Professional Documents
Culture Documents
Posttest Urinary
Uploaded by
AilatiLiamOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Posttest Urinary
Uploaded by
AilatiLiamCopyright:
Available Formats
Post-Test
1. Assessment factors which determine severity of burns are the following except:
a. Age and general health
b. Height and weight
c. Site of burns
d. Associated injuries and causative agents
2. Plan of care of burns includes the following:
i. Patent airway established
ii. Degree of burns and extent are determined
iii. Fluid balance maintained
iv. Tetanus toxoid
a. 1, 2 and 3 only
b. 2, 3 and 4 only
c. 1, 2 and 4
d. 1 to 4
SITUATION: A Recent fire in SM Makati (shoemart) has caused several lives of firemen injured and burned,
mostly third degree burns. Numbers 56 to 62 refer to BURNS.
3. Assessment of severity of burns is determined by:
i. Type of chemicals which caused the fire
ii. Depth of tissue damaged
iii. Extent of body surface burned
iv. How the patient was burned
a. 1, 2 and 3
b. 2 and 3
c. 2, 3 and 4
d. All of the above
4. Use of Rule of Nines is one of the common guides in:
a. Determining the percentage of body surface burned
b. Determining the depth of body tissue burned
c. Determining the severity of tissue damaged
d. All of the above
5. Which of the following measures the ER nurse would do first?
a. Prepare patient for IV insertion
b. Remove patients clothing and wash burns
c. Check patients vital signs for signs of respiratory distress
d. Dress the burned areas with sterile Vaseline
6. During the first 48 hours, nursing measures should be focused on the following except:
a. I and O hourly
b. Strict aseptic technique
c. Forced oral fluids
d. Isolate patient
7. Which of these developments should be noted within 24-48 hours for patients with third degree burns?
a. Infection
b. Hypostatic pneumonia
c. Phlebitis
d. Oliguria
8. Most common complication of extensive burns is:
a. Infection after shock
b. Pneumonia
c. Deformities
d. Dehydration
9. Symptoms of shock that may result after severe burns are:
a. Increased respiration, skin, cold and clammy, rapid pulse
b. Increased respiration, cold and clammy skin, decreased pulse
c. Slow respiration, warm skin, rapid pulse
d. Slow respiration, warm skin, rapid pulse
10. The nurse is reviewing the laboratory results of a client diagnosed with multiple myeloma. Which of the
following would the nurse expect to note specifically in this disorder?
a. Increased calcium level
b. Increased WBC
c. Decreased BUN level
d. Decreased plasma cells in the bone marrow
11. Nurse Liza is assigned to care for a client who has returned to the nursing unit after left
nephrectomy. Nurse Lizas highest priority would be
a. Hourly urine output
b. Temperature
c. Able to turn side to side
d. Able to sips clear liquid
12. The nurse observed the UAP performing perineal care for a client. Which of the following actions
indicates that further teaching is required?
a. Used a clean portion of the washcloth for each stroke
b. Wiped from the pubis to the rectum
c. Used clean gloves
d. Did not retract the foreskin
13. Because a client reports having dyspareunia, it is most appropriate to ask which of the following
questions?
a. Have you talked with your partner about this discomfort?
b. Have you had these spasms since you become sexually active?
c. Do you have pain before your period begins?
d. Do your breasts swell large enough to need a larger bra?
SHOCK and MULTISYSTEM FAILURE
14. The primary mechanism of blood pressure regulation results from the initial stimulation of _____
receptors.
a. Chemical
b. Hormonal
c. Neural
d. Pressure
15. Calculate a patients mean arterial pressure (MAP) when the blood is 110/70.
a. 65
b. 73
c. 83
d. 91
16. The stage of shock characterized by a normal blood pressure is the ___ stage:
a. Initial
b. Compensated
c. Progressive
d. Irreversible
17. A nurse assesses a patient in shock whose lungs have decompensated. The nurse would not expect to
find the following symptoms:
a. A heart rate >100/min
b. Crackles
c. Lethargy and mental confusion
d. Respirations fewer than 15/min
18. Oliguria occurs in the progressive stage of shock because the kidneys decompensate. To assess for this
condition, the nurse should look for the following signs and symptoms:
a. Congestive heart failure
b. Decreased capillary permeability and localized edema
c. Increased BUN and serum creatinine
d. Systolic BP >120mmHg
19. Hematologic system changes in the progressive shock would not be characterized by:
a. Generalized hypoxemia
b. Hypertension
c. Metabolic acidosis
d. Sluggish blood flow
20. Depleted ATP stores and multiple organ failure are characteristic of the ____ stage of shock:
a. Initial
b. Compensatory
c. Progressive
d. Irreversible
21. The primary goal in treating cardiogenic shock is to:
a. Improve the hearts pumping
mechanism
b. Limit further myocardial damage
c. Preserve the healthy myocardium
d. Treat the oxygenation needs of the
heart muscle
22. The drug of choice for cardiac pain relief is IV:
a. Codeine
b. Demerol
c. Dilaudid
d. Morphine
23. Sympathomimetic drugs increase cardiac output by all of the following except:
a. Decreasing preload and afterload
b. Increasing myocardial contractility
c. Tachycardia
d. Vasoconstriction
24. The vasoactive effects of dopamine are diminished when high doses are given because vasoconstriction
increases cardiac workload. Doses are titrated for therapeutic range. A nontherapeutic drug dose for a
154-lb (70kg) man would be:
a. 210g/min
b. 350g/min
c. 490g/min
d. 630g/min
25. The negative effect of intravenous nitroglycerin (Tridil) for shock management is:
a. Reduced preload
b. Reduced afterload
c. Increased cardiac output
d. Increased blood pressure
26. Intra-aortic balloon counterpulsation (IABC) is a mechanical device; assistive device used as a
temporary means of improving the hearts pumping ability. IABC is primarily meant to:
a. Decrease cardiac work b. Decrease stroke volume
c. Increase preload d. Maintain current coronary
circulation
27. The primary etiology of distributive shock is:
a. Arterial and venous dilatation
b. Compromised cardiac contractility
c. Decreased blood volume
d. Obstructed blood flow
28. Patients receiving fluid replacement should frequently be monitored for:
a. Adequate urinary output
b. Changes in the mental status
c. Vital sign stability
d. All of the above
29. The most commonly used colloidal solution to treat hypovolemic shock:
a. Blood products
b. 5% albumin
c. 6% dextran
d. 6% hetastarch
30. Vasoactive agents are effective in treating shock because of their ability to:
a. Decrease blood pressure
b. Decrease stroke volume
c. Increase cardiac output
d. Increase cardiac preload
31. A common vasoactive agent used to improve cardiac contractility is:
a. Dopamine
b. Epinephrine
c. Nitroprusside
d. Phenylephrine
32. Approximately how much fluid is lost in acute weight loss of .5kg?
A. 50 ml
B. 750 ml
C. 500 ml
D. 75 ml
ASSESSMENT of URINARY and RENAL FUNCTION
33. An abnormal constituent of urine is:
a. Creatinine
b. Glucose
c. Potassium
d. Urea
34. The normal quantity of water ingested and excreted in the urine is approximately:
a. 0.5L/day
b. 1.5L/day
c. 2.5L/day
d. 4.0L/day
35. The normal amount of sodium ingested and excreted in the urine is approximately:
a. 2 to 3g/day
b. 4 to 5g/day
c. 6 to 8g/day
d. 9 to 10g/day
36. Increased blood osmolality will result in:
a. Antidiuretic hormone (ADH)
stimulation
b. An increase in urine volume
c. Dieresis
d. Less reabsorption of water
37. The nephritic syndrome causes hypoalbuminemia, which results in:
a. Activation of the renin-angiotensin
system
b. Decreased oncotic pressure
c. Edema
d. All of the above
38. A major sensitive indicator of kidney disease is the:
a. Blood urea nitrogen level
b. Creatinine clearance level
c. Serum potassium level
d. Uric acid level
39. A major manifestation of uremia is:
a. A decreased serum phosphorus level
b. Hyperparathyroidism
c. Hypocalcemia with bone changes
d. Increased secretion of parathormone
40. Oliguria is said to be present when urinary output is:
a. Less than 30ml/hr
b. About 100ml/hr
c. Between 300 and 500ml/hr
d. Between 500 and 1000ml/hr
41. Significant nursing assessment data relevant to renal function should include information about:
a. Any voiding disorders
b. The patients occupation
c. The presence of hypertension or
diabetes mellitus
d. All of the above
42. A 24-hour urine collection is scheduled to begin at 8am. The nurse should begin the procedure:
a. After discarding the 8am specimen
b. At 8am,with or without a specimen
c. 6 hours after the urine is discarded
d. With the first specimen voided after
8am
43. The nurse should inform a patient that preparation for intravenous pyelography includes:
a. A liquid restriction for 8 to 10 hours
before the test
b. Liquids before the test
c. Enemas until clear
d. Remaining NPO from midnight before
the test
44. Nursing responsibilities after renal angiography include:
a. Assessment of peripheral pulses
b. Color and temperature comparisons between the involved and uninvolved extremities
c. Examination of the puncture site for swelling and hematoma formation
d. All of the above
45. A cystoscope allows visualization of the:
a. Bladder
b. Ureteral orifices
c. Urethra
d. Above areas
46. Nursing management after a renal biopsy includes:
a. Assessing for the clinical manifestations of hemorrhage
b. Encouraging a fluid intake of 3L every 24 hours
c. Obtaining a sample of each voided urine to compare it with a prebiopsy specimen
d. All of the above
MANAGEMENT of PATIENTS with URINARY and RENAL DYSFUNCTION
47. The most accurate indicator of fluid loss or gain in an acutely ill patient is:
a. Blood pressure
b. Capillary refill
c. Serum sodium levels
d. Weight
48. The type of incontinence that results from a sudden increase in intra-abdominal pressure is:
a. Reflex incontinence
b. Stress incontinence
c. Overflow incontinence
d. Urge incontinence
49. The major cause of death for patients with neurologic impairment of the bladder is:
a. Myocardial infarction
b. Pulmonary edema
c. Septicemia
d. Renal failure
50. A spastic neurogenic bladder is associated with all of the following except:
a. A loss of conscious sensation and cerebral motor control
b. A lower motor neuron lesion
c. Hypertrophy of the bladder walls
d. Reduced bladder capacity
51. . The major complication of neurogenic bladder is:
a. Hypertrophy
b. Infection
c. Pain
d. Spasm
52. Nursing measures for a patient with a neurogenic bladder include:
a. Encouraging a liberal fluid intake
b. Keeping the patient as mobile as
possible
c. Offering a diet low in calcium
d. All of the above
53. When managing a closed urinary drainage system, the nurse needs to remember not to:
a. Allow the drainage bag touch to the floor
b. Disconnect the bag
c. Raise the drainage bag above the level of the patients bladder
d. Do any of the above
54. A sign of a possible urinary tract infection is:
a. A negative urine culture
b. An output of 200 to 900ml with each
voiding
c. Cloudy urine
d. Urine with a specific gravity of 1.005
to 1.022
55. A female patient is taught to catheterize herself by inserting the catheter into the urethra:
a. to 1in
b. 2in
c. 3in
d. 5in
MANAGEMENT of PATIENTS with BURN INJURY
56. A full thickness burn is:
a. classified by the appearance of blisters
b. identified by the destruction of the
entire dermis
c. not associated with edema formation
d. usually very painful because of exposed
nerve endings
57. With partial-thickness (second-degree) burns, skin regeneration begins to take place:
a. Within 7 days b. In 2 to 4 weeks
c. After 2 months d. Between the third and sixth months
58. Plasma seeps out into surrounding tissue after a burn. The greatest amount of fluid leaks out in:
a. The first 2 hours
b. 4 to 8 hours
c. 12 hours
d. 24 to 36 hours
59. As fluid is reabsorbed after injury, renal function maintains a dieresis for up to:
a. 3 days
b. 1 week
c. 2 weeks
d. 1 months
60. Fluid shifts during the first week of the acute phase of a burn injury cause electrolyte movements that
result in:
a. Hypernatremia
b. Hypokalemia
c. Hyperkalemia
d. Hypercalcemia
61. An unexpected laboratory value during the fluid remobilization phase of a major burn is a:
a. Hematocrit of 45%/dl
b. pH 7.20; PaO2 38 torr; bicarbonate
15mEq/L
c. serum potassium of 3.2 mEq/L
d. serum sodium of 140mEq/L
62. Plasma leakage produces edema, which increases:
a. Circulating blood volume
b. The hematocrit level
c. Systolic blood level
d. All of the above
63. The leading cause of death in fire victims is believed to be:
a. Cardiac arrest
b. Carbon monoxide intoxication
c. Hypovolemic shock
d. Septicemia
64. A serious gastrointestinal disturbance that frequently occurs with a major burn is:
a. Diverticulitis
b. Hematemesis
c. Paralytic ileus
d. Ulcerative colitis
65. A child tips a pot of boiling water onto his bare legs. The mother should:
a. Avoid touching the burned skin and take the child to nearest emergency department
b. Cover the childs legs with ice cubes secured with a towel
c. Immerse the childs legs in cool water
d. Liberally apply butter or shortening to the burned area
66. A man suffers leg burns from spilled charcoal lighter fluid. His son extinguishes the flames. While
waiting for an ambulance, the burn victim should:
a. Have someone assist him into a bath cool water, where he can wait for emergency personnel
b. Lie down, have someone cover him with a blanket, and cover his legs with petroleum jelly
c. Remove his burned pants so that the air can help cool the wound
d. Sit in a chair, elevate his legs, and have someone cut his pants off around the burned area
67. As the first priority care, a patient with a burn injury will initially need:
a. An airway established
b. An indwelling catheter
c. Fluid replaced
d. Pain medication administered
68. Eyes that have been irritated or burned with a chemical should be flushed with cool, clean water:
a. Immediately
b. In 5 to 10 minutes
c. After an eye examination
d. After 24 hours
69. Decreased urinary output during the first 48 hours of a major burn is secondary to all of the following
except:
a. Decreased adrenocortical activity
b. Hypernatremia
c. Hypovolemia
d. Sodium retention
70. Electrolyte changes in the first 48 hours of a major burn include:
a. Base bicarbonate deficit
b. Hypernatremia
c. Hypokalemia
d. All of the above
71. The Evan formula for replacing fluid lost during the first 24 to 48 hours recommends the
administration of:
a. Colloids
b. Electrolytes
c. Glucose
d. All of the above
72. The most recent Concensus formula for fluid replacement recommends that a balanced salt solution be
administered in the first 24 hours of a burn in the range of 2ml.kg/% of burn. A 176lb (80kg) man
with a 30% burn should receive:
a. 1200ml in the first 8 hours
b. 2400ml in the first 8 hours
c. 3600ml in the first 8 hours
d. 4800ml in the first 8 hours
73. One parameter of adequate fluid replacement is an hourly urinary output in the range of:
a. 10 to 30ml
b. 30 to 50ml
c. 80 to 120ml
d. 100 to 200ml
74. Fluid remobilization usually begins:
a. Within the first 24 hours, when massive amounts of fluid are being administered intravenously
b. After 48 hours, when fluid is being reabsorbed from the interstitial tissue
c. After 1 week, when capillary permeability has returned to normal
d. After 1 month, when scar tissue covers the wound and prevents evaporative fluid loss
75. Wound cleansing and debridement usually begin when eschar begins to separate at:
a. 72 hours
b. 1 week
c. 1-1/2 to 2 weeks
d. 1 month
76. Leucopenia within 48 hours is a side effect associated with the topical antibacterial agent:
a. Cerium nitrate solution
b. Gentamicin sulfate
c. Sulfadiazine, silver (Silvadene)
d. Mafenide (sulfamylon)
77. After an occlusive dressing is applied to a burned foot, the foot should be placed in the position of:
a. Adduction
b. Dorsiflexion
c. External rotation
d. Plantar flexion
78. Biological dressings that use skin from living or recently deceased humans are known as:
a. Autografts
b. Heterografts
c. Homografts
d. Xenografts
79. The recommended route for administration of low dose narcotics is:
a. Intramuscular
b. Intravenous
c. Oral
d. Subcutaneous
80. To meet his early nutritional demands for protein, a 198lb (90)kg burned patient ill need to ingest a
minimum of:
a. 90g/day
b. 110g/day
c. 180g/day
d. 270g/day
81. Early indicators of late-stage septic shock include all of the following except:
a. Decreased pulse pressure
b. A full bounding pulse
c. Pale cool skin
d. Renal failure
FLUIDS and ELECTROLYTES: BALANCE and DISTURBANCES
82. A febrile patients fluid output is in excess of normal because of diaphoresis. The nurse should plan
fluid replacement based on the knowledge that insensible losses in an afebrile person are normally not
greater than:
a. 300ml/24hr
b. 600ml/24hr
c. 900ml/24hr
d. 1200ml/24hr
83. A patients serum sodium is within normal range. The nurse estimates that serum osmolality should
be:
a. Less than 136mOsm/kg
b. 280 to 295mOsm/kg
c. Greater than 408mOsm/kg
d. 350 to 544mOsm/kg
84. A nurse is directed to administer a hypotonic intravenous solution. The nurse expects that
compensatory mechanisms associated with hypovolemia would cause all of the following symptoms
except:
a. O.45% sodium chloride
b. O.90% sodium chloride
c. 5% dextrose in water
d. 5% dextrose in normal saline solution
85. A patient is hemorrhaging from multiple trauma sites. The nurse expects that compensatory
mechanisms associated with hypovolemia would cause all of the following symptoms except:
a. Hypertension
b. Oliguria
c. Tachycardia
d. Tachypnea
86. Nursing interventions for a patient with a diagnosis of hyponatremia includes all of the following
except:
a. Assessing for symptoms of nausea and malaise
b. Encouraging the intake of low-sodium liquids, such as coffee or tea
c. Monitoring neurological status
Restricting tap water intake
87. The lungs regulate acid-base balance by all of the following except:
a. Excreting HCO3 in the blood
b. Slowing ventilation
c. Controlling carbon dioxide levels
d. Increasing ventilation
88. For clients with hyponatremia due to fluid retentionTo return a patient with hyponatremia to normal
sodium levels, it is safer to restrict fluid intake than to administer sodium:
a. In patients who are unconscious
b. To prevent fluid overload
c. To prevent dehydration
d. In patients who show neurologic
symptoms
89. Hypernatremia is associated with a:
a. Serum osmolality of 245mOsm/kg
b. Serum sodium of 150mEq/L
c. Urine specific gravity below 1.003
d. Combination of all of the above
90. One of the dangers of treating hypernatremia is:
a. Red blood cell crenation
b. Red blood cell hydrolysis
c. Cerebral edema
d. Renal shutdown
91. Your semiconscious patient presents with restlessness and weakness. He has a dry, swollen tongue.
His body temperature is 99.3 F, and his urine specific gravity is 1.020. Choose the most likely serum
sodium (Na) value for this patient.
a. 110mEq/L
b. 140mEq/L
c. 155mEq/L
d. 165mEq/L
92. A patient is admitted who has had severe vomiting for 24 hours. She states that she is exhausted and
weak. The results of an admitting ECG show flat T waves and ST segment depression. Choose the
most likely potassium (K) value for this patient.
a. 4.0mEq/L
b. 8.0mEq/L
c. 2.0mEq/L
d. 2.6mEq/L
93. A patient complains of tingling in his fingers. He has positive Trousseaus and Chvosteks signs. He
says that he feels depressed. Choose the most likely serum calcium (Ca) value for this patient:
a. 11mg/dl
b. 9mg/dl
c. 7mg/dl
d. 5mg/dl
94. To supplement a diet with foods high in potassium, the nurse should recommend the addition of:
a. Fruits such as bananas
b. Green leafy vegetables
c. Milk and yogurt
d. Nuts and legumes
95. If a patient has severe hyperkalemia, it is possible to administer calcium gluconate intravenously to:
a. Immediately lower the potassium level by active transport
b. Antagonize the action of K on the heart
c. Prevent transient renal failure (TRF)
d. Accomplish all of the above
96. Management of hypercalcemia includes all of the following actions except administration of:
a. Fluid to dilute the calcium levels
b. The diuretic furosemide (Lasix), without saline, to increase calcium excretion through
kidneys
c. Inorganic phosphate salts
d. Intravenous phosphate therapy
97. A patient is admitted with a diagnosis of renal failure. He also mentions that he has stomach distress
and ha ingested numerous antacid tablets over the past 2 days. His blood pressure is 110/70, his face is
flushed, and he is experiencing generalized weakness. Choose the most likely magnesium (Mg)
value.
a. 11mEq/L
b. 5mEq/L
c. 2mEq/L
d. 1mEq/L
98. Management of the foregoing patient should include:
a. Regular diet with extra fruits and green
vegetables
b. Potassium-sparing diuretics
c. Discontinuance of any oral
magnesium salts
d. All of the above measures
99. The most common buffer system in the body is the:
a. Plasma protein buffer system
b. Hemoglobin buffer system
c. Phosphate buffer system
d. Bicarbonate-carbonic system
100. The kidneys regulate acid-base balance by all of the following mechanisms except:
a. Excreting hydrogen ions (H)
b. Reabsorbing or excreting HCO into
the blood
c. Reabsorbing carbon dioxide into the
blood
d. retaining hydrogen ions
You might also like
- A Simple Guide to Hypovolemia, Diagnosis, Treatment and Related ConditionsFrom EverandA Simple Guide to Hypovolemia, Diagnosis, Treatment and Related ConditionsNo ratings yet
- BraKay 5th January, Medical Nursing ClassDocument11 pagesBraKay 5th January, Medical Nursing ClassKwasikyie QuarshieNo ratings yet
- COMPREHENSIVE NURSING ACHIEVEMENT TEST (RN): Passbooks Study GuideFrom EverandCOMPREHENSIVE NURSING ACHIEVEMENT TEST (RN): Passbooks Study GuideNo ratings yet
- Cardio NewDocument10 pagesCardio NewnotadagNo ratings yet
- Foundation of Nursing - Comprehensive Test Part 1 EasyDocument7 pagesFoundation of Nursing - Comprehensive Test Part 1 EasyJeizel MadayagNo ratings yet
- Posttest. Renal DisordersDocument3 pagesPosttest. Renal Disordersjbagacay100% (3)
- Urinary System DisordersDocument14 pagesUrinary System DisordersGideon P. CasasNo ratings yet
- Hematology - 2013 SDDDocument17 pagesHematology - 2013 SDDOrlan Defensor BalanoNo ratings yet
- CorrectsDocument46 pagesCorrectsnursing_hallNo ratings yet
- Chapter 55Document8 pagesChapter 55DelindaEvansNo ratings yet
- L TEST SERIES - 4Document24 pagesL TEST SERIES - 4Dr-Sanjay SinghaniaNo ratings yet
- Chapter 07 - Hematologic ProblemsDocument8 pagesChapter 07 - Hematologic ProblemscariNo ratings yet
- E1 Fall 20Document10 pagesE1 Fall 20Alexander BarbechoNo ratings yet
- Acute Renal Failure-Student-Rapid ReasoningDocument4 pagesAcute Renal Failure-Student-Rapid Reasoningapi-268403950No ratings yet
- Multiple Choice Questions-Acid Base BalanceDocument6 pagesMultiple Choice Questions-Acid Base Balanceyeshi janexoNo ratings yet
- Chapter 33 Lewis Q&ADocument6 pagesChapter 33 Lewis Q&Ajaikovsky100% (2)
- Chapter 42 - Antidiabetic DrugsDocument11 pagesChapter 42 - Antidiabetic DrugsHannaNo ratings yet
- Fundamentals of Nursing Exam 4Document22 pagesFundamentals of Nursing Exam 4Putu EprilianiNo ratings yet
- Medical Surgical NursingDocument179 pagesMedical Surgical NursingLloyd Rafael EstabilloNo ratings yet
- MCQSDocument13 pagesMCQSUzair Khan100% (1)
- Medical Surgical Nursing Pre-Test 2 RATIONALEDocument8 pagesMedical Surgical Nursing Pre-Test 2 RATIONALEBlaine ManiegoNo ratings yet
- CardiovascularDocument3 pagesCardiovascularNicomille T. CaligingNo ratings yet
- Chapter 3 Fluids and Electrolytes - Acid-Base BalanceDocument8 pagesChapter 3 Fluids and Electrolytes - Acid-Base BalanceDiony CruzNo ratings yet
- Fundamentals of Nursing Exam 1Document8 pagesFundamentals of Nursing Exam 1Marjorie TuazonNo ratings yet
- Renal and Urinary SystemDocument5 pagesRenal and Urinary SystemStaceyNo ratings yet
- NCLEX HomeostasisDocument10 pagesNCLEX HomeostasisAngie MandeoyaNo ratings yet
- CH 59 Care of Patients With Problems of The Biliary System and PancreasDocument28 pagesCH 59 Care of Patients With Problems of The Biliary System and Pancreasjrflores1284No ratings yet
- MS Powerpoint ExamDocument31 pagesMS Powerpoint ExamBobet ReñaNo ratings yet
- RN Physiological Integrity GIDocument14 pagesRN Physiological Integrity GIAaLona RobinsonNo ratings yet
- D. Subcuticular SuturingDocument15 pagesD. Subcuticular SuturingkassahunNo ratings yet
- Chapter 32 - Assessment and Management of Patients With HypertensionDocument6 pagesChapter 32 - Assessment and Management of Patients With HypertensionMichael BoadoNo ratings yet
- Medical-Surgical Nursing Exam 6 (50 Items)Document7 pagesMedical-Surgical Nursing Exam 6 (50 Items)lovely_omegaNo ratings yet
- Chronic Kidney Disease: Prepared by Zakia RogerDocument27 pagesChronic Kidney Disease: Prepared by Zakia Rogerbene dugaNo ratings yet
- NeuroSensory ExamsDocument26 pagesNeuroSensory Examsquidditch07100% (1)
- ExamDocument8 pagesExamkrull243No ratings yet
- Chapter 47 - Endocrine SystemDocument3 pagesChapter 47 - Endocrine SystemStacey100% (1)
- Medical Papers 17112018Document36 pagesMedical Papers 17112018maharghafoor786No ratings yet
- Chapter 50: Nursing Management: Endocrine Problems Test BankDocument16 pagesChapter 50: Nursing Management: Endocrine Problems Test BankPrince K. TaileyNo ratings yet
- Chapter 27 - Management of Patients With Dysrhythmias and ConductionDocument8 pagesChapter 27 - Management of Patients With Dysrhythmias and ConductionMichael Boado100% (1)
- College Final Paper 1 (2) - 1Document6 pagesCollege Final Paper 1 (2) - 1Rita MoraaNo ratings yet
- Medical and Surgical NursingDocument4 pagesMedical and Surgical NursingCrystal Ann Monsale TadiamonNo ratings yet
- TP4Document13 pagesTP4AsdfghjlNo ratings yet
- Maternal and Child Health Nursing 1 Saundrs Pink EdDocument149 pagesMaternal and Child Health Nursing 1 Saundrs Pink EdVin SantosNo ratings yet
- Medical Surgical ATI Proctored Exam 2019 Questions and Answers Verified 100Document7 pagesMedical Surgical ATI Proctored Exam 2019 Questions and Answers Verified 100ianshirow834No ratings yet
- Chapter 30 - Management of Patients With Complications From Heart DiseaseDocument7 pagesChapter 30 - Management of Patients With Complications From Heart DiseaseMichael BoadoNo ratings yet
- CA CardiovascularDocument10 pagesCA CardiovascularNina OaipNo ratings yet
- QuizDocument8 pagesQuizJohara Mae De RamaNo ratings yet
- Respiratory Disorder - NclexDocument27 pagesRespiratory Disorder - NclexDefensor Pison GringgoNo ratings yet
- RenalDocument8 pagesRenalVallesh ShettyNo ratings yet
- L Lfiicht : Rtti L (If 1 Ffis1I'1Document14 pagesL Lfiicht : Rtti L (If 1 Ffis1I'1Gloria JaisonNo ratings yet
- Chapter 036Document9 pagesChapter 036Neverends201160% (5)
- GIT DisordersDocument28 pagesGIT Disordersbpt2100% (1)
- D.s.s.aiims Prepration Test Series - 8Document36 pagesD.s.s.aiims Prepration Test Series - 8Dr-Sanjay SinghaniaNo ratings yet
- D.S.S. Aiims Prepration Test Series - 10 DR - SANJAY 7014964651 All Subject MCQDocument24 pagesD.S.S. Aiims Prepration Test Series - 10 DR - SANJAY 7014964651 All Subject MCQDr-Sanjay SinghaniaNo ratings yet
- Gastrointestinal System Review QuestionsDocument10 pagesGastrointestinal System Review QuestionsSiena PlacinoNo ratings yet
- Chapter 39: Nursing Assessment: Gastrointestinal System Test BankDocument6 pagesChapter 39: Nursing Assessment: Gastrointestinal System Test BankNurse UtopiaNo ratings yet
- Care PlanDocument11 pagesCare PlanAlyssa CardinalNo ratings yet
- NCLEX QuestionsDocument5 pagesNCLEX QuestionsMeganNo ratings yet
- 2 Nursing ProcessDocument50 pages2 Nursing ProcesssechzhenNo ratings yet
- Suargey MCQDocument77 pagesSuargey MCQBilal Ahmad100% (1)
- Shock & Fluid Therapy KSKBDocument55 pagesShock & Fluid Therapy KSKBArnold Daniel100% (1)
- Emergency Nursing Pediatric CourseDocument7 pagesEmergency Nursing Pediatric Coursefagawe7100% (1)
- Clinical Signs To Categorize Shock and Target Vasoactive Medications inDocument38 pagesClinical Signs To Categorize Shock and Target Vasoactive Medications inNadifa IffaNo ratings yet
- Pna 2022Document49 pagesPna 2022MafaldaGomesNo ratings yet
- Intraoperative Cardiac ArrestDocument19 pagesIntraoperative Cardiac ArrestMark Andrew CruzNo ratings yet
- Stress Response To Multi TraumaDocument33 pagesStress Response To Multi TraumaFerry SofyanriNo ratings yet
- Sepsis and Nursing Care in Pediatric Patients: Journal of Science and TechnologyDocument3 pagesSepsis and Nursing Care in Pediatric Patients: Journal of Science and TechnologyAli FalihNo ratings yet
- SNHD Protocol ManualDocument128 pagesSNHD Protocol ManualMedic03431100% (6)
- Management of Cardiogenic Shock After Acute - 2023Document10 pagesManagement of Cardiogenic Shock After Acute - 2023Angy KarakostaNo ratings yet
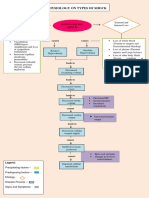
- Pathophysiology On Types of ShockDocument4 pagesPathophysiology On Types of ShockJessa Mae Alforque AsentistaNo ratings yet
- MSF Clinical Guidelines PDFDocument356 pagesMSF Clinical Guidelines PDFKirthinath BallalNo ratings yet
- Trauma/Hypovolaemic Shock: Clinical Practice GuidelinesDocument5 pagesTrauma/Hypovolaemic Shock: Clinical Practice GuidelinesRobertNo ratings yet
- Emergency MedicineDocument346 pagesEmergency MedicineSetio Hartomo100% (6)
- Renal EmergenciesDocument8 pagesRenal EmergenciesRENEROSE TORRESNo ratings yet
- Elementary First Aid Power Point (Efa) - oRIGINALDocument183 pagesElementary First Aid Power Point (Efa) - oRIGINALClark Llamera100% (1)
- Library Dissertation On Dental ImplantsDocument8 pagesLibrary Dissertation On Dental ImplantsHelpWritingPapersForCollegeSalem100% (1)
- Ischaemic Cardiogenic ShockDocument7 pagesIschaemic Cardiogenic ShockHerbert Baquerizo VargasNo ratings yet
- Drug Study PreeclampsiaDocument14 pagesDrug Study PreeclampsiaBiway RegalaNo ratings yet
- NCP - Fluid Volume DeficitDocument2 pagesNCP - Fluid Volume DeficitMarielle Osalvo83% (59)
- 1.1. Pocus en Emg y Critical Care 2018 PDFDocument8 pages1.1. Pocus en Emg y Critical Care 2018 PDFEmergencias RebagliatiNo ratings yet
- Uworld Notes.2 Rounds TPDocument14 pagesUworld Notes.2 Rounds TPjuli100% (1)
- APPENDIX XIII: Daily Lesson Plan - Anaphylaxis Unit (Sample)Document1 pageAPPENDIX XIII: Daily Lesson Plan - Anaphylaxis Unit (Sample)erikriyaNo ratings yet
- Wini JR - Treatment of Suspected Sepsis and Septic Shock in Children With Chronic Disease Seen in The Pediatric Emergency DepartmDocument6 pagesWini JR - Treatment of Suspected Sepsis and Septic Shock in Children With Chronic Disease Seen in The Pediatric Emergency DepartmwiniNo ratings yet
- Burns - Lewis Flashcards - QuizletDocument31 pagesBurns - Lewis Flashcards - QuizletNursyNurseNo ratings yet
- Ch. 19. Postoperative Nursing CareDocument51 pagesCh. 19. Postoperative Nursing Careمحمد الحواجرةNo ratings yet
- 10.6.09 Altman Lactic AcidosisDocument11 pages10.6.09 Altman Lactic AcidosisCosmina Andreea TudoracheNo ratings yet
- Dehydration AssessmentDocument2 pagesDehydration AssessmentzaheerbdsNo ratings yet
- Lesson Plan On Shock and HaemorrhageDocument44 pagesLesson Plan On Shock and HaemorrhageVeenasravanthiNo ratings yet
- 4 Perioperative NursingDocument216 pages4 Perioperative Nursingmaricor_28174462No ratings yet
- NORADRENALINE (Norepinephrine) : Presentation DescriptionDocument3 pagesNORADRENALINE (Norepinephrine) : Presentation DescriptionMutiaraNo ratings yet
- Strong Is the New Beautiful: Embrace Your Natural Beauty, Eat Clean, and Harness Your PowerFrom EverandStrong Is the New Beautiful: Embrace Your Natural Beauty, Eat Clean, and Harness Your PowerRating: 4 out of 5 stars4/5 (5)
- Chair Yoga: Sit, Stretch, and Strengthen Your Way to a Happier, Healthier YouFrom EverandChair Yoga: Sit, Stretch, and Strengthen Your Way to a Happier, Healthier YouRating: 3.5 out of 5 stars3.5/5 (5)
- Functional Training and Beyond: Building the Ultimate Superfunctional Body and MindFrom EverandFunctional Training and Beyond: Building the Ultimate Superfunctional Body and MindRating: 4.5 out of 5 stars4.5/5 (1)
- Power of 10: The Once-A-Week Slow Motion Fitness RevolutionFrom EverandPower of 10: The Once-A-Week Slow Motion Fitness RevolutionRating: 3.5 out of 5 stars3.5/5 (11)
- Peak: The New Science of Athletic Performance That is Revolutionizing SportsFrom EverandPeak: The New Science of Athletic Performance That is Revolutionizing SportsRating: 5 out of 5 stars5/5 (96)
- Aging Backwards: Reverse the Aging Process and Look 10 Years Younger in 30 Minutes a DayFrom EverandAging Backwards: Reverse the Aging Process and Look 10 Years Younger in 30 Minutes a DayNo ratings yet
- Whole Body Barefoot: Transitioning Well to Minimal FootwearFrom EverandWhole Body Barefoot: Transitioning Well to Minimal FootwearRating: 4 out of 5 stars4/5 (16)
- Muscle for Life: Get Lean, Strong, and Healthy at Any Age!From EverandMuscle for Life: Get Lean, Strong, and Healthy at Any Age!Rating: 4.5 out of 5 stars4.5/5 (22)
- Boundless: Upgrade Your Brain, Optimize Your Body & Defy AgingFrom EverandBoundless: Upgrade Your Brain, Optimize Your Body & Defy AgingRating: 4.5 out of 5 stars4.5/5 (66)
- Yamas & Niyamas: Exploring Yoga's Ethical PracticeFrom EverandYamas & Niyamas: Exploring Yoga's Ethical PracticeRating: 4.5 out of 5 stars4.5/5 (111)
- Mind Your Body: 4 Weeks to a Leaner, Healthier LifeFrom EverandMind Your Body: 4 Weeks to a Leaner, Healthier LifeRating: 4.5 out of 5 stars4.5/5 (5)
- The Yogi Code: Seven Universal Laws of Infinite SuccessFrom EverandThe Yogi Code: Seven Universal Laws of Infinite SuccessRating: 4.5 out of 5 stars4.5/5 (104)
- Relentless: From Good to Great to UnstoppableFrom EverandRelentless: From Good to Great to UnstoppableRating: 5 out of 5 stars5/5 (784)
- Buteyko Breathing Course Manual: For use with the Advanced Buteyko CourseFrom EverandButeyko Breathing Course Manual: For use with the Advanced Buteyko CourseRating: 5 out of 5 stars5/5 (1)
- Easy Strength: How to Get a Lot Stronger Than Your Competition-And Dominate in Your SportFrom EverandEasy Strength: How to Get a Lot Stronger Than Your Competition-And Dominate in Your SportRating: 4.5 out of 5 stars4.5/5 (17)
- 80/20 Running: Run Stronger and Race Faster by Training SlowerFrom Everand80/20 Running: Run Stronger and Race Faster by Training SlowerRating: 4.5 out of 5 stars4.5/5 (97)
- Music For Healing: With Nature Sounds For Natural Healing Powers: Sounds Of Nature, Deep Sleep Music, Meditation, Relaxation, Healing MusicFrom EverandMusic For Healing: With Nature Sounds For Natural Healing Powers: Sounds Of Nature, Deep Sleep Music, Meditation, Relaxation, Healing MusicRating: 5 out of 5 stars5/5 (1)
- Wall Pilates: Quick-and-Simple to Lose Weight and Stay Healthy. A 30-Day Journey with + 100 ExercisesFrom EverandWall Pilates: Quick-and-Simple to Lose Weight and Stay Healthy. A 30-Day Journey with + 100 ExercisesNo ratings yet
- The Yoga Sutras of Patanjali: The Final Guide for the Study and Practice of Patanjali's Yoga SutrasFrom EverandThe Yoga Sutras of Patanjali: The Final Guide for the Study and Practice of Patanjali's Yoga SutrasNo ratings yet
- Weight Lifting Is a Waste of Time: So Is Cardio, and There’s a Better Way to Have the Body You WantFrom EverandWeight Lifting Is a Waste of Time: So Is Cardio, and There’s a Better Way to Have the Body You WantRating: 4.5 out of 5 stars4.5/5 (38)
- If You Like Exercise … Chances Are You’Re Doing It Wrong: Proper Strength Training for Maximum ResultsFrom EverandIf You Like Exercise … Chances Are You’Re Doing It Wrong: Proper Strength Training for Maximum ResultsRating: 4.5 out of 5 stars4.5/5 (7)
- Endure: Mind, Body, and the Curiously Elastic Limits of Human PerformanceFrom EverandEndure: Mind, Body, and the Curiously Elastic Limits of Human PerformanceRating: 4.5 out of 5 stars4.5/5 (237)
- Structural Integration and Energy Medicine: A Handbook of Advanced BodyworkFrom EverandStructural Integration and Energy Medicine: A Handbook of Advanced BodyworkRating: 4 out of 5 stars4/5 (1)
- Not a Diet Book: Take Control. Gain Confidence. Change Your Life.From EverandNot a Diet Book: Take Control. Gain Confidence. Change Your Life.Rating: 4.5 out of 5 stars4.5/5 (124)
- Fascial Training: With Easy Exercises To More Mobility And Less Pain (10 Minutes Fascia Workout For Home)From EverandFascial Training: With Easy Exercises To More Mobility And Less Pain (10 Minutes Fascia Workout For Home)Rating: 5 out of 5 stars5/5 (3)
- The Yamas & Niyamas: Exploring Yoga's Ethical PracticeFrom EverandThe Yamas & Niyamas: Exploring Yoga's Ethical PracticeRating: 4.5 out of 5 stars4.5/5 (19)