Professional Documents
Culture Documents
Allnursesareleaders 04 27 2014
Uploaded by
api-238156787Original Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Allnursesareleaders 04 27 2014
Uploaded by
api-238156787Copyright:
Available Formats
Running head: ALL NURSES ARE LEADERS
All Nurses Are Leaders
Naomi Everett
Frostburg State University
ALL NURSES ARE LEADERS
2
All Nurses Are Leaders
What is leadership?
Leaders focus on people, whereas managers focus on systems and structure (Blais &
Hayes, 2011, p. 164). This basic description of leadership speaks to the first tenet of nursing
practice as described in the American Nurses Association (ANA) publication of Nursing: Scope
and Standards of Practice which is: Nursing practice is individualized (American Nursing
Association [ANA], 2010, p. 4). A skilled nurse leader has mastered the ability to communicate
and recognize the strengths and weaknesses of individual nurses and provide guidance based
upon that individuals needs. By focusing on the individual rather than tasks, a strong leader has
the ability to support each nurse to further her career and improve her practice. The Magnet
Recognition Program describes transformational leaders as a person who leads people where
they need to be in order to meet the demands of the future (ANA, 2010, p. 6). The nursing
profession needs strong leaders to promote nursing as a profession.
Nurses demonstrate leadership in many roles whether it is in the work setting, through
professional behaviors, or within the community (Blais & Hayes, 2011). On the job, nurses
serve as patient advocates. Within the profession, nurses serve as active members of nursing
associations to advance nursing as a profession. Nurses are valued within the community
because of their healthcare knowledge and they use their knowledge to promote healthcare
concepts in the community (Blais & Hayes, 2011). Simply put, leaders influence others.
Leaders derive their power from the ability to incite others to act. Attributes of the skilled leader
include: emphasis on interpersonal relationships, a focus on group process and communication,
and a talent for empowering others (Blais & Hayes, 2011). A nurse leader develops
relationships; whether it is with her patients, within an interdisciplinary care team, or within the
ALL NURSES ARE LEADERS
community. Within these relationships her credibility is transformed into power. Nursing
represents the largest sector of the health professionals, with more than 3 million registered
nurses in the United States (Institute of Medicine [IOM], 2011, p. xi); nursing has the potential
to wield great power.
Leadership Options
The nurses hold positions of leadership in all aspects of healthcare; from the bedside to
the boardroom (IOM, 2011, p. S-6). At the bedside a nurse leader influences patients through
education. Within a department a nurse influences her peers by modeling professional behavior
and mentoring new nurses. As a member of the interdisciplinary team a nurse acts as a full
partner with physicians and other health professionals, and must be accountable for their own
contributions to delivering high-quality care while working collaboratively with leaders from
other health professions (IOM, 2011, p. S-6). The unique role of the Clinical Nurse Specialist
(CNS) allows for direct influence on patients, empowerment of other nurses, and allows them to
use their influence to shape policy within organizations. Community nurses have even greater
influence as the community nurse practices in a wide variety of settings and reaches a wide range
of age groups; community nursing is population focused (Blais & Hayes, 2011).
Nurses not engaged in direct patient care focus their leadership skills on influencing
nursing as a profession rather than focusing on individuals. Mason defines politics as
influencing specifically, influencing the allocation of scarce resources (as cited in Blais &
Hayes, 2011, p. 204). The nurse as political advocate influences policy on the community level,
in the workplace, within professional organizations, and within government (Blais & Hayes,
2011). Effective nurse managers communicate well and influence policy on a unit level, a
facility level and every level in between. The nursing professor plays a vital role in grooming
ALL NURSES ARE LEADERS
the nurse leaders of tomorrow as the ANA standard of leadership is one of the standards of
professional nursing practice that all nursing students study (ANA, 2010). One could say that
the nursing professor is the first line of defense in promoting nursing professionalism and
training the nurse leaders of the future.
Pros and Cons of Leadership Development for Nurses
Although the public is not used to viewing nurses as leaders, and not all nurses begin
their career with thoughts of becoming a leader, all nurses must be leaders in the design,
implementation, and evaluation of, as well as advocacy for, the ongoing reforms to the
system that will be needed (Scott & Miles, 2013, para. 3).
Scott and Miles (2013) describe two central issues regarding leadership training for nurses. The
first is that the majority of leadership in nursing literature available today has been devoted to
leader training rather than leadership development. Nurses must come to recognize that leaders
are needed in all aspects of nursing and nurse educators must alter nursing curricula to include
leadership as a dimension of practice for all nurses, not just nurses pursuing formal leadership
roles (Scott & Miles, 2013). The second issue is the need to define the leadership skills that are
essential for nurses and developing a framework for leadership development that spans from the
novice nurse to the advanced practice nurse (Scott & Miles, 2013). While the Leadership
Institute of the ANA, the nations largest professional organization for nurses, states that nurse
leaders are needed in all aspects of healthcare: at the bedside, within healthcare facilities,
community nursing, professional associations, or the halls of Congress; they offer few programs
that focus on leadership development rather than leader training ("ANA Leadership," n.d.).
While formal leadership development in sorely lacking in nursing education, nurses
demonstrate leadership when they practice with integrity. Credibility has been called the
ALL NURSES ARE LEADERS
foundation of leadership ("Every Nurse," 2010, para. 4). Nurses establish credibility when they
take responsibility for mistakes, identify personal values and communicate them through action
and are knowledgeable in their field of practice ("Every Nurse," 2010). Although not formally
labeled as leadership development, nurses are schooled in basic leadership skills. All nurse
education curricula include: patient assessment and being proactive in selecting and acting on
nursing interventions, taking the time to research conditions or medications that the nurse may
not be familiar with in order to provide quality care to the patient, speaking up when an order
does not seem right, and patient advocacy ("Every Nurse," 2010). The challenge is for all nurses
to recognize themselves as leaders, not just nurses on a leadership track.
Nurse Leadership in Society
Nursing leadership takes on an important role in society. Nurses are role models for
healthy behaviors, community health promoters and viewed as a source of health information.
The idea that nurses should promote wellness in the community is not a new one. Florence
Nightingale believed that nurses should work to prevent disease and care for well patients with
the same approach as caring for sick patients (Strout, 2012, para. 10). She encouraged nurses
to empower society to improve environments outside hospitals such as schools, homes, and
communities in order to prevent disease (Strout, 2012, para. 10).
Societal focus has shifted from disease care to healthcare and wellness; this is an
opportunity for nursing to influence community health in new ways. Nurses are uniquely
positioned to lead society on its path to wellness because nursing has also experienced a shift in
focus that has expanded the tenets of health care to an increased focus on educating clients in
health promotion and health protection (Blais & Hayes, 2011, p. 363). Wellness coaching is a
relatively new career in nursing that specifically addresses the promotion of a healthy society.
ALL NURSES ARE LEADERS
Wellness coaches work one-on-one with clients either via independent practice or via partnership
with fitness facilities. While some wellness coaches focus on disease prevention, others choose
to focus on managing chronic illness such as diabetes or heart disease.
Promotion of Nurse Leadership
The American Nurses Credentialing Centers Magnet Recognition Program (Magnet) has
been the single most important innovation in promoting leadership in nursing. Magnet
recognizes health care organizations for quality patient care, nursing excellence and innovations
in professional practice ("Magnet Overview," n.d., para. 1). The first of five model components
is transformational leadership; a transformational leader leads nurses where they need to go to
meet the demands of the future ("Magnet Model," 2008, para. 6). The second component of the
Magnet model is structural empowerment in which nurses are empowered to find the best way
to accomplish the organizational goals and achieve desired outcomes ("Magnet Model," 2008,
para. 9). The third component of the Magnet model speaks to nurse autonomy and nurses as
teachers and leaders; this is the component of exemplary professional practice ("Magnet Model,"
2008, para. 12).
Shared governance is part of the core of Magnet status; even though the American Nurses
Credentialing Center (ANCC) avoids using the term (Porter-OGrady, 2004). The shared
governance model encourages nurses to demonstrate accountability and ownership of their
practice though participation in nursing councils. These nursing councils, whether it is unit
based or facility wide, give nurses a voice in creating standards of practice for their facility.
Active participation in the shared governance model promotes leadership skills by encouraging
nurses to take ownership of their practice (Ward, 2012).
Intradisciplinary and Interdisciplinary Issues in Nurse Leadership
ALL NURSES ARE LEADERS
In the intradisciplinary role the nurse leader models behaviors that demonstrate
proficiency in the competencies outlined in the ANA nursing standards of practice, including:
demonstrates commitment to lifelong learning, mentors colleagues, treats colleagues with
respect, participates in professional organizations, and seek ways to advance autonomy and
accountability (ANA, 2010). The most important task of the intradisciplinary nurse leader is to
lead by example in everyday practice; providing quality, proactive care. This straightforward
approach to leadership builds credibility which we know is the foundation of leadership (Every
Nurse," 2010, para. 4). Also of importance is that the intradisciplinary nurse leader supports her
peers by clearly communicating the standards of practice and promoting autonomy.
In the contemporary healthcare environment, nurses, physicians, patients, and other
health professionals are increasingly interdependent (IOM, 2011, para. 9). As part of an
interdisciplinary team, a nurse leader represents all of nursing. For an interdisciplinary nurse
leader, effective communication skills play a crucial role in her ability to collaborate with the
care team. As the nurse spends more time at the bedside than any other discipline, nurse input
has great influence to achieve positive outcomes for the patient. Effectively communicating
between the nurse and both the patient and the care team is yet another competency of the ANA
standard of leadership (ANA, 2010). Communication is a two-way street; in its simplest form,
communication involves the sending and receiving of messages between two people (Blais &
Hayes, 2011, p. 235). An effective nurse leader communicates with patients to assess their needs
and acts as a patient advocate when interacting with the interdisciplinary care team.
Leadership and Its Effect on the Nursing Profession
The changing role of nursing is both a challenge and an opportunity. Nurses currently
form the largest sector of health care providers, with more than three million currently registered;
ALL NURSES ARE LEADERS
but few have led or even been involved in the formal policy discussions regarding the future care
of patients (Chen, 2010, para. 9). Because of our sheer numbers, nurses hold great influence
but we must devise a cohesive message. This is why membership and active participation in a
professional organization, such as the ANA, is so important. The ANA works diligently to
coordinate the nursing message so we are heard as one voice, loud and clear. Nurses are their
own best advocate, but as Porter-OGrady (2011) notes:
There's no doubt that it's up to the profession and its leaders to demonstrate the political
and professional maturity to negotiate the complex landscape of interdisciplinary
collaboration; resolution of disparate advocacy positions; positioning of nurses on key
organizational, legislative, and policy boards; and asserting nursing's legitimate role in
decisions and actions, which advance effective quality healthcare (para. 23).
Nursing must be proactive and trigger change rather than reacting to it. It is the opinion
of the Institute of Medicine (IOM) that nursing is positioned to have a significant impact on the
healthcare system (Porter-OGrady, 2011, para. 23). Our nurse leaders will determine the
extent of that impact [which] is entirely dependent on the willingness of the profession to
develop the role capacities and leadership essential to make a difference in ensuring quality,
accessible healthcare in a reformed and transforming health system (Porter-OGrady, 2011,
para. 23). Through strong leadership nursing has the potential to have a great impact on
healthcare. Is nursing living up to its potential?
For nurse leaders to have an impact upon nursing as a profession, nurses must educate
themselves on health policy. Since nursing education curricula generally treat health policy as
extra rather than core, the naivet of graduates, is no surprise. With few exceptions, nurses
generally view themselves as being shaped by, not shaping, policy (IOM, 2011, p. I-73). The
ALL NURSES ARE LEADERS
IOM also states that Since nurses largely take a back seat to policy processes, the professions
input has been relatively invisible (IOM, 2011, p. I-73) and that our silence is surely an
outgrowth of the inattention of nursing curricula to health policy (IOM, 2011, p. I-73). How
has leadership effected the nursing profession? Not as much as could be.
Is Nursing a profession yet?
What is a profession? A profession is an occupation whose core element is work based
upon the mastery of a complex body of knowledge and skills (Cruess, Johnston, & Cruess,
2004, para. 2). If considering this very limited definition of what a profession is then yes,
nursing is a profession. A profession is also governed by codes of ethics and profess a
commitment to competence, integrity and morality, altruism, and the promotion of the public
good within their domain (Cruess, et al., 2004, para. 2). Nursing also meets these requirements
of a profession. The waters become murky regarding Cruess et al.s (2004) the next criteria of a
profession:
These commitments form the basis of a social contract between a profession and society,
which in return grants the profession a monopoly over the use of its knowledge base, the
right to considerable autonomy in practice and the privilege of self-regulation (para. 2).
Nursing holds a social contract with the community it serves; meaning that nursing has an
unwritten agreement to work for the benefit of society. Nursing also holds a monopoly over its
knowledge base; meaning that nursing has a unique perspective and is attempting to
communicate this perspective through standardized nursing terminology. As of 2010 the ANA
has recognized seven active nursing terminologies that are used to describe nursing diagnoses,
nursing interventions, and nursing outcomes (McGonigle & Mastrian, 2012). McGonigle and
Mastrian warn that Without consistent terminology, nursing runs the risk of becoming invisible;
ALL NURSES ARE LEADERS
10
it will remain difficult to quantify nursing, the unique contribution and the impact of nursing will
go unrecognized (McGonigle & Mastrian, 2012, p. 111). This statement is true; nursing does
designate nursing diagnoses, formulate nursing interventions, and measure nursing outcomes
utilizing nursing terminologies. Nursing diagnoses were created and intended to be used to
describe the knowledge and practice of nursing (Herdman, 2011). Unfortunately, nursing
diagnoses as currently used and taught are treated as simply documentation tools as nursing
education fails to teach them as concepts (Herdman, 2011). Herdman would revamp nurses
curriculum to one designed around the core concepts of nursing knowledge; teaching modules
based upon nursing diagnoses such as: pain, decreased cardiac output, and acute confusion
(Herdman, 2011).
In practice, nurses implement the orders of medicine first, we act the eyes of medicine as
we report what we see and request medical interventions. By no means do nurses simply follow
medical orders, but currently nursing views patients from a medical point of view; concentrating
on and clustering care around a medical diagnosis. This forces us to address the statement from
Cruess, et al. (2004): Does nursing possess the right to considerable autonomy in practice and
the privilege of self-regulation (para. 2)? Can nursing call itself an autonomous profession
while implementing orders of another profession, namely medicine? Professional autonomy
means having the authority to make decisions and the freedom to act in accordance with one's
professional knowledge base (Skar, 2010, para. 1). Yes, the ANA standards of practice include
the implementation competency of collaboration with healthcare providers to put into action a
plan of care (ANA, 2010). Nursing care is differentiated from medical care in that the care that
nurses provide is above and beyond medical orders; nursing interventions make the difference
between good healthcare and exceptional healthcare. Presently, the whole of nursing does not
ALL NURSES ARE LEADERS
11
work as autonomous entities; even as a nurse advances her education most states still require
some level of physician collaboration for nurse practitioners (Maryland Board of Nursing
[MBON], 2011).
Is nursing a profession yet? Nursing is caught in limbo; the pendulum swings ever closer
to profession. The challenge is to embrace our role as professional nurses and nurse leaders and
better define the concepts of our own practice; both for ourselves as nurses and for the
community. These concepts should be well researched, well developed, and internationally
disseminated (Herdman, 2011, para. 7) so that the unified voice of professional nursing is heard
loud and clear.
ALL NURSES ARE LEADERS
12
References
ANA leadership institute. (n.d.). Retrieved from http://www.ana-leadershipinstitute.org/
American Nursing Association. (2010). Nursing: Scope and standards of practice (2nd ed.).
Silver Spring, MD: American Nurses Association.
Announcing a new model for ANCCs magnet recognition program. (2008). Retrieved from
http://www.nursecredentialing.org/MagnetModel
Blais, K. K., & Hayes, J. S. (2011). Professional nursing practice: Concepts and perspectives
(3rd ed.). Upper Saddle River, NJ: Pearson Health Science.
Chen, P. W. (2010, November 18). Nurses role in the future of health care. The New York
Times. Retrieved from
http://www.nytimes.com/2010/11/18/health/views/18chen.html?_r=0
Cruess, S. R., Johnston, S., & Cruess, R. L. (2004). Profession: A working definition for
medical educators. Teach Learn Med, 16(1), 74-76. Abstract retrieved from PubMed.
Every nurse can be a leader. (2010). Retrieved from
http://www.americansentinel.edu/blog/2010/11/30/every-nurse-can-be-a-leader/
Herdman, T. H. (2011). What nursing knowledge is needed to develop nursing practice?
[Editorial]. Revista Electronica de Enfermagen, 13(2), 159-160. Retrieved from
http://www.fen.ufg.br/revista/v13/n2/v13n2a01-en.htm
Institute of Medicine. (2011). The future of nursing: Leading change, advancing health.
Retrieved from The Future of Nursing website:
http://thefutureofnursing.org/sites/default/files/Future%20of%20Nursing%20Report_0.pd
f
ALL NURSES ARE LEADERS
13
Magnet recognition program overview. (n.d.). Retrieved , from
http://www.nursecredentialing.org/magnet/programoverview
Maryland Board of Nursing. (2011). Instructions for completing and submitting the nurse
practitioner (NP) attestation frorm & supporting documents . Retrieved from
http://www.mbon.org/adv_prac/attestation_instructions.pdf
McGonigle, D., & Mastrian, K. G. (2012). Nursing informatics and the foundation of knowledge
(2nd ed.). Burlington, MA: Jones & Bartlett Learning.
Porter-OGrady, T. (2004, January 31). Overview: Shared governance: Is it a model for nurses to
gain control over their practice? The Online Journal of Issues in Nursing, 9-2004(1).
Retrieved from
http://www.nursingworld.org/MainMenuCategories/ANAMarketplace/ANAPeriodicals/
OJIN/TableofContents/Volume92004/No1Jan04/Overview.html
Porter-OGrady, T. (2011, May). Future of nursing special: Leadership at all levels. Nursing
Management, 42(1), 32-37. Retrieved from
http://www.nursingcenter.com/lnc/journalarticleprint?Article_ID=1163290
Scott, E. C., & Miles, J. (2013). Advancing leadership capacity in nursing. Nursing
Administration Quarterly, 37(1), 77-82. Retrieved from
http://www.nursingcenter.com/lnc/journalarticleprint?Article_ID=1479260
Skar, R. (2010). The meaning of autonomy in nursing practice. Journal of Clinical Nursing,
19(15-16), 2226-2234. Abstract retrieved from PubMed. (Accession No. PMID:
19538554)
ALL NURSES ARE LEADERS
Strout, K. (2012). Wellness promotion and the institute of medicines future of nursing report:
Are nurses ready? Holistic Nursing Practice, 26(3), 129-136. Retrieved from
http://www.nursingcenter.com/lnc/journalarticleprint?Article_ID=1333059
Ward, J. (2012). Shared governance: What exactly is it? Retrieved from
http://www.nursetogether.com/shared-governance-what-exactly-is-it-
14
You might also like
- CommunityhealthassessmentsurveythurmontmarylandDocument40 pagesCommunityhealthassessmentsurveythurmontmarylandapi-238156787No ratings yet
- Running Head: Completed Service Learning Project 1Document6 pagesRunning Head: Completed Service Learning Project 1api-238156787No ratings yet
- Running Head: Service Learning Project Plan 1Document12 pagesRunning Head: Service Learning Project Plan 1api-238156787No ratings yet
- EfolioessentialviiDocument4 pagesEfolioessentialviiapi-238156787No ratings yet
- ExecutivesummaryDocument3 pagesExecutivesummaryapi-238156787No ratings yet
- Efolioessential II 07 16 2015Document4 pagesEfolioessential II 07 16 2015api-238156787No ratings yet
- EfficacyoffoamdressingsinthepreventionofhospitalaquiredpressureulcerscomparedtohydrocolloiddressingsDocument21 pagesEfficacyoffoamdressingsinthepreventionofhospitalaquiredpressureulcerscomparedtohydrocolloiddressingsapi-238156787No ratings yet
- Running Head: A Discussion On Assisted Suicide 1Document10 pagesRunning Head: A Discussion On Assisted Suicide 1api-238156787No ratings yet
- Nurs 496 Resume EverettDocument2 pagesNurs 496 Resume Everettapi-238156787No ratings yet
- Efolioessential III 07 16 2015Document4 pagesEfolioessential III 07 16 2015api-238156787No ratings yet
- 2015 07 Letter of Recommendation WelikDocument1 page2015 07 Letter of Recommendation Welikapi-238156787No ratings yet
- Mutz 07 29 2009Document1 pageMutz 07 29 2009api-238156787No ratings yet
- Chronic Kidney Disease Group Paper 04 2013Document15 pagesChronic Kidney Disease Group Paper 04 2013api-238156787No ratings yet
- StatementofprofessionalgoalsDocument5 pagesStatementofprofessionalgoalsapi-238156787No ratings yet
- Fisch 10 25 2005Document1 pageFisch 10 25 2005api-238156787No ratings yet
- Efolio Essential Ix 07 2015Document4 pagesEfolio Essential Ix 07 2015api-238156787No ratings yet
- EfolioessentialviiiDocument4 pagesEfolioessentialviiiapi-238156787No ratings yet
- Efolio Essential VDocument4 pagesEfolio Essential Vapi-238156787No ratings yet
- Frey 12 29 1992Document1 pageFrey 12 29 1992api-238156787No ratings yet
- EfolioessentialivDocument4 pagesEfolioessentialivapi-238156787No ratings yet
- Menker 01 21 2010Document1 pageMenker 01 21 2010api-238156787No ratings yet
- Canilla 10 20 2005Document1 pageCanilla 10 20 2005api-238156787No ratings yet
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Edcn 103 Micro StudyDocument17 pagesEdcn 103 Micro StudyYlesar Rood BebitNo ratings yet
- All University Programs and Ways of Applying For Courses of 2011-2012Document172 pagesAll University Programs and Ways of Applying For Courses of 2011-2012Cleverence Kombe100% (1)
- Table of ContentsDocument9 pagesTable of Contents099153432843No ratings yet
- (DOC) UNIQUE - Gina Cruz - Academia - EduDocument18 pages(DOC) UNIQUE - Gina Cruz - Academia - EduAbelardo Ramos DiasNo ratings yet
- Teaching Methods in Practical Lab: 1.4 Theoretical/Conceptual FrameworkDocument5 pagesTeaching Methods in Practical Lab: 1.4 Theoretical/Conceptual FrameworkselowestNo ratings yet
- QF EheaDocument200 pagesQF Eheajose_dias_58No ratings yet
- Psumt Newsletter FallDocument3 pagesPsumt Newsletter Fallapi-251592269No ratings yet
- Agnes GreyDocument165 pagesAgnes GreyLaura Elena ApetroaieNo ratings yet
- Intertrial Interval On Motor Skill PerformanceDocument7 pagesIntertrial Interval On Motor Skill PerformanceBenÜt BalleraNo ratings yet
- Science Lesson Plan Uv BeadsDocument4 pagesScience Lesson Plan Uv Beadsapi-259165264No ratings yet
- ACCT 245.004 - Business Law Spring Semester 2020Document11 pagesACCT 245.004 - Business Law Spring Semester 2020Ali Abbas LakhaniNo ratings yet
- BSC Sem Iv Regular PDFDocument100 pagesBSC Sem Iv Regular PDFJitendra VishwakarmaNo ratings yet
- Appln Aeo&deoDocument11 pagesAppln Aeo&deomanusurya68No ratings yet
- Environmental Planners Board ExamDocument7 pagesEnvironmental Planners Board ExamAngelu Via Claridades64% (11)
- In Re LanuevoDocument23 pagesIn Re LanuevoJoJONo ratings yet
- Latest LLB StructureDocument7 pagesLatest LLB StructureMary MichaelNo ratings yet
- Rhodes Sgholar$Hips: India I 201 ODocument5 pagesRhodes Sgholar$Hips: India I 201 OayuloNo ratings yet
- Law AtractionDocument29 pagesLaw AtractionCássia MoratoNo ratings yet
- Department of Education: San Jose Provincial High SchoolDocument3 pagesDepartment of Education: San Jose Provincial High SchoolStephanie100% (1)
- ACI FormDocument1 pageACI FormToyosi OlugbenleNo ratings yet
- CHSL Exam PaperDocument27 pagesCHSL Exam PaperArpit KumarNo ratings yet
- Passed 5104 13 21MELCS Baguio Roles of Theater EdtDocument89 pagesPassed 5104 13 21MELCS Baguio Roles of Theater EdtChristopher David OlivaNo ratings yet
- Calculus Modules - Scope and SequenceDocument13 pagesCalculus Modules - Scope and SequenceKhushali Gala NarechaniaNo ratings yet
- Camp Mateo Capinpin Elementary SchoolDocument6 pagesCamp Mateo Capinpin Elementary SchoolLorriline April Rivera SantillanNo ratings yet
- Accomplishment Report IN W.A.T.C.H (We Advocate Time Consciousness and Honesty) For The Month of AugustDocument4 pagesAccomplishment Report IN W.A.T.C.H (We Advocate Time Consciousness and Honesty) For The Month of AugustHarvey Cabrera50% (2)
- Bredendieck Hin - The Legacy of The BauhausDocument7 pagesBredendieck Hin - The Legacy of The BauhausMarshall BergNo ratings yet
- Unit Plan Lesson 1 - VocabDocument4 pagesUnit Plan Lesson 1 - VocabLeeann RandallNo ratings yet
- BehaviourismDocument30 pagesBehaviourismAsma Riaz0% (1)
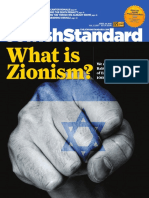
- Jewish Standard Newspaper 4/29/16Document56 pagesJewish Standard Newspaper 4/29/16New Jersey Jewish StandardNo ratings yet
- Fes-School Action Plan Sy2019-2020 Updated01Document21 pagesFes-School Action Plan Sy2019-2020 Updated01api-250691083No ratings yet