Professional Documents
Culture Documents
Final Draft Senior Project
Uploaded by
api-300510109Original Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Final Draft Senior Project
Uploaded by
api-300510109Copyright:
Available Formats
Holmes 1
Calista Holmes
Mrs. DeBock
English 4 Honors
October 13, 2015
Effects of the Job on Emergency Responders
Emergency responders include those individuals who respond to 911 emergencies and are
often the first to arrive on scene of a tragedy at any time of the day or night, whether they are
cross trained firefighters, EMTS, or paramedics. No amount of time and hard work put into
training and receiving certifications can fully prepare an individual for the hardships he or she is
setting forth to face in the future while in the profession. Firefighters and emergency medical
responders are exposed to many stressors that cause psychological and physiological effects such
as Post-Traumatic Stress Disorder, sleep deprivation, poor health and development of bad habits
that can all result in work-stress burnout.
Working as an emergency responder exposes individuals to scenarios often traumatizing
and indelible. Amongst that, he or she also faces dangerous and/or unpredictable situations
(Beaton 822). These exposers are categorized into five components containing many
subcomponents. Component 1 is Catastrophic Injury to Self or Co-worker composed of;
witnessed and unwitnessed duty-related death of co-workers, career ending injury to self or
coworkers, third degree burn or exposure to hazardous chemicals, multiple casualty motor
vehicle accidents, sudden infant death syndrome, and fire incidents with multiple burn victims.
Component 2 is Gruesome Victim Incidents composed of; completed suicide hangings,
Holmes 2
completed gunshot suicide, mutilated adult homicide attempt, attempted domestic homicide,
gunshot victim, attempted suicide/drug overdose, and adult dead on arrivals with multiple
injuries. Component 3 is Render aid to seriously injured vulnerable victims including adolescents
and friends or relatives. Component 4 is Minor Injury to self, including muscle strains,
concussions and fractures. Lastly, Component5 is Exposure to Death and Dying which was
composed of; cardiopulmonary resuscitation, adult dead on arrivals from natural causes and
death of a patient after long resuscitation efforts. Multiple data inputs suggested that routine
CPR is stressful, at least to some degree, for these emergency workers, even though they are
experienced daily (Beaton 827). Along with that, incidents involving children have been
reported to be the most stressful (Haslam 278). Other stressors include managerial or
organizational problems, shift work and time restraints exposures to the listed stressors are the
underlying factors for many physical and emotional repercussions (Haslam 278).
Exposure to multiple stressors as mentioned above inevitably puts emergency responders
at high risk of developing post-traumatic stress disorder (Haslam 277). A present study showed
that feelings of helplessness can lead to beliefs that they should have done more, causing an
incident to be perceived as traumatic (Haslam 281). PTSD is commonly characterized by
three types of symptoms; re-experiencing, avoidance, and arousal (Haslam 277). Reexperiencing includes flashbacks, intrusive memories dreams and distressing stimuli relevant to
the event. Avoidance is the pushing away of thoughts and feelings, and avoiding specific places
or people. Arousal is the increased jumpiness, irritability and sleep disturbances and the fear of
similar events happening to their family or themselves (Haslam 277). Questionnaires were given
to participants asking to identify and rate which of the events caused them most distress, how
long ago it occurred, if they were hurt and if they felt at all helpless or terrified. To diagnose
Holmes 3
PTSD a participant needs to endorse at least one re-experiencing, three avoidance and two
arousal symptoms (Haslam 279). There was a ninety minute one-on-one interview section for
personalized and in depth information; participants revealed hypersensitivity to smell was most
commonly linked to the smell of burnt flesh; the smell of burning pork was very much like
human beings burningsometimes I flashback to that event of that motor cyclist burning and
said that the number and severity of road traffic accidents they had attended had affected their
driving along with worrying when members of the family went out in the car and would remind
them to be careful (Haslam 281). Results showed that child fatalities were found to cause most
distress, followed by serious accidents and life-threatening illness in the firefighters family. The
most stressful aspects of the job frequently cited was the innocence of children, which was a
waste of life and familiarity to children of their own, and the second most common was
incidents involving gore, dead bodies or where people were in pain (Haslam 280). A total of
1,403 of 2,389 firefighters counseled required mental health-related medical leave as
determined by a mental health professional after the evaluation. (Corrigan 705). The most
common symptoms included feeling emotionally upset when reminded of the traumatic event,
having upsetting thoughts or images of the event, and having trouble falling asleep or staying
asleep (Haslam 280). Other symptoms indicative of distress that could lead to PTSD include
persistent fatigue, increase negativity, diminished motivation, emotions such as anger,
frustration and irritability, headaches and/or backaches unrelated to injury, tightness, clenched
jaws/fist, feeling chronically overwhelmed, diminished motivation, overindulgence in food,
drugs or nicotine, crying easily, feeling helpless, diminished concentration, sense of isolation
and in severe cases substance abuse, feelings of paranoia and suicidal thoughts (Vettor 218).
Holmes 4
According to Schmitz, even at low levels of sleep deprivation, peak performance is
difficult, often leading to mistakes, interpersonal conflicts and medical errors. Over one-third
participants said that they had experienced a disruption in their sleep cycle, some experiencing
bad dreams related to incidents involving serious injuries, others concerned feelings of failure
and being trapped (Haslam 281). Early start times and shift work along with reduced sleep
opportunities due extended work hours, long commutes and being on-call can also disrupt sleep.
Based on Wolkows data, emergency personnel have reported continuous periods of wakefulness
lasting for more than 24 hours. They believe this wakefulness is linked to the fact that the state of
constant readiness to respond to an emergency alarm felt while on-duty can transfer to the offduty environment (Wolkow 185). Evidence shows that periods of partial and total sleep
restriction can impair immune functions, hormone secretions and instigate adverse psychological
differences. For instance, a disruption in sleep cycle has been associated with cardiovascular
diseases, metabolic diseases along with depression, anxiety, anger, confusion, elevated cytokines
and cortisol levels. These increased levels can lead to a suppressed anti-inflammatory response,
glucose intolerance, hypertension and atherosclerosis. One study discovered that less than five
hours of sleep per night can lead to an increased chance of being named in a malpractice lawsuit
while on the job. Emergency medicine has been notorious for being at a high risk due to patient
acuity, lack of control over patient volume, and limited interaction time with patients and
families (Schmitz 66). Accumulating less than five hours of sleep can also cause major motor
vehicle accidents, conflict, burnout and depression outside of the workplace (Schmitz 66).
Working as an emergency responder leads to a lack of emphasis on a few things and
development of bad habits in place. Exercise and nutrition play key roles in avoiding obesity and
promoting wellness, but unfortunately they are frequently neglected during medical training and
Holmes 5
practice due to increased time at work, decreased time for exercise, lack of control over food
choices and eating times and disrupted sleep patterns (Schmitz 67). Emergency responders are
constantly on the go, leading to grabbing fast food, this schdeule also leads to abnormal
adrenaline levels, which can suppress appetite and lead to over eating later on. Poor nutrition
and lack of exercise often lead to mood swings, poor productivity levels and many health
problems and concerns (Schmitz 67). Attention to exercise, rest and nutrition is rare, and it is
documented that most work even when they are sick and expect their colleagues to do the
same (Schmitz 68). Another bad habit often developed when working as an emergency
responder is patient mortality. As a first responder they are forced into the position of breaking
bad news to loved ones while coping with our own emotions. Often responders are trained to fill
that role, then quickly move on to the next patient. Emotions that can arise from this lack of
coping time can range from depression, guilt, failure and unworthiness. Due to the lack of
adjustment and coping time between patients, humor is often a picked up as a safety valve to
release built up tension (Haslam 283). EMTs are also known to develop a thick skin approach
when treating a patient along with educational desensitization, language alteration, scientific
fragmentation and rationalization (Vettor 217). While these coping strategies are crucial in a first
responders health, allowing them to continue to concentrate on treating patients whose lives
they can save, it can often be misinterpreted by the media and bystanders. Emergency responders
are also been noted to have a higher prevalence of substance abuse compared to other specialties.
Schmitzs study reported that thirty one percent of responders indicated that burnout was,
and still is, a significant problem in emergency medicine. Burnout is defined as a combination of
the following three elements, emotional exhaustion: the depletion of emotional energy due to
work-related reasons, depersonalization: a feeling of distance from a patient or job, and lastly
Holmes 6
low personal accomplishment: a decreased feeling of self-worth or efficiency related to work
(Schmitz 64). Decreases in overall work performance has also been reported, including
inaccurate diagnosis, deficiencies in relational skills, and a tendency to trivialize the complaints
of patients (Vettor 217). Paramedics and EMTs are very susceptible to burnout since they face
chronic stressors such as dealing with injury, mutilation and death on a day to day basis, often
in a dangerous environment, while being scrutinized by bystanders and the traumatized relatives
of the patients (Vettor 217). The stress that EMTs undergo is not just due to their experiences in
the field but also compounded by the regular monotonous routine of paperwork, lack of support,
low wages, long hours, irregular shifts and cynical attitudes of hospital and law enforcement
personnel. Another frustration faced by EMTs is their position at the bottom of the medical
hierarchy. They are required to request permission to perform the simplest procedures from
someone with far less experience in emergency medicine. Even with that being said, Paramedics
are reported to have the highest burnout rate with the average length of their career being
reported as less than four years, due to the perception that the public takes advantage of them by
calling them to perform routine non-emergent services. These levels of stress and burnout can
result in high job-turnover rates, increased absenteeism, and low morale.
Firefighters and emergency medical responders are exposed to many stressors that cause
psychological and physiological effects such as Post-Traumatic Stress Disorder, sleep
deprivation, poor health and development of bad habits that can all result in work-stress burnout.
These effects can lead to a deficit in emergency responders in our future if awareness is not
raised on the subject and if changes are not made. Our future emergency health services lie in our
own hands, and will be impacted based on how we act now.
Holmes 7
Works Cited
Beaton, Randal, et al. Exposure To Duty-Related Incident Stressors In Urban Firefighters And
Paramedics. Journal Of Traumatic Stress 11.4 (1998):821. Advanced Placement Source.
Web. 21 Sept. 2015.
Corrigan, Malachy, et al. A Computerized, Self-Administered Questionnaire To Evaluate
Posttraumatic Stress Among Firefighters After The World Trade Center Collapse.
American Journal Of Public Health 99.S3 (2009): S702-S709. Business Source Premier.
Web. 21 Sept. 2015.
Haslam, Cheryl, and Krissie Mallon. A Preliminary Investigation Of Post-Traumatic Stress
Symptoms Among Firefighters. Work & Stress 17.3 (2003): 277-285. Business Source
Premier. Web. 21 Sept. 2015.
Schmitz, Gillian, et al. Strategies For Coping With Stress In Emergency Medicine: Early
Education is Vital. Journal of Emergencies, Trauma, And Shock 1 (2012): Academic
OneFile. Web 17 Sept. 2015.
Vettor, Susan M., and Frederick A. Kosinski Jr. Work-Stress Burnout In Emergency Medical
Technicians And The Use Of Early Recollections. Journal Of Employment Counseling
37.4 (2000): 216. Business Source Premier. Web. 21 Sept. 2015.
Wolkow, Alexander, et al. Effects of Work-Related Sleep Restriction On Acute Physiological
And Psychological Stress Responses And Their Interactions: A Review Among
Emergency Service Personnel. International Journal Of Occupational Medicine &
Environmental Health 28.2 (2015): 183-208. Academic Search Complete. Web 21 Sept.
2015.
Holmes 8
You might also like
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (894)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- 2007 MCQDocument67 pages2007 MCQTiffani Gutierrez100% (1)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- Ericksonian Approaches To Pain ManagementDocument6 pagesEricksonian Approaches To Pain Managementosher2650% (2)
- Prescription - 1717848 - 19 10 2021 - Dr. Syeda - Apollo 2471634614902285Document2 pagesPrescription - 1717848 - 19 10 2021 - Dr. Syeda - Apollo 2471634614902285Arunangshu DevNo ratings yet
- Case report of 3-year old boy with asthmaDocument6 pagesCase report of 3-year old boy with asthmaJiaYee GoNo ratings yet
- Pre Final Exam NCM 118Document26 pagesPre Final Exam NCM 118Faith BugtongNo ratings yet
- Service Topic Relevant To ResearchDocument1 pageService Topic Relevant To Researchapi-300510109No ratings yet
- Real World Narrative Senior ProjectDocument4 pagesReal World Narrative Senior Projectapi-300510109No ratings yet
- Service Final Draft Senior ProjectDocument5 pagesService Final Draft Senior Projectapi-300510109No ratings yet
- Service Annotated Bibliography Senior ProjectDocument4 pagesService Annotated Bibliography Senior Projectapi-300510109No ratings yet
- Annotated Bibliography Senior ProjectDocument5 pagesAnnotated Bibliography Senior Projectapi-300510109No ratings yet
- Hyun-Yoon Ko - Management and Rehabilitation of Spinal Cord Injuries-Springer (2022)Document915 pagesHyun-Yoon Ko - Management and Rehabilitation of Spinal Cord Injuries-Springer (2022)JESSICA OQUENDO OROZCONo ratings yet
- I. Bedsores A. What Are Bedsores?Document3 pagesI. Bedsores A. What Are Bedsores?peter911xNo ratings yet
- The Lightning-Fast Quest For COVID Vaccines - and What It Means For Other DiseasesDocument3 pagesThe Lightning-Fast Quest For COVID Vaccines - and What It Means For Other DiseasesKathiravan M NNo ratings yet
- SepanskiDocument13 pagesSepanskiTammy Utami DewiNo ratings yet
- Supplement-1115 2020Document216 pagesSupplement-1115 2020Laura PaunicaNo ratings yet
- 2023 ACC Expert Consensus Decision Pathway On Comprehensive Multidisciplinary Care For The Patient With Cardiac AmyloidosisDocument51 pages2023 ACC Expert Consensus Decision Pathway On Comprehensive Multidisciplinary Care For The Patient With Cardiac AmyloidosisERIK EDUARDO BRICEÑO GÓMEZNo ratings yet
- Jurnal Kesehatan Gigi: Perilaku Dan Keterampilan Menyikat Gigi Terhadap Timbulnya Karies Gigi Pada Anak Di Kota JambiDocument7 pagesJurnal Kesehatan Gigi: Perilaku Dan Keterampilan Menyikat Gigi Terhadap Timbulnya Karies Gigi Pada Anak Di Kota JambiUntuk TugasNo ratings yet
- "HIV Depletes T-Helper17, We Simply Stimulate It": by Prof. DR - Pichaet Wiriyachitra PH.D., F.R.A.C.IDocument37 pages"HIV Depletes T-Helper17, We Simply Stimulate It": by Prof. DR - Pichaet Wiriyachitra PH.D., F.R.A.C.IfroggyzzNo ratings yet
- Cam4 5 1239Document12 pagesCam4 5 1239kadiksuhNo ratings yet
- Ayurved TerminologiesDocument30 pagesAyurved TerminologiesVipul RaichuraNo ratings yet
- Chapter 4 A1 Poster Example 2Document3 pagesChapter 4 A1 Poster Example 2Krisna PamungkasNo ratings yet
- The Microbial World & You: NomenclatureDocument9 pagesThe Microbial World & You: NomenclatureApryll DarlineNo ratings yet
- Is Early Surgical Treatment For Benign Prostatic Hyperplasia Preferable Medical Therapy - Pros and ConsDocument11 pagesIs Early Surgical Treatment For Benign Prostatic Hyperplasia Preferable Medical Therapy - Pros and ConsClaudia FreyonaNo ratings yet
- Fellowship Course 3 Program v1Document15 pagesFellowship Course 3 Program v1Joice RumondangNo ratings yet
- AIIMS Dental PG November 2009 Solved Question Paper PDFDocument16 pagesAIIMS Dental PG November 2009 Solved Question Paper PDFDr-Amit PandeyaNo ratings yet
- PVC Unido ConDuplicadosDocument1,181 pagesPVC Unido ConDuplicadosJorge Chachaima MarNo ratings yet
- Combination lipid therapy as first-line strategy for very high-risk patientsDocument4 pagesCombination lipid therapy as first-line strategy for very high-risk patientsYo MeNo ratings yet
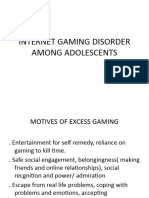
- Internet Gaming Disorder Among AdolescentsDocument10 pagesInternet Gaming Disorder Among AdolescentsGurumoorthy Dr.SureshkumarNo ratings yet
- FFT Neuroma Morton PDFDocument6 pagesFFT Neuroma Morton PDFdasamoroNo ratings yet
- Penicillin Drug StudyDocument2 pagesPenicillin Drug StudyEmagra AzilNo ratings yet
- Anatomi Dan Fisiologi PerkemihanDocument89 pagesAnatomi Dan Fisiologi Perkemihannia djNo ratings yet
- Mandala Coloring For Children With Symptoms of Attention Deficit Hyperactivity Disorder - A Case SeriesDocument7 pagesMandala Coloring For Children With Symptoms of Attention Deficit Hyperactivity Disorder - A Case Seriesindex PubNo ratings yet
- Fora 6 Brochure PDFDocument8 pagesFora 6 Brochure PDFFatma IsmawatiNo ratings yet
- Risk Factors and Indications of Orthodontic Temporary Anchorage Devices: A Literature ReviewDocument10 pagesRisk Factors and Indications of Orthodontic Temporary Anchorage Devices: A Literature ReviewSarath KumarNo ratings yet
- CT ScanDocument37 pagesCT ScanBayu Ihkshan Yamada TriatmojoNo ratings yet