REM sleep behavior disorder? - Olivopontocerebellar atrophy - Lewy body dementia What benzodiazepine is efficacious in 90% of pts w/ REM sleep behavior disorder? - Clonazapam
RANDOMNESS What 4 dissociative disorders are described in DSM-IV? - Dissociative amnesia - dissociative fugue - dissociative identity disorder - depersonalization disorder What condition has the worst prognosis of all the dissociative disorders? - Dissociative identity disorder What are the 3 criteria for delusional disorder? - Nonbizarre, fixed delusions for at least 1 month - does not meet criteria for schizophrenia - functioning in life not severely impaired What is selective mutism? - Rare condition characterized by refusal to speak in certain situations (e.g. school) for at least 1 month despite the ability to comprehend and use language What is Ganser syndrome? - The giving of approximate answers to simple questions What is ataque de nervios? - Culturally-bound trance disorder common in Puerto Rico that consists of convulsive movements, fainting, crying, and visual problems What are the 5 stages of normal sexual response? - Desire; excitement; plateau; orgasm; resolution
What are the 3 most common paraphilias? - Pedophilia; voyeurism; exhibitionism The most important factor in assessing a patient's risk of violence is _____. - Individual's history of violence Describe reaction formation. - A defense mechanism by which an individual deals w/ emotional conflict or stressors by substituting behavior, thoughts, or feelings that are diametrically opposed to his or her own unacceptable thoughts or feelings
Medication Adverse Reactions What are HAM side effects? - antiHistamine (sedation, weight gain) - antiAdrenergic (hypotension) - antiMuscarinic (dry mouth, blurred vision, urinary retention) HAM side effects are found w/ what 2 classes of psychiatric medications? - TCAs; low-potency antipsychotics Extra-Pyramidal Side Effects What is the drug of choice to treat EPS produced by neuroleptics? - Benztropine Describe 3 forms of EPS. - Parkinsonism (masklike face, cogwheel rigidity, pill-rolling tremor) - akathisia (restlessness, agitation) - dystonia (sustained contraction of muscles of neck, tongue, eyes, diaphragm) Name 3 medications that may be used to treat EPS. - Benztropine - Diphenhydramine - amantadine What scale is used to quantify and monitor for tardive dyskinesia? - Abnormal Involuntary Movement Scale (AIMS) What medication may be used to treat akathisia? - Propranolol Neuroleptic Malignant Syndrome What are 2 characteristic features of neuroleptic malignant syndrome? - Elevated creatine phosphokinase (CPK) - "lead pipe" rigidity What 2 medications are commonly used to treat NMS? - Dantrolene - bromocriptine Serotonin Syndrome Describe the neuromuscular excitability a/w serotonin syndrome. - Hyperreflexia; "electric jolt" limb movements What class of medications may be useful in treating serotonin syndrome? - Calcium channel blockers (e.g. nifedipine) Wait at least _____ before switching from SSRI to MAOI, and at least _____ w/ fluoxetine. - 2 weeks; 5 - 6 weeks Drug Interactions Name 4 important inducers of the CYP450 enzyme. - Smoking (1A2) - carbamazepine (1A2, 2C9, 3A4)
- barbituates (2C9) - St. John's wort (2C19, 3A4) What are 5 important inhibitors of the CYP450 enzyme? - Fluvoxamine (1A2, 2D6, 3A4) - fluoxetine (2C19, 2C9, 2D6) - paroxetine (2D6) - duloxetine (2D6) - sertraline (2C19) SSRIs What SSRI has a weekly dosing form available? - Fluoxetine What SSRI has the highest risk for GI disturbances? - Sertraline Name 7 SSRIs. - Fluoxetin; sertraline; paroxetine; fluvoxamine; citalopram; escitalopram What SSRI is currently only approved for the treatment of OCD? - Fluvoxamine What SSRI is preferred in the treatment of intermittent explosive disorder? - Fluoxetine Low levels of what neurotransmitter is a/w impulsiveness and aggression? - Serotonin What class of SSRI-related side effects may occur later in the treatment course? - Sexual dysfunction poor libido, anorgasmia SNRIs Name 2 SNRIs. - Venlafaxine; duloxetine What are 3 clinical indications for venlafaxine? - Depression - anxiety disorders (e.g. GAD) - ADHD Duloxetine is often used for patients w/ depression and _____. - Neuropathic pain What contraindication is a/w venlafaxine? - May increase BP; do not use in pts w/ untreated for labile HTN NDRI Describe the mechanism of bupropion. - Norepinephrine-dopamine reuptake inhibitor it is so stimulating, Ive had patients have spontaneous orgasms on it. Stimulating, seizure threshold. Other Antidepressants What are 3 clinical indications for trazodone and nefazodone? - Refractory major depression; major depression w/ anxiety; insomnia What major adverse effect is a/w trazodone? Nefazodone? - Trazodone: priaprism - nefazodone: liver failure Describe the mechanism of mirtazapine. - 2-adrenergic receptor antagonist o first SNRI to enter the market as opposed to Prozac minor weight gain, sedation o all of the SSRIs and all of the SNRIs amphetamines, topiramate, and bupropion dont cause weight gain. Tricyclic Antidepressants
Describe the mechanism of tricyclic antidepressants. - Inhibit reuptake of norepinephrine and serotonin, increasing availability of monoamines in the synapse Name 7 tricyclic antidepressants and their subcategories. - Tertiary amines: amitriptyline, imipramine, clomipramine, doxepin; secondary amines: nortriptyline, desipramine What TCA may be used to treat insomnia? - Doxepin What are 2 clinical indications for use of imipramine? - Enuresis; panic disorder What TCA has the least anticholinergic side effects? - Desipramine What TCA is least likely to cause orthostatic hypotension? - Nortriptyline The mainstay of treatment for TCA overdose is _____. - IV sodium bicarbonate Name 2 tetracyclic antidepressants. - Amoxapine; maprotiline What are the "3 C's" of TCA side effects? - Cardiotoxicity - Convulsions - Coma What tricyclic antidepressant is preferred for use in the elderly population? - Nortriptyline, as it has the fewest side effects TCA absolute contraindication to TCA is glaucoma can exacerbate closed angle decrease reabsorption; 1015% of glaucoma is narrow angle. Mono-Amine Oxidase Inhibitors Describe the mechanism of MAOIs. - Prevent the inactivation of biogenic amines such as norepinephrine, serotonin, dopamine, and tyramine by irreversibly inhibiting the MAO-A/B enzymes Describe the selectivity of MAO-A and MAO-B enzymes. - MAO-A preferentially deactivates serotonin and MAO-B preferentially deactivates norepinephrine; both types also act on dopamine and tyramine MAOIs are considered more effective in treating _____ depression, characterized by hypersomnia, increased appetite, and increased sensitivity to interpersonal rejection. - Atypical Name 3 MAOIs. - Phenelzine; tranylcypromine; isocarboxazid What is the most common side effect of MAOIs? - Orthostatic hypotension Antipsychotics Quetiapine sedating Name 6 atypical antipsychotic medications. - Clozapine; risperidone; quetiapine; olanzapine; ziprasidone; aripiprazole _____ is the only antipsychotic that has been proven to decrease the risk of suicide. - Clozapine (T/F) 30% of treatment-resistant psychosis will respond to clozapine. - true Differentiate between the mechanism of typical and atypical antipsychotics. - Typical: block dopamine (D2) receptors; atypical: block both dopamine (D2) and serotonin (2A) receptors (T/F) Atypical antipsychotics may be more effective in treating negative psychotic sx, such as flattened affect and social withdrawal. - true Name 2 low potency typical antipsychotic medications and the pigment-related side affects a/w each. - Chlorpromazine (bluish skin discoloration)
thioridazine (retinitis pigmentosa) _____ may be used to treat intractable hiccups. - Chlorpromazine Why are low potency typical antipsychotics more lethal in overdose than mid- and high-potency typical antipsychotics? - QTc prolongation and potential for heart block and ventricular tachycardia Name 4 mid-potency typical antipsychotics. - Loxapine; thiothixene; trifluoperazine; perphenazine Name 3 high-potency typical antipsychotics. developed for the treatment of psychosis - Haloperidol; fluphenazine; pimozide What 2 first-generation antipsychotic medications are a/w ocular abnormalities? - Thioridazine: irreversible retinal pigmentation - chlorpromazine: deposits in lens and cornea A risk of agranulocytosis, requiring weekly prophylactic blood draws, is a/w _____. - Clozapine What 2 atypical antipsychotic medications are most a/w metabolic syndrome? - Clozapine; olanzapine o Olanzapine = causes WEIGHT gain average of 25 lbs weight gain. What atypical antipsychotic is considered "weight neutral"? - Ziprasidone What atypical antipsychotic is a/w elevated prolactin levels? Risperidone Differentiate between the mechanism of typical and atypical antipsychotics. - Typical: block dopamine (D2) receptors - atypical: block both dopamine (D2) and serotonin (2A) receptors (T/F) Atypical antipsychotics may be more effective in treating negative psychotic sx, such as flattened affect and social withdrawal. - true Mood Stabilization Name 4 mood stabilizers. - Lithium; valproic acid; lamotrigine; carbamazepine Describe the therapeutic, toxic, and lethal ranges of lithium. - Therapeutic: 0.6 - 1.2; toxic: > 1.5; lethal: > 2.0 Lithium thyroid function tests to get baseline, EKG can exacerbate existing arrhythmias, kidney function KNOW lithium b/c it is the gold standard Most of the time you are starting lithium on manic patient. What is the effect of concurrent NSAID use w/ lithium? - increased lithium levels What is the only mood stabilizer w/ FDA approval for treatment of bipolar disorder in children older than 12? - Lithium Lithium Side Effects: - weight gain, tremor, GI disturbances (anal ulcers, lip lesions, N/V, anything in between), fatigue, arrhtyhmias, seizures, goiter/hypothyroidism, leukocytosis (benign) may be used to increase WBC in clozapine users, coma, polyuria, polydipsia, alopecia, metallic taste - Acute: nausea with or without vomiting, fine tremor, polyuria, mild confusion, t-wave EKG changes, muscle weakness o Then: coarse tremor, ataxia, confusion, slurred speech, persistent nausea and diarrhea o Then: convulsions, hypotension, irregular heart beat, coma - Chronic: nephrogenic DI, hypothyroidism/goiter, weight gain, edema, rashes and aggravation of skin conditions (acne, psoriasis), benign leukocytosis, teratogen (ebsteins anomaly)
In cases of bipolar disorder where the use of lithium is contraindicated, what is the drug of choice? - Valproic acid Describe the clinical indication for use of carbamazepine.
Especially useful in treating mixed episodes and rapid-cycling bipolar disorder, and less effective for the depressed phase Describe the mechanism of carbamazepine. - Acts by blocking sodium channels and inhibiting action potentials What are 2 catastrophic side effects of carbamazepine? - Stevens-Johnson syndrome - teratogenic effects when used during pregnancy Describe the mechanism of lamotrigine. - Effective on sodium channels that modulate glutamate and aspartate Lamotrigine is most efficacious for treating _____. - Bipolar depression (though little efficacy for acute mania or prevention of mania) Name 3 side effects of topiramate. - Weight loss; hypochloremic non-anion gap metabolic acidosis; kidney stones Legal What are the "4 D's" of malpractice? - Deviation (neglect) from Duty that was the Direct cause of Damage In what 3 situations is informed consent not required to treat unemancipated minors? - Obstetric care - STD treatment - substance abuse treatment What are the "4 R's" of informed consent? - Reason for treatment - Risks and benefits - Reasonable alternatives - Refused treatment consequences Under what 4 conditions are minors considered emancipated? - Self-supporting - in the military - married - have children Differentiate between capacity and competence. - Capacity: clinical term and may be assessed by physicians - competence: legal term and can be decided only by a judge (T/F) Decisional capacity is task specific and can fluctuate over time. - true What is Parens Patriae? - Legal principle that supports involuntary commitment of citizens who cannot care for themselves What is the M'Naghten test? - Most stringent test used as a standard of the insanity defense; indicates person does not understand what he/she was doing or its wrongfulness
DSM-IV diagnostic Criteria Psychotic Disorders - Schizophrenia 2 or more for at least 1 month with total disease > 6 months causing significant social/occupational functional deterioration o delusions, hallucinations, disorganized speech, grossly disorganized or catatonic behavior, negative symptoms (anhedonia, flattened or inappropriate affect, alogia (poverty of speech), avolition (apathy), attention poor) when she writes on schizophrenia, she writes on 4As. Ambivalence Allusions (delusions/hallucinations) Affect flattened or inappropriate Association (tangentiality) o tx 4 weeks before efficacy determined - Brief psychotic disorder - < 1 month - Schizophreniform 1-6 months - Schizoaffective disorder major depressive, manic, or mixed episode + delusions or hallucinations for 2 weeks in the absence of mood d/o sx. o Tx: antipsychotics, mood stabilizers, antidepressants, ECT for depression/mania - Delusional Disorder non-bizarre, fixed delusions for > 1 month, but does not meet criteria for schizophrenia and functioning in life is not significantly impaired. - Shared Psychotic Disorder tx: separate; psychotherapy + antipsychotics if sx do not improve 12 weeks after separation - Koro asia penis shrinking and will disappear = death - Amok Malaysia, SE Asia sudden unprovoked outbursts of violence w/ no recollection often commits suicide afterwards - Brain Fag Africa HA, fatigue, visual disturbances in male students Mood Disorders (symptoms with depression as a symptom) - Major Depressive Disorder: o At least one episode of Major Depression: 5/9 sx w/ one being depression or anhedonia for at least 2 weeks. Sleep, psychomotor, appetite, concentration, energy, depression, interest, guilt, suicidal ideations o Without mania/hypomania o With psychotic features ECT alone (better when rapid response is needed) or antidepressant + antipsychotic - Bipolar I o One manic or mixed episode (depression NOT required for dx) Mania = 3 of the following for at least 1 week: distractability, insomnia, grandiosity, flight of ideas, activity/agitation, speech pressured, thoughtlessness (or 4, with irritable mood) Mixed = mania/depression sx present for at least 1 week - Bipolar II o Recurrent major depressive episodes with HYPOmania Hypomania at least 4 days; no marked impairment in social or occupational functioning, no psychotic features; does not require hospitalization - Dysthymic Disorder 2 or more of the following symptoms for at least 2 years (or 1 year in children), not without symptoms for > 2 months at a time, with no major depressive episode
CHASES concentration, hopelessness, appetite (+/-), sleep (+/-), Energy low, selfesteem low o NEVER have psychotic features Double Depression MDD with dysthymic d/o during residual periods. Tx: cognitive therapy and insight oriented psychotherapy; antidepressants concurrently Cyclothymic Disorder alternating periods of hypomania/mild-moderate depressive sx. o Numerous periods of hypomania/depressive sx for > 2 years with no asx periods > 2 months and no hx of major depressive or manic episodes. minor depressive disorder depressive sx that do not meet criteria for MDD, with euthymic periods (unlike dysthymic disorder) Adjustment disorder with depressed mood Secondary to a medical disorder o MSE: affect labile (sudden rapid shifts congruent with mood), TP irrelevant, TC frank visual hallucinations (not hypnogognic/hypnopompnic) have a metabolic, toxic or structural property unless proven otherwise. The one exception visual hallucinations of knee-high men (I see little men, sometimes green) = malingering, Intellectual function concentration is often the first thing to go and the rest of the exam is questionable Secondary to substance disorder
MSE: TP irrelevant = depression secondary to medical disorder, loosening and tangentiality and concretism ANXIETY AND ADJUSTMENT DISORDERS - Panic Disorder at least 1 Spontaneous, recurrent panic attack followed by at least 1 month of the following: worrying about recurrence, worry about implications of the attack, significant change in behavior related to attack o Panic attack = intense fear and discomfort plus 4 of the following symptoms that peaks in several minutes; subside w/i 25 min. (10-20 minutes maximum for chest pain/pulmonary) rarely > 1 hr Palpitations Abdominal distress Numbness, Nausea Intense fear of death; sense of impending doom Choking, Chills, Chest pain Sweating, Shaking, SOB o Rule Out: Asthma Breathing - COPD Cardiac (MVP, arrhythmia, CHF) Drugs (cocaine, amphetamines, caffeine, nicotine, hallucinogen intoxication; alcohol or opiate withdrawal) Endocrine (thyroid, pheochromocytoma) - Agoraphobia anxiety about being in places/situations where escape may be difficult; situations are either avoided, endured with distress, or faced only with companion; sx not otherwise explainable. Tx: SSRI - Specific Phobias
Persistent excessive fear brought on by specific situation/object where exposure brings immediate anxiety, pt recognizes fear is excessive, situation is avoided when possible, and if person < 18 yo, sx for at least 6 months Tx: systematic desensitization and supportive psychotherapy Straight behavioral therapy = flooding or desensitization Cognitive behavioral therapy = not either of these. USE FOR DEPRESSION BZD or beta blockers (short course) Social Phobias same as specific w/ fear related to social setting where embarrassment or humiliation may occur. o Paroxetine = social anxiety disorder Obsessive Compulsive Disorder obsessions and compulsions that the person is aware are unreasonable and excessive; cause marked distress, are time consuming, or significantly interfere with daily functioning. Tx: SSRI, clomipramine, behavioral therapy (exposure and response prevention) PTSD response to life-threatening traumatic experience where patient re-experiences the trauma, avoids reminders of the event, and experiences emotional numbing or hyperarousal (difficulty sleeping, outbursts of anger, exaggeurated startle response, difficulty concentrating) with symptoms present for at least 1 month and may occur any time after experience Acute Stress Disorder major life-threatening traumatic event but anxiety symptoms for only a short duration: event occurred < 1 month ago and symptoms last < 1 month Generalized Anxiety Disorder excessive persistent anxiety about daily events and activities with hyperarousal for at least 6 months o Must be associated with 3 or more of the following: restlessness, fatigue, difficulty concentrating, irritability, sleep disturbance, muscle tension o Tx: buspar, BZD (should be tapered off ASAP), SSRI +/- CBT, venlafaxine o Free floating anxiety does not involve any specific person, event, or activity Adjustment Disorders development of emotional or behavioral symptoms within 2 months after a stressful but non-life threatening event (severe distress in excess of what would be expected after such an event with significant impact in daily functioning and sx are NOT those of bereavement. o Sx resolve within 6 months of termination of stressor o Tx: supportive psychotherapy most helpful; group therapy; pharmacotherapy for associated symptoms
PERSONALITY DISORDERS Cluster A: Accusatory, aloof, awkward - Paranoid 4 or more of the following: o Suspicion w/o evidence of exploitation/deception o preoccupation with doubts of loyalty or trustworthiness o Reluctance to confide in others o Interpretation of benign remarks as threatening or demeaning o Persistence of grudges o Perception of attacks on his/her character that are not apparent to others/quick to counterattack o Recurrence of suspicions regarding fidelity of spouse/lover - Schizoid no desire for close relationships - 4 or more of the following o Neither enjoying nor desiring close relationships
o Generally chosing solitary activities o Little interest in sexual activity o Taking pleasure in few activities o Few close friends or confidants o Indifference to praise or criticism o Emotional coldness, detachment, or flattened affect Schizotypal magical thinking, eccentric behavior, peculiar thought processes. 5 or more of the following: o Ideas of reference o Odd beliefs or magical thinking, inconsistent with cultural norms o Suspiciousness o Inappropriate or restricted affect o Odd or eccentric appearance/behavior o Few close friends or confidants o Odd thinking or speech (vague, stereotyped) o Excessive social anxiety
Cluster B: Bad - Antisocial pattern of disregard and violation of rights of others since age 15, and patient is at least 18 years old. (R/O drug abuse difficult to determine which came first); Begins in childhood as conduct disorder. 3 or more of the following should be present: o Failure to conform to social norms by committing unlawful acts o Deceitfulness/repeated lying/manipulating others for personal gain o Impulsivity/failure to plan ahead o Irritability and aggressiveness/repeated fights or assaults o Recklessness and disregard for safety of others and self o Irresponsibility/failure to sustain work or honor financial obligations o Lack of remorse for actions - Narcissistic superiority, need for admiration; consider themselves special and will exploit others for personal gain, but fragile self esteems; antidepressants or lithium may be used as needed if co-morbid mood d/o exists; and at least 5 of the following: o Exaggerated sense of self-importance o Preoccupation with fantasies of unlimited money, success, brilliance o Belief that he or she is special or unique and can associate only with other high-status individuals o Needs excessive admiration o Sense of entitlement o Takes advantage of others for self-gain o Lacks empathy o Envois or others or believes others are envious of him/her o Arrogant or haughty - Histrionic Tx: psychotherapy, pharmacotherapy for depressive/anxiety sx as necessary attention-seeking, flamboyant behavior unable to form long-lasting, meaningful relationships with at least 5 of the following: o Uncomfortable when not the center of attention o Inappropriately seductive or provocative o Uses physical appearance to draw attention to self o Has speech that is impressionistic and lacking in detail
o Theatrical and exaggerated expression of emotion o Easily influence by others or situation o Perceives relationships as more intimate than they actually are Borderline on the borderline of neurosis and psychosis Tx: DBT, with pharmacotherapy to treat psychotic and depressive symptoms as necessary (low dose antipsychotic or SSRI pharmacotherapy more effective in BPD than any other PD) - at least 5 of the following must be present: o Impulsive in at least 2 harmful ways (spending, sexual activity, substance abuse) o Moody/unstable affect o Paranoid under stress transient stress-related paranoid ideation or dissociative symptoms o Unstable body image o Labile, intense relationships o Suicidal recurrent threats or self-mutilation o Inappropriate anger o Vulnerable to abandonment o Emptiness
Cluster C: cowardly, compulsive, clingy - Avoidant desire companionship but are extremely shy and easily injured; cling to relationships but SLOW to get involved; 4 or more of the following: o Avoids occupation that involves interpersonal contact due to fear of criticism or rejection o Unwilling to interact unless certain of being liked o Cautious of interpersonal relationships o Preoccupied with being criticized or rejected in social situations o Inhibited in new social situations because he or she feels inadequate o Believes he or she is socially inept or inferior o Reluctant to engage in new activities for fear of embarrassment. - OCPD egosyntonic; motivated by work itself, vs. narcissistic who are motivated by status. preoccupation with orderliness, control, and perfectionism at the expense of efficiency, present in early adulthood in a variety of contexts. at least 4 of the following: o Preoccupation with details, rules, lists, and organization such that the major point of the activity is lost o Perfectionism that is detrimental to the completion of task o Excessive devotion to work o Excessive conscientiousness and scrupulousness about morals and ethics o Will not delegate tasks o Unable to discard worthless objects. o Miserly o Rigid and stubborn. - Dependent must manifest by early adulthood. cling to relationships, but actively and aggressively seek relationships; Submissive and clinging behavior with excessive need to be cared for with at least 5 of the following: o Difficulty making everyday decisions without reassurance from others o Needs others to assume responsibilities for most areas of life o Cannot express disagreement due to fear of loss of approval o Difficulty initiating projects due to lack of self-confidence
o o o o
Goes to excessive lengths to obtain support from others Feels helpless when alone Urgently seeks another relationship when one ends Preoccupation with fears of being left to take care of self.
COGNITIVE DISORDERS - Cortical Dementias = decline in intellectual functioning o Alzheimers memory impairment plus at least 1: apraxia, aphasia, agnosia, diminished executive functioning Apraxia = cant do Practiced movements even though motor system is intact Aphasia cant speek/understand phrases Agnosia cannot identify even though sensory system is intact o Multiinfarct = stepwise increase in severity, focal neuro signs Memory impairment plus at least 1: apraxia, aphasia, agnosia, diminished executive functioning Personality changes (depression, anger, suspiciousness common), but greater overall preservation of personality Paranoia also common o Picks/Frontotemporal Dementia slowly progressive Aphasia, apraxia, agnosia Personality and behavior changes are more prominent early in disease vs. alzheimers. Disinhibited or more apathetic. Atrophy of frontotemporal lobes, pick bodies (intraneuronal inclusion bodies) o CJD Rapidly progressive dementia (6-12 months) after onset of symptoms with myoclonus. May also have EPS, ataxia, cortical blindness, muscle atrophy, and mutism - Subcortical dementias prominent affective and movement symptoms. o Huntington Disease = choreiform movement, 35-50 yo, AD, hypertonicity, depression, psychosis, CAG repeat on Ch4, MRI with caudate atrophy o LBD/PD = cogwheel rigidity, resting tremor PD: bradykinesia, resting (pill rolling) tremor, cogwheel rigidity, masklike facial expression, shuffling gait, dysarthria (abnormal speech) LBD: visual hallucinations, REM sleep disturbances, PD symptoms, o NPH = ataxia, urinary incontinence, dilated ventricles Due to trauma, infection, hemorrhage. Tx with shunt o Hypothyroidism = obesity, coarse hair, constipation, cold intolerance o Vitamin B12 deficiency = diminished position/vibratory sense, megaloblasts o Wilsons Disease = tremor, abnormal LFT, kayser-fleischer rings o Neurosyphilis = diminished position/vibratory sense, Argyll-robertson pupils - Delirium detect with EEG (very sensitive to slowing of the waves) o Causes of Delirium = IM DELIRIOUS Impaired delivery of brain substrates (vascular insufficiency stroke) Metabolic Drugs Endocrinopathy Liver disease Infrastructure (structural disease of cortical neurons)
o o o o o o
Renal failure Infection Oxygen UTI Sensory deprivation After cardiac surgery age, alcohol, brain damage, diabetes CVA or mass lesion delirium + hemiparesis or other focal neuro ssx HTN encephalopathy elevated BP, papilledema, delirium Drug Intoxication dilated pupils, tachycardia, delirium Meningitis nuchal rigidity, photophobia, fever, delirium Thyrotoxicosis tachycardia, tremor, thyromegaly delirium
GERIATRIC - Pseudodementia o Apparent cognitive deficits in pts with major depression. o Onset is acute, patient emphasizes failures (vs. dementia where delights in accomplishments), sundowning uncommon (vs. dementia where common), often answers Dont know (vs. confabulation in dementia), aware of problems (vs. unaware in dementia) - Bereavement o Normal grief guilt and sadness, mild sleep disturbances and weight loss, illusions, attempts to resume daily activities/work, symptoms that resolve within 1 year, with the worse symptoms within 2 months o Abnormal grief (major depression) feelings of severe guilt or worthlessness, significant sleep disturbances or weight lsos, hallucinations or delusions, no attempt to resume activities, suicide ideation, persisting > 1 year with worse symptoms > 2 months CHILDREN have a lot of anxiety d/o, not as many mood d/o. - Mental Retardation Causes: o Down Syndrome o Anoxia (perinatal) o Prematurity o Birth trauma o Hypothyroidism o Malnutrition o Toxin exposure o trauma o Fragile X o TORCH infections and toxins - Learning disorders o Achievement in reading (boys), math (girls), or written expression lower than expected for age. Tx: remedial education - Pervasive developmental disorders o Autism kids appear to be developing normal until after 2 At least 6 symptoms must be present: at least 2 problems with social interaction at least 1 impairment in communication at least 1 repetitive and stereotyped pattern of behavior and activities
Asperger Impaired social interaction (at least 2) and restricted or steortyped behaviors, interests, or activites BUT NORMAL COMMUNICATION and cognitive development o Rett Normal prenatal and perinatal development, psychomotor development during first 5 months of life, normal initial head circumference with decreasing rate of head growth between 5-48 months loss of purposeful hand skills between 5-30 months with handwringing, handwashing, loss of social interaction, probelmsw ith gait or trunk mvmts, seizures, cyanotic spells, and severely impaired language and psychomotor development o Childhood disintegratice disorder Normal development in first 2 years of life with loss of previously acquired skills in at least two of the following areas: language, social skills, bowel or bladder control, play or motor skills. Also, at least two of the following: impaired social interaction, impaired use of language, or restricted, repetitive, and stereotyped behaviors and interests. MORE COMMON IN BOYS! (4-8xs) Disruptive behavioral disorders o Conduct disorders by self Major depression from conduct d/o in kids Failing in schools, stealing cars conduct disorder acting out in 2 places = conduct disorders Doing find in school, very obedient, stealing cars depression (acting out in one place = depression) Violation of basic rights of others or social norms and rules with at least 3 acts of: Aggression towards people or animals Destruction of property Deceitfulness/theft Serious violations of rules Tx: structure environment; pharmacotherapy (SSRI, lithium), behavior modification o Oppositional Defiant disorder after being told not to do something; something to which opposition is being demonstrated at least 6 months of negativistic, hostile, or defiant behavior during which at least 4 of the following are present: frequent loss of temper arguments with adults defying adults rules deliberately annoying people easily annoyed anger and resentment spiteful blaming others for mistakes or misbehaviors Tx: behavior modification and problem solving skills ADHD with and without hyperactivity know classes
Inattnetive, hyperactive-impulsive, OR combined type. At least 6 symptoms persisting for at least 6 months presenting before age 7 Inattention: Problems listening, concentrating, paying attention to details, organizing tasks Easily distracted, often forgetful. Hyperactivity/impulsivity: Blurting out, interrupting, fidgeting, leaving seat, talking excessively Tourette/Tic o Involuntary mvmt or vocalizations with tics occurring multiple times a day almost everyday for > 1 year with no tic free period > 3 months, with onset prior to age 18 and distress and impairment in social/occupational functioning Elimination o Enuresis involuntary voiding after age 5, which occurs at least twice a week for 3 months or with marked impairment. o Encopresis involuntary or intentional passage of feces in inappropriate places; must be at least 4 years old with at least once a month episodes for 3 months Selective Mutism o Not speaking in certain situations (school), with onset usually 5-6 years old and more common in girls. Present for at least 2 months KNOW normal child cling to child? Normally messy?
o o
DISSOCIATIVE - Dissociative Amnesia at least one episode of being unable to recall important personal information, usually involving traumatic or stressful event, which cannot be explained by ordinary forgetfulness, and symptoms cause distress or impairment in daily functioning (cannot be explained by another disorder, medical condition, or substance use). (often unable to recall name but will remember obscure details, vs. dementia pt who recalls name but not details) - Dissociative Fugue sudden, unexpected travel away from home or work plus the inability to recall ones past, with confusion about personal identity or assumption of new identify, NOT due to dissociative identity disorder or physiologic effects of a substance/medical disorder. Impairment in social or occupational fxn. - Dissociative Identity Disorder at least two or more distinct identities that recurrently take control of a persons behavior with the inability to recall personal information of one personality when the other is dominant; not due to substance use/medical condition o WORST prognosis of all dissociative disorders - Depersonalization disorder o Persistent or recurrent experiences of being detached from ones body or mental processes, but reality testing remains intact during episode; social or occupation impairment hat cannot be accounted for by amouther mental or physical disorder Tx: retrieve lost memories using hypnosis, sodium amobarbital or lorazepam during the interview.
PRACTICE QUESTIONS Q1) A 4-year-old boy has just been reunited with his biological mother after spending 6 months in foster care. He was initially removed from his home for severe neglect secondary to substance abuse. The boy is noted to play in a destructive and disorganized manner, throwing and breaking his toys. When the mother tries to stop him from throwing blocks at her, he starts kicking and biting. Which of the following is the most likely diagnosis? a) Oppositional defiant disorder (ODD) b) ADHD c) Reactive attachment disorder d) PTSD e) Major depression Q2) Secondary prevention is best exemplified by which of the following? a) Enrollment of a 2 year-old in a play group in the hopes of preventing antisocial behaviors. b) Restraing a violent teen after a suicide attempt. c) Visiting the home of a child after a neighbor reports that the child is being neglected. d) Treating new onset feelings of depression and anhidonia with an SSRI. e) Enrolling siblings of bipolar patients in group therapy. Q3) A 56-year-old man is brought to your office by his wife because she has noted a personality change in the past 3 months. While the patient is being interviewed, he continually discusses event on the news, what he ate for lunch and other topics unrelated to the questioning prior to providing appropriate answers to your questions. Which of the following symptoms best fits this patient's behavior? a) Negative symptoms b) Disorientation c) Concrete thinking d) Perseveration e) Circumstantiality 1. A 3-year-old girl is brought to the physician by her parents because they are concerned about her behavior. They describe their daughter as stubborn and always on the go. She can rarely sit still for more than 10 minutes. She often refuses to comply with their requests and sometimes throws 3- to 5minute temper tantrums. They report that she dawdles at bedtime and requires frequent direction and assistance in preparing for bed. Her preschool teacher notes that she is active and talkative without being disruptive and is beginning to demonstrate more interactive play with her peers. She generally sleeps through the night and occasionally wets the bed. Her appetite is good. Her first word was at the age of 11 months, and she began walking without assistance at the age of 14 months. Physical examination shows no abnormalities. On mental status examination, she initially hides behind her mother but warms to the interviewer after a few minutes and begins playing with toys in the office. Her speech is 90% intelligible, and her vocabulary is large for her age. Which of the following is the most appropriate next step in management? (A) Reassurance (B) Play therapy (C) Speech therapy (D) Enuresis alarm (E) Trial of fluoxetine (F) Trial of methylphenidate
2. A 45-year-old man is brought to the physician by his spouse. He has been drinking heavily since he was passed over for a job promotion 3 days ago. He stayed in bed over the weekend. He has no personal history of psychiatric disorders and no personal or family history of alcohol abuse. He is crying and states, AI can't believe it,@ when addressed. When asked what he will do, he states, AI don't know, but if I don't go back to work tomorrow, I'll lose my job.@ Which of the following is the most likely diagnosis? (A) Adjustment disorder with depressed mood (B) Bipolar disorder (C) Dysthymic disorder (D) Major depressive disorder (E) Substance abuse 3. A previously healthy 18-year-old woman is brought to the physician for evaluation because of loss of appetite, sleeplessness, and extreme irritability for 3 weeks. After missing many practices, she quit the college softball team that she previously enjoyed. She often feels tired and has difficulty sitting still and concentrating on schoolwork. Her menses occur at regular intervals. She weighs 50 kg (110 lb) and is 168 cm (5 ft 6 in) tall; her BMI is 18 kg/m2. Her pulse is 74/min, respirations are 16/min, and blood pressure is 110/70 mm Hg. Which of the following is the most likely diagnosis? (A) Adjustment disorder with mixed disturbance of emotions and conduct (B) Anorexia nervosa (C) Attention-deficit/hyperactivity disorder (D) Dysthymic disorder (E) Major depressive disorder 4. A 57-year-old man comes to the physician accompanied by his wife because of a 2-year history of fatigue. He reports waking up tired nearly every morning, often with a headache. He naps almost every afternoon. He thinks that the fatigue is affecting his concentration and performance at work. His wife says that he snores frequently during the night and sometimes wakes up gasping for air. She describes him as a restless sleeper. His tonsils and adenoids were removed when he was a child. He has no history of serious illness and takes no medications. He is 178 cm (5 ft 10 in) tall and weighs 115 kg (253 lb); BMI is 36 kg/m2. His pulse is 86/min, and blood pressure is 164/88 mm Hg. The nasal septum is at the midline. Examination shows no other abnormalities. Which of the following is the most likely diagnosis? (A) Chronic fatigue syndrome (B) Narcolepsy (C) REM sleep behavior disorder (D) Restless legs syndrome (E) Sleep apnea 5. A 52-year-old woman whose husband died 2 months ago consults a physician because of headaches and feelings of
uncertainty. She describes the headaches as a band around her head; they occur unpredictably and are not accompanied by any other symptoms. She has no history of psychiatric illness. While talking with the physician, the patient begins to cry and talk about her deceased husband; she feels her life is empty now and worries about her future. Which of the following is most appropriate at this point? (A) Allow her to express herself (B) Prescribe an antianxiety drug (C) Prescribe an antidepressant drug (D) Refer her for psychological testing (E) Obtain a psychiatric consultation 6. A 47-year-old man is brought to the emergency department by police after he was found eating garbage from a dumpster behind a restaurant. He says that he just came to this town and that he is homeless, so he has no money for food. He admits to several psychiatric hospitalizations in the past but says that he no longer needs medication. He appears dirty and is malodorous. Vital signs are within normal limits. Physical examination shows no abnormalities. On mental status examination, his speech is clear, but his thought process is disorganized with many loose associations. At several times during the interview, he appears to be preoccupied with internal stimuli. He says that he hears voices having an ongoing conversation in his head. Which of the following is the most likely diagnosis? (A) Bipolar disorder (B) Brief psychotic disorder (C) Delusional disorder (D) Major depressive disorder with psychotic features (E) Psychotic disorder due to a general medical condition (F) Schizophrenia (G) Schizotypal personality disorder 7. A 32-year-old woman is brought to the emergency department because of fever, hallucinations, agitation, and confusion for 8 hours. She has a history of alcohol, cocaine, and benzodiazepine abuse. Her temperature is 37.8C (100F), pulse is 110/min, respirations are 16/min, and blood pressure is 150/90 mm Hg. Examination shows tremors and telangiectasia. The lungs are clear to auscultation. There is a holosystolic murmur; the abdomen is tender, and the liver edge is palpable 3 cm below the right costal margin. Rectal examination shows no abnormalities. Her serum alkaline phosphatase activity is 200 U/L, serum ALT activity is 60 U/L, and serum AST activity is 90 U/L. Which of the following is the most likely cause of this condition? (A) Acute cocaine toxicity (B) Alcohol withdrawal (C) Benzodiazepine withdrawal (D) Panic disorder (E) Schizophreniform disorder 8. A 10-year-old boy is brought to the physician because of
increasing behavior problems in school since starting 5th grade 3 months ago. His teacher states that he is unable to sit quietly through a classroom period and frequently disrupts the class and interrupts other children while they are talking. His parents report that he has always been an active child and are concerned because he is inattentive when he runs or walks. During examination, he fidgets with his hands and feet and is easily distracted from completing a task. Which of the following is the most appropriate pharmacotherapy? (A) Amitriptyline (B) Fluoxetine (C) Haloperidol (D) Imipramine (E) Methylphenidate 9. A 27-year-old woman is brought to the emergency department 1 hour after a friend found her barely arousable in her disorderly apartment with a nearly starving cat. The patient appears extremely thin. Her pulse is 90/min, respirations are 6/min, and blood pressure is 90/60 mm Hg. Physical examination shows small pupils, cracked lips, and bruises and scratches over the upper extremities. Mental status examination shows mild obtundation, blunted affect, and slow, incoherent speech. Which of the following is the most appropriate next step in management? (A) Observation in a quiet darkened room (B) Oral administration of chlorpromazine (C) Intramuscular administration of naloxone (D) Intravenous administration of haloperidol (E) Intravenous administration of lorazepam 10. A healthy 9-year-old boy is brought to the physician by his parents because they are concerned that he dislikes attending school. Every morning he cries and begs to stay home. He misses school at least 1 day weekly because his mother is exhausted from fighting with him to attend. His teachers report that he is quiet in class and rarely participates. He has difficulty reading at the level of his peers and lacks confidence. At home, he tends to stay in the same room as his mother and will sometimes follow her around the house. When his parents plan an evening out, he often becomes tearful and asks many questions about when they will return. He likes to have friends over to his house and appears to enjoy being with them. Physical examination shows no abnormalities. During the examination, he sits on his mother's lap and is quiet but cooperative. He makes brief eye contact and speaks in a low volume, becoming tearful when questioned about being away from his mother. Which of the following is the most likely diagnosis? (A) Dysthymic disorder (B) Mild mental retardation (C) Oppositional defiant disorder (D) Reading disorder (E) Separation anxiety disorder (F) Social phobia
11. A 47-year-old woman is brought to the physician by her husband because of bizarre behavior for 1 week. Her husband says that she makes no sense when she speaks and seems to be seeing things. She also has had difficulty sleeping for 2 months and has gained approximately 9 kg (20 lb) during the past 5 months. During this time, she has been moody and easily fatigued. He also notes that the shape of her face has become increasingly round and out of proportion with the rest of her body despite her weight gain. She has no history of psychiatric or medical illness. She is 160 cm (5 ft 3 in) tall and weighs 70 kg (155 lb); BMI is 28 kg/m2. Her pulse is 98/min, respirations are 8/min, and blood pressure is 148/92 mm Hg. Physical examination shows truncal obesity and ecchymoses over the upper and lower extremities. Neurologic examination shows no focal findings. Mental status examination shows pressured speech and a disorganized thought process. There is evidence of visual and auditory hallucinations. Urine toxicology screening is negative. Which of the following is the most likely diagnosis? (A) Brief psychotic disorder (B) Major depressive disorder with psychotic features (C) Psychotic disorder due to a general medical condition (D) Schizophrenia (E) Schizotypal personality disorder 12. One day after admission to the hospital for agitation and hallucinations, a 19-year-old man has the onset of severe muscle stiffness that prevents him from rising out of bed. At the time of admission, treatment with haloperidol was begun. Today, he appears lethargic and diaphoretic. His temperature is 39.7C (103.5F), pulse is 120/min, and blood pressure is 160/110 mm Hg. Physical examination shows generalized severe rigidity of the upper extremities bilaterally. On mental status examination, he is not oriented to person, place, and time. Which of the following is the most appropriate next step in management? (A) Observation only (B) Add fluoxetine (C) Add lithium carbonate (D) Discontinue haloperidol (E) Increase the dosage of haloperidol 13. A 32-year-old woman comes to the physician because of a 3week history of depressed mood. She works as a local news anchor. She says that she has always had a busy schedule, but lately she has not had her usual amount of energy and has had difficulty getting up and going to work. She describes herself as normally a "hyper" person with energy to perform multiple tasks. During the past 10 years, she has had similar episodes in which she has had depressed mood associated with a decreased energy level that makes her feel "slowed down." The episodes never last more than a few weeks. She sometimes goes through periods when she feels a surge in energy, sleeps very little, feels at the top of her mental powers, and is able to generate new ideas for the news station;
these episodes never last more than 5 days. She says that she loves feeling this way and wishes the episodes would last longer. She takes no medications. She does not drink alcohol or use illicit drugs. Her temperature is 37C (98.6F), pulse is 70/min, and blood pressure is 125/80 mm Hg. Physical examination shows no abnormalities. Mental status examination shows a depressed mood and flat affect. Which of the following is the most likely diagnosis? (A) Attention-deficit/hyperactivity disorder (B) Cyclothymic disorder (C) Dysthymic disorder (D) Major depressive disorder (E) Mood disorder due to a general medical condition 14. A 77-year-old woman is brought to the emergency department by her husband because of agitation and confusion for 3 hours. He states that she has been intermittently crying out and does not appear to recognize him. A routine health maintenance examination 3 days ago showed no abnormalities except for mild memory deficits. Her current temperature is 37.8C (100F), pulse is 100/min, respirations are 14/min, and blood pressure is 130/60 mm Hg. Physical examination shows no abnormalities except for mild tenderness to palpation of the lower abdomen. Mental status examination shows confusion; she is oriented to person but not to time or place. Which of the following is the most appropriate next step in diagnosis? (A) Determination of erythrocyte sedimentation rate (B) Measurement of serum alkaline phosphatase activity (C) Measurement of serum folate concentration (D) Urinalysis (E) Western blot assay 15. A 14-year-old boy is brought to the physician by his mother after she found an unsmoked marijuana cigarette in his bedroom. The mother reports that her son has never done anything like this before. His academic performance is excellent. When interviewed alone, the patient reports that his friends heard about smoking marijuana and acquired some from their peers to find out what it was like. He adds that he has never smoked marijuana before. He requests that his teachers not be informed because they would be very disappointed if they found out. Physical examination shows no abnormalities. On mental status examination, he is pleasant and cooperative and appears remorseful. Which of the following is the most likely diagnosis? (A) Conduct disorder (B) Marijuana abuse (C) Marijuana dependence (D) Parent-child relational problem (E) Normal adolescence 16. An otherwise healthy 27-year-old man is referred to a cardiologist because of three episodes of severe palpitations, dull chest discomfort, and a choking sensation. The episodes occur suddenly and are associated with nausea, faintness,
trembling, sweating, and tingling in the extremities; he feels as if he is dying. Within a few hours of each episode, physical examination and laboratory tests show no abnormalities. He does not abuse drugs or alcohol and has no history of interpersonal problems. Which of the following is the most likely diagnosis? (A) Delusional disorder (B) Generalized anxiety disorder (C) Hypochondriasis (D) Panic disorder (E) Somatization disorder 17. A 42-year-old woman is brought to the physician by her husband because of persistent sadness, apathy, and tearfulness for the past 2 months. She has a 10-year history of systemic lupus erythematosus poorly controlled with corticosteroid therapy. Physical examination shows 1-cm erythematous lesions over the upper extremities and neck and a malar butterfly rash. On mental status examination, she appears depressed. She says that she would be better off dead. Which of the following is the most appropriate next step in management? (A) Ask the patient about her suicidal thoughts (B) Reassure the patient that she will get well (C) Recommend psychiatric hospitalization (D) Begin paroxetine therapy (E) Increase the dose of corticosteroid 18. A 27-year-old man is brought to the emergency department by police 2 hours after threatening his next door neighbor. The neighbor called the police after receiving a note demanding that she stop videotaping all of the activities in the patient's home or he would call the police. During the examination, the patient is cooperative. He explains that he has lived in the neighborhood for 8 months. Three months ago, he noticed that his neighbor installed a new satellite dish and says that since that time, she has been watching every move he makes. He reports no personal or family history of psychiatric illness. He has not had changes in sleep pattern and performs well in his job as a car salesman. He appears neatly dressed. Physical examination shows no abnormalities. On mental status examination, his thought process is organized and logical. There is no evidence of suicidal or homicidal ideation or hallucinations. He says that he is not suspicious of anyone other than his neighbor. Which of the following is the most likely diagnosis? (A) Bipolar disorder (B) Brief psychotic disorder (C) Delusional disorder (D) Major depressive disorder with psychotic features (E) Schizophrenia 19. A 9-year-old girl is brought to the physician by her adoptive parents because they are concerned about her increasing difficulty at school since she began third grade 7 weeks ago. Her teachers report that she is easily frustrated and has had
difficulty reading and paying attention. She also has had increased impulsivity and more difficulty than usual making and keeping friends. Her biologic mother abused multiple substances before and during pregnancy, and the patient was adopted shortly after birth. She is at the 20th percentile for height and 40th percentile for weight. Examination shows a flattened nasal bridge and a long philtrum. During the examination, she is cheerful. Psychoeducational testing shows an IQ of 82. The most likely explanation for these findings is in utero exposure to which of the following? (A) Alcohol (B) Cocaine (C) Ecstasy (3,4-methylenedioxymethamphetamine) (D) Heroin (E) Marijuana (F) PCP (phencyclidine) (G) Toluene 20. A 77-year-old man comes to the physician with his daughter for a follow-up examination to learn the results of neuropsychological testing performed 1 week ago for evaluation of a recent memory loss. Results of the testing indicated cognitive changes consistent with early stages of dementia. Three weeks ago, he received the diagnosis of prostate cancer and has shown signs of a depressed mood since then. Twenty years ago, he required treatment in a hospital for major depressive disorder. His symptoms resolved with antidepressant therapy, and he has not taken any psychotropic medication for the past 15 years. The patient's daughter comes into the examination room before her father and asks that the physician not tell her father any information that might be upsetting, given his vulnerability to depression. She says she is concerned about what the results might be and how her father will handle them. The patient enters the room soon after his daughter makes her request. Which of the following is the most appropriate initial physician statement to this patient? (A) "Because of your history of depression, I would like you to start on an antidepressant medication before we talk any further about your neuropsychological testing." (B) "Before going over your test results, I'd like to hear how you have been doing. You have been through a difficult time." (C) "I would like to talk with your daughter a bit about your test results, and then I will go over things with you." (D) "Your daughter is concerned about you. I think you need to see a psychiatrist before we go any further here." (E) "Your tests were inconclusive, and I would like to have you start on a medication to help with your memory as a precaution."
1. A previously healthy 17-year-old girl is brought to the physician for evaluation because of loss of appetite, sleeplessness, and extreme irritability for 3 weeks. After missing many practices, she quit the softball team that she previously enjoyed. She often feels tired and has difficulty sitting still and concentrating on schoolwork. Her menses occur at regular intervals. She weighs 50 kg (110 lb) and is 168 cm (66 in) tall. Her blood pressure is 110/70 mm Hg, pulse is 74/min, and respirations are 16/min. Which of the following is the most likely diagnosis? (A) Adjustment disorder with mixed disturbance of emotions and conduct (B) Anorexia nervosa (C) Attention-deficit/hyperactivity disorder (D) Dysthymic disorder (E) Major depressive disorder 2. A 45-year-old man is brought to the physician by his spouse. He has been drinking heavily since he was passed over for a job promotion 3 days ago. He stayed in bed over the weekend. He has no personal history of psychiatric disorders and no personal or family history of alcohol abuse. He is crying and states, "I can't believe it," when addressed. When asked what he will do, he states, "I don't know, but if I don't go back to work tomorrow, I'll lose my job." Which of the following is the most likely diagnosis? (A) Adjustment disorder with depressed mood (B) Bipolar disorder (C) Dysthymic disorder (D) Major depressive disorder (E) Substance abuse 3. A 52-year-old woman whose husband died 2 months ago consults a physician because of headaches and feelings of uncertainty. She describes the headaches as a band around her head; they occur unpredictably and are not accompanied by any other symptoms. She has no history of psychiatric illness. While talking with the physician, the patient begins to cry and talk about her deceased husband; she feels her life is empty now and worries about her future. Which of the following is most appropriate at this point? (A) Allow her to express herself (B) Prescribe an antianxiety drug (C) Prescribe an antidepressant drug (D) Refer her for psychological testing (E) Obtain a psychiatric consultation 4. A 10-year-old boy is brought to the physician because of increasing behavior problems in school since starting 5th grade 3 months ago. His teacher states that he is unable to sit quietly through a classroom period and frequently disrupts the class and interrupts other children while they are talking. His parents report that he has always been an active child and are concerned because he is inattentive when he runs or walks. During the examination, he fidgets with his hands and feet and is easily distracted from completing a task. Which of the following is the most appropriate pharmacotherapy? (A) Amitriptyline (B) Fluoxetine (C) Haloperidol (D) Imipramine (E) Methylphenidate 5. A 32-year-old woman is brought to the emergency department because of fever, hallucinations, agitation, and confusion for 8 hours. She has a history of alcohol, cocaine, and benzodiazepine abuse. Her temperature is 37.8 C (100 F), blood pressure is 150/90 mm Hg, pulse is 110/min, and respirations are 16/min. She is tremulous. The lungs are clear to auscultation. She has a holosystolic murmur; the abdomen is tender, and the liver edge is palpable 3 cm below the costal margin. Rectal examination shows no abnormalities. She has telangiectasia. A complete blood count and liver function tests show no abnormalities. Her serum alkaline phosphatase activity is 200 U/L, serum alanine aminotransferase (ALT, GPT) activity is 60 U/L, and serum aspartate aminotransferase (AST, GOT) activity is 90 U/L. Which of the following is the most likely cause of this condition? (A) Acute cocaine toxicity (B) Alcohol withdrawal (C) Benzodiazepine withdrawal
(D) Panic disorder (E) Schizophreniform disorder Answers to first set of questions: A1) c - Reactive attachment disorder results from a severely dysfunctional early relationship between the principal caregiver and the child. When caregivers consistently disregard the child's physical or emotional needs, the child fails to develop a secure and stable attachment with them. This failure causes a severe disturbance of the child's ability to relate to others, manifested in a variety of behavioral and interpersonal problems. Some children are fearful, inhibited, withdrawn, and apathetic; others are aggressive, disruptive, and disorganized with low frustration tolerance and poor affect modulation. This condition is often confused with ODD or ADHD. A2) d - Treating new onset feelings of depression and anhidonia with an SSRI. he goal of secondary prevention is to address problems at an early stage to avoid future more severe problems. A3) e- Circumstantiality is a disturbance in which the patient digresses into unnecessary details before communicating the central idea. Answer Key for Psychiatry Sample Questions (Questions 1-20) 1. A 2. A 3. E 4. E 5. A 6. F 7. B 8. E 9. C 10. E 11. C 12. D 13. B 14. D 15. E 16. D 17. A 18. C 19. A 20. B Last 5 sample questions 1. 2. 3. 4. 5. E A A E B
You might also like
- Psych Shelf StuffDocument16 pagesPsych Shelf Stuffbostickdrew16100% (7)
- ManifestEverythingNow DR Robert AnthonyDocument23 pagesManifestEverythingNow DR Robert AnthonyMokhtar Mohd100% (6)
- High Yield PsychiatryDocument43 pagesHigh Yield Psychiatryconfusedmage91% (11)
- High Yield Internal Medicine Compatible VersionDocument100 pagesHigh Yield Internal Medicine Compatible VersionAhsan X Baig100% (5)
- Psychiatry Shelf Spreadsheet P.montenigro M3Document5 pagesPsychiatry Shelf Spreadsheet P.montenigro M3JamesHowson100% (1)
- Study Notes PsychiatryDocument50 pagesStudy Notes PsychiatryMedShare90% (10)
- Psychiatry Clerkship Study GuideDocument31 pagesPsychiatry Clerkship Study GuideJuanCarlos Yogi100% (9)
- High Yield PsychiatryDocument44 pagesHigh Yield PsychiatryAntony Awad100% (2)
- Psych Case FilesDocument21 pagesPsych Case Filesshina100% (1)
- Medication Fact Book for Psychiatric Practice, Fifth EditionFrom EverandMedication Fact Book for Psychiatric Practice, Fifth EditionNo ratings yet
- HY NBME Psych Review: Some MS4Document114 pagesHY NBME Psych Review: Some MS4Swisskelly1100% (2)
- BoardReviewClass PsychiatryDocument28 pagesBoardReviewClass PsychiatryyepherenowNo ratings yet
- CMS Int. Med1 AnswersDocument15 pagesCMS Int. Med1 AnswersDiego Al Gutierrez50% (2)
- HighYieldPsychiatry PDFDocument43 pagesHighYieldPsychiatry PDFYay100% (4)
- High Yield Surgery Shelf Exam Review CompleteDocument11 pagesHigh Yield Surgery Shelf Exam Review Completeslmrebeiro92% (12)
- Psychiatry Shelf ReviewDocument11 pagesPsychiatry Shelf ReviewAhmad Syahmi YZ75% (4)
- Study Guide For OBGYNDocument34 pagesStudy Guide For OBGYNFiorellaBeatriz100% (1)
- Pestana Review - Surgery ShelfDocument8 pagesPestana Review - Surgery ShelfJayson Marwaha100% (2)
- Psychiatric DISORDERSDocument9 pagesPsychiatric DISORDERSNilay Bhatt100% (1)
- "Serotonin Syndrome Causes HARM": Psychiatry PharamacologyDocument9 pages"Serotonin Syndrome Causes HARM": Psychiatry Pharamacologytycobb63100% (4)
- Significant Functional ImpairmentDocument4 pagesSignificant Functional Impairmentxcupcakex122006No ratings yet
- Psychiatry - Shelf ReviewDocument101 pagesPsychiatry - Shelf Reviewluck2liv100% (4)
- Notes On Psychiatry: TypesDocument17 pagesNotes On Psychiatry: TypesMAY100% (1)
- Psychiatry High Yield NotesDocument6 pagesPsychiatry High Yield Notesgregry2100% (2)
- Mehlmanmedical Hy PsychDocument19 pagesMehlmanmedical Hy PsychJennifer Ross-ComptisNo ratings yet
- Psych Shelf StuffDocument16 pagesPsych Shelf Stuffskeebs23100% (2)
- Psychiatry Shelf AnswersDocument8 pagesPsychiatry Shelf AnswersJoan Choi100% (1)
- Medicine Shelf ReviewDocument6 pagesMedicine Shelf ReviewSara AH80% (5)
- Nbme Obgyn Searchable AnsweredDocument50 pagesNbme Obgyn Searchable Answeredexplore100% (8)
- Study Guide For The Psychiatry NBME Content Exam AKA The Psychiatry Shelf Exam!Document2 pagesStudy Guide For The Psychiatry NBME Content Exam AKA The Psychiatry Shelf Exam!DoriNo ratings yet
- Quick Review/Pearl Sheet: These Are in Random Order To Help You Prepare For You NBME ExamDocument19 pagesQuick Review/Pearl Sheet: These Are in Random Order To Help You Prepare For You NBME ExamWyoXPat100% (11)
- Neuro Notes Misc.Document11 pagesNeuro Notes Misc.slmrebeiroNo ratings yet
- Psychiatry History Taking and Physical ExaminationDocument16 pagesPsychiatry History Taking and Physical ExaminationEma100% (17)
- Divine Intervention Episode 22 Obgyn Shelf Review PDFDocument167 pagesDivine Intervention Episode 22 Obgyn Shelf Review PDFSwisskelly1100% (1)
- Psych Med ChartsDocument5 pagesPsych Med ChartsNursingSchoolNotes100% (5)
- History Taking in PsychiatryDocument13 pagesHistory Taking in PsychiatryvinodksahuNo ratings yet
- CMS Ob&Gyn 1 AnswersDocument13 pagesCMS Ob&Gyn 1 AnswersMohamed Abib100% (6)
- Psychiatry Practice Boosters 2016: Insights from research to enhance your clinical workFrom EverandPsychiatry Practice Boosters 2016: Insights from research to enhance your clinical workNo ratings yet
- HY PsychDocument19 pagesHY PsychJamesIwuNo ratings yet
- 2012-13 Psychiatry Board ReviewDocument79 pages2012-13 Psychiatry Board Reviewlizzy596100% (1)
- Antipsychotic Drugs: (Neuroleptics, Major Tranquillizer Ataractic)Document63 pagesAntipsychotic Drugs: (Neuroleptics, Major Tranquillizer Ataractic)Muhammad Masoom Akhtar100% (1)
- PsychDocument12 pagesPsychkaranNo ratings yet
- CMS Psychiatry 1 FormDocument41 pagesCMS Psychiatry 1 FormDuriye Damla Sevgi100% (6)
- Prescribing Psychotropics: From Drug Interactions to PharmacogeneticsFrom EverandPrescribing Psychotropics: From Drug Interactions to PharmacogeneticsRating: 5 out of 5 stars5/5 (1)
- Psychiatry, Usmle Endpoint by DR Ahmed SheblDocument63 pagesPsychiatry, Usmle Endpoint by DR Ahmed SheblDaNy Chiriac100% (1)
- Antipsychotic DrugsDocument47 pagesAntipsychotic DrugsIkram UddinNo ratings yet
- High Yield Psychiatry: Shelf Exam Review Emma Holliday RamahiDocument43 pagesHigh Yield Psychiatry: Shelf Exam Review Emma Holliday Ramahigreg100% (1)
- Functional Approach - Katz (1960)Document4 pagesFunctional Approach - Katz (1960)Pujo DuriatNo ratings yet
- Acting & Animation RubricDocument2 pagesActing & Animation Rubricjoycetan50% (2)
- Sexual Behavior in ChildrenDocument4 pagesSexual Behavior in ChildrenJoshua RingorNo ratings yet
- Pediatric Clerkship NotesDocument4 pagesPediatric Clerkship Notesxx_caligurl_93xxNo ratings yet
- Case StudyDocument4 pagesCase StudyYdynn Parejas GavinaNo ratings yet
- Behaviorist TheoriesDocument33 pagesBehaviorist Theoriesnasyratul100% (4)
- Divine Intervention Episode 21 Peds Shelf Review PDFDocument139 pagesDivine Intervention Episode 21 Peds Shelf Review PDFSwisskelly1No ratings yet
- FM Shelf Exam ReviewDocument5 pagesFM Shelf Exam ReviewMohammad Katato100% (1)
- USMLE Step 2 CK: CMS: Psychiatry Form 3Document17 pagesUSMLE Step 2 CK: CMS: Psychiatry Form 3usmleaddict pro57% (7)
- Nervous System: Chapter # 7Document69 pagesNervous System: Chapter # 7saddam ud dinNo ratings yet
- NBME PrepDocument33 pagesNBME PrepAnonymous BWH5I76RNo ratings yet
- Psychiatry Chapter 4Document50 pagesPsychiatry Chapter 4Online Money In EthiopiaNo ratings yet
- Psych 2AP3 - SchizophreniaDocument7 pagesPsych 2AP3 - SchizophreniadeanNo ratings yet
- Schizophrenia: DR - RahmanDocument17 pagesSchizophrenia: DR - RahmanPineappleNo ratings yet
- BurchGene Džana MulaomerovićDocument3 pagesBurchGene Džana MulaomerovićAhmed OsmanovicNo ratings yet
- Major Depressive Disorder: By: YOHANES AYELE, M.Pharm, Lecturer, Harar Health Science CollegeDocument48 pagesMajor Depressive Disorder: By: YOHANES AYELE, M.Pharm, Lecturer, Harar Health Science Collegehab lemNo ratings yet
- Name That TuneDocument3 pagesName That Tuneapi-541744798No ratings yet
- Skill Acquisition TheoryDocument14 pagesSkill Acquisition TheoryLiezel GamaoNo ratings yet
- Geronaga Elizabeth A. Module 10Document4 pagesGeronaga Elizabeth A. Module 10elizabeth2geronagaNo ratings yet
- Chapter IiDocument2 pagesChapter IiRizka HartatiNo ratings yet
- Chapter 1 - The Nervous SystemDocument8 pagesChapter 1 - The Nervous SystemRadha RamineniNo ratings yet
- Essential Functions - InterpreterDocument3 pagesEssential Functions - InterpreterMinh NguyễnNo ratings yet
- Pressing - Improv MethodsDocument50 pagesPressing - Improv Methodsmatejadolsak_7303486No ratings yet
- The Science of Emotional IntelligenceDocument6 pagesThe Science of Emotional Intelligencemontano2379No ratings yet
- Fields of Specialization in PsychologyDocument1 pageFields of Specialization in PsychologyAdrian BulusanNo ratings yet
- JNBibliography September 2016Document14 pagesJNBibliography September 2016il_memoNo ratings yet
- Class 4 - LeadingDocument37 pagesClass 4 - LeadingMignionDavisNo ratings yet
- Using Rewards and Sanctions in The Classroom: Pupils' Perceptions of Their Own Responses To Current Behaviour Management StrategiesDocument4 pagesUsing Rewards and Sanctions in The Classroom: Pupils' Perceptions of Their Own Responses To Current Behaviour Management StrategiesmarlazmarNo ratings yet
- Referral Counseling - List For WebsiteDocument3 pagesReferral Counseling - List For Websiteapi-425649572No ratings yet
- Department of Pharmacology and Experimental Neurosciences, University of Nebraska Medical Centre, Omaha, NE, USADocument2 pagesDepartment of Pharmacology and Experimental Neurosciences, University of Nebraska Medical Centre, Omaha, NE, USAArieleNo ratings yet
- Disposition, Parts and FunctionsDocument21 pagesDisposition, Parts and FunctionsGulzar AhmadNo ratings yet
- Effect of Reciprocal Teaching and Motivation On Reading Comprehension2016Document5 pagesEffect of Reciprocal Teaching and Motivation On Reading Comprehension2016Aqila HafeezNo ratings yet
- UtilDocument24 pagesUtilowenlgaoNo ratings yet
- I-O Psychology Material For Exam 2Document8 pagesI-O Psychology Material For Exam 2aw1435No ratings yet
- CHAPTER 2 - The Neural Basis For CognitionDocument18 pagesCHAPTER 2 - The Neural Basis For Cognitionbui mariaNo ratings yet
- Visual Business Intelligence - Why Do We Visualize Quantitative DataDocument5 pagesVisual Business Intelligence - Why Do We Visualize Quantitative DataAshwath Singh RainaNo ratings yet
- Dutch LBP Physiotherapy FlowchartDocument2 pagesDutch LBP Physiotherapy FlowchartyohanNo ratings yet