Professional Documents
Culture Documents
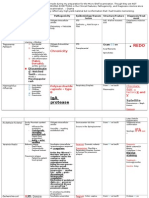
Staphylococcus Aureus (Toxin-Mediated) : Clinical Presentation
Uploaded by
ridin0070 ratings0% found this document useful (0 votes)
19 views1 pageTampon use, trauma / surgery introduce bacteria - bacteria colonize. Toxic shock syndrome promotes excess cytokines released (e.g., IL-1, TNF) antibiotics are not curative--they kill bacteria but do not remove already-released exotoxin.
Original Description:
Original Title
MicroCards Ex 23
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentTampon use, trauma / surgery introduce bacteria - bacteria colonize. Toxic shock syndrome promotes excess cytokines released (e.g., IL-1, TNF) antibiotics are not curative--they kill bacteria but do not remove already-released exotoxin.
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
19 views1 pageStaphylococcus Aureus (Toxin-Mediated) : Clinical Presentation
Uploaded by
ridin007Tampon use, trauma / surgery introduce bacteria - bacteria colonize. Toxic shock syndrome promotes excess cytokines released (e.g., IL-1, TNF) antibiotics are not curative--they kill bacteria but do not remove already-released exotoxin.
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
You are on page 1of 1
CLINICAL PRESENTATION
Toxic Shock Syndrome (TSS)
Scalded Skin Syndrome
Ritters disease in newborn
food poisoning
PATHOBIOLOGY
Toxic Shock Syndrome: tampon use, trauma/surgery introduce bacteria bacteria colonize toxic shock syndrome
toxin-1 (TSST-1) released and diffuses systemically TSST-1 is a superantigen promotes excess cyto-
kines released (e.g., IL-1, TNF) acute fever, rash, desquamation on palms and soles, hypotensive shock
organ hypoperfusion and dysfunction possible death
Scalded Skin Syndrome: skin wound or cutting umbilicus in neonates promotes local epidermal infection exfolia-
tive toxins (e.g., ET-A,B) released and diffuse systemically epidermis separates and skin sloughs off
fluid loss and potential secondary infection possible death
food poisoning: bacteria release toxin in food such as custards heat-stable toxins (e.g., Enterotoxin SE-A)
ingested gastroenteritis self-limited, 8- to 24-hour nausea, vomiting, diarrhea, and abdominal pain
DIAGNOSIS
detection of toxin production by in vitro culture (blood cultures negative because organism does not invade bloodstream)
TREATMENT
removal of foreign bodies, drainage of purulent collections; fluid replacement; penicillinase-resistant penicillins hasten
recovery; (future) blocking effects of IL-1 and TNF with antibodies
QUICK FACTS
Antibiotics are not curativethey kill bacteria but do not remove already-released exotoxin.
Scalded skin syndrome has a 50% mortality rate among adults due to complications from hypovolemia and secondary
infection.
Ritters syndrome is the most severe form of scalded skin syndrome in neonates. It occurs after S. aureus colonizes the
cut umbilicus and releases ET-A,B systemically.
Staphylococcus aureus (toxin-mediated)
(TSS)
011-033_Harpavat_CoreCards_GramPosBacteria.indd 12b 7/10/11 1:15 AM
You might also like
- Complete Medical Guide for Disease Volume VII; Atopic DermatitisFrom EverandComplete Medical Guide for Disease Volume VII; Atopic DermatitisNo ratings yet
- Global Warfare: Boost Your Immune System In Order To Survive A PandemicFrom EverandGlobal Warfare: Boost Your Immune System In Order To Survive A PandemicNo ratings yet
- Micro Bacterial ReviewDocument18 pagesMicro Bacterial ReviewAaron D. Phoenix0% (1)
- Microbiology - Bacteria Summary (Updated)Document26 pagesMicrobiology - Bacteria Summary (Updated)moZZeltovNo ratings yet
- High Yield - Bacteriology ChartsDocument9 pagesHigh Yield - Bacteriology ChartsAmirsalar EslamiNo ratings yet
- Toxic Shock SyndromeDocument10 pagesToxic Shock Syndromealice_lim01100% (1)
- Livestock Diseases 1: Bovine Mastitis and AnthraxDocument108 pagesLivestock Diseases 1: Bovine Mastitis and AnthraxchachaNo ratings yet
- LP Bacteria ChartDocument21 pagesLP Bacteria ChartTaman HoangNo ratings yet
- HANDOUT 3Y Inflammatory Dermatoses 5-28-2012Document23 pagesHANDOUT 3Y Inflammatory Dermatoses 5-28-2012Monica ArmonioNo ratings yet
- Week 25 ParasiticprotozoansDocument64 pagesWeek 25 Parasiticprotozoansapi-26938624No ratings yet
- Ricketsiae BacteriaDocument2 pagesRicketsiae BacteriaErnie G. Bautista II, RN, MDNo ratings yet
- Clostridiose RuminantsDocument12 pagesClostridiose Ruminantseutamène ramziNo ratings yet
- Ssti 2021Document65 pagesSsti 2021Ausu OfficialNo ratings yet
- Reporting GuideDocument43 pagesReporting GuideGeevee Naganag VentulaNo ratings yet
- Defence Against Microorganisms: Gopika Suresh - Ims20121Document2 pagesDefence Against Microorganisms: Gopika Suresh - Ims20121Gopika SureshNo ratings yet
- Lecture 5Document52 pagesLecture 5Shahd Abou SharkhNo ratings yet
- Transmission of ToxoplasmosisDocument7 pagesTransmission of Toxoplasmosissheyla salsabilaNo ratings yet
- Tetanus: Causes, Symptoms, Treatment and PreventionDocument102 pagesTetanus: Causes, Symptoms, Treatment and PreventionMo Oo MooNo ratings yet
- MMG 301 Bacterial InfectionsDocument13 pagesMMG 301 Bacterial InfectionsActress VeriyanNo ratings yet
- Tetanus: Mrs.G.Manibharathi, MSC (N), Associate ProfessorDocument26 pagesTetanus: Mrs.G.Manibharathi, MSC (N), Associate ProfessormanibharathiNo ratings yet
- Hipo HiperthyroidDocument49 pagesHipo HiperthyroidMuhammad Bilal Bin AmirNo ratings yet
- An Allergy Is An Adverse Reaction That The Body Has To A Particular Food or Substance in The EnvironmentDocument15 pagesAn Allergy Is An Adverse Reaction That The Body Has To A Particular Food or Substance in The EnvironmentwengieNo ratings yet
- DermatologyvetDocument120 pagesDermatologyvetWanderlust ExplorerNo ratings yet
- Anthrax and Ts PreventionDocument60 pagesAnthrax and Ts PreventionZahid Qamar100% (1)
- Ebook PDF Current Medical Diagnosis and Treatment Study Guide 2nd PDFDocument41 pagesEbook PDF Current Medical Diagnosis and Treatment Study Guide 2nd PDFcecil.slocum194100% (38)
- Tetanus: Dr.I.SelvarajDocument47 pagesTetanus: Dr.I.SelvarajimyoongsNo ratings yet
- Infection: Dr. Mehrunnisa Umar Assistant Professor Department of MedicineDocument57 pagesInfection: Dr. Mehrunnisa Umar Assistant Professor Department of MedicinedrusmanjamilhcmdNo ratings yet
- Clinical Bacteriology: Gram Positive Spore Forming RodsDocument26 pagesClinical Bacteriology: Gram Positive Spore Forming RodsAfeefa IdreesNo ratings yet
- Anaerobic BacteriaDocument65 pagesAnaerobic BacteriaJames TorresNo ratings yet
- Wa0021Document8 pagesWa0021Bakul PariNo ratings yet
- Food IntoleranceDocument95 pagesFood IntoleranceShirin Syailandira100% (1)
- Jurnal RosiDocument7 pagesJurnal RosiGledi IskandarNo ratings yet
- Clostridium Botulinum: DescriptionDocument6 pagesClostridium Botulinum: DescriptionJada ShblNo ratings yet
- 4th Year Semmelweis University Itay NotesDocument41 pages4th Year Semmelweis University Itay Notesאיתי עוזרNo ratings yet
- Primary Skin Lesions and Differential DiagnosesDocument200 pagesPrimary Skin Lesions and Differential Diagnosesapi-25914483No ratings yet
- The Human Immune SystemDocument2 pagesThe Human Immune SystemGaurav GulatiNo ratings yet
- Micr3011 NotesDocument3 pagesMicr3011 NotesKatherine WangNo ratings yet
- Disease Blueprint For Exam 3: ST NDDocument4 pagesDisease Blueprint For Exam 3: ST NDIvan ReyesNo ratings yet
- Systemic LupusDocument8 pagesSystemic LupusMarielle Liwanag AcostaNo ratings yet
- P E-ReviewerDocument4 pagesP E-ReviewerSuiluj AzodnemNo ratings yet
- Infectious DiseasesDocument65 pagesInfectious DiseasesFathimah UswahNo ratings yet
- Bahasa Inggris Kek 8Document12 pagesBahasa Inggris Kek 8Umi FaridaNo ratings yet
- SKIN PATHOLOGY GUIDEDocument32 pagesSKIN PATHOLOGY GUIDEragnarok meroNo ratings yet
- Impetigo Overview, Causes, Symptoms, Diagnosis & TreatmentDocument11 pagesImpetigo Overview, Causes, Symptoms, Diagnosis & TreatmentShailendra RijalNo ratings yet
- Allergy PediatricsDocument1 pageAllergy Pediatricspapermate9293No ratings yet
- Cataracts Open-Heart Surgery Congenital Heart Disease: Infections/treatment - HTMLDocument3 pagesCataracts Open-Heart Surgery Congenital Heart Disease: Infections/treatment - HTMLDara N PobrienaNo ratings yet
- DermatomycosesDocument2 pagesDermatomycosesRay CullenNo ratings yet
- Atopy and Characteristics of AtopyDocument5 pagesAtopy and Characteristics of Atopyayisha thazyNo ratings yet
- IMMUNITYDocument19 pagesIMMUNITYMuslimNo ratings yet
- Group 1 Tuberculosis: - Andika Hemawan - Eti Rahmawati - Risma Defriyanti - Siska Juliati - Widya Akmalia ADocument28 pagesGroup 1 Tuberculosis: - Andika Hemawan - Eti Rahmawati - Risma Defriyanti - Siska Juliati - Widya Akmalia APaulNo ratings yet
- "PAPER ON Abdominal Typhus": BackgroundDocument13 pages"PAPER ON Abdominal Typhus": BackgroundPriskila AvheNo ratings yet
- MicroPara Lecture 5Document31 pagesMicroPara Lecture 5Pearl NoconNo ratings yet
- Week 2 Chapter 10: Alterations in Immune FunctionDocument55 pagesWeek 2 Chapter 10: Alterations in Immune FunctionAshley Diane HenryNo ratings yet
- Microbiology viriology immunology guideDocument44 pagesMicrobiology viriology immunology guideRoseline AdebisiNo ratings yet
- Surgery I Block 4 Super Reviewer PDFDocument14 pagesSurgery I Block 4 Super Reviewer PDFlems9No ratings yet
- Medically BacteriaDocument2 pagesMedically BacteriaCik SaraNo ratings yet
- Bab I Pendahuluan: Typos. Terminologi Ini Dipakai Pada Penderita Yang Mengalami Demam DisertaiDocument19 pagesBab I Pendahuluan: Typos. Terminologi Ini Dipakai Pada Penderita Yang Mengalami Demam DisertaiangelaNo ratings yet
- GenPath Mod3 InflammationDocument56 pagesGenPath Mod3 InflammationDanielle HayagNo ratings yet
- BSC Amw3, Bvs3 Angela Bayfield 2010Document31 pagesBSC Amw3, Bvs3 Angela Bayfield 2010Laura Joanne SteadNo ratings yet
- Gram-positive Cocci Virulence Factors and DiseasesDocument33 pagesGram-positive Cocci Virulence Factors and DiseasesnurulNo ratings yet
- DFN Nba DK 12 - 28Document418 pagesDFN Nba DK 12 - 28ridin007No ratings yet
- 0305results Val SystemDocument4 pages0305results Val Systemridin007No ratings yet
- 6 Por at Min 8:00 PM MIN by 4.5 214.5 O/uDocument9 pages6 Por at Min 8:00 PM MIN by 4.5 214.5 O/uridin007No ratings yet
- 2015 NFLWeek 4Document2 pages2015 NFLWeek 4ridin007No ratings yet
- DFP Fantasy Basketball Player ProjectionsDocument16 pagesDFP Fantasy Basketball Player Projectionsridin007No ratings yet
- SocDocument1 pageSocridin007No ratings yet
- DFN Nba DK 3-4 ResultsDocument87 pagesDFN Nba DK 3-4 Resultsridin007No ratings yet
- DFN Nba DK 12 - 12Document248 pagesDFN Nba DK 12 - 12ridin007No ratings yet
- IM - Facts From Case Files CRCDocument80 pagesIM - Facts From Case Files CRCridin007No ratings yet
- Sap BookDocument445 pagesSap BookSai ChivukulaNo ratings yet
- Sap Basic NavDocument27 pagesSap Basic NavJessica AlvarezNo ratings yet
- SAP Terminology LessonDocument54 pagesSAP Terminology LessonKrishna ChaitanyaNo ratings yet
- Scrumprimer 121Document22 pagesScrumprimer 121Paulo Henrique Vieira NevesNo ratings yet
- Erp Very GoodDocument35 pagesErp Very Goodridin007No ratings yet
- Sap Hybris Americas Summit 2016 Best PracticeDocument23 pagesSap Hybris Americas Summit 2016 Best Practicesudeepk_sapNo ratings yet
- Atlas of Primary Care Procedures (1st Ed.)Document362 pagesAtlas of Primary Care Procedures (1st Ed.)dianadirgau2399No ratings yet
- Important Features of Gram and Gram BacteriaDocument1 pageImportant Features of Gram and Gram Bacteriaridin007No ratings yet
- Crash RespiratoryDocument245 pagesCrash Respiratoryridin007100% (5)
- CardioDocument1 pageCardiokurra123No ratings yet
- Musculoskeletal ASSOCIATED SYMPTOMS/ROS: HPI, RAMPPS, Description, Sudden or Gradual, Hot, Red, Swollen, FeverDocument3 pagesMusculoskeletal ASSOCIATED SYMPTOMS/ROS: HPI, RAMPPS, Description, Sudden or Gradual, Hot, Red, Swollen, FevercsevideoNo ratings yet
- Crash RespiratoryDocument245 pagesCrash Respiratoryridin007100% (5)
- Staphylococcus Aureus (Toxin-Mediated) : Protein ADocument1 pageStaphylococcus Aureus (Toxin-Mediated) : Protein Aridin007No ratings yet
- MicroCards Ex 25Document1 pageMicroCards Ex 25ridin007No ratings yet
- MicroCards Ex 20Document1 pageMicroCards Ex 20ridin007No ratings yet
- Staphylococcus Aureus (Infections) : Protein ADocument1 pageStaphylococcus Aureus (Infections) : Protein Aridin007No ratings yet
- Hiv and Aids: Common Opportunistic Infections in HivDocument1 pageHiv and Aids: Common Opportunistic Infections in Hivridin007No ratings yet
- Hiv and Aids: Viral Life CycleDocument1 pageHiv and Aids: Viral Life Cycleridin007No ratings yet
- Hepatitis Virus Infections: Serology Course of Hepatitis B InfectionDocument1 pageHepatitis Virus Infections: Serology Course of Hepatitis B Infectionridin007No ratings yet