Professional Documents
Culture Documents
An Integrative Review
Uploaded by
api-293060983Original Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
An Integrative Review
Uploaded by
api-293060983Copyright:
Available Formats
Running head: AN INTEGRATIVE REVIEW: LOCAL INFILTRATION ANALGESIA
An Integrative Review: Local Infiltration Analgesia
Loyce Anne Caldwell
Bon Secours Memorial College of Nursing
I have neither given nor received aid, other than acknowledged, on this assignment or test, nor
have I seen anyone else do so. Anne Caldwell
AN INTEGRATIVE REVIEW: LOCAL INFILTRATION ANALGESIA
2
Abstract
The goal of this integrative review is to evaluate the literature regarding the effectiveness
of pain control using local infiltration analgesia (LIA) following total knee arthroplasty (TKA).
TKA is a surgical procedure commonly used to treat damaged or disease knee joint.
Postoperative pain is usually severe and is frequently treated with intravenous morphine. The
research design is an integrative review. The search for literature was conducted using the
computer-based search engines PubMed, Ovid, EBSCO, and Science Direct. The search
produced 25 articles, of which five met the inclusion criteria. An analysis of the results and
findings of the five articles revealed LIA is effective in controlling postoperative pain for TKA
patients. Limitations to the review included the researchers lack of experience and knowledge,
time to complete the assignment, and limits on the number of articles used for the review. Future
research should focus on a reduction in length of stay in the hospital, cost reductions, and
different drugs and doses of LIA.
AN INTEGRATIVE REVIEW: LOCAL INFILTRATION ANALGESIA
3
An Integrative Review: Local Infiltration Analgesia
The purpose of this integrative review is to search for literature regarding the use of LIA
and its effects on pain control in patients following TKA. Patients that have undergone TKA
typically have severe pain after surgery, which can interfere with ambulation and the recovery
process (Xu, Li, Wang, Song, & Yu, 2014). For this reason, an essential part of the postoperative
recovery process is aggressive pain control methods, such as nerve blocks, epidurals, and
intravenous (IV) narcotics. Unfortunately, all of these pain control options have the potential for
numerous and sometimes severe side effects. Narcotics, such as morphine, are associated with
nausea, vomiting, decreased gastrointestinal motility, urinary retention, and respiratory
depression. Recently, in 2008, doctors Kerr and Kohan developed the LIA technique (Essving, et
al., 2010). LIA contains a long-acting local anesthetic, ropivacaine, a nonsteroidal antiinflammatory, ketorolac, and epinephrine, and is injected directly into the joint. This new
technique is of interest because of the potential it has to reduce pain and other postoperative
complications, and improve postoperative recovery in patients undergoing TKA. Therefore, the
proposed PICO question by this researcher is: In adult patients, undergoing a total knee
replacement how effective is local infiltration analgesia compared to IV morphine in controlling
postoperative pain during the first 48 hours.
Research Design, Search Methods, & Search Outcomes
The research design is an integrative review. A computerized search for research articles
was conducted using PubMed, Ovid, EBSCO, and Science Direct databases. The search terms
included were knee replacement, knee arthroplasty, TKA, TKR, pain, local infiltration
analgesia, periarticular injections, morphine, and patient controlled analgesia or PCA. The
search produced 25 articles, 12 articles from PubMed, 7 articles from EBSCO, 4 articles from
AN INTEGRATIVE REVIEW: LOCAL INFILTRATION ANALGESIA
4
Ovid, and 2 articles from Science Direct. The search was limited to peer-reviewed articles,
published in English, and written between 2010 and 2015. The articles were required to relate to
the researchs PICO question In adult patients undergoing total knee replacements how effective
is local infiltration analgesia compared to IV analgesics in controlling postoperative pain during
the first 48 hours? The inclusion criteria for articles included in this integrative review were:
adults receiving TKA use of LIA, morphine, and effects on pain control. All articles were
assessed based on the inclusion criteria and their significance to the proposed PICO question;
articles that did not meet the set criteria were exclude from the review. This assessment produced
five articles regarding LIA use in TKA patients, which includes three random control trails
(RCTs), a meta-analysis and a combination meta-analysis and systematic review.
Findings/Results
The findings and results of all five reviewed articles indicate that the use of LIA in
patients undergoing TKA is an effective method in reducing postoperative pain and consumption
of narcotics (Essving, et al., 2010; Essving, et al., 2011; Marques, et al., 2014; Niemelainen,
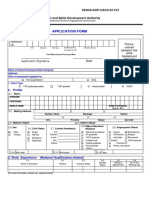
Kalliovalkama, Aho, Moilanen, & Eskelinen, 2014; Xu, Li, Wang, Song, & Yu, 2014). Table 1
provides an outline of the main characteristics of the five articles. The researcher framed the
review according to the following themes: postoperative pain relief, morphine consumption, and
mobility.
Postoperative Pain Relief
All five articles examined pain after a TKA in patients that had received LIA compared to
control groups (Essving, et al., 2010; Essving, et al., 2011; Niemelainen, et al, 2014; Xu, Li, et
al., 2014; Marques, et al., 2014). In a RCT, LIA injection was given to group A and saline
injections were given to group P prior to would closure and again 22 hours after surgery
AN INTEGRATIVE REVIEW: LOCAL INFILTRATION ANALGESIA
5
(Essving, et al., 2010). Using a visual analog scale (VAS) for pain, where 0 is no pain and 100 is
worst pain possible, the recorded median pain at rest and on flexion of the knee by 60 degrees for
the LIA group was statistically significantly lower. The researchers used nonprobability sampling
of 48 TKA patients, VAS data was collected using verbal reports at 3, 6, 12, ,21,22, 27, & 48
hours postoperative and analyzed using the Mann-Whitney U test. The statistical significant
lower VAS scores contributes to the body of literature by providing strong evidence that LIA is
an effective pain control method following TKA.
A RCT by Essving, et al. (2011) studied LIA in comparison with morphine spinal
anesthesia. In a nonprobability sampling of 50 patients undergoing TKA, VAS data, again 0
being no pain and 100 being the worst pain possible, was collected at 6, 12, 22, 24,35 and 46
hours postoperative and analyzed using the Mann-Whitney U test, Bonferroni-Holm method, x2,
or Fishers exact test, when appropriate. LIA injections were administered to group L prior to
wound closure. Then, on postop day 1 and 2, LIA was given to group L, while saline was given
to group M via intraarticular catheter. The results were a lower median VAS at rest for the LIA
group, 5 versus 20 for the morphine group, and with flexion, 30 for the LIA group versus 59 for
the morphine group. This study contributes to the body of literature by supporting the evidence
that LIA is an effective pain control method following TKA.
A RCT by Niemelainen, et al. (2014) concerning single LIA injection and its effects on
reducing opiate consumption 48 hours after TKA, VAS scores were used to evaluate pain. In a
nonprobability sample, 56 TKA patients were randomly assigned LIA or placebo by a researcher
not involved in patient care, by drawing a sealed envelope from a collection of 60 envelopes.
Postoperative pain at rest was recorded by the nurse or physiotherapist using VAS scores, where
0 was no pain and 10 was the worst pain possible. The VAS data was collected at 0, 3, 9, 18, and
AN INTEGRATIVE REVIEW: LOCAL INFILTRATION ANALGESIA
6
8 hours after surgery and analyzed using a Mann-Whitney U-test. The VAS scores were all lower
in the LIA group, but there was no statistical significance. This study contributes to the body of
literature by supporting that LIA does provide effective pain control following a TKA.
A meta-analysis of 18 RCTs, regarding the efficacy and safety of single-dose LIA in TKA
patients, studied the reported VAS values (Xu, et al., 2014). The studies were selected based on
TKA patients, use of single-dose LIA, comparison intervention of either placebo or nothing, and
had outcome measure for VAS, postoperative morphine consumption, recorded length of stay,
functional recovery, and side effects. Data was analyzed using the DerSimonian and Laird
random effects model results were confirmed using a sensitivity analysis. Sixteen of the studies
recorded VAS values and each reported pain was significantly lower in the first 48 hours after
surgery in the LIA group than in the control group. This study contributes to the body of
literature by farther supporting the finding of individual studies in which LIA is effective for pain
control in TKA patients.
A systematic review and meta-analysis of 23 studies, with a total of 1439 patients,
regarding short and long-term effectiveness of LIA for pain control in TKA, lower pain scores
were reported in patients receiving LIA (Marques, et al., 2014). Studies were selected based on
RCTs using the Cochrane Collaboration's tool for assessing risk of bias and was conducted in
accordance with preferred reporting items for systematic reviews and meta-analyses (PRISMA)
guidelines. Data was collected regarding study characteristics, participant characteristics,
anesthesia procedures, content, and volume of LIA, additional interventions, and control group
treatments of placebo or alternative analgesia. The data was analyzed using Stata 12 and Review
Manager 5. In patients that received LIA, pain was reduced by an average of 10 points at rest and
AN INTEGRATIVE REVIEW: LOCAL INFILTRATION ANALGESIA
7
points during activity. This study contributes to the body of literature by providing evidence from
multiple studies that reviewed the effectiveness of LIA for pain control after TKA.
Morphine Consumption
Three of the five research studies assessed the effectiveness of LIA in reducing morphine
consumption (Essving, et al., 2010; Essving, et al., 2011; Xu, et al., 2014). In a study done by
Essving, et al. (2010) PCA morphine was given to both the placebo group and the LIA group,
and consumption was recorded for 0 to 24 hours, 24 to 48 hours, and 0 to 48 hours. Tramadol
consumption was also recorded at the same times and converted to equivalent morphine dose
using the ratio of 100 mg tramadol to 10 mg of morphine. The results illustrate that morphine
and tramadol consumption was lower in the LIA group during the first 48 hours after TKA, 54
mg in the LIA group versus 109 mg in the placebo group. This study contributes to the body of
literature by providing evidence that LIA reduces use of morphine used for pain control after
TKA.
In a RCT that studied the use of LIA for postoperative pain management following a
TKA compared to intrathecal morphine, the primary endpoint was to review PCA morphine
consumption (Essving, et al., 2011). Group L was given spinal anesthesia with bupivacaine and
saline, plus the LIA injection, and group M was given spinal anesthesia with bupivacaine and
morphine, and no injection. Both groups were given PCA morphine and consumption was
recorded during 0 to 24 hours, 24 to 48 hours, and 0 to 48 hours. The mean morphine
consumption was less in-group L, 26, than group M, 54, during the 48 hours after surgery. This
study provides evidence that supports the use of LIA in TKA patients reduces the amount of
morphine needed after surgery and there by contributes to the body of literature.
AN INTEGRATIVE REVIEW: LOCAL INFILTRATION ANALGESIA
8
Eight of the eighteen RCTs in a meta-analysis of the safety and efficacy of single dose
LIA in TKA patients, studied whether LIA was associated with decreased morphine consumption
(Xu, et al., 2014). The findings of the study show that the use of LIA in TKA patients reduced the
amount of morphine consumed. However, after conducting a sensitivity analysis, the removal of
one study greatly changed the results, morphine consumption was still decreased in the LIA
groups, but there was no longer significant difference between the two groups. This reduction in
morphine consumption following TKA in patients given LIA contributes to the body of literature.
Mobility
All of the five studies assessed the functional ability or mobility after TKA in patients
that received LIA (Essving, et al., 2010; Essving, et al., 2011; Niemelainen, et al., 2014; Xu, et
al., 2014; Marques, et al., 2014). In a study by Essving (2010), maximum knee extension and
flexion were assessed at 24 and 48 hours postoperatively. A timed up and go (TUG) test was
preformed 48 hours after surgery and a value of less than 20 seconds indicated independent
mobility. Patients that received LIA had an increase of 30 degrees in flexion at 24 hours and 15
degrees flexion at 48 hours postoperatively when compared to the placebo group. There were no
significant differences between the groups with knee extension and the TUG test. The increased
mobility in patients that received LIA contributes to the body of literature.
In a RCT of 48 patients studying LIA and the reduction of opiate consumption following
a TKA, the ability to climb stairs was recorded at 24 hours and 48 hours postoperative (Essving,
et al., 2011). 50 % of the patients in the LIA group were able to climb the stairs at 24 hours, and
70 % at 48 hours compared to only 4% of the morphine group were able to climb the stairs 24
hours after surgery and 22% at 48 hours postoperatively. The researchers also recorded
maximum knee flexion and extension, and the TUG test, but these were not preformed until
AN INTEGRATIVE REVIEW: LOCAL INFILTRATION ANALGESIA
9
postop day 3 and were therefore irrelevant to this review regarding the first 48 hours. The
increased amount of patients in the LIA group to climb the stairs indicates increased mobility and
therefore contributes to this body of literature.
Niemelainen, et al., (2014) conducted a RCT of 48 patients regarding whether LIA
reduces opiate consumption until 48 hours after TKA. The secondary endpoint was funcional
outcome, and the range of motion (ROM) was assessed by a physiotherapist at 6, 24, and 48
hours postopertively. The LIA group achieved an average of 90 degrees at 6 hours, 65 degrees at
24 hours, and 75 degrees at 48 hours postop, compared to 55 degrees, 50 degrees, and 65 degrees
respectively in the plecebo group. The mean differences in ROM contributes to the body of
literature by providing evidence of increased mobility in the first 48 hours after TKA in patients
that received LIA.
In a meta-analysis of RCTs regarding the safety and efficacy of LIA in TKA patients,
there was a significant difference in ROM for patients that received LIA versus the control
groups (Xu, et al., 2014). The study reviewed secondary outcomes of functional recovery
including, ROM, time to straight leg rise (T-SLR), and the time to 90 degrees knee flexion. The
T-SLR and time to 90-degree knee flexion were both shorter in the LIA groups then the control
groups. There was an increase in the ROM in the LIA groups versus the control groups. A
sensitivity analysis was performed by omitting one study at a time, and the results did not
change. The significant difference in the ROM between the LIA groups and the control groups
after TKA contributes to the body of literature.
Mobilization outcomes were reported in 19 of 23 studies in the meta-analysis and
systematic review of RCTs of LIA for pain control in TKA (Marques, et al., 2014). In six of the
studies, patients who received LIA were able to achieve a straight leg rise on the first day after
AN INTEGRATIVE REVIEW: LOCAL INFILTRATION ANALGESIA
10
surgery when compared with the control groups. In four studies, patients achieved better flexion
and earlier ambulation than in the control groups. The early ambulation, greater degree of knee
flexion and faster times to straight leg rise in patients that received LIA following TKA
contributes to the body of literature.
Discussion/Implications
The findings of this integrative review address the efficacy of LIA for patients
undergoing TKA in controlling postoperative pain and therefore relate to the researchers PICO
question. The PICO question specifically asked about if LIA in adult patients undergoing a TKA
is effective in controlling pain when compared to IV morphine. All of the studies reported
decreased pain and increased mobility in patients that received LIA compared to the control
group, indicating that LIA is effective in controlling pain after surgery (Essving, et al., 2010;
Essving, et al., 2011; Marques, et al., 2014;Niemelainen, et al., 2014;Xu, et al., 2014). Three of
the five studies reported a reduction in IV morphine use in patients that received LIA compared
to the control group, thus supporting that the use of LIA is more effective in controlling pain and
IV morphine (Essving, et al., 2010; Essving, et al., 2011; Xu, et al., 2014). Two of the studies
reported that along with the decreaed morphine use, there was also a reduction in the known side
effects of morphine in the LIA group (Essving, et al., 2010; Essving, et al., 2011)
In the RCTs a nonprobabilty sample was used, the participants were chosen based on
certain criteria, this is appriopriate for these studies (Essving, et al., 2010; Essving, et al., 2011;
Niemelainen, et al., 2014). A sample size of 48 participants is adequate for Essving, et al. (2010),
based on the power analysis preformed prior to the study. In Essving, et al. (2011) the sample
size needed was determined using the results from a previous study and the pilot study.
According to Fain (2013), a power analysis is the best way to calculate the exact sample size
AN INTEGRATIVE REVIEW: LOCAL INFILTRATION ANALGESIA
11
needed, and therefore the reviewer is unable to determine if the sample used was adequate.
Marques, et al. (2014) reports that out of 60 patients, four from the plecebo group and one from
the LIA dropped out of the study, leaving 55 patients. Based on the power analysis only 34
patients were needed, thus the sample size was still adequate. Only one study mentioned validity
or reliability, Essving, et al. (2011) discusses the validity and reliability of the Oxford Knee
Score, but did not discuss other instruments used in data collection, such as VAS scoring.
Although all of the articles included the VAS scale to determine pain, they did not reference the
validity or reliability of the tool. The VAS scale has been previously tested and shown to be both
valid and reliable when used correctly (Hawker, Mian, Kendzerska, & French, 2011). The
specificity of the population of the studies limits generalizability.
Limitations
The researcher acknowledges there were many limitations that affected this integrative
review. This is the researchers first attempt at writing an integrative review and therefore there is
an inherent lack of knowledge. The review is a class assignment being conducted solely by the
researcher, who is a full-time nursing student with limited time available due to class schedule
and other commitments. The criteria for the assignment were restricted to five journal articles
that were published within the last five years.
Conclusion
The findings of this integrative review support that the use of LIA for TKA surgery is an
effective pain control method compared to the traditional IV morphine. Valuable findings from
the review include reduced pain, decreased morphine consumption, and early mobilization.
Improved patient outcomes and satisfaction were seen with improved pain control. Early
mobilization is essential after surgery in order to reduce the risk of blood clots, pneumonia, and
AN INTEGRATIVE REVIEW: LOCAL INFILTRATION ANALGESIA
12
skin breakdown. Reducing the amount of morphine consumed after surgery decreased incidences
of known side effects such as, nausea, vomiting, pruritus, and sedation.
AN INTEGRATIVE REVIEW: LOCAL INFILTRATION ANALGESIA
13
References
Essving, P., Axelsson, K., Aberg, E., Spannar, H., Gupta, A., & Lundin, A. (2011). Local
infiltration analgesia versus intrathecal morphine for postoperative pain management
After Total Knee Arthroplasty: A randomized Control Trial. International Anesthesia
Research Society, 113(4), 926-933. doi:10.1213/ANE.0b013e3182288deb
Essving, P., Axelsson, K., Kjellberg, J., Wallgren, O., Gupta, A., & Lundin, A. (2010). Reduced
morphine consumption and pain intensity with local infiltration analgesia (LIA)
following total knee arthroplasty. Acta Orthopaedica, 81(3), 354-360.
doi:10.3109/17453674.2010.487241
Hawker, G., Mian, S., Kendzerska, T., & French, M. (2011). Measures of adult pain: Visual
Analog Scale for Pain (VAS Pain). Arthritis Care & Research, 63(S11),
doi:10.1002/acr.20543.
Marques, E. M., Jones, H. E., Elvers, K. T., Pyke, M., Blom, A. W., & Beswick, A. D. (2014).
Local anesthetic infiltration for peri-operative pain control in total hip and knee
replacement: Systematic review and meta-analyses of short- and long-term effectiveness.
BMC Musculoskeletal Disorders, 15(220). doi:10.1186/1471-2474-15-220
Niemelainen, M., Kalliovalkama, J., Aho, A. J., Moilanen, T., & Eskelinen, A. (2014). Single
periarticular local infiltration analgesia reduces opiate consumption until 48 hours after
total knee arthroplasty. Acta Orthopaedica, 85(6), 614-619.
doi:10.3109/17453674.2014.961399
Xu, C.-P., Li, X., Wang, Z.-Z., Song, J.-Q., & Yu, B. (2014). Efficacy and safety of single-dose
local infiltration of analgesia in total knee arthroplasty: A meta-analysis of randomized
controlled trials. The Knee, 21, 636-646. doi:10.1016/j.knee.2014.02.024
AN INTEGRATIVE REVIEW: LOCAL INFILTRATION ANALGESIA
14
NUR 4122: Nursing Research Table of Evidence
Effectiveness of LIA in TKA Patients
First Author Conceptual
(Year)
Framework
Design/
Method
Sample/
Setting
Essving, P.
(2010)
None
identified
Randomized 48 TKA
doublepatientsblind
two
groups of
24 each
with 13
F/11 M
Essving, P.
(2011)
None
identified
Doubleblind
randomized
control trial
Major
Variables
Studied (and
their
definition)
Analgesic
consumption
(PCA
morphine &
tramadol use
for 48 hours),
Measurement
Data
Analysis
Findings
Morphine &
tramadol
consumption
from 0 to 48
hours post op
were recorded
MannWhitney U
test, chisquared test,
Fisher exact
test
Morphine
consumption
and post-op
pain was
lower,
discharge
readiness
was shorter,
and patient
satisfaction
was higher
in LIA
group.
Appraisal:
Worth to
practice
LIA is an
effective and
safe
alternative to
morphine for
pain control
in TKA
LIA (given to Pain
surgical
rebro
group A,
patients. It is
University periarticularly) Length of
more
Hospital
hospital stay
effective at
during
reducing pain
April 2007
surgical
and reduces
through
outcome
the risk of
September
side effects
2008
plasma
associated
concentrations
with
of LIA
morphine.
50 TKA
Group L was
Morphine
MannMorphine
LIA
patientsgiven spinal
consumption, Whitney U
consumption produced
two
anesthesia
pain relief,
test, x2,
and VAS
better pain
groups of (bupivacaine
patient
fishers exact were lower, relief, which
25 each
and saline) and satisfaction
test, & SPSS patient
is associated
AN INTEGRATIVE REVIEW: LOCAL INFILTRATION ANALGESIA
First Author Conceptual
(Year)
Framework
Design/
Method
Sample/
Setting
(group L16 F/9 M;
group M15 F/10
M)
Niemelainen, None
M. (2014)
identified
Randomized
doubleblind,
placebocontrolled
study
56 TKA
patientstwo
groups:
LIA group
27 patients
(15 F/12
M),
Placebo
group 29
patients
15
Major
Measurement
Data
Variables
Analysis
Studied (and
their
definition)
LIA
were recorded version 15.0
intraoperative,
post op day 1 Functional
Shapiro-Wilk
&2
recovery
test
Group M was
given spinal
anesthesia
(bupivacaine
and morphine)
and Saline
injection
intraoperative,
post op day 1,
&2
LIA (given
intraoperative
to LIA group)
Saline (given
intraoperative
to placebo
group)
Home
readiness
Consumption
of PCA
oxycodone
recorded post
op at 6, 12,24
and 48 hours
HAAS &
OKS, or 15 D
instrument
MannWhitney Utest, IBM
SPSS
statistics
version 20.0
Findings
Appraisal:
Worth to
practice
satisfaction
was higher,
and home
readiness
was shorter
in group L
with
increased
patient
satisfaction
and better
patient
outcomes
VAS scores
were lower
and ROM
was
increased in
the LIA
group
A single dose
of LIA given
in surgery
can reduce
the amount
of opiate
consumption
post-op,
thereby
reducing the
risk of side
AN INTEGRATIVE REVIEW: LOCAL INFILTRATION ANALGESIA
First Author Conceptual
(Year)
Framework
Design/
Method
Xu, C.P.
(2014)
None
identified
Metaanalysis of
randomized
controlled
trials
Marques,
E.M. (2014)
Random
effects
model
systematic
review and
metaanalyses
Sample/
Setting
Major
Variables
Studied (and
their
definition)
16
Measurement
Data
Analysis
Findings
Appraisal:
Worth to
practice
(14 F/15
M)
18 RCTs; LIA
1858 TKA administration
patients
effects from
opiate use.
VAS for pain, DerSimonian LIA is
LIA is an
consumption and Laird
effective for effective and
of morphine
random
post-op pain safe for short
post-op, length effects model management term pain
of stay, side
in TKA
relief after
effects
patients.
TKA
23 TKA
studies
(1,439
patients)
Pain, opioid
Sata 12
consumption,
mobilization, Review
length of
Manager 5
hospital stay,
complications,
and long term
outcomes
13 THR
studies
(909
patients)
LIA
intervention
patients that
received LIA
reported less
pain,
Opioid
consumption
was reduced
LIA is
effective for
short-term
post-op pain
control
following a
TKA. It can
be used in
Earlier
conjunction
mobilization with other
and hospital pain control
discharge
methods.
You might also like
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5795)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Las Week1 - Math5-Q3Document3 pagesLas Week1 - Math5-Q3Sonny Matias100% (2)
- Noam Chomsky: A Philosophic Overview by Justin Leiber - Book Review by Guy A. DuperreaultDocument3 pagesNoam Chomsky: A Philosophic Overview by Justin Leiber - Book Review by Guy A. DuperreaultGuy DuperreaultNo ratings yet
- Ata 46Document28 pagesAta 46Zbor Zbor100% (1)
- Capability Maturity Model (CMM) : 1. Initial - Work Is Performed InformallyDocument5 pagesCapability Maturity Model (CMM) : 1. Initial - Work Is Performed InformallyAyeshaaurangzeb AurangzebNo ratings yet
- Recommendation LetterDocument2 pagesRecommendation LetterAhmad Rizal Alias100% (1)
- Lesson Plan Heat and TemperatureDocument2 pagesLesson Plan Heat and TemperatureAlfred Angelo Cordura100% (1)
- Module2 Chapter 4Document30 pagesModule2 Chapter 4Keren ElishebaNo ratings yet
- K-8 Lunch Menu December 2014Document1 pageK-8 Lunch Menu December 2014Medford Public Schools and City of Medford, MANo ratings yet
- Solicitation For Mis AlumniDocument2 pagesSolicitation For Mis AlumniARJAY BANIQUEDNo ratings yet
- Strategies For Reading Comprehension Read Naturally, IncDocument7 pagesStrategies For Reading Comprehension Read Naturally, IncSARMAD ALINo ratings yet
- CASE STUDY - VAE Application - Quiz - Attempt ReviewDocument6 pagesCASE STUDY - VAE Application - Quiz - Attempt Reviewvinay MurakambattuNo ratings yet
- Animal KingdomDocument5 pagesAnimal KingdomArthav KumarNo ratings yet
- Asdfghnm, LDocument5 pagesAsdfghnm, Lziade roalesNo ratings yet
- Uhit Quiz 26 May 2021Document3 pagesUhit Quiz 26 May 2021dad sadNo ratings yet
- Differentiated LearningDocument27 pagesDifferentiated LearningAndi Haslinda Andi SikandarNo ratings yet
- Key Data Extraction and Emotion Analysis of Digital Shopping Based On BERTDocument14 pagesKey Data Extraction and Emotion Analysis of Digital Shopping Based On BERTsaRIKANo ratings yet
- Cdev 2 Child and Adolescent Development 2Nd Edition Spencer A Rathus Full ChapterDocument51 pagesCdev 2 Child and Adolescent Development 2Nd Edition Spencer A Rathus Full Chapterdarrell.pace172100% (18)
- Prueba Ingles InchalamDocument11 pagesPrueba Ingles InchalamCatalina BelloNo ratings yet
- Welcome To NPTEL Online Course - Integrated Marketing Management - Vasimahmad83@gmail - Com - GmailDocument1 pageWelcome To NPTEL Online Course - Integrated Marketing Management - Vasimahmad83@gmail - Com - GmailVasim AhmadNo ratings yet
- Guia Aprendizaje Ingles 5basico Semana14 Mayo 2013Document3 pagesGuia Aprendizaje Ingles 5basico Semana14 Mayo 2013Yiglia Barile SNo ratings yet
- Needs AnalysisDocument2 pagesNeeds AnalysisDianaNo ratings yet
- Client Brief, Creative SideDocument16 pagesClient Brief, Creative SidejasmeetNo ratings yet
- Jamila Bell Teaching Resume 2014 UpdatedDocument1 pageJamila Bell Teaching Resume 2014 Updatedapi-271862707No ratings yet
- BAMA 516 Customer Relationship Management - Feb2020Document6 pagesBAMA 516 Customer Relationship Management - Feb2020sherryNo ratings yet
- Form Ac17-0108 (Application Form) NewformDocument2 pagesForm Ac17-0108 (Application Form) NewformEthel FajardoNo ratings yet
- Module 1.2 Evaluating The Strengths and Weaknesses of Cultural RelativismDocument28 pagesModule 1.2 Evaluating The Strengths and Weaknesses of Cultural RelativismAnn Claire ArtajoNo ratings yet
- JBI Nationwide 2023 Group of SubrabasDocument6 pagesJBI Nationwide 2023 Group of SubrabasDonnabel BicadaNo ratings yet
- Educ 8 Lesson PlanDocument4 pagesEduc 8 Lesson PlanBRETT DEIL ARAPOCNo ratings yet
- Explicit TeachingDocument8 pagesExplicit TeachingCrisanta Dicman UedaNo ratings yet
- Qdoc - Tips Physical Metallurgy Principles and Practice ThirdDocument2 pagesQdoc - Tips Physical Metallurgy Principles and Practice ThirdAkhil KumarNo ratings yet