Professional Documents
Culture Documents
Perianesthesia Nursing Standards of Practice Jennifer J Smith
Uploaded by
api-239605726Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Perianesthesia Nursing Standards of Practice Jennifer J Smith
Uploaded by
api-239605726Copyright:
Available Formats
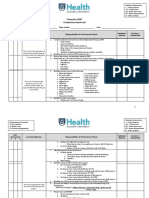
Running head: PERIANESTHESIA NURSING STANDARDS OF PRACTICE
Perianesthesia Nursing Standards of Practice
Jennifer J. Smith
Ferris State University
PERIANESTHESIA NURSING STANDARDS OF PRACTICE
Abstract
The American Society of PeriAnesthesia Nurses, 2012-2014 Perianesthesia Nursing Standards,
Practice Recommendations and Interpretive Statements sets standards of practice for providing
safe, high quality care. A self-evaluation was completed analyzing current nursing practice
according to each of these standards. Professional goals are identified after self-reflection
allowing opportunity for professional growth and development.
PERIANESTHESIA NURSING STANDARDS OF PRACTICE
Perianesthesia Nursing Standards of Practice
Perianesthesia nursing encompasses a scope of practice that includes preanesthesia and
postanesthesia levels of care. The American Society of PeriAnesthesia Nurses (ASPAN)
provides the standards of perianesthesia nursing practice, clinical practice guidelines and
recommendations for professional nurses. This paper will provide a self-assessment of these
standards and an analysis of current clinical experiences that meet the standards. The selfevaluation will determine professional goals and develop a measureable plan to attain these
goals.
Standards of Perianesthesia Nursing Practice
Standard 1: Patient Rights
This standard identifies the importance of patient rights that includes recognizing and
maintaining the autonomy, confidentiality, privacy, dignity and worth of individuals (ASPAN,
2012). As a perianesthesia nurse, it is important to value and understand each patients
individuality in order to provide comprehensive, quality care. This also includes providing
culturally competent care, which can affect the patients understanding of instructions and
compliance with the proposed treatment plan. It is vital to include the patient and family in the
development of the treatment plan in order to establish what they value and address the patients
needs and concerns.
Maintaining confidentiality protects the patients rights. Closing a door or a curtain
assists with maintaining confidentiality. I introduce myself to the patient and indicate what my
role is in caring for the patient. One of the questions I ask patients is if they want information
shared with their family. This question establishes that the nurse will only share information
about the patients care if they give their permission. It also helps to establish a relationship of
PERIANESTHESIA NURSING STANDARDS OF PRACTICE
trust and respect and it demonstrates to the patient that the nurse is concerned with the patients
privacy.
I feel that one of my strengths is the patient rights nursing standard. I strive to adhere to
preserving patient rights and act as a patient advocate throughout the perianesthesia experience.
The perianesthesia environment is challenging as patients are anxious about having surgery and
there is limited time to spend with the patient and family. By utilizing Jean Watsons Theory of
Human Caring (2008), when entering the room I am able to focus on connecting with the patient,
being present, and developing a transpersonal relationship. Applying nursing theory into
practice has enhanced my effectiveness as a nurse and provided a way to connect with patients
and families while maintaining patient privacy and dignity.
I plan to maintain competency for this standard by keeping the patient as the center of my
focus and care. To do this I will continue to utilize Jean Watsons theory of human caring to
establish a transpersonal relationship. This will focus my attention on the individual and their
unique needs, providing non-judgmental care regardless of their socio-economic status, culture,
personal attributes, or age. I will continue to ask the patients permission prior to sharing
information with family. In order to evaluate my effectiveness, each month I will do a selfevaluation of my nursing care along with asking for feedback from patients and families.
Standard 2: Environment of Care
According to the ASPAN (2012) standards, perianesthesia nursing practice promotes and
maintains a safe, comfortable and therapeutic environment of care. The perianesthesia practice
environment involves administration of medications, anesthetic agents and the performance of
procedures that can have a significant impact on patient safety altering motor and sensory
functions (ASPAN, 2012). Maintaining competency with perianesthesia clinical skills is crucial
PERIANESTHESIA NURSING STANDARDS OF PRACTICE
with providing safe, patient care. In addition, knowledge of medications and anesthetic agents
along with the appropriate dosage, side effects, and possible complications is important to
maintaining a safe environment of care.
I maintain the necessary perianesthesia skills by completing continuing educational
opportunities along with clinical experience. I participate in internal/external disaster drills to
ensure patient safety should a disaster occur. This also includes practicing mock drills with
evacuation of patients in case of an emergency.
There are policies in place to ensure patient safety in the perianesthesia environment. I
initiate appropriate safety measures when assisting with invasive lines such as hand hygiene,
administration of medication, application of oxygen and closely monitoring the patient for any
adverse effects. As a patient advocate, I promote a therapeutic, calming environment by giving
the patient warm blankets, dimming the lights, and turning the television to the relaxation
channel. Patient safety is vital to providing the patient with a positive outcome.
For this standard, I plan to maintain a safe environment of care by following policies and
procedures that protect the patient from harm. This includes monitoring the patient closely after
administering sedation. I will also adhere to infection prevention and isolation standards to
protect staff, patients, and families. On a yearly basis, I will keep up to date on policies and
procedures that affect patient safety and care.
Standard 3: Staffing and Personnel Management
Staffing and personnel management refers to appropriate staffing levels with competent
staff to meet the needs of patients and families based on patient acuity, census, patient flow
process and physical facility (ASPAN, 2012). Nurses working in the perianesthesia areas need
to maintain a current Advance Cardiac Life Support (ACLS) and Pediatric Advanced Life
PERIANESTHESIA NURSING STANDARDS OF PRACTICE
Support (PALS) provider status. There are also two specialty certifications available to increase
the expertise of practicing in this area. I maintain my ACLS and PALS certifications along with
successfully completing the Certified Ambulatory PeriAnesthesia (CAPA) certification to
maintain competency and increase expertise.
I am actively involved with ensuring safe staffing levels and skill mix in providing care
to perianesthesia patients. My role and responsibility as a patient care coordinator is to adjust
staffing on a daily basis to meet the individual needs of the patients based on acuity, census, and
patient flow. This includes assessing staffs skill levels and determining appropriate
assignments, along with assigning mentors to new staff for optimal patient outcomes.
My professional goal for this standard is to maintain my perianesthesia skills in order to
meet the needs of patients and families. To do this, every two years I will renew my ACLS and
PALS provider status. Every three years I will maintain the CAPA certification by meeting the
necessary requirements. In addition, I will continue to evaluate staffing on a daily basis to
ensure appropriate staffing levels to provide safe, quality care to patients. This will be evaluated
at daily huddles as well as at weekly leadership meetings.
Standard 4: Quality Improvement
Quality improvement for perianesthesia nursing includes monitoring and evaluating
patient care to identify issues, implement resolutions and evaluate outcomes to improve care and
safety (ASPAN, 2012). Nurses need to be actively involved in quality improvement initiatives to
provide quality care and to enhance the surgical experience for the patient and their family. An
example of a quality improvement initiative that I am involved with is an identified increase in
post-operative surgical site infections for total joint replacement patients. Surgical site infections
are part of a Surgical Care Improvement Project (SCIP) measurement to improve surgical care
PERIANESTHESIA NURSING STANDARDS OF PRACTICE
by significantly reducing surgical complications (Joint Commission, 2014). A multidisciplinary
team was formed to review evidence-based practice (EBP) along with current practices. This
included the current processes for pre-operative patient cleansing, surgical clipping, appropriate
pre-operative antibiotic selection, and the intra-operative surgical site prep process.
I am leading a multidisciplinary team to implement a new pre-operative patient cleansing
protocol based on EBP. To accomplish this new process, the team is focusing on planning,
collaboration, education, and implementation. A baseline measurement was conducted prior to
implementation to monitor compliance with the new protocol. Further evaluation will include a
short-term goal to increase patient compliance and a long-term goal to monitor the effect on
infections rates. Perianesthesia nurses need to seek opportunities for improvement, utilize
research and evidence, and incorporate new processes into practice to improve outcomes for
patients.
My goal for meeting and exceeding this standard is to monitor quality of patient care by
monitoring compliance with quarterly SCIP measures. If SCIP measures fall below standards, I
will participate in developing an action plan to meet the quality measures and re-evaluate six
months after implementation. Another intervention is to review patient satisfaction scores to
determine the patients perception of quality and care. This information is beneficial as it
provides the patients perception of their surgical experience and allows an insight into
developing interventions to improve patient satisfaction scores. Patient satisfaction scores will
be reviewed bi-annually to assess if quality improvement initiatives need to be developed.
Standard 5: Research and Clinical Inquiry
According to ASPAN (2012), research and clinical inquiry is important mechanisms for
describing, understanding and validating perianesthesia nursing practice (p. 23). Research and
PERIANESTHESIA NURSING STANDARDS OF PRACTICE
EBP need to guide decision making in the nurses clinical, educational and management roles
(ASPAN, 2012). Perianesthesia nurses need to challenge current practices by participating in
clinical inquiry projects and reviewing EBP to determine the best interventions for preventing
surgical complications.
Currently, one challenging area for perianesthesia nurses is determining best practice
protocols for safely caring for patients with sleep apnea. I am participating in an
interdisciplinary team to review EBP and to develop protocols for sleep apnea patients. There
has been limited research conducted on recommended types of anesthesia, perioperative use of
medications, and length of stay for scheduled outpatient surgeries. Benchmarking with other
organizations has resulted with inconsistent practices in caring for these types of patients. It is
essential to use research and clinical inquiry to guide decision-making and development of
protocols for optimal patient outcomes.
I plan to maintain my yearly ASPAN membership that allows me to receive monthly
journals containing EBP articles about current practices and recommended guidelines. Being an
ASPAN member provides an opportunity to network with other perianesthesia units and nurses
to benchmark about best practices and ask clinical questions. I will challenge myself to read
each monthly ASPAN journal and look for opportunities to change processes and to improve
patient outcomes.
Standard 6: Nursing Process
The perianesthesia nurse needs to systematically assess each patient to develop an
individualized plan of care across the perianesthesia continuum (ASPAN, 2012). This process
includes assessment, planning and implementation, and evaluation. Perianesthesia nurses need
to be knowledgeable of clinical protocols and practice guidelines and develop interventions that
PERIANESTHESIA NURSING STANDARDS OF PRACTICE
will result in positive patient outcomes. Collaboration with the patient, family and other
healthcare personnel is vital to developing an effective plan of care throughout the patients
surgical experience.
The nursing process is my strength in the pre-operative and discharge areas. I am able to
develop a plan of care that is individualized for each patient and prioritize care based on the
patients needs. Providing the patient and family with a description of the surgical process helps
to decrease anxiety. Perianesthesia nursing is an art, and being able to establish trust and respect
in a short amount of time can increase patient satisfaction and allow for open communication. In
Watsons (2008) caritas process number eight, the caring relationship and environment are
generated by the nurses heartfelt, loving presence, and the consciousness he or she holds,
helping shape the patients health and healing experience as well as the nurses own experiences
(p. 137). I believe that by connecting with the patient and family, the nurse can positively
influence their care by creating an environment of positive, spiritual energy.
My goal is to continue diligence with thorough, individualized assessments involving the
patients and families. Understanding the patients needs and concerns will help to develop a
perianesthesia care plan. Thorough documentation and communication is the key to sharing this
information with other healthcare providers. I will monitor the effectiveness of the interventions
by reviewing quarterly documentation and patient outcomes. I will also participate in annual
peer reviews to receive constructive input into my professional practice and develop goals based
on the feedback.
Conclusion
This self-assessment of the perianesthesia standards of practice has provided me with
valuable information about my professional nursing practice. Analyzing the standards along
PERIANESTHESIA NURSING STANDARDS OF PRACTICE
10
with my current practice and clinical experience has helped me establish a plan for maintaining
competency and promoting professional growth. Self-reflection allowed me to evaluate my
current level in my specialty area and enhance my professional identity.
PERIANESTHESIA NURSING STANDARDS OF PRACTICE
11
References
American Society of Perianesthesia Nurses [ASPAN]. (2012). 2012-2014 Perianesthesia nursing
standards, practice recommendations and interpretive statements. Cherry Hill, NJ:
ASPAN.
Joint Commission. (2014). Surgical Care Improvement Project. Retrieved from http://
www.jointcommission.org/surgical_care_improvement_project/
Watson, J., (2008). Nursing: The philosophy and science of caring (Rev. ed.). Boulder, CO:
University Press of Colorado.
Yoder-Wise, P. S. (2014). Leading and managing in nursing (5th ed.). St. Louis, MO: Elsevier
Mosby.
You might also like
- Self-Assessment of Nursing Standards of PracticeDocument17 pagesSelf-Assessment of Nursing Standards of Practiceapi-260548731100% (1)
- Clinical Nursing JudgmentDocument5 pagesClinical Nursing Judgmentapi-508051902No ratings yet
- Neuroscience Nursing: Scope and Standards of PracticeFrom EverandNeuroscience Nursing: Scope and Standards of PracticeRating: 2.5 out of 5 stars2.5/5 (3)
- Correctional Nursing: Scope and Standards of Practice, Third EditionFrom EverandCorrectional Nursing: Scope and Standards of Practice, Third EditionRating: 5 out of 5 stars5/5 (1)
- The COAT & Review Approach: How to recognise and manage unwell patientsFrom EverandThe COAT & Review Approach: How to recognise and manage unwell patientsRating: 5 out of 5 stars5/5 (1)
- Pain Management Nursing: Scope and Standards of Practice, 2nd EditionFrom EverandPain Management Nursing: Scope and Standards of Practice, 2nd EditionRating: 5 out of 5 stars5/5 (1)
- Nursing's Leading Edges: Advancing the Profession through Specialization, Credentialing, and CertificationFrom EverandNursing's Leading Edges: Advancing the Profession through Specialization, Credentialing, and CertificationNo ratings yet
- Transplant Nursing: Scope and Standards of PracticeFrom EverandTransplant Nursing: Scope and Standards of PracticeNo ratings yet
- Professional Role Development Paper - Final 1Document7 pagesProfessional Role Development Paper - Final 1api-532705739No ratings yet
- New Nurse Evaluation Form in PDF-3Document14 pagesNew Nurse Evaluation Form in PDF-3coco1210No ratings yet
- Legal Implications Document A Schneider PDFDocument52 pagesLegal Implications Document A Schneider PDFAmrod Inglorion100% (2)
- Observation Summary 2Document5 pagesObservation Summary 2api-493028287No ratings yet
- CHOP Nursing Shared Governance Structure Ensures Quality Patient CareDocument18 pagesCHOP Nursing Shared Governance Structure Ensures Quality Patient CareHendra HefaNo ratings yet
- Evidence Based Standards For Measuring Nurse Staffing and PerformanceDocument208 pagesEvidence Based Standards For Measuring Nurse Staffing and Performancemr_jamzNo ratings yet
- APN Adult Gerontology PresentationDocument57 pagesAPN Adult Gerontology PresentationMelissa Makhoul100% (1)
- Program Graduate CompetencyDocument10 pagesProgram Graduate Competencyapi-349372265No ratings yet
- SOP TemplateDocument2 pagesSOP TemplatePaulin NiyomugaboNo ratings yet
- Deep Sternal Wound Infections: Evidence For Prevention, Treatment, and Reconstructive SurgeryDocument12 pagesDeep Sternal Wound Infections: Evidence For Prevention, Treatment, and Reconstructive Surgerylsintaningtyas100% (1)
- SGNA StandardsofClinicalNursingPractice 2014 FinalDocument26 pagesSGNA StandardsofClinicalNursingPractice 2014 FinalSimona Adaniloae0% (1)
- RN Self Assessment ExamplesDocument10 pagesRN Self Assessment ExamplesAmbika SuwalNo ratings yet
- Surgical Safety ChecklistDocument20 pagesSurgical Safety ChecklistAnonymous h8gt8KlpiCNo ratings yet
- Personal Philosophy of Nursing 2015Document8 pagesPersonal Philosophy of Nursing 2015api-283120230100% (1)
- Resume CrnaDocument2 pagesResume Crnaapi-239217849No ratings yet
- Root Cause Analysis FallsDocument8 pagesRoot Cause Analysis Fallsapi-355495007No ratings yet
- Medication Administration Error 3Document16 pagesMedication Administration Error 3Priya bhattiNo ratings yet
- Ethical DilemmaDocument5 pagesEthical Dilemmaapi-520874386No ratings yet
- CEN Guide 4: Guide For The Inclusion of Environmental Aspects in Product StandardsDocument18 pagesCEN Guide 4: Guide For The Inclusion of Environmental Aspects in Product StandardsLauren GarciaNo ratings yet
- Rapid Response Team WorksheetDocument1 pageRapid Response Team Worksheetapi-403028741No ratings yet
- Medication Errors PaperDocument6 pagesMedication Errors Paperapi-542442476No ratings yet
- The Intersection: Where Evidence Based Nursing and Information Literacy MeetFrom EverandThe Intersection: Where Evidence Based Nursing and Information Literacy MeetSue PhelpsRating: 2 out of 5 stars2/5 (1)
- Crit Care Nurse 2013 Stites 68 78Document13 pagesCrit Care Nurse 2013 Stites 68 78Patricia TelloNo ratings yet
- Medication Errors FinalDocument5 pagesMedication Errors Finalapi-379817190No ratings yet
- Saudi Nursing Lisencure Examination Applicant GuideDocument16 pagesSaudi Nursing Lisencure Examination Applicant GuideSomaya SiddiqueNo ratings yet
- How To Improve Patient Safety in Intensive Care Units Albert Castellheim MASTER's THESISDocument158 pagesHow To Improve Patient Safety in Intensive Care Units Albert Castellheim MASTER's THESISAngeline Adrianne100% (1)
- Continuous Renal Replacement Therapy (CRRT) Initial Competency Assessment and ValidationDocument2 pagesContinuous Renal Replacement Therapy (CRRT) Initial Competency Assessment and Validationalex100% (1)
- Personal Statement 2Document2 pagesPersonal Statement 2Raunak PrasadNo ratings yet
- Nurising Assignment ConflictDocument10 pagesNurising Assignment ConflictLauren KalantaNo ratings yet
- Documentation: Basic Nursing: Foundations of Skills & Concepts DocumentationDocument8 pagesDocumentation: Basic Nursing: Foundations of Skills & Concepts DocumentationJona GarzonNo ratings yet
- Morton Ch01Document11 pagesMorton Ch01headepartmentNo ratings yet
- DNP Application Essay Michelle MilesDocument6 pagesDNP Application Essay Michelle Milesapi-521620733No ratings yet
- TransitionDocument13 pagesTransitionDonna NituraNo ratings yet
- Advanced Practice NursingDocument11 pagesAdvanced Practice NursingSaher Kamal100% (2)
- Future Scope of Independent Nurse Practitioners in IndiaDocument34 pagesFuture Scope of Independent Nurse Practitioners in IndiaSanjana Namchoom67% (3)
- Quality Improvement PaperDocument8 pagesQuality Improvement Paperapi-401406690No ratings yet
- Basic of Implementating SSCDocument12 pagesBasic of Implementating SSCArik Faisal100% (1)
- Assessment of An ICU PatientDocument71 pagesAssessment of An ICU PatientTito Tesfaye100% (1)
- Restraint CompetencyDocument6 pagesRestraint CompetencyFrederick RyanNo ratings yet
- Critical Care Nursing EssentialsDocument42 pagesCritical Care Nursing Essentialsikram ullah khanNo ratings yet
- Patient Safety: An Introduction: Jhessie L. Abella, RN, RM, MAN, CpsoDocument22 pagesPatient Safety: An Introduction: Jhessie L. Abella, RN, RM, MAN, Cpsoprinsepejesse100% (1)
- ICU Admission PolicyDocument4 pagesICU Admission PolicySapiah RamanNo ratings yet
- Clinical ExemplarDocument4 pagesClinical Exemplarapi-272451466No ratings yet
- Research Paper - FinalDocument16 pagesResearch Paper - Finalapi-455663099No ratings yet
- MedManagement48 50Document3 pagesMedManagement48 50Fausto David Herrera UrreaNo ratings yet
- Personal Philosophy of Nursing PaperDocument10 pagesPersonal Philosophy of Nursing Paperapi-433883631No ratings yet
- RN Interview - Medical-Surgical NurseDocument4 pagesRN Interview - Medical-Surgical Nurserwilson71No ratings yet
- Long Term Care ToolkitDocument11 pagesLong Term Care Toolkitapi-546503976100% (1)
- Prismaflex CRRT Competency Based Tool PDFDocument5 pagesPrismaflex CRRT Competency Based Tool PDFalex100% (1)
- Nursing LeadershipDocument264 pagesNursing LeadershipAllo Lora100% (2)
- Nursings Leadership Role in Population Based Issues Jennifer J SmithDocument9 pagesNursings Leadership Role in Population Based Issues Jennifer J Smithapi-239605726No ratings yet
- Self-Assessment of Reasoning Weebly Jennifer J SmithDocument5 pagesSelf-Assessment of Reasoning Weebly Jennifer J Smithapi-239605726No ratings yet
- Healthcare Disparities and Healthcare Policy For Rural Populations WeeblyDocument8 pagesHealthcare Disparities and Healthcare Policy For Rural Populations Weeblyapi-239605726No ratings yet
- Personal Health Promotion Plan-WeeblyDocument17 pagesPersonal Health Promotion Plan-Weeblyapi-239605726No ratings yet
- Critique of Watsons Theory of Human Caring WeeblyDocument9 pagesCritique of Watsons Theory of Human Caring Weeblyapi-239605726100% (1)
- Service Learning Synthesis PaperDocument8 pagesService Learning Synthesis Paperapi-239605726No ratings yet
- Jennifer J Smith Portfolio RN-BSN Checklist Completed For Nurs 440Document1 pageJennifer J Smith Portfolio RN-BSN Checklist Completed For Nurs 440api-239605726No ratings yet
- The Role of A Perianesthesia ManagerDocument7 pagesThe Role of A Perianesthesia Managerapi-239605726No ratings yet
- Nurs 350 Ebnp Group Project PaperDocument12 pagesNurs 350 Ebnp Group Project Paperapi-239605726No ratings yet
- Eng 321 Formal Academic Summary Jennifer J Smith Draft 2Document3 pagesEng 321 Formal Academic Summary Jennifer J Smith Draft 2api-239605726No ratings yet
- MangaDocument73 pagesMangaRita BrandãoNo ratings yet
- Best Practices for Vulnerability Assessments (VADocument25 pagesBest Practices for Vulnerability Assessments (VAdehnhaide100% (1)
- Management Consulting and International Business S PDFDocument15 pagesManagement Consulting and International Business S PDFsamaNo ratings yet
- Benchmark Railway Infrastructure ManagementDocument19 pagesBenchmark Railway Infrastructure ManagementAdhitya Setyo PamungkasNo ratings yet
- 202010-02 Lowland WASH Weekly Reports PDFDocument24 pages202010-02 Lowland WASH Weekly Reports PDFAbebaw KebedeNo ratings yet
- 5 Models For Data Stewardship 106846Document23 pages5 Models For Data Stewardship 106846Rocío Vázquez100% (1)
- RGS6035.E2 Research Study ProposalDocument15 pagesRGS6035.E2 Research Study ProposalJoel EckelNo ratings yet
- I Oniqua 12 Best Practices OG FINALDocument9 pagesI Oniqua 12 Best Practices OG FINALHasan Ali AssegafNo ratings yet
- Barbering Course DesignDocument94 pagesBarbering Course DesignNovalyn PaguilaNo ratings yet
- Leading with Compassion: A Guide to Compassionate Healthcare LeadershipDocument73 pagesLeading with Compassion: A Guide to Compassionate Healthcare LeadershipnibretzwNo ratings yet
- IVT Network - Quality Risk Management and Qualification-A Maturing Partnership With Real Patient Benefits - 2017-01-20Document10 pagesIVT Network - Quality Risk Management and Qualification-A Maturing Partnership With Real Patient Benefits - 2017-01-20Marco LopezNo ratings yet
- Week 10 ControllingDocument51 pagesWeek 10 ControllingMefilzahalwa AlyayouwanNo ratings yet
- Assess your leadership skills for innovation and changeDocument3 pagesAssess your leadership skills for innovation and changeGeancarlo Guilliano Alexandre Sandoval SolisNo ratings yet
- MBPGDocument225 pagesMBPGgodex7No ratings yet
- Guide To Benchmarking Oct2007Document24 pagesGuide To Benchmarking Oct2007Akhil Ayyakutty100% (2)
- Checking Best Practices For Preventive MaintenanceDocument5 pagesChecking Best Practices For Preventive MaintenanceGeviena Pinky Sy SarmientoNo ratings yet
- 2 - ESBM - LEVEL of Practice6Document5 pages2 - ESBM - LEVEL of Practice6QUEENIE BUTALIDNo ratings yet
- Hibernia Study (Flare)Document178 pagesHibernia Study (Flare)bmgarisNo ratings yet
- SOP Implementation Success-EbookDocument56 pagesSOP Implementation Success-Ebookranga.raman100% (3)
- Roland Berger Corporate Headquarters Short Version 20130502 PDFDocument27 pagesRoland Berger Corporate Headquarters Short Version 20130502 PDFEmmanuellPuzoGalvanNo ratings yet
- RINA Academy technical courses for naval ships personnelDocument24 pagesRINA Academy technical courses for naval ships personnelmaria_bustelo_2No ratings yet
- Bestufs II Brochure Draft 002Document2 pagesBestufs II Brochure Draft 002api-3756494No ratings yet
- An Integrated System For Change Management in ConstructionDocument2 pagesAn Integrated System For Change Management in ConstructionMike MorrisNo ratings yet
- Making Onboarding Work - Kaiser AssociatesDocument12 pagesMaking Onboarding Work - Kaiser Associatessimmi2768No ratings yet
- Performance Automation and Tuning 3 DayDocument5 pagesPerformance Automation and Tuning 3 DayraunakrayrnkNo ratings yet
- ERM-Enterprise Risk ManagementDocument13 pagesERM-Enterprise Risk ManagementUsman Hamid100% (1)
- Public Sector Reform in Central Asia and The CaucasusDocument12 pagesPublic Sector Reform in Central Asia and The CaucasusManivannan M.BNo ratings yet
- Best Practices For Organizing 360° Construction PhotosDocument9 pagesBest Practices For Organizing 360° Construction PhotosnandaNo ratings yet
- FortiAnalyzer Best Practices GuideDocument18 pagesFortiAnalyzer Best Practices GuideElbarni MohamedNo ratings yet
- Budgeting Budgetary Control Techniques PDFDocument26 pagesBudgeting Budgetary Control Techniques PDFPunit JainNo ratings yet