Professional Documents
Culture Documents
8 - Toronto Notes 2011 - Emergency Medicine
Uploaded by
prekos 65Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
8 - Toronto Notes 2011 - Emergency Medicine
Uploaded by
prekos 65Copyright:
Available Formats
ER
Emergency Medicine
Mike Romano, John Sauve and Ryan Zufelt, chapter editors
Christophel' Kitamura and Michelle Lam, associate editors Janine Huston, EBM editor Dr. Simon Kingsley, staff editor Initial Patient Assessment/Management ..... 2 Rapid Primary Survey (RPS) Resuscitation Detailed Secondary Survey Definitive Care Ethical Considerations Traumatology ........................... 6 Considerations for Traumatic Injury Head Trauma Spine and Spinal Cord Trauma Chest Trauma Abdominal Trauma Genitourinary Tract Injuries Orthopaedic Injuries Life and Limb Threatening Injuries Upper Extremity Injuries Lower Extremity Injuries Wound Management Trauma in Pregnancy Approach to Common ER Presentations .... 19 Abdominal Pain Acute Pelvic Pain Altered Level of Consciousness (LOC) Chest Pain Epistaxis Headache Joint Pain Otalgia Seizures Shortness of Breath Syncope Sexual Assault Medical Emergencies.. 30 Anaphylaxis and Allergic Reactions Asthma Cardiac Dysrhythmias Chronic Obstructive Pulmonary Disease (COPD) Congestive Heart Failure DVT and Pulmonary Embolism Diabetic Emergencies Electrolyte Disturbances Hypertensive Emergencies Stroke Gynecology/Urology Emergencies......... 39 Vaginal Bleed Pregnant Patient in the ER Nephrolithiasis (Renal Colic) Ophthalmology Emergencies ............. 42 Ophthalmologic Foreign Body and Corneal Abrasion Dermatologic Emergencies .. 43 Life Threatening Dermatoses Environmental Injuries . . . . . . . . . . . . . . . . . . 44 Heat Exhaustion and Heat Stroke Hypothermia and Cold Injuries Burns Inhalation Injury Bites Near Drowning Toxicology ... 48 Alcohol Related Emergencies Approach to the Overdose Patient ABCs of Toxicology D1 -Universal Antidotes D2- Draw Bloods D3- Decontamination and Enhanced Elimination E- Examine the Patient G - Give specific Antidotes and Treatments Disposition from the Emergency Department Psychiatric Emergencies ................. 56 Approach to Common Psychiatric Presentations Acute Psychosis Suicidal Patient Violent Patient Common Pediatric ER Presentations ....... 57 Modified Coma Score Respiratory Distress Febrile Infant and Febrile Seizures Abdominal Pain Common Infections Child Abuse and Neglect Procedural Sedation .................... 61 Common Medications ................... 61 References . . . . . . . . . . . . . . . . . . . . . . . . . . . . 62
Toronto Notes 2011
Emergency Medicine ERI
ER2 Emergency Medicine
Initial Patient Assessment/Management
Toronto Notes 2011
Initial Patient Assessment/Management
1. Rapid Primary Survey (RPS)
----(_-.,
A!lllfOich 1D die Criticellr II Pdent 1. Rapid Primary Survey [RPS) 2. RRuscitJdion [Dfml concwnntwith
RPS)
3. Deteilad Sacondary Survey
4. Definitive Care
Airway maintenance with cervical spine (C-spine) control Breathing and ventilation Circulation (pulses, hemorrhage control) Disability (neurological status) Exposure (complete) and Envirorunent (temperature: control) Continually reassessed during secondary survey IMPORTANT: always watch for signs of shock while doing primary survey (see Table 1)
A. AIRWAY
.._' I
,.l------------------,
Noisy breathing is obstructed breathing until prawn olherwi&a.
first priority is to secure airway assume a cervical injury in every trauma patient and immobilize with collar assess ability to breathe: and speak can change rapidly, therefore reassess frequently
----(_-.,
Signs of Airway Obllrualian Agi1iltion, confusion, "universal choking sign" Respirmry dis1Jess Feiuruto IIPaek. dy$phonia Cymosis
Airway Management
goals permit adequate oxygenation and ventilation facilitate ongoing patient management give drugs via endotracheal tube (ETT) if IV not available Note: start with basic management teclmiques before progressing to advanced (see below)
Medic:nona that c:u b Deliqrld
� � �
I. Basic Airway Management (Temporizing Measures) protect the C-spinc: head-tilt (if C-spine injury not suspected) or jaw thrust to open the airway sweep and suction to clear mouth of foreign material
2. Definitive Airway Management ETT intubation with inline stabilization of spine (Figure 1) orotracheal Rapid Sequence: Intubation (RSI) preferred nasotracheal- may be better tolerated in conscious patient relatively contraindicated with basal skull fracture does not provide 100% protection against aspiration surgical airway (if unable to intubate using oral/nasal route and unable to ventilate) cricothyroidotomy
3. Rescue or Temporizing Measures nasopharyngeal airway oropharyngeal airway (not if gag reflex present) "rescue" airway devices (e.g. laryngeal mask airway (LMA); Combitube) transtracheal j c:t ventilation through cricothyroid membrane (last resort)
NAVEL Naloxone [Nen:en)
A1ropina
Ventolin [Salbutamol)
Epinephrine Lidoc:eins
----(_-.,
lndit:lltiDna fur lntallilticm Unable to pratec:t airwly [e.g. Glasgow Coma Scale [GCS) < 8; airway tmuma)
lnlldequate axygenation with IIPontBneous !85pimlion [0 2 setumion � � � � with 1� � � 02 or rising � � � � �
Trauma requiring nubltian
Profound .tlack Anticiplllory: in trauma, overdose,
congestive heart flliluru [CHF), asthma. chronic obstructive pulmonary dileasa [COPO) and $/lloka inhalation injury Anticipllled transfer of criticaUy iU
... No immldiate neld
�� CIIPine x-my
I
Fiberoptic m or nasel m or RSI
Immediate need
Apn&IC
peti81111
� � � �
0ra1m
[:!: RSI)
..._,I
Oralm
Breathing
,.l------------------,
Addld Equipmllllt 11111 Techniques In llltuWicm Bougi {usld liklegJiUwin) Retrograde intubation {ffi threaded over a wirl inserted through skin and
Unable
out mouth) Lighted stylet {use light through skin 111 detErmine if ffi in CO!Tilct place) Fibreoptic in11Jbation- indiruct vision using fibraop1ic cable
Rescue devices or cricothyroidotomy
11...: CleoriiiQ lhe C.Spine � � � � � � � � � � cli'lical -.sment. which ,..quim: 1) No midline tenderness 2) No focal neurol01,1ical delleits 3] No dlltracting factors 111ch .. intOJication, lllt8racl LOC or dimctiiiQ injuri..
Unable
Omlm [no RSI)
��
I
Rescue devices or cricothyroido1Dmy
lklable
Rescue � � � � � � � � or cricothyroidotomy
Nasalmororalm
[:!: RSI)
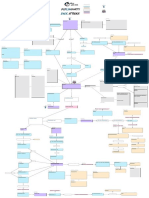
Figura 1. Approach to Endotracheal Intubation in an Injured Patient m- andalrlchaliltDI illublliDn; RSI-IIpid sequancs illubllim
Toronto Notes 2011
B. BREATHING
Initial Patient Asaeument/Manqement
Emergency Meclidne ER3
Look
mental status (anxiety, agitation, decreased WC), colour, chest movement (bilateral vs. asymmetrical), respiratory rate/effort, nasal flaring Listen sounds of obstruction (e.g. stridor), breath sounds, symmetry of air entry, air escaping Fed flow of air, tracheal shift, chest wall for crepitus, flail segments, sucking chest wounds, subcutaneous emphysema
Breathing Assessment measurement of respiratory function: rate, pulse oximetry, arterial blood gas (ABG), A-a gradient Management of Breathing nasal prongs -+ simple face mask-+ oxygen reservoir -+ CPAP/BiPAP Venturi mask: used to precisely control Oz delivery Bag-Valve mask and CPAP to supplement ventilation
C. CIRCULATION
Definition of Shock inadequate organ and tissue perfusion with oxygenated blood (brain, kidney, extremities) (see Table 2)
Table 1. Major Types of Shock
llypavalemic Hamon1lage (IIXIII'nill and illbll'nlll) C.nliogenic Myoc:ll'dial Ischemia AnhytlmiiiS Congestive Heart Failure Cll'diomyopallies Cll'diac valve problems
Distributive {vaodilltian)
\to,
Shock in a trauma patient is hemorrhagic � � � � � proven otherwiae.
Dbllruc:tive
Cardiac tamponade Tension pnaumotho111X Nmonary entolism Aortic stenosis Constrictive � � � � � � � � � � �
�
SIMI'II bums
Hijl olllplt fistulas Dehy!htion {diarrhea, DKA)
Septic Anaphylactic Neurogenic (spinal cord injury)
't'
&-!If Shack
Septic, SpinaVnaurovunic,
Hernonhagic Ob5buctive (e.g. blnsion pneumolhomc, c.-diac tamponadll, pumonary BITiboliiiTI)
SHOCKED
Clinical Evaluation early: tachypnea. tachycardia. narrow pulse pressure, reduced capillary refill, cool extremities and reduced central venous pressure (CVP) late: hypotension and altered mental status, reduced urine output
Table 2. Estimation of Degree of Hemorrflagic Shock
CIBS
Cardioqenic (e.g. blunt myocardial injury, arrhythmia, Ml)
anaphylactiK Endocrine (e.g. Addison's, myxedema, coma)
II
Ill
IV
Drugs
Blood Loss
%of blood volume
<750 cc <15% <100
Normal
750.1500 cc 15-311% >100
Ncrmal
1500.2000 cc 30-40% >120
Decreased
>2000 cc >411% >140
Decreased
.....
''
� � � � � � � � � � � � � � � � � � � � �
�
Pulse Blood pressure Respinrtory 111111 Capillary ntil UriiiiiY output Auid replacement
Estimm.d Sysbllk: Blo.cl � � � � � � � � Baed on Palhlon !If MDII Dlmll
I'Bip.-ldtiPul
20
Normal
30
Decreased
35
Decreased
>45
Decreased None Crystalloid + blood
� �
siP (mmllg)
Radial
Femoral
30 ce/lr"
Crystaloid
20 cC/lr"
Crystalloid
10 cC/lr"
Crystalloid + blood
Carotid
>80 >70 >60
Management of Hemorrhagic Shock secure airway and supply 0 2 TREAT TilE CAUSE OF TilE SHOCK control external bleeding directpressure elevate extremities if no obvious unstable fracture consider vascular pressure points (brachial, axillary, femoral) do not remove impaled objects as they tamponade bleeding tourniquet only as last resort prompt surgical consultation for active internal bleeding infusion ofl-2 L ofNS/RL as rapidly as possible-+ 2large bore (14 gauge) IVs wide open warm blood!IV fluids, especially for massive transfusions replace lost blood volume at ratio of 3:1 with crystalloid if inadequate response, consider ongoing blood loss (e.g. chest, abdomen, pdvis, extremities) -+ operative intervention required indications for blood transfusion severe hypotension on arrival shock persists following crystalloid infusion rapid bleeding
� � � � � � � � � � Manqm18111
RED
Rest
Elavat81ha bleeding area above the level of the � � � � � � � � � �
Dirac! prauura on the blll8ding sitll
....
',
� � � � � � � � � � � � � � � � � � � � �
Fluid � � � � � � � � � �
Give bolus until HR diiCrlllllllll, � � � � � output picks up, and p!dierrt stabilizn
fir1t , Okg: 4CCI!qVhr 1G-20kg: 2cc;/kg/hr remaining weight 1�
Maintenance: 4-2-1 rule
� � �
(lllmll , 0'11 of body weight)
replace ongoing lou lll1d deficitli
ER4 Emergency Medicine
Initial Patient Assessment/Management
Toronto Notes 2011
� � � Since only 30% of infused isotonic cryllllllloid& ruiTIIIin& in inlnlvm:ul space, you must give 3x estimallld
blood IDA.
� � � lnllllll � � � � � � � � � � � � � � � af Any l'llllent inSbacll ABCs IV fluids Oxygen Monitor(HR, BP. urinl, manlldion, � � ut.l
transfusion options with packed red blood cells (pRBCs) crossmatched if possible type-specific (provided by most blood banks within 10 minutes) preferred to 0-negative un-crossmatched blood if both available 0-negative (children and women of child-bearing age) 0-positive if no time for cross-match (males/postmenopausal women) anticipate complications with massive transfusions consider replacement of other blood products (plalelets, FFP) after 2-4 units pRBCs transfusion with fresh frozen plasma (FFP) used for clinical evidence of impaired hemostasis ongoing hemorrhage, PT >1.5x normal range
Control hemonbaQe
D. DISABILITY assess level of consciousness by AVPU method (see sidebox) or GCS
It'
L-1 af ConsciousnHI
Mllhod uf Aeleaintl
AVPU AI art
Responds 1D Verbal stimuli Responds 1D Painful stimuli
Unmponsivl
Glasgow Coma Scale (GCS} for use in trauma patients with decreased LOC; good indicator of severity of injury and neurosurgical prognosis may be used for metabolic coma. but less meaningful most useful if repeated and used for monitoring of trend change in GCS with time is more relevant than the absolute number patient with deteriorating GCS needs immediate attention prognosis based on best post-resuscitation GCS reported as a 3 part score: Eyes +Verbal+ Motor = Total (see Table 3) if patient intubated, GCS score reported out of 10 + T (T= tubed, ie. no verbal component)
Unprovwn or Hermful T-lnlllnts fw Hemenbegl Shock � � � � � � � � � � � � � � � position Steroids (used only in spilll cord
Table 3. Glasgow Coma Scala Best Yalbll Response EyasOp Spontln!ously Answers � � � � � � � � � � � appropriatl!ly 4
To voice To pain No response
Bill Motor lllsponsa
injuryl MAST g11n11en!s
3
2
Confused, disoriented
� � � � � � � � � � � � � � words
5 4
3
Obeys commands
Localizes ID pain
Withdraws from pain
5 4 3 2
Vuopressors
lncCJIT1lll!hensible sounds No varbal respansa
Decorticate (flexionl lleclllllbrate (axlllnsionl No response
. . . . .ii-Nwlljiiiiijftilil...... il l'lliiiD will s.,ti: SIIICk NE.IA 2008; 358:877-87 � � � lllldorril8d,doublt-bindlrilll l'llim: m pllilllllMllslplic shock ........ � � � VIIQIIIIIIil (0.01 tu0.03 upnmal mnpilaplrillii51D 1511Qper mirWI in addition � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � a mininun af 5UQ rl nllllpinlphri111. o.au Mcr1Jij;y llle 28 days ilf1lr ilart al irlu&illlll. ......_: No signilicart dill!tence helween 1he � � � � � � � � � � � � � IIIII the � � � � � � � � � � � � � � � � II � � � � � � � or 90dlys. HcMt., ilpililro Nth lisa -.1lplic lhol:t,IIIIOI!y IIIIIW1117Mir in lhe � � � � � � � � � � � � group.
13-15 =mild injury. !1-12 = mod81118 � � � � � � � � = sem injUJY Sal Tlbll28 for modliad r.cs for infants 111d childm
E. EXPOSURE/ENVIRONMENT undress patient completely and assess entire body for injury; logroll to examine back digital rectal exam keep patient warm with a blanket radiant heaters; avoid hypothermia warm IV fluids/blood keep providers safe (contamination, combative patient)
2. Resuscitation
done simultaneously with primary survey attend to ABCs (see Table 4) manage life-threatening problems as they are identified vital signs qS-15 minutes ECG, BP and 0 2 monitors Foley catheter and nasogastric (NG) tube if indicated tests and investigations: CBC, electrolytes, BUN, Cr, glucose, amylase, INR/PTT, � toxicology screen, cross and type
Folly Contrlindiclllelll Blood at urelhn.l meatus Scrutal hematoml
High-riding pro1111!1 on DRE
� � � � � �
Nil 1WI Conlreindbtion Si!Jlificlnt mid-face 1niUR11
BIHI skull frllcturu
Toronto Notes 2011
Initial Patient Asaeument/Manqement
Emergency Meclidne ER5
Table 4. 2005 AHA CPR Guidelines
Stlp/Aclion
Airway
Adult>Jvn
Breaths Foreign-body airway obstruction
Cernpression landmarks Cernpression msthod: pU&h hard and fast and allow fur cCJIT1llele recoil Ccmpression depth Compression rile Compressionventilation rllio Compression � � � CPR llefilrillation
Child: 1-8 yan Head tilt-chin lift 2 breaths 111 second/breath
Infant <1 yw
Abdcminal thrust
Back slaps and chest thrusts
In the centre Ill the chest, between � 2 Hands: Heel of 1 hand, &econd hand on top
� � � � � �
Just below nipple line
2fingers
2 Hands: Heel of 1hand with sBCOnd on IDp, or 1Hand: Heel of 1hand only
11h ID 2inches
About IJliD 1/z the depth of the chest 101Vmin 3D ccmpressians ID 2ventiations
Handscmly CPR is preferred � � � � � byslllnder is not t111ined or does not feel confident in their ability ID provide COIMintional CPR or if 1hB bystander is tained but choD&es ID use � � � � � � � � � � � � lmmadiatll delibrilation fur all rescuers responding ID a sudden No delitrillation witnessed collapse. CCJIT1llession � � � � � � � � � � � � before A8l is considered if EMS arrival is >4-5 rrinutes aftsrthe cell
3. Detailed Secondary Survey
done after rapid primary survey problems have been addressed identifies major injuries or areas of concern full physical exam and x-rays (e-spine, chest. pdvis -required in blunt trauma. consider T-spine and L-spine)
HISTORY
"SAMPLE": Signs and Symptoms, Allergies, Medications, Past medical history, Last meal, Events related to injury
PHYSICAL EXAMINATION Head and Neck pupils assess equality, size, symmetry, reactivity to light inequality/sluggish suggests local eye problem or lateralizing CNS lesion relative afferent pupillary defect (swinging light test) - optic nerve damage extraocular movements and nystagmus fundoscopy (papilledema, hemorrhages) reactivity/level of consciousness (LOC) reactive pupils + decreased we -+ metabolic or structural cause non-reactive pupils+ decreased we-+ structural cause (especially if asymmetric) palpation of facial bones, scalp
�
.....
,,
� � � � � � � � � � � � � � � � � � �
� � � � � � � � � � Dllmd,
NeiHMCtlve
Pupil, Think: Focelmnslasion Epidlnl hematoma
Subdurlll hema!DRII.
Chest inspect for midline trachea, flail segment: � � � rib fractures in � associated hemothorax, pneumothorax, and contusions auscultate lung fields palpate for subcutaneous emphysema
Non-contrail held CT is lila bait imfll!ing modality for intracerabral injury.
� � places; if present look for
� � � �
Sip af 111-.d lntrCfllnil
� � � � � � � � � � � � �
Abdomen assess for peritonitis, abdominal distention, and evidence of intra-abdominal bleeding FAST (Focused Abdominal Sonogram in Trauma), diagnostic peritoneal lavage (DPL) or CT rectal exam for GI bleed, high riding prostate and anal tone (best to do during the log roll) bimanual exam in females as appropriate
Deteriorating LOC (hallmft) Deteriorating ra.pimory pM!llm Cushing reflex (high BP. low hellrt rate, irregular mpindions) Latnlizing CNS signs (e.g. cranial
nerve pal$ie5, hemiparesis)
SlizUI'II
Musculoskeletal (MSK) examine all extremities for swelling, deformity, contusion, tenderness, range of motion check for pulses and sensation in all injured limbs log roll and palpate thoracic and lumbar spines palpate iliac crests and pubic symphysis, pelvic stability (lateral, AP, vertical)
NNand WA
� � � � � � � � � � � � � � � � � � � illtel
ER6 Emergency Medicine
Initial Patient AasessmenUManagementJTraumatology
Toronto Notes 2011
Neurological
alterations of rate and rhythm of breathing are signs of structural or metabolic abnormalities progressive deterioration of breathing pattern implies a failing CNS assess spinal cord integrity conscious patient: assess distal sensation and motor unconscious patient: response to painful or noxious stimulus applied to extremities
GCS full cranial nerve exam
4. Definitive Care
continue therapy continue patient evaluations and special investigations specialty consultations including OR as needed disposition: home, admission, or transfer to another setting (e.g. OR, ICU)
,,.. ,
� � �
Ethical Considerations
� � � � � � � � � � � � � � �
.llbovab"s wrm Capabl adults haY8 the right to rafuu madiall traatmant May r.fus whole blood, pRBCs, platalllbi lll1d plalma evan lliflt-
saving Should be questioned directly about tha us of albumin, imrmrloglobuli'la. hamophilic preparations Do not alow autologous transfusion unless there is unlntenupted exira corporul cin:ulation Ulllllly ask for the highest possible quality of care � � � � � � � the usa of the above interventions (e.g. crystalloids for volume expansion, attempts at biDOdiiiS SUrQII'ff
Patient will generally &ign h05pital forms rel11sing medical stall from
Consent to Treatment: Adults Emergency Rule: consent is not needed when patient is at imminent risk from a serious injury (e.g. severe suffering, loss oflimb, vital organ or life) AND obtaining consent is either: a) not possible (e.g. patient is comatose); OR b) would increase risk to the patient (e.g. time delay) assumes that most people would want to be saved in an emergency any capable and informed patient can refuse treatment or part oftreatment, even if it is life-saving consider: is the patient truly capable? Does pain, stress, or psychological distress impair their judgment? exceptions to the Emergency Rule: treatment cannot be initiated if a competent patient has previously refused the same or similar treatment and there is no evidence to suggest the patient's wishes have changed an advance directive is available - e.g. do not resuscitate (DNR) order refusal of help in a suicide situation is not an exception; care must be given if in doubt, initiate treatment care can be withdrawn if appropriate at a later time or if wishes clarified by family Consent to Treatment: Children treat immediately if patient is at imminent risk parents/guardians have the right to make treatment decisions if parents refuse treatment that is life-saving or will potentially alter the child's quality of life, Children's Aid Society (CAS) must be contacted- consent of CAS is needed to treat Other Issues of Consent need consent for HIV testing, as well as for administration of blood products Duty to Report law may vary depending on province and/or state gunshot wounds, potential drunken drivers, suspected child abuse, various communicable diseases medical unsuitability to drive
liability
Molt I� � � � � CIIN involv1 childrln of Jehovah's Witnesses; if lifit.saving treatment is refuaad contacllld CAS
Traumatology
epidemiology leading cause of death in patients <45 yrs 4th highest cause of death in North America causes more deaths in children/adolescents than all diseases combined trimodal distribution of death minutes: lethal injuries, death usually at the scene early: death within 4-6 hours - "golden hour" (but decreased mortality with trauma care) days-weeks: death from multiple organ dysfunction, sepsis, etc. injuries generally fall into two categories blunt (most common): motor vehicle collision (MYC), pedestrian-automobile impact, motorcycle collision, fall, assault, sports penetrating (increasing in incidence): gunshot wound, stabbing, impalement
� � � � � � � � � � � � � � � �
,,.. ,
� �
Considerations for Traumatic Injury
important to know the mechanism of injury in order to anticipate traumatic injuries always look for an underlying cause (alcohol, medications, illicit substances, seizure, suicide attempt, medical problem) always inquire about head injury, loss of consciousness, amnesia, vomiting, headache and seizure activity
High Rilk ....rill.
MVC at high speed, resulting in ejKiion from vehicle Motorcycl collisions v.hicll vs. flldertrian cruhn
FaD tram height >12ft [3.6 ml
Toronto Notes 2011
Traumatology
Emergency Meclidne ER7
Motor Vehicle Collision (MVC}
vehicle(s) involved: weight, size, speed, amount of damage type of crash (to assess location of possible injuries) lateraVT-bone and head-on: head. cervical spine, thoracic, abdominal, pelvic and lower extremity rear-end: hyper-extension of cervical spine (whiplash injury to neck) roll over: energy dissipated, less likely severe injury ifvictim restrained by seatbelt, however still significant potential morbidity location of patient in vehicle use and type of seatbelt lap belt: spine and abdominal injury shoulder belt: look for major vessel injury ejection of patient from vehicle/entrapment of patient under vehicle airbag deployment use of helmet in motorcycle or bicycle collisions
Pedestrian-Automobile Impact
high morbidity and mortality vehicle speed is an important factor site of impact on car children tend to be run over adults tend to be struck in lower legs, impacted again on car (truncal injury) and thrown to the ground (head injury)
....
,,
� � � � � � � � � � � � � � � � � �
Vthicll ... Pldellrilll er.h In adults look lor triad of injuries (waddle's triad):
1. Tibi&-fibula or femur fnlctwe Z. TrQICIII injury 3. Craniofacial injury
Falls
1 storey= 12 feet = 3.6 m distance of fall: 50% mortality at 4 stories and 95% mortality at 7 stories position in which patient landed and type of surface assess for shock, lower extremity, spine and pelvic fractures
Gunshot Wounds (GSW)
typeofgun handgun injuries: low or medium velocity, extent of injury may be limited to a small area hunting and rifle injuries: high velocity, widespread injury shot gun: widespread tissue destruction type of ammunition (e.g. hollow point bullets) range of shot close range: massive tissue destruction, deposition of wadding into wound characterize route of entry, even or odd number of wounds and site of exit wound (if any) GSW with hypotension: immediate transport to OR hypotension indicates severe blood loss (>2 L blood loss in 70 kg patient is required to produce hypotension)
\,
Cardiac box: sbllllll notch. nipples and xiphoid process; injuries inside this � � � � � lhould incmsaiUSpicion of Cllrdiac injury.
�
Stab Wounds
route/direction of entry, length of blade type of penetration (stab, slash, impalement) victim recollection and witness reports are often inaccurate and may not correlate with depth/ severity of wound ifblade in-situ, DO NOT REMOVE- it may be tamponading bleeding vessel (to be removed in OR)
Head Trauma
see � � � � � � � � � � � NS29 6096 oftrauma admissions have head injuries 6096 ofMVC-related deaths are due to head injury
Specific Injuries
fractures (diagnosed by CT head, often not visible on x-ray) A. skull fractures vault fractures linear, non-depressed - most common - typically occur over temporal bone, in area of middle meningeal artery (commonest cause of epidural hematoma) depressed - open (associated overlying scalp laceration, torn dura) vs. closed basal skull typically occur through floor of anterior cranial fossa (longitudinal more common than transverse) clinical diagnosis superior as poorly visualized on CT (Battle's sign. raccoon eyes, CSF rhinorrhea/otorrhea, hemotympanum)
....
,,
� � � � � � � � � � � � � � � � � � �
Signs llf Bual Sladl fl'llcture
Battle's sign {bruised mastoid process)
Hamotympanum
Raccoon ayes (periorbital bruising) CSF Rhinorrhae./()toniiSI
ER8 Emergency Medicine
Traumatology
B. facial fractures (see Plastic Surgery. PL26) neuronal injury beware of open fracture or sinus fractures (risk of infection) unstable or displaced fractures (need semi-urgent plastics referral) severe facial fractures may pose risk to airway from profuse bleeding neuronal injury
Toronto Notes 2011
A. diffuse
� � � �
Warning Sig af S.vwrlllll&d lnjmy
GCS <8 Dell!riDrlling GCS Unequal pupils L.amralizing sip N.B. Altered LOC is a hallmlllk of brain injury.
concussion mild: temporary disturbance of neurological function, complete recovery classical: temporary, reversible neurological disturbance, with temporary (<6 hrs) loss of consciousness, complete recovery diffuse axonal injury mild: coma 6-24 hrs, possibly lasting deficit moderate: coma >24hrs, little or no signs ofbrainstem dysfunction severe: coma >24hrs, frequent signs ofbrainstem dysfunction B. focal injuries contusions intracranial hemorrhage (epidural, subdural, intracerebral)
ASSESSMENT OF BRAIN INJURY
History
pre-hospital status mechanism of injury
Physical Examination
assume C-spine injury until ruled out vital signs shock (not likely due to isolated brain injury, except in infants) Cushing's response to increasing ICP (bradycardia, hypertension, irregular respirations} severity of injury determined by l.level of consciousness (LOC) GCS :s;s intubate, any change in score of 3 or more = serious injury 2. pupils: size, anisocoria >1 mm (in patient with altered LOC), response to light 3.lateralizing signs (motor/sensory} may become more subtle with increasing severity of injury re-assess frequently
llilor
C.utlianCT"-dR....
1lle lMcrl2001; 357:921i6;13911396
er lllld .., ,..._
llllll �
� wilb
mr .. IMialawilg:
� �
r.,....
Investigations
labs: CBC, electrolytes, coags, glucose, tox screen CT scan (non-contrast) to exclude intracranial mass lesions C-spine imaging, often with CT head and neck to exclude intracranial mass lesions
. .risk(fwllllliQioP �
GCSSCOII<15d2hlbrijly &.p.c:tad opllllll dipru.d ltul fnlc:tn Allr sign ri belli tlwl f1ldln (hlmotympnJm, "nr;coon'"""" � � � � � � � Glurrherl
Yamiti'G 0!2 episodes
� � � � � � � � � � � �
lilincmh-. illllll'l 191
Management
general ABCs ensure oxygen delivery to brain through intubation and prevent hypercarbia maintain BP treat other injuries, must treat hypotension, hypoxia (both contribute significantly to mortality) early neurosurgical consultation for acute and subsequent patient management medical seizure treatment/prophylaxis - benzodiazepines, phenytoin, phenobarbital - steroids are of no proven value treat suspected raised ICP -+ consider if head injury with signs of increased ICP: - raise head of stretcher 20 ifpatient hemodynamically stable - intubate and hyperventilate (100% 0 2) to a pC02 of 30-35 mmHg - mannitollglkg infused as rapidly as possible - consider paralysing meds if agitated/high airway pressures - maintenance of cerebral perfusion pressure is critical surgical
. . . . risk !fw IJIIia ijny 111 Almlliuftlr � � � � � >30 mil llqelaus mechllilm !pedntrim 111\Uby mallllwbicil, OCcupllllljlctld from 111111111 wllicle, fdfmm heiglt >311111arfiveslllrs) .......... ildlftn... � � rllliiiiCi--. deliiiE lll'llesil, orwitniiiiSd disorianlllion ill IJIIilriwith I GCS ICCAof 13-15.
en
Tr111tm11nt af ln-ldiCP Elevate head of bed Mannitol Hyperventilate Paralyzing agenl.t58dating agenl$
See also Neumsurqert NS6
Disposition
neurosurgical ICU admission for severe head injuries (HI) in hemodynamically unstable patient with other injuries, prioritize most life-threatening injuries and maintain cerebral perfusion for minor head injury not requiring admission, provide 24-hour HI protocol to competent caregiver, follow-up with neurology as even seemingly minor HI may cause lasting deficits
Toronto Notes 2011
Traumatology
Emergency Medicine ER9
Spine and Spinal Cord Trauma
assume cord injury with significant falls (> 12 ft), deceleration injuries, blWlt trauma to head, neck or back spinal inunobilization (cervical collar, spine board during patient transport only) must be maintained until spinal injury has been ruled out (Figure 2) vertebral injuries may be present without spinal cord injury; normal neurologic exam does not exclude spinal injury cord may be injured despite normal C-spine x-ray (SCIWARA = spinal cord injury without radiologic abnormality) injuries can include: complete/incomplete transection, cord edema, spinal shock
"-{_9,
1118 FoiiDwlng Cl'llllrlll
Midline tandarnass Neurological symptoms or signs Significant distracting injuries Hllld injury Intoxication Dangerous macllanism History of altered LDC
eau.r E"'JOII' with �
� One
of
History
mechanism of injury, previous deficits, SAMPLE neck pain, paralysis/weakness, paresthesia
Physical Exam
ABCs abdo: ecchymosis, tenderness neuro: complete exam, including mental status spine: maintain neutral position, palpate C-spine for tenderness, step-otf, log-roll, then palpate thoracic and lumbar spine; assess rectal tone extremities: check cap refill, suspect thoracolumbar injury with calcaneal fractures labs: CBC, electrolytes, creatinine, glucose, coags, cross and type, tax screen imaging full C-spine x-ray series for trauma (AP, lateral, odontoid) thoracolumbar x-rays AP and lateral views indications: patients with C-spine injury Wlconscious patients (with appropriate mechanism of injury) patients with neurological symptoms or findings patients with deformities that are palpable when patient log-rolled patients with back pain patients with bilateral calcaneal fractures (due to fall from height) - concurrent burst fractures of the lumbar or thoracic spine in 10% (T 11-U) consider CT (for subtle bony injuries), MRI (for soft tissue injuries) if appropriate
Suapac:tad C-spine Injury based on mech111ism of ir1ury (e.g. MVC, fllll, sports)
.....
',
� � � � � � � � � � � � � � � � � � � � � �
Naill: Patients with penetrating trauma {especially gunshot 111d knife wounds)
Cll1 alia hllva spinal
cord injury.
Investigations
... '9l------------------. ,
Of tha investigations, the IIIIBnll C-spina
lf-111'( is the single most important film. 95% of radiologically visible � � � � � � � � � � � � are found on 1llis film.
.....
',
� � � � � � � � � � � � � � � � � � � � � �
CIIUda Equina Syndrome can occur with any spinal cord injury bllow T10 vertebrae. Look for incontinence, anteriar thigh pain. quadriceps weakness. abnormal sacral sensation, decreased rectal tone 111d vuiable reflexes.
History: midline nack pail, numbness or pansthasia, pn1111nce of dirtnu:ting pail, patient haed-injurad, pllliant intoxicated, lOS$ of con1ciousnll$$ or pall history of spinal mobility di1order PhpicaiiiiWII: posterior neck spasm, tenderness or crepitus, any neurologic deficit or autonomic dysfunction, altered mental state
I
Norm11j
C-1pine cleared
No
Yes
C-spine claarad
I
Neck pain
Flexio!Vextension films
j+-
1. Plain Hll'f', 3 viiiWI 2. CT8CII1 if: Inadequate plain film survey Suspicious plain Om findings To bBttar dalinaate injuries sean on plain Oms Any clinical suspicion of atlanto-axial dislocation High clinical suspicion of injury despite nonnal x-ray To include C1-C3 when head CT is indicated in � � � � � � tr-..ma
����������
� � � � � � � spina sarvica
RamBin immobilized,
I
I+Abnonnal neurological axam
H
+-
Nonnalfilms
Abnonnal films
Abnormal
i
MRI
Remain immobilized, consult spine se!Vice
'-tilt Cllblllln I'IMI wllh 'hma NEJM 2003; 341(26):251"l'llpole: To com11111 tile clili:ll IJII(Dnrlnct II tile Can.tiln C.Spine Rule (CCRiand the Nltionll � � � � � � � � � � � � � � � � Udllllion Sludy INEXUSI Law-llit Critliriii!NLCJ. Sllllr. TI1IITI pnllniJ (n=12131 in stJIJia conditioll were � � � � � � � � � � bybolhthe CCR snd If by 384 physicians hlbll radiogrlplv. Z\of1hnl patimhld I C-spin1 injury. llldl: Conlplllld 1111118 If. lhl CCJIMS mora .... 199.4 "1. 90.7\) and1111n !l*lic � � � � � vs. 38.8"1 Iller excusion o1 inddeminlleTh1llllllblr ofmiuld pdlllll would bll far 1111 CCR snd 1& !artie tt.C. The range of motionnot Mltmld ilme CCR C1181ialy blctus8 pilysicilns were no1 con-lur1lbk! will lhe procedure snd lhis ny � � � � � � � � � � � 11111itiuity111 !p1Cili:ilyof1111 CCII in pn1cticl. s..m.y. The CCII il s..... 1111111 If inllart and stable pllillniJ Mh IIIINnl. The u 111111 CCR Clllrtajk i1 bwar lldionlrf lila
n..e...-. e..,m. ....__1111 NEXUS
� � � � � � � �
C-spine claarad
Figura 2. Approach to Clearing tlla C-spina
ER10 Emergency Meclidne
Traumatology
1'oroDio �
� � � � 2011
� � � � � � � � � � � � � � � � � � � � � � �
..Milt (lilllprC.. . .- ; ; 151 . . . . .Trwll .....loflnCd:ll...
Can Clear Cspine if: no posterior midline cervical tenderness
� � �� � �� � � �� � ��
AgaO!liS,_a
(I
(I
� � � � � � � � � �
no evidence of intcW.cati.on oriented to person, place. time and event no focal neurological defidt8 no painful dJ.stracting Injuries (e.g. long bone#)
Management of Cord Injury
U.UIIIIdlrilnr"
l'nllhllils �
� � � � � � �
immobilize
i.
evaluate ABCs
...... � � � ..., �������
-IIH!dr.r.tt
(I
� � � � � � � � � � � � � � � � � � � �
..
�
lt!irtiJI)Iiilllillll
(I
ArriUiDty -vtn
(I
..... � 1
Dri!JIIInatllir.kplill
.......
(I
AlllntIll �
....
� � � � � � � � � � �
1111111tncllllr-.ld7
.....
treat shock: (maintain sBP >100 mmHg) insert NG and Foley catheter high dose steroids: methylprednisolone 30 mg/kg bolus, then SA mglkglhr drip. !tart within 6-8 brs ofInjury (controvenial. and recently has less support) complete imaging of spine and consult spine service if amiable continually reassess high cord Injuries as edema can travel up cord ifcervical cord lesion. watch for respiratory insufficiency low cervical transection (CS-Tl) produces abdomins.l breathing (phrenic innervation of diaphragm still intact) high cervical cord injury (above C4) may require intubation and ventllation beware of hypotension (neurogenl.c shock) treatment: warm blanket. 'fre:ndelenbergposition (occaaionally), volume infusion, consider vasopresson
Approach to C.Spine XRays 3-view C-spine series is the screening modality of choice 1. lateral Cl-Tl swimmer's view (Figure 3, see Table 5 for interpretation) lateral view is best. identifies 90-95% of Injuries 2. odontold view (open mouth or oblique submental view) (see Figure 4) enm1ne the dens fur fi:a.ctures - beware ofartifact (horizontal or vertlcal) caused by the radiologl.calsbadow of the
......
>5'111fllnd ril#f
1--1
'llqanilaMlllihl'ism; � � � � � � � � � � � � � � � � � � � �
� �
M\t � � � � splld (> liiiiMt MIIDril!d--wlicles
Bqdt tdlilln
� � � � � � iml � �
� � � � � � � � � � � � � � � � �
roba;.,.
- ifunable to rule out fracture, repeat view or consider CT or plain film tomography examine laters.l aspects ofCl and spacing relative to C2
3.APview alignment of spinous processes In the midline spacing ofspinous proce88es should be equal check vertebral bodies and facet dlsl.ocatl.ons
teeth overlying the dens
tslrciiiiiHIII MVC .W.:
11br llftrgltnd
RGIDwr
� � � �
� � � � � � � � � � � � �
_ . . NctimllllilllllllrllnaPiil
Supine Oblique VIews
JUM..I001; 216:18411848
rarely used
better visualization of posterior element fractures Oamina. pedicle, facet joint) good tD assess patency of neural foramina can be used to visualize the C7-Tl junction
Tabla 5. lllterpratltion of l..atllral Viaw: Tha ABCS
A _.ICY 11d.Aig11111t Mist a C1 1D C7-TI jnliln; if nat. dllwrMwd 1rBc1ian d thcUdn. swilllllll"s viaw. � � � � � � � � � � � � � � � obliques. II' CT SCII'I needed Linea of CIIIIClll'- in chictan <8 ,.-" of age: Cllll88 jlbyliolagic aubUartion of C2 on C3, and C3 on C4, but the spind.ninallina is rnai1111in.. � � � � � � d spinau& 111'DC811811- suggests pas1llilr liglrnlldllus diiiUIDJn Widrii;J r1 facal joirt$ lhd IIIIIIJID.occipit:!ll joint Lina axtanding inferiorlyfrom clivus ahiUd tnmect odanlllid AllantD-IXiallllii:UII1ion -widening of pradnal space (ncrmal: <3 mm in adui1J, <5 nm in chtlnln) inclcates inillY ofC1 ar C2
3. l'ostlrior barthl' of fiiC81s
2. l'ostlrior 'tWIIbnllline (antJrlor maraln olaplnal canal)
1. Anlllrior vartlbrallile
.l2
4. Llmillr fusion line (pollerior margin of 1pilll CIDII) 5. f'llllaior iipiloua Ina (alq dPI of IIPMUI 1RC88188)
.ii! E
:
fi
111111111 o Hail#lt, wicllland llhlpa at IIICh vertebral body l'ediclas, facats, and ilrillla &h!Ud IPfiR" ana - dDiilling �
� � � � � � ratlllion
c
S
c:.tilll o lnlllvlltllbl'll disc &pleas - wadging lllleriady ar poslaillty suggast& lllltlllnl campiiS&ion
Flgar8 3. Un11 of Crmtour 01 1
Lmral C.Spina x-Ray
SaltTIISUII � � � � � r1 reliqJIIII'jllgelll (no1TT181: <7 rrm at C1-4,1111'f be wide in chidren <2 yrs an apiraticnl or relmlndullll 8piC88 (nonnel: <22rmut C6-T1, <14 mm in chlrhn <5 '/II)
Toronto Nota 2011
TraUIIllltology
.Em.c:lzeocy Medicine ERll
Saqualaa af C-spina Fracturu deaeased descending sympathetic tone (neurogenic/spinal shock) responslble for most sequelae autonomic dysretl.exia: in patients with spinal cord inJurles at or above the T6lem common signs and symptoms: pounding headache, naaal congestion, feeling of apprehension or anxiety, visual changes, and marked increue in systolic and diastolic blood pressure common triggers urinary system.: bladder distention, urinary tract Infection, and kidney stones GI causes: fecal impaction or bowel distention treatment: monitoring and controlling blood preslllll'e. prior to addressiDg CllllBative issue
cardiac no autoregulation, falling BP, decreasing HR. vasodilation management: give IV fluids vasop:ressors respiratory no cough reflex (risk of aspiration pneumonia) no intercostal muscles diaphragm movement management intubate and maintain vital capacity
gastrointestinal ileus, vasodilation, bile and panaeati.c secretion continues (>lUday): risk of asplration, GI
stress ulcers
1. Dana 2. Cl Lateral MaR 3.C2
� � lhll: A. The denl ia centnld belween lhl lateral of Cl B. Cl and C2 1n align-' llltarwly C. The � � � � � � � � � � � � � � � � � � � � � syn111etrical illizi
To c'- th!IJH8'( �
m-
j
0
Figunt 4. C.Spiae X-Ray; Dduntoill View
renal
management: NG tube may be required fur sw:tioning. feeding, etx:.
hypoperfusl.on -+ give IV fluids kidney still producing urine (bladder can rupture ifpatient not urinating) management: Foley catheter may be required (measure urine output)
skin
vasodilation, heat loss, no thermoregulation, atrophy (risk ofskin ulcera) muscle ftaccidity. atrophy, decreued venous return
penis priapism
...... ,
� � � � � � � � � � � � � � � � � �
to OR.
20'1. Ill C.lpin1 frac:luiBIID ICCDm!*lild by othar spilll frlctures. 10 ensu11111uncic Md 1pine x-rays n nDIIIIII before proc.IMilg
mr
Chest Trauma
twotypes A. found and managed in 1 survey B. found and managed in 2 survey A. l.Jt..Thraatenlng Chest InJuries Found In 1 Survey (see Table 6)
Tabla 6. l.ifelllreetening Cllast lnjuriaa Fauad ia 1 Sunray
Anxiety, stridor, lanl111111a, allarad III8IDIIUIIII
\,,
Tra111111 to lhl ches!IICQiu!Qfor 50% of trmnadllllthL
...... ,
� � � � � � � � � � � � � � � � � �
Do nrt wait fer ABG to in11meta
Daliitive liway lllllllglllllll
� � � � � � � � �
Aplaa. cyanosil
� � � � � � � � �
RSIDMI Fll hirilla with IIIYI'CIDIC!fll prior to inbJIItian
80'1. Ill all chill in;.i can b&lllllnqal niii-IU111iCBIIyo with li111JI8 1118111UI'M IUch inbation. chilli: lub18, IIIII pain conlrOI.
Clinical diaplil 0118-W11Y Vlllva c:ausing � � � � � � � � � � � � of air in plaual
l!piiC8
Respil'ltary dislma, NIIHldawaphic lllclr,alrdia. dislandad nack. diacJiasis vails, cyanasis,llyJTIII8by of chest wal malian Tlll:haal daviltion r11R1f fmm pnaui11Dibarlx Percussion � � � � � � � � � � � � � � � � LnlatBnllllbsanceli lnllth aollldl
Needle 1lalcoatDnty -large bara n11lllla, 2nd ICS mid cllwicul.-lile, ftlllawed by chest tube il 5th ICS. lllllliar IIXi'-vhl
\,,
3-lny IMI far Ope1 l'nlllnlltiiDIU � � � � � � � � � Alcrws 1irto - lllring tha expil'l!llrV pl1ale I that YGU don't Gfl I laaian ,..lftlothiiiU) but all ibalf to aiDw ldeqLIIIII br81111s dwing lhl iiiiPil'l!llrV pima.
p......... �
MllllwllllllcdlaiD
cavity
>1500 cc l*lod loss il chalt
Gunshot or CJiher wtml (hde >2/31racheal dimeter) axitwtuld � � � bruh SCU!ds PaiD, flat neck. veins, shock. U..lly any allle1o da lnlllerll dulneu tupine ClCII - entire 1111!1 lJIIII8IIli mdioapllque as ' .Abslft lnllth IOUnds. hypabmilll blood Sjl1!flds out IM!f pastrriar tluncic CIYily
Air-tight dressing l8lled on
3sides Cheat1ube
Sll!liiV
Restare blood wlume Cheat1uba Tlun:otamv if: >1500 cc total biDDd loa � � � � cc.1r conti1118d drainaga
ER12 Emergency Medicine
Traumatology
T1ble 6. Ufe-Threltening Chest Injuries Found in 1a Survey (continued)
Toronto Notes 2011
It'
DDx of Lh Thra...ning Cl-.st lnjurin
Physical Exam
Filii Chast Paradoxical movement Dl o Fre&-ftoating segment of chest flail segment o Palpable crepitus of ribs wall due to >2 ril fractures, o Decreased air entry on each ill 2 sites affected side Underlying lung contusion {cause Dl morbidity and mortlllity)
lnVIIIigllions ABG: decreased � � � � increased pC0 2 CXR: rib fractures, lung contusion 02 + fluid therapy + pain con1rol Judicious fluid therapy in absence of systemic hypotension Positive pressure ventilation intubation and ventilation IVftuids Paricardiocantasis Open thoracDI:omy
HOT 1mt FAT CHEST Hamothoru* Open pneumolhoru. Ta111ion pnaumothoru.*
flail chest Airway obllruc:tion Tamponade*
Cllntusion: pum-rv. myocardial Hernia: 1nlumltic, dilphragmltic ESophngalll perforltion Tracheobronchial disruptiorv' Traumatic injury/TllOr'IICic Aorta
Canlillc Tamponade
o o
Clinical diagnosis Pericardia! fluid accumulation impairing ventricular function
Ruptura*
*Rapidly Liflllhr'81111ning
Penetrating wound {usually) o Beck's 1riad: hypotansion, distended neck veins, muffled heart sounds o Tachycardia, tachypnea o Pulsus paracloxus Kussmaul's sign
EchocardiDIJliTI Bedside ultrasound {FAST}
� � � � � ��
� � � � � � � � � � � � � � � � �
B. Potentially Life-Threatening Chest lniuries Found in 2!' Survey (see Table 7) need to have high index of suspicion, usually dependent on mechanism of injury
Tabla 7_ Potentially UfThralltllning Chest Injuries Found in 2a Survay Pulmon.., Colltulion Blunt trauma to chest Interstitial edema impairs � � � � � � � � � and gas
Kullamuf Sign C...: Constrictive pericarditis Right ventricular myocardial iThlrction Tricuspid mnosis Cardiac Tamponade
CXA: areas of opacification ofllll'(l within 6 hours of trauma
axchange
� � �� � �
..
Maintain adequate ventilation Monitor with ABG, pulse oximeter and ECG Chest physiotherapy Positive pressure ventilation Wsevere Lllparutomy for diaphragm repair end because Dl associated intrHbdominal injurias
� � � � � � � � � � � � � � � � � �
Ruptured Dii!phl'lgm
Ruptured diaphragm is more often diagnosed on 1he left side, as liver concaall right sida dafect.
Blunt trauma to chest or abdomen {e.g. high lap belt in MVC)
CXR: abnormality Dl
o
dil!plngrn/lower lung fields,ING tube placement CT scan and endoscopysometimes helpful for diagnosis
� � � � � � � � � � � � � � � �
Usually penl!lnlting trauma {pain out Dl proportion to degree Dl � � � � � �
CXA: mediastinal air {not
always)
Early repair {withil 24 hrs) improves outcome but all
require repair
Esophagram {Gastrograffin) Flexible esophagoscopy
Aartic Tau: ABC WHITE
X-ray faaluras of Aortic lllar daprassld l.rt mainstlm Bronchus pleural Cap
Wid& mldiallinum (most consislllntl HemathOiliX Indistinct aortic lmuclda Tracheal deviation to right 5ide
(Note: pment in 85% Df cases, but cannot rule out)
Sudden high 1peed decBieration Aarlicleu {e.g. MVC, fall, airplane crash), 90% tear at subdavian {near ligamentum arteriosurn), corr1lfainls Ill chest pain, most die at scene dyspnea, hoarseness {fraquently absent) SSvageable Wdiagnosis Decreased femoral pulses. made rapidly differential arm BP {arch 1elr) Blunt trauma to chest {usually in setting Dl multi-system treuma � � � � therafore � � � � � � � � � to diagnose) Physical examination: overlying injury, e.g. fractures, chest wall contusion
o
CXR, CT scan. Thoracotomy {may treat transesophageal echo {TEE), other severe injuries frst) acrtography (gold standard) See sidebar for CXR features
ECG: arrhytlmias, Patients with anormal ECG and normal hemodynamics never get dysrhythmia
Esophagus (NG tubal deviatad to right
ST chroges
Antiarrhythmic agents Analgasia
� � �
rt,
C. Other Potentially Life-Threatening lniuries Related to the Chest Penetrating Neck Trauma includes all penetrating trauma to the three zones of the neck (Figure 5) management injuries deep to platysma require further evaluation by angiography, contrast CT or surgery do not explore penetrating neck wounds except in the OR
If l'nltrating N..:k T111uma pn1. .nt.
DONT: Clamp structures (can damage nerves) Probe Insert NG tuba {leads to bleeding)
Ramova WlllpllrVirnplllad objact
'IbroDlo Nota 2011
Emeqmcy Medidne ER13
Airway Injuries always maintain a high index ofsuspicion
larynx history: mangulation, clothes line, direct � � � � � blunt trauma, a.ny penetrating injury involving platysma triad: hoarseness, subcutaneous emphysema, palpable fracture crepitus other symptoms: hemoptysis, dyspnea, dysphonia investigations: CXR, cr scan, arteriography (ifpenetrating)
IDllJlll8eiii.ellt
airway - Ill81l8ge early because ofedema C-apine may also be injured, consider mechanism of injury Z'Dnal \ surgi.cal- tracheotomy vs. repair trachea/bronchus I frequently missed Z.. Ill: Superior If*! Df nec:k history: deceleration, penetration, increased intra-thoracic pressure; complaints ofdyspnea, Z.. II: Midportion al nack. (cricoid to hemoptysis the angle af mandible) examination: subc:uta.neous air, Hamman's sign (crunching sound synchronous with heart beat) Z..l: a- of nec:k (lhllracic ii'W ID cricoid cartlaga) CXR: mediastinal air, penistent pneumathoru: or penistent air leak after chest tube inserted fur pneumothorax Figure 5. Zon of tile Neck In management surgical repair if>1/3 circumference Tr111111
_..
Abdominal Trauma
two mechani&ms blunt: usually causes soll.d organ injury (spleen injury is most common) penetrating: usually causes hollow organ injury or liver injury (most common)
BWNTTRAUMA results in two types ofhemorrhage intta-abdominal bleed retroperitoneal bleed adopt high clinical suspicion ofbleeding in multi-system trauma History
mechanism of inJury, SAMPLE history
.....
',
',
� � � � � � � � � � � � � � � � � �
S.dbllt Ralroperi1D1111I dulldanal truna
nirias.., c-
lnlrllpllrilllnell bowallnlni8Ciion
MalaniBric injll'( Lspiolainjury
....
� � � � � � � � � � � � � � � � � �
Physical Exam often unreliable in multi-system trauma slow blood loss not immediately apparent other injuries may mask symptoms serial eumlnations are required abdomen inspect: contusions, abrasions, seatbelt sign, distention auscultate: bruits. bowel sounds palpate: tenderness, rebound tenderness, rigidity, guarding DRB: rectal tone, blood, bone fragments. prostate location placement ofNG, foley catheter should be considered part of the abdo exam other systems to assess: CVS, respiratory (possibility ofdiaphragm rupture), pelvis, back. neuro as it pertains to abdo sensation, GU
Investigations labs: CBC, electrolytes, coags, cross & type, glucose, creatinine, CK.lipase, amylase, liver enzymes. ABG, blood EtOH.Jl-hCG, U/A, tax screen imaging: see Table 8
11.....,11 far Faler IIIII NG Nlll11 Alnlllllinlll ,,_..
� � � � � � � � � � � � � � � uncon..-::iou. � � � willl nUiipla injuriaa who cannot void lpDnllnaousfy. �
COIDalrdclll-= blood 11t1118 meaiUI,
.. ..-::chymatic 1crDtlall, or '"higllriding" pniS1atl on DRE (r'llr'DOnlda � � � � � � � � � iJ nliealed to rule out
a ul'fllnl war or � � � � � bladd.-1. N6 ...,.: u.ed to dscomp!IIM1h8
llolliiCh IRI prmci'nllllllllll bawel.
COIDalrdclll-= facial frae1lnl ar ba11aJ llkl.l frac:tul8i IU.ped8d.
.....
',
� � �
Crbril far >10 ccpsi*Jod BIB, blcllril. foreign ll'llhlrill
Paililll._..
Tillie I. lm111ing i1 Al11laminel Tn1m1
X-Ray
RBC caunt >I 00,000 x 1OS,t WBC >500 x 10'1\, emylaa > 1751U
Chest (lootilg fir � � � � � � � � under diaplngm, diaph111g1Bic Saft tissue mt wei visualilld hernia. ai'.ftlid lewis!, peMs. � � � � � � � � � 1hlncic, lurmar spines
cr. .
Diqlllllli: ,.......
Most apecific tart Most S8IISi1iva I8St Tesls fir Dnl-pllii:Dneal bllllld
ldllllifia pnl&lll1ct/llbsln:a af frae til il pari1alaal t&Yily RAPID IIXllll: lass lim 5minute& C..lllsa IXII'IIins pwicardium nl pilunll cavitias
LMII(DPLJ
......._.:FAIT (FGCUI8d Abdamilll Sanag11m far T1111m1d
diaphiiiQIIIID:. , . C..nllt distivJjsh lethal from bivialllleed Ralullt can 111ka up to 1hr
t.lnot use � � lwmodynlllic ins1llblity t.lnot tart fa' nlll'apelitlnNII bllllld or
Radillion 8Xplll118 2Dx mn thmlHIY
NOT used til ilantify specific llf'llll" quria If patin hils asci11s. FAST wil be fBisely
positivl.l
ER14 Emergency Medicine
Traumatology
Toronto Notes 2011
.._,,
..
� � �
imaging must be done if equivocal abdominal examination, suspected intra-abdominal injury or di5tracting injuries multiple trauma patient resulting in unreliable physical exam (altc:rc:d sensorium, e.g. secondary to drugs, alcohol, head trauma. or distracting injury; spinal cord injury resulting in abdominal anesthesia) unexplained shock/hypotension multiple trauma patients who must undergo general anesthesia for orthopaedic, neurosurgic:al, or other injuries fractures oflower ribs, pelvis, spine positive FAST
� � � � � � � � � � � � � � �
l.aplrmmr 11 Mndaiiii'J if ............ l'raumllnd:
ShDt:k l'lritonilis Eviscemion
Management general: ABCs, fluid resuscitation and stabilization
surgical: watchful wait vs.laparotomy solid organ injuries: dc:ctsion based on hemodynamic stability, not the specific injuries hemodynamically unstable or persistently high transfusion requirements: laparotomy hollow organ injuries: laparotomy even if low suspicion on injury: admit and observe for 24 hours
Frle air in abdomen Blood in NG tube, Foley catheter, or
on racllll exam
.._,,
� � � � � � � � � � � � � � � � � � �
PENETRATING TRAUMA
high risk of gastrointestinal perforation and sepsis history: size of blade, calibre/di5tance from gun, route of entry local wound exploration under direct vision may determine lack of peritoneal penetration (not reliable in inexperienced hands) with the following exceptions: thoracoabdominal region (may cause pneumothorax) back or flanks (muscles too thick)
"Rulli Dllbinla" far tab waunda:
1/3 do not penslniiB paritoll&lll cavity
113 penellate but are harmless
1/3 CIIU$8 injury requiring IIUrgery
Management general: ABCs, fluid resuscitation and stabilization
gunshot wounds -+ always require laparotomy
Genitourinary Tract Injuries
see Urology. U32
Etiology
blunt trauma - often associated with pelvic fractures renal contusions (minor injury- parenchymal ecchymoses with intact renal capsule) renal parenchymal tears/laceration: non-communicating (hematoma) vs. communicating (urine extravasation, hematuria) extraperitoneal rupture of bladder from pelvic fracture fragments intraperitoneal rupture ofbladder from trauma and full bladder anterior (bulbous) urethral damage with pelvic fractures ureter: rare, at uretero-pelvic junction penetrating trauma damage to: kidney, bladder, ureter (rare) acceleration/deceleration injury renal pedicle injury - high mortality rate (laceration and thrombosis of renal artery, renal vein, and their branches) iatrogenic ureter (from instrumentation)
\,
G1011 hematuria 1111gg811J bladdlr injury.
History
mechanism of injury hematuria (microscopic or gross), blood on underwear d)15uria. urinary retention history ofhypotension
....
,,
Physical Examination
abdominal pain, flank pain, costovertebral angle (CVA) tenderness, upper quadrant mass, perineal lacerations DRE: sphincter tone, position of prostate, presence ofblood scrotum: ecchymoses, lacerations, testicular disruption, hematomas bimanual exam, speculum exam extraperitoneal bladder rupture: pelvic instability, suprapubic tenderness from mass of urine or extravasated blood intraperitoneal bladder rupture: acute abdomen
� � � � � � � � � � � � � � � � � � �
In the case of gross hematuria. the GU syst8m is invntig11t1d from distaltD proximal ii.e. urethrogram, cystugram, etc:.)
Toronto Notes 2011
Traumatology
Emergency Medicine ER15
Investigations urethra: retrograde urethrography bladder: urinalysis, CT scan, urethrogram, retrograde cystoscopy, cystogram (distended bladder +post-void) ureter: retrograde ureterogram renal: CT scan (best, ifhemodynamically stable), intravenous pyelogram (IVP) Management urology consult renal minor injuries - conservative management bedrest, hydration, analgesia, antibiotics major injuries -admit conservative management with frequent reassessments, serial urinalysis, reimaging surgical repair (exploration, nephrectomy): e.g. hemodynamically unstable or continuing to bleed >48 h, major urine extravasation, renal pedicle injury; all penetrating wounds and major lacerations, infections, renal artery thrombosis ureter uretero-uretostomy bladder extraperitoneal minor rupture: Foley drainage x 10-14 days major rupture: surgical repair intraperitoneal drain abdomen and surgical repair urethra anterior: conservative, if cannot void -+ Foley or suprapubic cystostomy and antibiotics posterior: suprapubic cystostomy (avoid catheterization) surgical repair
Orthopaedic Injuries
see Ortho.paedics (Shoulder, Knee, Wrist, Ankle)
Goals of ED Treatment identify injuries accurately and address potentially lifellimb threatening problems appropriately reduce and immobilize fractures (cast/splint) as appropriate provide adequate pain relief arrange proper follow-up if necessary History useSAMPLE mechanism of injury may be very important Physical Examination Look (inspection): "SEADS" Swelling, Erythema, Atrophy, Deformity, Skin changes (e.g. bruises) Feel (palpation): all joints/bones -local tenderness, swelling, warmth, crepitus, joint effusions, subtle deformity Move: joints affected plus above and below injury - active ROM preferred to passive Neurovascular status: distal to injury (BEFORE and AFTER reduction) LIFE AND LIMB THREATENING INJURIES (see Table 9) threat to life is usually due to blood loss (e.g. up to 3 Lin pelvic fractures, 1.5 L per long bone fracture) threat to limb is usually due to interruption of blood supply to distal part of limb or to susceptible part of bone Table 9. Life and Umb Threatening Ortllopedic Injuries
Ule Tlll'lllllning �
��������
'1:'
� � � � � � Ill Frac:tu-
SOlARTAT Sit&
Leng1t1 Articular lloiDion Translation
Open vs. closed
Type {a.g. �
� � � � � � � � � � � � � � � � �
� � � � � � � � � � � � � �
1111:.1
""'� � I
� � � � � � � � � � � � � � � � � �
Consultalian
a.u- fvr Ergent Orthop..UC
� � � � � � � � � � � � � IYfldroma Irreducible dislocation Circulatory compromise
Opan fnlcbn
Injury requiring surgiclll repair
� � � � � � �
Umb Tlln111bning �
Crush injuries
Major pelvic fraclires Traumatic amputations
Fracture/dislocation of artie {llllar AVN) Compartment syndrome
Massiwlcng bona injJri111 (bawara of fat emboli)
Vascular iljury proximal to knBII{albcw
Opanfr.lctum
Dislocations of knefo'hip Fractures above knee/elbow
ER16 Emergency Medicine
Traumatology
Toronto Notes 2011
� � �
When Dealing with an Open Fracture, Remember "STAND" Splint Tetanus prophylaxis Antibiotic Neurovascular status (before and after) Dressings (to cover wound)
Open Fractures communication between fracture site and external surface of skin - risk of osteomyelitis remove gross debris, irrigate, cover with sterile dressing - formal irrigation and debridement often done in the OR control bleeding with pressure (no clamping) splint antibiotics (1st generation cephalosporin and amino glycoside) and tetanus prophylaxis must secure definitive surgical care within 6-8 hours Vascular Injuries realign limb/apply longitudinal traction and reassess pulses (e.g. Doppler probe) surgical consult direct pressure if external bleeding
� � �
Vascular injury/compartment syndrome is suggested by "The 6 Ps": Pulse discrepancies Pallor Paresthesia/hypoesthesia Paralysis Pain (especially when refractory to usual analgesics) Polar (cold)
Compartment Syndrome increased interstitial pressure in an anatomical "compartment'' (forearm, calf) with little room for expansion, resulting in decreased perfusion and potential muscle/nerve necrosis excessive pain which is worse with passive stretching and refractory to analgesia is the hallmark sign early on; also look for "the 6 Ps" (see side bar) requires prompt decompression - remove constrictive casts, dressings; fasciotomy may be needed emergently
1. Dorsal tilt 2. Dorsal displacement 3. Ulnar styloid fracture 4. Radial displacement 5. Radial tilt 6. Shortening
UPPER EXTREMITY INJURIES anterior shoulder dislocation axillary nerve (lateral aspect of shoulder) and musculocutaneous nerve (extensor aspect of forearm) at risk seen on lateral view: humeral head anterior to glenoid reduce (traction, scapular manipulation), immobilize in internal rotation, repeat x-ray, out-patient follow-up with ortho with forceful injury, look for fracture Colles' fracture (Figure 6) distal radius fracture with dorsal displacement from Fall On an Outstretched Hand (FOOSH) AP film: shortening, radial deviation, radial displacement lateral film: dorsal displacement, volar angulation reduce, immobilize with splint, out-patient follow-up with ortho or immediate orthopedic referral if complicated fracture if involvement of articular surface, emergent orthopedic referral scaphoid fracture (see Figure 7 for review of carpal bones) tenderness in anatomical snuffbox, pain on scaphoid tubercle, pain on axial loading of thumb negative x-ray: thumb spica splint, re-x-ray in 1 week bone scan positive x-ray: thumb spica splint x 6-8 weeks, re-x-ray in 2 weeks risk of avascular necrosis (AVN) of scaphoid if not immobilized outpatient ortho follow-up
Figure 6. Calles' Fracture
Metacarpal bones (1-5)
Elisheva Marcus
LOWER EXTREMITY INJURIES ankle and foot fractures see Ottawa Ankle and Foot Rules (Figure 8) knee injuries see Ottawa Knee Rules (Figure 9) avulsion of the base of 5th metatarsal occurs with inversion injury supportive tensor or below knee walking cast for 3 weeks calcaneal fracture associated with fall from height associated injuries may involve ankles, knees, hips, pelvis, lumbar spine
Figure 7. Carpal Bones
Toronto Nota 2011
Trallllllltology
.Em.c:lzeocy Medicine ER17
\,
Rlutne ''" Spii'Die
IINit:M pain IINit:M firilar damaga tD vassals and niiMitl IINIC811 rilk Ill' inadwnlllntly converting clallad frll:ture into 1n opfnlelure
Faclibrtu �
� � � � � � � � � � � � � � � � � �
LATBIAL VIEW
MEDIAL VIEW
ArzmllfriiiiiMI.WII IIIIIIID Emili .llfJ Zll3; 321(131&1;411
� � � � � � � � � � �
An ankle raclog!IPhic l8liel il requi'ed only if there il any pain il maleolar mne llld any of lheee findi11111: 1. bone llndarness at A
2. bema tandamassllt B
or or
rna. ......
ai.Ankii . .
IMfalt,.....
3. ir.hility to be..- waight both iiTIIIadiBWy and il IRIIIIQIII1C'f �
Afuot �
� � � � � � � � � � � 11rie1 i1 �
� only if U.. ilany pain in midfuot l!lne md any of lheee fioldinp:
1. bona taldamass at C
2. bone IBndllmiiU 111: D
or
3. ir.hility to bear waight bDth immlldiBWy and i1 amargancy �
or
� � � � � � � � � � �
IIIIIiliirlillilg 15,58'1 � � � � � � � � � � � � � � � � � � � lpiCiicily r1111a Dlllwl rill IIMs flr..w61g frii:Uel Gltht nile ...tniclfuDt ....: 1111-paolad lbhodl1liJ rlaMQIIM flllllablaiilg I filii neaD!IIIIalilb 'Mth I hl:bn 111111 dlllllrial Dba 0.011 l'ur bdh IIIB
� � � � � � � � � � � � � � � � �
l8flliirin
,t,daJUdhm Stillltt.lll../NoM 1994; 211 ;121-832
F'111f8 a. DUnn Anlda Rulas
rilllnlll'id-illt .......� � � �
� � � � � � � � � � � � � � � � �
jiMia llllmlllll inllnlrllt ..w6lg frlnllllfiiiiButil...t mi!UoGiwlh 1 �
� � � pMillnts willl ana ar man Df:
A knlllHIJ Ulmilllti is nqund 11111r far acute �
Age 55 years Dr alder
riMriii!IIDIIIII...nliyriM. n. 1111 rllNs ils1nnwrt "" l'llllc8111a lllll'ia' rl 1111-.ylllf.,.....
"no .bon,...,_Gfm.. ott.tt.. potllll � � � � lllllllflrwelahti'Mce onto 8ICII 1oww lrm llglldeD olllmplng
Tanda1111SSat haed offibjja llcla!Bd tand.-n811 of patella blbility to flex 1o !Ill" blbility to bill' � � � � both immediately and in the emergency �
� � � � � � � � � � (faur � � � � � � � � �
,t,daJUd hm: StillIII. II.JW( 1987; �
F'111re 9. DUnn ICiae Halas
� � � � � � � �
Wound Management
Goals of ED Treatment identify InJuries and stop any active bleeding- direct pressure
manage pain 'WOUild examination and exploration (history and physical) cleansing antibiotic and tetanus prophylaD repair and dressing
Tetanus Prophylaxis both tetanus toxoid (Td) and immunoglobulin ('I'IG) are safe (and indicated) in pregnaru:y
AHie 'lhllhllt .t c...t.llne
RICE
lllllt
Elevation
ea.-ion
let
Table I D. Galdellnaa hr Tat Prophylaxla hr Weundl
Nan TIIIBau "'-W111ndl
..
..._. U.. Duration
reP
lh:llllil or <3 dose8
noa
No No
No
Td
Y8l
liG
Y8l
� � � � � � � �
Yea
. . . .Wilt
a. will!
3or111018.nonefor>10years
3 or 111018. 5to 10 years 9
Yes
No
Yes
Yas
No
No
3or11'1111!, <4yeaugo
1 Wllllll >& lanJ oM, >1 an dllp..
No
No
Yes
No
JU1CUa.wt1, aUialll, WIIIIIIIIIIUq fnRn niaia, tiUih 'MIIIII, U..,fml1lnl. Wlllliiii:IIDlrW!da! wi1h *'.
� � � � � � � � � � � � � � � � �
Solnt: /MMI2001; �
I tn1u1 imruJa � � � � � � � � � � � 250 UID. . . . � � � � � � � � � � � � � � � � � � � � � 401RRIZ)..1-5Z.
��������������������������������������������������
.
Fact
-Wit
....
1-0
..... ......,
� �
Not.Jailt
4-0
3-4
10
1
,._ ,........,.
...�
4-0
����������������
tt'A
Bruises
NB.I'IIiml111111ni1 thtnpy may 1111111 IIDnll i1 fir ..... parilll rllirll
non palpable = ecchymosis palpable collection (not swelling) = hematoma following blunt trauma assess for coagulopathy (e.g. liver disease), anticoagulant use
......
� � � � � � � � � � � � � � � � � �
.o.n.tivH ta ........
fiSSU8gU Steri8biPI* Slap!
ER18 Emergency Meclidne
Traumatology
1'oroDio �
� � � � 2011
Whn NOT to Ule local anlllthetie with !IPNplml: Ean. Noee. Fi9n. ,._ IIIII HOie
tl'lniJ
Abruions partial to full thickness break in skin management clean thoroughly; local anesthetk. with brush to prevent foreign body impregnation (tattooJng) antiseptic ointment (Polysporm or Vaseline) for 7 days for facial and complex abrasions tetanus prophylaxis (Table 10)
Lacerations see also Plastic Sw:ge:cy. PL6 consider every structure deep to a laceratlon injured untll proven otherwise In band InJury patients, Include following In history: handedness, occupation, mechanism of Injury, previous history of Injury
I{.,
llifflnlllild Diaalli of C.lltis Necntizing Ftllciitis Gat gqrene
CUIIIIB!UIIIIIIInx
Vecci1ia '11Cci111ion -.et bil8 (hypereellliiMt'fl
Al:ulagaut
physical exam think about underlying anatomy
DVT
Fixld*ua....cion
IC&waJaki'
� � � � � � � � � � QIUIIJIRiaJm
examine tendon function actively against reaiatance and neurovascular status distally clean and explore under local anesthetic; look fur partial tendon injuries x-ray or ultrasound wounds if a foreign body Ia suspected (e.g. shattered glass) and not found when exploring wound (remember: not all foreign bodies are radiopaque), or if suspect intra-IU"ti.cular involvement
It'
management disinfect skin/use ste:dle techniques Irrigate copiously with normal saline
FuluiR Ill NH..ming Faciilil
llflctilll
ABCDE
A- Anaerobic, Alll'llbic, MM. Antibiatice nlfrlcttry
1- lactaial aynargilllic QMQitln&,
Blood miDI h9lar than norm.. C- CIIIUitis, C111pilus, IIIII
D- D&mllllQIIIIIJIII1&, D*v in preuntalion almost fatll E- Eiythema with IPQIIding Edema
eoopethy
analgesia anesthesia (Figure 10) maximum dose oflidocaine: 7 mgllcg with epinephrine 5 mgflcg without epinephrine In clilldren, topical anesthetics such as LET (lidocaine, epinephrine and tetracaine) and In selected cases a short-acting benzodiazepine (midazolam or other agents) for sedation and amnesia are useful secure hemostasis evacuate hematomas, debride non-viable tissue, remove hair and remove foreign bodies propbylectic antibiotics suture unless dtlayed presentation, a puncture wound. or mammalian bite take into account patl.ent and wound factors when considering suturing advise patient when to have sutures removed
Digital arteriBa
Palmar digital n8MII
Flgera10. Digital Block- Local Anelltllllla of Dlgn.
I{.,
&.1y �
are 1ha most imparlllnt fllclln in
deer1181ing inflelion.
� irrigdion and dabridanun
Cellulitis see also Plastic SuQ:'ecy. PL12 localized Infection of the dermis bacterial (S. aureus, GAS, H. injlf.renzae. occasionally PseudomotUU spp., MRSA) infection of skin and subcutaneous tissues look fur "rubor, calor, dolor, tumour" (erythema, warmth. pain, swelling) have high Index ofsuspicion in patients who are immunocompromised (e.g. HIV; DM), vasculopaths, IV drug users treat with immobilization and elevation of infected area. antibiotics, analgesics. and close follow-up antibiotics for mild cellulitis: PO cephal.exin or cloxacillin ifMRSA: PO clindamycin, doxycycline, TMP-SMX; IV vancomycin ifbateremic
Abscess
I{.,
Wllic . _ _ 111111 AnlllialiCI'I Evidence all'(ltlmic ln1111le.g. calulilill 0 hmunDCOI'IVfllllisad pllillll l'ltillllt at risk for endol:ll'ditis
may be associated with a retained foreign body look for warm, swolle.n. painful, erythematous fluctuant masses ensure absence of systemic symptoms and presence ofsubcutaneous air In simple abscesses anesthetize locally treat with indsion and drainage antibiotics - apply warm compress, give analgesics
Toronto Notes 2011
Traumatology/Approach to CommonER Presentations
Emergency Medicine ER19
Trauma in Pregnancy
priorities: Airway, Breathing, Circulation
Hemodynamic Considerations near term, inferior vena caval compression in the supine position can decrease cardiac output by 30-40% (see Maternal Physiology, Obstetrics, OB3) use left lateral decubitus (LLD) positioning or hip bolster to alleviate compression and increase blood return ifBP is low BP drops 5-15 mmHg systolic in 2nd trimester, increases to normal by term HR increases 15-20 beats per minute by 3rd trimester Blood Considerations physiologic macrocytic anemia of pregnancy (Hb 100-120) WBC increases to high of20,000 Shock pregnant patients may lose 35% of blood volume without typical signs of shock (ie. tachycardia, hypotension) the fetus may be in shock" due to contraction of the uteroplacental circulation fetal HR changes are an early warning of maternal circulatory compromise Management Differences place bolster under right hip to stop inferior vena cava compression fetal monitoring (continuous tocographic monitoring if possible viable fetus >20 weeks) early obstetrical consult do not avoid necessaryx-rays, but shield as much as posssible consider need for RhoGAM if mother Rh negative
.....
,.. ,
� � �
The best 1relltment for 1ha fvlus � � 1ha IIIICIM netment of 1h1 mo1hw.
Approach to Common ER Presentations
Abdominal Pain
Rule Out Life-Threatening Causes CVS: MI, aortic dissection, ruptured AAA (tearing pain) GI: perforated viscus, hepatic/splenic injury, ischemic bowel (diffuse pain) gynecologic: ectopic pregnancy Additional Differential Diagnosis GI: appendicitis, divertic:ulitis, bowel obstruction, hepatitis, cholecystitis, pancreatitis urinary: cystitis, pyelonephritis, ureteral calculi genital female: pelvic inflammatory disease (PID)/salpingitis, tuba-ovarian abscess, ovarian torsion, ovarian cyst, endometriosis male: testicular torsion, epididymitis other: diabetic ketoacidosis (DICA), Herpes Zoster VllUS (HZV), intra-abdominal abscess, pneumonia, lead poisoning, porphyria. sickle cell crisis, psychiatric History and Physical Examination determine onset. course. location and character of pain: PQRST broad differential, including GU, Gyne. GI, respiratory, and CV systems recent/remote abdominal trauma/surgeries general appearance, vitals, ABCs respiratory, CVS abdomen and back: CVA tenderness, ecchymoses, stigmata ofliver disease, DRE, pelvic exam (females), genital exams (males) extremities: differential pulses, psoas/obturator sign Investigations do not delay consultation if patient unstable CBC, electrolytes, glucose. LFTs, amylase, BUN/creat, U/A, +others if indicated: � � troponins AXR: look for calcifications, free air, gas pattern, air fluid levels CXR upright: look for pneumoperitoneum (free air under diaphragm) U/S: biliary tract, ectopic pregnancy, AAA, free fluid CT: trauma. AAA, pancreatitis, nephro/urolithiasis, appendicitis and diverticulitis
I
IIIII Flap Exlr8mas of aga Unstable vital signs
Fava"
Sign.tsymptoms of shock Rapid onset savara pain
Abdamlnal AIHument In all
OuUram.
DR.GEIM
Distention Rigidity Guarding EvisceratiorVEcchymosis Rebound lllndemess Massas
.....
,,
� � � � � � � � � � � � � � � � � � �
� � � � �
ECG,
If both AST and ALT elevated, AST > All indicllbls polllntiallllcohol rUrted hlpatic disi8US All > AST indicllles viral hepatic pathology If ALP lind GGT elevated, 1hink
biliary traa
ER20 Emergency Medicine
Approach to Common ER Preaentations
Toronto Notes 2011
......
t-----------------,
Management
NPO, IY, NG tube, analgesics growing evidence that small amounts of narcotic analgesics improve diagnostic accuracy of physical exam of surgical abdomen consult as necessary: general surgery, vascular, gynecology, etc.
Old IIQ"I, pr.gnancy (T3), lll1d chronic carticiNilllnlid u1e can blunt parilllneal findings, so hava � � � � � � � � � � suspicion of intrabdomi1111l � � � � � � � � in these individuals I
Disposition
admission: in addition to a surgical abdomen, admission is sometimes required for workup of abnormal findings on investigation, IV antibiotics, pain control, etc. discharge: patients with a negative lab and imaging workup who improve clinically during their stay; instruct the patient to return if severe pain, fever, or persistent vomiting develop
Unllllble petien!lllllould not be sent for imaging.
Acute Pelvic Pain
Etiology
gynecological 2nd most common gynecological complaint after vaginal bleeding ruptured ovarian cysts - most common cause of pelvic pain, follicular cyst most common type ovarian torsion - rare, 50% will have ovarian mass leiomyomas (uterine fibroids) - especially with torsion of a pedunculated fibroid or in pregnant patient (degeneration) ectopic pregnancy- ruptured/expanding/leaking spontaneous abortion - threatened or incomplete infection - PID, endometritis, tuba-ovarian abscess dysmenorrhea and endometriosis non-gynecological GI - appendicitis, constipation, bowel obstruction, gastroenteritis, diverticulitis, IBD, IBS GU - cystitis, pyelonephritis, ureteric stone other - porphyria, abdominal angina, aneurysm, hernia, zoster
All woman of childb811t'ing IIQ"B assumed 1D be pregnant untH provan Dlherwise.
.....
, t-----------------,
Gynecol'lliclll C.uses .t' P.m.: Pain: av.illl1 Cyst
Dysmenorrhe1 MittelshmaR Endometriosis av.i1111 Torsion
lbrine Fibroidl/neopllsm Adnexal Neoplasm P1D + Cervicitis
History and Physical Exam
determine onset, course, location and character ofthe pain associated symptoms: vaginal bleeding, bowel or bladder symptoms, radiation
vitals
gynecological exam abdominal exam
.....
, J-----------------,
Investigations
fl-hCG for all women of childbearing age CBC and differential, PTT/INR pelvic and abdominal U/S - evaluate adnexa, look for free :O.uid in the pelvis or masses, evaluate thickness of endometrium doppler flow studies for ovarian torsion
illhe prefamld imaging madllity illhe ll55essment of ecute pelvic pain.
� � � � � � � � � � � �
Management general: analgesia, determine if admission and consults needed gynecology consult if history and physical suggestive of serious cause
other consults as indicated - general surgery, urology, etc. specific: ovarian cysts unruptured or ruptured and hemodynamically stable- analgesia and follow-up ruptured with significant hemoperitoneum - may require surgery ovarian torsion - surgical detorsion or removal of ovary uncomplicated leiomyomas, endometriosis and secondary dysmenorrhea can usually be treated on an outpatient basis, discharge with gynecology follow-up PID: requires broad spectrum antibiotics
Disposition
patients requiring IV therapy or surgery should be admitted patients to be discharged should be given clear instructions for appropriate follow-up
Toronto Notes 2011
Approach to CommonER Presentations
Emergency Medicine ER21
Altered Level of Consciousness (LOC)
Definitions altered mental status - collective, non-specific term referring to change in cognitivt: function, behaviour, or attentivt:ness delirium - acute. transient. fluctuating, potentially revt:ISible organic brain disorder presenting as altered LOC and attentiveness (see PYthiatry. PS 17) dementia - insidious, progressivt:, organic brain disorder with change in memory, judgment, personality and cortical function (see Psychiat:cy. PS18) lethargy- state of decreased awareness and alertness (patient may appear wakeful) stupor - unresponsiveness from which the patient can be aroused coma -a sleep-like state, not arousable to consciousness (Figure 11) use the GCS to evaluate LOC (see Initial Patient Assessment and Management, ER2)
C11111a (GCS :sBJ
I
MET AB-
...
(MaJorttvf
-I
(Minllltty]
Toxic,/Metabolic Major organ failure Electrolyte/Endocrine Toxi'1t11'11!111erature Acid disorders a.e disordtn decreased DX'(9an laval l.actab Insulin/Infection (sepsis) Canliac;lhyperCalcemia
Billl!nl Cerebral {affecting �
� � � � � � � � � � � � � � � � � � � � � � �
.
I
...
J
Primary CNS Dii8UII/Tra.Jma
Brainstem (affecting RAS)
It'
Polaillle C..n of Co1111
AEIDUTIPS Acidosis/Alcohol Epilepsy lnt.ction Dxyven (hypoxiai/'Dpialllli Uremia TempenrturW'JI'IIIIIMI (especially head) Insulin (too littlll or too much) Psychogenic;,ll'oisoning
DLI C-
...
Diflusa traumafiSchemia
II
...
Diffuse lesion
...
Compression Supn(lnfratentorial tumour Sub/epidural hemetoma
...
Direct Brainstem irnrct or hemorrhage
Strub
Figure 11. Etiology of Co11111
MANAGEMENT OF ALTERED LOC
..._, !
,.-----------------.
History obtained from family, friends, police, paramedics, old chart, etc. onset and progression abrupt onset suggests CNS hemorrhage/ischemia or cardiac cause progression ovt:r hours to days suggests progressive CNS lesion or toxic/metabolic cause preceding events it is essential to determine patient's baseline LOC preceding deterioration antecedent trauma, seizure activity, fever past medical history (e.g. similar episode, depression, avt:rdose) Physical Examination ABC's, vitals including temperature, cardiac, chest, respiratory, abdominal exam, and the "five Ns" (see sidebar) complete neuro exam, in particular examination of the eyes, look for medic alert bracelet Investigations rapid blood sugar, CBC, electrolytes, Cr, BUN, LFTs, glucose, serum osmolality; ABGs, coags, troponins, U/A ECG, CXR, CT head drug levt:ls of specific toxins if indicated Diagnosis administer appropriate univt:rsal antidotes thiamine 100 mg IV if history ofEtOH or patient looks malnourished one ampule DSOW IV if low blood sugar on finger-prick naloxone 0.4-2 mg IV or IM if opiate overdose suspected distinguish between structural and toxic-metabolic coma structural coma pupils, extraocular movt:ments and motor findings, ifpresent, are usually asymmetric look for focal or lateralizing abnormalities toxic-metabolic coma dysfunction at lower levels of the brainstem (e.g. caloric unresponsivt:ness) respiratory depn:ssion in association with an intact upper brainstem (e.g. equal and n:activt: pupils; see exceptions in Table 11) extraocular movements and motor findings are symmetric or absent
In general. GCS under 8, intublllll, but ability to protect aiiWIIy is pri'nr{ consideration!
't'
E'llll1181ian of ColllllaM htient
FW.Na
Noggin e.g. raccoon eyes and Battle's sign (bruising of the mastoid process) appears about 8 hours after trauma Neck C-11Pin1, 11111ropnic shock. nuchal rigidity Otorrhea, rhinorrhea, tongue biting, odour on bnlatl1. hematympanum Na1dlls Inspect lor track marb Neurological Concentrate on GCS. respiration, posture, 11111V1111111t. pupils, rwfl-
ENT
It'
Uninnal Antldatea
DDNT Dextrose
Oxv!lln
Naloxone 2 mg Thiamine 100 mg
ER22 Emergency Medicine
Approach to Common ER Preaentations
Toronto Notes 2011
essential to re-examine frequently - status can change rapidly diagnosis may become apparent only with the passage of time delayed deficit after head trauma suggestive of epidural hematoma (characteristic "lucid interval")
Tabla 11. 1Dxic - Mllblbolic Caus Df Fixad Pupils
Dlatlld
AnOllia
Anticholimrgic aganls (e.g. atropine, TCAsl
Dillllld 1D Normal
Hypothermia Barbiturates
Antipsychotics
Dlolinergic Bgllllts (e.g. organophosliJIIIBsl OpilllliS (e.g. hanlin), except nneparidine
Methanol (llRI
Cocaine Opioid � � � � � � � � � Anllhebmines Halklcinogens
Disposition
readily reversible alteration ofWC: discharge if adequate follow-up care available ongoing decreased WC: admit to service based on tentative diagnosis transfer patient if appropriate level of care not available
Chest Pain
� �
Rule Out Life-Threatening Causes
Uh
Th111rma c:auq Gf Chid Pllin
PET MAP
Pulm01111ry embolism
CVS: acute coronary syndrome/acute MI, pericarditis/cardiac tamponade, aortic dissection respiratory: pulmonary embolism (PE)/pneumothorax (tension or spontaneous) GI: esophageal rupture/pneumomediastinum
Elophageall14l!Ln Tamponade
Additional DHferential Diagnosis
cardiac: stable angina respiratory: pneumonia GI: peptic ulcer disease (PUD), pancreatitis, cholecystitis, esophagitis, reflux, esophageal spasm MSK: rib fractures, costochondritis, zoster, etc. psychogenic/anxiety (diagnosis of exclusion)
MVangina Aortic diuection PnlllmllhDriiX
Initial Resuscitation and Management 0 2 , IV; cardiac monitoring. CXR (portable if unstable), ECG History
Signs 1nd Symptoms llf Ml
PUlSE l'lrliltent chut pain
Upset stomach
ljghlheadldn111 Shortness of brellh
Ela:M$iv8 $W$11ing
..... ,
must evaluate cardiac risk factors (DM, HTN, hyperlipidemia, smoking, family history) classic presentations (but presentation seldom classic) aortic dissection: syncope with sudden severe tearing pain, often radiating to back, focal pain/neuologic loss in extremities secondary to major vessel ischemia pulmonary embolism: pleuritic chest pain {75%), dyspnea, anxiety, tachycardia, PERC SCORE pericarditis: anterior precordial pain, pleuritic, relieved by sitting up and leaning forward acute coronary syndrome (ACS): retrosternal squeezing/pressure pain, radiation to arm/ neck, dyspnea, nausea/vomiting. syncope esophageal: frequent heartburn, acid reflux, dysphagia, relief with antacids ACS more likely to be atypical in females, diabetics, and >80 years
� � � � � � � � � � � � � � � � � � � �
Physical Examination
vitals (BP in both arms, but unreliable indicator of dissection) palpate chest wall for tender points, but be aware that 25% of patients with acute MI have chest wall tenderness consider a diagnosis of MSK disease only if more serious causes excluded and palpation fully reproduces pain and symptoms cardiac exam, respiratory exam. peripheral vascular exam
PERC IICIIfl fur PE Age >50 yam HR >100 bpm Dtsllt on RA <94% Prior hiiiDry DIITJPE Recent 1rlluma or surgery
Hemoptysis Exogenous estroqen
Clinical signs sugpsting Dill
Investigations
CBC, electrolytes serial cardiac enzymes normal CK-MB does NOT rule out MI troponin I more sensitive (but positive later than CK-MB; can have false positives in renal failure, must follow for 8 hrs post onset of symptoms) ECG (see Table 12) always compare with previous PE and acute MI may have normal ECG in up to 50% of cases consider 15-lead ECG if hypotensive or ifECG shows inferior MI or AV node involvement
Sco111 1for each question; a scare Ml m1111s palilnt hu < 1.6'1 chanc having I I'E and IVOid5 further investigation.
Toronto Notes 2011
CXR
Approach to CommonER Presentations
.....
Emergency Medicine ER23
always compare with previous PE (see DVT, ER34) 50% completely normal atelectasis, elevated hemidiaphragm, pleural effusion aortic dissection (see sidebar ER12 for features) change from previous CXR is the most accurate finding CXR is normal in 20% of thoracic dissections pneumothorax may need inspiration and expiration views ABGs - normal in 20% of patients with PE, therefore do not perform D-dimer, V/Q scan or helical cr, venous leg Doppler, if PE suspected (see sidebar for Wells' Score) negative D-dimer rules out PE in low probability patients patients with intermediate or high probability Wells' score require imaging
,
,
� �
� � � � � � � � � � � � � � � � � � �
Signs of PE on CXR
W...marll's sign: abrupt bparing of a vasal on chntfilm.
Hutpllln's hump: a Wlldga-shaped infillnl1e that abuts the pleun1.
.....
� �
� � � � � � � � � � � � � � � � � � �
W.O.' Sctn far PE
Disposition patients at risk of developing dysrhythmias should be admitted to a monitored bed consult cardiology for patients with ACS; obtain a cardiothoracic surgery consultation for patients with valwlar lesions by echocardiogram, esophageal rupture, or aortic dissection discharge is appropriate for patients with a low probability of life-threatening illness due to resolving symptoms and negative workup; instruct the patient to return ifthey develop SOB or increased chest pain Table 12. Common Ufe Threatening ECG Changes
Pathology
Dy!rtlylhmia a) Torsade de Poinl85 b) Ventricular tachycardia c) Ventricular ftult8r d) Ventricular fibrillation
HR >1DD Recant immobility or Sx Clilical signs of DVT AIIBmllta llx lass likalylhan PE
IMmoptysis Cancer Low probability = D-2 Intermediate probability = Z& High probability = > 6
Previ011s Hx of DVT/emboli
+ 1.5
+1.5 + 1.5 +3 +3
+1
+1
.....
,
�
� �
� � � � � � � � � � � � � � � � � � �
ECG Finllnp
Ventricular complaxss in L.pWard1liJinling 111d downward-pointing contiiiiUm (250-350 bpm) 6 or more consecutive premature ventricular beats (15G-250 bpm) Smooth silll WBVB pattam of similll' amplitude (25G-350 bpm) Enatic ECG tracing. no identifiable waves
lmporlllnt to laok far reciprocal cllqes in STEM I in order to differantiata from
pericarditis I diffuse elevations!.
lm...ct-. Trutmllll: of Ac:..-111
Conduction
a) 2nd degree heart block (Mobitz Type II) b) 3rd degree hell'! block c) Left buncle branch block
PR ilteMI slllble, some DRS's dropped
Total AV dissociation, but stable P.P and R.ft intervals Prolonged QRS complex (>0.12s) RSR' in V5 or V6 Monophasic I and V6 May see ST elevation � � � � � � � � � to inlelpn!l, new LBBB is considered STEMI equivalent ST oiiMIIion in leeds associated with injured area of heart and reciprocal lead changes (depression)
Tall TWllvas
BEMOAN
Bate-Blockade
EnoXllpllrin
Morphine
ASA
Oxygen
Nitroglycerin
--g_
a)STEMI Melilbolic a) Hyperblemia
b) Hypokalemia
PWBVB flattening QRS complex widening and flattening U Wllves appear Flattl!ned T waves
Gradual downward curve Ill ST At risk far AV blocks and ventricular iTilabilily
Digillli1 Toxicity Syn!Rm a) Brugada
b) Wellens
c) Long
ar Syndrome
ar
RBBB with ST elevation in Vl, V2 and V3 Susceptible to deacly allhythmias, includilg V. Fib. Marbd T waw irrwr&ion in V2 and V3 LBft anterior descanding coronary stllnosis ilteiwllanger than \.i of cardiac cycle Predisposed to ventricular arrhythmia
ACUTE MYOCARDIAL INFARCTION see Cardiology. C25
Management immediate stabilization oxygen 4Umin IV access cardiac monitors STATECG cardiac enzymes (CK, Troponins) ASA 162-325 mg chewed nitroglycerin 0.3 mg SL q5min x 3 (IV for CHF, H1N, unresolved pain) morphine 2-5 mg IV q5-30min if unresponsive to NTG metoprolol5 mg slow IV qSmin x 3 if no contraindication (beware in inferior wall AMI)
I!R24 Emergency Medicine
Approach to CommonER Preaentations
Toronto Notes 2011
low molecular weight heparin 1 mg/kg SC bid (30 mg IV STAT post TNK infusion) thrombolytics or primary percutaneous coronary intervention (PCI) agents include t-PA, r-PA, Streptokinase, and TNK evaluate indications and contraindications prior to use other - antiarrhythmics, cardioversion, defibrillation, transthoracic pacing, angioplasty cardiology consult
Epistaxis
see Otolar_ytl&Olo&.v. OT27 90% of nosebleeds stem from the anterior nasal septum (at Kiesselbach's plexus located in Little's area) can be life-threatening
Etiology
most commonly caused by trauma (digital, blunt, foreign bodies), but can also be caused by barometric changes, nasal dryness, chemicals (cocaine, Otrivin), or systemic disease (coagulopathies, hypertension, etc.)
Investigations
,, ,
� � � � � � � � � � � � � � � � � � � �
CBC, PT/PTT (if indicated) x-ray, CT as needed
Treatment
aim is to localize bleeding and achieve hemostasis first-aid: ABC's, lean forward, pinch soft part of nose for 20 minutes assess blood loss: vitals, IV normal saline, cross match 2 units packed RBC if significant determine site of bleeding: use topical anaesthetidvasoconstrictor to facilitate; use nasal speculum and good lighting attempt to control the bleeding first line: Otrivin or cocaine second line: cauterize with silver nitrate (one side of septum only!) ifthese fail, or if bleeding is posterior --+ nasal packing (must monitor for complications) ifpacking fails, consult ENT
Tlrombocytopenic palient8 - 1111 n11orbable packa to avoid risk of
re-blaeding CIW&ad by pulling out the
removable pack.
,, I
� � � � � � � � � � � � � � � � � � �
Compllcadons Df N ...l Packing Hypoxemia Toxic-shock syndroms Aspimion l'hlrynoeal fibrosi.tstanosis Alar/sepllll necrosis
Disposition
most patients can be discharged after ensuring vitals are stable, bleeding is controlled and patient has appropriate follow-up educate patients about prevention (e.g. humidifiers, saline spray, topical ointments, avoiding irritants, managing hypertension) admission may be required for severe cases
Headache
see also Neurolo&.v, N39
Note: up to 5% of pllient8 with
subarachnoid hamonhaga llava a nonnal CT scan; � � 1111pact SAH with a n1gsliw CT. perform a lumbar puncture.
Etiology o the COJDJDOD
common migraine (no aura)/classic migraine (involves aura) gradual onset, unilateral/bilateral, throbbing nausea/vomiting, photo/phonophobia treatment analgesics, neuroleptics, vasoactive meds tension/muscular headache never during sleep, gradual over 24 hours posterior/occipital increased with stressors treatment modify stressor, local measures, NSAIDs, tricyclic antidepressants
thedeadly
subarachnoid hemorrhage (SAH) (see Neurosurgery. NS17) sudden onset, increased with exertion "worst" headache, nausea and vomiting, meningeal signs diagnosis: CT, LP (5-1 0% of patients with SAH have negative initial CT) - sensitivity of CT decreases with time and is much less sensitive by 48-72 hr management: urgent neurosurgery consult increased ICP worst in morning, supine, or bending down physical exam: neurological deficits, cranial nerve palsies, papilledema diagnosis: CT scan management consult neurosurgery
DDx Sullarub11111d Hamoll'hage
Berry aneurysm
Arteriovenous malfonmltiorVAduh polycystic kidney disa1111 Trauma Stroke
BATS
Toronto Notes 2011
Approach to CommonER Presentations
Emergency Medicine ER25
meningitis (see Infectious Diseases. ID6) flu-like presentation initially (fever, nausea/vomiting, malaise), meningeal signs, purpuric
rash
altered level of consciousness and confusion perfonn CT to rule out increased ICP then do LP for diagnosis treatment: early empiric antibiotics (depending on age group), steroid therapy temporal arteritis (not immediately deadly but causes great morbidity) (see QphthalmolollY, OP38) unilateral scalp tenderness, jaw claudication, visual disturbances labs: elevated ESR temporal artery biopsy is gold standard for diagnosis treatment: high-dose steroids immediately ifTA suspected
M.nmgitk
Da ncrt delay IV antibialil:s fur LP.
Disposition admit if underlying diagnosis is critical or emergent, if there are abnormal neurological findings, if patient is elderly or immunocompromised (atypical presentation), or if pain is refractory to oral medications most patients can be discharged with appropriate analgesia and follow up with their family physician; instruct patients to return for fever, vomiting, neurologic changes, or increasing pain
Joint Pain
see Rbeumatoloi:Y
Rule Out Life-Threatening Causes septic joint (see Ortho.paedics. OR8) Differential Diagnosis articular pain monoarticular infectious: bacterial, viral, fungal hemarthrosis: trauma/fracture, anticoagulants, bleeding diatheses crystal induced: gout, CPPD, hydroxyapatite inflammatory: seropositive, seronegative neoplasm degenerative: osteoarthritis polyarticular infectious: Lyme disease, bacterial endocarditis, septicemia, gonococcus, viral post-infectious: rheumatic fever, reactive arthritis, enteric infections inflammatory: seropositive, seronegative degenerative: osteoarthritis non-articular musculoskeletal localized: tendonitis, bursitis, capsulitis, muscle sprain generalized: :fibromyalgia, PMR other neurologic: spinal stenosis/spondyl.olithesis, degenerative disc disease, cauda equina syndrome, neoplasm, thoracic outlet syndrome, Charcot joint vascular: intermittent claudication History and Physical Examination determine onset, course, location, character of the pain (OPQRST) and recurrence determine which joint or joints are involved associated symptoms: fever, constitutional symptoms, skin lesions, conjunctivitis, urethritis patterns ofjoint involvement: polyarticular vs. monoarticular, symmetric vs. asymmetric inflammatory symptoms: prolonged morning sillfness, sillfness and pain ease through the day, midday fatigue, soft tissue swelling non-inflammatory symptoms: sillfness short lived after inactivity, short duration stiffness in the morning, pain increases with activity assess ROM, presence of joint effusion, warmth watch for: localized joint pain, erythema, warmth, swelling with pain on active ROM, inability to bear weight, fever as these may indicate presence of septic joint Investigations x-ray, CBC, ESR, CRP, WBC, INR/PTT, blood cultures, urate joint aspirate � � send for: WBC, protein, glucose, Gram stain, crystals
It'
C.usn .r Joint l'llin
SOFTER TISSUE
Sepsis
Osmaarthrilil
Fraduras
Tendon/muscle Epiphyseal
R.fi!T'Id
� � � � � � �
Ischemia
arthritides Seronegative � � � � � � � � � � � Unrte
� � � � � � � � � � � �
Extr&-articular rflaumatism
{e.g. palymyalgia]
ER26 Emergency Medicine
Approach to CommonER Preaentations
Management
Toronto Notes 2011
septic joint: IV antibiotics joint decompression and drainage antibiotics can be started empirically if septic arthritis cannot be ruled out crystalline synovitis: NSAIDs at high dose, colchicine with in first 24 hours, corticosteroids do not use allopurinol, as it may worsen acute attack acute polyarthritis: NSAIDs, analgesics {acetaminophen opioids), corticosteroids local or systemic hospitalization is required in the presence of(l) significant, concomitant internal organ involvement; {2) signs of bacteremia, including vesiculopustular skin lesions, Roth spots, shaking chills, or splinter hemorrhages; (3) systemic vasculitis; (4) severe pain; (5) severe constitutional symptoms; (6) purulent synovial fluid in one or more joints; or (7) immunosuppression osteoarthritis: acutely: NSAIDs, acetaminophen soft tissue pain: allow healing with enforced rest immobilization nonpharmacologic treatment: local heat or cold, electrical stimulation, massage pharmacologic: oral analgesics, NSAIDs, muscle relaxants, corticosteroid injections, topical agents
Otalgia
Differential Diagnosis (see also
� � � � � � � � � � � � � � � � � � OT6) local infections: AOE, AOM, OM with effusion, mastoiditis, myringitis, malignant otitis in diabetics, herpes simplex/zoster, auricular cellulites, external canal abscess others: trauma, neoplasm, foreign body, cerumen impactions, Wegener's determine onset, course, location and character of pain otorrhea, aural fullness, hearing loss, pruritis Q-tip use, hearing aids, headphones associated symptoms: fever observe for otorrhea, palpation ofouter ear, otoscope to see bulging erythematous TM, perforation
Investigations
consider audiogram ifhearing loss
Management
debridement and antibiotics for cerumen and infection
Seizures
see Neurology. N8
Definition
paroxysmal alteration of behaviour and/or EEG changes resulting from abnormal, excessive activity of neurons
Categories
generalized seizure (consciousness always lost): tonic/clonic, absence, myoclonic, atonic partial seizure (focal): simple partial, complex partial causes: trauma, intracranial hemorrhage, structural abnormality, infection, toxins/ drugs, metabolic disturbance (hypo/hyperglycemia, hypo!hypernatremia, hypocalcemia, hypomagnesemia); primary seizure disorder differential diagnosis: syncope, pseudoseizures, migraines, movement disorder, narcolepsy/ cataplexy, myoclonus
History
from patient and bystander: flaccid and unconscious, often with deep rapid breathing preceding aura, rapid onset, loss of bladder/bowel control, tongue-biting (sides of the tongue)
Physical Examination
...._,,
CBC 1111d diff 8ectrolytes including Ca. Mg. P0 4
injuries to head and spine and bony prominences (e.g. elbows), tongue laceration, aspiration, urinary incontinence
Investigations
� � � � � � � � � � � � � � � � � � Min. Wollwp In In Adull wdll Ill Timl SlizuN
Head CT
known seizure disorder: anticonvulsant levels Accu-Chek first time seizure: CBC, serum glucose, electrolytes, BUN, creatinine, Ca, Mg; consider prolactin, fi-hCG, tox screen initial: CT; x-ray if suspected extremity injuries. Definitive: MRI, EEG
Toronto Notes 2011
Table 13. Management of Status Epilepticus
Approach to CommonER Presentations
Emergency Medicine ER27
Time (mil
6-5
Slips
Give axygen; ensure ade!J.Ia'le ventilation Monilllr. vital signs, � � � � � � � � � � � � � � � � � � � � oximetry Establish IV access; obtai! blood samples for glucose level, CBC, electrolybls, toxins, and anticonwlsllnt IMis Giva 50 ml 50% glucose (preceded by thiamine 100 mg IM in adultsl
fi.9
111-ZD
IV lorazepam 0.1 ITigllqj at 2 mg{min or IV diazepam 0.2 � � � at 5mg{min Diazepam can be repeated if seizures do not stop after 5 min; if diazepam is used to stop the status, then r,ilenyloil should be administered pr0f11llly to prevent the � � � � � � � of status
.....
,,
� � � � � � � � � � � � � � � � � � �
2110
>60
If status persists, administer 15-20 � 1mw1qj/min in clildren
�
� of � � � � � � � � �
intravenously no faster than 50 m!Vmin in adults and
� � � �
If adminiQring phenytoin, patient must be on a cardiac monitor as anhytluniu
and/or hyputB!IIion 11111y occ:ur.
If status does not stop after � � � � � of phanytoil, giva additional doses of 5 mg/kg to a maxinal dose of � � If status pnisls, then giva 20 mlrkg of � � � � � � � � � � � � � � � at 100 mjfmin When � � � � � � � � � � � � � is given after a
benzodiiiZEpine, ventilatory assistance is usually required
If status persists, then give general anaesthesia (e.g., pentobarbilllll. Vasopressors or fluid volume are usually necessary. Electroencephalogram should be manitorad. Neuromuscular blockade may be needed.
Adllptad form: Ctd'sEs:!erltirlsDf.&fe*ite, 7tfuditian, Tabla 12H Used with panrillion.
Disposition
the decision to admit or discharge should be based on the underlying disease process identified if a patient has returned to baseline function and is neurologically intact, then consider discharge with outpatient follow-up first-time seizure patients being discharged should be referred to a neurologist for follow-up admitted patients should generally have a neurology consult patient should not drive until medically cleared (local regulations vary) complete notification form to appropriate authority re: ability to drive warn regarding other safety concerns (e.g. no swimming, bathing children alone, etc.)
Shortness of Breath
see Re$pirolQgy and CardiQlQgy
.....
,,
Etiology
categorized into one oftwo groups: respiratory or cardiovascular respiratory system dyspnea: discomfort related to disorders of the central controller (brain), the ventilatory pump (ventilatory muscles, peripheral nerves), and the gas exchanger (alveoli and pulmonary capillaries) cardiovascular system dyspnea: cardiac diseases (acute ischemia, heart failure, systolic dysfunction, valvular disorders, pericardial diseases), anemia, and deconditioning
� � � � � � � � � � � � � � � � � �
C.n of Acute DIYJIMI
Cllnliovncular: acul& Ml, CHF, cardiac
tamponade.
Rairatory: bronchospaiiTI, pulm01111ry
embolism, pnlllrllOthorax. infection (bronchitis, pneumonia), upper airway
obstruction (upimion, 11111phylaxis).
History/Physical
acute SOB is often due to a relatively limited number of conditions. Associated symptoms and signs are key to the appropriate diagnosis substernal chest pain with cardiac ischemia fever, cough and sputum with respiratory infections urticaria with anaphylaxis wheezing with acute bronchospasm dyspnea may be the sole complaint and the physical examination may reveal few abnormalities (e.g. pulmonary embolism, pneumothorax) chest tightness may be indicative of bronchospasm a sensation of rapid, shallow breathing may correspond to interstitial disease a sense of heavy breathing is typical of deconditioning vitals including pulse oximetry wheeze (airway) vs. crackles (parenchymal), JVP, and murmurs
.....
,,
� � �
Collll'lindiclllilln ta 1011% DXJtllln C01 rvt111inn (1.g. COPD).
Investigations
CBC + differential (hematocrit to exclude anemia), electrolytes, consider ABG CXR (hyperinflation and bullous disease suggestive of obstructive lung disease, or changes in interstitial markings consistent with inflammation, infection or interstitial fluid) serial cardiac enzymes and ECG if considering cardiac source CT chest usually is not indicated in the initial evaluation of patients with dyspnea, but can be valuable in patients with interstitial lung disease, occult emphysema, or chronic thromboembolic disease (PE) the history and physical examination lead to accurate diagnoses in patients with dyspnea in approximately two- thirds of cases; the decision to admit or discharge should be based on the underlying disease process identified consideration for intubation should be early in C02 retainers (e.g. COPD) if the decision to discharge is chosen, provide appropriate discharge instructions to return in case of returning/worsening SOB
Disposition
ER28 Emergency Medicine
Approach to CommonER Preaentations
Toronto Notes 2011
..... ,
Syncope
------------------------------------------------------
9t-----------------, Definition
sudden, transient loss of consciousness and postural tone with spontaneous recovery usually caused by generalized cerebral or reticular activating system hypoperfusion
S Types If Syncap1 1. Vasomotor 2. Canliac 3.CNS 4. Metabolic 5. Psychogenic
Etiology cardiogenic: arrhythmia, outflow obstruction (e.g. PE, tamponade, tension pneumothorax, pulmonary liTN), MI, valvular disease non-cardiogenic: peripheral vascular (hypovolemia), vaso-vagal, cerebrovascular disorders, CNS, metabolic disturbances (e.g. EtCH intoxication) History gather details from witnesses, and clarify patient's experience (e.g. dizziness, ataxia, or true syncope) distinguish between syncope and seizure (see � � � � � � � � � N9} some patients may have myoclonic jerks with syncope - NOT a seizure signs and symptoms during presyncope, syncope and postsyncope past medical history. drugs think anatomically in differential; pump (heart}, blood (quality}, vessels, brain sudden loss of consciousness with no warning or prodrome is cardiogenic until proven otherwise Physical Examination postural BP and HR cardiovascular, respiratory and neuro exam physical findings in the elderly patient who falls (I HATE FALIJNG): Inflammation of joints (or joint deformity) Hypotension (orthostatic blood pressure changes) Auditory and visual abnormalities Tremor (Parkinsoris disease or other causes of tremor) Equilibrium (balance) problem Foot problems Arrhythmia, heart block or valvular disease Leg-length discrepancy Lack of conditioning (generalized weakness) Illness Nutrition (poor; weight loss) Gait disturbance Investigations ECG (tachycardia, bradycardia, blocks, WPW, long QT interval), bedside glucose as indicated: CBC, electrolytes, BUN, creatinine, ABGs, Troponin, Ca, Mg. � � � � � consider drug screen
�
c - ot Syncope by 5ys1am
HEAD, HEART. VeSSElS
ICl
Hypoxii/Hypoglycamia
Epilapry
Anxiety Dysfunctional brainstem
lllllrt attack
Embolism (PE] Aortic obstruction lhylhm disturbance
Tachycardia
Vasovagal
Situational
Subclavian stall
ENT (glossophllryngelll nallflllgia] low systemic VUCUIIII" nllli51mlca
Sensitive carotid sioos
..... ,
� � � �
Management ABCs, IV, <l:2. monitor examine for signs of trauma caused by syncopal episode cardiogenic syncope: admit to medicine/cardiology non-cardiogenk syncope: discharge with follow-up as indicated by cause Disposition decision to admit is based on etiology most patients will he discharged on discharge, instruct patient to follow up with family physician educate re: avoiding orthostatic or situational syncope patients with recurrent syncope should avoid high-risk activities (e.g. driving)
Which 1'811111111 wllh Syncope should be AllmittR? ThO&B 11 risk of complicaliona: Older thin 60-70 years
Significant cardiac risk factors Racurrant syncopa Sarious undlllying il.,eu
Sexual Assault
..... ,
� � � � � � � � � � � � � � � � � � � �
Lagally raquirad to rapart sexual � � � � � � � if victim is < 16 years of age to Children's Aid Sociaty (CAS].
Epidemiology 1 in 4 women and 1 in 10 men will be sexually assaulted in their lifetime it is estimated that only 796 of rapes are reported General Approach ABCs, treat acute, serious injuries ensure patient is not left alone and provide ongoing emotional support set aside adequate time for exam (usually 1.5 hours)
Toronto Notes 2011
Approach to CommonER Presentations
Emergency Medicine ER29
obtain consent for medical exam and treatment, collection of evidence, disclosure to police (notify police as soon as consent obtained) Sexual Assault Kit (document injuries, collect evidence) if <72 hrs since assault label samples immediately and pass directly to police offer community crisis resources (e.g. shelter, hotline) do not report unless victim requests (legally required if <16 years old)
History ensure privacy for the patient - others should be asked to leave questions to ask: who? how many? when? where did penetration occur? what happened?
any weapons or physical assault? post-assault activities (urination, defecation, change of clothes, shower, douche, etc.) gynecologic history gravity, parity, last menstrual period contraception use last voluntary intercourse (sperm motile 6-12 hours in vagina, 5 days in cervix) medical history - acute injury/illness, chronic diseases, psychiatric history, medications, allergies, etc.
Physical Examination
evidence collection is always secondary to treatment of serious injuries never re-traumatize a patient with the examination general examination mental status sexual maturity patient should remove clothes and place in paper bag document abrasions, bruises, lacerations, tom frenulum/broken teeth (indicates oral penetration) pelvic exam and specimen collection ideally before urination or defecation examine for seminal stains, hymen, signs of trauma collect moistened swabs of dried seminal stains pubic hair combings and cuttings speculum exam lubricate with water only vaginal lacerations, foreign bodies Pap smear oral/cervical/rectal culture for gonorrhea and chlamydia posterior fornix secretions ifpresent or aspiration of saline irrigation immediate wet smear for motile sperm air-dried slides for immotile sperm, acid phosphatase, ABO group others fingernail scrapings saliva sample from victim
Investigations
VDRL -repeat in 3 months if negative
serum � � � � � � blood for ABO group, Rh type, baseline serology (e.g. hepatitis, HIV)
',.,
� � � � � � � � � � � � � � � � � � � �
After Suual AluuH Gonorrhea: 6-1 � �
Chlamydia: 4-17%
m.t 11f Suultlly TranMIIIW lhu
Management
involve local/regional sexual assault team medical suture lacerations tetanus prophylaxis gynecology consult for foreign body, complex lacerations assumed positive for gonorrhea and chlamydia management: azithromycin 1 gPO x 1 dose (alt: doxycycline 100 mg PO bid x 7 days) and cefixime 400 mg PO x 1 dose may start prophylaxis for hepatitis B and HIV pre and post counselling for lllV testing pregnancy prophylaxis offered levonorgestrel 0.75 mg PO STAT, repeat within 12 hours (Plan B) psychological high incidence of psychological sequelae have victim change and shower after exam completed
Syphilis: 0.5.J'J(,
HIV:<1'1(,
Disposition discharge if injuries/social situation permit
follow-up with MD in rape crisis centre within 24 hours best ifpatient does not leave ED alone
ER30 Emergency Medicine
Approach to CommonER Presentationa/Medical Emergencies
Toronto Notes 2011
..... ,
...-----------------,
Haw do you g.t p.ti...t who Is Ki:OIIIJianilld lly ...,. pllrlner . . _ witho.t lrDUiing lutpician?
Order 11'1 x-ray.
DOMESTIC VIOLENCE women are usually the victims, but male victimization also occurs identify the problem (need high index of suspicion) suggestive injuries (bruises, sprains, abrasions, occasionally fractures, burns or other injuries; often do not match up with history provided) somatic symptoms (chronic and vague complaints) psychosocial symptoms clinician impression {your 'gut feeling, e.g. overbearing partner that won't leave patient's side) if disclosed, be supportive and assess danger order an x-rayto secretly get patient alone to question re: abuse patient must consent to follow-up investigation/reporting (unless for children)
Management
treat injuries
ask about sexual assault and children at home
document findings safety plan follow-up: family doctor/social worker
Medical Emergencies
..... ,
Anaphylaxis and Allergic Reactions
Etiology
exaggerated immune response classically IgE mediated, sensitization then re-exposure anaphylaxis: a severe hypersensitivity reaction affecting at least two organ systems (e.g. GI, derm,resp) urticaria: a hypersensitivity reaction causing an itchy skin eruption angioedema: swelling that occurs in the tissue just below the surface of the skin, most often around the lips and eyes anaphylactoid reaction: non-IgE mediated, may occur with first exposure {e.g. radio contrast dyes); presentation and treatment same as for anaphylaxis
"-.phyluis l'e!liciUin Stings
Most c - Trigg.,. hlr
� � � � � � � � � � � � � � � � � � �
Nuts Shellfi$11
History and Physical Examination
general- marked anxiety, apprehension, tremor, cold sensation skin - generalized urticaria, edema, erythema, pruritus GI - abdominal pain, nausea, vomiting, diarrhea (most allergens are ingested, therefore GI symptoms common) respiratory- nasal congestion, sneezing, coryza, cough. hoarseness, sensation of throat tightness, dyspnea, stridor, wheeze eyes - itch, tearing, conjunctival injection cardiovascular - hypotension, tachycardia, weakness, dizziness, syncope, chest pain, arrhythmia, MI
..... , ...-----------------,
Trallnllnt
Airwlly contral Epinljlmrlll Establish IV 1nd give fluids Steroids Anti-llistamines
Management
remove causative agent; secure ABCs epinephrine on scene- epi-pen {injectable epinephrine) if available moderate signs and symptoms (minimal airway edema, mild bronchospasm, cutaneous reactions) adult: 0.3-0.5 mL of 1:1000 solution 1M epinephrine child: 0_01 mUkg/dose up to OA miJdose 1:1000 epinephrine severe signs and symptoms (laryngeal edema, severe bronchospasm and shock, severe hypotension) epinephrine via IV or ETT starting at 1 rnl ofl:10,000 (0.1 mg) in adults; 0.01 miJkg in children cardiac monitoring, ECG diphenhydramine (Benadryl) 50 mg IM or IV q4-6h methylprednisolone 50-100 mg IV {dose depending on severity) salbutamol (VentoJin) via nebulizer if bronchospasm glucagon (for those on !}-blockers with resistant hypotension and/or cardiac disease) 5-15 � � � � qlminiV
Disposition
monitor for 4-6 hours in ED (minimum) and arrange: follow up with family physician in 24-48hours can have second phase (rebound) reaction up to 48 hours later, patient may need to be supervised 3-day course of. H 1 antagonist (cetirizine 10 mg PO od) H 2 antagonist (ranitidine 150 mg PO od) corticosteroid (prednisone 50 mg PO od)
Toronto Notes 2011
Medical Emergencies
Emergency Medicine ER31
Asthma
see Res.pirology, R7 chronic inflammatory airway disease with episodes of bronchospasm and inflammation resulting in reversible airflow obstruction
', ,
� �
� � � � � � � � � � � � � � � � � �
Investigations 0 2 sat
pealdlow meter ABG (only in life threatening exacerbations) CXR if diagnosis in doubt or concerns of pneumonia. pneumothorax, etc.
Beware of tna silent asthmaticI This is a medical ernervency and may require
11111111111111C'f intubelion.
',,
�
Tabla 14. Asthma Assessment and Management
Classifications tistory and Pllysical Exallination
� � � � � � � �
Mlnagemant
1011% Oz, cardiac monitor, IV access o Intubate (consider pr&-induclion with ketamine) � � � � � � � � � � � � � � � � puffs OR nebuliz:sr 5 mg continually Anticholilergics: MDI � � puffs q20 minx 3 OR nebulizer 0.5 mg q20 minx 3 IV steroids: methylprednisolone 125 mg, hydrocortisone 500 mg
o
5 &MIIIw Elemenlll tm Hi.tory C111111 of 8XIIclllbation Previous EIVICU visib
llllpimary Amlt Exhausll!d, confused, diaphoretic, �
lmmilant
Silent chest, ineflective respiratory effort
DBCI8il&edHR � � sat <90% despite supplemeniBI � �
Previous intubations Tming af I'ICIITI st1roid UN Frequency of artllma medication usa
Severe Asthma
Agitated, diaph01'81ic, laboLI'IId respirations Difficulty speaking in lull santences No relief from � � � � � � � � � � � sat <90%, FEV1 <511% Nocturnal symptoms Inadequate raliul from jl-agonist FEV1 50-80'lo
Anticipall need for intubation Similar to above menagement (jl-agonist may be less frequent; q15-20 min) o Magnesilm sLJphate 2g IV
o
o
Tre.tmlnt of Asthm
ASTHMA
� � � � � � � � � � � � � � �
(beta-agonim)
STeroids
Modandl Allhma SOB at rest, cough, congestion, chest tiltltness
Oz to achieve Oz-sat >90% o � � � � � � � � � puffer of neb q1h St.oid&: pradni50ne 4()..60 mg PO Anticholilergics (Atrovent)
o
Hydration Muk!02)
� � � � � � � � � � � � � �
concurrent infection)
Mild Asthma
Exertional SOI!Icough � � � � some nocturnal
symptoms
Good response to � � � � � � � � FEV1 >80%
� � � � � � � � Monitor FEV1 Consider steroids (nebLJized or PO)
Disposition
P-agonist MDI regular use (2-4 puffs q2-4h) until symptoms controlled then pm prednisone 30-60 mg/dayfor 7-14 days with no taper inhaled steroid follow-up with primary care physician
Cardiac Dysrhythmias
see Cardiology. Cl2
Bradyarrhythmlas and AV Conduction Blocks
AV conduction blocks 1ot degree - prolonged PR interval (>200 msec), no treatment required 2nd degree Mobitz I - gradual prolongation of PR then dropped QRS, usually benign Mobitz II - PR constant with dropped QRS, can progress to 3rd degree AV block 3rd degree - P unrelated to QRS, PP and RR intervals constant atropine and transcutaneous pacemaker (TCP) ifTCP fails consider dopamine, � � � � � � � � � � � IV long term treatment for Mobitz n and 3 degree block - internal pacemaker sinus bradycardia (rate <60 bpm) can be normal (especially in athletes) causes: vagal stimulation, vomiting, myocardial infarction/ischemia, increased ICP, sick sinus node, hypothyroidism, drugs (e.g. P-blockers, CCBs) treat if symptomatic (hypotension, chest pain) acute: atropine transcutaneous pacing sick sinus: transcutaneous pacing drug induced: discontinue/reduce offending drug
',, .
� � � � � � � � � � � � � � � � � �
Atropine is unlikaly to wor1c. in 3nl dlgrM hllllt block.
ER32 Emergency Medicine
Medical Emergencies
Toronto Notes 2011
......
t-----------------,
If 1111 patiant �
� � � tachyanhythmia is unmble, perform immediabl
canliovmion.
......
, ...-----------------,
Clini:lll Flllllmla Df lnltUility Hypotension (.SP <90) CHF or pulmonary edema Clmt pain Altered LOC (may indiuta lhock)
......
If patient hu Wollf-ParkinsonWhite and is in Afib usa lllliodarona or procainamide. Avoid AV nodal blockinq agent5 {adenosine, digoxin, diltiazam, � � � � � � � � � � u 1his can inci'IISII conduction through bypan bact.
.,
Supraventricular Tachyarrhythmias (narrow QRS) sinus tachycardia (rate >100 bpm) causes: increased sympathetic tone, drugs, fever, hypotension, anemia, thyrotoxicosis, MI, PE, emotional, pain, etc. treat underlying cause, consider � � � � � � � � � � if symptomatic regular rhythm vagal maneuvres (carotid massage, Valsava), adenosine 6 mg IV push, if no conversion give 12 mg, can repeat 12 mg dose once rhythm converts: probable re-entry tachycardia monitor for recurrence treat recurrence with adenosine or longer acting medications rhythm does not convert: atrial flutter, ectopic atrial tachycardia, junctional tachycardia rate control (diltiazem, � � � � � � � � � � � � and consult cardiology irregular rhythm probable atrial fibrillation, atrial flutter or multifocal atrial tachycardia rate control (diltiazem, � � � � � � � � � � � � Atrial Fibrillation most common sustained arrhythmia; no organized P waves, irregularly irregular heart rate, narrow QRS (typically) etiology: HTN, CAD, thyrotoxicosis, EtOH (holiday heart), valvular disease, pericarditis, cardiomyopathy, Sick Sinus Syndrome treatment principles: stroke prevention, treat symptoms, identify/treat underlying cause decreases cardiac output by 20-30% (due to loss of organized atrial contractions) acute management if onset of AFib is >24-48 hrs: anticoagulate 3 wks prior to and 4 wks after cardioversion or do transesophageal echo to rule out clot if symptomatic or first presentation - cardiovert electrical cardioversion: synchronized DC cardioversion chemical cardioversion: amiodarone, procainamide, flecainide, propafenone (if decreased LV function use amiodarone) long term management: rate or rhythm control, consider anticoagulation (CHADS2) Ventricular Tachyarrhythmias (wide QRS) ventricular tachycardia (VT) (rate usually 140-200 bpm) definition: 3 or more consecutive ventricular beats at >100 bpm etiology: CAD with MI is most common cause treatment: sustained VT (>30 seconds) is an emergency hemodynamic compromise: DC cardioversion no hemodynamic compromise: DC cardioversion, lidocaine, amiodarone, procainamide ventricular fibrillation - call a code blue, follow ACLS for pulseless arrest torsades de pointes looks like VT but QRS 'rotates around baseline' with changing axis and amplitude (twisted ribbon) etiology: prolonged QT due to drugs (e.g. quinidine, TCAs, erythromycin, quinolones), electrolyte imbalance (hypokalemia, hypomagnesemia), congenital treatment: IV Mg. temporary overdrive pacing, isoproterenol correct cause of prolonged QT discontinue cardioversion if hemodynamic compromise
.----------------.
...... ._________________
Usa 1ha CHADS2 score from Tabla 3,
� � � � �
.,
.....
Nlell til Rule Out willl COPD
Eacelbalion
, ..----------------.
Chronic Obstructive Pulmonary Disease (COPD)
progressive development of irreversible airway obstruction, typically caused by smoking acute exacerbation: episode of increased dyspnea, coughing, increase in sputum volume or purulence
� � � � � � � � � �
Pneumothorax
CHF axacarbation
AcuteMI l'nelrnonia and oilier infectious CBU88S
Pulmonary embolus
History and Physical Examination worsening dyspnea or tachypnea acute change in frequency, quantity and colour of sputum production trigger: pneumonia, urinary tract infection, PE, CHF, Ml, drugs Investigations CBC, electrolytes, ABG, CXR, ECG, PFTs Management keep 0 2 sat 88-92% (beware of C02 retainers, but do not withhold Oz if hypoxic) ipratriopium is bronchodilator of choice, add salbutamol steroids: prednisone 40 mg PO (tapered over 3 weeks) antibiotics: TMP-SMX, cephalosporins, respiratory quinolones (if signs of infection) ICU admission iflife-threatening with ventilation (chance of ventilation dependency) lower threshold to admit if co-morbid illness
Toronto Notes 2011
Medical Emergencies
Emergency Medicine ER33
Disposition can use up to 4-6 puffs qid ofipratropium and salbutamol for exacerbations continue antibiotics if started and give tapering steroids
Congestive Heart Failure
also see Cardiology, C32
Etiology decreased myocardial contractility: ischemia, infarction. cardiomyopathy, myocarditis pressure overload states: hypertension. valve abnormalities, congenital heart disease restricted cardiac output: myocardial infiltrative disease, cardiac tamponade volume overload Causes of Exacerbation or Precipitants cardiac: acute myocardial infarction or ischemia, cardiac tachyarrhytlunias (e.g. atrial fibrillation), uncontrolled hypertension medications: non-compliance with or change in cardiac medications, NSAIDS, steroids dietary: increased sodium intake increased cardiac output demand: infection, anemia, hyperthyroidism, pregnancy other: pulmonary embolus, physical overcxc:rtion, renal failure History/Presentation left-sided heart failure dyspnea, decreased exercise tolerance, paroxysmal nocturnal dyspnea, orthopnea, nocturia, fatigue, possibly altered mental status, syncope, systemic hypotension in severe cases pulmonary edema: severe respiratory distress, pink frothy or white sputum, rales, S3 or S4 right-sided heart failure dependent edema, jugular venous elevation, hepatic enlargement, ascites patients often present with a combination of right-sided and left-sided symptoms Physical Examination vitals: tachypnea, tachycardia, hypo- or hypertension, hypoxia respiratory: crackles (acute), wheeze (chronic) cardiac: laterally displaced apex, S3 or S4, jugular venous distention, hepato-jugular reflex abdominal: hepatomegaly, ascites peripheral vascular: peripheral or sacral edema, weak peripheral pulses, pulsus altemans (alternating weak and strong pulse), cool extremities Investigations labs: CBC, electrolytes, AST, ALT, bilirubin, creatinine, BUN, cardiac enzymes, BNP (brain natriuretic peptide) chest X-ray (see side bar) ECG: look for Ml, ischemia in CHF: LVH, atrial enlargement conduction abnormalities ABG: if severe or refractory to treatment hypoxemia, hypercapnia and acidosis are signs of severe CHF echocardiogram: not usually used in emergency evaluation, previous results may aid in diagnosis may be precipitated by arrhythmia (e.g. sudden onset AFib) - correct if new Management (acute) ABC, may require intubation if severe hypoxia sit upright, cardiac monitoring and continuous pulse oximetry saline lock IV; Foley catheter (to follow effectiveness of diuresis) 100% � � � � mask if poor response may require CPAP, BiPAP, or intubation
It'
Cau111 of CHF Exacerbmon
FAIWRE
Forvot medication AnhytllrnWAnamill lsch1111illl'lnfarcti onllnflction � � � � � � � � (e.g. too much all) Upregulation of cardiac output
(p1111J111ncy, hyperthyroidism)
1111111 fllilunl Embolilm (pulmonary)
.....
,,
� � � � � � � � � � � � � � � � � � �
Hotpitll Mlnagement lequir.d if:
Acute Ml Pulmo111.ry edema or severe
respiratory distress Sevn complicating medical illnass (a.v. pnaumonia) Anasarca Symptomatic hypo1ension or syncope Raflactory to oUipltiant therapy Thromboerilolic compliclllions requiring interventions Clinically significant arrhythmias Inadequate social support for safe
outpatient m8111.Q8ment
l'lniltent hypoxia requimg IUJiplllllllllllll oxygm
.....
'_._ , ______________
� �
CHF an CXR Pulmonary Vllscular rvdistribution Perihilar inliltnnn lntamitilll edema, Karley B lin1111 AIVIIOiar edema, bilateral infillrltas May see cardiomegaly, pleural effusions
It' Aculll Traltnlllnt af CHF
LMNOP
Llsix (furos1111ide) Morphine
drugs
nitro 0.3 mg SL q5min PRN topical nitro patch (0.2-0.8 mg/hr) if not responding or ischemia: 10-200 f!g/min IV; titrate diuretic if volume overloaded (e.g. furosemide 40-80 mg IV) morphine l-2mg1Vpm ifhypotensive: dobutamine (2.51Jg!kg/min IV) or dopamine (5-10 f!glkg/min IV), titrate up to sBP 90-100 ASA 160 mg chew and swallow treat precipitating factor cardiology or medicine consult
Nitroglycerine
Oxygen
Position (sit upright)
ER34 Emergency Medicine
Medical Emergencies
Toronto Notes 2011
DVT and Pulmonary Embolism
It'
Biak hctun for VTE
----------------------
see also �
� � � � � � � � � � R18
THROMBOSIS Trauma, travel
� � � � � � � � � � � � � � � � � �
HRT
B1crwtional drugs (IVDUI Old (age >601
Maignancy Birth control piU Oblsily, obmlrics Surgery, smoking Immobilization Sickness (CHF. MI. nephrotic syndmme, Vlllculilis)
Risk Factors Vircltow's triad alterations in blood flow (venous stasis) injury to endothelium hypercoagulable state (including pregnancy, use of OCP, malignancy) most significant risk factors (see side bar for complete list) major surgery or trauma or prolonged hospitalization permanent immobilization and age malignancy, other hypercoagulable state prior venous thromboembolism History/Presentation DVT: calf pain. leg swelling/erythema/edema, palpable cord on exam; can be asymptomatic PE: dyspnea. pleuritic chest pain, tachypnea, hemoptysis, cyanosis, hypoxia, fever presence of risk factors and family history ofvenous thromboembolic disease clinical signs/symptoms are unreliable for diagnosis and exclusion ofDVT/PE; investigation often needed (see Figures 12 and Figure 13} calculate the PERC score to assess the need for PE work-up before assessing the likelihood of a PE (Well's criteria} Investigations (Figures 12-14) ECG and CXR are useful to look for other causes (e.g. ACS, pneumonia) D-dimer is only useful ifit is negative in low risk patients Ultrasound has high sensitivity and specificity for proximal clot but only 73% sensitivity for DVT below the knee CT angiography has high sensitivity and specificity for PE, may also suggest other etiology V/Q scan useful when CT angio not available, or patient unable to tolerate IV contrast (e.g. renal failure, allergy) Management of DVT/PE LMWH unless patient also has renal failure dalteparin 200 IU/kg SC q24h or enoxaparin 1.5 mg/kg SC q24h warfarin started at same time as LMWH (5 mg PO daily initially) LMWH discontinued when INRhas been therapeutic (2-3} for 2 consecutive days early ambulation with analgesia is safe if appropriately anticoagulated IVC filter or surgical thrombectomy considered if anticoagulation is contraindicated consider thrombolysis if extensive DVT or PE causing hemodynamic compromise often can be treated as outpatient, may require analgesia for chest pain (narcotic or NSAID) admit if hemodynamically unstable, require supplemental O:z, major comorbidities, lack of sufficient social supports, unable to ambulate, need invasive therapy long term anticoagulation ifreversible risk factor: 3-6 months ofwarfarin idiopathic VTE: may need longer term warfarin (5 yrs or more)
SuspiiCted (symptomatic) acute DVT
... ', ,._________________
PERC ICO,. for PE AQe >50 y&II'S
HR >100bpm 02 ut on RA <94% Prior history DVT/PE Recent trauma or surq&r( Hemoptysis
Clinical signs suggesting DVT Score 1 for each qullllion; ascon QIB m1111ns patient has < 1.6% chence
Exog-us estrogen
havilg aPE and avoids further investigation.
.._,, ,._________________
Weill Sllora for PE Previous Hx of DVT/emboli
+1.5
+1.5 +1.5 Clinical signs of DVT +3 Alternate Dx less likely than PE +3 Hemoptysis +1 Cancer +1
Recent immobility or Sx
HR >100
Low probability = G-2 lntarmedilta probability = � High probability = >6
� �
.._,,
� � � � � � � � � � � � � � � � � � �
511'!(; of patients with symptomatic proximal DVT will develop PE, ofUn within da'(IID wsek& of the IMIIIl
Compression U/S
Normal
DVTpresant
Tralllment
Figure 12. Approach to Suspected DVT
DVTabsant DVT present
Repeat U/S in 5 days
� �
Inconclusive or inadequate study
...
Venography or MRI
i
I
DVT present
Trelltment
Negative for DVT
...
...
Nonatment
Traatment
Nonatment
Toronto Notes 2011
Medical Emergencies
Determine need to investigate via PERC score
Emergency Medicine ER35
Clllil:ll Crillril. ,.._.. �
�
Walls criteria
<500 ng{mL
PE excludad
>500 nglml � � � � � � � � � � � Spiral CT pulmonary
Puoilivl :.1/8
PE excludad
Negatiw PEexcludad
.
I
angiog111m {CT-PA)
l
I
. . . . . . . . . illilerglnlr illplmllll l'lliiiD with Sulpldld I'UIIIIIIJ EIIWI
J7hmmblllemolt2004; Z(81:1Z47-55. ,_..ec To. . pWnonllly embolsm (1') ruleaut crillria !PEIIC) tlllt em b1 Ulld 111111 bldlill,
]IMI'B -wsti1g fur PERt. Also, il p!MII! awr-1Bstinu far Pf. wtidl ilcua th!Hln IBit � � � � � � � � � � � � � reds i1 poilives.
� � � � � � � � � � � � � � � � � � � � � � � � � � � � � � �
rue
� � � � � � � � � �
PE confirmed
Figure 13- Approach to Suspected PE
Detsrmine clinical probllbiity af PE via Wall's (high, moderab or low)
tram 3148 ER pllilrD MY!Id lor pilllihll PE 111 diMIIup RJit.autcritlril. ThlllppiiCition allllt dMbped rules- inwstiQifld i114271ow-risk pdenls 11111382 'le1'fliiW risk Pl1ierD. buill: Eigllt....mblll Will incl1111d i11 bbi � � � � � � <50Y'Ifl, pulse <100 � �� � >84\. no unillllll'llleg tw*g. no 1-.noptysia, no l1l*lt t1un1 or Sllgefy; no prior PE or DVT. no honnonallllj IIIIIIIIIIQIIIMIICOIIIUIId ID Ml<l PE.In lawiislt 111d V11V IDwiilk J)ltilnls. 1111 aa bid 1switMy all& and 1001. � � IIIII aspacificily al 'lland 15\
� � � � � � � � � lor PE 11111' nat hi 1iMinble f II eijJt fldDrs in the P8IC IIIli nagelivl.
Normal V/U scan and any clinical probability of PE PE excluded
V/Uscan
s..-y: �
respedt.letf.
Low probability V/U
scan and low clilical probability of PE PE excluded
...
High probability V/U scan and high clinical probability of PE PE confirmed
...
All other combimdions
af V/U scan 111sults and
clinical probability of PE Pulmonary angiogrem or sariallower IIX!nmity venous utlnsounds
Figure 14. VJQ.Based Algorithm for Suspected PE
Diabetic Emergencies
see also Endocrinolog)T, Ell
Diabetic Ketoacidosis (DKA) severe insulin deficiency resulting in hyperglycemia (11-55 mmol/L), dehydration and electrolyte abnormalities history and physical examination - often young, type 1 DM, may be first presentation of undiagnosed DM (may occur in small percentage of type 2 patients) early symptoms: polyuria, polydipsia, malaise late signs and symptoms anorexia, nausea, vomiting, dyspnea (often due to acidosis), fatigue abdominal pain drowsiness, stupor, coma Kussmaul's respiration fruity acetone breath investigations CBC, glucose, electrolytes, BUN/creatinine, Ca, Mg, phosphate, urine glucose and ketones ABG ECG (MI possible precipitant; electrolyte disturbances may predispose to arrhythmia) management rehydration bolus of NS, then high rate NS infusion (but beware of overhydration and cerebral edema, especially in pediatric patients) potassium essential to avoid hypokalemia: replace KCl (20 mEq/L if adequate renal function and initial K <5.5 mmol/L) use cardiac monitoring if potassium levels normal or low insulin critical, as this is the only way to turn off gluconeogenesis/ketosis do not give insulin ifK <33 mmol/L initial bolus of5-10 U short-acting/regular insulin (or 0.2 U/kg) IV in adults (controversial- may just start with infusion) followed by continuous infusion at 5-10 U (or 0.1 Ulkg) per hour add DSW when blood glucose <15 mM to prevent hypoglycemia bicarbonate is not given unless patient is at risk of death or shock (typically pH <7.0)
1'1-.cipUiing fllelor in DICA
The 5r.
lrnction
Ischemia
lrnll:lion lntoxiclllion lnulil missed
.....
4 crlterill far DICA Dx: hyparglycemia, metabolic acidosis, hyperketonemia,
Qlonurill_
, , ..-----------------.
ER36 Emergency Medicine
Medical Emergencies
Toronto Notes 2011
Hyperosmolar Hyperglycemic State (HHS)
state of extreme hyperglycemia (44-133.2 mmoUL) due to relative insulin deficiency; increased counter-regulatory hormones, gluconeogenesis, and dehydration (due to osmotic diuresis) in type 2 DM, high mortality (approaches 50% even with optimal management) history and physical examination mental disturbances, coma, delirium. seizures polyuria nausea, vomiting investigations CBC, electrolytes, creatinine, BUN, glucose, Mg, phosphate, urine glucose and ketones ABG ECG management rehydration with NS (total water deficit estimated at average 100 cc/kg body weight) 0 2 and cardiac monitoring, frequent electrolytes and glucose monitoring insulin as required identify and treat cause
...
..,
..
� � � � � � � � � � � � � � � � � �
�
Cerlbral 1dem11 may ocrur �
hyperosmolalily 1reated too
IIIKJM1ively,
..... ,
� � � � � � � � � � � � � � � � � �
Hypoglycemia very common ED presentation
management focus treatment ofhypoglycemia investigation of cause (most often due to exogenous insulin, alcohol, sulfonylureas) history and physical examination last meal, known diabetes, prior similar episodes, drug therapy and compliance liver/renal/endocrine/neoplastic disease depression, alcohol or drug use management IV access and rapid BG DSOW 50 mL IV push, glucose PO if mental status permits if IV access not possible, glucagon 1-2 mg IM, repeat x 1 in 10-20 min 0 2, cardiac, frequent BG monitoring thiamine 100 mg 1M full meal as soon as mental status permits if episode due to long acting insulin, or sulfonylurea&, watch for prolonged hypoglycemia due to long t 112 (may require admission for monitoring) search for cause
DRill Inducing Hypoglycemill Insulin Sulfa abx
Sulfonylur1u Cotrimazol1
Ethanol Salicylates
Acetaminophen
AmpiciUin Trtracycline Amphetamines
Cocaine Pyridoxine
NSAIDS
� � � � � � � � � � � � agoni5ts
lithium
Calcium
ACE-I Theophylline
Quinine
MAOI
Coumadin
Electrolyte Disturbances
see Ne.phrology and Endocrinology
Tabla 15. Elactralyta Dilturbanca&
Elactralyta Distwlllnce
C111111111 Caul
Symplllms
Treatment
Salt restrict 111d give free water
Spacial Clllllidaratians No more then 12 � � � � � � in 24 hrs drop i1 Na (0.5 mmoiiiJlrl due to risk of cerebral edelllil, seizure&, death
llypamllnlmia
lnadBIJlal! Hz(! intake (elderly/disabled) Lethargy, weakness, initabiity, 111d or inappropriate excretion of Hz(! edema. Seizures and coma occur (diurutie5, li, Dl) with 58IIIJ8 elevation& of Na levels (> 158 mmollt) Hypo-08111olll' (dilutional e.g. CHF. cirrhosis, ascites) and hyper-osmolar (usually glucose) Rhllbdornyolysis, insulin deficiency, mlblbolic acidosis Mstabolic alkalosis, insulin, diurutics, anorexia Ventolin Hyper.fTH and malignancy account
Hyp-m=mia
Acute: Neurologic symptoms 2" to cereml edema, IVa. decreased
LDC, depressed reflexes
Watur11181rict Acute: correct rapi!ly 3'l6 NaCI
� � � � �
Limittlllal rise to 8 mmolll in 241111 (0.5 mmoVIJhr � � � � � � � � � as plllierrts are at risk of central pontine myelinolysis ECG: Peaked/Narrow T wave, decreased Pwave, prolonged PR intarval, widening of QRS, AV block. Vfib
ECG: Uwaves most � � � � � � � � � � � � ftattenac11 iwerted Twaves, prolonged ar. depressed ST May need to restore Mg
Chronic: IV NS + furosemide Nausea, palpitations, mJscle stiffness, Prutect nell'!: Ca gluconate anrflaxill Shift Kinto cells: � � � � � � � R, � Vantol in Nausea, vomiting. fatigue, � cral!1)5, constipation
� � � � � � � � � � �
KDurf'l, Ksparing diu181ics, IV solutions with 20-40 mEq KCI pll' liter over 3-4 hours
for approx. 90% of cases
Multisystem including CVS, Gl (pms), renal (stones), rheumatological, MSK (bones), psychiatric (moans)
Isotonic saline+lasix if hypervolemic Patients with more severe or Bisphosphonates, dialysis, chelation symptomatic hypercalcemia n usually (BlTA or oral phosphate) dehydmted and require saline hydration as i1itialthe18f1V
Hypocalcemia
IB1rog111ic, low Mg. liver dysfunclicn
1" hypo-PTli
Llr{ngosparn, hypenellexia, pnsthesia, tebrly, Chvostek"s and Trousseau's sign
Acute (ionized Ca <0.7 mMl requires Prolonged QT interval cen arise leadi1g immediate treetment IV calcium to anhythmia es can uppll' airway gluconate 12 g in 1020 mils obsbuclion followed by slow infusion
Toronto Notes 2011
Medical Emergencies
Emergency Medicine ER37
Hypertensive Emergencies
Hypertensive Emergency (Hypertensive Crisis) definition: acute elevation of systolic and diastolic BP (sBP >200, dBP > 120) and associated acute end-organ damage (CNS. renal. CVS. haem, pregnancy related) hypertensive encephalopathy: cerebral hyperperfusion due to blood pressure in excess of the capacity for cerebral autoregulation signs and symptoms: headache, nausea, vomiting, mental status changes (lethargy to coma), fundoscopic changes, over hours can lead to coma and death acute renal failure: can be either the cause or effect of a hypertensive emergency diagnosis: proteinuria, RBCs and RBC casts in urine, elevated BUN and creatinine treatment: IV calcium channel blockers, emergent ultrafiltration cardiovascular: Ml, CHF, thoracic aortic dissection left ventricular failure (LVF): decreased LV function due to increased afterload, increased oxygen demand and decreased coronary blood flow - signs and symptoms: chest pain, SOB - treatment: avoid diazoxide, hydralazine. minoxidil as these drugs increase oxygen demand thoracic aortic dissection (see � � � � � � � � � � C48) Pregnancy Induced Hypertension {PIH) see Obstetrics, OB14 watch for HTN, abdominal pain with severe nausea and vomiting, seizures, proteinuria, thrombocytopenia, increased AST, clonus, and hyper-reflexia initial treatment: lower BP, check reflexes, consider MgS04 if at risk for developing eclampsia, and assess risk to mother and fetus (e.g. deliver) antihypertensives: hydralizine 5mg doses in 15 min intervals when dBP >105 or sBP >160, until dBP 90-100; consider IV labetalol as an alternative Catecholamine-Induced Hypertensive Emergencies etiology: discontinuation of short-acting sympathetic blocker (e.g. clonidine. propranolol), pheochromocytoma, sympathomimetic drugs (cocaine, amphetamines, phencyclidine}, MAOI in combination with sympathomimetic& or tyramine-containing foods (cheese, red wine) treatment: immediate goal of IV therapy is to reduce the mean arterial pressure (MAP) by 25% in 30-60 min (5-10 min for aortic dissection) then a gradual reduction in MAP over the next 6 hrs to 160/100 BP should NOT be lowered rapidly in patients with major cerebrovascular event decreasing BP too fast may extend or worsen stroke if dBP >120, aim to reduce dBP by 20% in the first 24 hrs treatment may be initiated in the ED followed by prompt admission to ICU for continuous BP monitoring re-administer sympathetic blocker if due to withdrawal (e.g. clonidine. propranolol) Hypertensive Urgency definition: severely elevated blood pressure (usually sBP >180, dBP > ll5) with no evidence of end-organ damage most commonly due to non-adherence with medications treatment: gradually reduce pressure over 24-48 hours to a level appropriate for the patient goal is to differentiate hypertensive emergencies from hypertensive urgencies History and Physical Examination prior hypertensive crises antihypertensive medications prescribed, adherence, and BP control MAOIs, substance use, use of stimulants or withdrawal from sedatives including EtOH blood pressure measurement in all limbs fundoscopic exam (hemorrhages, papilledema, etc.), gross motor examination Investigations CBC, electrolytes, BUN, creatinine, urinalysis peripheral blood smear - to detect microangiopathic hemolytic anemia CXR- if SOB or chest pain ECG, troponins, CK - if chest pain CT head - if neurological findings or severe headache Treatment of Hypertensive Emergencies see Table 16
....
,,
� � � � � � � � � � � � � � � � � � � �
Sia- of Rulli Depletion Increased heart nrte Postural changes in vital signs Decreased urine output (normal:
� � � � � � �
Hypertensive Dec1'81Sed .tin 1utgor Sunkan l'f8S Dry mucous membnnel Decreased capiUary l'lfill
HELLP Syndnlmo (saen only in
� � � � � � � � � � � � � � � � � � � � � �
Hemolytic anemia EIIYIIted Livw anzymas
lDw P111181et count
....
,_._ , ______________
__,
c.t.cholamint lnduc:ad Hyll'rtpsiva Emorgenciel Avoid use of non-selective Jl-blockers as thay inhibit Jl-madiatad vasodilation
and leave a-adrenergic vasoconstriction unopposed.
....
,...-----------------, , ,..._----------------, ,
,,
� � � � � � � � � � � � � � � � � � � � �
EmorlfliiiCY
N/V
S.izur8 Headache Dr altEred mental status Cushing response
....
Evidllnco of Eftd.Orgu Domogo CNS: headache, focal neurological signs, seizures CVS: angina, CHF, bllck pain (110rtic dissection} ln..: hematuria, oliguria Eyes: papilladam1, retinal hemorrhages
.....
� � � � � � � � � � � � � � � � � � � �
Wrth CNS manife5tations of SlMire hypertension. it is often difficult to diffaruntiatu caUAI rulalionlhips � � � � � hypartsnsion could ba secondary to primary cnb111l event (Culhing efl8ct}].
ER38 Emergency Medicine
Medical Emergencies
Toronto Notes 2011
......
t-----------------,
Teble 16. Most Commonly Used Agents for the Treatment of Hypertensive Crisis
DIUII VASODilATORS Sodium 0.25 10 � Nitroprusside (VliSCular 1mooth musde dilator) 1st line
� � �
DIISI88
Onsll of
Most commonly used agants for hypllllllnsiw crisis .,. illmllol and nitroprusside.
Actian
Durllion Advlne of Action Effects
Special
lnlkltians
Most hypertensive emergencies (esp CHF. aortic di$$eclion) Use in combination with � � � � � � � � � � � (e.g. esmalol) in aortic dissection Caution with high ICP and azcrtemia Most hypertensive emergencies Caution with acute CHF
Immediate 3-5 mil
......
.. ,
� � �
NN. muscle twitching, sweating. cyanide intaxication, COIOIIII'( steal syndrome
D111111 ht Inc- Adrnglc
Stimuldllll MAOis
TCAs
Amphataminas
Nicardipine (CCB) 2 mg IV bolus, then 4 m!Vkwbr IV
15-30 min
40 min
Cocaine
Techycllllia, headache, flushing. local phlebitis (e.g. encaphalopathy, RF. eclampsia. sympathetic crisis)
Fenoldopam Mesylate (dopamile receptor antagonist)
0.05-0.1 fJlllll/k3'min IV <5 min
8-10min Techycllllia, headache, nausea, flushing (e.g. acute RF)
Most hypertensive emergencies Caution with glaucoma
Enalapril (ACEI)
0.62S.1.25 mg IV q6h
15-30 min
12-24 hr
Theoretical filii in pressure Acute LV lililure in high renin states nat Avoid in acute Ml, pregnn:y, seen in studies acute RF Hypotension, bradyclldia, MVl'uhlonary edema haadache, lightheadedness, diz2iness
Nitroglycerin
S.20 11w'min IV
12mil
3-5 mil
llythlazine
S.10 mg IVIIM qZIInin (max2Dmg)
520 min
� � �
In
Dizziness, lhlwsiness, headache. tachycardia. Na rell!ntion
Vomiting, scalp tingling, � � � � � � in throat, dizziness, nausea, heart block, orthostatic hypotension
Eclllmpsia
ADRENERGIC INHIBITORS
Lablllalal 20mg1Vbolusq10min 5-10min or 0.52 mg/min
� � � � � �
Most hypertansiw ernergencies (esp. edampsia) Avoid in acute CHF, HB >1st degree Aortic dissection, acute Ml SVT dysrhythmias, perioperativa HTN Avoid in acute CHF, HB >1st degree Catecholamine excess (e.g. pheo)
Esmolal
250-500 !IIJikW'min 12 mil 1min, then 50 fiG"kkrmin for 4 min; repeat
11)..20 min Hypotension, nausea. bronchospasm
......
, .J-----------------.
Phentolamine
5-15 mg qS-15 min
1-2mil
3-10 min Tachycllllia. headache, flushing
'Hypotansian n.y occur will! Ill afthala agan1J
If patient presents within 4.5 llours of onsll of disabling neurological dlficits greater than 60 minutes with no signs of 1'11101ution, thay 11111y be Cllldidllte for 11Yombolysi5. Do brief ISSe55111enl and order Slit CT held.
Stroke
see Neurology. N44 can be ischemic (80% of all strokes) or hemorrhagic
Elu:lulian � � � � � far tPA: Suspected sublrechnoid hemorrhlllga Previous irtrecrenilll hemorrhlllae Cerebral infarct or � � � � � � � � held injwy within thl past 3 months
Recent pericarditis Major surgery within the past 14days Gl or urinary hemorrhlllga within the past 21 days Recent lumbar punctura or arterial puncture It noncornpressible silll
Pllient is pregnant � � � � � � � rnmHg systolic, � � � � 11 0mmHu diutDiic
History consider acute stroke if acute neurological deficit (focal or global) or altered LOC more likely to be hemorrhagic if: nausea, vomiting, headache, change in LOC, seizure common symptoms of stroke: abrupt onset of hemiparesis/monoparesis, visual loss/field deficits, diplopia, dysarthria, ataxia, vertigo, aphasia, sudden decrease in LOC determine time of symptom onset for consideration of thrombolytic therapy DDx includes hypoglycemia, Todds paralysis, peripheral nerve injury, Bell's palsy, tumour Physical Examination vitals if decreased LOC: assess for ability to protect airway rule out trauma, infection, meningeal irritation search for cardiovascular causes of stroke ocular fundi (retinopathy, emboli, hemorrhage) and pupils CVS (murmurs, gallops, AFib) PVS (auscultate for carotid bruits)
oriNR >1.4 Piltlllt count < 100,000 Blood giLK:ose <2.8 or >22 mmolll Intracranial hemormage on CT/or III'QI volume infllm
Seizu11 Ill onllll CIIUSing d8ficit Previously ADL dependent (clinical judgmsnt)
Bleeding diathesis Prolonged (more then 40 seconds)
Toronto Notes 2011
Medical Emergendea/Gynecologic/Urologic Emergencies
Emergency Medidne ER39
neuro mental status, WC, cranial � � � � � � � � � motor function, sensory function, cerebellar function, gait, deep tendon reflexes confirm presence of stroke syndrome, and distinguish from stroke mimics (seizure, systemic infection, brain tumour, positional vertigo, Bell's palsy) establish neurological baseline should patient improve/deteriorate
.....
,,
� � �
Table 11. Stroke Syndromes
llegiDI of S1rol!l
Straka Syndrama Primarily fronlllllobe function affected Altared mantlll status, impaired judgment, cootralaterallower axtJarity weakness and hypoesthesia, gait apraxia Contralllteral hemiparesis (arm and face weakness > leg weakness! and hypoesthesia, ipsilllteral hemianopsia. gaze pret.alce to side of lesion :!: agnosia, receptive/expressive aphasia Affects vision am � � � � � � Homonymous hemianopsia, cortical blindness, visual agnosia, �
� � � � � � �
Dlffwre..._ .t UlliN D._,
11RILMNDiletUUr dlicil � � � PJPI Rdws lraelsed r. ircnlled
fllciajRn
Anterior Cerebral Artery
Midcle Cerebral AriBry
Alllrt
Ablnl\riillli
Posterior Cerebral Artery Vertebrobasilar Almry
mental status, inpaired memory
.....
1
Wide variety of CN, cerebellar and brainstem deficits: Vl!rligo, nystagmus, diplopia, visual field deficits, dysphagia, dysarthria, facial hypoeslhesia, syncope, ataxia Loss of pain illd tempalilture 5ensation � � � � � � � � � face and conlr.llateral body
,,
Investigations
CBC, electrolytes, blood glucose, coagulation studies, cardiac biomarkers, toxicology screen non-contrast CT head: look for hemorrhage, ischemia ECG echocardiogram: rule out atrial fibrillation, acute MI as source of emboli other imaging: carotid dopplers, CfA, MRA as appropriate
V.Werdisa11111
llilllted cniamyaplllhy Left heart myxoma
Atrial Fib Ml Endocarditis
c.-., Enllllli tr..
� � � � � � � � � � � � � � � � � � �
till ....
Prosthllic Valves
Management
quickly detennine if patient is eligible for thrombolysis (need acute onset less than 4.5 hours from drug administration time AND compatible physical findings AND normal Cf with no bleed) - not much time to do all of this (often requires designated stroke team) ABCs with RSI if GCS :5':8, rapidly decreasing GCS, or inadequate airway protection reflexes IV cardiac monitoring judge fluid rate carefully to avoid overhydration (cerebral edema) as well as underhydration (underperfusion of the ischemic penumbra) BP control: only treat severe hypertension (sBP >200, dBP >120, mean arterial BP >140) or hypertension associated with hemorrhagic stroke transformation, cardiac ischemia, aortic dissection, or renal damage; use IV nitroprusside or labetalol cerebral edema control: hyperventilation, mannitol to decrease ICP if necessary consult neurosurgery, neurology as indicated
c-
It'
Aculll Ataxia UNABLE TO STAND Underlying weakness (mimic mxial Nu1ritianal nuoplllhy (Yitamil Bu deficiency)
Artlliti.,tvuc... �
� � �
BnU..migraine
� � � � � � � � � � � � � � � � � � � � � � � �
� � � � � � � � � � � � � � � � � �
neuronitis
Trauma [past-concussive)
Dlher (rare genetic or metabolic
disaasa)
Stroke {ischemia or hemorrhage)
Medications
acute ischemic stroke: thrombolytics (rt-PA, e.g. alteplase) if within 3 hours of symptom onset with no evidence of hemorrhage on cr scan antiplatelet agents: prevent recurrent stroke or stroke after TIAs, e.g. aspirin (1 11-line); clopidogrel. ticlopidine (2nd-line)
Toxins [drugs, toluene, mercury) Alcahal
Neaplasmtparanaaplastic syndrome Demyelillltian [Miler Fistler, Guin 8111'6, MS)
Gynecologic/Urologic Emergencies
Vaginal Bleed
see Gptecolog)T, GY6 and Obstetrics, OB20
Etiology
pregnant patient 1st/2nd trimester pregnancy: ectopic pregnancy, abortion (threatened, incomplete, complete, missed, inevitable, septic), molar pregnancy 2nd/3rd trimester pregnancy: placenta previa, placental abruption, premature rupture of membranes, preterm labour either: trauma, bleeding cervical polyp postpartum postpartum hemorrhage, uterine inversion, retained placental tissue, endometritis non-pregnant patients dysfunctional uterine bleeding, uterine fibroids, pelvic tumours, trauma, endometriosis, PID, exogenous hormones
.....
,,
� � � � � � � � � � � � � � � � � � �
Vaginal bleeding can be life thremnlng. Always start with ABCs and ensure your J)ltient is stable.
ER40 Emergency Medicine
Gynecologic/Urologic Emergencies History menstrual history, sexual activity, contraception, history ofPID pregnancy details determine amount ofblood urinary, GI symptoms
Toronto Notes 2011
Physical Examination look for signs of hypovolemia pelvic examination - NOT if suspected placenta previa (ultrasound first) speculum exam if pregnant use sterile speculum bimanual examination if pregnant use sterile gloves if patient is near term with possible rupture of membranes and without other indications defer bimanual examination {infection risk)
,, ,
� � � � � � � � � � � � � � � � � � � � �
Need Jl-hCG <::1200 to see interuterine
chllnges on hnsvagilllll LVS.
,, ,
� � � � � � � � � � � � � � � � � � � � �
Cl-ilying milcarlilge (allertlon): MiiMII - non-viable inlraut8rine prapncy
111.-..t.ned - viii!U intnlut.in1 prapncy with os clond Inevitable - os closed, no products of conception pll$$ed lncampJ.Ie- products of concaption partially uxpalled Compll&e - products of concaption completely expelled Septic -any of llbova with � � � � � � � � � � of infection (usually incompletll) hcrent- >3 spon!IIIICIUII abortions (recurrent P!e!llllllCV loss)
Investigations IJ-hCG test fur all patients with child-bearing potential CBC, blood and Rh type, quantitative !J-hCG, PTT, INR type and cross if significant blood loss 1st/2nd trimester/non-pregnant ultrasound (U /S) - intrauterine pregnancy, ectopic pregnancy, traumatic injury, foreign body must correlate U/S findings with IJ-hCG ifU/S is non-diagnostic (transvaginal ultrasound will not see gestation in uterus if IJ-hCG < 1200 - must repeat) 2nd/3rd trimester pregnancy U/S if no fetal heart tones, no documented intrauterine pregnancy or unknown lie of placenta non-stress test to assess fetal well-being during work up of mother DIC panel if placental abruption - CBC, PTT, INR, fibrinogen postpartum U/S for retained products P-hCG if concerned about retained tissue Management ABCs pulse oximeter and cardiac monitors if unstable Rh immune globulin for vaginal bleeding in pregnancy and Rh-negative mother 1st/2nd trimester pregnancy ectopic pregnancy: definitive treatment with surgery or methotrexate intrauterine pregnancy, no concerns of coexistent ectopic: discharge patient with obstetrics follow-up U/S indeterminate or � � � � � � >1000-2000 IU: further work-up and/or gynecology consult abortions: if complete, discharge if stable; for all others, acquire gynecology consult 2nd/3rd trimester pregnancy placenta previa or placental abruption: obstetrics consult for possible admission postpartum uterine inversion: replace uterus immediately, may require operative management postpartum hemorrhage: extraction of placenta if retained, hysterectomy if uncontrolled bleeding retained tissue: D&C endometritis: IV antibiotics non-pregnant dysfunctional uterine bleeding (prolonged or heavy flow breakthrough bleeding and without ovulation, a diagnosis of exclusion) <35-40 years of age: Provera 10 mg POx 10 days, warn patient of a withdrawal bleed, discharge if stable if unstable, admit for IV hormonal therapy, possible D&C >35-40 years of age: uterine sampling necessary prior to initiation of hormonal treatment to rule out endometrial cancer, U/S for any masses felt on exam structural abnormalities: fibroids or uterine tumours may require excision fur diagnosis/ treatment. U/S for workup of other pelvic masses, Pap smear/biopsy for cervical lesions Disposition the decision to admit or discharge should be based on the stability of the patient, as well as the nature ofthe underlying cause; consult gynecology fur admitted patients if patient can be safely discharged, ensure follow up with family physician or gynecologist instruct patient to return to emergency fur increased bleeding, presyncope
,, ,
� � � � � � � � � � � � � � � � � � � � �
Vaginal bleeding (and its underlying causes) can be vary emotionally
1ilxing presentation lor patients. Ensure approprill18 support il provided.
Toronto Notes 2011
Gynecologic/Urologic Emergencies
Emergency Medidne ER41
Pregnant Patient in the ER
Tabla 18. Complications of Pregnancy
-------------------------------------Mltlrllll
First 1-14wks
Pregnmcy failure
Sponlzroeous abortion Fetal demise Gesliltional trophoblastic disease Disorders of felal growth
Ectcpic pregnancy Anemia Hyperemesis gravidllllm
� � � � � � � � � � � � � � � � � � �
Second
� � � � � � � �
IUGA
Oligcllpolyhylhmnios
GIISialional diab818s � Ah D:ompatibility
� � � � � � � � � � � � � � � � � �
� � � � � � �
Third 28-40 wks
Vasa previa
Preterm labourJPPAOM PreeciBI!1lSia/eclall1lSiB Placenta previa Placental abruption Uterine rupture
DVT
Nephrolithiasis (Renal Colic)
� � � � � � � � �
..... I
� .� � � � � � � � � � � � � � � � � �
Kidney Stann
Epidemiology and Risk Factors
10% of population (twice as common in males) recurrence 50% at 5 yrs peak incidence 30-50 years of age 75% of stones <5 mm pass spontaneously within 2 weeks, larger stones may require consultation
8'"' Ca 1'"' S1ruvitB
1'"' Uric acid
Clinical Features
urinary obstruction -+ upstream distention of ureter or collecting system -+ severe colicky pain may complain of pain at flank, groin, testes, or tip of penis writhing, never comfortable, nausea, vomiting, hematuria (90% microscopic), diaphoresis, tachycardia, tachypnea occasionally symptoms oftrigonal irritation (frequency, urgency) fever, chills, rigors in secondary pyelonephritis
Differential Diagnosis of Renal Colic
acute ureteric obstruction (other causes) UPJ obstruction sloughed papillae clot colic from gross hematuria extrinsic (e.g. tumour) acute abdomen - biliary, bowel, pancreas, AAA gynecological- ectopic pregnancy, torsion/rupture of ovarian cyst pyelonephritis (fever, chills, pyuria, vomiting) radiculitis (Ll) -herpes zoster, nerve root compression
Investigations
screening labs CBC -+ elevated WBC in presence of fever suggests infection electrolytes, Cr, BUN -+ to assess renal function urinalysis: R&M (WBCs, RBCs, crystals), C&S imaging non-contrast spiral CT is the study of choice abdominal ultrasound may demonstrate stone or hydronephrosis strain all urine -+ stone analysis
Management
analgesics, antiemetics, IV fluids urology consult may be indicated, especially if stone >5 mm, or if patient has signs of obstruction or infection a-blocker helpful to increase stone passage in select cases
..._. I
,._________________
Disposition
most patients can be discharged ensure patient is stable, has adequate analgesia, and is able to tolerate oral medications may advise hydration, calcium supplementation, and limitation of protein, sodium, oxalate and alcohol intake
lndiclllillns for Admission to Hlllpital lntnlclabJ. pain Fever (suggests infection I Single kidney willllnllral obstruction Bilateral obstructing stones lntnlclabJ. � � � � � � �
Compromi1ed renal function
ER42 Emergency Medicine
Ophthalmologic Emergencies
Toronto Notes 2011
Ophthalmologic Emergencies
Ophthalmologic Foreign Body and Corneal Abrasion
see also Ophthalmology. OP17
History
AlWAYS assess visullacuity i1 both ayes when a patient prasants to the ER � � � � 111 ophthalmologic compllint.
..._,,
� � � � � � � � � � � � � � � � � �
pment with blun.d vision.
patient may complain of pain, tearing, itching, redness, photophobia, foreign body sensation elicit history of potential trauma to eye mechanism of foreign body insertion- if high velocity injury suspected (welding, metal grinding, metal striking metal), must obtain orbital x-rays or ultrasound to exclude presence of intraocular metallic foreign body see Table 19 for important considerations of red eye in the emergency department
Table 19. Differential Diagnosis of Red Eye in tile Emergency Deparbnent
Light Sensitivity Unilateral Significant pain Iritis, keratitis, abrasion. ulcer Above + herpes simpleK, acute angle closure � Above + scleritis Corneal ulcer All Df1he above
� � � � � � �
Alrf rrtiology of red ayes may alao
..._,,
� � � � � � � � � � � � � � � � � � �
Dlbu Opbthlllmalqic Em.,..ncills (S.1 Ophtbalmo!oPY OP5) lnfwctiaua-Red ll'fB (Table 19), andoplrthalmitis, � � � � � cellulitis Trau11111 - rutinal detachment, globe
White spot an cornea
Blurred vision
Non-reactive pupil
Copious discharge
Acute glaucoma, iritis
Gonococcal �
� � � � � � � � � � � � �
ruptura, orbital blow-out hcturas, chemical bums Autoimm-- Giant cal artsritis
Physical Examination
,, ,
� � � � � � � � � � � � � � � � � � �
Contrlndlcatl- lD Pupil DilatiDn Shallow lntlrior chamb. lril-wpported lens implant Pomntial niUI"Diogicelllbnonmality ruquiring pupillary uvlluation Caution with CV dis8111- mymatics
can cause tachycordia
visual acuity in both eyes with best corrected vision pupils, extraocular movement, external ocular structures fundoscopy tonometry - measurement of intraocular pressure (with Tonopen) normal pressure: 10-20 mmHg, glaucoma associated with increased pressures slit lamp exam: start with unaffected eye, perform a systematic examination: lids, lashes, lacrimal apparatus, conjunctiva, sclera, cornea, anterior chamber, iris, lens, vitreous proparacaine anaesthetic drops may ease examination look for rust ring with metallic foreign body; corneal edema, anterior chamber cells/flare may use tluoroscein dye which stains de-epithelialized cornea green when viewing with cobalt blue filter
Management
copious irrigation with saline for any foreign body remove foreign body under slit lamp exam with cotton swab or sterile needle antibiotic drops qid until healed patching may not improve healing or comfort - do not patch contact lens wearers limit use of topical anesthetic to examination only consider tetanus prophylaxis ophthalmology consult if globe penetration suspected
Initial Management of other Opthalmologic Emergencies
ruptured globe - stabilize any foreign body, shield eye with no pressure, elevate head of bed to 30, tetanus prophylaxis, IV antibiotics, NPO, analgesic, antiemetic, sedation prn retinal artery occlusion - globe massage, paper bag breathing, carbogen inhalation (95% oxygen, 5% carbon dioxide) chemical burn - immediate copious irrigation, may consider topical anaesthetic drops to facilitate irrigation acute angle-closure glaucoma - IV or PO acetazolamide, topical pilocarpine and timolol preseptal cellulitis (2 to superficial trauma) - topical or systemic Ahx orbital cellulitis (2 to sinusitis) - admit, IV antibiotics, blood cultures, CT
Disposition
most patients can be discharged with outpatient ophthalmology follow-up admit patients requiring emergent ophthalmologic procedures or IV antibiotics
Toronto Notes 2011
Dermatologic .Emergencies
Emergency Medicine ER43
Dermatologic Emergencies
Life Threatening Dermatoses
Rash Characteristics
DIFFUSE RASH stapbylococcalscalded skin syndrome (SSSS) caused by an exotoxin from infecting strain of coagulase-positive S. aureus mostly occurs in children prodrome: fever, irritability, malaise and skin tenderness sudden onset of diffuse erythema: skin is red. warm, and very tender flaccid bullae that are diffi.cult to see, then desquamate in large sheets Nikolsky's sign: gentle lateral stroking of skin causes epidermis to separate toxic epidermal necrolyais (TEN) see Dermatology, D22 caused by drugs (e.g. phenytoin, sulfas, penicillins and NSAIDs), bone marrow transplantation, blood product transfusions usually occurs in adults diffuse erythema followed by necrosis severe mucous membrane blistering entire epidermis desquamation high mortality (>50%) toxic &hock syndrome (TSS) see Infectious Diseases, ID27 caused by superantigen from S. aureus or GAS activating T-cell and cytokines patient often presents with onset of shock and multi-organ failure, fever diffuse erythematous macular rash at least 3 organ systems involved: CNS, respiratory, GI, muscular, mucous membranes, renal, liver, hematologic, skin (necrotizing fasditis, gangrene) VESICOBULWUS LESIONS erythema multiforme (EM) see Dermatology. D22 immunologic reaction to herpes simplex viral prodrome 1-14 days before rash "target lesion: central gray bulla or wheal surrounded by concentric rings of erythema and normal skin Stevens-Johnson syndrome (SJS) see Dermatology, D22 related to drugs such as antiepileptics and biologic agents, e.g. intliximab EM with constitutional symptoms and mucous membrane involvement (milder mucous membrane involvement than TEN) DISCRETE LESIONS pyoderma gangrenosum often associated with immunocompromised patients (HIY,leukemia or lymphoma) with Gram-negative sepsis often occurs in arms, hands, feet, or perineal region usually begins as painless macule/vesicle � � pustule/bulla on red/blue base � � sloughing, leaving a gangrenous ulcer
diaseminated. gonococcal infection (DGI)
see Dermatology, D32 fever, skin lesions (pustules/vesicles on erythematous base -5 mm in diameter), arthritis Qoint swelling and tenderness), septic arthritis (in larger joints, e.g. knees, ankles and elbows) most commonly in gonococcus positive women during menstruation or pregnancy skin lesions usually appear in extremities and resolve quickly (<7 days) meningococcemia flu-like symptoms of headache, myalgia, nausea and vomiting petechial, macular or maculopapular lesions with gray vesicular centres usually a few millimeters in size but may become confluent and hemorrhagic usually appear in extremities but may appear anywhere look for signs ofmeningeal irritation: Brodzinski, Kernig, nuchal rigidity, jolt accentuation
History and Physical Examination
determine onset, course, location of skin lesions fever, joint pain associated symptoms: CNS, resp, GU, GI, renal, liver, mucous membranes medication history vitals
ER44 Emergency Medicine
Dermatologic Emergencies/Environmental Injuries
Toronto Notes 2011
..,., ,
t----------------.
Thorough d111118tol0ilic uaminations 1111 raquirad; axaminatian of IIIYITiplomlltic skin mav identify ma111lasionsl Ensure adequal8 drapiniJ duriniJ dermataiOIJic axaminlltions.
Investigations immediate consultation if patient unstable CBC, electrolytes, creatinine, AST, ALT, ALP, blood culture, skin biopsy, serum immunoglobulin levels (serum IgE) Management general: judidous IV fluids and electrolyte control, consider vasopressors if hypotensive, prevention of infection determine if admission and consult needed: dermatology or infectious diseases specific management is determined by etiology SSSS, TSS, DGI and meningococcemia IV antibiotics EM, SJS, and TEN stop predpitating medication fluids symptomatic treatment: antihistamines, antacids, topical corticosteroids, systemic corticosteroids (controversial), prophylactic oral acyclovir, consider IVIG TEN: debride necrotic tissue Disposition most cases will require urgent care and hospitalization TEN: early transfer to bum centre improves outcome
Environmental Injuries
Heat Exhaustion and Heat Stroke
predisposing factors: young persons who overexert themselves, older adults who cannot dissipate heat at rest (e.g. using anticholinergic drugs such as antihistamines or TCAs), and patients with schizophrenia who are using anticholinergic or neuroleptic medications
..,., ,
Heat exhaustion IHEI mav claselv � � � � � � � � � � heat stroka. HE mav IMII1tulllly PIOIJress to heat stroke. Therefore � �
diagnosis is uncerl:lin trlllt as halt
.----------------.
Heat Exhaustion (HE) clinical features relate to loss of circulating volume caused by exposure to heat stress "water depletion": HE occurs if lost fluid not adequately replaced "salt depletion: HE occurs when losses replaced with hypotonic fluid Heat Stroke life-threatening emergency resulting from failure of normal compensatory heat-shedding mechanisms divided into classical and exertional subtypes (see Table 20) if patient does not respond relatively quickly to cooling treatments, consider other possible etiologies ofhyperpyrexia (e.g. meningitis, thyroid storm, anticholinergic poisoning. delirium tremens, other infections)
Teble 20. Halt Exheustion vs. Halt Stroke
Eullio1111 Hilt Stroa
Clnicll Features
Non-specific malaise, headache, fatigue Occurs in salting Ill hi!#! Body temp <40.50C (usually IIOITTI81) ambiant l8111!1118tui"BII (e.g. No coma or seilii"8S heat wave. poor ventilation) Dehythtion {1' HR, orthostatic Often patients n okjer, pear, hypotension) and sedentary or immobile Dry, hot liki1 Temp uSUBIIy >4c.sc Altered mental status, seizures, deliiurn, coma May have elevated AST, ALT
strub.
Occurs with high endogenous heat production (e.g. exercise) illd owrwhelmed homeostatic meclllllisms Patients ellen younger, more aclive Skin often diaphoretic Olh111 fecrtum a& far clas&ical HS, but mav also have DIC, BCUte ranll failure, rhabdomyolysis, marked lactic acidosis
Tlllllmllll: Rast in acool anvironment Normal salile IV if orthostatic hypotension; otherwise replace losses slowly PO
Cool dawn body temperature with water mist (e.g. spray bottle) and standing fans Ice Wllll!r irnnersion also effective; monilar body temp closely to avoid hypothermic oversholll � � � � � airway because of risk of seizures and aspiration Gin ftuid IBIIU&eililtion if &till hypotensin after above 1herapy Avoid a-egonists (e.g. epinephrile) peripheral VBSOConstriction and antipyretics (e.g. ASA)
Toronto Notes 2011
Environmental Injuries
Emergency Medicine ER45
Hypothermia and Cold Injuries
predisposing factors: extremes of age, lack ofhousing, drug overdose, EtOH ingestion, trauma
(incapacitating), cold water immersion, outdoor sports treatment based on: (a) re-warming and (b) supporting cardiorespiratory function complications: coagulopathy, acidosis, ventricular arrhytluni.as (VFib), asystole, volume and electrolyte depletion labs: CBC, electrolytes, ABG, serum glucose, creatinine/BUN, Mg, Ca. amylase, coagulation profile imaging: CXR (aspiration pneumonia, pulmonary edema are common) monitors: ECG, rectal thermistor, Foley catheter, NG tube, monitor metabolic status frequently Tabla Zl. Classification of Hypothermia
Mild
Moderate
32-34.9"C 28-31.9C <Z8C
Tachypnea, tachycardia, ataxia, dysar111ia, shivering
s_.
Loss of slivering. arrytimias, Osborne (J) waves on ECG, decreesed LOC, combative behBViour, musde rigidity, dilated !XJpils Coma, hypot1111ion. acidemia. ventricular fibrillation, asystole, flaccidity, a111aa
Re-warming Options gentle fluid and electrolyte replacement in all (due to cold diuresis) Passive External Re-warming (PER) suitable for most stable patients with core temperature >32.2C involves covering patient with insulating blanket; body generates heat and re-warms through metabolic process, shivering Active External Re-warming (AER) involves use of warming blankets beware "afterdrop" phenomenon (warming of extremities causes vasodilation and movement of cool pooled blood from extremities to core, resulting in a drop in core temperature -+ cardiac arrest) safer when done in conjunction with active core re-warming Active Core Re-warming (ACR) generally for patients with core temperature <32.20C, and/or with cardiovascular instability avoids "afterdrop" seen with AER alone re-warm core by using warmed humidified oxygen, IV fluids peritoneal dialysis with warm fluids gastric/colonic/pleural irrigation with warm fluids external circulation (cardiopulmonary bypass machine) is most effective, fastest Cardiac Arrest in the Hypothermic Patient do all procedures gently or may precipitate VFib check pulse and rhythm for at least 1 minute; may have profound � � � � � � � � � if any pulse at all (even very slow) do NOT do CPR if in VFib try to defibrillate up to max 3 shocks if core temperature <300C intubate gently if required, ventilate with warmed, humidified 0 2 medications (vasopressors, antiarrhythmic&) may not be effective at low temperatures controversial; may try one dose focus oftreatment is re-warming
FROSTBITE Classification
ice crystals form between cells
classified according to depth - similar to burns (1st to 3rd degree) 1st degree symptoms: initial paresthesia. pruritus signs: erythema. edema. hyperemia. no blisters
lnddegree
symptoms: numbness signs: blistering (clear), erythema, edema
3rddegree
symptoms: pain, burning, throbbing (on thawing); may be painless if severe signs: hemorrhagic blisters, skin necrosis, edema. no movement
Management treat for hypothermia: � � � � � fluids, maintenance of body warmth remove wet and constrictive clothing
ER46 Emergency Meclidne
Emironmeatal.lnjuries
1'oroDio � � � � � 2011
,, ,
� � � � � � � � � � � � � � � � �
lhllllllll (flamll, 8elld)
a..n ....:
a.ma1
,,.,
� �
Rldillion (UV. mlldiciUitunparticJ Bactrical
immerse in 4042"C agitated water for 1030 mlmrtes (very painful; administer adequate analgesia) dean injured area, leave injured region open to air
consider aspiration/debridement of blisters (controversial) debride skin gently tetanus prophylaxis consider penicillin G as frost bite injury Bl: high risk of infection surgical intervention may be required to release restrictive eschars never allow a thawed area to re-dilll/freeze
High llilll Fubln1 far lliwctilln
Pili
..._,,
Puncbn wol.ftds Crush ll)riM 1Naunda .,..ta" th., 12 l'llu111 Did HIIWl orfootwwwls, WMds rajDi11s lmmunocampromised patient .....,than 50 years Prasthalic jairts Dl' - - bilk "' andoclnlitis)
Burns
see �
� � � � � � � � � � PL15
..
�
U palm of the patient'a hand Ill wti111111111" of BSA lllflletlld.
Physical Examination bum size rule of nines (see Figure 15); does not include 1 degree burns bumdepth superfu:ial: epidermis ocly (e.g. sunburn) partial thickness: into superficial dermis deep or hair follicles, sweBI: glands full thiclcness: all layers ofthe skin deep: to fat, muscle, even bone Management remove noxious agent/stop burning process establish airway ifneeded (indicated with bums >4096 BSA or smoke inhalation injury) resuscitation for 2nd and 3rd degree bums (after initiation of2large bore IVs) Parkland Formula: Ringer's lactate 4 cc/kgi%BSA burned; give half in first 8 hours, halfin next 16 hours; mamtenance fluids are also required ifpatient cannot tolerate PO hydration urine output ls best measure of resusdtation, should be 40-50 cc/br or 0.5 cc/kgfbr; avoid diuretic& pain relief- continuous morphine infusion with breakthrough bolus investigations: CBC, electrolytes, urinalysis. CXR. ECG, ABG, carboxyhemoglobin bum wowul care- prevent infection, dean/debride with mild soap and water. sterile dressings escharotomy or fasdotomy for circumfi:rential burna (chest, extremities) topical antlbiotle&, systemic antibiotics Infrequently indicated tetanus prophyluls ifbum is deeper than superfidal dermis Disposition admit 2nd degree burns to >1096 BSA; any slgnificant 3rd degree burns 2nc1 degree on face, hands, feet, perineum or across major joints electrical. chemical burns and inhalation injury burn victims with underlying medical problems or immunosuppressed patients
Inhalation Injury
� � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � � �
Etiology carbon monoxide (CO) poisoning direct thermal inJury - limited to upper airway smoke causes bronchospasm and edema from particulate matter and toxic inhalants (tissue asphyxiates, pulmonary irritants, systemic tmins)
History and Physical risk factors: closed space fires, period of WlCODScioumess, nonoua chemicals involved cherry red skin (unreliable, usually post-mortem finding) singed nasal haira, soot on oral/nasal membranes, sooty sputum
hoarseness, stridor, dyspnea dec.reased we, confusion P02 normal but � � sat low suggests CO poisoning
� � � � � � � � � � � Rl all's far Tobll
Investigations measure carboxyhemoglobin levels
ABG CXR bronchoscopy
� � �
lady SrfaGa Ani liSA)
..._,,
� �
dletDidllme.
q..y, as aiwly Din bacama Dllslructad
lniiJbllb a.ly if you 1111pld inhallllian
Management CO poisoning: 10096 0 2 hyperbaric Oa (controversial) direct thermal inJury: humidifted oxygen, early intubation, pulmonary toilet, bronchodllators
Toronto Notes 2011
Environmental Injuries
Emergency Medicine ER47
Bites
Mammalian Bites see Plastic � � � � � PL6 history time and circumstances of bite, symptoms, allergies, tetanus immunization status, comorbid conditions, rabies risks, HIV/hepatitis risk (human bite) high morbidity associated with clenched fist injuries (CFI), "fight bites"
physical enmination
assess type of wound: abrasion, laceration, puncture, crush injury assess for direct tissue damage: skin, bone, tendon, neurovascular status investigations ifbony injury or infection suspected check for fracture and gas in tissue with x-rays get skull films in children with scalp bite wounds, CT to rule out cranial perforation initial management wound cleansing and copious irrigation as soon as possible irrigate/debride puncture wounds if feasible, but not if sealed or very small openings; avoid hydrodissection along tissue planes debridement is important in crush injuries to reduce infection and optimize cosmetic and functional repair culture wound if signs of infection (erythema, necrosis or pus); obtain anaerobic cultures if wound foul smelling, necrotizing, or abscess; notify lab that sample is from bite wound
prophylacti.c antibiotiC8
....
,,
� � �
High lllsk Criteria for lnfecti
WDUmlhc:bml Puncture wounds Cru511 injuries Wounds >12m old Hand or foot wounds Wounds near joints
htient hc:bml lmmunacarnpramised Age >50 Vear1 Prosthllic joints or wives
types of infections resulting from bites: cellulitis, lymphangitis, abscesses, tenosynovitis, osteomyelitis, septic arthritis, sepsis, endocarditis, meningitis a 3-5 day course of antibiotics is recommended for all bite wounds to the hand and should be considered in other bites if any high-risk factors present (efficacy not proven) dog and cat bites (pathogens: Pasteurella multocida, S. aureus, S. viridans) 80% of cat bites, 5% of dog bites become infected 1st line: amoxicillin + clavulinic acid human bites (pathogens: Eikenella corrodens, S. aureus, S. viridans, oral anaerobes) 1st line: amoxicillin + clavulinic acid rabies (see Infectious Diseases, IDS) reservoirs: warm-blooded animals except rodents, lagomorphs (e.g. rabbits) post-exposure vaccine is effective; treatment depends on local prevalence suturing vascular structures (i.e. face and scalp) are less likely to become infected, therefore consider suturing allow avascular structures (i.e. pretibial regions, hands and feet) to heal by secondary intention tetanus immunization if> 10 yrs or incomplete primary series Snake Bites history, physical exam, investigations and initial management similar to mammalian bites additional management issues snake bites are rarely fatal but proper precautions must be taken supportive management, observe for compartment syndrome, analgesia, tetanus prophylaxis contact regional Poison Control Centre for consultation constriction band should be placed proximal to bite observe for signs and symptoms of envenomation 15min-2hrs after bite (pain, sweating, edema, chills, weakness, numbness, tingling, HR changes, faintness, ecchymosis, NN); if no envenomation then remove band and monitor closely for 24 hrs if envenomation present, administer antivenom Insect Bites BeeStiop 5 types of reactions to stings (local, large local, systemic, toxic, unusual) history and physical exam key to diagnosis; no lab test will confirm investigations: CBC, electrolytes, BUN, creatinine, glucose, ABGs, ECG ABC management, epinephrine 0.1 mg IV over 5 minutes if shock. antihistamines, cimetidine 300mg IV/IM/PO, steroids, � � � � � � � � � � � for SOB/wheezing 3 mg in 5 mL NS via nebulizer, local site management West NUe VlrWI (see Infectious Diseases, ID28) severity: asymptomatic 80%, flu-like symptoms 20%, encephalitis <1% clues: aseptic meningitis/encephalitis in late summer in prevalent area incubation 3-14 days, symptoms last 3-6 days general symptoms: fever, malaise, anorexia, headache, altered mental status, motor weakness, ataxia, extrapyramidal signs, GI signs, myalgias, lymphadenopathy, rash, myocarditis, optic neuritis investigations: CBC, electrolytes, CSF, Cf/MRI diagnosis: CSF and serum for serology management: ABCs, IV fluids for dehydration, antibiotics if meningitis (based on CSF analysis), analgesia, antipyretics, interferon-a 2b, ribavirin
....
,,}-----------------, ,
CNS
ConUd AdmiaiDn if: Maclnta to severe inflctians Infections in inmunocampramised paliants Nat responding to oral Rx Penetnlting injuries to tendons, joints,
0plll1 fm:lures
ER48 Emergency Medicine
Environmentallnjurlesi'I'micology
Toronto Notes 2011
Near Drowning
most common in children <4 yrs and teenagers causes lung damage, hypoxemia and may lead to hypoxic encephalopathy must also assess for shock, C-spine injuries, hypothermia, scuba-related injuries (barotrauma, air emboli, lung re-expansion injury) complications: volume shifts, electrolyte abnormalities, hemolysis, rhabdomyolysis, A1N, DIC
Physical Examination ABCs, vitals: watch closely for hypotension lungs: rales (ARDS, pulmonary edema), decreased breath sounds (pneumothorax) CVS: murmurs, arrhythmias, JVP (CHF, pneumothorax) H&N: assess for C-spine injuries neuro: GCS or AVPU, pupils, focal deficits Investigations labs: CBC, electrolytes, ABGs, Cr, BUN, urinalysis imaging: CXR (pulmonary edema, pneumothorax) ECG Management ABCs, treat for trauma. shock, hypothermia cardiac and 0 2 sat monitors, IV access intensive respiratory care ventilator assistance if decreased respirations, pC02 >50 mmHg, or p02 <60 mmHg on max 0 2 may require intubation for airway protection, ventilation, pulmonary toilet high flow 0 2/CPAP/BiPAP may be adequate but some may need mechanical ventilation with PEEP arrhythmias: usually respond to corrections of hypoxemia, hypothermia, acidosis vomiting: very common, NG suction to avoid aspiration convulsions: usually respond to 0 2; if not, diazepam 5-10 mg IV slowly bronchospasm: bronchodilators bacterial pneumonia: not necessary to prophylax with antibiotics unless contaminated water or hot-tub (Pseudomonas) must observe for at least 24 hours as non-cardiogenic pulmonary edema may develop late Disposition non-significant submersion - discharge after short observation significant submersion (even if asymptomatic) -long period of observation (24 hrs) as pulmonary edema may appear late CNS symptoms or hypoxemia - admit severe hypoxemia, decreased LOC - ICU
Toxicology
Alcohol Related Emergencies
see Psychiatcy. PS20
.....
',.}-----------------, � �
Alc:ohol intwtication 11111y inVIIIidatll
inlonned consent
Acute Intoxication slurred speech, CNS depression, disinhibition, lack of coordination nystagmus, diplopia, dysarthria, ataxia -+ may progress to coma frank hypotension (peripheral vasodilation) if obtunded rule out head trauma/intracranial hemorrhage associated depressant/street drugs, toxic alcohols may also contribute to respiratory/cardiac depression hypoglycemia (screen with bedside glucometer) hepatic encephalopathy: confusion, altered LOC, coma precipitating factors: GI bleed, infection, sedation, electrolyte abnormalities, protein meal Wernicke's encephalopathy (ataxia, ophthalmoplegia, delirium) post-ictal state, basilar stroke
Toronto Notes 2011
Toxicology
Emergency Medicine ER49
Withdrawal
beware withdrawal signs (see Table 22) treatment diazepam 10-20 mg IV or PO OR lorazepam 2-4 mg IV or PO q 1hr until calm may use CIWA protocol and give benzodiazepines as above until CIWA <10 thiamine 100 mg 1M then 50-100 mglday magnesium sulfate 4 g IV over 1-2 h (ifhypomagnesemic) admit patients with delirium tremens (DT), arrhythmias, or multiple seizures
Table 22. Alcohol Wlllldrawal Signs
Time Since Last Drink
&-1 hr
....
Description
Generalized 1nmar, anxiety, agillltian, but no delirium
,,
Syndrome
Mild withchwal Alcoholic hallucinations
� � � � � � � � � � � � � � � � � � �
Aut!lnornic hyperactivity (silus tachycardial. insomnia, nausea. vomiting
Visual (most common), audi!Dry 111d tactile hallucinations Vrtals often normal
CIWA Wdhdr-llymptams N1U181 and vomiting Tremor
Pnxysmal SW181s Anxiety
1-2 dByl
I hr-2 dByl
J.5 dByl
WrthdlliWIII seizures
Delirium ln!mens (Dl)
Typically brief generalized tonic-clonic seizures May have several within afew hours
5% af urrtn!ated withdrawal patients Severely confused state, fluctuating levels af consciousness Agitation, insomnia, hallucination&idelusions. 1nmar Tachycardia, hyperpyraxia. diaphoresis High morlillity rate
Agitation Visual distubances Tactile disbriJances Auditory disturbances
Headache
Disarienlatian
10 rymptomallllch scored out of 7 except orientation is out of 4.
Seizures
associated with ingestion and withdrawal withdrawal seizures occur 8-48 hrs after last drink (typically brief generalized tonic-clonic seizures) if >48 hrs, think of DT (see Table 22) prophylaxis: diazepam 20 mg PO q lh x 3 minimum, regardless of CIWA score CT head if focal seizures have occurred
Cardiovascular Complications lfi'N
cardiomyopathy: SOB, edema arrhythmias ("holiday heart'") atrial fibrillation (most common), atrial flutter, SVT, VT (especially Torsades if hypomagnesemic/hypokalemic)
Metabolic Abnonnalities
alcoholic ketoacidosis history of chronic alcohol intake with abrupt decrease/cessation malnourished, abdominal pain with nausea and vomiting anion gap (AG) metabolic acidosis, urine ketones, low glucose and normal osmolality treatment: dextrose, thiamine (50-100 mg prior to dextrose), volume repletion (with NS) generally resolves in 12-24 hr other alcohols ethylene glycol -+ CNS, CVS, renal findings methanol early: lethargy, confusion late: headache. visual changes, N/V, abdominal pain, tachypnea both produce severe metabolic acidosis with AG and osmolar gap EtOH co-ingestion is protective treatment fomepizole 15 mg/kg IV bolus OR EtOH 10% IV bolus and drip to achieve blood level of 20mmoi/L - EtOH loading may be done PO consider folic acid for methanol and pyridoxime for ethylene glycol- both help reduce conversion to active metabolites urgent hemodialysis required other abnormalities associated with alcohol: hypomagnesemia, hypophosphatemia, hypocalcemia, hypoglycemia, hypokalemia
....
,,._ , ________________
Thiamine Niacin Falalll Glycopn
eo..man Ddciencilla
Potassium
� � � � � � � � � � � �
Gastrointestinal Abnonnalities
gastritis common cause of abdominal pain and GI bleed in chronic alcohol users pancreatitis serum amylase very unreliable in patients with chronic pancreatitis, may need serum lipase hemorrhagic form (15%) associated with increased mortality fluid resuscitation very important hepatitis AST/ALT ratio >2 suggests alcohol as the cause as well as elevated GGT with acute ingestion
ER50 Emergency Medicine
Toxicology
Toronto Notes 2011
peritonitis/spontaneous bacterial peritonitis occasionally accompanies cirrhosis leukocytosis, fever, generalized abdominal pain/tenderness paracentesis for diagnosis (common pathogens: E. coli, KlebsieUa, Strep) GI bleeds most commonly gastritis or ulcers, even if patient known to have varices consider Mallory-Weiss tear secondary to retching often complicated by underlying coagulopathies minor - treat with antacids severe or recurrent - endoscopy
Miscellaneous Problems
rhabdomyolysis presents as acute weakness associated with muscle tenderness usually occurs after prolonged immobilization increased creatinine kinase (CK), hyperkalemia myoglobinuria - may lead to acute renal failure treatment: IV fluids, forced diuresis (mannitol20% 15 mglkg IV over 30 min) increased infections - due to impaired host defenses, immunocompromise, poor living conditions
Disposition
before patient leaves ED ensure stable vital signs can walk unassisted fully oriented offer social services to find shelter or detox program ensure patient can obtain any medications prescribed and can complete any necessary follow-up
Approach to the Overdose Patient
-----------------
,, ,
History
who? age, weight, underlying medical problems, medications what? substance and how much when? time since exposure determines prognosis and need for decontamination, symptoms since how? route why? intention, suicidality
� � � � � � � � � � � � � � � � � � �
Suspect OVIIniDH when: Altered level of consciousnessfcoma Young patient with ln-1hrntaning arrhythmia Trauma patient Bizarre or pUlZiing clinical prasantlllion
Physical Examination focus on: ABCs, LOC/GCS, vitals, pupils Principles of Toxicology
4 principles to consider with all ingestions I. resuscitation (ABCs) II. screening (toxidrome? clinical clues?) III. decrease absorption of drug IV. increase elimination of drug
ABCs of Toxicology
basic axiom of care is symptomatic and supportive treatment address underlying problem only once patient is stable A Airway (consider stabilizing the C-spine) B Breathing C Circulation
Dl
Drugs
ACLS as necessary to resuscitate the patient universal antidotes D2 Draw bloods D3 Decontamination (decrease absorption) E Expose Oook for specific toxidromes)/Examine the Patient F Full vitals, ECG monitor, Foley, x-rays, etc. G Give specific antidotes, treatments Go back and reassess Call poison information centre Obtain corroborative history from family. bystanders
Toronto Notes 2011
Toxicology
Emergency Medicine ER51
01 - Universal Antidotes
treatments that will not harm patients and may be essential
Oxygen
do not deprive a hypoxic patient of oxygen no matter what the antecedent medical history (ie. even COPD with COz retention) if depression of hypoxic drive, intubate and ventilate exception: paraquat or diquat (herbicides) inhalation or ingestion (oxygen radicals increase morbidity)
Glucose
give to any patient presenting with altered measure blood glucose prior to glucose administration if possible adults: 0.5-1.0 glkg (1-2 mL/kg) IV ofD50W children: 0.25 glkg (2-4 mUkg) IV of D25W
we
.....
,,
Thiamine {Vitamin 81) 100 mg IVliM to all patients with IV/PO glucose
a necessary cofactor for glucose metabolism, but do not delay glucose if thiamine unavailable to prevent Wernicke-Korsakotf syndrome must assume all undifferentiated comatose patients are at risk
� � � � � � � � � � � � � � � � � � �
D.W.ncy Alcoholics
Po!MHtio111 at Iiiii fllr Thilllline
AnoriiXicl
H'1J)81'81118Sis of pregnancy
Malnutrition lllatn
Naloxone (central Jlreceptor competitive antagonist, shorter t 112 than naltrexone)
antidote fur opioids: administration is both diagnostic and therapeutic (1 min onset of action) used fur the undifferentiated comatose patient loading dose adults 2 mg initial bolus IV/IM/SUSC or via ETT (ETT dose= 2-2.5x IV dose) if no response after 2-3 minutes, increase dose by 2 mg increments until a response or to
Admilistnllion of naloxone can cause
opillle wilhdniWIII in chronic usm. Minor withd111Wl11 may present as lacrimation, lhinonilH, dilphomil, yawning, piloerection, ffrn, and lllchyl;llrdill. SevenJ withcnwal may pmant as hat and cold fllllhn, arthnllgial, myalgiu, N/V, and abdominal CRIIIPI.
max10mg
known chronic user, suspicious history, or evidence of track marks, give 0.01 mglkg
child
0.01 mglkg initial bolus IV/IO/ETT 0.1 mg/kg if no response and narcotic still suspected to max of 10 mg maintenance dose may be required because half-life of naloxone (30-80 mins) is much shorter than many narcotics hourly infusion rate at 2/3 of initial dose that produced patient arousal
02 - Draw Bloods
essential tests (see Table 24) CBC, electrolytes, BUN/creatinine, glucose, INRJPTT, osmolality ABGs, measure 0 2 sat acetylsalicylic acid (ASA), acetaminophen, EtOH levels potentially useful tests drug levels - this is NOT a serum drug screen
Ca,Mg,P04
protein, albumin, lactate, ketones, liver enzymes, CK - depending on drug and clinical presentation
Serum Drug Levels
treat the patient, not the drug level negative tox screen does not rule out a toxic ingestion - signifies only that the specific drugs tested were not detectable in the specimen specific drugs available on general screen vary by institution; check before ordering urine screens also available (qualitative only)
ER52 Emergency Medicine
Toxicology
Toronto Notes 2011
Table 23. Toxic Gaps (see also Neohrologv)
....
'.. ,
� � � � � � � � � � � � � � � � � � �
- (2 Na + glucose + urea)- pl8SIIIl
Normal POG < 10 m0sm/11ci
P1111111 Clsmollr Bap(POG)
o.molllrity
.... .-----------------,
Ani1111 Gap (AG) � � Na- Cl - bicarb Normal AG S12 mEqll
'..,
METABOUC ACIDOSIS lncrtllllld AG: "MUDPILES CAT'(* � � toxic) Melhlllol* Uremia Diabetic kl!toacidosis/Starvalion kl!toacidosis Phanftrmin*/Pareldahyda* Isoniazid. Iron, Ibuprofen Lacliltll (anything that caU&85 seizurv& or shock) Ethylene glycol* Salicylat&s* Cyanide, carbon monoxide* Alcoholic Ketoacidosis Toluene, theophyllile*
Increased POG: "MAE DIE" (if it ends in .or, it will likely 1' the POGI Methi11ol Acetone
Ethanol
Diuretics (glycerol, mamitol, sorbitol) Isopropanol Ethylene glycol
Nota: nonnal osmolll' gap does not rule out toxic � only an elevated gap is helpful
lncreaad Oz saullion gap Carboxyhemoglobin
� � � � � � � � � � � � �
� � � � � � �
DecreuedAG Elaclrolyla ii'Ttalanca (increasad N..x/Mg) H-,poalbuminernia (50% fall in albumin -5.5 mmoll d8Cillasa in the AG) U. Br elevation Pareproteins � � � � � � myeloma)
NormaiAG High K: pyelonephritis, obstructive nephropathy, renal tubular acidosis (RTA), IV, TPN Low K: small bowel losses, acetazolamide, RTA I, II
� � � � � � � � � � � � � � � �
Table 24. Use of the Clinical Laboratory in the Initial Diagnosis of Paisoning
Test ABG Finding Hypovenlilation ('I' pCOzl Hypervanlilation (II; pCCJ21 Selected C111111 CNS depressanls (opioids, sedaliv&-hypnotic agenls, phencrthiazines, EtOH) Salicylat&S, CO. other asphyxianiS "MUDPILES CAT': see "Melabolic Acidosis" above Digilllli& glycosides, fluoride, pDtassium Theophylline, caffeine, beta-edrenergic agents, soluble barium salts, diuretics, insulin Oral hypoglycemia agenls, insulin, EtOH, ASA "MAE DIE": sea "Toxic Gaps" above
Bacttolytes
1' � � � � � � � � � � � metabolic acidosis
Hyperkalemia Hypokalemia
GIIICOie
� � � � � � � � � � � �
Osmolality and OmuGIP
ECG
Bevatad osmolll' gap Wide ORS con-Pax Pllllonged QT interval Abiovenbicular black
TCAs, quinidine, crthar clil$5 Ia il'ld lc il'ltiarrhythmic agents � � � � � � � � � and related antiarrlrythmics, terfenadine, astemizale,
antipsychotics Ca anlagonists, digitalis glycosides, phenylpropanolamile "CHIIES": Calcium, Chloral hytele, CCI. Heavy metals, nn, Potassium, Enleric COBII!d Salicylates, and some fnn!ign bodies
Abd0111i111l X-ay Serum .Acllllminaph1111
Radiopaque pills or objects
Bevated level (> 140 mWL or May be only sign of acebmilophen poisonilg 1DOD !lii1Dil4 hours afler ingestion)
D3 - Decontamination and Enhanced Elimination
Ocular Decontamination
saline irrigation to neutralize pH; alkali exposure requires ophthalmology consult
,,..-----------------, ,
Sullltl- NOT AdlorbMI by
Actlvatad CIIIICOII
Dermal Decontamination (wear protective gear) remove clothing, brush off toxic agents, irrigate all c::xternal surfaces Gastrointestinal Decontamination
single dose activated charcoal (SDAC) (see Table 27 for drug toxidromes that are treated with charcoal) adsorption of drug/toxin to AC prevents availability contraindications: caustics, SBO, perforation dose: lOglgdrugingested or lglkg body weight odourless, tasteless, prepared as slurry with H 2 0 whole bowel irrigation 500 mL (child) to 2000 mL (adult) of polyethylene glycol solution/hour by mouth until clear effluent per rectum start slow (500 mL in an adult) and aim to increase rate hourly as tolerated indications awake, alert, can be nursed upright delayed release product drug/toxin not bound to charcoal drug packages (if any evidence of breakage -+ emergency surgery) recent toxin ingestion
Lilllium Iran
Alcohols
Lelld Caustics
Toronto Notes 2011
Toxicology
Emergency Medicine ER53
contraindication& evidence of ileus, perforation, or obstruction surgical removal in extreme cases indicated for drugs that are toxic, form concretions, or cannot be removed by conventional means no evidence for the use of cathartics (or ipecac)
EXTRA-CORPOREAL DRUG REMOVAL (ECDRJ
Urine Alkalinization may be used for: ASA, methotrexate, phenobarbital, chlorpropamide weakly acidic substances can be trapped in alkali urine (pH >7.5) to increase elimination
Multidose Activated Charcoal (MDAC)
may be used for: carbamazepine, phenobarbital, quinine, theophylline for toxins which undergo enterohepatic recirculation removes drug that has already been absorbed by drawing it back into GI tract various regimens: 12.5 g (1/4 bottle) PO q1h or 25 g (1/2 bottle) PO q2h until non-toxic
Hemodialysis
indications/criteria for hemodialysis toxins that have high water solubility, low protein binding, low molecular weight, adequate concentration gradient, small volume of distribution (Vd) or rapid plasma equilibration removal oftoxin will cause clinical improvement advantage is shown over other modes of therapy predicted that drug or metabolite will have toxic effects impairment of normal routes of elimination (cardiac, renal, or hepatic) clinical deterioration despite maximal medical support useful for the following blood toxins: methanol ethylene glycol salicylates lithium phenobarbital: 430-650 mmoUL chloral hydrate (-+ trichloroethanol): >200 rnglkg others include theophylline, carbamazepine, valproate, methotrexate
E - Examine the Patient
vital signs (including temperature), skin (needle tracks, colour), mucous membranes, pupils, odours and CNS head-to-toe survey including C-spine signs oftrauma. seizures (incontinence, "tongue bitint(. etc.), infection (meningismus), chronic alcohol/drug abuse (track marks, nasal septum erosion) mental status
Tabla 25. Specific TOllidromes
Tllllidrama Ovanla Sip IIIII SVnJpiDIII
Hyperthermia Dlated pupils Dry skin Vasodlation Agitationlhalucinations Ileus Urinary ratantion "Hot as a hare" "Blind as a bat" "llry asa bona "Red as abeat" "Mad as a hatter" lhe bowel and bladder lose thllir tone and 111& ha.t goss on alone" Examples ul Drup Antidepressants (e.g. TCAs) Cyclobenzalfine (FiexeriPI Cll'oamazepina Antihistaminas {a.g. diphenhydramine) Antiparkinsonians Antipsychotics Antispasmolics Beladonna alkllloids (e.g. atropinal
Antichalinergics
Taclryardia Chalnqics
"OUMBELS" OiaphDI8Sis, Oianhaa. Decreased blood prvssure Urination Miosis
Bronchospasm, Bronchonhea, Bradyt:ll'dia Emesis, Excitation of skeletal muscle Lacrimation Salivlltion, Seizures
Anticholinasteresas: physostigmina,
Natural plants: rooshrooms. tru111l81 Hower
Insecticides {organophosphates, carballlllles) Nerve gases
Extrapyr1111idll
Dysphonia, dysphagia Rigidity and tremor Motor restlessness, crawling sensation (llkathisial Constant mavamants (dyskinesia) Dysmnia (muscle spasms,llryrcjospasm. trismus, oculogyric crisis, torticallisl
Major tllllquilizers Antipsychotics
ER54 Emergency Medicine
Toxicology
Toronto Notes 2011
Table 25. Specific Toxidromes (continued)
TIIJiid1011111
Hemaalabin
Owenlllse Signs and Symptoms
Increased respiratory nrte Decreased level of consciousness Sei211111S Cyanosis unresponsive to � � Lactic acidosis Hypothermia Hypotension Respiratory depression Dilated or constricted pupils (pinpoint in opiate OD) CNS depnMion lncr&ISed � � � � � � � � CNS &KCitation (including seizures) Tachyclldia, hypertension Nausea and vomiting Diaphoresis Dilated pupils Carbon monoxide poisoning � � � � Drug ingestion (methemoglobin, sulfmethemoglobin)
� � � � � � � � � � � � �
Dnnaements
EtDH Benmdiazepiles Opiates (morphine, heroin, etc.)
Barbiturates
GHB Amphetamines, caffeine, cocaile, LSD, PCP Ephedrine and other decongestlrltl Thyroid hormone Sedatives, EIOH withdrawal
Serotonin Syndl'llllle
Mental stlltus changes, autonomic hyperactivity, neuromuscular abnormalities. hyperthermia. diarrhea, HTN
MAOI, TCA. SSRI, opiate analgesics Cough medicine, weijrt reduction medications
Nlllt: JSA �
� � � � � � � lnl hypoglycamia mimic syn'llllhamil1111ic: lllxidroma
G- Give Specific Antidotes and Treatments --Urine Alkalinization Treatment for ASA Overdose
urine pH >7.5 fluid resuscitate first, then 3 amps NaHC03/litre ofD5W@ 1.5 x maintenance add 20-40 mEq KCIJlitre if patient is able to urinate
Table 26. Protocol for Warfarin Overdose
INR
<5.0 5.1-9.0
Mlnlglllllnt
Cessation of warfarin adminirlrlllion, observation. seriaiiNRIPT
If no risk factoli for bleeding, hold Wilfarin x 1-2 days and reduce maintenance dose
OR Vltlrnil K1-2 mg PO W patient at increased risk of bleeding or fresh frozen plesma (FPP) � � active bleed
9.1-20.0 >20.0
Hold warfarin. Vitamin K2--4 mg PO. seriaiiNRIPT, additional Vrtamin Kif neces511Y or FFP if active bleed FFP 1G-15 miJkg, Vitamin K10 mg rl over 10 min, increase VItamin Kdosing (q4h) if needed
Table 27. Specific Antidotes and Treatments call local poison information centre for specific doses and treatment recommendations
Toxin
Acalllmilop'-
Tl'llllnlnt
Decontsninate (activated chcucoal) N-acetylcysteine
Canlillll'lli111111
OftEn clilically silent; evidence of liverfrenal damage delayed >241n Toxic dose > 200 rngtlg (>7.5 g achJt)
Monitor drug level immediately and 41n post-ingestion; also liver enzymes, INR, PIT. BUN, Cr Hypoglycemia. metabolic acidosis. encephalopathy -+ poor prognosis
ASA
Decontaminelll (activated chcucoal) Ablinize urine; want urine pH >7.5
Monitor serum pH and drug levals dosaly Monitor Klevet mav IIIJiire supplement lor urine alkalinization Hemodialysis may be needed Wintraclllble metabolic acidosis, very high IMis, or end-organ damage (i.e. unable to diul'86e) Special antidotes available. ConsuH Poison lnlormation Centre (PIC)
Antic:holilarvics Blnzudiutpiles
Decontsninate (activated chcucoal) Supportive ca111 Decontsninelll (activated chcucoal) Supportive ca111 Decontsninelll (activated chcucoal) CorJSider � � � � � � � � or high dose insulin
jl-llloc:bn
� � � � � � � � � �
� � � � � � � � � � � � � � � � � (HDIE)
Calcium Channel Blcx:bn
� � � � � 1-4 gof 10'1o sol'n rl if hypotensive Atropine or isopruterenol if severe Other: HIJE inotropes or aggressive supportive lhe111py
()der ECG. electrdytes (especially Ca. Mg.. Na. IQ, gb:agon
(2-5 mg)
mav help
Cyanide
Cyanide antidota kit or hydroxycoballlmin
Toronto Notes 2011
Toxicology
Emergency Medicine ER55
Table 27. Specific Antidotes and Treatmentscall local poison information centra far specific doses and treatment recommendations (continued)
TDJdn Digllllil
Tnlltment DecontaminaiB (activlt&d � � � � � � � � � � Digoxin-specific Ab fragments
16-20 vials IV Wacute; 3-6 Wchronic 1 vial (40 mg) neutralizes 0.5 mg oftoxil
Censidendions Use for lile-1hrsat&ning anhythmias unresponsive Ill conventiona11herapy, 6hr serum digoxin >19 nmol/1., initial K
>5 mM, ingestion > 10 mg � � � � � � � � >4 mg (child) Common llllhythmiu include VFib, VTach, and conduction blocks
Aclllll Dystanic Rxn BenziJOpina: 1-2 mg IMIIV then 2 mg PO x3 days OR Diphanhylhmina 1-21111111. then 25 mg PO qid x 3days
Benztropine (Cogantin111) has euphoric alfact and potantial
for libuse For unfrllctionated heparin overdose only Glylnride carries hips! risk of �
� � � � � � � � among oral
Heparin
Pro1amine sulfate �
� � � mg IV
Insulin/ Glucose IVJPWNG lllbe Oralllypaglyl:emic: Glucagon: 1-2 mg IM Iff noacce&1illl �
� � � � � �
Consider octreotide lor oral � � � � � � � � � � � (5!HOO 1111 SC q&h) in these cues; consun local PIC Hypoltftemia vefY common in childlal Mouthwash =70% EtOH; perfumes and colops =
4!).Wl(, EtOH
� �
Thiamine 100 mg IM/IV Manage airway and circulltoly suppot
Order serum EtOH level and glucose level; treat glucose level appropriately E111anol (1 0%)1 0mlotg over 30 min, then 1.5 mlo'll orlomepizole (4.fllelhylpyrazole) 15 rr111V load owr 30 min, 1han 10 IJIIVkg q12h
CBC, elec:lnllytes, gU:ose, ethanol level Consider hemodialysis
CO Poi10ning
See ER46 See ER51
Aggressive supportive care � � � � � boii.IS for wide DRS/seinlrss
Opiaidl
TCAI
Fluiii8ZI!nil antidote contraindiCided in combined TCA and benzodimpine overdose Also consider cardiac and hypotension support, gastric dacon1llmination, ii8inllll control lntmlipid 1henvf (consun loclll PIC)
� � � � � � � CK; tllllt rhllbdornyolysis wi1h high flow fluids
MDMA
Decontaminl1e (activlt&d � � � � � � � � � � �
supportive care
Decontaminate (activated � � � � � � � � � � if orsl
Aggressive supportive care
P-blockers me contraindicated in acute cocaine taxicily
Disposition from the Emergency Department
methanol, ethylene glycol delayed onset, admit and watch clinical and biochemical markers TCAs prolonged/delayed cardioto:xicitywarrants admission to monitored (ICU) bed if asymptomatic and no clinical signs of intoxication: 6 hour ED observation adequate with proper decontamination and no ECG abnonnalities sinus tachycardia alone (most common finding) with history of OD warrants observation in ED hydrocarbons/smoke inhalation pnewnonitis may lag 6-8 hours consider observation for repeated clinical and radiographic examination ASA, acetaminophen ifborderline level, get second level2-4 hours after first for ASA must have at least 2levels going down before discharge (3 levels minimum) oral hypoglycernics admit all patients for minimum 24 hours if hypoglycemic observe asymptomatic patient for at least 8 hours
Psychiatric Consultation
once patient medically cleared, arrange psychiatric intervention if required beware - suicidal ideation may not be expressed
ER56 Emergency Medicine
Psychiatric Emergencies
Toronto Notes 2011
Psychiatric Emergencies
Approach to Common Psychiatric Presentations
see Psychiatry before seeing patient, ensure your own safety; have security/police available if necessary
....
,"
� � � � � � � � � � � � � � � � � �
ICily FanctiDM af Elllllrgency ITtohilltrlc ARIIHIIIIIIIt 1. Is !he patient medicelly stable? 2. Rule out medical cause 3. Is P"(Chialric � � � � � � � needed? 4. Are !here safely issues !SI, HI)? 5. Is patient certifilble? (must demanstral8 risk � � � � � � � � � � list)
and apparent mental illness [future
list))
History safety assess suicidality: suicidal ideation, intent, plan, lethal means, past attempts assess homicidality: access to weapons, intended victim, history of violence command hallucinations identify current stressors and coping strategies mood symptoms: manic, depressive anxiety: panic attacks, generalized anxiety, phobias, OCD, PTSD psychotic symptoms: delusions, hallucinations, disorganized speech, disorganized or catatonic behaviour, negative symptoms (affective flattening, alogia, avolition) substance use history: most recent use, amount, previous withdrawal reactions past psychiatric history, medications, adherence with medications medical history: obtain collateral if available Physical complete physical exam focusing on: vitals, neurological exam, signs of head trauma, signs of drug toxicity, signs ofmetabolic disorder mental status exam: general appearance, behavior, cooperation, speech, mood and affect, thought content and form, perceptual disturbances, cognition (including MMSE if indicated), judgment, insight. reliability Investigations investigations vary with: age, established psychiatric diagnosis vs. first presentation, history and physical suggestive of organic cause as indicated: blood glucose, urine and serum toxicology screen, pregnancy test, electrolytes, TSH, AST/ALT, bilirubin, serum creatinine, BUN, osmolality blood levels of psychiatric medications CT head if suspect neurological etiology LP if indicated
Acute Psychosis
It'
Fl8tures 1hat � � � � � � � � OI'QIIIic
Etiology Age >40 yellr$ old Babbling {incaherenl speech or speech difficulties) Concerning vital signs Disorientation Emotional lability FluctUBiing course Global impainnent of cognitive function
Differential Diagnosis primary psychotic disorder (e.g. schizophrenia) secondary to medical condition (e.g. delirium) drugs: substance intoxication or withdrawal, medications (e.g. steroids, anticholinergics) infectious (CNS) metabolic (hypoglycemic, hepatic, renal, thyroid) structural (hemorrhage, neoplasm) Management violence prevention remain calm, empathic and reassuring ensure safety of staff and patients, have extra staff and/or security on hand patients demonstrating escalating agitation or overt violent behavior may require physical restraint and/or chemical tranquilization (see Violent Patient, ER57) treat agitation: whenever possible, offer medication to patients as opposed to administering with force (helps calm and engage patient) benzodiazepines -lorazepam 2 mg PO, IM or SL antipsychotics - olanzapine 5 mg PO, haloperidolS mg PO/IM treat underlying medical condition psychiatry or Crisis Intervention Team consult
Headaches Immodesty
Just sbrted (sudden onset) K Lass of consciousness Movanant abnormalities (tremor, atllxia. psychomotor rwlanlation) Neurological findings (fol:al) 01her lbnarmalitin an physicaiiXIm Perceptions (visual hallucinations)
Toronto Notes 2011
Psychiatric .EmergendesJCommon Pediatric ER PresentatiOlUI
Emergency Medicine ER57
Suicidal Patient
Epidemiology
attempted suicide F>M, completed suicide M> F second leading cause of death in people <24 years
......_._
� � �
, ________________,
� �
PS24 for certiliclllian
cansidendiana
Management
ensure patient safety: close observation, remove potentially dangerous objects from person and room assess thoughts (ideation), means, action (preparatory, practice attempts), previous attempts admit if there is evidence of intent and organized plan, access to lethal means, psychiatric disorder, intoxication (suicidal ideation may resolve with few days of abstinence) patient may require certification if unwilling to stay voluntarily do not start long-term medications in the emergency department psychiatry or crisis team consult
High m.lc l'ltilnt.
���
Sex= male
SADPEISDNS
Aa >45 yi8I'S old Depression
Previo\IS attempts
Ethanol use
lllionallhinki1g lo" Suicide in hmily Organized plan
Sarious illna"
Violent Patient
Differential Diagnosis
rule out lethal organic cause (e.g. EtOH, drugs, and head injuries)
No spousa, no suppan systJm
Prevention
be aware and look for prodromal signs ofviolence: anxiety, restlessness, defensiveness, verbal attacks try to de-escalate the situation: address the patient's anger, empathize
Restraints
pharmacological often necessary- may mask clinical findings and impair exam haloperidol5-10 mg IM (be prepared for dystonic reactions, especially with multiple doses of neuroleptics over a short period) + lorazepam 2 mg IMJIV look for signs of anticholinergic overdose first (see Table 25) benzodiazepines best option if suspected substance-induced violence physical present option to patient in firm but non-hostile manner sufficient people to carry it out safely restrain supine or on side; preferably 4-point restraints, never less than 2-points (opposite armand leg) suction and airway support available in case ofvomiting once restrained, search person/clothing for drugs and weapons
Common Pediatric ER Presentations
Modified Coma Score
Table ZB. Modified GCS
Modified GCS lor llfants
f.yl Oping 4 - spontaneously
3-tospeech 2-topain 1- no response
Vlrbllllllspanse 5- COOS, babbles 4- inilllble ay 3 - cries to pain 2- moans to pain 1 - no response
MDIDr Response 6 - nonnal, spontaneous movement 5 - witlmws to 111uch 4- WillmWll to pail
3 - decorticate flexion 2 - decerebrate axtension 1- no 1111ponse
Any infant < 1,_ of age witll 1 llfV&,
baggy IICI!IIp hematoma requires CI
Modified GCS lor Clildn1n <4 years Vlrbllllllspanse 4- spontaneously 5- oriented, � � � � � � � speaks, interacts 3-tospeech 4- confused speech, disoriented, cnolable 2-topain 3 - inappropriate words, not consolable/aware 1- no response 2- incomprehensible, agitated, restless, not aware 1 - no response
f.yl Oping
Mlllllr Response 6 - nonnal, spontaneous movement 5 -localizes pain 4 - witlmws to pain 3 - decorticate flexion
2 - decerebrate extension 1- no rasponse
ER58 Emergency Medicine
Common PedJatric ER Preaentationa
Toronto Notes 2011
Respiratory Distress
..... ,
...-----------------,
see also Pediatrics
In Pllfilllric reapir.tory dim.-. mpt aiiOru.. olll: AnaphyiiiXis Foreign body
Pneumonia
Bronchiolitis
History and Physical Examination infants not able to feed, older children not able to speak in full sentences anxious, irritable, lethargic - may indicate hypoxia tachypnea >60 (>40 if preschool age, >30 if school age), retractions, tracheal tug see Pediatrics Table 1 for age specific vital signs pulsus paradoxus wheezing, grunting, vomiting
Tabla 29. Stridorous Upper Airway Disaasas: Diagnosis
fllluN
Croup
D.5-4 Days
Low grade
� � � � � � � � � � �
Bacterial Tracheitis
Aalllulvnl
Pradrome
5-1 D
Hrsto days High Exudates in trlchea
2-8
Minutes to In Hijl
� � � � � � � � �
T.,..el'ltll'e
llldiogl'lplly
Etiology BerkyCaugh
Parainlluenm
s_ illlreus/GAS
Yes No
Yes
Yes
H. lit type b No
Yes
Yes
Drooling
Appear Toxic
Ya6
Yes Yes
No No No
lntulmion? ICU?
Antililllics
NDTE:
Yes
Ya6
No oral exam
1Now rare with Hib vaccine in common use
..... ,
...-----------------,
Admlsllon Crflllrlll far C1'011p Stridor at rast or lignilicent respiramry distress Relapse after 2 doses Df epinephrine or incampl111 mpons1 Co-morbid respinrtory or underlying
condition
..... ,
� � � � � � � � � � � � � � � � � � � �
Admi11ion Critlrlll far Adln111 Re1piratory diltn!H &In after ltaroidl Ventalin required > q3h Naod for supplamantal DX'(ilan Consider I pnrvio1111 ICU ldminion
management of croup (laryngotracheitis caused by parainfluenza m-uses) humidified 0 2 should not be given (no evidence for efficacy) racemic epinephrine q1h x 3 doses, observe for 'rebound effects' dexamethasone x 1 dose consider bacterial tracheitis/epiglottitis if unresponsive to croup therapy management of bacterial tracheitis start croup therapy, but may have poor response usually require intubation, ENT consult, ICU start antibiotics (e.g. cloxacillin), pending C&S management of epiglottitis 4 D's: drooling. dyspnea, dysphagia, dysphonia + tripod sitting do not examine oropharynx or agitate patient immediate anaesthesia, ENT call- intubate then IV fluids, Abx, blood cultures management of asthma supplemental 0 2 if sats <90% or Pa02 <60% bronchodilator therapy: salbutamol (Ventolin) 0.15 mg!kg by masks q20 minx 3 add 250-500 1!8 ipratropium � � � � � � � � � � � to first 3 doses salbutamol give corticosteroid therapy as soon as possible after arrival (prednisolone 2 mg!kg, dexamethasone 0.3 mg/kg) MgS04 if critically ill, not responding to inhaled bronchodilators, steroids; give IV bolus, then infusion IV � � � � � � � � � � � � if critically ill and not responding to above
..... ,
..
Febrile Infant and Febrile Seizures
FEBRILE INFANT
see also Pediatrics for fever >38C without obvious focus <28days
}-----------------,
Rochlltar Critllril far Fellrile Infants Age 2WO Dap Old Non-toxic looking Prsvio1111ly wall (>37 weeu GA, horne willl mother, no hyparbilirubinamia, no prior antibiotics or hospitalizations, no chronic/ Lnllrlying illnanl No skin, soft tissue, bona, joint, or &ar infection on physical exam wac sooo-1 s,ooo, bands < 1soo; ll'ine <10 WBC/HPF, stool < 5 WBC/ HPF
admit
full septic work up (CBC & � � � � blood C&S, urine C&S, CSF, CXR if indicated) treat empirically with broad spectrwn IV antibiotics 28-90days as above unless infant meets Rochester criteria (see sidebar) >90days toxic: admit, treat, full septic workup non-toxic and no focus: investigate as indicated by history and physical
Toronto Notes 2011
Common Pediatric ER Presentations
Emergency Medicine ER59
FEBRILE SEIZURES see Pediatrics. P52
Etiology children aged 6 months to 5 years with fever or history of recent fever simple vs. complex febrile seizures normal neurological exam afterward no evidence of intracranial infection or history of previous non-febrile seizures often positive family history of febrile seizures relatively well looking after seizure Investigations and Management if it is a febrile seizure: treat fever and look for source of fever if not a febrile seizure: treat seizure and look for source of seizure note: may also have fever but may not meet criteria for febrile seizure Tabla 30. Simpla vs. Complex Fabrila Saizuras
Charsc:tarillic:
Sinple C.....IIX
Durillion
Tp al Seizure
frllquncy
<15min Generalized
>15min Focal features >1 in 24 hours
1 in 24 hours
Abdominal Pain
see also Pediatrics. P41
History nature of pain, associated fever assodated GI, GU symptoms anorexia, decreased fluid intake Physical Examination HEENT, respiratory, abdominal exam including DRE, testicular/genital exam Tabla 31. Differential Diagnosis uf Abdominal Pain in lnfants,/Childrao/Adolascents
Medical
Colic UTI Constipation Gastroenteritis Sepsis HSP (Henoch Schonlein purpura) Inflammatory Bowel Disease HUS (Hemolytic Uremic Syndrome) Pneumonia Strep Throat SCD crisis DICA F111ctional
Surgical
Malrotatim with volwus
� � � � � � � � � �
Necrotizing enterocolitis lncan:ntlld hernia Intussusception
� � � � � � � �
atresia
Appendidis Cholecystitis Pancrartitis Testiculil"tol8iDn Ectopic pregna1cy Trauma Pyloric stsnosis
'llamlll'llar tD lalap an indlx rlupil:iln for chid lhU18
ER60 Emergency Medicine
Common PedJatric ER Preaentationa
Toronto Notes 2011
Common Infections
see also Pediatrics
Tabla 32. Antibiotic Traabnant of Pediatric Bacterial Infections
lnr.:tion
MENINGinS SEPSIS
Neonalal
� � � � � � � � � �
GBS, E. coli, listeria, S. auretl$, Gram-negative bacilli
ampicilin + aminoglycoside {gentamicin or ampicilin + cefotaxime cloxacili1 arisk of S. aureus ampicilin + cefotaxime cloxacili1 risk of S. aureus cefumxime ceftriaxone or celotaxime, � � risk of meningitis
1-3 months
>3 months
Same pathogens as above and below
S. pneumoctJCCUS, H. inlfuenzae type b {>5 yrs), meningococcus
vancomycin. � � penicillin'cephalospom188istant
pneumococci
aTTnSMEDIA 1st line
2nd line
S. pneumonia8. H. inffu8nzJJe type b. M. Catlnhalis
amoxicili180-90 mQI1cg per day
amoxiciln.davutanata {Ciawlin) high dose Clawlinat or ceflroxime or ceflriaxone
Treatment failure
STREP PIIARYNGmS
Group A beta-hemolytic StreptrJcoccu$
penicilirv'amoxicillin or aythromycin {pencilli1 allergy) amoxiciliVampicillin or bimethoprim-sulfamelhaxazole
un
PNEUMONIA 1-3 months 3 months� � � � � � � � � � � � � �
f. coli. Pn1teus, H. itrffuenzae, Pseudomonas. S. S6(JfiJIJhyticu fntenx:occus, GBS
� � � � � � S.
S. �
� � � � � � S.
pneumonia&, C. trat:honlllis, B. p8llussis, � H. inffuenzle
cefumxime macrolide {erythromycin) or ampicillin macrolide
pneumoniae, S. �
�
� inlfuenzae.
ampicilirv'amoxicillin or cefuroxime
ampicilirv'amoxicillin + macrolide or celuroxime +
macrolide
M;cop/8sm& pneumoniee
As above
Child Abuse and Neglect
.... � �
, ...-----------------,
I'Nqntation uf Neglect Failu111 ta thrive, diiValopmanllll dilley lnadequaiB or dirty clothing. poor hygi Child axhibits poor attachment to paran11, no st111ngar lriXillty
see also Pediatrics obligation to report any suspected/known case of child abuse or neglect to CAS yourself (do not delegate) document injuries consider skeletal survey x-rays, ophtho consult, CT head injury patterns associated with child abuse head injuries: tom frenulum, dental injuries, bilateral black eyes, traumatic hair loss, diffuse severe CNS injury, retinal hemorrhage Shaken Baby Syndrome: diffuse brain injury, subdural/subarachnoid hemorrhage, retinal hemorrhage, minimal/no evidence of external trauma, associated bony fractures skin injuries: bites, bruises/bums in shape of an object, glove/stocking distribution ofbums, bruises of various ages, bruises in protected areas bone injuries: rib fractures without major trauma, femur fractures age <1 year of age, spiral fractures oflong bones in non-ambulatory children, metaphyseal fractures in infants, multiple fractures of various ages, complex/multiple skull fractures genitourinary/gastrointestinal injuries: chronic abdominal/perineal pain, injury to genitals/ rectum, STI!pregnancy, recurrent vomiting or diarrhea
Toronto Notes 2011
Procedural Sedation/Common Medications
Emergency Medicine ER61
Procedural Sedation
procedural sedation: the technique of sedative or dissociative agent administration with or without analgesics to induce a state that allows a patient to tolerate an unpleasant or painful procedure while maintaining all protective cardiorespiratory functions (Le. a depressed level of consciousness without loss of a patient's protective airway reflexes) must weigh degree ofpain and expected relief versus risk/complications of sedation and procedure examples of procedures that may require sedation in the emergency department: setting fractures, reducing dislocations, draining abscesses, exploring wounds/ulcers/ superficial infections, endoscopic examination may also be required to reduce patient agitation if imaging is acutely required
Requirements for Safe Procedural Sedation in the Emergency Department airway suitable for safe intubation and ventilation appropriate equipment/personnel available intact and functioning cardiorespiratory and neurological system ideally, NPO for minimum 4-6 hours anesthetic history and drug allergies, including manifestations appropriate IV access, monitoring (oxygen saturation, BP, HR, etc.) informed consent obtained Common Procedural Sedation Medications (titrate to effect) see Common Medications, below
Common Medications
Table 33. Commonly Used Medications
Drug D11ing Schedule 0.51.0 �
� � � � �
lnllc:atiOII
Procedural sedation Procedural sedation
� � � � � � � � �
fantllnyl
midazolam
Very short acting narcotic �
� � � � � � � � � � � � � � � � � �
50 �
�
Short acting benzodiazapine � � � � � � � � � � � � � � � � � � when used with narcotic) Fentanyl and midamlam often used together fur procldlral sedation Short acting Anestheticisedative (complication=apnea, decreased BP) Benzodimpine antagonist NB don't usa in chronic biiiZOdiazapine user Not to be used in fingers, nose, toes, penis. ears
1J11palol
������������
0.25.{).5111Q11qj IV 0.3 mg IV bolus q5min x 3doses
Procedural sedation Revetsal a! procedual sedation Locelanesthlllic Local anesthetic
� � � � � � � � � � infections
lidocaine with api lidocaine w/o api l'olysporin8 morphine
max7 mg./kg SC
max 5 mg/kg SC
� � � � to aff&ctad araa bid-tid
15-30 mg PO qll-12h 0.1.n.2111Q11qj max 15 mg IV q4h 12 tabs PO q6h pm 325-650 mg PO q4-6h pm 1-2 tabs PO q4-6h pm
Mild to modaralll acute/chronic pain Prescribed in combinlllion with NSAIDs or acetaminophen Moderate pain colllrDI Pain control Pain control Mild to modaralll acuta pain AnalgBSia and anti-ilfllrnmatory prupertiBS To treat/prevent Wemicke's encephalopa1hy
Gl and constipation side ellects DO NOT CRUSH, CUT or CHEW Oxycodane + acetaminophen Max 4 gacetaminophen daily Max 4 g daily Max 4 gacetaminophen daily
Percocet 10,1'3258
acetaminophen Tylenol #38 Ibuprofen 1hiamine
ZOO.BDO mg PO tid pm max 1200 mgld
Wernicke's encephalopathy: 100 mg IV/1M � � � � � � � � then 5G-1 00 mg IM/IV ODJl'O x3d anxiety: 2-1 0 mg PO tid/qid alcohol withdrawal: 10-20 mg POJ1V q1h tibated to sig!Wsymptoms anxiety: 0.5-2 mg POIIIINIV q6.ah status epilepticus; 4 mg IV rapaat up to q5min status epilepticus: see Table 13 anaphylaxis: 0.1.{).5 mg IM; can repeat q1 G-15min
Caution use in pregnancy
diazepam
Anxiety
Alcohol withdrawal
lorazepam
Anxiety
Status epiepticus Status apiepticus
Anaphylaxis Begin maint..ance dose 12hr liter loading dose Continuous ECG. BP moritoring mandatory Max 1mg/dose
phanyt!lin epinephine
ER62 Emergency Medicine
Table 33. Commonly Used Medications (continued)
Drug salbllllmol ipratropium bromide
� � � � � � � � � � � � �
Common MedicationsJR.eferenc:es
Toronto Notes 2011
Dosing Schedulll 2 IXIIf1 inhaled q4-6h (4yrs) max 12 pull!/day 2-3 pulls inhaled tid-qid, max 12 pufk/day
lndicllians Asthma Asthma
Ca11menls Caution with cardiac abnormalities Contraindicated with peallll/soy allergy Caution with narrow-angle glaucoma
acute angina: 0.3-0.6 mg SL q5min. OR 5 � � � � � � � � IV inCilNISilg
by 5-20 �
� � � � � � q3-!imin
An gila Al:uteMI
Pain control Cardiac pravanlion
Nllt to be used with lither illtt-hypertensives
ASA
� � � � � � � � � � (metoprclol)
325-650 mg PO q4h max 4W'day stroka.IMI risk: 81-325 mg PO OD
enoxaparin insulin
5 mg slow IV q5rnin x 3 if no contraildications 1mglkg SC BID
bolus 5-10 U(0.2 UAcg) then 5-1 0 U (0.1 IJAcg) per hour
AculeMI AculeMI
Hyperglycemia Monitor blood glucose levels Consider Kreplacement. also measure blood glucose lavals bal0111 administration Monitor 1or electrolyta imbalances Monitor with Parkilson's; results in CNS depression
glucose furosemide � � � � � � � haloperidol naloxone
activated charcoal
0.5-1.0 glkg � � � � � � � � IV of D50W CHF: 40--80 mg IV HTN: 10--40 mg PO BID 2.5-5.0 mg POIIM initial eflective dose 620 mw'day 0.5-2 mg or 0.010.02 mwq initial bolus IVJIMISI/SC or via ETT (2-2.5x IV dose), increase dose by 2 mg until responsl!/max 10 mg 3G-100 gPO in 250 ml H 20
Hypoglycamill"DKA CHF HTN
Psychosis
Comatose patient Opioid overdose Reversal in procedural sedation Poisoninw'overdose
References
Boob Cecifs llnentials of Medicine 7th ed. And!eoiTE. Clrpede! CJ. Griggs IK:, Benjamin LJ. Saunders, 2007. Clinical Anasllialill4th lid. Beruh PG. Cullin BF. SID ailing RK. Philadelphia: lil!lhmt. 2001. Clinical prac:eiMes in emergency medicine. 3rd ed. Aoberbi JA and Hedges JR (ed). WB Suders Co, 1198. Emargancy macicill: Acompralwlsiw SUJdy IPde, 5th ad. Tinlillllli JE and ICIIan GE !adl- McGIIW-Itilll'lofaasillllll � Emsrvsncv Macicill 011 Cal lain. Salal. Mclimw Hil. 2004. Emervencv Macicillllecllll Wood1, WA et al (ad). Uppncotl:Wiliams 111d � � � � � � � � 2000. Physiologic and Pllarn-.cologic Bues !I Anesthesia. Collins VJ. Pennsylvania: Willms &Wilkils, 1996. Pmctical QJida to tha Care oftha Medical Patient. 5th ad. Farri Flad). Mosby. 2001. � � � � Medical Pharmlcology. Klllnt H, � � � � � � � � � Wll Naw 'foR:: OxfOTd Uniwrsity l'niA, 1998. Aan's Elrwglncy Mlldicina: ConCIPIIIlld Clinicall'nlctict. 5th Ill. Marx lid). Mosby 2002.
� � � � � � 1999.
JuniiArticl18 AmariCill collaIll of emargarv:y � � � � clilical polcyfor tha iritialapproach ID patianll � � � � � � � � � � � Nth altarad IIWIIIIIIIIIUs. Alln Emlla Mad Feb 1999; 33:251-280 llll:hrnml LM, Kall E, 1*1 MT. Sllu111 J. tar Riel G. AccUillcy of � � � � � � � � � � � Nlas ID Kludt fnlctum ofthl.ndl and nid-loot: sys!lrnltic lllriaw. BMJ 2003; 32611386):417. Chu, P. Blunl Abdaninal Tnauma: current conc:ep1l. Clmnt Orlhopadics 2003; 17, 254-258. Dlr!llll P. Walllce C. Jones AI.. An evidence bued flowchart ID guide the menagemem of acute � � � � � � laspiin) overdose. Emerv Med J. 2002; 19;20&-209. Ellioll WJ. Hypnnsiw.wgancies. Crit C.Cin. 2001; 1712):435-51. Eplllin M. � � � � � � � � � � 1111111118mBnl!l hypartanlsiwl � � � � � � Cil Comarslunl. 1191; 211 ):41-54. Ftm-an A. Re!Jorting It pshat wounds by dilctars in emergency depirtmen1s: Atilly ora 111111? SDI!E legal and e11ii:al issues suii!MIIIrG breakDJ patient confidentiality. Emerg. Mad. J. 2005; 22;8"6 Kile JA. Mildiell AM. Kabrliel C. Richman I'll. Colmey 11.1. CiiicalcriWriaiD prewtd Unneces511'f diagnostic tesling in eJ111i1V1i11:Y department patienls Nth suspeclldpulmonary mbiilm. J Thromb Hlemost 2004; 218):1241-55. Munro P. Managamanl of eclln1lSia in tha accidanl and am11111sncv depwlment Emarg. Mild. J. 2!Dl; 17;7-11. Au111l JA llal. Vasoprelsin \IIIIIIIIIIDIIJiinaphril infusion in pllianll with septic lhock. NEJM 2008; 35819):877-87. Slbltina MS alai. Addition It lilpiqr.IID aspirin 111d fibrinolytic thllllf'l'lor rnyocanlill infln:tian with ST-siiiJI*II aiMtion. NEJM 2005; 352(12):1171-.'19. StiaiiiG eta!. The Canlldiiiii;T Head Rule for patient. Nth llilorhelll � � � � � � LII1Cfl2001; 357[9266):1391-&. StieiiiG etal. The Canlldilll C.spine Nlefor...,hy in alert and sllble trauma patients. JAMA 2001; 286(15):1841-8. Varon J, Marik P. Tha Diagnosis and menlglll*lt of hyparllnsiw crilas. Chast. 2000; 11811):21 4-27. VidiDG. Emervencr room mngement It hype!tlnsive urvencies and emervencies. J Clin llypeltens. 2001; 3131:15U4. WlnllnC llal. EvUJIIion and managamant offabrilsailuras in 1hl out-lt-IIIJIIIitlland lllllllllancv dlpartmentllllings. Alln &r.g Mad. 2003; 41;21!1-222 Wall PS. And&!"$011111. RodGer M. 11111. � � � � � � � � � � � � � � � � � � clniCIII modal to clt8QO!iz9 patianl$ problbiity of pulmoniiY ambolitm: incrlirG the models utiily with the � � � � � � � cl-dimer. Tlwomb Haemost. 2000; 83: 416-20. Wall PS. Allda!"$011111. RodGer M. at al. Excluding Jllinonary eriolsm Bl tha balil11'1ithout diagnostic imaging: Managemant of patianiJ with su!I)IC!Id Plinonary ambolitm prassnting 1D 1ha emargancy depertmanl by using 1 simp II clinical modll. Ann lnl Mad. 2000; 135: 98-107.
You might also like
- Approach To TruamaDocument29 pagesApproach To TruamaIbsa ShumaNo ratings yet
- Basic Emergency MedicineDocument16 pagesBasic Emergency MedicineAdi Heryadi100% (1)
- Pediatrics Slides 23C 2020 8 Banvir 1aDocument344 pagesPediatrics Slides 23C 2020 8 Banvir 1aBanvir SinghNo ratings yet
- 1 - Mattu, Amal ECGsDocument68 pages1 - Mattu, Amal ECGsKhan A Reh50% (2)
- Emergency Medicine: The Core CurriculumDocument208 pagesEmergency Medicine: The Core CurriculumAshu Agarwal0% (1)
- Survival GuideDocument32 pagesSurvival Guidemahi_elsemary7011No ratings yet
- Emergency Medicine Simulation Workbook: A Tool for Bringing the Curriculum to LifeFrom EverandEmergency Medicine Simulation Workbook: A Tool for Bringing the Curriculum to LifeTraci L. ThoureenNo ratings yet
- Advanced Medicine Recall A Must For MRCP PDFDocument712 pagesAdvanced Medicine Recall A Must For MRCP PDFKai Xin100% (2)
- Medical Student Survival Skills: The Acutely Ill PatientFrom EverandMedical Student Survival Skills: The Acutely Ill PatientRating: 5 out of 5 stars5/5 (1)
- STEMI Equivalents: DR Elesia Powell-Williams Emergency Medicine Resident PGY3Document39 pagesSTEMI Equivalents: DR Elesia Powell-Williams Emergency Medicine Resident PGY3elesia powell100% (1)
- Orthopedic Essentials in Emergency MedicineDocument35 pagesOrthopedic Essentials in Emergency MedicineMohd Tarmizi100% (1)
- MCEM Original Practice MCQs No2Document11 pagesMCEM Original Practice MCQs No2Ugeshwaran Aristotle Reddy100% (2)
- Approach To The Limping ChildDocument12 pagesApproach To The Limping ChildinfinityonwardNo ratings yet
- In-Service Exam Review 2009 Emergency MedicineDocument147 pagesIn-Service Exam Review 2009 Emergency Medicineiamo107501100% (1)
- 2 - Toronto Notes 2011 - Ethical 2C Legal and Organizational Aspects of MedicineDocument22 pages2 - Toronto Notes 2011 - Ethical 2C Legal and Organizational Aspects of MedicineqobsarNo ratings yet
- MCC Qe1 - Nov. 2002Document37 pagesMCC Qe1 - Nov. 2002BasirQidwaiNo ratings yet
- Mediwood 3.0 by DR Naveen Koval (With Links)Document707 pagesMediwood 3.0 by DR Naveen Koval (With Links)Rahul B100% (1)
- Icu Survival Guide: SUNY Upstate Medical UniversityDocument36 pagesIcu Survival Guide: SUNY Upstate Medical UniversitySAUMOJIT MAJUMDERNo ratings yet
- Pediatric ECG Survival Guide - 2nd - May 2019Document27 pagesPediatric ECG Survival Guide - 2nd - May 2019Marcos Chusin MontesdeocaNo ratings yet
- Intern Ward Survival Guide 2009Document5 pagesIntern Ward Survival Guide 2009mediquest100% (1)
- PediatricsDocument4 pagesPediatricsFaraz100% (1)
- Rational Laboratory and Diagnostic TestsDocument26 pagesRational Laboratory and Diagnostic TestsCeline dela cruzNo ratings yet
- Examination of The Newborn BabyDocument12 pagesExamination of The Newborn BabytjmtjmtjmNo ratings yet
- Intern Ward SuccessDocument3 pagesIntern Ward Successporfyra_No ratings yet
- Internal Medicine A Guide To Clinical Therapeutics by Rebecca L Attridge Monica L Miller Rebecca Moote Laurajo Ryan 0071745807Document5 pagesInternal Medicine A Guide To Clinical Therapeutics by Rebecca L Attridge Monica L Miller Rebecca Moote Laurajo Ryan 0071745807Hesbon MomanyiNo ratings yet
- 000-Intro To Internal MedicineDocument6 pages000-Intro To Internal MedicineRizky KykyNo ratings yet
- Intern Survival Guide (UIC)Document51 pagesIntern Survival Guide (UIC)medstick100% (1)
- Blueprints - Pediatric Infectious Diseases PDFDocument140 pagesBlueprints - Pediatric Infectious Diseases PDFHabu John Kocu100% (1)
- Pediatric ECG Survival Guide - FinalDocument21 pagesPediatric ECG Survival Guide - FinalEmily VlasikNo ratings yet
- ED Study GuideDocument59 pagesED Study Guidemmmmz100% (1)
- Cardiology A. Woo PDFDocument52 pagesCardiology A. Woo PDFiuliNo ratings yet
- Rash BookDocument12 pagesRash BookPhoebe UsmleNo ratings yet
- Toronto Notes - PaediatricsDocument100 pagesToronto Notes - Paediatricsmun_chloe100% (7)
- CDM CasesDocument24 pagesCDM CasesmalcomxNo ratings yet
- Pediatrics MnemonicsDocument21 pagesPediatrics Mnemonicsdrabhisheck50% (2)
- Ottawas Clerkship GuideDocument44 pagesOttawas Clerkship GuideHugo LuceroNo ratings yet
- MCCQE PediatricsDocument80 pagesMCCQE PediatricsDrSheika Bawazir100% (1)
- 2022.02.10 MCCQE Study Plan Canada 2Document52 pages2022.02.10 MCCQE Study Plan Canada 2joann15marrieNo ratings yet
- Alcapa SyndromeDocument38 pagesAlcapa SyndromeZiaNo ratings yet
- Hands:, Tablets, Wheelchair, WarfarinDocument16 pagesHands:, Tablets, Wheelchair, WarfarinRhythm VasudevaNo ratings yet
- Emergency Medicine SummaryDocument4 pagesEmergency Medicine SummaryokibreazyNo ratings yet
- PharmacologyDocument14 pagesPharmacologyakufahabaNo ratings yet
- SurvivalDocument61 pagesSurvivalsgod34No ratings yet
- SAQ OptimiseDocument109 pagesSAQ OptimiseSricharan SairiNo ratings yet
- Pediatric Spot Diagnosis: Abdulrahman BashireDocument20 pagesPediatric Spot Diagnosis: Abdulrahman Bashireعبدالرحمن بشير100% (1)
- Approach To Emergency PatientDocument18 pagesApproach To Emergency PatientJuan Pablo Gallardo ContrerasNo ratings yet
- American Heart Association Guidelines For CPR 2015: Wanida Chongarunngamsang, MD. Faculty of Srinakarinwirot UniversityDocument49 pagesAmerican Heart Association Guidelines For CPR 2015: Wanida Chongarunngamsang, MD. Faculty of Srinakarinwirot UniversityZulkarnainBustamamNo ratings yet
- EM Basic - Pocket GuideDocument97 pagesEM Basic - Pocket Guidemainertoo100% (2)
- Approach To Neurological DiseaseDocument68 pagesApproach To Neurological DiseaseNEuRoLoGisT CoFFeeCuPNo ratings yet
- Orientation ResidenecyDocument18 pagesOrientation ResidenecyReeMii AngeLa100% (1)
- Emergency Medicine Sample SampsDocument19 pagesEmergency Medicine Sample SampsH!TNo ratings yet
- Internal Medicine Highlights by Conrad Fischer (2008) PDFDocument34 pagesInternal Medicine Highlights by Conrad Fischer (2008) PDFLi SacNo ratings yet
- Abg by DR Manna, Department of Emergency Medicine, Amrita Institute of Medical Sceinces, Kochi, KeralaDocument50 pagesAbg by DR Manna, Department of Emergency Medicine, Amrita Institute of Medical Sceinces, Kochi, KeralaAETCM Emergency medicine100% (1)
- LMCC II GuideDocument79 pagesLMCC II GuideSoleil DaddouNo ratings yet
- Guns Don't Kill People: They They They'veDocument1 pageGuns Don't Kill People: They They They'veprekos 65No ratings yet
- WTACriticalDecisionsEsophagealInjuries PDFDocument7 pagesWTACriticalDecisionsEsophagealInjuries PDFprekos 65No ratings yet
- Textbook of Adult Emergency Medicine : Book ReviewDocument2 pagesTextbook of Adult Emergency Medicine : Book Reviewprekos 65No ratings yet
- General Surgery Resident HandbookDocument32 pagesGeneral Surgery Resident Handbookprekos 65No ratings yet
- Epidemiological Approach Surgical The: of Casualties ofDocument5 pagesEpidemiological Approach Surgical The: of Casualties ofprekos 65No ratings yet
- Evidence Concerning The Regulation of Firearms Design, Sale, and Carrying On Fatal Mass Shootings in The United StatesDocument42 pagesEvidence Concerning The Regulation of Firearms Design, Sale, and Carrying On Fatal Mass Shootings in The United Statesprekos 65No ratings yet
- DiMaio-Minimal Velocities Necessary For Perforation of Skin by Air Gun Pellets and BulletsDocument5 pagesDiMaio-Minimal Velocities Necessary For Perforation of Skin by Air Gun Pellets and Bulletsprekos 65No ratings yet
- Roadside: Clear Zones (1 of 2)Document3 pagesRoadside: Clear Zones (1 of 2)Cristian Camilo Londoño PiedrahítaNo ratings yet
- Work Sheet 8 The Nervous System: Structure of A NerveDocument5 pagesWork Sheet 8 The Nervous System: Structure of A NerveJapet Floyd AlipioNo ratings yet
- Three Digit BCD Counter MC1453B Data SheetDocument12 pagesThree Digit BCD Counter MC1453B Data Sheetmata1802No ratings yet
- Ten Years For 1st ProfDocument54 pagesTen Years For 1st ProfParijatNo ratings yet
- Anatomy Practical OSPEDocument33 pagesAnatomy Practical OSPEAbdi Ñãśìr Møhàmèď ŚàĺàhNo ratings yet
- Skull Procedures 1. PA Projection 2. AP ProjectionDocument215 pagesSkull Procedures 1. PA Projection 2. AP ProjectionradioNo ratings yet
- Pathophysiology of SyringomyeliaDocument14 pagesPathophysiology of SyringomyeliaGerardo100% (2)
- Installation PDFDocument63 pagesInstallation PDFLeonardusNo ratings yet
- 01 Wrist MobilityDocument5 pages01 Wrist MobilityhatemfaroukNo ratings yet
- Ballard/OUR Injury LawsuitDocument19 pagesBallard/OUR Injury LawsuitRobert GehrkeNo ratings yet
- Back Attacks Enter The System - FlowChart 1.2 2Document1 pageBack Attacks Enter The System - FlowChart 1.2 2Kellar Carnes0% (1)
- Tashb CSDocument136 pagesTashb CSFaqRO100% (6)
- Dyson Upright DC25 Vacuum User GuideDocument16 pagesDyson Upright DC25 Vacuum User Guidesteven dixonNo ratings yet
- Report On The Death of Taurean WilsonDocument8 pagesReport On The Death of Taurean WilsonFOX 61 WebstaffNo ratings yet
- JainismDocument3 pagesJainismEliseNo ratings yet
- P1Document12 pagesP1Roykedona Lisa TrixieNo ratings yet
- Inverted L OsteotomyDocument9 pagesInverted L OsteotomyhaneefmdfNo ratings yet
- Top 5 Exercises That Can Be Done at Home - Yahoo! Lifestyle IndiaDocument4 pagesTop 5 Exercises That Can Be Done at Home - Yahoo! Lifestyle IndiaRakesh MkNo ratings yet
- Balsa 2015Document17 pagesBalsa 2015Pipe VodNo ratings yet
- 7 Things You'd Better Know WorksheetDocument7 pages7 Things You'd Better Know WorksheetIvan Parker40% (5)
- Cat Muscles Data SheetDocument4 pagesCat Muscles Data Sheetapi-245583659No ratings yet
- Corticosteroid Injection For de Quervain's Tenosynovitis (Review)Document19 pagesCorticosteroid Injection For de Quervain's Tenosynovitis (Review)intan rosliNo ratings yet
- Antegrade Versus Retrograde Nailing TechniquesDocument11 pagesAntegrade Versus Retrograde Nailing TechniquesJian Wei LowNo ratings yet
- Injury ReportingDocument1 pageInjury ReportingJessica YimNo ratings yet
- Casualty EvacuationDocument29 pagesCasualty Evacuationdibera18No ratings yet
- Assessment of The Peripheral Vascular SystemDocument91 pagesAssessment of The Peripheral Vascular SystemKeid Reuma100% (1)
- Leprosy MsDocument78 pagesLeprosy MsAmit Kochhar67% (3)
- Datafortress 2020 - Interlock Unlimited - CP2020 GM ScreenDocument23 pagesDatafortress 2020 - Interlock Unlimited - CP2020 GM ScreenFabricio MoreiraNo ratings yet
- Approach To The Adult With Unspecified Knee Pain - UpToDateDocument55 pagesApproach To The Adult With Unspecified Knee Pain - UpToDateCamila Gomes Santos MoraesNo ratings yet
- Atlas of Approaches in Neurosurgery - J.FischerDocument7 pagesAtlas of Approaches in Neurosurgery - J.FischerZdravko HeinrichNo ratings yet
- Love Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)From EverandLove Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)Rating: 3 out of 5 stars3/5 (1)
- Breaking the Habit of Being YourselfFrom EverandBreaking the Habit of Being YourselfRating: 4.5 out of 5 stars4.5/5 (1460)
- ADHD is Awesome: A Guide to (Mostly) Thriving with ADHDFrom EverandADHD is Awesome: A Guide to (Mostly) Thriving with ADHDRating: 5 out of 5 stars5/5 (2)
- The Age of Magical Overthinking: Notes on Modern IrrationalityFrom EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityRating: 4 out of 5 stars4/5 (29)
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionFrom EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionRating: 4 out of 5 stars4/5 (404)
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsFrom EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsNo ratings yet
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedFrom EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedRating: 5 out of 5 stars5/5 (81)
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeFrom EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeRating: 2 out of 5 stars2/5 (1)
- Summary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisFrom EverandSummary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisRating: 4.5 out of 5 stars4.5/5 (42)
- Why We Die: The New Science of Aging and the Quest for ImmortalityFrom EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityRating: 4 out of 5 stars4/5 (5)
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsFrom EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsRating: 5 out of 5 stars5/5 (1)
- The Obesity Code: Unlocking the Secrets of Weight LossFrom EverandThe Obesity Code: Unlocking the Secrets of Weight LossRating: 4 out of 5 stars4/5 (6)
- How to Talk to Anyone: Learn the Secrets of Good Communication and the Little Tricks for Big Success in RelationshipFrom EverandHow to Talk to Anyone: Learn the Secrets of Good Communication and the Little Tricks for Big Success in RelationshipRating: 4.5 out of 5 stars4.5/5 (1135)
- The Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaFrom EverandThe Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaRating: 4.5 out of 5 stars4.5/5 (266)
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsFrom EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsRating: 4 out of 5 stars4/5 (4)
- Summary of The 4-Hour Body: An Uncommon Guide to Rapid Fat-Loss, Incredible Sex, and Becoming Superhuman by Timothy FerrissFrom EverandSummary of The 4-Hour Body: An Uncommon Guide to Rapid Fat-Loss, Incredible Sex, and Becoming Superhuman by Timothy FerrissRating: 4.5 out of 5 stars4.5/5 (82)
- Peaceful Sleep Hypnosis: Meditate & RelaxFrom EverandPeaceful Sleep Hypnosis: Meditate & RelaxRating: 4.5 out of 5 stars4.5/5 (143)
- Dark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.From EverandDark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Rating: 4.5 out of 5 stars4.5/5 (110)
- Empath: The Survival Guide For Highly Sensitive People: Protect Yourself From Narcissists & Toxic Relationships. Discover How to Stop Absorbing Other People's PainFrom EverandEmpath: The Survival Guide For Highly Sensitive People: Protect Yourself From Narcissists & Toxic Relationships. Discover How to Stop Absorbing Other People's PainRating: 4 out of 5 stars4/5 (95)
- Raising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsFrom EverandRaising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsRating: 4.5 out of 5 stars4.5/5 (170)
- When the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisFrom EverandWhen the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisRating: 3.5 out of 5 stars3.5/5 (2)