Professional Documents
Culture Documents
Dykstra, Amber Evidencebasedpractice
Uploaded by
api-284180001Original Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Dykstra, Amber Evidencebasedpractice
Uploaded by
api-284180001Copyright:
Available Formats
RUNNING HEAD: Evidence Based Practice
Evidence Based Practice Paper
Amber Dykstra
NURS 324
Evidence Based Practice
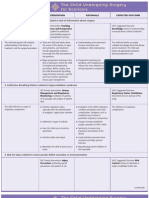
Purpose of Paper
1. Purpose (all reasoning has a purpose)
The purpose of my Evidence Based Practice
topic is to review the wet to dry dressing
procedure and find alternative dressing
choices. Wet to dry is a very painful dressing
change that can be done up to three times a
day. If there are less painful, but just as
effective dressings, they should be considered.
2. Questions at issue or central problem (all
The issue at hand is wet to dry dressing is very
reasoning is an attempt to figure something
painful. Does the effectiveness of wet to dry
out, to settle some question, solve some
dressing justify the pain a patient has to go
problem)
through? Are there other procedures that are
just as effective as wet to dry dressing but less
painful?
3. Point of view (all reasoning is done from
I have had patients with stage three pressure
some point of view; think about the
ulcers and diabetic foot wounds and have a wet
stakeholders)
to dry dressing. When I changed their
dressings, my patients cry out in pain.
According to Lee Johnson of Johns Hopkins
University School of Medicine, this pain
occurs because sensitive nerve fibers in the
wound bed are being exposed.
4. Information (all information is based on
According to Lee Johnson, there are
data, information, evidence, experience,
alternatives to wet to dry dressings. Wet to dry
research)
dressings can delay wound healing by
removing migrating epithelium. Alternatives
include but are not limited to foams, alginate
and hydrofibers, hydrogels and cellulose, and
hydrocolloids.
5. Concepts and ideas (all reasoning is
Debridement gets rid of the slough, but what if
expressed through, and shaped by, concepts
it is being performed four times a day, how
and ideas)
effective is that?
6. Assumptions (all reasoning is based on
I believe that there are more humane methods
assumptions-beliefs we take for granted)
to debride a wound. When a patient
experiences pain, they do not heal as well.
7. Implications and consequences (all
A consequence to reducing wet to dry
reasoning leads somewhere. It has implications dressings is the cost of wound supplies may go
and when acted upon, has consequences)
up. The type of wound being treated depends
on the dressing type. The mechanics of wound
Evidence Based Practice
8. Inference and interpretation (all reasoning
contains inferences from which we draw
conclusions and give meaning to data and
situations)
alternatives also would have to be taught to
nurses and doctors. The cost to run classes may
make the budget rise as well.
Wet to dry dressing has been used for years by
physicians and nurses. The medical world has
evolved and focused more on the patients,
experience. I have experienced my patients
being in pain. My goal as a nurse is to reduce
their pain level and assist in healing the wound.
Annotations
Annotation 1
Johnson, L. (2009). Beyond wet-to-dry: a rational approach to treating chronic wounds. E Plasty.
Retrieved from http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2680240/.
Lee Johnson has a BA and works at the Johns Hopkins University School of Medicine. This
article is targeted for nurses and doctors who treat different kinds of wounds. Johnson describes
three categories of wound dressings and what they are intended for. Occlusive dressings create a
moist environment, promote mechanic debridement, and reduce wound pain. Antimicrobials are
used when there are too many bacteria and healing is inhibited. These antimicrobials aide in
protecting wounds from MRSA and VRE as well. The last wound dressing is the impregnated
gauze. These gauzes have multiple uses but continue to keep the wound moist and debride
without as much pain caused by wet to dry dressing changes. Johnsons article describes
alternatives that are less painful but just as effective, if not more, than wet to dry dressings. He
demonstrates my point on how wet to dry dressings may cause more harm than good when being
performed.
Annotation 2
Evidence Based Practice
Dinah, F. (2006). Gauze packing of open surgical wound: empirical or evidence-based practice?
Ann R Coll Surgical English, 88(1), 33-36.
Dinah is a surgical physician in the Department of Orthopaedic at St. Helier Hospital in
Carshalton in the United Kingdom. The article is discusses the types of dressings appropriate for
surgical use. Dinah also discusses the cost of the dressings. Although the more advanced
dressings to cover wounds are more expensive, the cost equals and is sometimes less, than wet to
dry dressing. Wet to dry dressings are performed multiple times a day and labor has to factor into
the cost as well. The more advanced dressings require changing daily and allow nurses to
perform other duties. This article is for the nurses who specialize in wound treatment. It shows
that wet to dry dressings doesnt save as much money as it was thought to.
Annotation 3
Ovington, L.G. (2007). Hanging wet-to-dry dressings out to dry. Home Healthcare Nurse, 19(8),
477-484.
Liz Ovington is a consultant for wound products. In the article she discusses why gauze dressing
changes should not be the first option. Her first reasoning is that there is impeded healing due to
a lack of heat. When the gauze becomes cold and wet, it does not evaporate the wound fluids
such as slough. She also discusses why there is in increased risk for infection. In one study she
states that bacteria could get through 64 layers of dry gauze. Infection rates are higher than if
hydrocolloids were used. Ovington also discusses how there are many patients who change a
wet-to-dry dressing at home and the risks of not having a clean environment. If these patients
were to have foam, they could replace the foam daily without difficulty. Ovington is educated
clinicians that there are more options and why they should be appropriately utilized.
Evidence Based Practice
Reflection
How did the planning process, where you thought about what you wanted to change,
prepare you for the EBPP?
While planning I had to think about what I really wanted to change and be able to have
more knowledge to educate people on my point of view. I thought about my recent work
experiences and how my patients did not look forward to their dressing change. I realized that it
was a topic that there has to be research on, and more people need to be educated on alternatives
to wet-to-dry dressing.
How did the peer evaluation process prepare you for the EBPP?
The peer evaluation made me evaluate why I felt wet-to-dry dressing is more
inappropriate. I feel that as nurses we dont always question the physician practice. I feel that we
should be able to make suggestions as to what to do for treatment. I realized while reading others
evidence based practice that there are many topics that should be changed and evaluated.
Evidence based practice is in place for a reason and as nurses we should review the research to
come up with appropriate protocols and policies.
Do you feel you are prepared to elicit change in your practice with your proposal?
How does it fit into quality health care?
If the opportunity were to present itself to me I feel that I have the knowledge and
courage to ask the physician questions. My first question would be why they chose wet-to-dry
dressing. Next would be to ask why the other alternatives were not appropriate for the particular
wound being discussed. I dont see many wet-to-dry dressings on my current floor, but my
patients surprise me everyday. I now feel a little more educated on the alternatives being used.
However, they are still the physician, but I can learn from them.
Evidence Based Practice
What could you have done better?
I feel that I shouldve explained both the pros and cons of wet-to-dry dressing. There is a
reason that it is still the number one form of dressing used in surgical rooms today. I understand
why physicians would use it first. It does absorb a lot of the blood. However, post-surgical
settings should be reviewed and the dressing type changed.
How well do you think you are using the EOR? Do they make sense to you (why or
why not?)
I feel that I use the EOR but not all of the time. They make sense to me, but again, while
in my everyday nursing practice I dont think about it. If I have a question I research the answer.
I believe I perform the 8 steps. The step I think most about while doing it is the implications and
consequences. I feel that it is an important part of decision making.
You might also like
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Amber Dykstra, R.N.: 4506 Bonanza Drive NE Grand Rapids, Michigan 49525Document1 pageAmber Dykstra, R.N.: 4506 Bonanza Drive NE Grand Rapids, Michigan 49525api-284180001No ratings yet
- Dykstra, Amber Healthpromotion2Document7 pagesDykstra, Amber Healthpromotion2api-284180001No ratings yet
- Amber Dykstra ResumeDocument2 pagesAmber Dykstra Resumeapi-284180001No ratings yet
- Dykstra, Amber ProfessionaldevelopmentDocument10 pagesDykstra, Amber Professionaldevelopmentapi-284180001No ratings yet
- Dykstra, Amber ServicelearningDocument7 pagesDykstra, Amber Servicelearningapi-284180001No ratings yet
- Dykstra, A ClinicalquestionDocument9 pagesDykstra, A Clinicalquestionapi-284180001No ratings yet
- Dykstra, Amber EvaluatingownpracticeDocument6 pagesDykstra, Amber Evaluatingownpracticeapi-284180001No ratings yet
- Dykstra, Amber PolicybriefDocument6 pagesDykstra, Amber Policybriefapi-284180001No ratings yet
- Dykstra, Amber HealthpromotionDocument10 pagesDykstra, Amber Healthpromotionapi-284180001No ratings yet
- Rural NursingDocument17 pagesRural Nursingapi-284180001No ratings yet
- Dykstra, Amber HealthyworkenvironmentDocument24 pagesDykstra, Amber Healthyworkenvironmentapi-284180001No ratings yet
- Handwashing BoothDocument8 pagesHandwashing Boothapi-284180001No ratings yet
- Dykstra, Amber WatsonnursingmodelDocument32 pagesDykstra, Amber Watsonnursingmodelapi-284180001No ratings yet
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- 2001 Self-Assessment Examination For Residents (Sae-R) Multiple-Choice Questions Booklet Abridged VersionDocument23 pages2001 Self-Assessment Examination For Residents (Sae-R) Multiple-Choice Questions Booklet Abridged VersionSoumabho DasNo ratings yet
- Immunomodulators For AsthmaDocument7 pagesImmunomodulators For AsthmadarmariantoNo ratings yet
- About Integrated Management of Childhood IllnessDocument5 pagesAbout Integrated Management of Childhood IllnessRouena Santiago VillaramaNo ratings yet
- Denture Sequelae: Common Side Effects of Wearing Complete DenturesDocument58 pagesDenture Sequelae: Common Side Effects of Wearing Complete Denturesaayush100% (2)
- Beautiful Girls InsideDocument16 pagesBeautiful Girls InsideEnglishUrduDiaryNo ratings yet
- Soap ChartingDocument31 pagesSoap ChartingterefagcanganNo ratings yet
- Brochure XT-2000i and XT-1800i MKT-10-1136Document8 pagesBrochure XT-2000i and XT-1800i MKT-10-1136Cinthia Lizaraso VelapatiñoNo ratings yet
- Gap Co2 Cocc 2018Document9 pagesGap Co2 Cocc 2018Cesar Rivas CamposNo ratings yet
- Retinoblastoma Clinical and Pathological ClassificationDocument9 pagesRetinoblastoma Clinical and Pathological ClassificationSonia SaulésNo ratings yet
- Genetics Practice NCLEX Questions HandoutDocument6 pagesGenetics Practice NCLEX Questions HandoutAlvin L. Rozier100% (3)
- Occupation in Occupational Therapy PDFDocument26 pagesOccupation in Occupational Therapy PDFa_tobarNo ratings yet
- European PRM Board ExamDocument23 pagesEuropean PRM Board ExamAmer WasimNo ratings yet
- Pharmacy MCQSDocument132 pagesPharmacy MCQSomair zafar100% (6)
- Con 475306Document24 pagesCon 475306Jagdish ChanderNo ratings yet
- EdMatters Teachers PDFDocument39 pagesEdMatters Teachers PDFbala muruganNo ratings yet
- Coding For Anesthesia Services: Saving Faces Changing LivesDocument4 pagesCoding For Anesthesia Services: Saving Faces Changing LivesShell VenkatNo ratings yet
- 6.PIO TTG Seven Step Handling QueryDocument29 pages6.PIO TTG Seven Step Handling QueryNurinaAdaniSukiakusumahNo ratings yet
- Beat CancerDocument114 pagesBeat CancerGeorge Dragoi100% (8)
- CT Scanning - Techniques and Applications PDFDocument358 pagesCT Scanning - Techniques and Applications PDFMinionNo ratings yet
- BCS: An Account of the Biopharmaceutical Classification SystemDocument10 pagesBCS: An Account of the Biopharmaceutical Classification Systemruchit_darjiNo ratings yet
- Platelet Function TestsDocument31 pagesPlatelet Function TestsJino BugnaNo ratings yet
- Ocular Drug DeliveryDocument99 pagesOcular Drug DeliveryRishi ModyNo ratings yet
- NURSING CARE PLAN The Child Undergoing Surgery For ScoliosisDocument3 pagesNURSING CARE PLAN The Child Undergoing Surgery For ScoliosisscrewdriverNo ratings yet
- 6 - B.arun., Safety Positions For Healthy Sex Following Back PainDocument5 pages6 - B.arun., Safety Positions For Healthy Sex Following Back PainDr. Krishna N. SharmaNo ratings yet
- HeartsInHarmony PDFDocument103 pagesHeartsInHarmony PDFVanessa100% (9)
- 1 Social Administrative and Management Sciences Q&A Content Ver1Document34 pages1 Social Administrative and Management Sciences Q&A Content Ver1bhaveshnidhi64100% (1)
- PEWS Training IndonesiaDocument36 pagesPEWS Training IndonesiaBbenq Prasetyo100% (1)
- Antioxidant Micronutrient Impact On Hearing Disorders: Concept, Rationale, and EvidenceDocument7 pagesAntioxidant Micronutrient Impact On Hearing Disorders: Concept, Rationale, and EvidenceFongmeicha Elizabeth MargarethaNo ratings yet
- GABBARD - Term Psychodynamic Psychotherapy (Extrait) - 1Document6 pagesGABBARD - Term Psychodynamic Psychotherapy (Extrait) - 1Moëa NmtNo ratings yet
- QigongDocument12 pagesQigongCarlos EdreiraNo ratings yet