Professional Documents
Culture Documents
Sample Soap
Uploaded by
Douglas Greg CookCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Sample Soap
Uploaded by
Douglas Greg CookCopyright:
Available Formats
Student: Greg Cook Date of patient visit: 3/11/2011 Reason for Patient Visit: Annual physical Identification and
problem statement: Patient initials: J. H. Age: 50 Sex: Male Marital Status: Married Race: Caucasian Occupation: Police dispatcher Source of Information: Patient; appears reliable Problem Statement: Im here for a physical. Its been about a year since Ive seen a doctor. My wife and I are applying for foster parent status and are required to have a physical. Subjective HPI: 50 y/o white male presents today for annual physical. Patient states requires physical for foster parent status approval. Patient states that he is usual state of good health. Reports that he has occasional problems with hemorrhoids (occasional notice of bright red streaks on stool and toilet paper after passage of large hard stools). States that his hemorrhoids are not currently causing him any problems. He also reports occasional and self-limiting episodes of diarrhea, which he attributes to stress (currently symptom free). Denies chest/abdominal pain. States usually has one formed stool in morning. Denies change in bowel frequency or consistency (except as previously noted). Denies nausea/emesis. Denies dark tarry stools. Denies recent weight gain/loss. Eats regular diet with no recent changes. His only other complaints are for seasonal itchy eyes, sneezing, and runny nose (currently symptom free). Pertinent Medical Denies chronic medical conditions. Immunizations up to date (last TD 2006). States passed 5mm kidney stone 2007. Right ankle fracture (non-displaced, football) 1991. Preventive screenings: colonoscopy (never). Patient does not want colonoscopy because he does not like the, idea of anesthesia. Last eye exam 2010, last dental exam 2009. Current Medications NKDA. Ibuprofen, 600mg PO prn knee pain.
Surgical History Vasectomy 2007. Family History Father died at 74 years of age from prostate cancer that traveled to brain. Mother living (85 years old) has history of glaucoma and osteoarthritis. Has one sibling (brother, 57 years old) with history of hypertension, otherwise in good health. Social History The patient reports his health to be pretty good. He never smoked and admits to drinking 1 six-pack of beer every month or so. The patient is married and has no children. He is physically active outside of work (plays intramural baseball and takes care of his three horses), but does not participate in routine aerobic exercise. He consciously watches his caloric and fat intake, but is otherwise on a regular diet. He is sexually active in a monogamous relationship. He denies the use of recreational drugs. His wife also works outside of the home and they are both self-supportive on their current combined incomes. He has no current concerns regarding his activities of daily living. Review of Systems General Reports in usual state of Good health and weight. Denies fever, chills, recent weight gain or loss, weakness, fatigue, pain. States that his last physical exam was in 2010. Skin Denies recent rashes or changes in texture or moles. HEENT Denies headaches. Denies problems with vision or hearing. Wears reading glasses, last eye exam 2010. Denies use of hearing aids. Denies glaucoma or cataracts. Denies frequent nasal congestion/stuffiness, but occasional seasonal teary eyes, runny nose and sneezing (currently asymptomatic). Denies nosebleeds. Denies permanent/removable dental prosthetics. Last dental exam 2010. Denies swollen glands/limps, neck stiffness. Thorax and Lungs Denies history of lung disease, allergies, or asthms. Denies episodes of unexplained shortness of breath. Cardiovascular Denies heart trouble, high blood pressure, rheumatic fever, heart murmurs, irregular beat, palpitations, or chest pain/discomfort. No prior stress test or EKG. Peripheral Vascular Denies extremity edema, coldness, leg cramps, skin ulcers. Abdomen Regular diet. No swallowing difficulties. Denies problems
with nausea/vomiting, heartburn, or food intolerances. Regular diet. No recent change in weight. Denies chronic diarrhea, but has selflimiting episodes of diarrhea which he attributes to stress. Also reports episodic problems with hemorrhoids with blood on toilet paper and streaking of passage of hard stool. States currently has a couple small hemorrhoids with no bleeding. Denies history of jaundice, gall bladder, or liver disease. Genitourinary Denies urinary frequency, hesitancy, incontinence, or burning with urination. History of passing 5mm kidney stone 2007. In a long-term monogamous relationship. Denies sexual issues. Metabolic/Hematologic Denies thyroid problems, heat/cold intolerance, excessive hunger, thirst, or history of diabetes. Denies concerning bruising, ease of bleeding. No history of blood transfusions. Psychiatric Denies trouble concentrating, nervousness, anxiety, or panic attack. Denies difficulty falling or staying asleep. Occasional (once/week) getting out of bed earlier than waking time to urinate (associated with drinking fluids at night). Denies mood changes, hearing voices, frequent unhappiness, or desire to harm self or others. Denies nightmares, memory loss, or excessive life stresses. No recent deaths in family or close friends. Musculoskeletal Right ankle fracture (football, non-displaced) 1991. Occasional pain both knees, which he attributes to years of playing sports and not to a traumatic event. Denies other orthopedic injury or arthralgia. Neurologic Denies history of stroke, seizures or frequent/incapacitating headache. Denies tremors. Objective General Appearance 50 year-old male who is awake, alert, and cooperative. Clothing is well kept and appropriate for season. He is oriented to person, place, and time and answers all questions appropriately. Appears stated age, appears to be healthy, and does not appear to be in any acute distress. Vitals BP Right arm sitting. 152/92 HR 72 RR 16 Sa02 99% on room air
Tympanic temp 98.7 Head Normocephalic, short cut hair clean with fine texture. Scalp with no lesions, tenderness. TMJ full ROM without clicks o pain bilaterally. No frontal or maxillary sinus tenderness. Eyes Symmetrical, sclera white, conjunctiva pink. No drainage. PERLA 3/2. Fundoscopy (without pharmacologic mydriasis): red reflex present, no hemorrhages, lens opacities, disk cupping, papillidema, optic vessels appreciated 2:3 AV ratio. Visual acuity deferred. Ears External ear, no lesions, masses, drainage, or tenderness. CN I grossly intact. Otoscopic exam: TMs pearly grey with + cone of light, no bulging, no erythema, landmarks appreciated bilaterally. Nose No nasal flaring. Septum midline, turbinates pink and moist. No lesions, polyps, or nasal discharge bilaterally. Throat and Mouth Membranes pink/moist. Uvula is midline, tonsils at pillars, no redness or exudates. Neck Trachea midline. Thyroid and lymph nodes not palpable. Breasts Inspection: no gynecomastia, nipples symmetrical, everted, no drainage. Palpation: Breasts/axilla node palpation deferred. Heart No JVD at 90 degrees. Carotids not assessed. S1 best at apex. S2 best at base. No extra sounds. Thorax and Back No abnormal curvatures. Symmetrical expansion with respiration Lungs Lung fields not palpated/percussed. Anterior and Posterior lung fields clear to auscultation. Abdomen Round and non-distended with no scars, striae. No abdominal tenderness to palpation. Liver and spleen not palpable. Normoactive tympanic bowel sounds x 4, no abdominal bruits. Extremities (Upper) Nails without cyanosis or clubbing. Muscles well developed. Distal pulses +2. Capillary refill < 3 seconds. Full active ROM. (Lower) Nails without cyanosis or clubbing. Muscles well developed. Distal pulses +2. Capillary refill < 3 seconds. Full active ROM. Hair
growth + great toes bilaterally. Negative Homans. Skin Color consistent with race. Warm, dry, intact with good turgor. No peripheral/central cyanosis. No obvious rashes. Multiple small (<0.5 cm) flat hyperpigmented (brown) lesions on abdomen, chest, back, upper extremities, and neck (several with irregular borders). Lymph Nodes Not palpable in head or neck or axilla or groin Neurologic: Mental status: Awake, alert, oriented to person, place, and time. No confusion, anxiety, or agitation noted. Cranial Nerves: II, III PERLA, + consensual movement, + accommodation II, IV, and VI: EOM intact Remaining Cranial Nerves: CN I not assessed. CN V and CN VII XII grossly intact. Motor System: Muscle strength 5/5 in all extremities bilaterally. Gait steady w/o ataxia. Finger-to-nose, Rhomberg, heel to shin and pronator drift all performed bilaterally without deficit. Sensory: Sharp, dull, light in all extremities tested without deficit. Reflexes: Triceps 2+ 2+. Biceps 2+ 2+, Brachioradialis 2+ 2+, Patellar 2+ 2+, Ankle 1+ 1+. Babinski not assessed. Genitals Not examined Rectal Not examined Labs: TSH, T3, T4, BMP, CBC, HA1C, PSA (all wnl). Assessment 1) 2) 3) 4) 5) Essential stage 1 hypertension Multiple congenital/dysplastic nevi Hemorrhoids Seasonal allergic rhinitis Occasional non-bloody diarrhea of unknown etiology
Plan 1) Three day BP check with plan to initiate ACEI if remains elevated 2) Dermatology referral for evaluation of multiple hyperpigmented skin lesions 3) Discussed importance of colon cancer screening colonoscopy and GI referral for hemorrhoids, episodic diarrhea. Discussed use of procedural anesthesia options. GI referral placed which will be good for six months if patient changes mind. 4) azelastome nasal, 1-2 sprays/nostril bid prn during allergy season. 5) Consider ASA 81mg po QD after cleared by GI
NORTHERN ARIZONA UNIVERSITY SCHOOL OF NURSING FAMILY NURSE PRACTITIONER PROGRAM NUR 661, Spring 2011 Self-Analysis A completed self-analysis will accompany each SOAP note that you turn in. The self-analysis will address the patient contact that is the topic of the SOAP note and will address your analysis of how you are doing overall in the clinical experience. Address the following areas: 1. Clinical Decision Making: how well did you think you did in your clinical decision making? What worked/what didnt work? For the rest of the semester (SOAPs 5, 6 and 7), please address the following: a) what are 4 common differential diagnoses that you considered on this patient? What subjective and objective data helped you to rule-in or rule-out each of these diagnoses; and b) what are 2 zebra differential diagnoses that you consider? What subjective and objective data helped you to rule-in or ruleout each of these? Essential hypertension: Secondary hypertension Congenital/dysplastic nevi: Melanoma Lentigo Hemorrhoids: Rectal polyps Rectal fissures Lower GI Bleed I ruled out secondary hypertension with this patient; there is no indication of endocrine or renal dysfunction (clinical presentation, ROS, exam, labs). Secondary hypertension is normally caused by: coarctation of aorta (Zebras), Cushings, diabetes, pheochromocytoma (another Zebra, but he has no tachycardia, nervousness, palpitations, sweating or other sympathetic/adrenergic symptoms) , and drugs such as antidepressants, appetite suppressants, glucocorticoids, and MAOIs. I do want to rule out white coat hypertension so I will ask patient to check BP in out of clinic environments. He is not pregnant so I can rule out pre-eclampsia. The main concern with his skin lesions is the possibility of malignancy. His lesions are concerning and should be evaluated and biopsied for a definitive diagnosis by a dermatologist.
The patient gave a good description of his hemorrhoids and does not have any other GI symptoms (lower GI bleed). He does associate the bright blood with passage of hard stool so a rectal fissure could certainly be the cause. Either way, I really want this patient to see a GI specialist for additional work-up and cancer screening colonoscopy. 2. Use of PDA: how did you use PDA to enhance your clinical decision making and incorporate evidence-based, point-of-care information into the decision making process? I used the PDA to run through some of the differentials (primary hypertension vs secondary) and to research some of the Zebras (pheochromocytoma). I also ran through the U.S. Preventive Services Task Forces application to nail down preventive screening interventions (for this patient, SDT screening but he is in a long-term monogamous relationship, ASA prevention, lipids, hypertension screening). 3. Interaction, Communication and Collaboration with the Patient/Family This patient was a good historian with an uncomplicated med/surgical history. The physician and I both spent time with this patient reviewing the importance of a cancer screening colonoscopy, but he refuses the procedure because he does not like the idea of anesthesia. We both spent additional time discussing the anesthetics and sedative agents used for this procedure (very short acting, very few side effects, rapid clearing of effects, no ET tube, etc). We did put in a referral, which will be good for 6 months if he changes his mind. We also tied the fact that the GI consult is needed for eval of his diarrhea as well as his hemorrhoids and that we would hold starting ASA therapy for his heart health until he kicks this can further down the road. 4. Interaction, Communication and Collaboration with Your Preceptor (and others pertinent to the process) 5. Additional Self-Reflections: What did you learn from this experience? Was the learning important for you? Why or why not? What did you learn/observe about yourself this week? How did you advocate for yourself? What do you believe about what you learned this week? How will you transfer the knowledge and learning you gained to other situation? Also address, how well you were able to address psycho social, cultural, and/or family-related issues, any ethical/legal issues, etc. with the patient. I need to discuss why my preceptor deferred doing a rectal exam (has hemorrhoids), and prostate exam, or genital exam for this 50 year-old. My female preceptor is very thorough doing breast exams, genital exams (but again
no rectal exams) on her female patients. This may be a cultural issue with my preceptor, but I wonder how she got through med school (it was a foreign school howeverso there may be something there). Id appreciate pointers on this. Please be specific and insightful. We are looking for depth and breadth of selfanalysis and self-reflection. Add additional pages as needed. Reference: Gutierrez, K. (2008). Pharmacotherapeutics: clinical reasoning in primary care (2nd ed.). St. Louis, Mo: Saunders Elsevier.
You might also like
- FAMILY NURSE PRACTITIONER: Passbooks Study GuideFrom EverandFAMILY NURSE PRACTITIONER: Passbooks Study GuideNo ratings yet
- Final Practicum - Soap Note 2Document19 pagesFinal Practicum - Soap Note 2api-494643478No ratings yet
- Nurse Practitioner Board ReviewFrom EverandNurse Practitioner Board ReviewRating: 5 out of 5 stars5/5 (1)
- Nurs 5018 - Soap Note Well-Woman ExamDocument7 pagesNurs 5018 - Soap Note Well-Woman Examapi-308904543No ratings yet
- Back to Zero: FNP Board Review NotesFrom EverandBack to Zero: FNP Board Review NotesRating: 5 out of 5 stars5/5 (2)
- ICM SOAP Note 11:3Document4 pagesICM SOAP Note 11:3Warren G Lawless67% (3)
- Secrets From The World's Most Productive Nurse PractitionerFrom EverandSecrets From The World's Most Productive Nurse PractitionerNo ratings yet
- Final Practicum - Soap Note 3Document17 pagesFinal Practicum - Soap Note 3api-494643478100% (2)
- Family Nurse Practitioner Certification Prep Plus: Proven Strategies + Content Review + Online PracticeFrom EverandFamily Nurse Practitioner Certification Prep Plus: Proven Strategies + Content Review + Online PracticeRating: 5 out of 5 stars5/5 (2)
- Complete SOAP Note for 39-Year-Old Female with Nausea and VomitingDocument6 pagesComplete SOAP Note for 39-Year-Old Female with Nausea and VomitingLorrie83% (6)
- Psychiatric-Mental Health Nursing: Scope and Standards of Practice, 3rd EditionFrom EverandPsychiatric-Mental Health Nursing: Scope and Standards of Practice, 3rd EditionNo ratings yet
- SOAP NoteDocument8 pagesSOAP NoteAnonymous p0y5mmLQNo ratings yet
- Textbook of Urgent Care Management: Chapter 17, Physician Extenders in the Urgent Care CenterFrom EverandTextbook of Urgent Care Management: Chapter 17, Physician Extenders in the Urgent Care CenterNo ratings yet
- Soap NoteDocument4 pagesSoap Noteapi-252633788100% (7)
- ADULT NURSE PRACTITIONER: Passbooks Study GuideFrom EverandADULT NURSE PRACTITIONER: Passbooks Study GuideNo ratings yet
- Geriatric Soap NoteDocument6 pagesGeriatric Soap Noteapi-282282363100% (6)
- SOAP Annual PhysicalDocument11 pagesSOAP Annual Physicalniknshell100% (1)
- Nurs 5018 - Soap Note Chronic IllnessDocument5 pagesNurs 5018 - Soap Note Chronic Illnessapi-308904543No ratings yet
- Episodic SOAP Note Template - RX PedsDocument11 pagesEpisodic SOAP Note Template - RX PedsBrianne Foster75% (4)
- Soap Note 3 FinalDocument9 pagesSoap Note 3 Finalapi-272656243No ratings yet
- Chapter 3 SOAP NoteDocument2 pagesChapter 3 SOAP NoteKatrina Litzko50% (2)
- Focused Soap NoteDocument9 pagesFocused Soap NoteJAMES KIHATO100% (2)
- Acute Cholecystitis ER AdmissionDocument6 pagesAcute Cholecystitis ER Admissionjessica100% (5)
- Sample Soap NoteDocument7 pagesSample Soap Notesedaka260% (1)
- Headache H&P SOAPDocument3 pagesHeadache H&P SOAPRauf Ab67% (3)
- Nurs 5024 - Soap - Well AdultDocument6 pagesNurs 5024 - Soap - Well Adultapi-308904543100% (1)
- SOAP Note Fall 2018 4Document18 pagesSOAP Note Fall 2018 4arunatejaNo ratings yet
- Clinical Performance Evaluation → Asthma ACR-DIDDocument1 pageClinical Performance Evaluation → Asthma ACR-DIDveronica100% (1)
- Focused Soap NoteDocument4 pagesFocused Soap Noteapi-24735887592% (13)
- Soap Note1 - Gyn ComplaintDocument6 pagesSoap Note1 - Gyn Complaintapi-482726932100% (3)
- Soap Note Week 1 Sep7Document3 pagesSoap Note Week 1 Sep7dondavis77No ratings yet
- SOAP Note DiabetesDocument16 pagesSOAP Note Diabetesmichael thorn92% (25)
- Chronic SOAP Note for 51 Year Old Female with HyperlipidemiaDocument3 pagesChronic SOAP Note for 51 Year Old Female with HyperlipidemiaJeffrey ViernesNo ratings yet
- Soap Note - Musculoskeletal and Nervous SystemsDocument2 pagesSoap Note - Musculoskeletal and Nervous SystemsSummer Keller88% (8)
- Adult Health - Soap Note 5Document3 pagesAdult Health - Soap Note 5api-546259691100% (3)
- Soap Note 4 (CPII)Document5 pagesSoap Note 4 (CPII)Flor OM89% (37)
- Contraception SOAP Note ReviewDocument7 pagesContraception SOAP Note ReviewAnnah AnnNo ratings yet
- ITP - SOAP Note #3 (Genitourinary)Document4 pagesITP - SOAP Note #3 (Genitourinary)FrozenMan67% (3)
- Soap Well Women S KellyDocument6 pagesSoap Well Women S Kellyapi-415083061No ratings yet
- Womens Health - Soap Note 1Document11 pagesWomens Health - Soap Note 1api-494643478100% (2)
- Soap Note 5 - Part 2Document6 pagesSoap Note 5 - Part 2api-494643478100% (1)
- Adult Medical SOAP NoteDocument4 pagesAdult Medical SOAP NoteBhanu100% (6)
- 2Document50 pages2Scott Russell McGillivray100% (1)
- Abdominal Pain Diagnosis and Treatment PlanDocument2 pagesAbdominal Pain Diagnosis and Treatment PlanSandhya Rubens67% (9)
- ITP - SOAP Note #1 (Cardiac)Document3 pagesITP - SOAP Note #1 (Cardiac)FrozenMan100% (1)
- Peds - Soap Note 5Document3 pagesPeds - Soap Note 5api-546259691No ratings yet
- ITP - SOAP Note #2 (Pulmonary)Document12 pagesITP - SOAP Note #2 (Pulmonary)FrozenMan90% (10)
- Nsg6435 Soap Note 2Document7 pagesNsg6435 Soap Note 2Hephzibah Beulah100% (1)
- Episodic-Focused Soap NoteDocument4 pagesEpisodic-Focused Soap Notemoses okumuNo ratings yet
- SOAP Note Cheat Sheet - Complete H&PDocument2 pagesSOAP Note Cheat Sheet - Complete H&PAdeline N. Omene95% (19)
- LM Soap NoteDocument5 pagesLM Soap NoteSpreeha Choudhury100% (2)
- Soap 5 - Geriatric 65Document13 pagesSoap 5 - Geriatric 65api-482726932No ratings yet
- Pain Case - SOAP Note (2011)Document2 pagesPain Case - SOAP Note (2011)Alfie Lee100% (3)
- Obgyn Soap Note ExampleDocument2 pagesObgyn Soap Note ExampleBluerobins94% (33)
- Soap Note 3 DominguezDocument6 pagesSoap Note 3 Dominguezapi-320062911No ratings yet
- SOAP For Upper Respiratory Infection #4Document3 pagesSOAP For Upper Respiratory Infection #4carlos fernandezNo ratings yet
- Esther ParksDocument6 pagesEsther ParksMyrnaivette Pierson63% (19)
- Nurs 5023 - Soap 5Document5 pagesNurs 5023 - Soap 5api-308904543100% (2)
- Soap Note 2 Dominguez 2015Document5 pagesSoap Note 2 Dominguez 2015api-320062911No ratings yet
- COVID SOAP NoteDocument7 pagesCOVID SOAP NoteBryan100% (1)
- Do Not CrushDocument16 pagesDo Not CrushDouglas Greg CookNo ratings yet
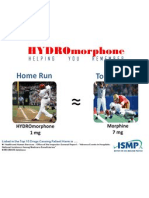
- Hydro Morph OneDocument2 pagesHydro Morph OneDouglas Greg CookNo ratings yet
- FindingsDocument2 pagesFindingsDouglas Greg CookNo ratings yet
- ECG InterpretationDocument52 pagesECG InterpretationMarcus, RN98% (44)
- Normal ExamDocument2 pagesNormal ExamDouglas Greg CookNo ratings yet
- ACLS Rhythms For The ACLS Algorithms: AppendixDocument32 pagesACLS Rhythms For The ACLS Algorithms: Appendixyan_ricci19100% (4)
- Normal ExamDocument2 pagesNormal ExamDouglas Greg CookNo ratings yet
- Do's and Don'tsDocument1 pageDo's and Don'tsDouglas Greg CookNo ratings yet
- Rhythm Strip ReviewDocument8 pagesRhythm Strip ReviewDouglas Greg Cook100% (2)
- Autonomic DrugsDocument2 pagesAutonomic DrugsDouglas Greg CookNo ratings yet
- Acls Patient Algorithms: Greg Cook's Version of A Phoenix Fire DPT ClasicDocument4 pagesAcls Patient Algorithms: Greg Cook's Version of A Phoenix Fire DPT ClasicDouglas Greg CookNo ratings yet
- ACLS-2010 (PDF Library)Document5 pagesACLS-2010 (PDF Library)Charlo SantosNo ratings yet
- Cook and Tillman Thesis WorkDocument30 pagesCook and Tillman Thesis WorkDouglas Greg CookNo ratings yet
- Cook Clinical Decision MakingDocument13 pagesCook Clinical Decision MakingDouglas Greg CookNo ratings yet
- HimdagDocument4 pagesHimdagDouglas Greg CookNo ratings yet
- Tohono CultureDocument20 pagesTohono CultureDouglas Greg CookNo ratings yet
- Cook and Tillman ThesisDocument26 pagesCook and Tillman ThesisDouglas Greg CookNo ratings yet
- Thesis - Stefano CrispinoDocument45 pagesThesis - Stefano CrispinoStefano CrispinoNo ratings yet
- Kasol Travel GuideDocument3 pagesKasol Travel GuidevivekNo ratings yet
- Simple Guide To Very Low Carb Diets - Shelby StarnesDocument37 pagesSimple Guide To Very Low Carb Diets - Shelby Starnesleary12gmailcom94% (18)
- Strange Horizons - Have Your #Hugot Harvested at This Diwata-Owned Café by Vida Cruz, Art by Nina SatieDocument36 pagesStrange Horizons - Have Your #Hugot Harvested at This Diwata-Owned Café by Vida Cruz, Art by Nina SatieGuillermo Guadarrama MendozaNo ratings yet
- Final Test Welcome 2Document2 pagesFinal Test Welcome 2jasminamina222No ratings yet
- Know Your FatsDocument348 pagesKnow Your Fatstamy_001100% (3)
- Soal PAS Bhs - Inggris Kelas IXDocument8 pagesSoal PAS Bhs - Inggris Kelas IXsangayu pramiNo ratings yet
- CC0006 Week3 PPTDocument29 pagesCC0006 Week3 PPTjie minNo ratings yet
- R Nenglish Practice 1: B. Stomach B. Improves D. Listen A. Change D. Angle B. Tor'nado C. De'ny A. Worried C. Po'liticsDocument5 pagesR Nenglish Practice 1: B. Stomach B. Improves D. Listen A. Change D. Angle B. Tor'nado C. De'ny A. Worried C. Po'liticsPhuong AnhhNo ratings yet
- Separating Substances Class 6 Science AssessmentDocument2 pagesSeparating Substances Class 6 Science Assessmentsifat monga100% (1)
- Group 17Document18 pagesGroup 17Abdul WahabNo ratings yet
- Unit 3 Carbohydrates Notes PacketDocument15 pagesUnit 3 Carbohydrates Notes PacketAmartya PoovaiahNo ratings yet
- Milk Tea (Bubble Tea) Demand in Vietnam: Asia Plus IncDocument30 pagesMilk Tea (Bubble Tea) Demand in Vietnam: Asia Plus IncKankanNguyenNo ratings yet
- The Hidden SoldierDocument246 pagesThe Hidden SoldierWendi PutraNo ratings yet
- The Importance of Nutrition Education in SchoolsDocument12 pagesThe Importance of Nutrition Education in SchoolsTitis Retno Sawitri SawitriNo ratings yet
- Present Perfect Past Simple WorksheetDocument3 pagesPresent Perfect Past Simple Worksheetаниме- -мангаNo ratings yet
- Menu Arunika JogloDocument2 pagesMenu Arunika JogloGisattNo ratings yet
- Power Air Fryer Cook BookDocument32 pagesPower Air Fryer Cook BookMusafir Adam100% (1)
- Full Elementary PDF v1Document40 pagesFull Elementary PDF v1rodrigo marquesNo ratings yet
- Habeco: Customers Service: Supply Chain ManagementDocument13 pagesHabeco: Customers Service: Supply Chain ManagementNguyễn Hồng HạnhNo ratings yet
- 10000017582Document2,275 pages10000017582Chapter 11 DocketsNo ratings yet
- 2000 Cau Trac NghiemDocument106 pages2000 Cau Trac NghiemLan AnhNo ratings yet
- Water Water Water WaterDocument7 pagesWater Water Water WaterAvie WriterNo ratings yet
- IBSDocument1 pageIBSIris MambuayNo ratings yet
- FOOD Expo Exhibitor ListDocument5 pagesFOOD Expo Exhibitor ListDhiman Dodhia0% (1)
- Basic Concept of Ecology and Energy Flow in An EcosystemDocument16 pagesBasic Concept of Ecology and Energy Flow in An Ecosystemcrishamae gentilesNo ratings yet
- Chapter-1 FILIPINIANADocument44 pagesChapter-1 FILIPINIANAEmalyn MadrigalNo ratings yet
- Interchange Level 3 Presentation Plus - Newson 39 S Language CentreDocument331 pagesInterchange Level 3 Presentation Plus - Newson 39 S Language CentreCatana TeodoraNo ratings yet
- Email TLUD For Rice HuskDocument4 pagesEmail TLUD For Rice HuskKewl DudzNo ratings yet
- Đề KT Unit 8 - Tiếng Anh 3 ExtraDocument5 pagesĐề KT Unit 8 - Tiếng Anh 3 ExtraHoaiNo ratings yet
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionFrom EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionRating: 4 out of 5 stars4/5 (402)
- Why We Die: The New Science of Aging and the Quest for ImmortalityFrom EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityRating: 3.5 out of 5 stars3.5/5 (2)
- Outlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisFrom EverandOutlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisRating: 4 out of 5 stars4/5 (1)
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedFrom EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedRating: 5 out of 5 stars5/5 (78)
- The Age of Magical Overthinking: Notes on Modern IrrationalityFrom EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityRating: 4 out of 5 stars4/5 (13)
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeFrom EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeNo ratings yet
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsFrom EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsRating: 3.5 out of 5 stars3.5/5 (3)
- Techniques Exercises And Tricks For Memory ImprovementFrom EverandTechniques Exercises And Tricks For Memory ImprovementRating: 4.5 out of 5 stars4.5/5 (40)
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsFrom EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsRating: 5 out of 5 stars5/5 (1)
- Raising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsFrom EverandRaising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsRating: 4.5 out of 5 stars4.5/5 (169)
- The Obesity Code: Unlocking the Secrets of Weight LossFrom EverandThe Obesity Code: Unlocking the Secrets of Weight LossRating: 5 out of 5 stars5/5 (4)
- The Ultimate Guide To Memory Improvement TechniquesFrom EverandThe Ultimate Guide To Memory Improvement TechniquesRating: 5 out of 5 stars5/5 (34)
- Roxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingFrom EverandRoxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingRating: 5 out of 5 stars5/5 (4)
- The Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaFrom EverandThe Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaRating: 4.5 out of 5 stars4.5/5 (266)
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsFrom EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsNo ratings yet
- Summary: Limitless: Upgrade Your Brain, Learn Anything Faster, and Unlock Your Exceptional Life By Jim Kwik: Key Takeaways, Summary and AnalysisFrom EverandSummary: Limitless: Upgrade Your Brain, Learn Anything Faster, and Unlock Your Exceptional Life By Jim Kwik: Key Takeaways, Summary and AnalysisRating: 5 out of 5 stars5/5 (8)
- Roxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingFrom EverandRoxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingRating: 3.5 out of 5 stars3.5/5 (33)
- Dark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.From EverandDark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Rating: 4.5 out of 5 stars4.5/5 (110)
- Summary: It Didn't Start with You: How Inherited Family Trauma Shapes Who We Are and How to End the Cycle By Mark Wolynn: Key Takeaways, Summary & AnalysisFrom EverandSummary: It Didn't Start with You: How Inherited Family Trauma Shapes Who We Are and How to End the Cycle By Mark Wolynn: Key Takeaways, Summary & AnalysisRating: 5 out of 5 stars5/5 (3)
- The Happiness Trap: How to Stop Struggling and Start LivingFrom EverandThe Happiness Trap: How to Stop Struggling and Start LivingRating: 4 out of 5 stars4/5 (1)
- The Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeFrom EverandThe Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeRating: 4.5 out of 5 stars4.5/5 (253)
- The Garden Within: Where the War with Your Emotions Ends and Your Most Powerful Life BeginsFrom EverandThe Garden Within: Where the War with Your Emotions Ends and Your Most Powerful Life BeginsNo ratings yet
- The Tennis Partner: A Doctor's Story of Friendship and LossFrom EverandThe Tennis Partner: A Doctor's Story of Friendship and LossRating: 4.5 out of 5 stars4.5/5 (4)