Professional Documents
Culture Documents
Mattson Riley 1988
Uploaded by
api-302192077Original Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Mattson Riley 1988
Uploaded by
api-302192077Copyright:
Available Formats
0 145-6008/98/2202-0279$03.
00/~
Ai.coi~oiI \ M : CI INICAL AND EXrl KIM1 N I A I
Vol. 22, No. 2
April 1998
Rl-sZ~Rcl1
A Review of the Neurobehavioral Deficits in Children
with Fetal Alcohol Syndrome or Prenatal Exposure to
Alcohol
Sarah N. Mattson and Edward P. Riley
of children of alcoholic parents, particularly alcoholic
mothers. . . . This report went virtually unnoticed in the
United States until 1973, when Seattle dysmorphologists
documented similar findings3and defined a specific pattern
of malformations in children born to chronic alcoholic
women as fetal alcohol syndrome (FAS).4
More than 20 years later, it is estimated that FAS affects
approximately 0.29 to 0.4SilOOO live born children. Prevalence estimates vary depending on socioeconomic and ethnic factors, and those that include Native American populations report incidences of up to 2.99/1000 births. In the
HROUGHOUT HISTORY, the negative effects of United States, at least 1200 children are born each year
maternal drinking on offspring have been suspected. with FAS, and the annual cost associated with caring for
Aristotle has been quoted as saying that foolish, drunken, such infants is estimated at 74.6 million dollar^.^ These
or hare-brain women, for the most part bring forth children estimates are strictly limited to those children who meet the
like unto themselves, morosos et Zanguidos, and in clinical criteria for FAS and do not include the spectrum of
Carthage and Sparta, laws prohibited the use of alcohol by effects caused by prenatal alcohol exposure. It is obvious,
newlyweds presumably to prevent conception during intox- however, that the effects of alcohol use during pregnancy
ication. During the gin epidemic in England, in the first are widespread and devastating, and that these problems
half of the 18th century, physicians warned against alcohol are entirely preventable.
consumption during pregnancy, claiming this was the cause
The effects of prenatal alcohol exposure fall on a conof weak, feeble, and distempered children. Such beliefs tinuum with FAS and perinatal death at one end and
continued until the early 20th century. In the postprohibi- relative normalcy on the other. Between these two endtion medical community, however, the idea that alcohol points are a variety of behavioral and physical features that
taken during pregnancy could be harmful to the developing are termed fetal alcohol effects (FAEs) or alcohol-related
fetus was dismissed as moralism. It was thought that harm- birth defects. The wide range of behavioral and cognitive
ful effects noted in the offspring of alcoholic women were effects associated with prenatal alcohol exposure is reprethe result of constitutional factors that also were the cause sentative of the continuous nature of alcohols behavioral
of the alcohol problem. It was not until the late 1960s and teratogenicity. Importantly, FAS represents only one point
early 1970s that interest in the adverse effects of alcohol on the continuum, and the effects of in utero alcohol
was renewed. In 1968, a group of French researchers pub- exposure on children without FAS should also be assessed.
lished the results of a study of 127 children of alcoholic
In the offspring, the diagnosis of FAS is based on a triad
parents.2 They reported the highly distinctive appearance
of features: (1) pre- and/or postnatal growth deficiency; (2)
a pattern of craniofacial malformations; and (3) central
From the Center for Behavioral Teratology, Department of Psychology, nervous system (CNS) dysfunction. Babies born with FAS
San Diego State University, San Diego, California.
are often small for gestational age4 and continue to show
Presented at the 1996 Borchard Foundation Symposium on the Behavioral
evidence
of growth deficiency.6For example, in a sample of
Effects in Children following Prenatal Alcohol Exposure, Missillac, France,
adolescents and adults with FAS, the mean height and
July 28-30, 1996.
This work was supported by the National Institute on Alcohol Abuse and weight were 2.1 and 1.4 standard deviations below the
Alcoholism Grant AA10417 and AA10820.
population mean, re~pectively.~
The pattern of craniofacial
Reprint requests: Sarah N. Mattson, Ph.D., Center for Behavioral Teramalformations
includes
microcephaly,
short palpebral fistolog?! 6363 Alvarado Court, Suite 209, San Diego State University, San
sures,
a
long
smooth
philtrum,
a
thin
vermilion border,
Diego, CA 92120.
epicanthal
folds,
and
flat
m
i
d
f
a
~
e
The
.
~
CNS
dysfunction is
Copyright 0 1998 by The Research Society on Alcoholism.
Fetal alcohol syndrome is a devastating developmental disorder
caused by prenatal exposure to high amounts of alcohol. In addition
to structural abnormalities and growth deficits, fetal alcohol syndrome is associated with a broad spectrum of neurobehavioral
anomalies. This paper reviews the behavioral and cognitive effects of
prenatal alcohol exposure. More than 20 years of research are discussed, with a focus on 10, activity, attention, learning, memory,
language, motor, and visuospatial abilities in children prenatally exposed to varying amounts of alcohol, including those with fetal alcohol syndrome.
Key Words: FAS, PrenatalAlcohol Exposure, Brain Function, Neuropsychological Effects.
Alcohol Clm Exp Res, Vol22, No 2, 1998: pp 279-294
279
MATTSON AND RILEY
280
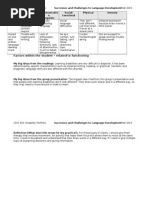
Table 1. IQ Scores of Individual Cases of FAS or Alcohol-Exposed Individuals Reported in the Literature, Presented in Chronological Order Through 1996
_
Authors
Jones, Smith, Ulleland, 8 Streissguth3
Palmer, Ouellette, Warner, 8 Leichtman
Root, Reiter, Andrioia, 8 Ducken
Tenbrinck 8 B ~ c h i n ~
Ko~sseff~
Char
Mulvihill Klimas, Stokes, 8 Ri~emberg~
Bierich, Majewski, Michaelis, 8 Tillner40
Majewski, Bierich, Loeser, Michaelis, Leiber, 8
Bette~ken~
Ijaiya, Schwenk, 8 Gladtke14
Van BiervlietS5
Fryns, Deroover, Parloir, Goffaux, Lebas, & Van Den
Berghe 42
Dehaene, Walbaum, Titran, Samaille-Villette,
Samaille, Crepin, Delahousse, Decocq, Delacroix,
Caquant, 8 Q ~ e r l e u ~ ~
Koranyi 8 CsikyiiZ
Neidengard, Carter, 8 Smith
Ballesta 8 Cruz17
Slavney 8 Grau
Qazi, Masakawa, Milman, McGann, Chua, 8 HalleP
Qazi, Madahar, Masakawa, 8 McGann
Maller, Brandt, & T y g s t r ~ p ~ ~
Shaywitz, Caparulo, 8 Hodgson l 3
losub, Fuchs, Bingol, Stone, 8 G r ~ m i s c h ~ ~
Naselli. De Toni. Vianolo. Di Battista. 8 AicardP4
Age
14m
3m
57m
46m
40m
48m
34m
3yl Om
14.5m
22m
14.5m
22m
14.5y
11.7~
11.oy
9.9y
2y4m
3y5rn
1l Y
6m
NfA
5Y
3y7m
6y2m
7y9m
6y6m
lY
2y6m
15Y
1 6 ~
21Y
31-17
6m
7m
1Om
I am
26m
13Y
4y6m
7y3m
llm
21m
16Y
1lY
1OY
15Y
7Y
8Y
4y6m
7Y
6Y
16m
3yl m
4y4m
4yl Om
9Y
13Y
17Y
1OY
17Y
1am
4Y
6~
8y6m
6v6m
Tests
1 (case 1)
1 (case 2)
1 (case 3)
1 (case 4)
1 (case 6)
1 (case 7)
1 (case 8)
1 (case 1)
1 (case 2)
Bayley MDI
Bayley MDI
Stanford-Binet
Stanford-Binet
Stanford-Binet
Stanford-Binet
Bayley MDI
Stanford-Binet
Bayley MDI
1 (case 3)
Bayley MDI
1 (KC)
1 (AC)
1 (PC)
1 (RC)
1
1
1
1 (case 5)
1 (case 2)
1 (case 5)
1 (case 23)
NfA
1 (case 1)
HAWIK
(German WISC)
Stanford-Binet
Stanford-Binet
Griffith
1 (case 3)
1 (case 4)
1
1 (case 2)
1 (case 3)
I (case 4)
1 (case 7)
1 (case 10)
1 (case 11)
1 (case 12)
1 (case 13)
I (case 14)
1 (case 1)
1 (case 2)
1 (case 3)
1 (case 4)
1 (case 5)
1 (case 2)
1 (case 1)
1 (case 2)
1
1 (case 1)
1 (case 2)
1 (case 3)
1 (case 4)
1
1
1 (case 1)
1 (case 1)
1 (case 2)
1 (case 3)
Cattell
NIA
NfA
Cattell
Kramer
Kramer
NfA
Brunet-Lezine
NfA
N/A
N/A
WISC-R
NIA
Merrill-Palmer
Cattell
NfA
Leiter
NIA
NIA
WAlS
N/A
WAlS
Bayley MDI
Stanford-Binet
WlSC
WlSC
WlSC
IQ estimatet
Comments
59
83
75
57
79
70
150
65
56
76
59
70
80
75
112
68
36
75
85
41
93
84
105
76
a7
54
52
65
52
35
25
37
75
58
50
60
72
59
82
54
72
73
33
70
55
66
52
70
65
74
68
50
45
68 P a )
69 (DQ)
120
70
a0
67
60
72
50
50
50
50
46
Twins placed in foster home between
testings
Siblings; case PC had fewer
dysrnorphic features
Not identified as FAS by author$
Noonan syndrome
AEIf
Klippel-Feil malformation
Chromosomal abnormalities$
Schizophrenia
Renal anomalies
Chromosomal abnormalities$
Language disordered+
Siblings
NEUROBEHAVIORAL FINDINGS IN FAS
281
Table 1. Continued
Authors
Age*
Ticha, Santavy, & Matlochaz3
3Y
3Y
5m
4Y
<3Y
<3Y
4Y
6y2m
6y4m
<lY
1OY
4y9m
8Y
4Y
14Y
3Y
13Y
4Y
14Y
3Y
13Y
<lY
1OY
4Y
14Y
17m
5yl Om
5y4m
1Oy3m
2y2m
5yllm
12Y
14Y
1 6 ~
Tests
IQ estimate7
Comments
Aronson & OlegPrdZ4
Streissguth, Clarren, & Jones
Usowicz, Golabi, & Curry6
Marcus
Mattson, Riley, Jernigan, Ehlers, Delis, Jones, Stern,
Johnson, Hesselink, & B e l l ~ g i ~ ~
Mattson, Riley, Jernigan, Garcia, Kaneko, Ehlers, &
Jones45
Harris, MacKay. & O ~ b o r n ~ ~
Ernhart, Greene, Sokol, Martier, Boyd, & Ager23
41-17
6.5m
12m
19m
25m
9m
13.5m
20m
7m
1 (case 1)
1 (sib of C1)
1 (case 2)
1 (case 5)
1 (sib of C5)
1 (case 6)
1
1
1 (case 2)
1 (case 3)
Terman-Merrill
Terman-Merrill
Brunet-Lezine
Terman-Merrill
Brunet-Lezine
Brunet-Lezine
Terman-Merrill
N/A
Bayley MDI,
WISC, WISC-R,
Stanford-Binet,
or WPPSI*
1 (case 4)
1 (case 6)
1 (case 7)
1 (case 8)
1 (case 9)
1 (case 11)
1 (case 3)
1 (case 1)
1 (case 2 )
1 (case 3)
1 (case 4)
1 (case 5)
1 (case 1)
1 (case 2)
2 cases
with PEA
1 (case 1)
Bayley MDI
NIA
WISC-R
WISC-R
Bayley MDI
1 (case 2)
1 (case 3;
FAE)
13m
17m
25m
3y.4ylOm case 1
case 2
case 3
case 4
case 5
case 6
case 7
case 8
Stanford-Binet.
WPPSl
80
50
50 (DQ)
50
60-70 (DQ)
50 (DQ)
55
70
76
83
86
66
76
47
48
68
81
60
57
50
80
43
40
30
20
50
50
100
55
95
85
51
41
64, 69
89
77
<50
<50
69
<50
50
<50
81
57
63
54
95, 94
105,87
79,95
65, 79
83,87
78, 101
98, 87
50,25
Siblings of patients also were alcoholexposed and had at least some
features of FAS, if not frank FAS
Laryngeal web
Agenesis of corpus callosum
All three cases displayed autistic
behaviors
Testing at earlier dates also reported*
N/A, not applicable; sib, sibling.
* m, months: y, years.
t IQ estimates in italics are included in the mean (see text for details).
See text for details.
9 W, developmental quotient.
# Some of these cases overlap with Jones, Smith, Ulleland, & Streissguth (1973) listed above; however, since the 1973 publication, the normative data for the
0 scores for cases 3, 4, 6, and 7.
Stanford-Binet have been revised, which explains the revised 1
variable and can present as hyperactivity, attention deficits, leading known cause of mental retardation in the Western
world. The average IQ of children with FAS falls close to
learning disabilities, or mental retardation.
In
Although the diagnosis of FAS does not require frank 70, although the range is quite large (e.g., 20 to
exposed
children
who
do
not
meet
the
criteria
for
FAS,
mental retardation, intellectual capacity is very often compromised in these children. In fact, FAS has been called the some of the previously mentioned features may still be
282
MATTSON AND RILEY
Table 2. IQ Scores for Groups of Alcohol-Exposed Subjects Reported in the Literature, Presented in Chronological Order Through 1996
Authors
Age
Streisguth & R o h s e n o ~ ~ ~ * ~
8m
4Y
7Y
Dehaene, Samaille-Villette, Samaille, Crepin, NIA
Walbaum, Deroubaix, & B l a n ~ - G a r i n ' ~ ~ ' ~
9m-2.5y
Streissguth, Herman, & Smith26^Rb
2.51-5y
6-1 5y
20-21 y
Streissguth, Herman, & Smith54'R"
7m-21y
21m-22y
M a j e ~ s k i ~ ~ . Majewski
~ ~ . ' ~ ~&f ~ ;
5-9Y
Maje~ski"~~
5
10
3
2
17
Bayley MDI
Stanford-Binet
WISCNVISC-R
WAlS
Bayley MDI, Stanford-Binet,
WISCNVISC-R, or WAlS
Kramer IQ test
15-63
47-99
60-1 05
57-67
15-99
10-96
50-95
47-1 02
61-130
NIA
47.4
68.9
84.7
62
66
67
66 (AE Ill)
79 (AE II)
91 (AE I)
<70n = 9
70-85 n = 19
98.2
82-1 13
98
101
109
114
116
116
NIA
64-150+
4-25y
NIA
15
Streissguth, Barr, Martin, & Herman39*P
Em
losub, Fuchs, Bingol. & G r o m i ~ c h ~ " ~
1day-23y
10 (AAP 2 4)d
12 (AAP 2 3)
25 (AAP 2 2)
97 (AAP 2 1)
365 (AAP < 1)
216 (AAP 5 0.10)
63
Golden, Sokol, Kuhnert, &
Steinhausen, Nestler, & Spohr'
3-1 5y
12
32
Aronson & Oleglrd'32*R
6y3m (SD = 34m) 32
8y7m (SD = 15m) 16
1y6m-7y
13 pairs
7-9y
8 pairs
12m
25 total
(AAP 2 1.0)
(AAP < 1.0)
(AAP c 0.1)
6m
22 (cont. drinking)
11 (stopped drinking)
27 (never drank)
2.5-3oy
95
Fried & Watkir~son~'*~"
12m
Coles, Smith, 8 Falek66*P
10 (AA > 0.85)B
116 (AA < 0.14)
8 (AA > 0.85)
71 (AA < 0.14)
421
24m
Streissguth, Barr, Sampson, Darby, &
Ma~tin~~*~
IOffe 8 C h e m i ~ k ~ ~ ' ~
conry71'~
Streissguth, Barr, & S a m p ~ o n ~ ~ * ~
Fried 8 W a t k i n s ~ n ~ ~ * ~ ~
4Y
1.5-9m
5.2-18.5~
5.2-15.8~
5.2-18.5
7.5y
3Y
4Y
Streissguth. Aase, Clarren. Randels, LaDue,
& Smith7R
Carney & Chermak'Z''R
Forrest, Florey, Taylor, McPherson, 8
Y o ~ n g ~ ~ * ~
Streissguth, Randels. & Smith34Rc
Coles, Brown, Smith, Platzman, Erickson, &
Falek4'*'
12-4oy
8y6m (SD
18m
8.0~
16.9~
9.oy
16.0~
5yl Om
2.3y)
IQ range
79.93 (vs. 80.47)"
87.92 (vs. 95.69)
80.73 (vs. 94.90)
66
Oleglrd, Sabel, Aronsson, Sandin,
Johansson, Carlsson, Kyllerman, Iversen.
& HrbekZgfR
Shaywitz. Cohen, 8 S h a y ~ i t z ~ ~ ' ~
Steinhausen,
Spohr & Steinhau~en'~'~~;
Gobel, 8 N e ~ t l e ? ~ ' ~ ~
Aronson, Kyllerman. Sabel, Sandin, 8
Oleglrd3Z*R
O'Connor, Brill, & Sig~nan~O*~
Mean IQ
Bayley MDI
Stanford-Binet
WlSC FSlQ
Brunet-Lezine
4
9
48 total
12m
Tests
15
13
15
22
17
13 (FAS)
6 WE)
19 (controls)'
482
69 (AA/day 2 0.14)
64 ( W d a y < 0.14)
71 ( W d a y 2 0.14)
59 W d a y < 0.14)
38 (FAS)
14 (FAE)
10
592
27 (FAS)
WISC, WPPSI, or StanfordBinet
Bayley MDI
Bayley, Stanford-Binet.
Denver, Wechsler
Bayley MDI
Columbia Mental Maturity
Scale
Columbia Mental Maturity
Scale
Griffith
WISC
Bayley MDI
Bayley MDI
NIA
Bayley MDI
WPPSI
Bayley MDI
WPPSI, WISC-R, or WAIS-R
WISC-R
McCarthy GCI
WISC-WWAIS-R
WISC-R
Bayley MDI
WISC, WISC-R, StanfordBinet, WAIS, WAIS-R
13 (FAE)
25 (AA/week = 11.8)
21 (Wweek = 0)
K-ABC
33-1 12
50-97
86 (SD = 20)
89
NIA
NIA'
NIA
92 (controls = 111)
99 (controts = 114)
95 (SD = 2.99)
108 (SD = 8.48)
115 (SD = 7.72)
102.9
111.03
113.11
NIA
98.4
109.5
110.7
119.5
NIA'
67.4
60.1
86.0
87.3
NIA'
115.8
114.8
123.4
124.4
66
73
79
NIA'
66.0
66.7
79.5
82.2
83.91 (SD = 12.61)
91.91 fSD = 13.81)
<70 (n = 12)
70-85 (n = 33)
NIA
50-89
For FASIFAE:
40-1 01
NIA
20-1 05
50-91
NIA
NEUROBEHAVIORAL FINDINGS IN FAS
283
Table 2. Continued
Authors
Age
5 ( P P M > 3.5)9
11 (PPAA < 3.5)
97 (PPAA < 1)
39 (Abstainer)
6rn
297
Greene, Ernhart. Ager, Sokol, Martier, 8
279
1Y
275
2Y
269
3Y
4yl Om
260
LaDue, Streissguth, & Randels6"*R
12-42~
(mean = 18.4) 92 (FASIFAE)
Autt-Ramo, Korkman, Hilakivi-Clarke,
27m
20 (3 trimesters exp.)
Lehtonen. Halrnesmaki. & G r a n ~ t r o m ~ ~ * '
20 (2 trimesters exp.)
20 (1 trimester exp.)
71 ( W d a y > 0.14)
Fried, O'Connell, & W a t k i n s ~ n ~ ' * ~ ~
5Y
64 ( W d a y < 0.14)
67 ( W d a y > 0.14)
6Y
70 ( W d a y < 0.14)
382
Jacobson, Jacobson, Sokol. Martier, Ager,
13m
& Kaplan-Estrin7'*'
OConnor. Sigrnan, & K a ~ a r i ' ~ ~ * ~
12m
24 ( W d a y > 0.10)
20 ( W d a y < 0.10)
17m-30~
12 (FAS)
Streissguth 8 D e h a e r ~ e ~ ~ ~
7 (FAE)
10 (PEA)h
Caruso B ten B e n ~ e I ' ~ ~ ' ~
N/A
15
Steinhausen. Willms, & Spoh?s*Rc
15
5y4m (SD = 13m)
8y9m (SD = 24m)
5y5m (SD = 14m)
16
15ylm (SD = 25m)
31
9y10m (SD = 18m)
13y2m (SD = 19m)
41
Spohr, Willms, & S t e i n h a u ~ e n ' ~ ~ ' ~ ~ 15y4m (SD = 21.61-4
Russell, Czarnecki, Cowan, McPherson. &
MudaP7*'
Janzen. Nanson, & Block68'R
Larroque, Kaminski, Dehaene, Subtil,
Delfosse, & Q u e r l e ~ ~ ~ * ~
Mattson, Riley, Gramling. Delis. &
18m
52.7~1
(SD = 8.82m)
-4.5y
8 . 5 ~(SD = 3 . 8 ~ )
8 . 5 ~(SD = 4.0~)
10
32 2 1.5 oz/day
123 < 1.5 odday
34 with FAS
13 with PEA
Mean IQ
Tests
WPPSI VIQ/PIQ
Bayley MDI
101.1/101.7
111.8/99.9
107.7/101.9
107.8/100.7
N/A'
WAIS-WISC-R
Bayley
70
N/A'
McCarthy GCI
120.9
122.2
126.8
124.2
N/A'
Bayley MDI
107.79 (SD = 10.7)
113.1 (SD = 8.99)
69.6
93.0
91.7
Bayley MDI
Bayley, WISC-R, WAIS-R,
Stanford-Binet, TermanMemill, Brunet-Lezine
WISC-R
69.7
Columbia Mental Maturity
NIA'
Scale, WPPSI, or WISC-R
WPPSIMIISC-R
8G116; n = 10
71-85; n = 14
51-70; n = 6
36-50; n = 5
C35; n = 6
McCarthy GCI
McCarthy GCI
67.6
WPPSI-WWISC-R
89.5 (SD = 2.92)
103.2 (SD = 1.69)
74.4
83.6
IQ range
N/A
12-1 08
N/A
NIA
56-120
NIA
NIA
NIA
NIA
NIA
N/A, not applicable; FSIQ, Full scale IQ; GCI, General Cognitive Index; K-ABC, Kaufman Assessment Battery for Children: VIQ, Verbal IQ; PIQ, Performance IQ: exp,
exposure.
* Subjects are FAS: t subjects are AE 1-3; $ subjects are alcohol-exposed to varying degrees.
Retrospective study: prospective study.
a Values for controls included for comparison purposes.
This sample includes patients reported earlier in Jones, Smith, Ulleland. and Streissguth (1973).
Retest.
AAP = oz of absolute alcohol consumed/day in the month prior to pregnancy recognition; IAA = 1-2 drinks of beer, 2 drinks of wine, or 2 drinks of liquor.
AA = oz of absolute alcohol/day during pregnancy.
'See text for details.
PPAA = oz of absolute alcohol consumed prior to pregnancy recognition.
This study involves 16 sets of twins; PEA = prenatally exposed to alcohol, no diagnosis.
present. Importantly, in the absence of the specific facial
malformations, and thus the diagnosis of FAS, cognitive
deficits, even mental retardation can still be present.
The intent of this paper is to review the behavioral and
cognitive effects of prenatal alcohol exposure. More than
20 years of research are discussed, with a focus on IQ,
activity, attention, learning, memory, language, motor, and
visuospatial abilities in children prenatally exposed to varying amounts of alcohol, including those with FAS. Animal
studies will only be briefly discussed in support of human
studies.
INTELLIGENCE
In the more than 20 years since FAS was first described,
an array of cognitive and behavioral characteristics have
been identified in children and animals exposed to alcohol
Various authors have addressed the effect of
prenatal alcohol exposure on IQ, and in general, such
exposure leads to a decreased IQ score. Both individual
cases and group means have been reported in the literature. Although some comparability between reports is possible, there are differences in the measures that have been
284
MATrSON AND RILEY
used to evaluate intellectual functioning. The predominant ment at the ages of 3 years 10 months, 14.5 months, and
tests that have been used are the Bayley Scales of Infant 14.5 months of age, respectively. After the twins were
Mental and Motor Development (subsequently called the placed in a good foster home, they were reassessed and
Bayley), which provides a Mental Development Index earned MDI values of 76 and 70. Four new cases, who were
(MDI); the Stanford-Binet Intelligence Scale; and the all children of one alcoholic woman, were described by
Wechsler scales that include the Wechsler Preschool and Root et a1.12 All were diagnosed as having FAS, although
Primary Scale of Intelligence, original and revised versions one (PC, the third child) had fewer dysmorphic features.
(WPPSI and WPPSI-R); Wechsler Intelligence Scale for The IQ scores of these children were 80,75,112, and 68. It
Children, original and revised versions (WISC and WISC- is notable that PC, the third child, had fewer dysmorphic
R); and the Wechsler Adult Intelligence Scale, original and features and the highest IQ of the group. In a report
revised versions (WAIS and WAIS-R). The Stanford-Binet proposing a new syndrome, a child was described who
and the Wechsler scales provide Intelligence Quotients or seemed to meet the criteria for FAS and had an alcoholic
IQ scores based on comparison with large standardization mother. Although the author did not recognize the case as
groups. In the following discussion of IQ in FAS, the FAS, an editorial note identified the similarity between the
specific tests used will be mentioned if this information is case and the recent description of FAS by Jones and colavailable. Individual case reports that include IQ estimates leagues. This child had an IQ of 75.13
are listed in Table 1 and IQ reports of alcohol-exposed
Majewski et al. l4 reported three examples of alcohol
groups are listed in Table 2. Although general information embryopathy (AE), including one boy with AE I who had
about intelligence in FAS will be reviewed, only cases that an IQ of 105, using Kramers method of assessment. The
require more detailed description will be discussed here, term alcohol embryopathy is used in place of fetal alcohol
and the reader is referred to the tables for a complete list syndrome by German researchers who considered it more
of reports that include measures of IQ.
appropriate because the associated dysmorphology occurs
during the embryonic period of development. In addition,
the use of AE terminology includes a gradation of effects
Reports of Individual Cases of Children with FAS
that is not traditionally associated with the FAS terminolEarly reports of children with FAS were often descriptive ogy. Three degrees (I, 11, and 111) are used to describe
studies of very small groups of children or individuals. alcohol-exposed children with mild (I) to severe (111) alcoMeasurements of intelligence were not always included or hol-related e f f e ~ t s . ~
were described qualitatively (i.e., borderline or mentally
Intellectual functioning has been reported for children
retarded) rather than quantitatively. A review of the avail- with FAS who also have other disorders or malformations.
able reports, detailed in Table 1, reveals a mean IQ of FAS In 1976, a child with FAS and Noonan phenotype was
cases is 65.73 (SD = 20.2), with a range of 20 to 120. This reported to have an IQ of 85.16 Chromosomal abnormalimean encompasses all cases that are clearly FAS and had ties in children with FAS have been reported in three cases.
an exact IQ estimate (n = 79). When more than one testing The first report described two children with IQ scores of 66
was reported for the same individual, only the most recent and 55 and had the following chromosomal abnormalities:
score was included in the mean. Several of these cases 46, XY, inv. (3) (p13q27) and 45, XY, -14, -15, +t
deserve a more detailed discussion. The earliest reports of (14q15q). It is unclear what role these abnormalities had in
Jones and his colleagues3 on eight infants and young chil- the etiology of the dysmorphic and cognitive anomalies
dren with FAS documented MDIs and IQ scores for seven observed in these two children. It is notable that other
patients in the range of 50 to 83 (mean = 67.6) using the family members, including one mother, had similar dysmorBayley and the Stanford-Binet. In a 10-year follow-up, phic feature^.'^ The second report was of a girl with an IQ
these cases were rereported according to the revised Stan- of 50 and 47 chromosomes in all cells. In addition, a
ford-Binet normative data. The new range of the original 15-year-old girl with FAS and schizophrenia was deIQ scores for six of the seven children was rereported as 47 scribed. Her IQ was estimated to be 52, although psyto 83 (mean = 62.3). Two additional cases were also re- chotic symptomatology may have interfered with valid asported with IQ scores of 30 and 43 at the ages of 7 months sessment. IQ scores of additional cases of FAS with
and 4 years, respectively. At the 10-year follow-up, the IQ Klippel-Feil malformation2 and renal anomalies21 have
scores of these eight patients were 20 to 86 (mean = 61) also been noted.
using the Stanford-Binet and WISC6 The issue of the
In the 1980s, fewer case reports included a measure of
stability of IQ over time in individuals exposed to alcohol IQ, although a similar number of cases were reported.
prenatally is addressed later in this paper.
According to Abe1,22 245 cases of FAS were documented
In 1974, the cases of three siblings (one singleton and between 1973 and 1979, with 45 reports of IQ (18.4%).
monozygotic twins) born to an alcoholic mother were de- Alternatively, in the 205 cases reported between 1980 and
scribed by Palmer et al. These three children met the 1988, only 13 included IQ scores (6.3%). A review of the
existing criteria for FAS and had MDI/IQ scores of 65 literature uncovered four more IQ reports. Two come from
(Stanford-Binet), 56, and 59 (Bayley) at their first assess- a study included by Abel but not included in his listingz3
NEUROBEHAVIORAL FINDINGS IN FAS
and two from a review article by Aronson & OlegHrd.24
Since Abels comprehensive summary of FAS reports, very
few reports have included IQ scores or even individual case
descriptions. This decrease in case reports reflects the
growing recognition of FAS and the increase in retrospective and prospective group studies.
Reports of Groups of FAS or Alcohol-Exposed Children:
Retrospective and Prospective Studies
As the study of the effects of prenatal alcohol exposure
progressed, larger retrospective and prospective studies
were initiated. Retrospective studies have evaluated groups
of children with FAS or varying degrees of alcohol-related
effects and have reported results as a function of group
means for FAS/alcohol-exposed and nonexposed controls.
Benefits of this type of study include the value of larger
groups of subjects and the inclusion of control groups.
Alternatively, confounding factors, such as cultural or socioeconomic effects, as well as the possibility of an ascertainment bias, sometimes confuse the results. Additional
difficulties arise in these and other studies in terms of
potential confounding variables, such as maternal IQ, paternal effects, medication usage, and other comorbidity
factors. These factors are often not addressed in retrospective studies, but their relevance cannot be ignored. Wellcontrolled studies, including well-matched control groups,
help reduce the problem of confounds but ascertainment
remains a difficulty with this type of sample. In addition,
because the children in retrospective studies are identified
after birth and frequently medical records and/or contact
with the biological mother is unavailable, there is often
little reliable information about the degree of alcohol exposure. When only children with FAS are evaluated, less of
a problem exists because alcohol exposure is typically included in the diagnostic criteria and the relationship between such exposure and the resulting physical features is
clear. In other words, because alcohol exposure is part of
the traditional diagnostic criteria, children with unknown
prenatal histories are excluded by definition. When less
affected non-FAS children are evaluated, there is more
reliance on prenatal alcohol history for study inclusion.
Retrospective studies (see Table 2 for complete list),
such as the early Seattle s t ~ d i e s ~or
~ studies
~
out of German~,~-~
reported an overall mean IQ of 72.26 (range of
means = 47.4-98.2). This weighted mean (the mean was
adjusted for sample size differences) encompasses all retrospective group studies (17 studies) of children with FAS
or AE (total n = 269) as detailed in Table 2.
A few retrospective studies require more detailed discussion. Although traditional studies of intellectual functioning in FAS began with children of alcohotic mothers, Shaywitz et al.30started with a large group of learning disabled
children and discovered 15 who were born to alcoholic
Women. This group had a mean IQ of 98.2 (range =
80-113) using the WISC, WPPSI, or Stanford-Binet. The
285
authors, however, were interested in learning difficulties in
children of normal intelligence who were born to alcoholic mothers, and these children may not truly be representative of FAS. In a different group of 63 children with
FAS, IQ information was available for the 30 that were
over the age of 3 years. The IQ scores ranged from 50 to 97,
with most patients having IQ scores between 65 and 70, and
mental retardation was found in 14 of the 30 (46%).31 A
group of 21 alcohol-exposed subjects and a well-matched
control group were assessed by Aronson and colleagues32
using Griffiths Mental Developmental Scales and the
WISC. The mean performances of the alcohol-exposed
group were 19 and 15 IQ points below the control group on
the Griffiths and WISC, respectively. Only 10 of the 21
alcohol-exposed individuals met criteria for FAS, reiterating that the effects of alcohol are important even in the
nondysmorphic individual. Finally, in a long-term follow-up
of adolescents and adults with FAS (n = 38) or FAE (n =
14), mean IQ was determined to be 68 (range = 20-105).
The mean I Q of the FAS group, at 66, was lower than that
of the FAE group that was 73.7
Recently, the IQ performances of children with FAS were
compared with alcohol-exposed children with few if any features of FAS.33 All chddren in this study were exposed prenatally to high amounts of alcohol; however, only the FAS
group displayed the craniofacial anomalies and growth deficits
associated with the diagnosis. The other group was designated
as having prenatal exposure to alcohol (PEA) and had documented exposure to high levels of alcohol, but were not dysmorphic, microcephalic, or growth retarded. In comparison
with normal controls, both groups of alcohol-exposed children
displayed significant deficits in overall IQ measures, as well as
deficits on most of the subtest scores. Importantly, these
deficits in IQ were found in both alcohol-exposed groups.
Whereas the PEA subjects usually obtained marginally higher
IQ scores than those with FAS, few significant differences
were found between the two alcohol-exposed groups. These
results indicate that high levels of prenatal alcohol exposure
are related to an increased risk for deficits in intellectual
functioning and that these deficits can OCCUT in children without all of the physical features required for a diagnosis of FAS.
Similarly, individuals with the partial phenotype of FAS, or
FAE, display IQ d e f i ~ i t s .Our
~ , ~ PEA subjects may be somewhat similar to individuals identified by other groups as having
FAE; however, individuals with PEA display few if any of the
facial features of FAS, and are not growth retarded or microcephalic.
Prospective studies of the effects of prenatal alcohol
exposure have evaluated pregnant women using a variety of
prenatal measurements, including alcohol consumption.
The resulting offspring have been followed longitudinally,
up to 14 years in the case of Streissguth et al.35 The
strengths of such studies are obvious. They allow for a
better understanding of the exposure patterns and can
include measurement of other, possibly confounding, factors (e.g., smoking, other drug use). Although very often
286
MATSON AND RILEY
the children in these prospectively identified groups do not rospective studies is that they allow greater understanding
have FAS and the level of alcohol exposure is relatively low, of the effects of pregnancy drinking dose and pattern.
the use of large groups of mothers allows for an assessment Although animal studies (e.g., Refs. 45 to 47) clearly indiof the relationship between alcohol exposure and offspring cate the importance of pattern and timing of alcohol expobehavior. As a consequence of the design of these large sure and binge-drinking has been identified as a significant
prospective studies, relationships between the variables are risk factor for negative neurobehavioral outcome (e.g., Ref.
described, and group means are often not reported. How- 44), more information is needed. For example, beyond
ever, some prospective studies still include IQ values pre- trimester of exposure (e.g., Ref. 48), little is known about
the relationship between timing of alcohol exposure and
sented as a function of alcohol exposure level.
Similar to the retrospective studies, prospective studies later neurobehavioral outcome in humans. Future studies
have found decrements in IQ related to alcohol exposure. should emphasize more detailed analyses of factors such as
Golden et al.36 assessed twelve 1-year-old children who timing and dose of in-pregnancy drinking.
were identified as having FAS, based on prospectively gathered information on alcohol exposure and neonatal exam- Studies Finding No Effect of Prenatal Alcohol Exposure do
ination. Using the Bayley, the mean MDI for this group was Exist
estimated as 86. In 1990, Ioffe and C h e r n i ~ kreported
~~
a
Not all studies report decreases in intellectual performean MDI of 67.4 in a group of 17 alcohol-exposed infants
mance,
however. A 1991 report from Scotland used the
(1.5 to 9 months of age) identified prospectively. Additionally, a group of 20 prospectively identified, alcohol-exposed Bayley to assess five hundred ninety-two 18-month-olds
children (only six with FAS) whose mothers continued to and found an increase in performance related to pre- and
.~~
alcodrink throughout pregnancy had significantly lower scores postpregnancy alcohol c o n ~ u m p t i o n Furthermore,
hol
exposure
was
unrelated
to
cognitive
outcomes
on
the
on the Bayley than children whose mothers drank during
McCarthy
in
children
3
through
6
years
of
age.50751
As
the
the first trimester only.38
authors
point
out,
however,
the
exposure
levels
in
this
study
With the use of prospective investigation of alcohol use
during pregnancy, more information has become available were very low (mean = 0.43 to 0.45 M d a y ) in the higher
about the effects of different levels of alcohol exposure. exposure group. Another study of children exposed to low
Streissguth and her colleagues have followed the children amounts of alcohol (mean = 0.07 M d a y ) found no effect
of nearly 500 mothers from the prenatal period through the of alcohol exposure on the Bayley at ages 6 months and 1,
age of 14 years. In 1980, she reported a relationship be- 2, and 3 years, and the WPPSI at age 4 years, 10 monthss2
tween the amount of alcohol consumed and performance
on the Bayley at 8 months of age.39The mean MDIs ranged Concordance of IQ in Twins Exposed to Alcohol Prenatally
from 116 for infants of mothers who drank <0.10 AAP
Additional information on IQ as a function of in utero
(ounce of absolute alcohol per day prior to pregnancy alcohol exposure is also available in studies examining twin
recognition) to 98 for infants whose mothers consumed >4 pairs. In an interesting report of the concordance of diagnosis
AAP. O'Connor et a1.4' reported a similar result. In twenty- and IQ in twin children of alcoholic mothers, Streissguth and
five 12-month-old infants, mean Bayley MDI decreased DehaeneS3described 16 pairs of twins, both monozygotic and
from 115 with <0.1 AAP to 95 with >1 AAP.
dizygotic. For the most part, the twin pairs were concordant
Similarly, other groups have reported decreases in for diagnosis (i.e., FAS, FAE, or none). Monozygotic twins
MDI/IQ in relation to alcohol exposure. Moderate alcohol were exclusively concordant for diagnosis; and, as would be
use during pregnancy [mean consumption = 0.31 oz abso- expected, there was more variability in the dizygotic twins. In
lute alcohol per day ( M d a y ) ] was related to decreased no case, however, did one twin receive the diagnosis of FAS,
performance on the Bayley in 24-month-old ~ f f s p r i n g . ~whereas
~
the other received no diagnosis. In terms of mental
Furthermore, Coles et a1?* reported a decrease in overall development, the IQ scores for diagnosis-concordant pairs
mental processing on the Kaufman Assessment Battery for differed by an average of 8.1 points, whereas the discordant
Children in a group of children (mean age = 5 years, 10 pairs differed by 12.5 points. In the three pairs of monozygotic
months) whose mothers drank throughout pregnancy twins tested, the mean difference was 4.3 IQ points, and the
(mean consumption = 11.8 M w e e k ) . Importantly, Stre- dizygotic twins differed by an average of 11 points. For this
issguth has continued to find decreases in IQ in relation to sample, the mean IQ for the FAS, FAE, and no diagnosis (but
alcohol exposure as the study population matured. Specif- alcohol-exposed) groups were 69.6, 93.0, and 91.7, respecically, at 4 years of age, exposure to M d a y was related to tively.
a decrease in full-scale IQ of nearly 5 points43and exposure
to 1 M d a y was associated with a 6-point decrement in
full-scale IQ at age 7.44 IQ was not assessed at the 14-year Stability of IQ in Children Exposed to Alcohol Prenatally
follow-up (Streissguth, personal communication, October
The stability of IQ over time in patients with FAS was
1994).
evaluated in a report by Streissguth et al.54 Retest of 17
Importantly, one benefit of prospective studies over ret- patients 1 to 4 years (median interval = 1.75 years) after
NEUROBEHAVIORAL FINDINGS IN FAS
initial evaluation revealed a high correlation between test
and retest IQ scores, although four of these patients
(23.5%) achieved scores >1 SD from their original evaluation (two improved). The mean IQ from the first testing
was 66 (range = 15-99), and the second testing was 67
(range = 10-96). In the 10-year follow-up mentioned previously,6the mean improvement was 9.1 IQ points (range =
1-30), with only one patient (12.5%) improving >1 SD. In
an extension of these earlier studies, Streissguth reported
additional test-retest data of adolescents and adult^.'^ Over
an average test-retest interval of 8.3 years, the correlation
of IQ between testings was 0.78 for FAS patients (n = 27)
and 0.88 for FAE patients (n = 13). The mean IQ scores
were 66.0 (range = 29-105) at initial test and 66.7 (range =
20-91) at retest for the FAS group and 79.5 (range =
56-101) and 82.2 (range = 65-114) for the FAE group. In
all, only 7 of 40 patients (17.5%) were >1 SD from their
previous test performance (five improved). Other reports
of repeated
indicate relatively good stability
of IQ over time, with the most variability in younger patients (see Table 1 for summary). One study indicated
improvement in intellectual functioning over a 3-year peri~ d although
, ~ this
~ may have been due to a few children
who moved from the below average range (70-85) to average range (86-115) of i n t e l l i g e n ~ eIn
. ~the
~ children with
IQ scores in the mentally retarded (<70) and above average ranges (>115), there was no significant change in
performance. Later reports by the same authors suggest
greater stability over longer periods of time.59
WQ vs. PZQ in Individuals with FAS
It has been suggested that FAS is associated with greater
decrements in Verbal I Q (VIQ) than in Performance I Q
(PIQ).60,61However, a review of the studies where this
information is actually available suggests that the results
are equivocal. In eight case reports of individuals with FAS,
four cases16,19,62,63 displayed PIQ > VIQ, with a mean
difference of 8.5 IQ points (range = 3-22). However, six
cases11,56,64,65
demonstrated VIQ > PIQ, and the mean
difference was 17 IQ points (range = 11-26). In two case ~ ,there
~ ~
was, no~ difference
~
between the two subscales.
The average VIQ and PIQ scores from these case reports
are 61.00 (SD = 12.82) and 55.33 (SD = 13.45), respectively. In the 17 group studies of individuals with FAS
where the relevant data were available, 10 studies25,32,33,44,49,50,66-69
indicated no differential effect of prenatal alcohol exposure on verbal versus nonverbal abilities.
although the scores for VIQ and
In one of these
PIQ were equal, PIQ was more affected than VIQ. Howthe opposite was true. PIQ (or
ever, in another
PDI) was greater than VIQ (or MDI) in five group studies,7341,61270,71
whereas VIQ was greater than PIQ in two
s t ~ d i e s .In~ one
~ , ~of~ these studies,71 which has been cited
as evidence for the PIQ-VIQ differential, the FAS and
FAE subjects did in fact display greater PIQ than VIQ
2x7
scores. However, the greatest difference between these two
subscales was in the control group; in fact, PIQ appeared to
be more affected than VIQ when the alcohol-exposed subjects were compared with these controls. It is therefore
unclear whether VIQ is consistently affected to a greater
degree than PIQ in individuals with FAS. It is clear, however, that FAS is related to decreased intellectual functioning with an average IQ between 65 and 75, and that this
level of performance is stable across time. Furthermore this
decrease in performance is also seen in children with prenatal alcohol exposure in the absence of FAS.
OTHER NEUROBEHAVIORAL DOMAINS
The following sections detail the ability levels of children
with FAS in five neurobehavioral domains: activity and
attention, learning and memory, language, motor, and
visuospatial functioning. Studies involving children with
FAS or prenatal alcohol exposure are included, and brief
discussions of animal studies are included when appropriate. The results of neuropsychological studies of children
with FAS are summarized in Table 3.
ACTIVITY AND ATTENTION
Hyperactivity and attentional deficits are hallmark features
of prenatal alcohol exposure. In fact, offspring activity level
may be a more sensitive indicator of alcohols teratogenicity
than physical
Children with FAS have been described as tremulous, hyperactive, and irritable.74Caretakers
note that the children are always on the go, and never sit
In a long-term follow-up of children with FAS, hyperlanetic disorders were among the most frequently diagnosed disorders and persisted throughout ~hildhood?~
In addition, hyperactivity may occur in the absence of intellectual
impairment. One study of 15 alcohol-exposed children of
average intelligence (IQ range = 82-113, mean = 98.2) reported all but one as being hyperactive? Even in the absence
of the diagnosis of FAS, moderate levels of alcohol exposure
(mean = 0.45 AA/day) have caused offspring to be more
fidgety and less ~ompliant?~
Animal models of prenatal alcohol exposure have reiterated and emphasized the effect of maternal alcohol exposure on activity levels in o f f ~ p r i n g .In
~ ~a , review
~~
of the
literature concerning prenatal alcohol and hyperactivity,
Bond77 concluded that, if rats are exposed to alcohol
greater than 6-7 g/kg/day, and are tested prior to 70 days of
age, they exhibit an increase in activity in comparison with
control offspring. Hyperactivity in rats is easily tested in a
variety of ways, and all methods of prenatal treatment and
assessment appear to produce similar results.10778
In addition to hyperactivity, attentional deficits have long
been associated with FAS and prenatal alcohol exposure.
Early naturalistic observations of infants suggested that prenatal alcohol exposure was associated with an increased
nonalert state. That is, the infants spent more time with eyes
288
open, but not attending.79Such deficits in attention appear to
continue through
to those Of
and may be
children with Attention Deficit Disorder (ADD).8oBoth FAS/
FAE and ADD children showed deficits in investing, organizing, and maintaining attention and had an increase in impulsive responses. Similarly, adolescents and adults with FAS
demonstrated deficits in tasks involved in the focusing (Talland Letter Cancellation Test), encoding (WISC-R Digit
Span), and shifting [Wisconsin Card Sorting Test (WCST)] of
attention.8l Alternatively, in an examination of children with
and
with ADD the
performed similarly to controls and better than ADD children on
tests of reaction time and vigilance.
Attentional deficits have also been related to prenatal
alcohol exposure in non-FAS children. Four-year-old children of social drinkers (mean consumption = 0.45 AA/
day during pregnancy, 0.88 AA/day prior to pregnancy)
were observed to have poorer attention spans than control
children when parity, maternal smoking, home environment, and sex of the child were used as covariates.73Streissguth et al.83 also examined 4-year-old children for sustained attention using a continuous performance task.
After covarying maternal smoking, caffeine use, nutrition,
education, and childs birth order, prenatal alcohol exposure was significantly associated with an increase in errors
of omission, commission, and a decrease in the ratio of
correct to total responses. Importantly, in this study the
level of activity did not differ from normal controls,
indicating that hyperactivity did not play a significant role
in the attentional problems noted in this sample. At age 7,
this cohort again demonstrated an increase in reaction
time, and errors of commission and vigilance84;and, at age
11, maternal binge drinking was associated with behavioral
difficulties at school, including hyperactivity and attentional problems.85At age 14, prenatal alcohol exposure was
again related to attentional measures,86 as well as performance on the WISC-R Arithmetic ~ u b t e s twhich
, ~ ~ is commonly thought of as a measure of attention and freedom
from
Streissguths findings of deficits on
attentional measures were supported by Brown et al.,89who
reported deficits in the ability to sustain attention following
alcohol exposure throughout pregnancy.
Not all studies find effects on attention, however. Fried and
colleaguesg0found no relationship between alcohol exposure
and attentional measures at 6 years of age. In fact, there was
a decrease in impulsive responses and maternal perception of
behavior in relation to alcohol exposure. These authors suggest differences between study cohorts and measures as possible reasons for the discrepancies between their findings and
those of Streissguth et al.83Importantly, the alcohol exposure
levels in this cohort were very low. However, Boyd and colleagues also reported no effect of prenatal alcohol exposure
on sustained attention in preschool children of alcoholic
mothers who drank during pregnancy. The alcohol exposure
levels in this study, while still relatively low, were higher than
in the previous study.go
MATSON AND RILEY
LEARNING AND MEMORY
Although learning processes, per se, have not been systematically addressed until recently, learning abilities, broadly
defined, have been described in alcohol-exposed infants and
children. The earliest studies of Streissguth and colleagues
measured early learning and behaviors thought to be related
to learning. In an operant learning study, extinction after
reinforcement of two simple behaviors was measured in newborns exposed to alcohol and nicotine prenatally? Alcohol
and nicotine interacted to produce significantly poorer learning in the infants. In the same sample, decreased habituation
on the Brazelton Scale was related to alcohol use in mid
pregnancy.93Deficits in learning continue to be reported from
the Seattle cohort. Decreased academic achievement and increased parent and teacher ratings of learning problems at 7%
years of age were related to maternal binge drinkinga and
measures associated with learning ~kills.8~
In addition, learning difficulties were also observed in children with IQ scores
within the average range who were born to alcoholic mothers: although this sample was selected from a learning disabilities clinic.
Studies targeting more specific aspects Of learning and
learning
are now being reported*
and memory were assessed in 2o
with FAs.94
When compared with children matched for age, sex, and
race, the children with FAS demonstrated deficits in both
learning and recalling a word list. Their recall was impaired
on both free and recognition recall trials, and they made an
increased number Of intIllSiOn, perseveration, and falsepositive errors. These errOr.5 are COnSiStent with deficits in
response inhibition. However, given their decreased level
Of learning, their retention Of the material Was relatively
intact. This Same pattern Of impaired learning and relatively unimpaired retention was also dtmonstrated in
adults with FAS95and are suggestive of pervasive deficits in
encoding verbal information.
Reports from the Seattle cohort also SukXest a relationship
between memory functioning and Prenatal alcohol exposure.
For example, deficits have been noted in auditory memoIy,8196
memory for stories and designs97and spatial memoryF6 Other reports of spatial memory deficits have been reported in chMren with FAS98 as have deficits on some
measures of working
Alternatively, in the Ottawa
cohort, prenatal alcohol exposure was not related to performance on the memory component of the McCarthy Scales of
Childrens Abilities in 3- or 4-year-old childred or 5- or
6-year-old children.51In addition, prenatal alcohol exposure
was not related to Visual recognition memory in alcoholexposed infants in a study of the Detroit cohort.00
The animal literature is replete with studies of learning
deficits following prenatal alcohol exposure.lo Offspring of
rats given alcohol during gestation show learning deficits
that include active avoidance,75passive avoidance, discrimination and reversal, and taste aversion learning.lo3
Memory deficits have also been reported in rats exposed to
NEUROBEHAVIORAL FINDINGS IN FAS
289
alcohol prenatally. Specifically, deficits in spatial memo- between maternal alcohol use and offspring Word Atry104,105and retention of learned tasks'06 have been re- tack performance at 14 years of age.87Word Attack is a
ported following prenatal alcohol exposure. Other studies, subtest of the Woodcock Reading Mastery Tests and
however, suggest that long-term retention of information involves reading of nonwords. This task requires a
after learning is relatively i n t a ~ t . ~ ' " Whereas
' ~ ~ ' ~ ~a~com- knowledge of pronunciation rules and is related to readplete discussion of the findings of animal studies, as well as ing ability. To summarize, children with FAS appear to
their strengths and limitations, is beyond the scope of this have deficits in speech and language, and similar deficits
paper, several reviews of the literature
are noted in some groups of prospectively identified
alcohol-exposed children.
LANGUAGE
The effects of prenatal alcohol exposure on language
have been mixed. Case reports suggest the presence of
speech and language disturbances resulting from prenatal
alcohol exposure. Abe122lists 53 reports of speech delay or
impediment in 550 FAS cases published between 1973 to
1988. These reports range from complete lack of intelligible
speech"' to mild dysarthria"' or lisping."2 Both receptive
(e.g., Ref. 113) and expressive (e.g., Ref. 114) language
deficits have been noted as have articulation disord e r ~ ~and~ developmental
, ~ ~ , ~ ~
Group studies of language functioning in children with
FAS also find deficits in speech and language functioning
(e.g., Refs. 38 and 118). Reported deficits include word
c o m p r e h e n s i ~ n ,l9~naming
~ , ~ ~ ~ability,'"
~ ~ ~ ~ articulation,"'
and expressive and receptive language skills.68,'21On tests
of verbal fluency, children with FAS display impairments in
letter fluency although category fluency appears to be less
affected.993122
In contrast, a recent report of eight children
with FAS documented relatively intact language development, when compared with controls.'23
In prospective studies of children exposed to varying
amounts of alcohol, however, the results are not as clear. In
a sample of alcohol-exposed children from Ottawa, Canada, decreases in language comprehension were found in
13-m0nth-old,~'2-year-0ld,~'and 3-year-old5' children exposed to relatively low levels of alcohol (mean exposure =
0.31 M d a y for the entire 2-year-old sample, 0.45 M d a y
for the "heavier" exposed group in the 3-year-old sample).
No deficits were found, however, in the same cohort at' ;4
5, or 651years of age. Furthermore, no effect on expressive
or receptive language skills was found in a separate group
of alcohol-exposed children at 1, 2, or 3 years of age.124
Like the Ottawa cohort, this group of children were exposed to relatively low levels of alcohol exposure (mean
exposure = 0.07 M d a y ) .
Other studies have documented effects of alcohol on
language, however. Russell and colleagues67 reported
deficits in offspring receptive language functioning related to indications of maternal problem drinking (e.g.,
an individual's perceptions of what others think about
their drinking or reported alcohol-related family problems). This same report also documented deficits in
WPPSI Verbal IQ, which has a significant language component. Finally, a recent report from the Seattle prospective study demonstrated a dose-response relationship
MOTOR ABILITIES
In addition to alcohol's effects on higher level cognitive
functions, there is also an effect on the developing motor
system. Although a few studies find no effect of prenatal
alcohol on motor d e v e l ~ p m e n t , ~ ~most
- ~ ~studies
. ' ~ ~ of motor development and motor skills suggest an effect of prenatal alcohol exposure. Early descriptions of children of
chronic alcoholic mothers3 reported delayed motor development and fine-motor dysfunction. One report noted a
"nonspecific dyscoordinated motor pattern," hemiplegia,
ataxia, and an increase in cerebral palsy in children of
alcohol abusing women.29Later studies also noted delayed
motor development in infants and children exposed to
alcohol prenatall~9,'00,'26and fine- and gross-motor dysfunctions were noted in children of alcoholic mothers127
and social drinkers.12' In addition, Marcus'" noted axial
ataxia and kinetic tremor in children with FAS. Finally,
several reports exist of deficits in motor speed/precision,
finger tapping speed, and grip strength in children with
~~s.68~71~119
Animal models have also provided evidence for motor
dysfunction following prenatal alcohol exposure. Gait dist u r b a n c e ~ , 'delays
~~
in reflex de~elopment,'~'and poor
balan~e'~'
have all been reported in rats exposed to alcohol
during the perinatal period.
VlSUOSPATlAL ABILITIES
Visuospatial abilities in children with FAS have not been
well documented. Many studies report deficits in simple
drawing tasks like the Beery Developmental Test of Visual
Motor I n t e g r a t i ~ n ~ ~ and
, ~ ~the
, ~ Frostig
~ , " ~ Developmental
Test of Visual P e r ~ e p t i o n ~ ~ ~however,
" ~ , ' ~ ~ ;very few studies have addressed more complex visuospatial abilities in
FAS. As mentioned previously, spatial memory appears to
be impaired in children with FAS.81,96,98
Interestingly, the
study of Uecker and Nadel suggested deficits in memory
for the location of objects but not for the objects themselves. In addition, this study documented alcohol-associated deficits in clock drawing, a traditional measure of
visuospatial ability.133In a recent
of more specific
visuospatial ability, children with FAS displayed deficits in
local processing of hierarchical stimuli. These children
were impaired in recalling and copying local (details) but
not global (configural) features of the stimuli. These defi-
92 adolescents and adults with FAS/
FAE
16 FAS Ss with borderline (6) or
normal (10) IQ
8 children with FAS and cpntrols
LaDue, Streissguth, &
Randels"
Don, Kerns, Mateer, &
Streissguthg5
Ernhart, Greene, Sokol,
Martier, Boyd, & AgerlZ3
Kodituwakku, Handmaker,
Cutler, Weathersby, &
HandmakePg
15 children with FAS and controls
Children with alcohol exposure (25
dysmorphic, 62 nondysmorphic),
ADHD. and controls
20 children with FAS and controls
Uecker & NadeIg8
Coles, Platzman, RanskindHood, Brown, Falek, &
Smith"
Mattson, Riley, Delis, Stern, &
Jonesg4
Mattson, Gramling. Delis,
Jones, & Riley134
Mattson, Riley, Gramling,
Delis, & Joneslig
CVLT-C, PPVT-R, Boston Naming Test, Grooved
Peg Board Test, Children's Category Test, WRATR, VMI
Global-Local Test
-/+
-/+
-/+
-/+
LearningIMemory
Attention
+/-
Language
Motor
-/+
Visuospatiai
+/-
Other
Test-Children's Version.
assessments were conducted in this area and deficits were reported.
Ss, Subjects; PPVT-R, Peabody Picture Vocabulary Test-Revised; ADHD, attention deficit hyperactive disorder; K-ABC, Kaufman Assessment Battery for Children; CVLT-C, California Verbal Learning
+, assessments were conducted in this area and no deficits were reported; -,
14 children with FASIPEA and
controls
15 children with FAS; 10 children
with PEA; and controls
10 preschoolers with FAS and
controls
Janzen, Nanson, & Block6'
10 FASIFAE children and controls
Adolescents and adults with FAS
Carmichael Olson, Sampson,
Barr, Streissguth, &
BooksteinS5
Sequenced Inventory of Communication
Development
Raven's Standard Progressive Matrices, PPVT-R,
Wide Range Assessment of Memory and
Learning, Attentional Capacity Test, Progressive
Planning Test, Delayed Response Tasks,
Controlled Oral Word Association Test, SubjectOrdered Task, WCST, Competing Motor Programs
(go-no-go)
McCarthy Scales of Children's Abilities, Grooved
Peg Board Test, VMI, Recognition-Discrimination
Test, Test of Early Language Development
Memory for 16 Objects task, VMI, K-ABC Facial
Recognition Test, Draw-a-Clock test, WISC-R
Mazes
WISC-R Coding, K-ABC Number Recall, Paired
Associate Memory Task, CPT (including simple
reaction time and vigilance measures), WCST
CVLT-C
20 FASlFAE Ss vs. ADD and
controls
7 adults with FASIFAE and controls
Nanson & Hiscock''
Gray & Streissguthg6
Tests
Frostig Test of Visual Perception, Illinois Test of
Psycholinguistic Abilities
Frostig Test of Visual Perception, Human Figure
Drawing Test
Peabody Picture Vocabulary Test-Revised (PPVT-R),
Expressive One Word Picture Vocabulary Test,
Finger Tapping, Grip Strength, Finger Localization,
Reaction Time, Motor Speed and Precision Test,
Beery's Developmental Test of Visual Motor
Integration (VMI)
Choice Reaction Time Test, Delay Reaction Time
Test, Vigilance Test
Stepping Stone Maze, Seashore Rhythm Test,
Dynamic Visual Retention Test, Memory for Faces,
PPVT-R, Wechsler Memory Scale
Digit Span, Seashore Rhythm Test, Stepping Stone
Maze, Nissen Serial Reaction Time Test,
Wisconsin Card Sorting Test (WCST), Continuous
Performance Test (CPT), Talland Letter
Cancellation Test
PPVT-R, Wide Range Achievement Test-Revised
(WRAT-R)
California Verbal Learning Test (CVLT) and others
Subjects
32 children (from a larger sample)
with FAS
21 children of 30 alcoholic women
(10 with FAS) and controls
19 Ss with FAS (13) or FAE (6) and
controls
Authors
Steinhausen, Nestler, &
Spohr' l6
Aronson, Kyllerman, Sabel,
Sandin, & OlegArd32
conry71
Table 3. Summary of Neuropsychological Findings in Children with FAS, Presented in Chronological Order Through 1996
<
m
r
-2=
NEUROBEHAVIORAL FINDINGS IN FAS
cits were not due to the size of the stimuli or to deficits in
memory, and suggested a specific impairment in processing
local features of hierarchical visual information. Similar
deficits have been noted in other d e ~ e l o p m e n t a l and
~~
d e m e n t i ~ ~ disorders.
g~~
OTHER NEUROPSYCHOLOGICAL ABILITIES
In addition to the abilities already discussed, a few studies have documented other specific neuropsychological deficits in individuals with FAS. The WCST is a test of nonverbal problem solving, which requires both problem
solving and cognitive flexibility, and has been proposed to
be sensitive to frontal system dysfunction. Adolescents and
adults with FAS display decreased accuracy,81 achieve
fewer categories, and make more perseverative responses99
on the WCST. Alternatively, the computerized version of
the WCST was found to be only moderately sensitive to
prenatal alcohol exposure in the 14-year assessment of the
Seattle cohort.s6 Our data suggest that, whereas children
with FAS perform more poorly than controls, these deficits
are considerably less severe than we would expect, given
their overall level of ability (i.e., IQ).i37
Finally, tests of planning ability are also thought to be
sensitive to frontal systems dysfunction, although few such
studies have been done in individuals with FAS. On the
Progressive Planning Testy9 which is similar to the Tower
of London Test, children with FASFAE had difficulty
with planning ahead and tended to perseverate on incorrect
strategies.
SUMMARY
In summary, FAS is a devastating developmental disorder that is associated with a wide variety of neurobehavioral
deficits. Studies of FAS have documented consistent deficits in language, motor, learning, and visuospatial functioning. Memory seems to also be affected; however, studies
that include a comparison of learning and recall suggest
that, at least in the verbal domain, retention is fairly normal. That is, learning deficits (i.e., encoding) may be at the
root of observed memory deficits and that once information is learned it can be retained. In addition, most studies
of attention suggest deficits in this domain, although the
study of Coles et a1.82 suggests that further, more specific
evaluation of the components of attention is necessary. In
addition, visuospatial functioning and problem solving are
two, as yet, understudied areas in FAS. Existing studies
suggest deficits in simple visuospatial functioning, but more
complex abilities are yet to be described. Similarly, several
studies show deficits on the WCST, although it is unclear
how these deficits relate to overall cognitive ability. Many
of these deficits have been supported by cohort studies that
provide invaluable information about the role of prenatal
alcohol exposure in the development of neurobehavioral
abilities. Future research is required to more clearly delin-
291
eate whether areas of relative strength or weakness exist in
children with FAS and how their cognitive abilities relate to
other types of mental retardation. In addition, correlation
of neuropsychological and neuroanatomical data may help
us understand the role of abnormal brain development in
cognitive ability. Taken together, results from these two
types of studies can help provide the background for educational and training programs specific to individuals with
FAS or prenatal alcohol exposure.
REFERENCES
1. Warner RH, Rosett H L The effects of drinking on offspring.
J Stud Alcohol 36:1395-1420, 1975
2. Lemoine P, Harousseau H, Borteyru J-P, Menuet J-C: Les enfants
de parents aicooliques: Anomalies observkes. A proposos de 127 cas
[Children of alcoholic parents: Abnormalities observed in 127 cases].
Ouest Med 21:476-482, 1968
3. Jones KL, Smith DW, Ulleland CN, Streissguth AP:Pattern of
malformation in offspring of chronic alcoholic mothers. Lancet 1:12671271, 1973
4. Jones KL, Smith DW: Recognition of the fetal alcohol syndrome
in early infancy. Lancet 2:999-1001, 1973
5. Abel EL, Sokol RJ: A revised conservative estimate of the incidence of FAS and its economic impact. Alcohol Clin Exp Res 15:514-524,
1991
6. Streissguth AP,Clarren SK, Jones KL: Natural history of the fetal
alcohol syndrome: A 10 year follow-up of eleven patients. Lancet 2:85-91,
1985
7. Streissguth AP,Aase JM, Clarren SK, Randels SP, LaDue RA,
Smith DF: Fetal alcohol syndrome in adolescents and adults. JAh4A
265:1961-1967, 1991
8. Streissguth AP: The behavioral teratology of alcohol: Performance, behavioral, and intellectual deficits in prenatally exposed children,
in West JR (ed): Alcohol and Brain Development. New York, Oxford,
1986, pp 3-44
9. Abel EL, Sokol RJ: Incidence of fetal alcohol syndrome and
economic impact of FAS-related anomalies. Drug Alcohol Depend 195170, 1987
10. Meyer LS,Riley EP: Behavioral teratology of alcohol, in Riley EP,
Vorhees CV (eds): Handbook of Behavioral Teratology. New York, Plenum Press, 1986, pp 101-140
11. Palmer RH, Ouellette EM, Warner L, Leichtman SR: Congenital
malformations in offspring of a chronic alcoholic mother. Pediatrics 53:
490-494, 1974
12. Root AW, Reiter EO, Andriola M, Duckett G: Hypothalamicpituitary function in the fetal alcohol syndrome. J Pediatr 87585-588,
1975
13. Kousseff B: KI-A possible new syndrome. Birth Defects 11:
459-463, 1975
14. Majewski F, Bierich J, Loeser H, Michaelis R, Leiber B, Bettecken
F: Zur Klinik und pathogenese der alkohol-embryopathie. Bericht uber 68
falle [Diagnosis and pathogenesis of alcohol embryopathy: Report of 68
cases]. Munchener Medizinische Wochenschrift 118:1635-1642,1976
15. Majewski F, Majewski B: Alcohol embryopathy: Symptoms, auxological data, frequency among the offspring and pathogenesis, in
Kuriyama K, Takada A, Ishii H (eds): Biomedical and Social Aspects of
Alcohol and Alcoholism. Elsevier Science Publishers, 1988, pp 837-844
16. Char F: Fetal alcohol syndrome with Noonan phenotype. Birth
Defects 12:81-82, 1976
17. Ballesta F, Cruz M: Sindrome alcoholico fetal y alteraciones
cromosomicas [Fetal alcohol syndrome and chromosome aberrations].
Arch Pediatr 29:435-443, 1978
18. Qazi QH, Madahar C, Masakawa A, McGann B: Chromosome
abnormality in a patient with fetal alcohol syndrome, in Galanter M (ed):
292
MATTSON AND RILEY
Currents in Alcoholism, vol 5. New York, Grunc & Stratton, 1979, pp A Effects of prenatal alcohol exposure at school age. I. Physical and
155-1 61
cognitive development. Neurotoxicol Teratol 13:357-367, 1991
43. Streissguth AP,Barr HM, Sampson PD, Darby BL, Martin DC:
19. Slavncy PR, Grdu JG: Fetal alcohol damage and schizophrenia.
IQ at age 4 in rclation to maternal alcohol use and smoking during
J Clin Psychiatry 39:782-783, 1978
pregnancy. Dev Psycho1 25:3-11, 1989
20. Neidengard L, Carter TE. Smith DW: Klippel-Feil malformation
44. Streissguth AP,Barr HM, Sampson PD: Moderate prenatal alcocomplex in fetal alcohol syndrome. Am J Dis Children 132:929-930, 1978
21. Qazi Q, Masakawa A, Milman D, McGann B, Chua A, Haller J: hol exposure: Effects on child IQ and learning problems at age 7% years.
Renal anomalies in fetal alcohol syndrome. Pediatrics 63:886-889, 1979 Alcohol Clin Exp Res 14:662-669, 1990
45. Goodlett CR, Lundahl KR: Temporal determinants of neonatal
22. Abcl EL: Fctal Alcohol Syndromc. New Jersey, Mcdical Economalcohol-induced cerebellar damage and motor performance deficits. Pharics Company, Inc., 1990
23. Ticha R, Santavy J, Matlocha Z: Fetal alcohol syndrome: Amino macol Biochcm Behav 55531-540, 1996
46. Thomas JD, Wasserman EA, West JR, Goodlett CR: Behavioral
acid pattern. Acta Paediatr Hungar 24:143-148, 1983
24. Aronson M, Olegird R: Fetal alcohol effects in pediatrics and deficits induced by bingelike exposure to alcohol in neonatal rats: Imporchild psychology, in Rydberg U (ed): Alcohol and the Developing Brain. tance of developmental timing and number of episodes. Dev Psychobiol
29:433-452, 1996
New York, Raven Press, 1985, pp 135-145
47. Clarren SK, Astley SJ, Gunderson VM, Spellman D: Cognitive
25. Strcissguth AP, Rohsenow DJ: Intellectual development in offand
behavioral deficits in nonhuman primates associated with very early
spring of chronic alcoholic mothers and matched controls. Paper prcembryonic binge exposures to ethanol. J Pediatr 121:789-796, 1992
sented at the Western Psychological Association, San Francisco, 1974
48. Goldschmidt L, Richardson GA, Stoffer DS, Geva D, Day NL:
26. Streissguth AP,Herman CS, Smith DW: Intelligence, behavior,
and dysmorphogenesis in the fetal alcohol syndrome: A report on 20 Prenatal alcohol exposure and academic achievement at age six: A nonlinear fit. Alcohol Clin Exp Res 20:763-770, 1996
patients. J Pediatr 92:363-367, 1978
49. Forrest F, Florey C du V, Taylor D, McPherson F, Young JA:
27. Majewski F: Uber schadigende einfliisse des alkohols auf die
nachkommen [The damaging effects of alcohol on offspring]. Der Nerve- Reported social alcohol consumption during pregnancy and infants development at 18 months. Br Med J 303:22-26, 1991
narzt 49:410-416, 1978
50. Fried PA, Watkinson B: 36- and 48-month neurobehavioral fol28. Majewski F: Unterzuchungen zur alkohol-embryopathie [Studies
low-up of children prenatally exposed to marijuana, cigarettes, and alcoon alcohol embryopathy]. Fortschritte der Medizin 96:2207-2213, 1978
hol. J Dev Behav Pediatr 11:49-58, 1990
29. Oleglrd R, Sabel K-G, Aronsson M, Sandin B, Johansson PR,
51. Fried PA, OConnell CM, Watkinson B: 60- and 72-month folCarlsson C, Kyllerman M, Iversen K, Hrbek A: Effects on the child of
low-up of children prenatally exposed to marijuana, cigarettes, and alcoalcohol abuse during pregnancy. Acta Paediatr Scand 275:112-121, 1979
hol: Cognitive and language assessment. J Dev Behav Pediatr 13:383-391,
30. Shaywitz SE, Cohen DJ, Shaywitz BA: Behavioral learning diffi1992
culties in children of normal intelligence born to alcoholic mothers. J Pe52. Greene T, Ernhart CB, Ager J, Sokol R, Martier S, Boyd T:
diatr 96978-982, 1980
Prenatal alcohol exposure and cognitive development in the preschool
31. Iosub S, Fuchs M, Bingol N, Gromisch DS: Fetal alcohol synyears. Neurotoxicol Teratol 1357-68, 1991
drome revisited. Pediatrics 68:475-479, 1981
53. Streissguth AP,Dehaene P: Fetal alcohol syndrome in twins of
32. Aronson M, Kyllerman M, Sabel K-G, Sandin B, Olegird R:
alcoholic mothers: Concordance of diagnosis and IQ. Am J Med Genet
Children of alcoholic mothers: Developmental, perceptual, and behav- 47357-861, 1993
ioural characteristics as compared to matched controls. Acta Pzdiatr
54. Streissguth AP,Herman CS, Smith D W Stability of intelligence in
Scand 74:27-35, 1985
the fetal alcohol syndrome: A preliminary report. Alcohol Clin Exp Res
33. Mattson SN, Riley EP, Gramling L, Delis DC, Jones KL: Heavy 2:165-170, 1978
prenatal alcohol exposure with or without physical features of fetal alcohol
55. Van Biervliet JP: The foetal alcohol syndrome. Acta Paediatr Belg
syndrome leads to IQ deficits. J Pediatr 131:718-721, 1997
30~113-116,1977
34. Streissguth AP, Randels SP, Smith DF: A test-retest study of
56. Iosub S, Fuchs M, Bingol N, Stone RK, Gromisch DS: Long-term
intelligence in patients with fetal alcohol syndrome: Implications for care. follow-up of three siblings with fetal alcohol syndrome. Alcohol Clin Exp
J Am Acad Child Adolesc Psychiatry 30584-587, 1991
Res 5523-527, 1981
35. Streissguth AP,Barr HM, Sampson PD, Bookstein FL: Prenatal
57. Steinhausen H-C, Gobel D, Nestler V: Psychopathology in the
alcohol and offspring development: The first fourteen years. Drug Alcohol offspring of alcoholic parents. J Am Acad Child Psychiatry 23:465-471,
Depend 36:89-99, 1994
1984
36. Golden NL, Sokol RJ, Kuhnert BR, Bottoms S: Maternal alcohol
58. Spohr H-L, Steinhausen H-C Clinical, psychopathological and
use and infant development. Pediatrics 70:931-934, 1982
developmental aspects in children with the fetal alcohol syndrome: A
37. Ioffe S, Chernick V: Prediction of subsequent motor and mental four-year follow-up study, in Ciba Foundation Symposium: Mechanisms of
retardation in newborn infants exposed to alcohol in utero by computer- Alcohol Damage In Utero. London, Pitman, 1984, pp 197-211
ized EEG analysis. Neuropediatrics 21:11-17, 1990
59. Steinhausen H-C, Willms J, Spohr H-L Long-term psychopatho38. Autti-Ram0 I, Korkman K, Hilakivi-Clarke L, Lehtonen M, logical and cognitive outcome of children with fetal alcohol syndrome.
Halmesmaki E, Granstrom M-L: Mental development of 2-year-old chil- J Am Acad Child Adolesc Psychiatry 32:990-994, 1993
dren exposed to alcohol in utero. J Pediatr 120:740-746, 1992
60. Don A, Rourke BP: Fetal alcohol syndrome, in Rourke BP (ed):
39. Streissguth AP,Barr HM, Martin DC, Herman CS: Effects of Syndrome of Nonverbal Learning Disabilities: Neurodevelopmental Manmaternal alcohol, nicotine, and caffeine use during pregnancy on infant ifestations. New York, Guilford Press, 1995, pp 372-406
mental and motor development at eight months. Alcohol Clin Exp Res
61. LaDue RA, Streissguth AP,Randels SP: Clinical considerations
4152-164, 1980
pertaining to adolescents and adults with fetal alcohol syndrome, in Son40. OConnor MJ, Brill NJ, Sigman M: Alcohol use in primiparous deregger TB (ed): Perinatal Substance Abuse: Research Findings and
women older than 30 years of age: Relation to infant development.
Clinical Implications. Baltimore, Johns Hopkins Press, 1992, pp 104-131
Pediatrics 78:444-450, 1986
62. Usowicz AG, Golabi M, Curry C: Upper airway obstruction in
41. Fried PA, Wathnson B: 12- and 24-month neurobehavioural fol- infants with fetal alcohol syndrome. Am J Dis Children 140:1039-1041,
low-up of children prenatally exposed to marihuana, cigarettes and alco- 1986
hol. Neurotoxicol Teratol 10:305-313, 1988
63. Mattson SN, Riley EP, Jernigan TL, Ehlers CL, Delis DC, Jones
42. Coles CD, Brown RT, Smith IE, Platzman KA, Erickson S, Falek KL, Stern C, Johnson KA, Hesselink JR, Bellugi U: Fetal alcohol syn-
NEUROBEHAVIORAL FINDINGS IN FAS
drome: A case report of neuropsychological, MRI, and EEG assessment
of two children. Alcohol Clin Exp Rcs 16:lOOl-1003. 1992
64. Naselli A, De Toni T, Vignolo M, Di Battista E, Aicardi G:
Auxological findings and endocrine function in a case of fetal alcohol
syndrome. Acta Med Auxolog 14:23-30, 1982
65. Harris SR, MacKay LLJ, Osborn JA: Autistic behaviors in offspring of mothers abusing alcohol and other drugs: A series of case
reports. Alcohol Clin Exp Res 19:660-665. 1995
66. Coles CD, Smith IE, Falek A: Prenatal alcohol exposure and
infant behavior: Immediate effects and implications for later development.
Adv Alcohol Subst Abuse 697-104, 1987
67. Russell M, Czarnecki DM, Cowan R, McPherson E, Mudar PJ:
Measures of maternal alcohol use as predictors of development in early
childhood. Alcohol Clin Exp Res 15:991-1000, 1991
68. Janzen LA, Nanson JL, Block GW: Neuropsychological evaluation of preschoolers with fetal alcohol syndrome. Neurotoxicol Teratol
17:273-279, 1995
69. Larroque B, Kaminski M, Dehaene P, Subtil D, Delfosse M-J,
Querleu D: Moderate prenatal alcohol exposurc and psychomotor development at preschool age. A m J Public Health 85:1654-1661, 1995
70. Gusella JL, Fried PA: Effects of maternal social drinking and
smoking on offspring at 13 months. Neurobehav Toxicol Teratol6:13-17,
1984
71. Conry J: Neuropsychological deficits in fetal alcohol syndrome
and fetal alcohol effects. Alcohol Clin Exp Res 14:650-655, 1990
72. Jacobson JL, Jacobson SW, Sokol RJ, Martier SS, Ager JW,
Kaplan-Estrin MG: Teratogenic effects of alcohol on infant development.
Alcohol Clin Exp Res 17:174-183, 1993
73. Landesman-Dwyer S, Ragozin AS, Little RE: Behavioral correlates of prenatal alcohol exposure: A four-year follow-up study. Neurobehav Toxicol Teratol 3:187-193, 1981
74. Hanson JW, Jones KL, Smith DW: Fetal alcohol syndrome: Experience with 41 patients. JAMA 235:1458-1460, 1976
75. Bond NW,DiGiusto EL: Avoidance conditioning and Hebb-Williams maze performance in rats treated prenatally with alcohol. Psychopharmacology 58:69-71, 1978
76. Ulug S, Riley EP: The effect of methylphenidate on overactivity in
rats prenatally exposed to alcohol. Neurobehav Toxicol Teratol 5:35-39,
1983
77. Bond NW: Prenatal alcohol exposure in rodents: A review of its
effects on offspring activity and learning ability. Austral J Psychol 33:331344, 1981
78. Bond NW: Behavioural teratology: Fetal alcohol exposure and
hyperactivity, in Bond NW (ed): Animal Models in Psychopathology.
Sydney, Academic Press, 1984, pp 279-311
79. Landesman-Dwyer S, Keller LS, Streissguth AP:Naturalistic observations of newborns: Effects of maternal alcohol intake. Alcohol Clin
Exp Res 2171-177, 1978
80. Nanson JL, Hiscock M: Attention deficits in children exposed to
alcohol prenatally. Alcohol Clin Exp Res 14:656-661, 1990
81. Carmichael Olson H, Feldman JJ, Streissguth AP,Gonzalez RD:
Neuropsychological deficits and life adjustment in adolescents and adults
with fetal alcohol syndrome. Alcohol Clin Exp Res 16:380, 1992
82. Coles CD, Platzman KA, Raskind-Hood CL, Brown RT, Falek A,
Smith I E A comparison of children affected by prenatal alcohol exposure
and attention deficit, hyperactivity disorder. Alcohol Clin Exp Res 21:
150-161, 1997
83. Streissguth AP,Martin DC, Barr HM, Sandman BM, Kirchner
GL, Darby B L Intrauterine alcohol and nicotine exposure: Attention and
reaction time in 4-year old children. Dev Psychol 20:53>541, 1984
84. Streissguth AP, Barr HM, Sampson PD, Parrish-Johnson JC,
Kirchner GL, Martin DC: Attention, distraction and reaction time at age
7 years and prenatal alcohol exposure. Neurobehav Toxicol Teratol8:717725, 1986
85. Carmichael Olson H, Sampson PD, Barr H, Streissguth AP,Bookstein F L Prenatal exposure to alcohol and school problems in late childhood: A longitudinal prospective study. Dev Psychopath014:341-359,1992
2Y.7
86. Streissguth AP, Sampson PD, farmichacl Olson 1i. Bookstcin FL.
Barr HM, Scott M, Feldman J, Mirsky AF: Maternal drinking during
pregnancy: Attention and short-term memory in 14-year old offspring-A
longitudinal prospective study. Alcohol Clin Exp Rcs 18:202-218. I994
87. Streissguth AP,Barr HM, Carmichael Olson H, Sampson PD.
Bookstein FL, Burgess DM: Drinking during pregnancy dccrcascs word
attack and arithmetic scorcs on standardized tests: Adolcsccnt data from
a population-based prospective study. Alcohol Clin Exp Rcs 18:238-251.
1994
88. Sattler JM: Assessmcnt of Childrcn. San Dicgo. Jcromc M. Sattler, 1992
89. Brown RT, Coles CD, Smith IE. Platzman KA, Silvcrstcin J.
Erickson S, Falck A: Effccts of prenatal alcohol cxposurc at school age. 11.
Attention and behavior. Neurotoxicol Teratol 13:369-376. 1991
90. Fried PA, Watkinson B, Gray R: A follow-up study of attcntional
behavior in 6-year-old children cxposed prenatally to niarihuana, cigarettes, and alcohol. Neurotoxicol Tcratol 14:299-311, 1992
91. Boyd TA, Ernhart CB, Greene TH, Sokol RJ, Martier S: Prcnatal
alcohol exposure and sustained attention in the preschool years. Ncurotoxicol Teratol 13:49-55, 1991
92. Martin J, Martin DC. Lund CA, Streissguth AP: Matcrnal alcohol
ingestion and cigarette smoking and their cffccts on ncwborn conditioning. Alcohol Clin Exp Res 1:243-247, 1977
93. Streissguth AP,Barr HM, Martin DC: Matcrnal alcohol use and
neonatal habituation asscsscd with the Brazclton scalc. Child Dev 54:
1109-1118, 1983
94. Mattson SN, Riley EP, Dclis DC, Stern C, Jones KL: Verbal
learning and memory in children with fctal alcohol syndrome. Alcohol
CIin Exp Res 20510-816, 1996
95. Don A, Kerns K, Matecr CA, Streissguth AP:Cognitive deficits in
normal IQ and borderline IQ adults with fetal alcohol syndrome. Alcohol
Clin Exp Res 17:458, 1993
96. Gray JK, Streissguth AP:Memory deficits and life adjustment in
adults with fetal alcohol syndrome: A case control study. Alcohol Clin Exp
Res 14:294, 1990
97. Streissguth AP,Bookstein FL, Sampson PD, Barr HM: Ncurobehavioral effects of prenatal alcohol. Part 111. PLS analyses of ncuropsychologic tests. Neurotoxicol Teratol 11:493-507, 1989
98. Uecker A, Nadel L: Spatial locations gone awry: Objcct and
spatial memory deficits in children with fetal alcohol syndrome. Ncuropsychologia 34:209-223, 1996
99. Kodituwakku PW, Handmaker NS, Cutler SK, Weathersby EK.
Handmaker SD: Specific impairments in self-regulation in children cxposed to alcohol prenatally. Alcohol Clin Exp Res 19:1558-1564, 1995
100. Jacobson SW, Jacobson JL, Sokol RJ, Martier SS, Ager JW:
Prenatal alcohol exposure and infant information processing ability. Child
Dev 64:1706-1721, 1993
101. Riley EP, Lochry EA, Shapiro NR: Lack of response inhibition in
rats prenatally exposed to alcohol. Psychopharmacology 62:47-52, 1979
102. Anandam N, Stern JM: Alcohol in utero: Effects on preweanling
appetitive learning. Neurobehav Toxicol 2:199-205, 1980
103. Driscoll CD, Riley EP, Mcyer LS:Delayed taste aversion learning
in preweanling rats exposed to alcohol prenatally. Alcohol 2:277-280, 1985
104. Gianoulakis C: Rats exposed prenatally to alcohol exhibit impairment in spatial navigation test. Behav Brain Res 36:217-228, 1990
105. Reyes E, Wolfe J, Savage DD: The effects of prenatal alcohol
exposure on radial arm maze performance in adult rats. Physiol Behav
46~45-48, 1989
106. Lochry EA, Riley EP: Retention of passive avoidance and T-maze
escape in rats exposed to alcohol prenatally. Neurobehav Toxicol 2:107115, 1980
107. Hall JL, Church MW, Berman RF: Radial arm maze deficits in
rats exposed to alcohol during midgestation. Psychobiology 22:181-185,
1994
108. Driscoll CD, Streissguth AP,Riley EP: Prenatal alcohol exposure:
Comparability of effects in humans and animal models. Neurotoxicol
Teratol 12231-237, 1990
294
109. Becker HC, Randall CL, Salo AL, Saulnier JL, Weathersby RT:
Animal research: Charting the course for FAS. Alcohol Health Res World
18:lO-16, 1994
110. Tsukahara M, Kajii T: Severe skeletal dysplasias following intrauterine exposure to ethanol. Teratology 37:79-80, 1988
111. Marcus JC: Neurological findings in the fetal alcohol syndrome.
Neuropediatrics 18:158-160, 1987
112. Koranyi G, Csiky E: Az embryopathia alcoholica gyermekkorban
eszlelheto tuneteirol [Signs of alcohol embryopathy apparent in childhood]. Orvosi Hetilap 119:2923-2929, 1978
113. Shaywitz SE, Caparulo BK, Hodgson ES: Developmental language disability as a consequence of prenatal exposure to ethanol. Pediatrics 685350-855, 1981
114. Tenbrinck MS, Buchin SY: Fetal alcohol syndrome: Report of a
case. JAMA 232:1144-1147, 1975
115. Church MW, Gerkin KP: Hearing disorders in children with fetal
alcohol syndrome: Findings from case reports. Pediatrics 82147-154,1988
116. Collins E, Turner G: Six children affected by maternal alcoholism.
Med J Austral 2:606-608, 1978
117. Seeler RA, Israel JN, Royal JE, Kaye CI, Rao S, Abulaban M:
Ganglioneuroblastoma and fetal hydantoin-alcohol syndromes. Pediatrics
631524-527, 1979
118. Steinhausen H-C, Nestler V, Spohr H - L Development and psychopathology of children with the fetal alcohol syndrome. J Dev Behav
Pediatr 3:49-54, 1982
119. Mattson SN, Riley EP, Gramling L, Delis DC, Jones KL: Neuropsychological comparison of alcohol-exposed children with or without
physical features of fetal alcohol syndrome. Neuropsychology 12:146-153,
1998
120. Becker M, Warr-Leeper GA, Leeper HA: Fetal alcohol syndrome:
A description of oral motor, articulatory, short-term memory, grammatical, and semantic abilities. J Commun Disord 23:97-124, 1990
121. Carney LJ,Chermak GD: Performance of American Indian children with fetal alcohol syndrome on the test of language development.
J Commun Disord 24123-134, 1991
122. Mattson SN: The Role of the Basal Ganglia in the Behavioral
Teratogenicity of Alcohol. San Diego, SDSURJCSD Joint Doctoral Program in Clinical Psychology, 1994, pp 144
123. Ernhart CB, Greene T, Sokol RJ,Martier S, Boyd TA, Ager J:
Neonatal diagnosis of fetal alcohol syndrome: Not necessarily a hopeless
prognosis. Alcohol Clin Exp Res 19:1550-1557, 1995
124. Greene T, Ernhart CB, Martier S, Sokol R, Ager J: Prenatal
alcohol exposure and language development. Alcohol Clin Exp Res 14:
937-945, 1990
125. Chandler LS, Richardson GA, Gallagher JD, Day N L Prenatal
exposure to alcohol and marijuana: Effects on motor development of
preschool children. Alcohol Clin Exp Res 20:455-461, 1996
126. Autti-Ramo I, Granstrom M-L: The psychomotor development
during the first year of life of infants exposed to intrauterine alcohol of
various duration. Neuropediatrics 22:59-64, 1991
127. Kyllerman M, Aronson M, Sabel K-G, Karlberg E, Sandin B,
Olegird R: Children of alcoholic mothers: Growth and motor performance compared to matched controls. Acta Paediatr Scand 7420-26,
1985
128. Barr HM, Streissguth AP, Darby BL, Sampson PD: Prenatal
exposure to alcohol, caffeine, tobacco, and aspirin: Effects on fine and
gross motor performance in 4-year-old children. Dev Psycho1 26:339-348,
1990
129. Hannigan JH, Riley EP: Prenatal ethanol alters gait in rats. Alcohol 5~451-454,1989
130. Lee MH, Haddad R, Rabe A: Developmental impairments in the
M A T S O N AND RILEY
progeny of rats consuming ethanol during pregnancy. Neurobehav Toxicol
2:189-198, 1980
131. Meyer LS, Kotch LE, Riley EP: Neonatal ethanol exposure: Functional alterations associated with cerebellar growth retardation. Neurotoxic01 Teratol 12:15-22, 1990
132. Aronson M, Olegird R: Children of alcoholic mothers. Pediatrician 1457-61, 1987
133. Spreen 0, Strauss E: A Compendium of Ncuropsychological
Tests. New York, Oxford University Press, 1991
134. Mattson SN, Gramling L, Delis DC, Jones KL, Riley EP: Globallocal processing in children prenatally exposed to alcohol. Child Neuropsycho1 2:165-175, 1996
135. Bihrle AM, Bellugi U, Delis D, Marks S: Seeing either the forest
or the trees: Dissociation in visuospatial processing. Brain Cogn 11:37-49,
1989
136. Delis DC, Massman PJ, Butters N, Salmon DP, Shear PK, Dernadura T, Filoteo JV: Spatial cognition in Alzheimer's disease: Subtypes of
global-local impairment. J Clin Exp Neuropsychol 14:463-477, 1992
137. Mattson SN, Roebuck TM, Riley EP: Wisconsin card sorting
performance in children prenatally exposed to alcohol. Alcohol Clin Exp
Res 20:74A, 1996
138. Shallice T, Burgess P: Higher-order cognitive impairments and
frontal lobe lesions in man, in Levin HS, Eisenberg HM, Benton AL (eds):
Frontal Lobe Function and Dysfunction. New York, Oxford University
Press, 1991, pp 125-138
139. Mulvihill JJ, Klimas JT, Stokes DC, Risemberg HM: Fetal alcohol
syndrome: Seven new cases. Am J Obstet Gynecol 125:937-941, 1976
140. Bierich JR, Majewski F, Michaelis R, Tillner I: Uber das embryofetale alkoholsyndrom [On the embryofetal alcohol syndrome]. Eur J Pediatr 121:155-177, 1976
141. Ijaiya K, Schwenk A, Gladtke E Fetales Alkoholsyndrom [Fetal
alcohol syndrome]. Deutsche Medizinische Wochenschrift 101:1563-1568,
1976
142. Fryns JP, Deroover J, Parloir C, Goffaw P, Lebas E, Van Den
Berghe H: The foetal alcohol syndrome. Acta Paediatr Belg 30117-121,
1977
143. Dehaene P, Walbaum R, Titran M, Samaille-Villette C, Samaille
P, Crepin G, Delahousse G, Decocq J, Delcroix M, Caquant F, Querleu D:
La descendance des mitres alcoliques chroniques: A propos de 16 cas
d'alcoolisme foetal [The offspring of alcoholic mothers: A report of 16
cases of fetal alcohol syndrome]. Revue Francaise de Gyntcologie et
d'ObstCtrique 72:491-498, 1977
144. M ~ l l e rJ, Brandt NJ, Tygstrup I: Hepatic dysfunction in patient
with fetal alcohol syndrome. Lancet 1:605-606, 1979
145. Mattson SN, Riley EP, Jernigan TL, Garcia A, Kaneko WM,
Ehlers CL, Jones KL: A decrease in the size of the basal ganglia following
prenatal alcohol exposure: A preliminary report. Neurotoxicol Teratol
16~283-289,1994
146. Dehaene P, Samaille-Villette C, Samaille P-P, Crepin G, Walbaum R, Deroubaix P, Blanc-Garin A-P: Le syndrome d'alcoolisme foetal
dans le nord de la France [Fetal alcohol syndrome in the north of France].
Revue de L'Alcoolisme 23:145-158, 1977
147. Majewski F Alcohol embryopathy: Some facts and speculations
about pathogenesis. Neurobehav Toxicol Teratol 3:129-144, 1981
148. O'Connor MJ, Sigman M, Kasari C: Interactional model for the
association among maternal alcohol use, mother-infant interaction, and
infant cognitive development. Infant Behav Dev 16:177-192, 1993
149. Caruso K, ten Bensel R: Fetal alcohol syndrome and fetal alcohol
effects. Minn Med 76:25-29, 1993
150. Spohr HL, Willms J, Steinhausen HC. The fetal alcohol syndrome
in adolescence. Acta Pediatr 404:19-26, 1994
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Tbi ReflectionDocument2 pagesTbi Reflectionapi-302267315No ratings yet
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- Learning Disability ArticleDocument15 pagesLearning Disability Articleapi-302267315No ratings yet
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Tbi HandoutDocument3 pagesTbi Handoutapi-302267315No ratings yet
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- Tbi ArticleDocument9 pagesTbi Articleapi-302267315No ratings yet
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Learning Disability BibDocument1 pageLearning Disability Bibapi-302267315No ratings yet
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Learning Disability HandoutDocument3 pagesLearning Disability Handoutapi-302267315No ratings yet
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Learning Disability ReflectionDocument2 pagesLearning Disability Reflectionapi-302267315No ratings yet
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Hearing Loss ReflectionDocument2 pagesHearing Loss Reflectionapi-302267315No ratings yet
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- Fas ReflectionDocument2 pagesFas Reflectionapi-302267315No ratings yet
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- Hearing Loss ArticleDocument13 pagesHearing Loss Articleapi-302267315No ratings yet
- Hearing Loss BibDocument1 pageHearing Loss Bibapi-302267315No ratings yet
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Hearing Loss HandoutDocument4 pagesHearing Loss Handoutapi-302267315No ratings yet
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- Fas BibDocument2 pagesFas Bibapi-302267315No ratings yet
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Fas HandoutDocument2 pagesFas Handoutapi-302267315No ratings yet
- DyslexiareadingDocument19 pagesDyslexiareadingapi-302192077No ratings yet
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Down Syndrome BibDocument1 pageDown Syndrome Bibapi-302267315No ratings yet
- Dyslexia BibDocument1 pageDyslexia Bibapi-302267315No ratings yet
- Dyslexia ReflectionDocument2 pagesDyslexia Reflectionapi-302267315No ratings yet
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- Dyslexia HandoutDocument1 pageDyslexia Handoutapi-302192077No ratings yet
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Down Syndrome Refelction GuideDocument2 pagesDown Syndrome Refelction Guideapi-302267315No ratings yet
- Capd HandoutDocument3 pagesCapd Handoutapi-302267315No ratings yet
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Down Syndrome ArticleDocument6 pagesDown Syndrome Articleapi-302267315No ratings yet
- Capd Reflection GuideDocument2 pagesCapd Reflection Guideapi-302267315No ratings yet
- Capd ArticleDocument27 pagesCapd Articleapi-302267315No ratings yet
- Autism Spectrum HandoutDocument3 pagesAutism Spectrum Handoutapi-302267315No ratings yet
- Capd BibDocument1 pageCapd Bibapi-302267315No ratings yet
- Autism Spectrum ReflectionDocument2 pagesAutism Spectrum Reflectionapi-302267315No ratings yet
- Autism Spectrum BibDocument1 pageAutism Spectrum Bibapi-302267315No ratings yet
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- Autism ArticleDocument15 pagesAutism Articleapi-302267315No ratings yet
- Técnicas de EstudioDocument55 pagesTécnicas de EstudiojrdelarosaNo ratings yet
- Thematic RRL of Teachers' Level of Expertise On Modern Day TechnologyDocument11 pagesThematic RRL of Teachers' Level of Expertise On Modern Day TechnologyLourainne Faith AloceljaNo ratings yet
- Instructional Design-Learning TheoryDocument32 pagesInstructional Design-Learning Theorymkderwish0% (1)
- Book Club: Learn. Practise. Develop. TransformDocument21 pagesBook Club: Learn. Practise. Develop. TransformAyi EnhaNo ratings yet
- Tripp 1: The Western Diet and Hippocampus: Where Breakfast and Brain Power CollideDocument5 pagesTripp 1: The Western Diet and Hippocampus: Where Breakfast and Brain Power CollideCharlotte TrippNo ratings yet
- To Scroll or Not To Scroll Scrolling Working Memory Capacity and Comprehending Complex TextsDocument9 pagesTo Scroll or Not To Scroll Scrolling Working Memory Capacity and Comprehending Complex TextsAlfonso PiedrasantaNo ratings yet
- MatchaDocument29 pagesMatchaBurcuș AlexandruNo ratings yet
- Mental Status Examination: April 04, 2019 Sablan, BenguetDocument73 pagesMental Status Examination: April 04, 2019 Sablan, BenguetChristi MilanNo ratings yet
- How To Really Learn SpanishDocument47 pagesHow To Really Learn Spanishlightjp171% (7)
- Test Bank For Human Development 10th Edition CrandellDocument36 pagesTest Bank For Human Development 10th Edition CrandellMichelleSanchezokeys100% (32)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Module 32 WorksheetDocument2 pagesModule 32 WorksheetRyan JamesNo ratings yet
- Psy326 NotesDocument46 pagesPsy326 Notess_786886338No ratings yet
- Online GameDocument20 pagesOnline GameSubham ChoudhuryNo ratings yet
- Focus 4 Workbook Unit 1Document14 pagesFocus 4 Workbook Unit 1Sead Seky Nailovic80% (5)
- 2023-08-10 - Self-Practice 2Document13 pages2023-08-10 - Self-Practice 2Nguyễn Thị Cúc LyNo ratings yet
- An Insiders Guide To Sub-Modalities - Richard BandlerDocument127 pagesAn Insiders Guide To Sub-Modalities - Richard Bandlerjacobpalmer100% (15)
- 89295697360Document2 pages89295697360mosesbayang1No ratings yet
- CELF 4 Tech ReportDocument6 pagesCELF 4 Tech ReportRaghavendra RaoNo ratings yet
- English Model Papers - Dceb VZM 2020-21Document8 pagesEnglish Model Papers - Dceb VZM 2020-21narayana100% (1)
- 1 ATHA Readiness and Commitment Until One Is CommittedDocument14 pages1 ATHA Readiness and Commitment Until One Is Committedtsudhakar99No ratings yet
- 7 Laws of The LearnerDocument9 pages7 Laws of The Learnerluckieman100% (1)
- Research Paper Group 3Document77 pagesResearch Paper Group 3Sophia Aliyah Miel MacabeoNo ratings yet
- Document PDFDocument15 pagesDocument PDFdaytdeenNo ratings yet
- Introduction To Human CommunicationDocument27 pagesIntroduction To Human CommunicationYuriy KotNo ratings yet
- RRL NatinDocument6 pagesRRL NatinJessica DimayugaNo ratings yet
- A Strategy For Communication About UncertaintyDocument18 pagesA Strategy For Communication About UncertaintyhengkimyongNo ratings yet
- PGI - MadhubalaDocument2 pagesPGI - MadhubalaAshish DootNo ratings yet
- Understanding Movement-Lesson 1Document24 pagesUnderstanding Movement-Lesson 1jennylyn francisco100% (2)
- Expo 3 NEPSY II A Developmental Neuropsychological AssessmentDocument23 pagesExpo 3 NEPSY II A Developmental Neuropsychological AssessmentHugo Cruz LlamasNo ratings yet
- 1307446828000-Factors Influencing CreativityDocument19 pages1307446828000-Factors Influencing Creativityvlkanteti5258No ratings yet
- Healing Your Aloneness: Finding Love and Wholeness Through Your Inner ChildFrom EverandHealing Your Aloneness: Finding Love and Wholeness Through Your Inner ChildRating: 3.5 out of 5 stars3.5/5 (9)
- Allen Carr's Easy Way to Quit Vaping: Get Free from JUUL, IQOS, Disposables, Tanks or any other Nicotine ProductFrom EverandAllen Carr's Easy Way to Quit Vaping: Get Free from JUUL, IQOS, Disposables, Tanks or any other Nicotine ProductRating: 5 out of 5 stars5/5 (31)
- Allen Carr's Easy Way to Quit Smoking Without Willpower: The best-selling quit smoking method updated for the 21st centuryFrom EverandAllen Carr's Easy Way to Quit Smoking Without Willpower: The best-selling quit smoking method updated for the 21st centuryRating: 5 out of 5 stars5/5 (47)
- Breaking Addiction: A 7-Step Handbook for Ending Any AddictionFrom EverandBreaking Addiction: A 7-Step Handbook for Ending Any AddictionRating: 4.5 out of 5 stars4.5/5 (2)
- Save Me from Myself: How I Found God, Quit Korn, Kicked Drugs, and Lived to Tell My StoryFrom EverandSave Me from Myself: How I Found God, Quit Korn, Kicked Drugs, and Lived to Tell My StoryNo ratings yet
- THE FRUIT YOU’LL NEVER SEE: A memoir about overcoming shame.From EverandTHE FRUIT YOU’LL NEVER SEE: A memoir about overcoming shame.Rating: 4 out of 5 stars4/5 (7)