Professional Documents
Culture Documents
Focuspdca 7 26 14
Uploaded by
api-244230664Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Focuspdca 7 26 14
Uploaded by
api-244230664Copyright:
Available Formats
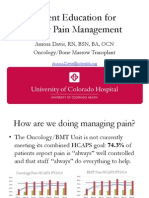
University of Colorado Hospital
Focus-PDCA
Performance Improvement Team Worksheet
Department BMT/OMG Date July 26, 2014
Primary Contact Person Aurora Davis Extension 84275
(F) Find a Process to Improve (name the process, describe the beginning and ending steps in
the process, name the customers served; state why it is important to work on this now).
Opportunity Statement
The BMT/OMG HCAHPS are not at the desired benchmark in the area of Pain Management.
Specifically, the questions Was your pain always well controlled? and Did staff do everything to
help with your pain? did not receive a response of Always 77% or more of the time.
Circle all that apply:
Dimension of Performance: Dimensions of health care performance are those definable,
preferably measurable, attributes of the system that are related to its functioning to maintain,
restore, or improve health care.
- Efficiency - Safety
- Staff Satisfaction - Effectiveness
- Patient Centeredness - Continuity
Prioritization:
- High Risk - High Impact on Performance
- High Volume - High Potential for Improvement
- Problem Prone - Supports Critical Success Factors
- Low Volume - Patient Safety
Other________________________________________________________________________
_____________________________________________________________________________
_____________________________________________________________________________
(O) Organize a team that knows the process:
List Team Members:
Aurora Davis, Clinical RN, Oncology/BMT Units
Regina Fink, Research Nurse Scientist
Barb Wenger, CNS, Oncology/BMT Units
Barb Krumbach, Peri-Op Nurse Educator (Retired)
Max Swedhin, Med/Surg Progressive Care Unit Nurse Educator
(C) Clarify the current knowledge
What do we know about the process?
A literature search was performed to indicate potential targets to improve patient satisfaction.
Evidence shows that patient education about pain management is critical. Lack of education can
be a barrier to proper pain management. Proper patient education significantly increases overall
patient satisfaction regarding pain management. Patient education reduces barriers to
adherence, which improves outcomes. While it is expected that education on pain management is
performed each shift by the patients RN, there is no formal teaching on pain being given to
patients.
(U) Understand sources of variation:
Why are we looking at this process? Why is the process not going the way planned?
It is an expectation that the patients RN will provide education on pain management each shift.
However, the preliminary results of a pain study being performed at UCH show that 43% of study
participants reported receiving no information about pain treatment options. Furthermore,
appropriate documentation in the EHR regarding pain education is sporadic, giving no way to
accurately verify the true frequency of pain education.
(S) Select the improvement:
A formal education tool will be developed. The tool will be used to educate patients about pain
management.
(P) Plan the improvement:
The tool will include information regarding pain management, the WILDA scale, alternative
therapies, and the comfort-function goal. It will be used to educate patients and create a team-
centered approach to pain management (with the patient an active member of the team). The tool
will be a single page teaching sheet on brightly colored paper, available in DOD. The tool will be
translated into Spanish.
(D) Implement the improvement:
The tool was designed and vetted through the units Leadership Team, the physician based Acute
Pain Service, the hospital wide Pain Champions of Change Committee, and the hospital wide
Patient Education Committee. As the design of the tool came to completion, the Pain Champions
decided the distribution and implementation of the tool should be hospital-wide, as opposed to
only unit based. The tool was presented to the Nurse Educators Committee, which agreed upon
a hospital-wide, Level 2 roll out. The tool was rolled out throughout UCH on 5/1/14.
(C) Check the results:
Initial HCAHPS data after implementation of the education tool shows mixed results. The data for
the BMT unit decreased in May to 54% and was a mere 66% in June. The data for OMG has
increased to 70% in May and 78% in June. These numbers are also based on incomplete data for
June, as the number of returned surveys is still small. More data is needed.
(A) Act to hold the gain:
More data will be needed to draw conclusions. However, planning has begun to implement
solutions if the data continues to be mixed or decreases further. Additional data may be gathered
from alternative sources, as well (specifically, Regina Finks UCH Pain Study). Suggested
interventions include: auditing to determine if the tool is being used, reeducation regarding the
pain tool, further education regarding effective pain management, surveys of RNs and patients
regarding the tools use, and additional pain management interventions through alternative
venues (such as the Pain Champions initiatives).
Repeat PDCA as needed and maintain documentation in your department.
You might also like
- Focus - Pdca FormDocument2 pagesFocus - Pdca Formapi-238694882No ratings yet
- Quality ImprovementDocument3 pagesQuality ImprovementViky SinghNo ratings yet
- Outcome Measures For Pain After Surgery - Gordon-ZaslanskyDocument5 pagesOutcome Measures For Pain After Surgery - Gordon-ZaslanskyeryxspNo ratings yet
- Logistics Management Midterm Quiz 1Document3 pagesLogistics Management Midterm Quiz 1Santi SeguinNo ratings yet
- Leadership Strategy Analysis Paper-Amy JohnsDocument9 pagesLeadership Strategy Analysis Paper-Amy Johnsapi-239145075No ratings yet
- Quality Improvement ProcessDocument8 pagesQuality Improvement Processapi-283424486No ratings yet
- Uxcel Focus PdcaDocument2 pagesUxcel Focus Pdcaapi-288762897No ratings yet
- Nurs 440 LeadershipstrategyanalysisgrouppaperDocument10 pagesNurs 440 Leadershipstrategyanalysisgrouppaperapi-253019091No ratings yet
- Screenshot 2024-04-02 at 10.15.12 PMDocument1 pageScreenshot 2024-04-02 at 10.15.12 PMMarwa Elsayed AbuelnourNo ratings yet
- Key Concepts, Chapter 15, Evaluating: Critically About How Best To Evaluate The Patient's Progress Toward Valued HealthDocument4 pagesKey Concepts, Chapter 15, Evaluating: Critically About How Best To Evaluate The Patient's Progress Toward Valued HealthmsbunnileeNo ratings yet
- Quality Improvement ProcessDocument10 pagesQuality Improvement Processapi-284596154No ratings yet
- Nrs 110 Lecture 1 Care Plan WorkshopDocument45 pagesNrs 110 Lecture 1 Care Plan Workshopalphabennydelta4468100% (2)
- Guelph General HospitalDocument7 pagesGuelph General Hospitalfrosty tarp100% (1)
- PC 4 NursingcareplanDocument2 pagesPC 4 Nursingcareplanapi-316769247No ratings yet
- Ambrose Osayo - Sample 1Document6 pagesAmbrose Osayo - Sample 1Ambrose Inc.No ratings yet
- Kuesioner American Pain SocietyDocument15 pagesKuesioner American Pain SocietyNamira Firdha KNo ratings yet
- StepsDocument4 pagesStepsshrikantNo ratings yet
- Literature Review Pain AssessmentDocument8 pagesLiterature Review Pain Assessmentc5r0xg9z100% (1)
- Cqi Project Presentation 2Document7 pagesCqi Project Presentation 2api-575381607No ratings yet
- Pain Management - A Systems Approach To Improving Quality and SafetyDocument143 pagesPain Management - A Systems Approach To Improving Quality and SafetyMiranda Robledo AmezcuaNo ratings yet
- Fundies II Exam 1 Blue PrintDocument24 pagesFundies II Exam 1 Blue PrintStephanieNo ratings yet
- Needs Assessment CycleDocument8 pagesNeeds Assessment Cycleapi-273554555No ratings yet
- Enhancing Nurses Pain Assessment To Improve.11Document2 pagesEnhancing Nurses Pain Assessment To Improve.11Na d'Nazaie CodeNo ratings yet
- Improving Team Structure and Communication: EffectiveDocument31 pagesImproving Team Structure and Communication: EffectiveSutisna NisaNo ratings yet
- Malnutrition Screening Tool (MST)Document3 pagesMalnutrition Screening Tool (MST)Aini SavinaNo ratings yet
- Section Six: Measuring Experience: Why Patient Experience Measurement Is ImportantDocument36 pagesSection Six: Measuring Experience: Why Patient Experience Measurement Is ImportantAdriu MorilloNo ratings yet
- Producing Competent Physicians - More Paper Work or IndeedDocument48 pagesProducing Competent Physicians - More Paper Work or Indeedapi-26176346No ratings yet
- Assessments of Safe Medication Administration in Nursing EducationDocument12 pagesAssessments of Safe Medication Administration in Nursing EducationMichael AmandyNo ratings yet
- BUS6004 Quality Management in A Care Setting - EditedDocument13 pagesBUS6004 Quality Management in A Care Setting - EditedMashaal FNo ratings yet
- DCP4B Manal (4) Health EconomicsDocument52 pagesDCP4B Manal (4) Health Economicsnancy alsharuNo ratings yet
- Leading Health ImprovementDocument2 pagesLeading Health ImprovementRosa Ravariere-SeamanNo ratings yet
- CPHQ ResponseSummaryDocument21 pagesCPHQ ResponseSummaryAlex AlemanNo ratings yet
- AbstractDocument4 pagesAbstractkhizarNo ratings yet
- Pain Minutes 121813Document5 pagesPain Minutes 121813api-244230664No ratings yet
- Nursing ProcessDocument20 pagesNursing Processwideyatma100% (2)
- Standart CostingDocument13 pagesStandart Costingboba milkNo ratings yet
- Quality Improvement Project Proposal WorksheetDocument9 pagesQuality Improvement Project Proposal Worksheetapi-427611602No ratings yet
- Health Economics Paper FinalDocument29 pagesHealth Economics Paper FinalVonrey Tiana73% (11)
- Assignment: 1 Date: 12.10.2021: SolutionDocument8 pagesAssignment: 1 Date: 12.10.2021: SolutionRS BGM PRONo ratings yet
- Stroke Thrombectomy Mentored Implementation ProgramDocument63 pagesStroke Thrombectomy Mentored Implementation ProgramAnonymous NIPCTC68xiNo ratings yet
- Defining Staffing:: Workforce ManagementDocument33 pagesDefining Staffing:: Workforce ManagementMari FeNo ratings yet
- Nursing Dissertation Pain ManagementDocument4 pagesNursing Dissertation Pain ManagementBuyPapersOnlineCanada100% (1)
- Using Client Outcome Monitoring As A Tool For SupervisionDocument5 pagesUsing Client Outcome Monitoring As A Tool For SupervisionDianaSantiago100% (1)
- Module I Group WorkDocument6 pagesModule I Group WorkNur Sanaani100% (1)
- NIC and NOCDocument4 pagesNIC and NOCFernando Oliveira0% (1)
- A Practical Guide To Using Service User Feedback Outcome ToolsDocument99 pagesA Practical Guide To Using Service User Feedback Outcome ToolsPeter LawsonNo ratings yet
- Pediatric Care Plan TemplateDocument15 pagesPediatric Care Plan TemplateKelseyNo ratings yet
- Health Planning - PSM Made EasyDocument6 pagesHealth Planning - PSM Made EasyChristiana OnyinyeNo ratings yet
- What Do Employer's Want For Their Employees?: Standardization With IndividualizationDocument4 pagesWhat Do Employer's Want For Their Employees?: Standardization With Individualizationapi-304631562No ratings yet
- What Do Employer's Want For Their Employees?: Standardization With IndividualizationDocument4 pagesWhat Do Employer's Want For Their Employees?: Standardization With Individualizationapi-304631562No ratings yet
- NR 465 Care of Childbearing Families and Reproductive HealthDocument5 pagesNR 465 Care of Childbearing Families and Reproductive HealthSam DanaNo ratings yet
- Program Development and DesignDocument6 pagesProgram Development and DesignSrikanth KasturiranganNo ratings yet
- Phases: Nursing CareDocument3 pagesPhases: Nursing CareKathryn LauditNo ratings yet
- 1968 - Kiresuk, T. Sherman, R.Document11 pages1968 - Kiresuk, T. Sherman, R.nataliacnNo ratings yet
- Contract Negotiations For NpsDocument9 pagesContract Negotiations For Npsapi-290250982No ratings yet
- Research Article Postop Recovery ProfileDocument8 pagesResearch Article Postop Recovery ProfileNi'mahNo ratings yet
- Baccountingackground Researc1Document6 pagesBaccountingackground Researc1Noor Ul AinNo ratings yet
- ISMP169-GAP Analysis-111418Document20 pagesISMP169-GAP Analysis-111418amira alyNo ratings yet
- Recommendation From Renee AbdellaDocument2 pagesRecommendation From Renee Abdellaapi-244230664No ratings yet
- Kudos Email 8 2 14Document1 pageKudos Email 8 2 14api-244230664No ratings yet
- PPPPC Meeting Minutes 071614Document5 pagesPPPPC Meeting Minutes 071614api-244230664No ratings yet
- Signed Final Evaluation 2014Document3 pagesSigned Final Evaluation 2014api-244230664No ratings yet
- Thank You Patient 1Document2 pagesThank You Patient 1api-244230664No ratings yet
- Recommendation From Jamie NordhagenDocument1 pageRecommendation From Jamie Nordhagenapi-244230664No ratings yet
- Kudos Email 10 11 13Document1 pageKudos Email 10 11 13api-244230664No ratings yet
- Advisor Checklist CompletedDocument7 pagesAdvisor Checklist Completedapi-244230664No ratings yet
- Kudos Email 8 25 13Document2 pagesKudos Email 8 25 13api-244230664No ratings yet
- Thank You New Grad 1Document2 pagesThank You New Grad 1api-244230664No ratings yet
- Kudos Email 1 13 14Document1 pageKudos Email 1 13 14api-244230664No ratings yet
- Presentation of Pain Patient Education ToolDocument10 pagesPresentation of Pain Patient Education Toolapi-244230664No ratings yet
- Kudos Email 3 29 14Document1 pageKudos Email 3 29 14api-244230664No ratings yet
- Preceptor Council AttendanceDocument2 pagesPreceptor Council Attendanceapi-244230664No ratings yet
- Preceptor Council AttendanceDocument2 pagesPreceptor Council Attendanceapi-244230664No ratings yet
- Ce Record 2014 Aurora Davis v2Document1 pageCe Record 2014 Aurora Davis v2api-244230664No ratings yet
- Lo6 FeedbackDocument2 pagesLo6 Feedbackapi-244230664No ratings yet
- January Staff Meeting MinutesDocument3 pagesJanuary Staff Meeting Minutesapi-244230664No ratings yet
- PSC Meeting Agenda 4 2014Document1 pagePSC Meeting Agenda 4 2014api-244230664No ratings yet
- Cancer Patients Barriers To Pain ManagementDocument12 pagesCancer Patients Barriers To Pain Managementapi-244230664No ratings yet
- Do Patients Beliefs Act As BarriersDocument13 pagesDo Patients Beliefs Act As Barriersapi-244230664No ratings yet
- Pain Severity Satisfaction With Pain ManagementDocument10 pagesPain Severity Satisfaction With Pain Managementapi-244230664No ratings yet
- A Pain Education ProgrammeDocument13 pagesA Pain Education Programmeapi-244230664No ratings yet
- Cancer Pain Part 2Document7 pagesCancer Pain Part 2api-244230664No ratings yet
- Hcahps BMT Data BeforeDocument1 pageHcahps BMT Data Beforeapi-244230664No ratings yet
- Hcahps Omg Data BeforeDocument1 pageHcahps Omg Data Beforeapi-244230664No ratings yet
- Daisy Nomination Bill ValentineDocument2 pagesDaisy Nomination Bill Valentineapi-244230664No ratings yet
- Pain Minutes 031914Document2 pagesPain Minutes 031914api-244230664No ratings yet
- Email From Mandy 7 14 14Document1 pageEmail From Mandy 7 14 14api-244230664No ratings yet
- Su-Ham Proposal FinalDocument1 pageSu-Ham Proposal FinalRohit KumarNo ratings yet
- 27Document2 pages27Helen UgochukwuNo ratings yet
- Yakeley 2018 Psychoanalysis in Modern Mental Health PracticeDocument8 pagesYakeley 2018 Psychoanalysis in Modern Mental Health PracticeJonathan RiveraNo ratings yet
- 19 Nov Malam Qara Fatikha FixDocument9 pages19 Nov Malam Qara Fatikha FixatikahNo ratings yet
- Intra Uterine Insemination - IUIDocument15 pagesIntra Uterine Insemination - IUIlayyous100% (1)
- Buku BacaanDocument329 pagesBuku BacaanNurhasni FebrianiNo ratings yet
- What Is Alzheimer's - Alzheimer's AssociationDocument6 pagesWhat Is Alzheimer's - Alzheimer's AssociationRatnaPrasadNalamNo ratings yet
- Preoperative NICE GuidelinesDocument117 pagesPreoperative NICE GuidelinesDana ApelaNo ratings yet
- FS13 PolycythemiaVera FactSheetDocument7 pagesFS13 PolycythemiaVera FactSheetMala 'emyu' UmarNo ratings yet
- Mood DisordersDocument1 pageMood DisordersTeresa MartinsNo ratings yet
- Doxazosin Mesilate - Martindale 36edDocument1 pageDoxazosin Mesilate - Martindale 36edSvetlana Maiochi LodovicoNo ratings yet
- International Skin Care 3.17.14Document8 pagesInternational Skin Care 3.17.14typing expertNo ratings yet
- The Magic of Ilizarov PDFDocument310 pagesThe Magic of Ilizarov PDFOrto Mesp83% (6)
- Novartis NVS Q4 2016 Ir PresentationDocument84 pagesNovartis NVS Q4 2016 Ir PresentationmedtechyNo ratings yet
- Pelvic Organ ProlapseDocument9 pagesPelvic Organ ProlapseSonny Dizon PareñasNo ratings yet
- Respiratory QuestionnaireDocument2 pagesRespiratory QuestionnaireMadhu SudhanNo ratings yet
- Efavirenz Chem OlympicsDocument1 pageEfavirenz Chem OlympicsdreamingsnowNo ratings yet
- Greywater Filtration Systems: For A Sustainable Water CultureDocument36 pagesGreywater Filtration Systems: For A Sustainable Water CultureJen Beatrice DiazNo ratings yet
- HarrisonDocument18 pagesHarrisonayuliadrNo ratings yet
- Amlodipine CPDocument2 pagesAmlodipine CPRose EchevarriaNo ratings yet
- Current Evidence For The Management of Schizoaffective DisorderDocument12 pagesCurrent Evidence For The Management of Schizoaffective DisorderabdulNo ratings yet
- Module 4 (Basics of Sti, Hiv & Aids)Document37 pagesModule 4 (Basics of Sti, Hiv & Aids)Marky RoqueNo ratings yet
- A Ryan Case StudyDocument6 pagesA Ryan Case StudycryziaNo ratings yet
- EyeDocument11 pagesEyeSyed Ali HaiderNo ratings yet
- Achytherapy 3HAXAPDocument464 pagesAchytherapy 3HAXAPIkang FauziNo ratings yet
- CystosDocument19 pagesCystosneenuj_5No ratings yet
- Pasifik Medikal CatalogueDocument24 pagesPasifik Medikal CatalogueAr ZahNo ratings yet
- My Sister's KeeperDocument27 pagesMy Sister's KeepersindhujaNo ratings yet
- Cholera & DysenteryDocument28 pagesCholera & DysenterySherbaz Sheikh100% (1)
- Katerina P Reilly ResumeDocument2 pagesKaterina P Reilly Resumeapi-286221742No ratings yet