Professional Documents
Culture Documents
NCP-Toddler-Tonsillitis & Lactose Intolerance
Uploaded by
tinatin989Original Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
NCP-Toddler-Tonsillitis & Lactose Intolerance
Uploaded by
tinatin989Copyright:
Available Formats
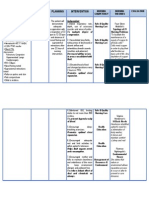
Nursing Care Plan
Name of Patient: Kelly Kaye Lee Date: July 1, 2008 Ward: Pediatric
Age: 3 Sex: Female Weight: 15 kg. (33 lbs.) Shift: 3-11
Diagnosis: Acute Tonsillitis Date of Admission: July 1, 2008
Assessment Explanation of the Objectives Nursing Interventions Rationale Evaluation
Problem
C/C: Sore throat, 3 days Exposure to cold and STO:> Within 8 hours of Dx:> Assess v/s and record. > Provides baseline data for > Goal was fully met as
weather and too much nursing intervention, the Pt. comparison; elevation in evidenced by verbal report
S:> “Masakit lagi yung ingestion of sweets will report a decrease in rates may indicate that pain has decreased
lalamunan niya lalo na pag ↓ level of pain from to , > Assess pain worsening condition. form to , and
lumulunok”, as verbalized Entry of Pathogen and body temperature will characteristics including > Provides baseline data for temperature lowered from
by Pt.’s mother. ↓ lower from 38ºC to 37ºC. location and severity (using comparison and as 38ºC to 37ºC.
> Rated pain as using Disruption of cell the faces scale). reference for appropriate
the faces scale. membrane of tonsils Tx: > Place Pt. in a position diagnosis and management.
↓ of comfort, possibly semi- > Promotes comfort;
O:> Initial v/s taken as Release of chemical Fowler’s. Maximizes respiratory and
follows: mediators cardiac functions.
T= 38ºC ↓ > Offer more fluids and > Promotes adequate
RR= 40 breaths/min Activation of nociceptors LTO:> Within 3 days of semi-solid or moist foods, nutrition while lessening > Goal was fully met. Pt.
CR= 110 bpm ↓ nursing intervention, the Pt. as tolerated. difficulty in swallowing. has non-swollen and non-
> febrile Nerve impulses sent to will manifest the following > Offer ice chips, as > Decreases swelling of the tender lymph nodes on
> with swollen and CNS and are interpreted signs of improved tolerated. tonsils. submandibular area, has
tender lymph nodes on ↓ condition: > Assist Pt. in gargling > Relieves sore throat and pinkish and non-swollen
submandibular area Response of CNS sent to a. non-swollen and non- with saline solution. reduces swelling. tonsils, can easily swallow
> with bright red and systems tender lymph nodes on > Provide diversional >Helps Pt. to cope with fluids and semi-solid or
swollen tonsils ↓ submandibular area activities such as watching incompletely relieved pain. moist foods, and has
> appears irritable > Start of inflammatory b. pinkish and non-swollen TV, giving pop-up or maintained stable v/s.
> has difficulty in process tonsils coloring books, or playing
swallowing - vasodilation (redness) c. can easily swallow fluids with toys. > Promotes energy
A:> Acute pain r/t - increased cell and semi-solid or moist > Promote rest by conservation and lessen
inflammation of tonsils permeability (swelling) foods providing a quiet metabolic demands.
secondary to tonsillitis > Pain perception d. stable v/s environment and limiting
visiting hours. > Facilitates fluid-
> Regulate IVF to electrolyte replacement and
prescribed rate. balance; support circulating
blood volume to hasten
healing process.
> Treats underlying cause
> Administer antibiotics, of inflammation.
as ordered. > Decreases level of pain.
> Administer analgesics,
as ordered. > Facilitates participation
Edx:>Encourage the of both the Pt. and SOs in
presence of SOs at all the management of the
times, especially during condition.
procedures. > Maintains adequate
> Encourage SOs to hydration.
offer more fluids. > Supports adequate
> Encourage SOs to nutrition while lessening
provide small frequent difficulty in swallowing.
feedings of semi-solid or
moist foods. > Ensures continuity of
> Emphasize the need care; Prevents
to complete the 10-day complications, or
antibiotic regimen. recurrence of condition, or
resistance.
> Emphasize the need > Prevents progression of
to avoid exposure to present condition.
irritants and people with
infectious diseases.
> Explain possible > Prevents complications
complications of conditionand recurrence of
if inadequately treated. condition; Ensures
continuity of care.
> Emphasize preventive > Prevents complications
measures such as non- and recurrence of
exposure to irritants, condition; Ensures
adequate nutrition and continuity of care.
hydration, and vitamin C
supplementation.
Nursing Care Plan
Name of Patient: Lucky Chan Date: July 10, 2008 Ward: Pediatric
Age: 7 mos. Sex: Male Weight: 8 kg. (17.6 lbs.) Shift: 7-3
Diagnosis: Lactose Intolerance-Secondary Date of Admission: July 10, 2008
Assessment Explanation of the Objectives Nursing Interventions Rationale Evaluation
Problem
C/C: Passage of yellowish, Previous diarrhea episode STO: Within 8 hours of Dx:> Assess v/s and record. > Provides baseline data for > Goal was fully met. Pt.’s
watery stools, 8x in the last ↓ nursing intervention, the Pt. comparison; alteration in frequency in passage of
48 h Damage to intestinal villi will have a decreased rates may indicate watery stools decreased
↓ frequency in passage of worsening condition from 8x to 5x and Tº was
S:> “ Pururot, matubig, at Decreased lactase watery stools from 8x to 5x (dehydration). lowered from 37.8ºC to
madilaw yung tae niya production and will have a lowered Tº > Observe and record > Provides baseline data for 37ºC.
kahapon pa”, as verbalized ↓ from 37.8ºC to 37ºC. stool characteristics, comparison and as
by Pt.’s mother. Decreased ability to amount, and frequency of reference for appropriate
breakdown lactose elimination. diagnosis and management.
O:> Initial v/s taken as ↓ > Assess for signs of > Provides baseline data for
follows: Increased amounts of dehydration (pale comparison and as
T= 37.8ºC lactose in the small conjunctiva, poor skin reference for appropriate
RR= 42 breaths/min intestine LTO: Within 3 days of turgor, etc.) diagnosis and management. > Goal was fully met. Pt.
CR= 130 bpm ↓ nursing intervention, the Pt. > Monitor I and O. > A decrease in output may manifested improved
> passage of yellowish GIT microflora ferment will manifest improved indicate dehydration, hydration state as
watery stools, 8x in the last lactose hydration state as urinary, or absorption evidenced by non-sunken
48 h ↓ evidenced by non-sunken problems. eyes and good skin turgor-
> frequent flatus a. Gas (CO2) and acid eyes and good skin turgor- Tx: > Give ORS, as > Facilitates fluid- skin returned to normal
> sunken eyes (lactic) production skin returned to normal necessary. electrolyte replacement and position immediately;
> poor skin turgor-skin > gas=flatus position immediately ; balance. improved bowel
returned to normal position > acid=present in stool improved bowel > Give supplemental > Promotes adequate elimination pattern and
slowly b. Increased water retention elimination pattern and semi-solid foods, as nutrition. characteristics, as
> appears irritable; cries > =watery stool characteristics: tolerated and as necessary. evidenced by:
most of the time c. GIT transit time is a. passing out of light > Provide prompt > Maintains skin integrity; a. passing out of light
shortened yellowish semi-formed diaper change and gentle Prevents growth of MOs. yellowish semi-formed
A:> Diarrhea r/t > = frequency stools cleansing. stools
malabsorption of lactose b. decreased frequency in > Provide diversional > Helps keep the infant b. decreased frequency in
secondary to lactose passage of stools from 8x to activities such as playing from crying therefore passage of stools from 8x to
intolerance 3x with toys and socialization. decreases metabolic 3x
c. flatus significantly demands and keeps v/s c. significant decreased in
decreased stable. passing flatus
> Promote adequate rest > Decreases metabolic
periods. demands essential for
healing.
> Provide for temporary > Promotes adequate
change in diet or milk nutrition and healing while
formula, as ordered. preventing aggravation of
condition.
> Regulate IVF to > Facilitates fluid-
prescribed rate. electrolyte replacement and
balance; support circulating
blood volume to hasten
healing process.
Edx:> Encourage SOs esp. > Facilitates participation
the mother to be present at of both the Pt. and SOs in
all times esp. during the management of the
procedures. condition.
> Instruct SOs on ORS > Promotes fluid-
preparation, indications, electrolyte replacement and
and dosages. balance; Ensures continuity
of care.
> Encourage SOs to > Promotes adequate
provide lactose-free nutrition; Presents
supplemental feedings to variations in feeding.
infant as necessary.
> Explain to SOs the > Facilitates understanding
mechanism of the condition and cooperation of SOs.
(cause/s, management,
prognosis, etc.)
CASE 1:
A 3 year-old female child was brought to the hospital by her mother due to sore throat for 3 consecutive days. The mother verbalized that she is most worried about the pain felt by
her child especially when swallowing which causes her to eat and drink inadequately. The mother claimed that it started with a simple sore throat described to her as somewhat
itchy so she let the child gargle with saline solution but to no avail. During the second and third days, the child reported to her pain and difficulty in swallowing which made
feeding and drinking problematic, although the mother claimed that her child was still able to feed and drink even in small amounts. For the past 3 days, the child was reportedly
afebrile. When asked on what she thinks might have caused such condition, the mother reported that the child was exposed to the cold weather or “nahamugan” during their
vacation and that the child was very fond of eating sweets and chocolates. Assessment of the child revealed the following:
> throat pain rated as using the faces scale
> T= 38ºC (febrile)
> RR= 40 breaths/min (increased)
> CR= 110 bpm (increased)
> swollen and tender lymph nodes on submandibular area
> bright red and swollen tonsils
> appears irritable
> notable difficulty in swallowing
CASE 2:
A 7–month old female infant was brought to the hospital due to passage of yellowish watery stools for 8 times for the last 48 hours. The mother verbalized her worries since this is
the second diarrhea episode of the infant in the last 2 weeks; the first was due to bacterial infection. Because of this, the mother continued breastfeeding the infant by demand.
However, 2 days ago the infant started passing out yellowish watery stools again, accompanied by frequent flatulence. She also noted that her baby has been irritable and cries
most of the time since the condition started. The mother then increased the infant’s frequency in breastfeeding (since she was unsure in giving the infant ORS and feels that the
infant is not yet ready for semi-solid foods), but this action seemed to aggravate the infant’s condition so she immediately brought the infant to the hospital. Assessment of the
infant revealed the following:
> T= 37.8ºC (slightly increased)
> RR= 42 breaths/min
> CR= 130 bpm
> passage of yellowish watery stools, 8x in the last 48 h
> frequent flatus
> sunken eyes
> poor skin turgor-skin returned to normal position in 4 s
> appears irritable, cries most of the time
You might also like
- Assessment Objectives: "Masakit Lagi Yung Lalamunan NyaDocument3 pagesAssessment Objectives: "Masakit Lagi Yung Lalamunan Nyaangel_pearl413100% (2)
- NCPDocument1 pageNCPJ. ishtelleNo ratings yet
- NURSING-CARE-PLAN-Lung-Cancerxxx 1Document3 pagesNURSING-CARE-PLAN-Lung-Cancerxxx 1Caroline ChaNo ratings yet
- NCP TonsilitisDocument11 pagesNCP TonsilitisGra Cie50% (6)
- Drug NameDocument4 pagesDrug Namecheanne003No ratings yet
- Assessment Diagnosis Planning Intervention Rationale EvaluationDocument2 pagesAssessment Diagnosis Planning Intervention Rationale EvaluationRomeo Avecilla CabralNo ratings yet
- Neonatal Sepsis NCPDocument9 pagesNeonatal Sepsis NCPHollan Galicia100% (1)
- Disturbed SleepDocument1 pageDisturbed Sleepmawel100% (1)
- Assessing and Managing Ineffective Airway ClearanceDocument3 pagesAssessing and Managing Ineffective Airway ClearanceNelle Agni100% (1)
- Nursing Care Plan Ineffective Airway Clearance (Bronchi)Document2 pagesNursing Care Plan Ineffective Airway Clearance (Bronchi)deric94% (17)
- Nursing Care Plan for Enhanced NutritionDocument2 pagesNursing Care Plan for Enhanced NutritionHippocrates Impressionist CostalesNo ratings yet
- Nursing Care PlanDocument2 pagesNursing Care PlanAbby GuiritanNo ratings yet
- NCP DobDocument3 pagesNCP DobLester BuhayNo ratings yet
- Nursing Care Plan Assessment Diagnosis Planning Implementation Rationale EvaluationDocument1 pageNursing Care Plan Assessment Diagnosis Planning Implementation Rationale EvaluationMyrien BanaagNo ratings yet
- NCP GrandcaseDocument5 pagesNCP GrandcaseSaima BataloNo ratings yet
- Nursing Care PlansDocument4 pagesNursing Care PlansanreilegardeNo ratings yet
- Assess and Care for Impaired Oral Mucous MembranesDocument2 pagesAssess and Care for Impaired Oral Mucous MembranesNolan Cabral100% (1)
- Nursing Care Plan: Cues Nursing Diagnosis Desired Outcome Interventions Rationale EvaluationDocument3 pagesNursing Care Plan: Cues Nursing Diagnosis Desired Outcome Interventions Rationale EvaluationPsycheNo ratings yet
- NCP For Ineffective Breathing Pattern - RMC CasepressDocument2 pagesNCP For Ineffective Breathing Pattern - RMC Casepressmissyuri08No ratings yet
- Nursing Care PlanDocument1 pageNursing Care PlanSHeenah Qo100% (1)
- Nursing DX: Acute Pain Related To Surgical Manipulation (Laminectomy) As Manifested by Reports of Pain On The Lumbar Area Rated As 7/10Document1 pageNursing DX: Acute Pain Related To Surgical Manipulation (Laminectomy) As Manifested by Reports of Pain On The Lumbar Area Rated As 7/10YESSAMIN GUADIZ100% (2)
- N C P For Perioperative Pts.Document4 pagesN C P For Perioperative Pts.Daisy Palisoc100% (1)
- NCP Delayed Wound RecoveryDocument5 pagesNCP Delayed Wound RecoveryDarkCeades100% (2)
- CARAGAN, Chantal Herpes Zoster Assessment Diagnosis Planning Interventions Rationale Evaluation Subjective: Short Term: Independent: Short TermDocument4 pagesCARAGAN, Chantal Herpes Zoster Assessment Diagnosis Planning Interventions Rationale Evaluation Subjective: Short Term: Independent: Short TermChantal Caragan100% (2)
- NCP PEDIA TonsillitisDocument2 pagesNCP PEDIA Tonsillitisdeliejoyce100% (1)
- NCPDocument4 pagesNCPMichelleNo ratings yet
- NCPDocument2 pagesNCPNikai PabayoNo ratings yet
- NCP Acute Pain RT CancerDocument3 pagesNCP Acute Pain RT CancerCharissa Magistrado De LeonNo ratings yet
- Delayed Growth NCPDocument3 pagesDelayed Growth NCPPau-pau BasiNo ratings yet
- Risk For Acute ConfusionDocument2 pagesRisk For Acute ConfusionChar PereaNo ratings yet
- NCP FoodDocument1 pageNCP FoodAdrian ArdamilNo ratings yet
- Fluid Volume DeficitDocument1 pageFluid Volume DeficitventimiglionNo ratings yet
- Nursing Care Plan for TonsillitisDocument3 pagesNursing Care Plan for TonsillitisEden Cruz40% (5)
- NCP AfDocument3 pagesNCP AfAngelica Mercado SirotNo ratings yet
- Hyperthermia NCPDocument3 pagesHyperthermia NCPJayr DiazNo ratings yet
- Impaired Verbal CommDocument3 pagesImpaired Verbal CommKM100% (2)
- Ineffective Airway ClearanceDocument1 pageIneffective Airway Clearancerozj0750% (2)
- Fluid Volume Assessment for Amoebiasis PatientDocument3 pagesFluid Volume Assessment for Amoebiasis PatientRellie CastroNo ratings yet
- NCP - Ineffective Airway ClearanceDocument2 pagesNCP - Ineffective Airway Clearancelarapatricia1215No ratings yet
- Case NCPDocument25 pagesCase NCPJoher Bolante Mendez100% (1)
- Drug Study Drug Name Mechanism of Action Dosage Indication Contraindication Side Effects Nursing InterventionsDocument5 pagesDrug Study Drug Name Mechanism of Action Dosage Indication Contraindication Side Effects Nursing InterventionsYvonne AgathaNo ratings yet
- Assessment Diagnisis Planning Intervention Rationale Evaluation SubjectiveDocument2 pagesAssessment Diagnisis Planning Intervention Rationale Evaluation SubjectiveDanica Kate GalleonNo ratings yet
- Nursing Measures To Maintain Normal Respiratory Function and OxygenationDocument2 pagesNursing Measures To Maintain Normal Respiratory Function and Oxygenationlodeth100% (2)
- NCP For Ears Nose ThroatDocument1 pageNCP For Ears Nose ThroatMcmac YangoNo ratings yet
- NCP - Anxiety Hypertension)Document3 pagesNCP - Anxiety Hypertension)Jaja Jaime100% (2)
- Ncp.-Fluid Volume DeficitDocument1 pageNcp.-Fluid Volume DeficitAdia Cavrinni De JesusNo ratings yet
- Betty Impaired Skin IntegrityDocument2 pagesBetty Impaired Skin IntegrityBenjie DimayacyacNo ratings yet
- Cleft Lip Palate NCPDocument2 pagesCleft Lip Palate NCPLerma PagcaliwanganNo ratings yet
- Nursing Care Plan ADocument6 pagesNursing Care Plan ACrystal WyattNo ratings yet
- NCP Pre EclampsiaDocument2 pagesNCP Pre EclampsiaFarrah Grace Birowa0% (1)
- Smart 2a Module3Document2 pagesSmart 2a Module3Mark Kenneth CeballosNo ratings yet
- NCP DMDocument6 pagesNCP DMstara123No ratings yet
- NCP-S/P AppendectomyDocument6 pagesNCP-S/P Appendectomytinatin989100% (7)
- Actual and Potential NCPDocument5 pagesActual and Potential NCPkevinzky100% (4)
- Managing Pain and Improving Comfort for a Patient with Urinary Tract InfectionDocument6 pagesManaging Pain and Improving Comfort for a Patient with Urinary Tract InfectionApril Ann PonceNo ratings yet
- 5 Benign Febrile Convulsions Nursing Care PlansDocument19 pages5 Benign Febrile Convulsions Nursing Care Plansaaron tabernaNo ratings yet
- Nursing Care for Post-Appendectomy PainDocument3 pagesNursing Care for Post-Appendectomy PainChristian Karl B. LlanesNo ratings yet
- NCP - Ineffective Airway Clearance R/T Retained Secretions 2° BPNDocument1 pageNCP - Ineffective Airway Clearance R/T Retained Secretions 2° BPNCarl Elexer Cuyugan Ano100% (2)
- NCP OB PainDocument1 pageNCP OB PainLouije MombzNo ratings yet
- Ineffective Tissue Perfusion Related To Decrease Hemoglobin Concentration in The BloodDocument2 pagesIneffective Tissue Perfusion Related To Decrease Hemoglobin Concentration in The BloodKit Alizon BarredoNo ratings yet
- To Douche or Not To DoucheDocument11 pagesTo Douche or Not To Douchetinatin989No ratings yet
- Journal On NSAIDs/Catheter UTI-reactionDocument3 pagesJournal On NSAIDs/Catheter UTI-reactiontinatin989No ratings yet
- Philifornia Foundation: Bringing The Best of Californian Healthcare To The Filipino PeopleDocument4 pagesPhilifornia Foundation: Bringing The Best of Californian Healthcare To The Filipino Peopletinatin989No ratings yet
- Grad SpeechDocument3 pagesGrad Speechtinatin989No ratings yet
- Double Gloving/surgical TimeOut-ReactionDocument2 pagesDouble Gloving/surgical TimeOut-Reactiontinatin989No ratings yet
- NCP-impaired Urinary Elimination-TAHBSODocument3 pagesNCP-impaired Urinary Elimination-TAHBSOtinatin9890% (1)
- Cranberries Give Boost To Cancer Drug-ReactionDocument3 pagesCranberries Give Boost To Cancer Drug-Reactiontinatin989No ratings yet
- Pathophysiology of Aplastic AnemiaDocument1 pagePathophysiology of Aplastic Anemiatinatin989100% (2)
- NCP-Esophageal Varices Pleural EffusionDocument6 pagesNCP-Esophageal Varices Pleural Effusiontinatin98933% (3)
- Clinical Paper-Acute Respi InfectionDocument11 pagesClinical Paper-Acute Respi Infectiontinatin989No ratings yet
- NCP-S/P AppendectomyDocument6 pagesNCP-S/P Appendectomytinatin989100% (7)
- Pathophysiology of Endometrial HyperplasiaDocument1 pagePathophysiology of Endometrial Hyperplasiatinatin989100% (2)
- Case Study Herniated DiscDocument20 pagesCase Study Herniated Disctinatin98960% (5)
- Pathophysiology of AppendicitisDocument1 pagePathophysiology of Appendicitistinatin98994% (17)
- Pathophysiology of AGEDocument1 pagePathophysiology of AGEtinatin9890% (1)
- Initial Database For Family Nursing Care-HeCare1Document5 pagesInitial Database For Family Nursing Care-HeCare1tinatin989No ratings yet
- Journal On NSAIDs/Catheter UTI-reactionDocument3 pagesJournal On NSAIDs/Catheter UTI-reactiontinatin989No ratings yet
- Case Analysis-Health EconDocument12 pagesCase Analysis-Health Econtinatin989No ratings yet
- The Effect of Piezoelectric and Magnetostrictive Scaling DevicesDocument38 pagesThe Effect of Piezoelectric and Magnetostrictive Scaling Devicesnotaden1849No ratings yet
- (90-55-3000) BIOLIS 50i - Operator's M - V5.7 PDFDocument498 pages(90-55-3000) BIOLIS 50i - Operator's M - V5.7 PDFMatrix100% (1)
- Carrillo & Associates, Inc: Rosa Antonia Carrillo, MSODDocument3 pagesCarrillo & Associates, Inc: Rosa Antonia Carrillo, MSODalberto1954No ratings yet
- Psychiatric Mental Health Nursing SuccessDocument407 pagesPsychiatric Mental Health Nursing Successwhatever1919191986% (49)
- Role of Fats in Periodontal DiseaseDocument9 pagesRole of Fats in Periodontal DiseaseandrealezamaNo ratings yet
- Interpretation of Abnormal CTG Pattern - 2Document17 pagesInterpretation of Abnormal CTG Pattern - 2Jaspreet Kaur100% (1)
- Hse Pja BtsguideDocument2 pagesHse Pja BtsguideMohamed Ismail ShehabNo ratings yet
- Dutra de Souza 2023Document11 pagesDutra de Souza 2023Paulo Emilio Marchete RohorNo ratings yet
- Lab-Ncm 105-Learn Mat Topic 1 WC WL Ob 2022-2023 1st SemDocument6 pagesLab-Ncm 105-Learn Mat Topic 1 WC WL Ob 2022-2023 1st SemDobby AsahiNo ratings yet
- WREE 4710 Water Supply LectureDocument13 pagesWREE 4710 Water Supply LectureZeleke TaimuNo ratings yet
- SW 103 2nd Topic PDFDocument12 pagesSW 103 2nd Topic PDFMarielle BringasNo ratings yet
- The Dark Triada Personality A Review PDFDocument18 pagesThe Dark Triada Personality A Review PDFAvengingBrainNo ratings yet
- PhD Fluid MechanicsDocument4 pagesPhD Fluid MechanicsGooftilaaAniJiraachuunkooYesusiinNo ratings yet
- Straight 5 2018 Super Mock Exam Samples: Sample Essay CollectionDocument25 pagesStraight 5 2018 Super Mock Exam Samples: Sample Essay CollectionPak Hei ChanNo ratings yet
- Factors Influencing Health Status (FIHS) : Rating GuidelinesDocument3 pagesFactors Influencing Health Status (FIHS) : Rating GuidelinesAyan Kumar GhoshNo ratings yet
- Gonzales Cannon Issue Nov. 3, 2011Document32 pagesGonzales Cannon Issue Nov. 3, 2011Nikki MaxwellNo ratings yet
- Instructions For Treatment and Use of Insecticide-Treated Mosquito NetsDocument51 pagesInstructions For Treatment and Use of Insecticide-Treated Mosquito NetsMaxwell WrightNo ratings yet
- Narrative Report: Intro To GMP, Hand Washing and Personal HygieneDocument6 pagesNarrative Report: Intro To GMP, Hand Washing and Personal HygieneKrystelle Mae Salas AbuyogNo ratings yet
- 2 Exam Budding ScientistsDocument3 pages2 Exam Budding ScientistsWassila Nour100% (1)
- Family Welfare Programme in IndiaDocument25 pagesFamily Welfare Programme in IndiaTirumalesha DadigeNo ratings yet
- RMT TrainningDocument2 pagesRMT TrainningDita Nadya RizkitaNo ratings yet
- GINA 2021 Guidelines for Asthma Diagnosis and TreatmentDocument24 pagesGINA 2021 Guidelines for Asthma Diagnosis and TreatmentBianca Watanabe - RatillaNo ratings yet
- Posterior Open Bite CausesDocument30 pagesPosterior Open Bite CauseschaitreeNo ratings yet
- Personal Data Sheet: Marcial Roel FranciscoDocument13 pagesPersonal Data Sheet: Marcial Roel FranciscoRoel MarcialNo ratings yet
- Soal Hots Bhs InggrisDocument2 pagesSoal Hots Bhs Inggrisdea ayu puspitaNo ratings yet
- Good Governance IndexDocument112 pagesGood Governance IndexWilliam ObengNo ratings yet
- Observational Studies: Usmle Endpoint StatisticsDocument32 pagesObservational Studies: Usmle Endpoint Statisticskarim khalil100% (1)
- Amniotic MembraneDocument8 pagesAmniotic Membraneapi-481789048No ratings yet
- Chinese General Hospital Nursing College Functional Pattern GuideDocument2 pagesChinese General Hospital Nursing College Functional Pattern GuideTin BernardezNo ratings yet
- Material Safety Data Sheet: Section 1 - Product InformationDocument2 pagesMaterial Safety Data Sheet: Section 1 - Product Informationmohamed AdelNo ratings yet