Professional Documents
Culture Documents
For E-Portfolio
Uploaded by
api-174496267Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
For E-Portfolio
Uploaded by
api-174496267Copyright:
Available Formats
1
Penile cancer treatment planning technique with matching photonelectron beams: A case study
Amanuel Negussie, B.S. R.T.(T), Nishele Lenards, M.S., CMD, R.T.(R)(T), FAAMD, Joseph G. Lynch, CMD, R.T.(T)(MR), and James Schmitz, A.A.S., CMD, R.T.(T) *Medical Dosimetry Program at the University of Wisconsin - La Crosse, WI and Department of Radiation Oncology, Minneapolis VA Health Care System, Minneapolis, MN Abstract: Introduction: This case study aims to communicate a treatment planning technique to treat penile cancer with matching photon-electron beams. Case Description: A patient with a squamous cell carcinoma of the penis was treated using 45 Gy at 1.8 Gy per fraction to the penis, pelvic and bilateral inguinal nodes with a concurrent electron beam of 45 Gy at 1.8 Gy per fraction to the bilateral inguinal nodes. This was followed by an electron boost to the penile shaft and left inguinal surgical scar. The penile shaft boost was delivered using 20 Gy at 2 Gy per fraction to the penile shaft and the left inguinal scar boost was delivered using 14.4 Gy in 1.8 Gy per fraction. The initial treatment was delivered with parallelopposed photon beams and matching bilateral electron beams. A bolus was used in the anterior aspect of the penis to provide an adequate dose distribution to the target. The boost treatment was delivered with two enface electron fields at 100 SSD. A layer of bolus and lead was used underneath the penis to reduce electron backscatter. Conclusions: Each plan was carefully evaluated based on the dose volume histogram, 100% of the prescription dose coverage, maximum and mean dose to the targets. The skin dose for both initial and boost plans were verified with TLDs. Key words: penile cancer, photon-electron matching, radiation therapy, electron backscatter
2 Introduction Penile cancer is rare and more common in men over age 60.1 It accounts for 1% of cancer in men in the United States and up to 10% in parts of Asia, Africa, and South America.2 The American Cancer Society estimates in the year 2013, there will be about 1,570 new diagnoses and 310 deaths from this cancer.2 Surgery is the most common and effective treatment option for all stages of penile cancer. Radiation therapy can be used as an initial treatment for early stage tumors and as a palliative treatment for advanced cancers.3 It can also be used along with surgery to treat lymph nodes and to reduce a chance of recurrence.3 In younger patients, radiation therapy can be a particularly beneficial alternative treatment as it prevents trauma associated with surgery.1 Radiation therapy is not well utilized in penile cancer treatment, partially due to referral bias.4 External beam radiation therapy (EBRT) and brachytherapy are an effective treatment option for penile cancer patients who seek penile preservation. Brachytherapy has the advantage to deliver higher tumor dose in a shorter time, which can limit tumor repopulation.5 EBRT can be used alone or with surgery, mainly for patients with stage T1N0.4 In a retrospective study from the United Kingdom6, patients with T1N0 penile cancer had a 71% 5 year survival and a 63% recurrence free survival for all stages after EBRT. In addition, Sarin et al7 showed that patients receiving radiation therapy had a significantly higher overall sexual function than those who underwent surgical procedures.7 Case Report A 72-year-old uncircumcised gentleman first noted a penile lesion in 2011. The patient neglected to seek medical attention, as it was painless and looked like a wart. However, he saw a dermatologist as it subsequently began to grow quickly. The patient underwent a shave biopsy in
3 March 2012. The biopsy showed a squamous cell carcinoma that was well differentiated and keratinizing. Given this finding, the patient was seen by a urologist. On examination, a 1.3 cm polypoid mass was noted on the dorsum of the prepuce. Retraction of the prepuce demonstrated numerous other squamous lesions along with hyperemic changes of the glans. Inguinal examination revealed bilateral palpable inguinal adenopathy. A penis glans biopsy showed linchenoid inflammatory infiltrate with mild epidermal atypia. It also demonstrated a larger polypoid lesion with infiltrating and well-differentiated squamous cell carcinoma that extended to the subepithelial connective tissue. The lesion measured 7 mm in thickness. There was also a secondary lesion that showed squamous cell carcinoma in situ with focal invasion. In addition, a diagnostic CT scan showed a mildly enlarged left external iliac node measuring 1.6 x 1.0 cm. The disease was staged rT1aN1M0 squamous carcinoma of the penis. The treatment options available for penile cancer were discussed with the patient. The patient declined to undergo surgery and chose to proceed with radiation therapy. Given the size of his hernia and its proximity to the penis, it was recommended that he undergo a repair procedure. It was also recommended that he have a circumcision procedure before starting his treatment. In penile cancer patients, circumcision prior to beginning a radiation treatment minimizes swelling, skin irritation, moist desquamation, and secondary infection.8 The patient underwent both procedures as recommended. Prescription Prescription for the initial treatment to the penis, pelvis, and inguinal nodes was 45 Gy at 180 cGy per fraction. A concurrent dose of 22.5 Gy at 90 cGy per fraction was prescribed to the bilateral inguinal nodes using electron beams. The boost was prescribed to 20 Gy at 200 cGy per fraction to the penile shaft and 14.4 Gy at 180 cGy per fraction to the left inguinal scar.
4 Simulation The patient was placed supine on the computed tomography (CT) simulator couch in a frog-leg position to avoid skin fold in the pubic region and minimize complication. A Vac-Lok cushion was used to form a custom mold of the patients setup position. The radiation oncologist marked the surgical scar with a solder wire. Two pieces of styrofoam were placed under the scrotum for support and immobilization. A 1 cm pink bolus was molded into shape to fit over the penis. In addition, a 1 cm bolus was placed on top of the surgical scar. The treatment planning CT (TPCT) was taken with 3 mm slices from the second lumbar spine (L2) to mid femur. The radiation oncologist placed the isocenter. Various techniques can be used to immobilize the penis, including Perspex block and water bath.9 It is essential to utilize devices that can be maintained as the penis possibly swells during the treatment course. Target Delineation The TPCT scan was imported into Pinnacle3 9.0 treatment planning system (TPS). The medical dosimetrist contoured all the organs at risk (OR) including rectum, right and left femur, and bladder along with the solder wire. The radiation oncologist contoured the surgical drainage sites, shaft of the penis, external genitalia, and the pelvic vessels to define the treatment volume. The pelvic vessels were used as a substitute for corresponding pelvic lymph nodes as this technique is widely used. The anterior (AP) and posterior (PA) treatment fields were designed using the contoured structures. No definite margin was used. The fields were systematically constructed to include the targets. The AP field included the penis, pelvic and bilateral inguinal lymph nodes (Fig. 1). The left field edge was extended to cover the positive nodal margin (Fig. 1). The posterior (PA) field was narrower and only incorporated the penis and pelvic nodes (Fig. 1). This
5 was done purposely to decrease toxicity to the femoral heads. In addition, the inferior field border was set lower to cover the drainage sites. Treatment Planning - Initial The photon field was designed using 6 MV for the AP field and 18 MV for the PA field. The TPS was set to deliver a point dose of 45 Gy to the isocenter equally weighted from both angles. After careful revision, the weighting was adjusted to achieve better dose coverage to the target. An 18 MV field in field photon beam was also created from the AP field to minimize the hot spot located in the genitalia area. It was not possible to use a hard wedge because of the field size. The right and left anterior inguinal electron fields were planned using 16 MeV electron beams (Fig. 2). The medial border was matched with the PA photon beams lateral border (Fig. 3). The electron fields were constructed in the TPS by the radiation oncologist. The calculation points were placed at 2.8 cm depth. The TPS was set to deliver a point dose of 22.5 Gy at dmax for each electron field. The plan was optimized and reviewed carefully to ensure adequate target coverage. While assessing the composite photon and electron plans, the skin dose was higher on the left inguinal region. As a result, the bolus placed on top of the surgical scar was removed to minimize the dose to that region. This was accomplished by contouring the bolus and assigning it with a density equivalent to air. The weighting of the photon beams were adjusted accordingly to achieve better target coverage (Fig. 4 and Fig. 5). The plan was completed with a total maximum dose of 65 Gy located at the edge of the genitalia. A monitor unit check was performed with MuCheck 8.2.0. The plan was approved with mu difference less than 3%. During treatment, the electron fields were matched with the PA photon beam by shifting laterally from the isocenter. A daily KV image was taken to verify the patient position. The scrotum was
6 also protected by taping it away from the treatment fields. In addition, the dose to skin was verified using thermoluminescent dosimeters (TLDs). The result showed the treatment dose was delivered appropriately as planned. Treatment Planning - Boost The left inguinal surgical scar and the penile shaft received a radiation dose boost with an electron beam. A clinical setup was used to determine the treatment area, the gantry angle, the collimator angle, and the couch angle. The patient was positioned the same as the initial treatment. The anterior portion of the penis was wrapped with a customized 1 cm bolus. The posterior aspect of the penis was supported in a layer of 1 cm bolus, 4.5 mm lead, and a styrofoam (Fig. 6). A layer of bolus and lead are clinically proven to be efficient in dissipating backscattered electrons. Thickness of the absorber materials required to minimize the electron backscatter can be mathematically determined.10 The left inguinal boost was prescribed to 16 MeV at 90% for 180 cGy per fraction to a total dose of 14.4 Gy and a cumulative dose of 59.4 Gy. This was delivered with a 15 x 15 cm cone size and a custom cutout block at 100 SSD (Fig. 7). The penile shaft boost was prescribed to 9 MeV at 90% for 200 cGy per fraction to a total dose of 20 Gy and a cumulative dose of 65 Gy. This was delivered using a 6 x 6 cm open field cone size at 100 SSD (Fig. 7). Since the boost field is a clinical setup, the radiation oncologist determined a composite plan would not be beneficial. The skin dose of both boost fields was verified with TLDs. During the initial treatment, the patient experienced acute scrotal swelling. An ultrasound study demonstrated diffused edema. Therefore, the patient was placed on hold for one week after the 22nd fraction. The patient was treated with Keflex (7 day course) and Fluconazole (1 day course). The treatment was resumed with no other complications.
7 Conclusion Due to the rarity of treating penile cancer with external beam radiation, it is important to work as a team to ensure accuracy and minimize side effects. Immobilization devices should be carefully determined to ensure accuracy and reproducibility. Matching photon-electron beams can provide a homogenous dose distribution to the penis and regional lymph nodes. However, the beam arrangements and blockings should be strategically arranged to minimize an overlap between the posterior photon and the bilateral inguinal electron beams. In addition, a skin dose should be carefully examined near the photon-electron match region.
8 References 1. Turner B, Drudge-Coates L, Henderson S. Nursing Standard. 2013;27(29):50-57. 2. American Cancer Society. What are the key statistics about penile cancer? http://www.cancer.org/cancer/penilecancer/detailedguide/penile-cancer-key-statistics. Accessed June 25, 2013. 3. American Cancer Society. Radiation Therapy for Penile Cancer. http://www.cancer.org/cancer/penilecancer/detailedguide/penile-cancer-treating-radiationtherapy. Accessed July 4, 2013. 4. Burt LM, Shrieve DC, Tward JD. Stage presentation, care patterns, and treatment outcomes for squamous cell carcinoma of the penis. Int J Radiat Oncol Biol Phys. 2013. In Press. doi:10.1016/j.ijrobp.2013.08.013 5. de Crevoisier RD, Slimane K, Sanfilippo N, et al. Long-term results of brachytherapy for carcinoma of the penis confined to the glans (N- or NX). Int J Radiat Oncol Biol Phys. 2009;74(4):1150-1156. doi:10.1016/j.ijrobp.2008.09.054 6. Mistry T, Jones RW, Dannatt E, et al. A 10-year retrospective audit of penile cancer management in the UK. BJU Int. 2007;100(6):1277-1281. doi:10.1111/j.1464410X.2007.07168.x 7. Sarin R, Norman AR, Steel GG, et al. Treatment results and prognostic factors in 101 men treated for squamous carcinoma of the penis. Int J Radiat Oncol Biol Phys. 1997;38(4):713722. 8. Chao K.S C, Perez CA, Brady LW. Radiation Oncology Management Decisions. 3rd ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2011.
9 9. Crook J, Ma C, Grimard L. Radiation therapy in the management of the primary penile tumor: an update. World J Urol. 2009;27(2):189-196. doi:10.1007/s00345-008-0309-5 10. Khan FM. The Physics of Radiation Therapy. 4th ed. Baltimore, MD: Lippincott Williams & Wilkins; 2010.
10 Figures
Fig. 1. Beams eye view of the anterior and posterior photon fields. The green contoured structure represents the pelvic vessels, the red line represents the patients surgical scar, the red oval shaped structure represents the penile shaft, the orange contoured structure represents the genitalia, and the two small green circles represent the surgical drainage sites.
Fig. 2. Beams eye view (BEV) of the bilateral electron fields
11
Fig. 3. Field matching of the bilateral anterior electron beams with a posterior photon field
12
Fig. 4. The sagittal, axial, and coronal views of dose distribution. The red isodose line represents 45 Gy and yellow isodose line represents 22.5 Gy.
13
Fig. 5. Dose volume histogram (DVH) of the initial plan demonstrating dose distribution to the penile shaft, pelvic vessels, and OR.
Fig. 6. A layer of bolus and lead placed underneath the penis to reduce electron backscatter
14
Fig. 7. Monitor unit calculation for the left inguinal and penile shaft boost fields
You might also like
- Breast Case StudyDocument15 pagesBreast Case Studyapi-318014709No ratings yet
- June Case Study Final RevisedDocument18 pagesJune Case Study Final Revisedapi-213108684No ratings yet
- March Case Study Final RevisionDocument13 pagesMarch Case Study Final Revisionapi-213108684No ratings yet
- March Case StudyDocument7 pagesMarch Case Studyapi-210258673No ratings yet
- Af Final Clincal ProjectDocument12 pagesAf Final Clincal Projectapi-247864638No ratings yet
- Hybrid Planning Case Study Final DraftDocument20 pagesHybrid Planning Case Study Final Draftapi-313040758No ratings yet
- Kevin FinalDocument20 pagesKevin Finalapi-213055674No ratings yet
- Modified Technique of Radical Inguinal Lymphadenectomy For Penile Carcinoma: Morbidity and OutcomeDocument7 pagesModified Technique of Radical Inguinal Lymphadenectomy For Penile Carcinoma: Morbidity and OutcomeAlwin PrasetyaNo ratings yet
- March Case StudyDocument13 pagesMarch Case Studyapi-212894050No ratings yet
- Electron Treatment For Male Breast Bud - Case StudyDocument13 pagesElectron Treatment For Male Breast Bud - Case Studyapi-395602816No ratings yet
- Group 5 FinalDocument11 pagesGroup 5 Finalapi-404851310No ratings yet
- Chest Wall With Nodes and IMRT Boost Case Study History of Present Illness: Patient RB Is A 65-Year-Old Female With A History of Early StageDocument19 pagesChest Wall With Nodes and IMRT Boost Case Study History of Present Illness: Patient RB Is A 65-Year-Old Female With A History of Early Stageapi-268707929No ratings yet
- March Case Study Dustin MelanconDocument14 pagesMarch Case Study Dustin Melanconapi-213116779No ratings yet
- May Case StudyDocument18 pagesMay Case Studyapi-213055674No ratings yet
- Adaptive Radiotherapy (ART) For A Prostate CaseDocument18 pagesAdaptive Radiotherapy (ART) For A Prostate Caseapi-299189797No ratings yet
- Sethraheeljong Final PaperDocument13 pagesSethraheeljong Final Paperapi-268623363No ratings yet
- March Final CsDocument10 pagesMarch Final Csapi-243468464No ratings yet
- Semester Case StudyDocument19 pagesSemester Case Studyapi-213116779No ratings yet
- Journal: Nursing Leadership and ManagementDocument9 pagesJournal: Nursing Leadership and ManagementdaliaNo ratings yet
- A Case Study of DIBH To Spare Abdominal Organs at Risk For Renal Cell Carcinoma MR-Guided RadiotherapyDocument14 pagesA Case Study of DIBH To Spare Abdominal Organs at Risk For Renal Cell Carcinoma MR-Guided Radiotherapyapi-525837437No ratings yet
- RM Rayos Carcinoma Canal AnalDocument9 pagesRM Rayos Carcinoma Canal Analouf81No ratings yet
- Intensity-Modulated Radiation Therapy (Imrt) in The Treatment of Anal Cancer - Toxicity and Clinical OutcomeDocument8 pagesIntensity-Modulated Radiation Therapy (Imrt) in The Treatment of Anal Cancer - Toxicity and Clinical OutcomejunfangokuNo ratings yet
- March Case StudyDocument9 pagesMarch Case Studyapi-247959633No ratings yet
- Case Study of Lung CancerDocument18 pagesCase Study of Lung CancerIsha .SNo ratings yet
- Intensity-Modulated Radiotherapy in Patients With Cervical Cancer. An Intra-Individual Comparison of Prone and Supine PositioningDocument8 pagesIntensity-Modulated Radiotherapy in Patients With Cervical Cancer. An Intra-Individual Comparison of Prone and Supine PositioningAlberto GonzalesNo ratings yet
- Nigro1991 (Si Desaparece Totalmente, No Biopsiar)Document5 pagesNigro1991 (Si Desaparece Totalmente, No Biopsiar)ouf81No ratings yet
- February Case StudyDocument6 pagesFebruary Case Studyapi-210258673No ratings yet
- New England Journal Medicine: The ofDocument10 pagesNew England Journal Medicine: The ofsyafahalimNo ratings yet
- April Case Study EditedDocument13 pagesApril Case Study Editedapi-174496267No ratings yet
- Pi Is 0360301611018256Document1 pagePi Is 0360301611018256Olyndo IwanNo ratings yet
- Se Hacía Biopsia A Los Tres Meses. Estudio Pequeño ADocument5 pagesSe Hacía Biopsia A Los Tres Meses. Estudio Pequeño Aouf81No ratings yet
- Final Case StudyDocument13 pagesFinal Case Studyapi-334402872No ratings yet
- JCO 2003 Lin 631 7Document7 pagesJCO 2003 Lin 631 7Adhika Manggala DharmaNo ratings yet
- Adaptative RT For Prostate Cancer Using KV CBCT - Jasper NijkampDocument8 pagesAdaptative RT For Prostate Cancer Using KV CBCT - Jasper NijkampMarcos sajcabunNo ratings yet
- Clinical Oncology Assignment RaverDocument7 pagesClinical Oncology Assignment Raverapi-635923017No ratings yet
- Percutaneous Laser Ablation: A New Contribution To Unresectable High-Risk Metastatic Retroperitoneal Lesions?Document10 pagesPercutaneous Laser Ablation: A New Contribution To Unresectable High-Risk Metastatic Retroperitoneal Lesions?Luke DengNo ratings yet
- MainDocument7 pagesMainHanaNo ratings yet
- Role of Percutaneous Ultrasonographic Guided Radiofrequency Ablation in The Management of Hepatocellular CarcinomaDocument8 pagesRole of Percutaneous Ultrasonographic Guided Radiofrequency Ablation in The Management of Hepatocellular CarcinomadickyaririsandyNo ratings yet
- Intravaginal Packing Eects of CT-Guided Intracavitary Radiotherapy For Cervical CancerDocument5 pagesIntravaginal Packing Eects of CT-Guided Intracavitary Radiotherapy For Cervical CancerLuis JorgeNo ratings yet
- Case Report A Rare Case of Metastatic Primary Peritoneal Ependymoma: A Case Report and Literature ReviewDocument8 pagesCase Report A Rare Case of Metastatic Primary Peritoneal Ependymoma: A Case Report and Literature Reviewnurul auliaNo ratings yet
- Capstone DraftDocument10 pagesCapstone Draftapi-450374689No ratings yet
- Klopp 2013Document8 pagesKlopp 2013Insighte ChildcareNo ratings yet
- A Case of Basal Cell Carcinoma of External Auditory Canal: Beom-Jun Lee, Seong-Cheon Bae, Jae-Hong Lee and Kyoung-Ho ParkDocument4 pagesA Case of Basal Cell Carcinoma of External Auditory Canal: Beom-Jun Lee, Seong-Cheon Bae, Jae-Hong Lee and Kyoung-Ho Parkdwi jayaNo ratings yet
- Laparoscopic Resection of Rectal CancerDocument4 pagesLaparoscopic Resection of Rectal CancerhoangducnamNo ratings yet
- Image-Guided Interstitial Brachytherapy Boost ForDocument6 pagesImage-Guided Interstitial Brachytherapy Boost ForBijay Kumar BarikNo ratings yet
- Clinical Oncology AssignmentDocument8 pagesClinical Oncology Assignmentapi-598481829No ratings yet
- Research Paper Conclusion v3 9-25Document22 pagesResearch Paper Conclusion v3 9-25api-602263051No ratings yet
- ACR 2018 TXIT Exam RationalesDocument94 pagesACR 2018 TXIT Exam Rationalesgermanfutbol7100% (3)
- Final Draft-Formatted12-2-14Document19 pagesFinal Draft-Formatted12-2-14api-237552707No ratings yet
- Hippocampal Sparing VMAT Using Pinnacle Treatment Planning SystemDocument12 pagesHippocampal Sparing VMAT Using Pinnacle Treatment Planning Systemapi-264047496No ratings yet
- Research Paper Results-Capston IIIDocument21 pagesResearch Paper Results-Capston IIIapi-602263051No ratings yet
- Bisa 1Document8 pagesBisa 1justforuroNo ratings yet
- A Dosimetric Comparison of Coplanar vs. Non-Coplanar VMAT SBRT Techniques For NSCLCDocument9 pagesA Dosimetric Comparison of Coplanar vs. Non-Coplanar VMAT SBRT Techniques For NSCLCapi-269672910No ratings yet
- ClinoncDocument15 pagesClinoncapi-631736561No ratings yet
- Final Draft6 Group1Document13 pagesFinal Draft6 Group1api-598481829No ratings yet
- Final Draft6 Group1Document13 pagesFinal Draft6 Group1api-598481829No ratings yet
- Wagner1994 (No Hace Biopsia)Document7 pagesWagner1994 (No Hace Biopsia)ouf81No ratings yet
- Reverse Boost in Breast CancerDocument38 pagesReverse Boost in Breast CancerSwarupa MitraNo ratings yet
- Capstone IIDocument16 pagesCapstone IIapi-602263051No ratings yet
- Atlas of Early Neoplasias of the Gastrointestinal Tract: Endoscopic Diagnosis and Therapeutic DecisionsFrom EverandAtlas of Early Neoplasias of the Gastrointestinal Tract: Endoscopic Diagnosis and Therapeutic DecisionsFrieder BerrNo ratings yet
- Ec 102 Eclipseinverseplanningimrtandrapidarcv 13 CamanuelnegussieDocument1 pageEc 102 Eclipseinverseplanningimrtandrapidarcv 13 Camanuelnegussieapi-174496267No ratings yet
- ResumeDocument2 pagesResumeapi-174496267No ratings yet
- Amanuel Negussie: Certificate of AttendanceDocument1 pageAmanuel Negussie: Certificate of Attendanceapi-174496267No ratings yet
- ImrtDocument3 pagesImrtapi-174496267No ratings yet
- Joe RTDocument1 pageJoe RTapi-174496267No ratings yet
- V 13 RtsummaryonsitetrainingworkshopfamanuelnegussieDocument1 pageV 13 Rtsummaryonsitetrainingworkshopfamanuelnegussieapi-174496267No ratings yet
- Amanuel Final 5 1 14Document19 pagesAmanuel Final 5 1 14api-174496267No ratings yet
- ElectronDocument2 pagesElectronapi-174496267No ratings yet
- Case Log FallDocument2 pagesCase Log Fallapi-174496267No ratings yet
- Fall EvalsDocument6 pagesFall Evalsapi-212894050No ratings yet
- PhotonDocument3 pagesPhotonapi-174496267No ratings yet
- Monthly EvalDocument2 pagesMonthly Evalapi-174496267No ratings yet
- Fall EvalsDocument6 pagesFall Evalsapi-212894050No ratings yet
- BrachytherapyDocument3 pagesBrachytherapyapi-174496267No ratings yet
- Fall EvalsDocument6 pagesFall Evalsapi-212894050No ratings yet
- Comprehensive Case Study Final - AdjustedDocument17 pagesComprehensive Case Study Final - Adjustedapi-174496267No ratings yet
- ConferenceDocument7 pagesConferenceapi-174496267No ratings yet
- Tally 1Document2 pagesTally 1api-174496267No ratings yet
- PT Case LogsDocument2 pagesPT Case Logsapi-174496267No ratings yet
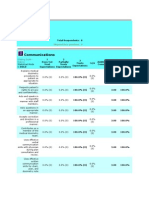
- ComptotalsDocument3 pagesComptotalsapi-174496267No ratings yet
- ConferencesDocument4 pagesConferencesapi-174496267No ratings yet
- 2nd Rotation PallDocument3 pages2nd Rotation Pallapi-174496267No ratings yet
- Conference LogsDocument1 pageConference Logsapi-174496267No ratings yet
- Comprehensive Case Study - AnDocument31 pagesComprehensive Case Study - Anapi-174496267No ratings yet
- October Case StudyDocument15 pagesOctober Case Studyapi-174496267No ratings yet
- September Case StudyDocument20 pagesSeptember Case Studyapi-174496267No ratings yet
- August Citation AssignmentDocument2 pagesAugust Citation Assignmentapi-174496267No ratings yet
- July Case StudyDocument18 pagesJuly Case Studyapi-174496267No ratings yet
- May EvalDocument6 pagesMay Evalapi-174496267No ratings yet
- Duties of A Labor and Delivery NurseDocument3 pagesDuties of A Labor and Delivery Nursefenan sollanoNo ratings yet
- Intraoperative CareDocument5 pagesIntraoperative CareraffineeNo ratings yet
- Surgical Incisions: STJ - Dr. Aylin Mert 0902110019Document22 pagesSurgical Incisions: STJ - Dr. Aylin Mert 0902110019NiyaNo ratings yet
- Noninvasive Ventilation Reduces Mortality in Severe PneumoniaDocument4 pagesNoninvasive Ventilation Reduces Mortality in Severe PneumoniaMulyasari LindaNo ratings yet
- Introduction To Endocrinology For Clinical StudentsDocument9 pagesIntroduction To Endocrinology For Clinical StudentsOhwovoriole ToketemuNo ratings yet
- The Foot Posture Index: Six Item Version FPI-6 User Guide and ManualDocument19 pagesThe Foot Posture Index: Six Item Version FPI-6 User Guide and ManualBryan AlimNo ratings yet
- DR Kamlesh Tandon Hospital and Test Tube Baby Centre Goyal City HospitalDocument388 pagesDR Kamlesh Tandon Hospital and Test Tube Baby Centre Goyal City HospitalM SidduNo ratings yet
- Prepaid PlansDocument27 pagesPrepaid PlansDee ReyesNo ratings yet
- Establishment of Trauma Center: Dr. Sanjay ShahDocument34 pagesEstablishment of Trauma Center: Dr. Sanjay ShahDr. Rakshit SolankiNo ratings yet
- Breastfeeding and YouDocument203 pagesBreastfeeding and YouEmman Acosta DomingcilNo ratings yet
- Jupiter EngDocument34 pagesJupiter EngakukauakuNo ratings yet
- Daftar PustakaDocument4 pagesDaftar PustakaBilly Aditya PratamaNo ratings yet
- A Project Report On: Fortis Hospital AnandapurDocument36 pagesA Project Report On: Fortis Hospital AnandapurKaran Karan100% (1)
- Prelim TFNDocument5 pagesPrelim TFNjokazelNo ratings yet
- Pacemaker Physics PaperDocument7 pagesPacemaker Physics PaperJose Rene BerliozNo ratings yet
- Ateneo de Davao University Graduate SchoolDocument10 pagesAteneo de Davao University Graduate SchoolDennis Nabor Muñoz, RN,RMNo ratings yet
- Edan ManualDocument14 pagesEdan ManualTony Nava100% (1)
- Nelson JaundiceDocument7 pagesNelson JaundiceJesly CharliesNo ratings yet
- Mobile phone distraction reduces dental anxietyDocument5 pagesMobile phone distraction reduces dental anxietyJude Aldo PaulNo ratings yet
- MenarcheDocument3 pagesMenarcheShiina LeeNo ratings yet
- Cervical ScreeningDocument4 pagesCervical ScreeningSanjay SharmaNo ratings yet
- Anatomy of Womans Sex OrganDocument5 pagesAnatomy of Womans Sex Organsumeer khan63% (8)
- Clinical TeachingDocument21 pagesClinical Teachingtanmai nooluNo ratings yet
- Assessment 2 Vital Signs Normal ValuesDocument4 pagesAssessment 2 Vital Signs Normal Valuesthannikkotte12345No ratings yet
- BRT Anatomy - NeuroanatomyDocument6 pagesBRT Anatomy - NeuroanatomyNicole Santos100% (3)
- sullivan1998 ເອກະສານອ້າງອີງ ຈາກ ວິທີວິທະຍາDocument10 pagessullivan1998 ເອກະສານອ້າງອີງ ຈາກ ວິທີວິທະຍາKab Zuag HaamNo ratings yet
- Letter of Recommendation 1Document1 pageLetter of Recommendation 1api-405020419No ratings yet
- Tibia Fibula Fanny - 2Document27 pagesTibia Fibula Fanny - 2Rakyat Kecil BerdasiNo ratings yet
- Menstrual DisordersDocument29 pagesMenstrual DisordersJesse EstradaNo ratings yet
- Dianosis Dan Resusitasi Pada Pasien Syok Perdarahan &Document31 pagesDianosis Dan Resusitasi Pada Pasien Syok Perdarahan &Strata PertiwiNo ratings yet