Professional Documents
Culture Documents
Week 9 Discussion
Uploaded by
api-239034911Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Week 9 Discussion
Uploaded by
api-239034911Copyright:
Available Formats
Question 1: The primary focus of my practice and my place of employment is diagnosis and treatment, but we also branch out
into the initial stages of rehabilitation and once the patient is able to participate shift the focus of care to illness prevention and maintenance of health. My place of employment is a not-for-profit hospital and this impacts employees several ways. Due to the fact that the hospital relies on insurance reimbursement, donations and charity we are tightly bound by the control of the insurance companies and what they are willing to pay and when they are not willing to pay. My practice itself does not change because of the hospital being a not-for-profit, but covered services may change. Quality and safety are HUGE issues and these areas are reflected in our mandatory education and well as bi-annual evaluations. With the list of NEVER events ever growing from the insurance reimbursement point of view there has been a renewed and continuing push to completely prevent pressure ulcers, patient falls, and catheter associated urinary tract infections and so on. Unfortunately the reality in providing healthcare is that you rely on and spend a lot of time dealing with insurance agencies as well as federal versions of healthcare coverage. Quality is something that should be provided at a baseline and should be expected from every patient entering any healthcare providing agency. However, now quality and satisfaction are being tied together to equal a reimbursement value from Medicare/Medicaid thus making customer satisfaction another top agenda in addition to quality and safety. Question 2: In my place of employment and on the critical care unit the health care team is multidisciplinary. Health care is delivered by medical staff, nursing staff, clinical pharmacists, dieticians, social workers, pastoral care, palliative care, nurse case managers, respiratory therapists, physical and occupational therapists, massage therapists, and speech therapists. Providing health care for the patient as a whole takes involvement from a team and participation from all areas of health care providers. Where I work most of the time all of the care team members work together seamlessly. Each provider has his or her own perspective and specialty care to offer, thus we all work together and complement each other providing well rounded and balanced care to the patient. In a critical care unit team work is not just desirable, it is necessary. People who do not work well or participate as a team member usually find themselves a new area to work in or learn and adapt to what it means to play as a team! I think that I regularly fulfill the role or care provider, educator, counselor, manager and collaborator daily at work. When I am working on the floor and have a patient assignment I am the direct care provider for the patients under my care. I work to educate the patient if they are able to understand and participate; I educate the family and field questions and concerns, and frequently readdress educational needs and learning and reassess a patients ability to learn. I am a counselor and listening/sounding board for patients and family members. I provide support
directly, or enlist the necessary help from social work, pastoral care, or palliative care as needed or required. I evaluate not only the patient in the bed, but the whole picture to make sure all of the needed specialties and resources are available and enlisted in their care. Daily I enlist and utilize research and best practice, but I do not regularly participate in research agendas or investigations. Collaboration is huge in my daily practice, with critically ill patient multiple specialty medical groups are involved in addition to our multidisciplinary team. I not only collaborate with all of my co-health care providers and specialists, I collaborate with my patient and his or her family to assure the best care and outcome possible. The nursing care delivery model most prominent in my place of employment is primary nursing missed with patient-centered care. On my unit each nurse is assigned between one and three patients based on acuity and is responsible and accountable for providing care to those patients. While every nurse starts work with a specific assignment, as patient acuity changes the nurse might also change but the patient remains in the same room. Our care is patient centered in that we offer a multidisciplinary care team and tailor patient care based on patient wishes. The hospital has several water features, works of art, painted/wallpaper walls, wood floors, food on demand with a menu designed for multiple different diet restrictions, music therapy, pet therapy, spiritual care, chapels, and massage therapy all designed with patient-centered care in mind. The advantages of primary nursing are immense with good relationships and trust developed between nurses and patients and families, full care of the patient within your assignment, and continuity of care which usually raises patient satisfaction. The disadvantage comes in when you have a particularly difficult/demanding patient and friction with patient or family members. On my floor we do primary nursing, but work within pods. We have pod mates and at the start of the day have a pod huddle to gain familiarity with all of the patients within our given pod so as to enable us to provide cross coverage for one another during breaks or when a pod nurse is traveling off of the floor. Patient-centered care promotes patient satisfaction and allows a patient to have some semblance of control over their healthcare and situation. Teamwork and collaboration are paramount in patient centered care and many specialties are utilized to provide whole person care. The biggest disadvantage to patient-centered care is the time that it takes to assure that the right nurse is placed with the right patient to deliver the right care. Overall I think that a union of primary nursing and patient-centered care is optimal for safe and quality health care delivery.
You might also like
- Key Selection Criteria: 1) A Patient Focused Approach To CareDocument2 pagesKey Selection Criteria: 1) A Patient Focused Approach To CareHuỳnh Ngọc Tuyền0% (2)
- Personal Philosophy of Nursing PortfolioDocument9 pagesPersonal Philosophy of Nursing Portfolioapi-290938460100% (2)
- Martha Rogers Case Study With AnswersDocument2 pagesMartha Rogers Case Study With Answersapi-239034911100% (3)
- NCM 102 Reflections Week 2Document4 pagesNCM 102 Reflections Week 2Lordgelyn Diane ViernesNo ratings yet
- Nursing Autonomy and Responsibilities To Family MembersDocument4 pagesNursing Autonomy and Responsibilities To Family MembersKoEy Are UNo ratings yet
- Philosophy of NursingDocument8 pagesPhilosophy of Nursingapi-300623329No ratings yet
- UteDocument6 pagesUteapi-708292653No ratings yet
- Promoting Family Health from Pregnancy to ParenthoodDocument4 pagesPromoting Family Health from Pregnancy to ParenthoodThrecia RotaNo ratings yet
- Roles of health care team members in patient educationDocument5 pagesRoles of health care team members in patient educationkrezia daasinNo ratings yet
- Nursing Metaparadigm - (Essay Example), 1629 Words GradesFixerDocument6 pagesNursing Metaparadigm - (Essay Example), 1629 Words GradesFixerjessicaokaka48No ratings yet
- A Description of Your Role Including Direct Patient CareDocument4 pagesA Description of Your Role Including Direct Patient Careد.شەماڵ احمد : پزیشکی دەرمانسازNo ratings yet
- Practicum ToolDocument2 pagesPracticum ToolrodcyruskentNo ratings yet
- NurseryDocument1 pageNurseryAyush SinhaNo ratings yet
- Nurs 478 Nursing Philosophy 1Document6 pagesNurs 478 Nursing Philosophy 1api-642424041No ratings yet
- Personal Nursing PhilosophyDocument7 pagesPersonal Nursing Philosophyapi-708278194No ratings yet
- Patient-Centric Care Is Directly Linked To Health Care Quality and Safety. NursesDocument2 pagesPatient-Centric Care Is Directly Linked To Health Care Quality and Safety. NursesShazney Aizle AlbizoNo ratings yet
- LFJ FormatDocument3 pagesLFJ Formatdennise reyesNo ratings yet
- The Role of The Nurse Is To Advocate For The Best Interests of The Patient and To Maintain The Patient's Dignity Throughout Treatment and CareDocument2 pagesThe Role of The Nurse Is To Advocate For The Best Interests of The Patient and To Maintain The Patient's Dignity Throughout Treatment and CareRikki Mae BuenoNo ratings yet
- Nursing Fields 2Document6 pagesNursing Fields 2Tonee Marie GabrielNo ratings yet
- Calling of the Healthcare ProviderDocument14 pagesCalling of the Healthcare ProviderNur SanaaniNo ratings yet
- Kaua'i Hospice & Palliative Care ExperienceDocument7 pagesKaua'i Hospice & Palliative Care ExperienceLlewelyn AgpaoaNo ratings yet
- Review of Lit-RevisedDocument18 pagesReview of Lit-Revisedapi-301889339No ratings yet
- Expanded and Extended Role of Pediatric Nurse: S. K Mohana SundariDocument34 pagesExpanded and Extended Role of Pediatric Nurse: S. K Mohana SundariShivangi SharmaNo ratings yet
- BSN Qsen CompetenciesDocument2 pagesBSN Qsen Competenciesapi-708978490No ratings yet
- Social Determinants of HealthDocument2 pagesSocial Determinants of HealthKeerthi sanapala7278No ratings yet
- Chapter - 1 - Perspective of Pediatric NursingDocument4 pagesChapter - 1 - Perspective of Pediatric NursingAhmad S Alkarmy100% (1)
- Personal PhilosophyDocument10 pagesPersonal Philosophyapi-283841044No ratings yet
- Fundamentals of Nursing: Scope, Principles, Ethics and RolesDocument12 pagesFundamentals of Nursing: Scope, Principles, Ethics and RolesDaksh AgrawalNo ratings yet
- Nursing PhylosophyDocument4 pagesNursing Phylosophyapi-689820167No ratings yet
- DocumentDocument17 pagesDocumentSamuel konaduNo ratings yet
- E-Portfolio - Philosophy of NursingDocument2 pagesE-Portfolio - Philosophy of Nursingapi-353669394No ratings yet
- Nur 300 PhilosophyDocument7 pagesNur 300 Philosophyapi-549106443No ratings yet
- Mclemore Synthesis EssayDocument4 pagesMclemore Synthesis Essayapi-283558804No ratings yet
- Nursing TheoriesDocument5 pagesNursing TheoriesKate AbellaNo ratings yet
- Management of Patients With Inflammatory DisordersDocument2 pagesManagement of Patients With Inflammatory DisordersMerald PerdigonNo ratings yet
- The Professional Nurse RoleDocument4 pagesThe Professional Nurse RoleSanthosh.S.UNo ratings yet
- Nursing PhilosophyDocument8 pagesNursing Philosophyapi-709719427No ratings yet
- Personal Nursing Philosophy-FinalDocument12 pagesPersonal Nursing Philosophy-Finalapi-480621329No ratings yet
- Extended and Expanded Role of NursesDocument20 pagesExtended and Expanded Role of NursesSandeep choudharyNo ratings yet
- Patient Education: A Key Nursing SkillDocument6 pagesPatient Education: A Key Nursing SkillMarie MayNo ratings yet
- What Is Synergy Model???: Patient CharacteristicsDocument3 pagesWhat Is Synergy Model???: Patient CharacteristicsRao anaNo ratings yet
- Role of Pediatric Nurse in Child CareDocument15 pagesRole of Pediatric Nurse in Child Carecharan pooniaNo ratings yet
- What is the Synergy Model in NursingDocument3 pagesWhat is the Synergy Model in NursingMaimona khanNo ratings yet
- THE HEALTH CARE TEAM: CORE VALUES IN NURSING ASSESSMENTDocument119 pagesTHE HEALTH CARE TEAM: CORE VALUES IN NURSING ASSESSMENTJustine Vens G. AgustinNo ratings yet
- 4140 Nursing PhilosophyDocument8 pages4140 Nursing PhilosophyZoe RaineNo ratings yet
- PCCPDocument6 pagesPCCPsharNo ratings yet
- Nurses Code of Ethics ®Document15 pagesNurses Code of Ethics ®jjj4519No ratings yet
- Graduate School 3 Trimester, Academic Year 2020-2021: St. Paul University Philippines Tuguegarao City, Cagayan 3500Document3 pagesGraduate School 3 Trimester, Academic Year 2020-2021: St. Paul University Philippines Tuguegarao City, Cagayan 3500Danica Lorine Robino TaguinodNo ratings yet
- Challenges in NursingDocument4 pagesChallenges in NursingAnju PandeyNo ratings yet
- Nursing Perceptions and Interprofessional CollaborationDocument4 pagesNursing Perceptions and Interprofessional CollaborationPeterNo ratings yet
- B Dailey Philosophy of Nursing Paper3 23 15Document8 pagesB Dailey Philosophy of Nursing Paper3 23 15api-283673800No ratings yet
- Austincupryk PersonalnursingphilosophyupdatedDocument8 pagesAustincupryk Personalnursingphilosophyupdatedapi-708744940No ratings yet
- Nursing Philosophy UpdatedDocument9 pagesNursing Philosophy Updatedapi-581236671No ratings yet
- Lithi 2Document13 pagesLithi 2Anonymous Gwg8WwNo ratings yet
- Role of Pediatric NurseDocument30 pagesRole of Pediatric NursePrecilla C. Stephen100% (2)
- Expanded RoleDocument19 pagesExpanded RoleVijith.V.kumar100% (2)
- Introduction To Nursing: Dr. Abdul-Monim Batiha Assistant Professor Critical Care Nursing Philadelphia UniversityDocument65 pagesIntroduction To Nursing: Dr. Abdul-Monim Batiha Assistant Professor Critical Care Nursing Philadelphia UniversityJohn peterNo ratings yet
- Philosophy of NursingDocument4 pagesPhilosophy of Nursingapi-299625168No ratings yet
- The Real Issue in Nursing Stress and Mental Illness A Short Book Every Nurse Should ReadFrom EverandThe Real Issue in Nursing Stress and Mental Illness A Short Book Every Nurse Should ReadNo ratings yet
- Group Process PaperDocument6 pagesGroup Process Paperapi-239034911No ratings yet
- Analysis of A Nursing Management RoleDocument7 pagesAnalysis of A Nursing Management Roleapi-239034911No ratings yet
- Research Paper Antibiotic Resistant GonorrheaDocument12 pagesResearch Paper Antibiotic Resistant Gonorrheaapi-239034911No ratings yet
- Healthcare Disparity PaperDocument7 pagesHealthcare Disparity Paperapi-239034911No ratings yet
- My New Cover Letter 1501162145Document1 pageMy New Cover Letter 1501162145api-239034911No ratings yet
- Graded Portfolio Checklist RN BSN ScholtensDocument1 pageGraded Portfolio Checklist RN BSN Scholtensapi-239034911No ratings yet
- Membership StatusDocument1 pageMembership Statusapi-239034911No ratings yet
- My New ResumeDocument2 pagesMy New Resumeapi-239034911No ratings yet
- Week 12 EconomicsDocument2 pagesWeek 12 Economicsapi-239034911No ratings yet
- CertificationverificationDocument1 pageCertificationverificationapi-239034911No ratings yet
- Pillar AwardDocument1 pagePillar Awardapi-239034911No ratings yet
- Group Process PaperDocument6 pagesGroup Process Paperapi-239034911No ratings yet
- Health Assessment PaperDocument17 pagesHealth Assessment Paperapi-239034911No ratings yet
- BSN Plan PaperDocument10 pagesBSN Plan Paperapi-239034911No ratings yet
- Unit 8Document2 pagesUnit 8api-239034911No ratings yet
- Discussion 4 Nursing TheoryDocument2 pagesDiscussion 4 Nursing Theoryapi-239034911No ratings yet
- Week 10 Legal Issues Influencing HealthcareDocument1 pageWeek 10 Legal Issues Influencing Healthcareapi-239034911No ratings yet
- Ebnp Group Project PaperDocument12 pagesEbnp Group Project Paperapi-239034911No ratings yet
- Nurisng Role PaperDocument9 pagesNurisng Role Paperapi-239034911No ratings yet
- Jason A Brown: 1374 Cabin Creek Drive, Nicholson, GA 30565Document3 pagesJason A Brown: 1374 Cabin Creek Drive, Nicholson, GA 30565Jason BrownNo ratings yet
- SOW Form 4 2017Document8 pagesSOW Form 4 2017ismarizalNo ratings yet
- Global Trustworthiness 2022 ReportDocument32 pagesGlobal Trustworthiness 2022 ReportCaroline PimentelNo ratings yet
- Pengaruh Implementasi Sistem Irigasi Big Gun Sprinkler Dan Bahan Organik Terhadap Kelengasan Tanah Dan Produksi Jagung Di Lahan KeringDocument10 pagesPengaruh Implementasi Sistem Irigasi Big Gun Sprinkler Dan Bahan Organik Terhadap Kelengasan Tanah Dan Produksi Jagung Di Lahan KeringDonny Nugroho KalbuadiNo ratings yet
- Lesson Plan 3Document6 pagesLesson Plan 3api-370683519No ratings yet
- Eng Listening Integrated Hkdse2022 UmayDocument21 pagesEng Listening Integrated Hkdse2022 UmayHoi TungNo ratings yet
- Ujpited ?tate of Americal: PresidentsDocument53 pagesUjpited ?tate of Americal: PresidentsTino Acebal100% (1)
- Completing-Your-Copy-With-Captions-And-Headlines Lesson-1Document24 pagesCompleting-Your-Copy-With-Captions-And-Headlines Lesson-1api-294176103No ratings yet
- ProbabilityDocument2 pagesProbabilityMickey WongNo ratings yet
- Reducing Healthcare Workers' InjuriesDocument24 pagesReducing Healthcare Workers' InjuriesAnaNo ratings yet
- Dmat ReportDocument130 pagesDmat ReportparasarawgiNo ratings yet
- Forum On Special Educational Needs: Phil Dexter Sharon Noseley Sophie FaragDocument14 pagesForum On Special Educational Needs: Phil Dexter Sharon Noseley Sophie Faragelena biancaNo ratings yet
- Yuri LotmanDocument3 pagesYuri LotmanNHNo ratings yet
- Vietnamese Grammar Questions and Answers DocumentDocument1 pageVietnamese Grammar Questions and Answers DocumentMinJenNo ratings yet
- Masala Kitchen Menus: Chowpatty ChatDocument6 pagesMasala Kitchen Menus: Chowpatty ChatAlex ShparberNo ratings yet
- Araminta Spook My Haunted House ExtractDocument14 pagesAraminta Spook My Haunted House Extractsenuthmi dihansaNo ratings yet
- Hem Tiwari Vs Nidhi Tiwari Mutual Divorce - Revised VersionDocument33 pagesHem Tiwari Vs Nidhi Tiwari Mutual Divorce - Revised VersionKesar Singh SawhneyNo ratings yet
- Bluetooth Mobile Based College CampusDocument12 pagesBluetooth Mobile Based College CampusPruthviraj NayakNo ratings yet
- James A. Mcnamara JR.: An Interview WithDocument22 pagesJames A. Mcnamara JR.: An Interview WithMiguel candelaNo ratings yet
- Critters Table MannersDocument3 pagesCritters Table Mannersapi-248006371No ratings yet
- United States v. Christopher King, 724 F.2d 253, 1st Cir. (1984)Document9 pagesUnited States v. Christopher King, 724 F.2d 253, 1st Cir. (1984)Scribd Government DocsNo ratings yet
- M5-2 CE 2131 Closed Traverse - Interior Angles V2021Document19 pagesM5-2 CE 2131 Closed Traverse - Interior Angles V2021Kiziahlyn Fiona BibayNo ratings yet
- Brittney Gilliam, Et Al., v. City of Aurora, Et Al.Document42 pagesBrittney Gilliam, Et Al., v. City of Aurora, Et Al.Michael_Roberts2019No ratings yet
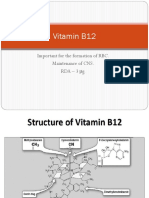
- Vitamin B12: Essential for RBC Formation and CNS MaintenanceDocument19 pagesVitamin B12: Essential for RBC Formation and CNS MaintenanceHari PrasathNo ratings yet
- Journal EntriesDocument10 pagesJournal Entriesapi-283322366No ratings yet
- Legend of GuavaDocument4 pagesLegend of GuavaRoem LeymaNo ratings yet
- Midterms and Finals Topics for Statistics at University of the CordillerasDocument2 pagesMidterms and Finals Topics for Statistics at University of the Cordillerasjohny BraveNo ratings yet
- Score:: A. Double - Napped Circular ConeDocument3 pagesScore:: A. Double - Napped Circular ConeCarmilleah FreyjahNo ratings yet
- Problem Set 12Document5 pagesProblem Set 12Francis Philippe Cruzana CariñoNo ratings yet
- 202002Document32 pages202002Shyam SundarNo ratings yet