Professional Documents
Culture Documents
Qualityimprovementprocess
Uploaded by
api-241392518Original Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Qualityimprovementprocess
Uploaded by
api-241392518Copyright:
Available Formats
Running head: QUALITY IMPROVEMENT PROCESS
Quality Improvement Process
Jack Arnold, Megan Moore
Haley VanWormer and Shannon Vandenberg
Ferris State University
Abstract
When patients are hospitalized, there are many protocols followed to decrease risk of
complications. Protocols are initiated to encourage evidence-based practice and high quality of
care. Anytime a catheter is placed, the patient becomes at risk for a catheter acquired urinary
tract infection (CAUTI). This is why protocols need to be re-examined from time to time to
ensure they are still within the best scope of practice. The quality improvement process requires:
identifying the clinical need, a professional team, data collection, establishing outcomes,
implementation of strategies and an evaluation of the process.
Quality Improvement Process
In health care, quality improvement is an ongoing process which every discipline
undertakes. Patient satisfaction and safety are two major areas which drive the need for these
improvements. This paper will outline the steps undertaken during a quality improvement
process. The steps which will be covered are as follows: identify a clinical need, assembly of an
interdisciplinary team, design a data collection method, established outcomes, implementation
and lastly evaluation. Catheter acquired urinary tract infections (CAUTI) are the process which
will be evaluated to determine if current standards of practice are still applicable to current
evidence based research. Through this process, it can be assured the best possible outcomes for
the patient are considered.
Clinical Need
CAUTIs account for approximately 75% of urinary tract infections acquired in the
hospital (Centers for Disease Control and Prevention [CDC], 2015). Medicare and Medicaid
have created a list of hospital acquired infections instituting a non-payment policy for these
hospital acquired infections, CAUTIs are one of 8 such infections on the list (Peasah, McKay,
Harman, Al-Amin, & Cook, 2013). According to Peasah et al., (2013), a study was conducted
three years post implementation of the non-payment policy only to find the number of CAUTIs
had actually risen by 0.04% among admitted patients. While this may seem insignificant, it
represents an increase of over fourteen-thousand additional cases per year (CDC, 2015). Since
reduction in this number has not occurred overall, it is more crucial now than ever for hospitals
to ensure their policies regarding urinary catheter use are up-to-date. Depending on the size of
the hospital, non-payment could have a significant financial impact. The other consideration is
the impact to the patient. An infection means a longer hospital stay, antibiotics, and other
QUALITY IMPROVEMENT PROCESS
possible repercussions due to the infection. All of the above examples demonstrate a clinical
need for urinary catheter use to be examined.
Interdisciplinary Team
To ensure comprehensive care, for patients with CAUTIs, many professionals are
involved in treatment. An interdisciplinary team will be developed to address the reduction of
CAUTIs. It will include a physician, quality management professional, a nurse, pharmacist and
a nurse technician. The physician will act as the team leader coordinating care with the other
team members. His/her responsibilities will include diagnosis and observation of the patient
during treatment and ensure orders for a urinalysis and medications. The quality management
professional focuses on research related to decreasing CAUTIs; he/she would help educate
professionals on new initiatives and hospital protocols. The quality management team member
is then in charge of collecting data and changing practices based on the outcomes. The
pharmacist will be involved to supply the proper antibiotics, if a CAUTI were to occur while
following protocol, and clarify there are no allergies or medication interactions with current
medications. The nurse provides proper hygiene, education on urinary tract infections,
medication administration and monitoring for further infections or symptoms. The nurse is
responsible for use of the tool created on newly admitted patients. The nurse technician will
assist with personal care and bathing. Working as a team is vital for proper patient care; in this
situation, the team addresses a hospital acquired infection. This team collectively creates new
protocols to decrease risk for CAUTIs in hospitalized patients.
Data Collection Method
For data collection purposes the CDCs official definition of CAUTI will be used,
QUALITY IMPROVEMENT PROCESS
A urinary tract infection (UTI) where an indwelling urinary catheter was in place for
greater than two calendar days on the date of event, with day of device placement being
day one, and an indwelling urinary catheter was in place on the date of event or the day
before. If an indwelling urinary catheter was in place for greater than two calendar days
and then removed, the date of event for the UTI must be the day of discontinuation or the
next day for the UTI to be catheter-associated. ("CDC device-associated module," 2015,
p. 7-2)
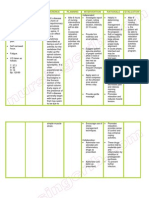
A chart was developed (see appendix A) to count the number of urinary tract infections
reported within the hospital which meet the defined criteria stated by the CDC. Any patient with
a urinary catheter will be included to monitor how the new protocol is affecting patient
outcomes. The chart will also include if catheter placement met the criteria stated in the policy,
how many days the catheter was in place and the patients medical record number for further
chart auditing. When a CAUTI is confirmed, the nurse assigned to the patient is to report the
laboratory results along with previously stated patient information to the nurse manager of the
unit, who will in turn report the information to the quality improvement team. From there, the
team will continue to analyze the effectiveness of the policy, as well as areas of improvement.
Establish Outcomes
After identifying a need for improvement in the CAUTI process, several goals were
recognized that reflect the evidence-based practice for the protocol. The primary outcome of this
quality improvement process is to reduce the incidence of CAUTIs hospital-wide by 50% within
6 months. This will be achieved through evidence-based education and awareness of the clinical
QUALITY IMPROVEMENT PROCESS
practice protocol change. To enhance the improvement, other goals were identified to
successfully implement and measure the expected outcome. The goals established included
increased education of the staff which will be measured through mandatory attendance
educational meetings. Secondly, achieve 100% compliance with the protocol. This will be
measured through auditing of charts of all patients with urinary catheters. Lastly, decreased
financial burden associated with CAUTIs which will be measured by reviewing of financial
reimbursement from Medicaid and Medicare and other insurance carriers. These goals are a
standard of care that improves the safety, efficiency, and effectiveness of quality patient care.
Implementation Strategies
In an effort to decrease the rates of CAUTIs within the healthcare facility a new policy
centered on CAUTI prevention will be implemented. This policy will begin with implantation in
the intensive care units, as they are among the highest rates of CAUTIs (Elpern, Killeen,
Ketchem, Wiley, Patel, & Lateef, 2009). The policy will include an easy to follow flow chart
(appendix B) to assist the staff in determining if an indwelling urinary catheter is appropriate for
a patient. The flowchart is based on current evidence based practice. According to the Centers
for Disease Control and Prevention (2009) the appropriate indications for use of an indwelling
urinary catheter are:
if the patient has acute urinary retention or bladder outlet obstruction, accurate urinary
output measurement in critically ill patients, perioperative use for selected surgical
procedures such as urologic surgery or organs of the urologic system, long surgeries,
patients who are to receive large amounts of fluids or diuretics during surgery, and a need
for intraoperative monitoring of urinary output, also to help with healing open wounds
such as sacral or perineal in incontinent patients, to help with comfort for the terminally
QUALITY IMPROVEMENT PROCESS
ill, and for patients requiring a long period of immobilization such as spine or pelvic
injury. (table 2)
The policy will also include a standard of work describing the role of nurses, nurse aids,
as well as the physicians when a patient has an indwelling catheter. Current practice states
proper catheter care should be done at a minimum of once a shift (twice daily), however, current
evidence based practice suggests this has no significant effect of bacteria introduction into the
urinary tract. The Center for Disease Prevention (2015) states: Unless clinical indications exist
(e.g., in patients with bacteremia upon catheter removal post urologic surgery), do not use
systemic antimicrobials routinely to prevent CAUTI in patients requiring either short or longterm catheterization. The CDC feels there is not enough evidence to support the use of
antibacterial cleansing of indwelling catheters, simple cleansing of the perineal and meatus is
sufficient. Due to this, a change in evidence based practice is in order. The work flow sheet will
not include routine catheter care. Rather, the policy will state the need to keep catheter clean and
free of obvious soiling and cleansing of the perineal area with every bath.
Along with implementation of the new policy, there will be frequent education
opportunities for nursing staff. Mandatory attendance of one of the educational meetings is
expected one week before the protocol's go-live date. Also included during education will be the
current CAUTI incident rates of the facility, the goal of the new policy, and who to contact with
any concerns or questions. Fliers will be distributed including information on alternatives to
placing indwelling urinary catheters, proper routine catheter care, and the nurses ability to use a
questioning attitude to determine whether an indwelling catheter is appropriate for a patient, and
when they should be removed. Once a week, an updated educational flier will be distributed
QUALITY IMPROVEMENT PROCESS
throughout the unit which consists of comparative statistics of the CAUTI incidence from the
previous week.
Evaluation
The evidence-based evaluation of the quality improvement process requires initial
assessments, monitoring, analyzing, and educating. There will be education and training
opportunities throughout the process to gain an insight on the initial protocol that will be
necessary to initiate the change. Monitoring the process reinforces the implementation because
compliance will determine the expected outcome. After the implementation of this new policy
the occurrences of CAUTIs in the facility will be evaluated weekly. The CAUTI prevention
committee will have meetings once a month to discuss how the policy has affected the nursing
staff as well as the patient population. The improved CAUTI protocol policy will be
implemented throughout the entire facility after six months of consistent positive feedback and
compliance of the protocol from nursing staff. Once the expected outcome of reduced CAUTIs
hospital-wide is established, the initiation of the protocol can be determine.
Conclusion
The purpose of the Quality Improvement process is to determine an area of care that can
be improved. An area in need of improvement is CAUTIs. Catheter acquired urinary tract
infection is one of the most common health care acquired infections (Nicolle, 2014, para. 2).
Once data is collected, goals and outcomes are created to help decrease risk. Strategies are then
created to meet the goals/outcomes; the overall process is then evaluated to determine the
effectiveness of the plan. The process will be further critiqued to ensure best quality of care for
patients.
QUALITY IMPROVEMENT PROCESS
8
References
Centers for Disease Control and Prevention. (2015). http://www.cdc.gov/
Elpern, E. H., Killeen, K., Ketchem, A., Wiley, A., Patel, G., & Lateef, O. (2009, November).
Reducing use of Indwelling Urinary Catheters and Associated Urinary Tract Infections.
American Journal of Critical Care, 18(6), 535-541.
http://dx.doi.org/10.4037/ajcc2009938
Guideline for Prevention of Catheter-associated Urinary Tract Infections, 2009. (2009).
Retrieved March 18, 2015, from
http://www.cdc.gov/hicpac/cauti/02_cauti2009_abbrev.html
Nicolle, L. E. (2014, July 25). Catheter associated urinary tract infections. Antimicrobial
Resistance & Infection Control, 3(23). http://dx.doi.org/10.1186/2047-2994-3-23
Peasah, S. K., McKay, N. L., Harman, J. S., Al-Amin, M., & Cook, R. L. (2013). Medicare NonPayment of Hospital-Aquired Infections: Infection Rates Three Years Post
Implementation. Medicare & Medicaid Research Review, 3(3). Retrieved from
https://www.cms.gov/mmrr/Downloads/MMRR2013_003_03_a08.pdf
Urinary tract infection (catheter-associated urinary tract infection [CAUTI] and non-catheterassociated urinary tract infection [UTI] and other urinary system infection [USI]) events.
(2015). Retrieved April 9, 2015, from
http://www.cdc.gov/nhsn/pdfs/pscManual/7pscCAUTIcurrent.pdf
QUALITY IMPROVEMENT PROCESS
MRN
placement
criteria met?
date of placement
Did patient develop
UTI
chart audited
# of days indwelling
1 2 3 4 5 6 7 8 9 10 1
1 2 3 4 5 6 7 8 9 10 1
1 2 3 4 5 6 7 8 9 10 1
1 2 3 4 5 6 7 8 9 10 1
1 2 3 4 5 6 7 8 9 10 1
1 2 3 4 5 6 7 8 9 10 1
1 2 3 4 5 6 7 8 9 10 1
1 2 3 4 5 6 7 8 9 10 1
1 2 3 4 5 6 7 8 9 10 1
Appendix A
QUALITY IMPROVEMENT PROCESS
10
Appendix B
Indwelling Urinary Catheter Protocol
Does the patients current condition meet any of the following approved reasons
for an indwelling urinary catheter?
-Hourly assessment of urinary output in critical care
-Hemodynamically unstable (not meeting vital sign parameters in the
last 4 hours and worsening condition requiring active titration,
excluding weaning, of vasoactive drugs in the last 4 hours)
-Select pre/postoperative procedures
-provider order for removal on post-op day 1 or 2 OR
-Urology, gynecology or colorectal surgery this admission
NO
Does the patients current condition meet any of the following approved
reasons for an indwelling urinary catheter?
-Acute renal failure/acute kidney injury
-Less than 0.5mL/kg/hr for greater than 6 hours OR
-Less than 24 hours of anuria (<0.3mL/kg/hour)
-Bladder outlet obstruction
-Improved comfort for end of life care
-Incontinence with open sacral/perineal wound
-for stage 3 or stage 4 pressure ulcers only
-Unstable spine or multiple traumatic injuries such as pelvic fracture
YES
Document indicated need
YES
NO
Does the patient have any of the following?
-Urology placement of catheter or urethral trauma
-Order of do NOT remove indwelling urinary catheter
-Chronic foley
NO
1) Discontinue the indwelling urinary catheter order per protocol
2) Discontinue and document removal of indwelling urinary catheter
Source: Spectrum Health Medical Group
YES
Document
indicated need
and discuss
possible
discontinuation
date with
provider
You might also like
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5795)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Salmon Dna: Introducing Scientific Breaktrough From JapanDocument6 pagesSalmon Dna: Introducing Scientific Breaktrough From JapanLeonardo100% (1)
- Nursing Care Plan Pott's DiseaseDocument2 pagesNursing Care Plan Pott's Diseasederic95% (21)
- Introduction of The Topic: Nano-BiotechnologyDocument7 pagesIntroduction of The Topic: Nano-BiotechnologyAbhishek YadavNo ratings yet
- Situs Inversus JClinSci - 2018 - 15 - 3 - 168 - 244747Document4 pagesSitus Inversus JClinSci - 2018 - 15 - 3 - 168 - 244747Anonymous 9QxPDpNo ratings yet
- Mental Health Class NotesDocument3 pagesMental Health Class Notessuz100% (4)
- Euthanasia ThesisDocument11 pagesEuthanasia ThesisAyush MathurNo ratings yet
- Mci Mbbs SyllabusDocument110 pagesMci Mbbs Syllabusmetabolicmedicine100% (1)
- Primary and Secondary AmenorrhoeaDocument72 pagesPrimary and Secondary Amenorrhoead clarkeNo ratings yet
- Neurologic Complications of Down Syndrome: A Systematic ReviewDocument15 pagesNeurologic Complications of Down Syndrome: A Systematic ReviewMáthé AdriennNo ratings yet
- Lecture 32 - Nutritional DisordersDocument43 pagesLecture 32 - Nutritional Disordersapi-3703352100% (3)
- Nursing Process Fon Chap 1Document20 pagesNursing Process Fon Chap 1Saqlain M.No ratings yet
- Bioassay For AntidiabetesDocument39 pagesBioassay For AntidiabetesNita TriadistiNo ratings yet
- Medical EnglishDocument133 pagesMedical EnglishKristina TomakNo ratings yet
- Guide For Writing NotesDocument10 pagesGuide For Writing Notesiamsera100% (1)
- IMNCIDocument13 pagesIMNCIJayalakshmiullasNo ratings yet
- From Outrage To Courage: The Unjust and Unhealthy Situation of Women in Poorer Countries and What They Are Doing About It PDFDocument97 pagesFrom Outrage To Courage: The Unjust and Unhealthy Situation of Women in Poorer Countries and What They Are Doing About It PDFNadine Avila100% (2)
- Ghidul de Prevenire A Miopiei - de Dr. Kaisu VIIKARI - Cu Coperta in RomanaDocument104 pagesGhidul de Prevenire A Miopiei - de Dr. Kaisu VIIKARI - Cu Coperta in Romanadlucian82No ratings yet
- Access To Primary Health Care Services For Indigenous PeopleDocument9 pagesAccess To Primary Health Care Services For Indigenous PeopleLawrence Ryan DaugNo ratings yet
- Psychogenic Nonepileptic Seizures - Management and Prognosis - UpToDateDocument18 pagesPsychogenic Nonepileptic Seizures - Management and Prognosis - UpToDateAndré MendonçaNo ratings yet
- FULL Download Ebook PDF Fundamentals of Human Neuropsychology 7th Edition PDF EbookDocument41 pagesFULL Download Ebook PDF Fundamentals of Human Neuropsychology 7th Edition PDF Ebookjennifer.lawver532100% (44)
- MMC 8Document27 pagesMMC 8Neil Patrick AngelesNo ratings yet
- Drug Related Problem (DRP)Document10 pagesDrug Related Problem (DRP)ERONADIAULFAH SUGITO50% (2)
- Hosa Happenings 2021 1Document8 pagesHosa Happenings 2021 1api-524471148No ratings yet
- Breast Cancer Staging SystemDocument4 pagesBreast Cancer Staging SystemGabriella PatriciaNo ratings yet
- AllRefer Health - PerichondritisDocument2 pagesAllRefer Health - PerichondritisandosaputraNo ratings yet
- Kode Penjelasan Keterangan: ObgynDocument14 pagesKode Penjelasan Keterangan: Obgynanon_507132438No ratings yet
- Endodontic Topics Volume 18 Issue 1 2008 (Doi 10.1111/j.1601-1546.2011.00260.x) YUAN-LING NG KISHOR GULABIVALA - Outcome of Non-Surgical Re-TreatmentDocument28 pagesEndodontic Topics Volume 18 Issue 1 2008 (Doi 10.1111/j.1601-1546.2011.00260.x) YUAN-LING NG KISHOR GULABIVALA - Outcome of Non-Surgical Re-TreatmentardeleanoanaNo ratings yet
- Zybio Company Profile 20211109CDocument46 pagesZybio Company Profile 20211109CĐức Hòa100% (1)
- Knee Dry NeedlingDocument24 pagesKnee Dry NeedlingJavi EgeaNo ratings yet
- Documents 34-51Document3 pagesDocuments 34-51api-575141270No ratings yet