Professional Documents
Culture Documents
Derek Ana Revised
Uploaded by
api-242603823Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Derek Ana Revised
Uploaded by
api-242603823Copyright:
Available Formats
Running head: AMERICAN NURSES ASSOCIATION STANDARDS AND ETHICS
American Nurses Association Scope and Standards of Practice and Ethics for Nursing
Derek Sibley
Ferris State University
AMERICAN NURSES ASSOCIATION STANDARDS AND ETHICS 2
2
Abstract
Nursing Scope and Standard of Practice and Code of Ethics have a combination of 25
professional standards for registered nurses. It articulates characteristics a registered nurse should
possess, various skills that should be assessed, and the mentality that accompanies superior
nursing care. The purpose of this paper is to analyze each of these standards and ethical
provisions, and relate them to personal experience that was provided by Ferris State Nursing and
its coursework. I am confident that I have met most of the 15 standards and 9 ethical principals,
For those guidelines I lack certainty in meeting, I present an evaluation of my practice using
those standards and offer a plan to meet the defined criteria.
AMERICAN NURSES ASSOCIATION STANDARDS AND ETHICS 3
3
AMERICAN NURSES ASSOCIATION STANDARDS AND ETHICS
Nurses have professional Scope and Standards (American Nurses Association [ANA,
2010) as well as a Code of Ethics (American Nurses Association [ANA], 2001) they should
abide by in order to remain viewed as professionals. Nursing is a care-based profession, and with
patients considered priority, ethical standards need to be upheld as well as the Scope and
Standard of Practice, in order to provide competent care. This paper is a self-assessment of my
competence in each standard as well as a professional plan to attain or retain competence in these
standards
Nursing Scope and Standards of Practice
Standards of Professional Nursing Practice
Standard 1: Assessment.
Assessment is one of the most valuable tools used by nurses to determine patients
problems. According to the American Nursing Association (ANA) (2010), the registered nurse
(RN) collects data relating to the clients health or situation. This includes patient information
relating to physical, psychosocial, emotional, cognitive, sexual, cultural, age-related,
environmental, spiritual/transpersonal, and economic assessments (p. 32). This information also
needs to be interpreted and customized to the patients individuality. The ANA states that a
proper assessment produces the consumers values, inclinations, and knowledge of the situation,
while also identifying communication barriers that may be an issue for the patient (p. 32). Nurses
must also look at family dynamics and their impact on health and wellness (ANA, p. 32).
Equally as important as assessment, documentation of assessments allow other healthcare
providers to more fully understand the situation. If charting is not adequate or accurate, it is
worthless and can also have a negative impact on the patients care in the future. On the other
AMERICAN NURSES ASSOCIATION STANDARDS AND ETHICS 4
4
hand, a thorough and properly documented assessment can help identify a problem that may
otherwise be overlooked.
Ferris States nursing program has shown the importance of assessment skills constantly
throughout all semesters. In the first semester, a class was dedicated purely to assessment to
provide a knowledge base from which to build upon. This knowledge has become extremely
important in the clinical settings, where it is required to assess patients every day. Through these
experiences, I have learned assessment is the most important tool to nurses. Personal experience
in the clinical setting has allowed me to observe patient status as well as changes in status, and
the assessment skills learned previously in the program has given me some insight and intuition
to the cause of patient status. Proper documentation of assessment in the clinical setting began
as a major part of clinical, and every semester I learned something new in regard to assessment
documentation.
Standard 2: Diagnosis.
A registered nurse evaluates various assessment data to define patient diagnosis or patient
issues (ANA, 2010, p. 34). Nurses should be able to conduct an assessment, or interpret the
results of an assessment or other data to derive nursing diagnoses and begin a care plan for the
patient. This standard includes several competencies: identifying possible risks to the clients
health/safety, possible barriers to health, and validating issues with the appropriate person (when
necessary) (ANA, 2010). Nurses should also be able to document issues properly; so as to
facilitate patient care and determination of outcomes and care plans (ANA, 2010, p. 34). A short
list of additional competencies for advanced practice nurses include comparing clinical findings
to normal or abnormal deviations to assist in determining a diagnosis. Advanced practice or
AMERICAN NURSES ASSOCIATION STANDARDS AND ETHICS 5
5
specialty nurses also assist staff in the diagnostic process, both developing and maintaining (p.
34).
Many opportunities have arisen to hone my diagnostic skills . Case studies, clinical
experiences, and other class projects have promoted my proper utilization of nursing diagnoses.
Along with diagnostics, I have developed various care plans in accordance with diagnoses and
patient outcomes or goals. I have been taught in both clinical and classroom settings to observe
possible patient issues and make plans to improve patient safety. Assessing the patients
environment for risk was especially important in my home care rotation, where every
environment was different, with different dangers lurking. In several homes, I observed upturned
carpets, unsteady handrails, and other tripping hazards. I also observed family interactions,
assessing a caregivers competence and knowledge of best practice when caring for children or
other clients. Knowing the patient and their abilities allows for further investigation into possible
risks and benefits to patient health.
Standard 3: Outcomes Identification.
Registered nurses should be skilled in identifying the expected outcomes for a care plan
or situation. The ANA (2010) states registered nurses involve the patient, their family,
healthcare providers, and any others needed when determining expected outcomes of care (p.34).
RNs need to consider cultural possibilities that would affect possible outcomes and care plans,
individualizing both according to the patients beliefs. When determining expected outcomes, it
is important to consider the risks, benefits, costs, up-to-date science, and clinical
experience/expertise. These outcomes should facilitate continuity of care, and be modified when
necessary. Outcomes should also be measurable and attainable goals (ANA, 2010, p. 35).
AMERICAN NURSES ASSOCIATION STANDARDS AND ETHICS 6
6
In my experience, the nursing program has allowed several opportunities to develop this
standard of care. TRUEPIC exercises, clinical experiences, and class/simulation settings
provided good knowledge to carry to my nursing career. Class education and clinical experiences
have provided me information on various cultures, their beliefs, values, and application of this
knowledge to patient care plans, facilitating attainment of patient goals. SMART goals exercises
have given the opportunity to refine my outcome formulation techniques, making them both
measurable and attainable to the patient. A specific clinical experience comes to mind when
thinking about continuity of care. The RN I shadowed for that day thoroughly grasped the
concept, and had the knowledge to advocate for his patient, making sure their overall care
experience was satisfactory. This RN made his patients feel comforted and cared for, and also
contributed greatly to their recovery and attainment of goals. Through observing her interaction
with this patient, as well as completing many TRUEPIC exercises, and participating in the
classroom, I feel confident that I meet this standard of care, and can effectively identify patient
outcomes. I also have been critiqued on making patient outcomes specific, measurable,
attainable, realistic, and timely with assignments including SMART goal material.
Standard 4: Planning.
A sizeable portion of nursing practice includes planning, which should include strategies
as well as alternative measures to assist the patient in attaining the expected outcomes for their
situation. The ANA states that this individualized plan should include the patient, family, and
others necessary for the patients, beliefs, and morals preferences (ANA, 2010, p. 36). It should
also include various strategies related to each issue/diagnosis, facilitating the patient and family
to meet their expected goals and outcomes (ANA, 2010, p. 36). Each patient provides an
individual case, and the registered nurse should analyze each situation and make proper
AMERICAN NURSES ASSOCIATION STANDARDS AND ETHICS 7
7
determinations in regards to care, outcomes, and the effects of the situation on everyone
involved. This helps to ensure holistic care, and allows the patient to be more comfortable, even
in the direst of situations.
Several assignments in the nursing program, as well as education opportunities in clinical
settings have helped me develop skills necessary when planning patient care, developing
outcomes, and strategies to help patients meet their individual goals. Through clinical, I have
seen several situations that the nurse is the sole reason the patient is facilitated to work towards
goals. These goals were formulated in part by the patient, to provide some motivation to meet the
outcomes defined for them. Experiences gained throughout the professional program have
allowed for many reflection opportunities, enhancing creativity to be used for the patients
benefit. Situational analysis is a constant skill used in every clinical environment, and I have
learned to take every situation individually, as well as modify my thinking so I can begin to
observe each situation in a professional and care-based fashion.
Standard 5: Implementation. After formulating the proposed care plan, initiation of the
plan is paramount in determining the patients reaction to it. If the plan isnt properly
implemented, the patient may see it as worthless, disregarding it completely and leaving
everyone at the beginning. The ANA states that implementation requires the RN to include the
patient, family, and other caregivers to implement the care plan safely and realistically (ANA,
2010, p. 38-39). Demonstration of caring and therapeutic behaviors towards the involved party,
utilization of technology and evidence-based practice, holistic and culturally competent care,
multidiscipline collaboration, use of traditional as well as complimentary healthcare practices,
and documentation of modifications to the plan are important parts of this step (ANA, 2010, p.
38-39). Additional competencies for the specialty nurse or advanced practice registered nurse, as
AMERICAN NURSES ASSOCIATION STANDARDS AND ETHICS 8
8
stated by the ANA, include assuming responsibility for the effective implementation of the plan,
facilitating use of resources to assist with implementation, and participating actively in the
improvement of systems supporting the patient/care plan (ANA, 2010, p. 39).
I have witnessed and taken part in the start of several care plans for patients with various
ailments. Patient as well as family inclusion to the implementation of a care plan is very
important, as the family members can also be caregivers, and they can be an important part in the
patient meeting goals. The longstanding and familial basis to family relationships give a certain
persuasion factor that nurses cannot always obtain. I have seen close family members become
the eyes and ears of the nurse, collaborating with them to modify care plans to better suit patient
needs. I realize that further experience is needed to refine and modify my implementation
techniques, but the opportunities provided by the nursing program, mostly in the clinical setting,
have given me a solid knowledge base on various implementation techniques, as well as utilizing
all necessary resources to facilitate the initiation of care plans.
5a: Coordination of Care.
Implementation of a plan includes coordinating care between healthcare providers,
allowing for efficient care delivery (ANA, 2010, p. 40). This is especially important for patient
safety and happiness with overall care. This standard recognizes the RN as an individual that
organizes various components of the care plan, manages care to maximize independence/quality
of life, assists the patient to identify possible alternate care, assists with transitions of care,
advocates for proper delivery of care, and documents the coordination of care regarding the
inter-professional team (ANA, 2010, p. 40). The ANA (2010) also includes leadership roles for
advanced practice nurses, providing direction in the coordination of care (p. 40).
AMERICAN NURSES ASSOCIATION STANDARDS AND ETHICS 9
9
In many clinical situations, I have observed nurses organize a patients day, making
certain that information is relayed to necessary interdisciplinary care team members, and
sometimes playing the role of case manager in certain patient situations. Transition of care is an
important part of the healthcare process, from hand-offs, to unit or facility transfers, and other
situations all call for proper passing of information. This gives the caregiver on the receiving end
of the transfer a better picture of the situation and needs of each patient.
5b: Health Teaching and Health Promotion.
Patient education is an extremely important aspect in nursing. nurses are the primary
patient educators, and have an impact on the quality of learning that occurs during education.
The ANA (2010) includes several components to this standard. A registered nurse can provide
teaching about various topics, like healthy life-styles, behaviors to reduce risk, developmental
teaching, daily activities and self care. They should use methods of teaching specific to the
patient, specifically their cognitive level, cultural beliefs/practices, language, and values in order
to provide education the patient retains and utilizes in the future. Nurses should know that
education is not unidirectional, and look for verbal/nonverbal feedback constantly to verify that
the teaching has been successful. They should use information and education in a variety of
settings, and provide the client with information about the effects (positive and possible
negative) of therapies/procedures (ANA, 2010, p. 41).
Experiences throughout the nursing program have allowed for some patient education
opportunities, along with observational examples of patient education and health promotion.
Nurses I have been shadowing or observing are constantly educating and re-educating patients
according to their individual needs. Even in passing, educational opportunities are endless.
Patients have many questions about their care, and I am glad that classroom experiences
AMERICAN NURSES ASSOCIATION STANDARDS AND ETHICS 10
10
previously in the program have provided knowledge and resources for patient education.
Personally, I have provided useful information to many patients regarding smoking cessation,
diabetes, healthcare procedures, and more. Patient education, as I have observed, makes them
feel much more comfortable about the situation than left in the dark. I once noticed anxious
behavior in a patient, and learned lack of knowledge about the procedure was the cause of his
anxiety. After he was educated, his demeanor changed and he seemed to visibly relax. This
reinforced the importance of education in practice.
5c: Consultation.
Consulting clients is a standard directed toward APRNs or specialty nurses should
provide clinical data, theoretical frameworks, and evidence for consultation, while maintaining
effectiveness of the consultation by including the client and other stakeholders in negotiations
and the decision process (ANA, 2010, p. 43).
We have learned nursing theories, and have used these theories to relate to life situation
in both clinical and class settings. The multitude of theoretical frameworks learned allow me to
find and utilize at least one theory and base it to the care of each patient or situation I encounter.
5d: Prescriptive Authority and Treatment.
Advanced practice nurses such as Nurse Practitioners have the authority to prescribe
medications, therapies, evaluate their effects, and incorporate complimentary/alternative
treatments into patient care (ANA, 2010, p. 44). This standard is above the scope of practice for
a baccalaureate prepared nurse.
As this is above the Scope of Practice for RNs, but I have been able to informally
evaluate the effects of treatments for every patient I encounter. More long term care of patients
may give student nurses a better insight to various effects of treatments or therapies.
AMERICAN NURSES ASSOCIATION STANDARDS AND ETHICS 11
11
Standard 6: Evaluation.
Evaluating progress toward goals and outcomes is also the role of a registered nurse. If
progress is not being noticed, something in the care plan may need to be changed so that the
patient can begin to work toward the established goals. The ANAs (2010) list of competencies
for RNs includes: Conducting systematic evaluations of the patients progress in relation to
outcomes, collaborating with other care providers when evaluating individuals, using constant
assessment to re-structure plans according to the patients care needs, and giving out results to the
patient, family, as well as others involved (following federal and state regulations). Nurses also
should thoroughly document evaluations for future reference (ANA, 2010, p.45).
Evaluating patient progress towards goals was experienced mostly in clinical settings, but
the knowledge base was obtained in the first semester. Formulating SMART goals help me to
objectify outcomes and analyze patient progress in concrete terms. With a good measurement
system, patient progress is more thoroughly interpreted, and can promote modification of care
plans to benefit the patient. My documenting skills are constantly refined by my clinical
preceptors, perfecting my technique for recording objective and descriptive information. While
caring for a patient, I questioned his smoking habits and reason for continuing the habit although
he stated a desire to quit. He said he couldnt find anything that satisfied his cravings, and we
worked together to identify alternative measures he hadnt yet tried. This included using a
nicotine vaporizer with a high nicotine content that mimicked cigarette smoke. This patients goal
was to cease smoking cigarettes completely, satisfying nicotine cravings with the vaporizer, in
six weeks time. He seemed excited to work toward this goal, which increased his motivation, and
probability to attain this goal.
Standard 7: Ethics.
AMERICAN NURSES ASSOCIATION STANDARDS AND ETHICS 12
12
Ethical care of healthcare consumers allows them to feel more comfortable and satisfied
with their experience. The Scope and Standards of Practice (2010) states that a RN should use
the Nurses Code of Ethics, deliver care that preserves and protects consumer autonomy, dignity,
rights, values, and beliefs (p. 47). The nurse should recognize that the patient and family are the
main members on their healthcare team, maintain patient confidentiality in accordance with
privacy laws, assist in informed decision-making, and maintain a professional/therapeutic
relationship with proper boundaries. Nurses should also act appropriately when situations
involving illegal or unethical behavior possibly endangering the situation or patient. Patient
avocation is also part of this standard, and the nurse should work to make sure the patient is
provided equitable care (ANA, 2010, p. 47).
Privacy laws rules and regulations are designed to protect patient rights and privacy.
Numerous education opportunities about patient confidentiality have been provided throughout
the nursing program and its pre-requisite courses. I have learned to maintain patient privacy and
anonymity, protecting patient information by logging out of medical networks, and speaking
about situations in a manner that abides by all privacy regulations. With experiences caring for
Michigans diverse population, I have become more culturally competent, allowing me to be
more respectful of patient beliefs and values. Ethical decision making is a trait every nurse
should possess, as it is a care-based profession.
Standard 8: Education.
Current nursing knowledge is necessary to provide up-to-date care that is acceptable by
todays standards. The ANA (2010) includes several competencies registered nurses should
uphold. These include going to various educational activities that can be useful in practice,
showing commitment to lifelong learning, and looking for opportunities to learn or maintain
AMERICAN NURSES ASSOCIATION STANDARDS AND ETHICS 13
13
knowledge. This evidence of learning should be recorded to show evidence of a nurses
competence and commitment to education. They should also share useful knowledge with other
healthcare professionals (ANA, 2010, p. 49).
Clinical settings and up-to-date education allow me to obtain knowledge about nursing in
todays healthcare world. Skills learned in laboratory and simulation settings are current
practice, with clinical experience as reinforcement for what really happens in nursing.
Opportunities to further education, like joining nursing based organizations, have given me
avenues to further education for the remainder of my nursing career.
Standard 9: Evidence-Based Practice and Research.
Evidence based practice and up-to-date research provides nurses with an opportunity to
better healthcare practices as well as provide the best possible patient care. Every day, new ideas
are being discovered and utilized in healthcare. Innovations can be as simple as using a different
style of dressing, to implementing an entirely new therapy procedure aimed towards bettering
patient outcomes. The ANA (2010) defines several competencies for this standard. Nurses
should use current nursing knowledge and research to help guide their practice, show positive
evidence when initiating a change in practice, as well as share personal and research findings
with other healthcare professionals (ANA, 2010, p. 51). Advanced practice nurses should
contribute to knowledge by conducting research to look at current healthcare practices, skills,
and other approaches to better patient outcomes while encouraging workplace research and
questioning of current practice (p. 51).
Research assignments, clinical practices, and classroom education have shown the
importance of evidence-based practice in healthcare. Knowledge is gained every day, and that
knowledge can lead to new therapies or protocols to improve patient outcomes. This evidence is
AMERICAN NURSES ASSOCIATION STANDARDS AND ETHICS 14
14
often interesting, and can drastically improve patient outcomes. Through assignments in the
program, I learned about Hypothermic Protocol, a new therapy for patients diagnosed with
acute ischemic attacks. This revolutionary therapy greatly lessens damage caused by the bodys
lack of oxygen. Post conferences in clinical settings allow for the sharing of findings and
experiences in a safe, and privacy laws approved manner.
Standard 10: Quality of Practice.
Quality nursing practice promotes patient satisfaction as well as patient outcomes. The
ANA (2010) provides various competencies that this standard should uphold. They include
quality documentation of the nursing process, creative and innovative thinking, information
collection for identification of improvement opportunities, recommendations for improving
healthcare practice, development and evaluation of procedures/policies for possible
improvement, and making efforts to minimize healthcare cost to the patient (ANA, 2010, p. 52).
This standard also includes that nurses should identify barriers in the workplace to weaken or
remove them completely (ANA, 2010, p. 53).
Quality healthcare is every patients right, regardless of patient status or situation.
Documentation of nursing process is taught in the first semesters of clinical, where I learned the
importance of documentation. If it isnt documented, then you didnt do it, was a statement
that has stuck in my memory, and pushes me to provide accurate documentation, as this helps
both the patient and all care providers to work toward desired outcomes. I document hourly
rounds on every patient, Critical thinking exercises promote an open-minded approach to
healthcare. I also provided quality care when explaining procedures that were happening to an
unresponsive patient, because he may have been able to hear, and the explanations could have
brought some comfort as well as reduce possible anxiety or fear.
AMERICAN NURSES ASSOCIATION STANDARDS AND ETHICS 15
15
Standard 11: Communication.
Effective communication in healthcare is possibly the most important aspect. It is
paramount in interdisciplinary care and collaboration, allowing for every member of the team to
know the situation completely. On the other hand, ineffective communication can have serious
and life threatening effects. Competencies included for this standard include analyzing
communication skills of ones self as well as the patients, and using this information to improve
communication and understanding. Information needs to be passed between team members
(including the family) in a style that is both complete and accurate (ANA, 2010, p. 54).
Communication always has room for improvement, and people that realize this will continue to
improve their skills, using experiences and information to better communicate with others.
My therapeutic communication and professional communication have been constantly
revised as I gain interpersonal experience in the healthcare setting. Before the program, I had
little patient care experience, and the communication dialogue was novel and difficult. After
different situations and education on communication techniques, my skill is improving
immensely. While attending a clinical rotation, I sat and talked with a patient admitted for
depression. I used the skills I learned to effectively talk to this patient, while assessing their
personal situation. I also modified my communication techniques to withdraw information, and
used therapeutic silence when necessary. There will always be room for improvement, and I will
ensure this through constant evaluation of my skills.
Standard 12:Leadership.
In the healthcare setting, nurses need to demonstrate leadership qualities, as they are on
the front line of healthcare. Observations made by competent nurses can later be used to direct
AMERICAN NURSES ASSOCIATION STANDARDS AND ETHICS 16
16
situations in the preferable direction. The ANA (2010) also includes that nurses should be
responsible and accountable for the quality of care they are giving as well as care given by
others. Mentoring other nurses and sharing knowledge gained in practice will continue to
advance nursing practice and the quality of healthcare. Other leadership qualities include treating
others with respect and dignity, using conflict resolution skills to diffuse situations, and seeking
ways to advance nursing autonomy and accountability (ANA, 2010, p. 55).
Ferris Nursing has promoted my independence and leadership qualities from the
beginning. Educators in the program have done a good job of teaching the accountability for my
actions, no matter the consequences. This is especially important when patient safety is
jeopardized. Leadership is also currently being taught in a mixed online/in class setting, showing
what a leader does, and facilitating further education opportunities in the leadership role. The
Manager Interview assignment also helped to open my eyes on the benefits of a good leader. I
have used these leadership qualities to educate a peer proper use of a continuous monitoring
device, enhancing comfort for the patient and reducing frustration for everyone involved.
Standard 13: Collaboration. According to the ANA (2010), collaboration involves the RN
partnering with others in order to improve outcomes via the sharing of knowledge, expertise, and
professional views. Communication with the entire care team regarding care, conflict
management, and application of conduct codes promote a cooperative and respectful workplace
all work toward improving patient outcomes and the overall healthcare environment (ANA,
2010, p. 57). Different techniques for interdisciplinary collaboration and negotiation should be
applied in regard to best practice and patient care (ANA, 2010, p, 57).
The Service Learning assignment gave me an entirely new respect for the benefits of the
interdisciplinary approach to healthcare. I had to the opportunity to work with a team involving
AMERICAN NURSES ASSOCIATION STANDARDS AND ETHICS 17
17
other student nurses, optometry students/faculty, and pharmacy students/faculty. This provided a
view into how other professions view the same patient, and we had the opportunity to see every
profession consulting a patient or two. In clinical, collaborating with other caregivers to provide
quality care to patients is interesting and can provide different insights. I have also seen instances
of poor communication, and unfortunately the patient is the harmed. Extra days of stay due to
miscommunication are far too common, and this is costly for the healthcare consumer, not to
mention agitating for the client.
Standard 14: Professional Practice Evaluation.
Analyzing ones professionalism and care practices should be done constantly so to
improve ones contribution to patient care as well as the organization. Constant evaluation of
ones professional practice allows nurses and other caregivers to continually improve
professional care and competence. The ANA states that both age and developmentally
appropriate care, while respecting cultural and ethical beliefs of the patient, are huge parts of a
respected professional. Identifying strengths and weaknesses in practice, using criticisms and
other informal feedback for professional growth, providing constructive criticisms for others to
improve their practice, interacting with other caregivers and healthcare professionals to improve
practice, and taking peer reviews seriously all benefit the idea of professional practice evaluation
(ANA, 2010, p. 59).
Multiple times per semester, I evaluate myself on professional performance, formally
filling in evaluation forms and grading my performance. I am also reviewed by my preceptor,
both formally and informally, constantly throughout the program to improve professionalism. I
have also been reviewed and evaluated by peers in simulation and class settings, and had the
AMERICAN NURSES ASSOCIATION STANDARDS AND ETHICS 18
18
opportunity to provide feedback to those peers, evaluating performance and reaction to the
situation with the goal of professional improvement.
Standard 15: Resource Utilization.
Knowing and using all resources available promotes patient care as well as improves
outcomes. Various resources are beneficial for different reasons, so use should be individualized
to that patient according to their personal and financial situation. ANA competencies include that
nurses should analyze individual patient needs and resources beneficial to the consumer.
Delegation of care, advocation of resources and technologies, and assistance in identification of
appropriate patient services are included in this practice standard (ANA, 2010, p. 60). Many
patients dont know which resources are available to help them, or if any exist at all. Nurses can
provide this information and get the patient started with recovery that much more easily.
There are many resources in which nurses have access, and they can be used for patient
care or benefit in many ways. The program has conditioned me to look for information when in
need, rather than asking. Many nurses that I have shadowed in clinical have used various
resources to help patient issues, from financial to medical and otherwise. I was able to save a
patient money by clearing their home medications with pharmacy, so he didnt have to pay for
hospital drugs. I have noticed many resources to be regional, so I plan to research different
resources for the area in which I choose to practice.
Standard 16: Environmental Health.
Environment plays a remarkable role in health and healthcare outcomes. The Scope and
Standards of Practice states that the registered nurse should have knowledge of various
environmental health concepts and strategies, support the workplace and uphold safety for both
healthcare providers and consumers, constantly analyze the area for sensory stimulations that
AMERICAN NURSES ASSOCIATION STANDARDS AND ETHICS 19
19
threaten the health of any individual. Scientific evidence should be brought forth when
evaluating treatments or protocols for possible health hazards.
Public health rotations, classroom material, and other clinical experiences have given
information. I took part in safety screenings for staff members of a courthouse, showing various
environmental effects and physiological effects of various job titles. The sedentary lifestyle of
many staff members lead to high cholesterol, high blood pressure, and other physiological signs
that health education was necessary. I was able to educate staff members on cholesterol lowering
methods, as well as other ways to improve health. Third-party research related to assignments
has also increased knowledge in various environmental health aspects.
Ethical Standards of Professional Nursing Practice
Nurses and other healthcare providers have a set of moral principles by which they
should abide. Nurses have a Code of Ethics defined by the ANA, including nine provisions for
ethical obligations and duties of every nurse (p.2).
Provision 1: Respect and Compassion
The ANA states that nurses should practice with compassion and respect for the patient,
unrestricted by judgment, patient demographic, or their illness (p. 3). Respecting human rights,
establishing patient rapport, understanding that the patient is a person (regardless of illness), and
preserving the right to self determination are included in this provision, along with maintaining
professional relationships with everyone encountered (p.4-5).
Respect and compassion is the definition of nursing. Classroom education has taught
cultural competence as well as respect for the patient as an individual. Clinical situations have
improved my ability to empathize and show compassion, traits I had previously had difficulty
displaying. I cared for a patient that was unresponsive and on palliative care. This involved
AMERICAN NURSES ASSOCIATION STANDARDS AND ETHICS 20
20
complete care for the client, which I carried out while respecting the patient. I explained what I
was doing as though he would respond. I also comforted the family in their difficult situation,
providing effective therapeutic communication as they worked through the grieving process.
Provision 2: Commitment to the Patient
The nurses primary commitment is to the patient, whether an individual, family, group,
or community (ANA, 2001, p. 5). Patients are priority, and nurses should strive to protect their
interests, even when in conflict with their own. The Nursing Code of Ethics (2001) states that
nurses should strive for a conflict resolution that prioritizes patient safety and best interests (p.
5). Collaboration with healthcare team members to attain patient goals, and a mutual, trusting
relationship between everyone involved promotes the sharing of ideas (Ethics, p. 5). With an
interdisciplinary approach, various professional views are put together, and a more complete
picture of the situation is seen. Professional boundaries must also be maintained, and the
commitment to the patient needs to remain within those boundaries (Ethics, p.5).
Educators in the program, caring for patients, and realizing that care should be holistic
have all shown me that nurses primary concern is the patient. In order to show commitment to
the patient that is visible to them, nurses need to be on the patients team, in all respects. In
clinical, I have observed nurses advocating for patients right down to tooth and nail, making sure
the patient received the treatment they deserved. In clinical, I collaborated with the RN and
pharmacy to find alternative routes for medications when caring for a patient that was NPO and
not receiving their medications for that reason. I contacted pharmacy several times in order to
obtain the correct medication order, and ensured that the patient received the medications they
needed.
Provision 3: Patient Health, Safety, and Rights
AMERICAN NURSES ASSOCIATION STANDARDS AND ETHICS 21
21
According to the ANAs Code of Ethics, the nurse promotes, advocates for, and strives
to protect the health, safety, and rights of the patient (Ethics, 2001, p. 6). This includes
respecting patient privacy and confidentiality, protecting research participants and educating
them on their rights, reviewing policies, and acting properly when questionable or impaired
practice is noticed (p. 7-8). The Code of Ethics informs us that impaired practice exposes the
patient to potential harm, and nurses should be vigilant in order to keep the patient safe, but we
should do so by following guidelines of the workplace to assist peers that may have a problem
affecting their performance (Ethics, 2001, p. 8). It also states that the nurse may override these
policies if they are not appropriate and seek advice from an employee assistance program or
similar resource (Ethics, 2001, p.8).
This provision is similar to the second provision, and through the program, I have learned
privacy laws rules and regulations to protect patient rights and identity. I have also learned that
there are protocols for conflict resolution, and following these guidelines can minimize negative
impact. I respected patient privacy in a situation that required me to ask an individual to leave the
room before assessing the patient, because the individual was not permitted to know medical
information, and I had several questions to ask pertaining to patient assessment.
Provision 4: Accountability and Responsibility
Registered nurses are both responsible and accountable for their practice, judgments, and
actions, including delegation of tasks (Ethics, 2001, p. 8-9). Nurses are the primary care provider
for patients, therefore they are also accountable for the care their patient receives (Ethics, 2001,
p.8). If a nurse delegates a task outside of an aides scope of practice, and something goes wrong
then the nurse is responsible for the mishap. When a patient case is outside of the nurses
AMERICAN NURSES ASSOCIATION STANDARDS AND ETHICS 22
22
knowledge base or competencies, that nurse should collaborate with other nurses and healthcare
professionals to make sure the patient gets proper care (Ethics, 2001, p. 9).
Information in class as well as clinical settings has shown that nurses are accountable for
their actions and practice. Nurses are the final person to check prescriptions, and they are the
ones to administer the medication, so they are responsible for that administration, even if it was
prescribed incorrectly by the doctor. In clinical, I have already seen several mistakes in
prescription by doctors, and the nurse was required to call the doctor and double check. If the
nurse had administered the drug, they would be held responsible. In class we also learned that
nurses need to carry malpractice insurance for such instances. I always check medications
properly before administration, and once I found the wrong medication in a patient drawer.
Provision 5: Self-Respect
Nurses have the responsibility to care for themselves, allowing themselves the same
rights they give their patients (Ethics, 2001, p. 9). This includes the retention of ones character
and integrity, as well as growing as a professional and maintaining competence in practice
(Ethics, 2001, p. 9-10). In relation to preservation of integrity, nurses have the right to refuse to
participate in a treatment that they feel violates patient rights or safety, but should do so in
advance so as not to abandon the patient (Ethics, 2001, p. 10-11).
I have learned that nursing is a very demanding profession, and often nurses have an
overload of patients, so they tend to forget about their own needs. Personally, I have missed
lunch because I was preoccupied with patient care, and delayed using the restroom until the last
possible second due to the fast-paced nature of nursing. I have also learned that if a caregiver is
not healthy, providing optimal care cannot be achieved.
Provision 6: Environment and Influence
AMERICAN NURSES ASSOCIATION STANDARDS AND ETHICS 23
23
According to the Code of Ethics, Nurses should help to maintain and improve the
healthcare environment as well as employment conditions to maintain quality health care that is
consistent with the values of the organization (Ethics, 2001, p. 11). This includes many
character attributes that are possessed by nurses. These include compassion and honesty as well
as patience and courage (Ethics, 2001, p. 11). The environment has a large effect on ethical
practice. The workplace can have positive or negative environmental effects on nurses and their
decisions to make moral and ethical decisions, while promoting an environment conducive to
ethical practice (Ethics, 2001, p. 11).
Several nursing theories taught in classroom material state that health is directly related
to the environment. The clinical settings also have shown how the workplace environment
affects the ethical decisions of its employees. If an individual enjoys working somewhere, they
tend to work harder to help the team accomplish their goals. I have worked jobs in which the
environment was extremely negative; it is both physically and mentally exhausting. But when
there is tension and unhappiness, ethical conflicts can soon follow. Nurses may start calling in
sick or start stealing. There are many decisions to be made, and a good work environment
facilitates honesty.
Provision 7: Advancement of Profession
Advancement of the nursing profession is job security at its finest. If nurses keep
verifying worth in the healthcare realm and persist in advancing practice, nursing will remain a
valuable asset to patient care. The Code of Ethics includes several ways we can participate in the
advancement of our profession. These include becoming actively involved in healthcare policy,
contributing to activities, becoming nurse mentors or role models, and maintaining standards of
the profession in all settings (Ethics, 2001, p. 12).
AMERICAN NURSES ASSOCIATION STANDARDS AND ETHICS 24
24
From the very beginning of the program, educators have instilled in the students a
passion for nursing, and a desire to better nursing as a profession. I have attended meetings
related to nursing and the advancement of its profession. Many other assignments have been
oriented toward research and nursing advancement. Specifically, I attended a meeting presented
by Alpha Tau Delta, where several speakers commented on how important advancing the
profession of nursing is to the future.
Provision 8: Health Needs
The ANAs Code of Ethics states that the nurse should collaborate with other healthcare
providers and the community to promote efforts to meet healthcare needs. The needs and health
concerns of all people, in various situations, is the responsibility of nurses as individuals and as a
whole. Nurses should take care not to impose ones beliefs and values on patients or others
(Ethics, 2001, p.12-13).
In various settings, I have been taught skills to remain non-judgmental and supportive of
the patient, while being careful to let them make their own decisions. One experience in clinical
challenged my ability to do so because the patient was asking my personal opinion on whether to
proceed with a surgery. The skills taught in class allowed me to be therapeutic towards the
patient, while refraining from steering them in any particular direction.
Provision 9: Values and integrity
According to the Code of Ethics, nurses as a group should assert their own professional
values to maintain integrity of the nursing profession and its practice (Ethics, 2001, p. 13).
Professional integrity, as the Code of ethics also states, is the organization or association and
their expression/upholding of stated professional values. One of the professions main jobs is to
promote the Code of Ethics and other mechanisms that define its principals (Ethics, 2001, p.13).
AMERICAN NURSES ASSOCIATION STANDARDS AND ETHICS 25
25
Nurses should take action with legislation, nursing organizations, and other agencies in reshaping
healthcare and resolving social or cultural issues (Ethics, 2001, p. 13).
As a student nurse, I have been taught to practice ethically, instilling the compassionate
values as well as integrity so I can provide quality and ethical patient care. In order to maintain a
workplace with these characteristics, I have seen nurses bring additional values, above those of
the organization, to care for the patient. The Code of Ethics has been revisited multiple times in
classroom material, and its importance to nursing and healthcare practice has been made known.
Professional Development Plan
I have developed basic competency in these care standards and ethical care standards, and
plan to continue developing each one as I enter and continue through nursing practice. I will use
evidence-based research to provide up-to-date care for patients. I plan to subscribe to nursing
journals upon entry into the professional world, to gain knowledge and insight, as well as expand
my thought processes. Once an RN, I plan to join a committee on my unit that improves patient
outcomes and safety. I also will further my education with opportunities provided by my
employer through in-services. I would also like to return to school to obtain a masters degree
within the first five years after becoming employed.
I will measure my improvement of competence in these standards through self, peer,
patient, and supervisor evaluation. Many facilities have a reward system that allows staff
members to comment positively when they feel it is necessary. This can allow me to evaluate my
skills and performance as a caregiver. Patients also comment on the care provided, and I plan to
use any criticism I may receive in a constructive manner. By doing so, I can assess my ability to
provide these standards of care, and make constant improvements to better patient care.
Conclusion
AMERICAN NURSES ASSOCIATION STANDARDS AND ETHICS 26
26
Nurses have many standards and provisions to uphold as professionals practicing in
healthcare. These include various ethical, moral, and value-driven statements requiring nurses to
provide culturally competent care that is most beneficial to the patient. As a future nurse, I need
to be constantly re-evaluating my professionalism, nursing skills, and healthcare knowledge,
because it is constantly changing in attempt to improve patient outcomes.
AMERICAN NURSES ASSOCIATION STANDARDS AND ETHICS 27
27
References
American Nurses Association. (2010). Scope and Standards of Practice: Nursing 2nd Edition.
Silver Springs, MD. Nursesbooks.org
American Nurses Association. (2001). Code of Ethics for Nurses with Interpretive Statements.
Retrieved from
http://www.nursingworld.org/MainMenuCategories/EthicsStandards/CodeofEthicsforNur
ses/Code-of-Ethics.aspx
AMERICAN NURSES ASSOCIATION STANDARDS AND ETHICS 28
28
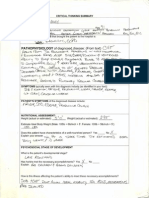
STANDARDS OF PRACTICE
DESCRIPTION AND ANALYSIS OF CURRENT BEHAVIORS
POINTS
POSSIBLE
POINTS
AWARDED
Description of standards
25 25
Supportive evidence (met or unmet)
25
15
Several standards
lacked personal
examples (-10)
Goals: Articulates clear professional goals which reflect a plan
to attain and maintain competency in each standard. These
must be specific and measurable! Refer to information on nursing
care plans re: writing clear & measurable goals to receive full credit
for this section!
15
0
No goals
identified
Action Plan: for goals; to include actions and timelines that are
consistent with the goal statements
15
0
No evaluation
plan identified
Evaluation Plan: to measure progress toward goals. This must be
specific and measurable!
15
0
No plan identified
APA checklist submitted with name of course peer who proofed.
(Points will earned if no APA errors by course instructor)
5 5
TOTAL POINTS 100 45
STANDARDS & APA CRITERIA
Writing: Analysis & Plan is presented with accuracy, precision,
clarity, relevance, depth, breadth, logic and personal significance.
Sentence structure, paragraphing, headings, spelling, typing,
grammar, neatness
Up to
30 point
deduction
21
APA: title page, running head, headers, abstract, margins, font
size, and references: citations in text & reference page.
FINAL POINTS EARNED 100 34
Spacing (-1), citation format (-5), subject verb agreement errors (-2), contractions (-1)
AMERICAN NURSES ASSOCIATION STANDARDS AND ETHICS 29
29
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Derek Sibley: Professional SummaryDocument2 pagesDerek Sibley: Professional Summaryapi-242603823No ratings yet
- Cover Letter 1Document1 pageCover Letter 1api-242603823No ratings yet
- Manager AnalysisDocument7 pagesManager Analysisapi-242603823No ratings yet
- Cticical ThinkingDocument2 pagesCticical Thinkingapi-242603823No ratings yet
- Sibley Theory in PracticeDocument6 pagesSibley Theory in Practiceapi-242603823No ratings yet
- Service Learning PosterDocument4 pagesService Learning Posterapi-242603823No ratings yet
- Leadership Strategy Analysis FinalDocument8 pagesLeadership Strategy Analysis Finalapi-242603823No ratings yet
- SibleydebpDocument5 pagesSibleydebpapi-242603823No ratings yet
- Derek SibleyDocument1 pageDerek Sibleyapi-242603823No ratings yet
- Critical Thinking SummaryDocument6 pagesCritical Thinking Summaryapi-242603823No ratings yet
- Paper OneDocument7 pagesPaper Oneapi-242603823No ratings yet
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (894)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Chapter 1Document15 pagesChapter 1ErikaNo ratings yet
- Overcoming Low Self-Esteem Extract PDFDocument40 pagesOvercoming Low Self-Esteem Extract PDFMarketing Research0% (1)
- Acupuncture Has Been Used For Thousands of YearsDocument13 pagesAcupuncture Has Been Used For Thousands of Yearsoluwasegun DavidNo ratings yet
- Lesson 6 (New) Medication History InterviewDocument6 pagesLesson 6 (New) Medication History InterviewVincent Joshua TriboNo ratings yet
- Birtcher 774 ESU - User and Service Manual PDFDocument39 pagesBirtcher 774 ESU - User and Service Manual PDFLuis Fernando Garcia SNo ratings yet
- Food and Exercise LogDocument24 pagesFood and Exercise LogmhetfieldNo ratings yet
- Music and MoodDocument5 pagesMusic and MoodNatalia TríasNo ratings yet
- Pharmacoeconomics - Part IIIDocument29 pagesPharmacoeconomics - Part IIISima JabbariNo ratings yet
- Five Element PointsDocument42 pagesFive Element PointsSundar Rajan78% (9)
- Migraine Hemicrania and Its Homeopathic Permanent Cure - DR Bashir Mahmud ElliasDocument6 pagesMigraine Hemicrania and Its Homeopathic Permanent Cure - DR Bashir Mahmud ElliasBashir Mahmud ElliasNo ratings yet
- Lesson Plan in English 8 Q2 Module 1Document8 pagesLesson Plan in English 8 Q2 Module 1Nicky SanchezNo ratings yet
- Pharyngitis Laryngitis TonsillitisDocument10 pagesPharyngitis Laryngitis Tonsillitisapi-457923289No ratings yet
- Gallbladder and Bile Duct Anatomy, Function and DiseasesDocument16 pagesGallbladder and Bile Duct Anatomy, Function and DiseasesKadenceFreya-Charisse G PosadasBulintao100% (2)
- Tibbonto: Knowledge Representation of Prophet Medicine (Tibb Al-Nabawi)Document5 pagesTibbonto: Knowledge Representation of Prophet Medicine (Tibb Al-Nabawi)INFOPARK CSCNo ratings yet
- Daftar Pustaka KolelitiasisDocument2 pagesDaftar Pustaka KolelitiasisReni IstiarNo ratings yet
- Machine Learning Predicts 5-Chloro-1 - (2 - Phenylethyl) - 1h-Indole-2,3-Dione As A Drug Target For Fructose Bisphosphate Aldolase in Plasmodium FalciparumDocument7 pagesMachine Learning Predicts 5-Chloro-1 - (2 - Phenylethyl) - 1h-Indole-2,3-Dione As A Drug Target For Fructose Bisphosphate Aldolase in Plasmodium FalciparumInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Desai - Palliative Medicine in Myelodysplastic Syndromes - Patients and Caregivers - A Qualitative StudyDocument5 pagesDesai - Palliative Medicine in Myelodysplastic Syndromes - Patients and Caregivers - A Qualitative StudyRafael TerceiroNo ratings yet
- Rheumatoid Arthritis: Pathophysiology PathophysiologyDocument34 pagesRheumatoid Arthritis: Pathophysiology PathophysiologyOmair RiazNo ratings yet
- The Art of Healthy Eating KidsDocument122 pagesThe Art of Healthy Eating KidsSenka SkenderovicNo ratings yet
- Radiographic EvaluationDocument12 pagesRadiographic EvaluationLuis Gerardo Castillo MendozaNo ratings yet
- Fatal Airway Obstruction Due To Ludwig'sDocument6 pagesFatal Airway Obstruction Due To Ludwig'sRegina MugopalNo ratings yet
- Standards OF Psychiatric Nursing PracticeDocument15 pagesStandards OF Psychiatric Nursing Practicesameeram83No ratings yet
- House-Tree-Person Projective Technique A Validation of Its Use in Occupational TherapyDocument11 pagesHouse-Tree-Person Projective Technique A Validation of Its Use in Occupational Therapyrspecu100% (1)
- Gas Transport 2Document29 pagesGas Transport 2Charmaine LucNo ratings yet
- BLS Adult Skills Checklist 2016Document2 pagesBLS Adult Skills Checklist 2016Wahyudi QorahmanNo ratings yet
- LevaquinDocument1 pageLevaquinKatie McPeek100% (1)
- Furunculosis: Pathology Diagnosis Aetiology Outcomes Management OptionsDocument2 pagesFurunculosis: Pathology Diagnosis Aetiology Outcomes Management OptionsGirish SubashNo ratings yet
- What Is Down SyndromeDocument4 pagesWhat Is Down SyndromeJanica GonzalesNo ratings yet
- Jan Marc Bulatao 10-Einstein BiologyDocument3 pagesJan Marc Bulatao 10-Einstein BiologyNomer SenadorNo ratings yet