Professional Documents
Culture Documents
Cloxacillin, Sodium: How Should I Take Cloxacillin?
Uploaded by
Stacy MC PelitoOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Cloxacillin, Sodium: How Should I Take Cloxacillin?
Uploaded by
Stacy MC PelitoCopyright:
Available Formats
CLOXACILLIN, SODIUM
Apo-Cloxi , Cloxapen, Cloxilean, Novocloxin , Orbenin, Tegopen Classifications: antiinfective; antibiotic, natural penicillin; beta-lactam
How should I take cloxacillin?
Take cloxacillin exactly as directed by your doctor. If you do not understand these instructions, ask your pharmacist, nurse, or doctor to explain them to you. Take each dose with a full glass of water. Take cloxacillin on an empty stomach 1 hour before or 2 hours after meals. Do not drink juice or carbonated beverages (soda) with your dose of cloxacillin. These beverages will decrease the effectiveness of the drug. Cloxacillin should be taken at evenly spaced intervals throughout the day and night to keep the level in your blood high enough to treat the infection.
Assessment & Drug Effects Determine previous exposure and sensitivity to penicillins and cephalosporins and other allergic reactions of any kind before treatment is initiated. Monitor for S&S of anaphylactoid reaction (see Appendix G) or other signs or symptoms of hypersensitivity reaction (see Appendix F) as with other penicillins. Lab tests: Periodic assessments of renal, hepatic, and hematopoietic function are advised in patients on long-term therapy. Patient & Family Education Take medication around the clock, do not miss a dose, and continue taking the medication until it is finished. Report to physician the onset of hypersensitivity reaction (see Appendix F) and superinfections. Check with physician if GI adverse effects (nausea, vomiting, diarrhea) appear. Do not breast feed while taking this drug.
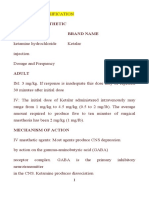
GENERIC NAME: Diazepam BRAND NAME: Valium CLASSIFICATION: Antianxiety agents, anticonvulsants, sedative/hyptonics, skeletal muscle relaxants (centrally acting) DOSAGE: 10 mg IM MECHANISM OF ACTION: - Depress the CNS, probably by potentiating GABA, an inhibitory neurotransmitter. - Produces skeletal muscle relaxation by inhibiting spinal polysynaptic afferent pathways. - Has anticonvul-sant properties due to enhanced presynaptic inhibition.Therapeutic effects: (1) Relief of Anxiety (2) Sedation (3) Amnesia (4) Skeletal muscle relaxant (5) Decreased seizure activity INDICATION: -Adjunct in the management of: 1) Anxiety 2) Preoperative sedation 3) Conscious sedation - Provides light anesthesia and anterograde amnesia - Treatment of status epilepticus/ uncontrolled seizures - Skeletal muscle relaxant - Management of the symptoms of alcohol withdrawal CONTRAINDICATIONS: - Hypersensitivity - Cross-sensitivity with other benzodiazepines may occurs - Comatose patients - Pre-existing CNS depression - Uncontrolled severe painUse cautiously in: 1) Hepatic dysfunction 2) Severe renal impairment 3) History of suicide attempt or drug dependence
SIDE EFFECTS/ ADVERSE EFFECTS: - CNS: 1) dizziness 2) drowsiness 3) lethargy 4) hangover 5) headache 6) depression - EENT: 1) blurred vision - RESP: 1) respiratory depression - CV: 1) hypotension - GI: 1) constipation 2) diarrhea 3) nausea 4) vomiting - DERM: 1) rashes - LOCAL: 1) pain (IM) 2) phlebitis (IV) 3) venous thrombosis - MISC: 1) physical & psychological depen-dence 2)tolerance NURSING IMPLICATIONS/RESPONSIBILITIES: - Monitor BP, PR,RR prior to periodically throughout therapy and frequently during IV therapy. - Assess IV site frequently during administration, diazepam may cause phlebitis and venous thrombosis. - Prolonged high-dose therapy may lead to psychological or physical dependence. Restrict amount of drug available to patient. Observe depressed patients closely for suicidal tendencies. - Observe and record intensity, duration and location of seizure activity. The initial dose of diazepam offers seizure control for 15-20 min after
administration. - IM injections are painful and erratically absorbed. If IM route is used, inject deeply into deltoid muscle for maximum absorption. - Caution patient to avoid taking alcohol or other CNS depressants concurrently with this medication. - Effectiveness of therapy can be demonstrated by decrease anxiety level; control of seizures; decreased tremulousness.
Generic and brand name: magnesium sulfate 250 mg/mL (25%) solution for injection Category: anticonvulsant Description: magnesium sulfate 250 mg/mL (25%) injection is a sterile, pyrogen-free solution of magnesium sulfate in water for injection. Formulation: Each mL contains: magnesium sulfate (anhydrous) = 250mg; water for injection, q.s. ad. = 1mL; no preservative added Mechanism of action: Magnesium sulfate inhibits convulsion by acting at the myoneural junction to prevent release of acetylcholine and to decrease the motor and plate potential. It inhibits the contraction of the uterus by directly acting on the myometrial cells and enhancing uterine blood flow. Indications: magnesium sulfate is indicated for the treatment of acute hypomagnesemia accompanied by signs of tetany, to control hypertension, encephalopathy and convulsions and for the prevention and control of convulsions in patients with pre-eclampsia or eclampsia. It is also used to prevent hypomagnesemia in patients receiving total parenteral nutrition (TPN). Dosage and administration: Magnesium deficiency, adult: 2 mL injected intramuscularly every 6 hours for 4 doses Nephritic seizures in children: 0.05 0.1 mL per kg body weight injected intramuscularly as needed Pre-eclampsia: 8 to 10 mL added into a 250 mL of 5% dextrose or 0.9% sodium chloride injection administered by intravenous infusion. Simultaneously, intramuscular dose of up to 20 mL of the undiluted solution may be given (10 mL in each buttock). Thereafter, 8 to 10 mL is injected intramuscularly into alternate buttocks depending on the presence of patellar reflex and adequate respiratory function. Therapy should be continued until paroxysms cease. Appropriate reduction in dosage should be made for patients with renal impairment.
Note: an isotonic solution of Magnesium Sulfate may be prepared by aseptically adding 7.3 mL of Magnesium Sulfate 250mg/mL injection to a 50mL of Sterile water for injection of other suitable parenteral solvent. Pharmacokinetics: About one third or orally administered Magnesium Sulfate is absorbed which is enhanced by the presence of the Vitamin D compound Calcitrol. It readily crosses the placenta but rarely causes toxicity to the neonate. Toxicity in the mother is indicated by the loss of patellar reflex which occurs when the blood level of magnesium is between 7 to 10 mEq/L. Adverse effects: Adverse effects due to high level of magnesium ion include flushing, sweating, hypotension, muscular weakness, sedation and confusion. As the blood level begins to exceed 4 mEq/L, deep tendon reflexes are decreased which may be absent at 10mEq/L. At 12 to 15 mEq/L, respiratory paralysis is a potential hazard. Treatment of Adverse effects: An injectable solution of calcium salt (i.e. as gluconate) should always be available for use as antidote. Calcium salt injection should be administered intravenously at a dose of up to 10mEq to counteract respiratory depression or heart block. If renal function is normal, adequate fluid should be given to assist removal of magnesium from the body. Dialysis may be necessary in patients with renal impairment or severe hypermagnesemia. Precaution: Use with extreme caution to patients with impaired renal function and those receiving digitalis glycosides. Magnesium Sulfate injection may enhance the effects of neuromuscular blocking agents. Contraindication: Magnesium Sulfate injection is contraindicated to patients with heart block or myocardial damage. Caution: foods drugs, devices and cosmetics act prohibits dispensing without prescription Storage condition: store at temperatures not exceeding 30 degrees Celsius. Availability: magnesium sulfate 250mg/mL (25%) injection is available in clear vials with 10 mL content.
You might also like
- High Alert MedicationsDocument17 pagesHigh Alert MedicationsJoanna Marie Datahan EstomoNo ratings yet
- TabletsDocument6 pagesTabletsRupesh Kumar DuttaNo ratings yet
- Fentanyl ParenteralDocument7 pagesFentanyl Parenteralstring44No ratings yet
- Drug Study 2Document8 pagesDrug Study 2rey_tengNo ratings yet
- Drug StudyDocument7 pagesDrug StudyJoy Jarin100% (1)
- Obat Emergensi Dalam AnestesiDocument32 pagesObat Emergensi Dalam AnestesiNaja NugrahaNo ratings yet
- OBG Latest DrugDocument71 pagesOBG Latest DrugT. Lamnunnem HaokipNo ratings yet
- ICU Drips: Stephanie Sanderson, RN, MSN, CNS, CCNS, CCRN Medical Cardiac ICU-UNMHDocument32 pagesICU Drips: Stephanie Sanderson, RN, MSN, CNS, CCNS, CCRN Medical Cardiac ICU-UNMHNicole Adkins100% (1)
- DRUG STUDY Magnesium SulfateDocument4 pagesDRUG STUDY Magnesium SulfateTempoNo ratings yet
- Drug StudyDocument16 pagesDrug StudyJibran Jones GarciaNo ratings yet
- Magnesium Sulfa-WPS OfficeDocument21 pagesMagnesium Sulfa-WPS OfficeNeha SinghNo ratings yet
- Cardiovascular Agent Central-Acting, Antihypertensive Autonomic Nervous System Agent Alpha-Adrenergic Agonist (Sympathomimetic)Document13 pagesCardiovascular Agent Central-Acting, Antihypertensive Autonomic Nervous System Agent Alpha-Adrenergic Agonist (Sympathomimetic)Maica EspañolaNo ratings yet
- Diazepam, Lanoxin, Hemostan, NaprexDocument6 pagesDiazepam, Lanoxin, Hemostan, NaprexRene John Francisco100% (1)
- Epinephrine and other emergency drug doses and indicationsDocument5 pagesEpinephrine and other emergency drug doses and indicationsColette Marie PerezNo ratings yet
- Antenatal Glucocorticoid Therapy and Fetal Lung MaturationDocument32 pagesAntenatal Glucocorticoid Therapy and Fetal Lung Maturationcclaire197% (37)
- Calcium Gluconate Drug Classification, Dosage and Side EffectsDocument4 pagesCalcium Gluconate Drug Classification, Dosage and Side EffectsStacy MC PelitoNo ratings yet
- Anasthetic DrugsDocument62 pagesAnasthetic DrugsMilda InayahNo ratings yet
- Availability: Verapamil HydrochlorideDocument21 pagesAvailability: Verapamil Hydrochloridesteffy sojanNo ratings yet
- Emergency Cardiac Medications for ArrhythmiasDocument14 pagesEmergency Cardiac Medications for ArrhythmiasRomzy BasañesNo ratings yet
- Emergency DrugsDocument15 pagesEmergency Drugsjheverly123100% (1)
- Drug Study On Emergency DrugsDocument16 pagesDrug Study On Emergency DrugsJosepNo ratings yet
- Drug Study On Emergency DrugsDocument15 pagesDrug Study On Emergency DrugsJAy TootNo ratings yet
- DrugsDocument5 pagesDrugsnurse_nurseNo ratings yet
- Action: Indications:: Drug: Oxygen Class of Medication: Oxidizing Agent (Gas)Document6 pagesAction: Indications:: Drug: Oxygen Class of Medication: Oxidizing Agent (Gas)Andreas100% (2)
- Lisinopril PDFDocument3 pagesLisinopril PDFHannaNo ratings yet
- NCP DrugDocument13 pagesNCP DrugMhar CamposanoNo ratings yet
- General Anesthetic Generic Name Brand NameDocument141 pagesGeneral Anesthetic Generic Name Brand NameLouise OpinaNo ratings yet
- Drug StudyDocument5 pagesDrug StudyKristoff CamposNo ratings yet
- Ecart For PrintingDocument10 pagesEcart For PrintingbluennaNo ratings yet
- Epinephrine: Uses, Dosages, Side EffectsDocument15 pagesEpinephrine: Uses, Dosages, Side EffectsDennise Juayang100% (1)
- Drug Study..DokcyDocument7 pagesDrug Study..DokcyPeArl Peralta0% (1)
- Casas - Mood StabilizersDocument16 pagesCasas - Mood StabilizersKarl Kuis SantanderNo ratings yet
- Emergency Drugs: (A Drug Study)Document13 pagesEmergency Drugs: (A Drug Study)Marichu BajadoNo ratings yet
- Topical corticosteroids, NSAIDs, beta-agonists, magnesium sulfate for medical conditionsDocument6 pagesTopical corticosteroids, NSAIDs, beta-agonists, magnesium sulfate for medical conditionsMegan LewisNo ratings yet
- Drug Presentation: Manisha M.Sc. Nursing 1 Year Con IlbsDocument57 pagesDrug Presentation: Manisha M.Sc. Nursing 1 Year Con IlbsManisha ShakyaNo ratings yet
- Drug StudyDocument12 pagesDrug StudyQueenie Gail Duarte RodrigoNo ratings yet
- Drugstudy OrsdDocument10 pagesDrugstudy OrsdRafmar A. SalundaguitNo ratings yet
- Labs Drug Study 1Document17 pagesLabs Drug Study 1Drei LanuzoNo ratings yet
- Drugs Used in Cardiac EmergenciesDocument18 pagesDrugs Used in Cardiac Emergencieshakky gamyNo ratings yet
- Midazolam (Dormicum) GuideDocument8 pagesMidazolam (Dormicum) Guidekarenkaren09No ratings yet
- Emergency Drugs Drug StudyDocument15 pagesEmergency Drugs Drug StudyCathrine Sandile Tangwara100% (1)
- Drug StudyDocument9 pagesDrug StudyChristine PunsalanNo ratings yet
- Magnesium SulfateDocument2 pagesMagnesium SulfateKarla Karina Dela CruzNo ratings yet
- Control Status Epilepticus SeizuresDocument35 pagesControl Status Epilepticus SeizuresLussy HendrikNo ratings yet
- FINAL Drug StudyDocument9 pagesFINAL Drug StudyKristen Leigh MarianoNo ratings yet
- CARDIO Intensive CareDocument6 pagesCARDIO Intensive CareDianne Erika MeguinesNo ratings yet
- Local Anesthetics (Slide Show)Document24 pagesLocal Anesthetics (Slide Show)Sheena Lou Regencia SalomonNo ratings yet
- Nalepsin: Presentation Drug InteractionsDocument1 pageNalepsin: Presentation Drug InteractionsAbid Hasan ZiKonNo ratings yet
- Side Effects:: AtropineDocument7 pagesSide Effects:: AtropinekletadaNo ratings yet
- Drug 25Document17 pagesDrug 25carol_gigliotti24100% (1)
- Drug Action Indication Adverse Effects Contraindications Nursing Considerations Ketorolac TromethamineDocument8 pagesDrug Action Indication Adverse Effects Contraindications Nursing Considerations Ketorolac TromethamineAiryn CanonNo ratings yet
- DRUG STUDY MAGNESIUM SULFATEDocument7 pagesDRUG STUDY MAGNESIUM SULFATEminervanatividadNo ratings yet
- Drug StudyDocument10 pagesDrug StudyFranco ObedozaNo ratings yet
- Chew, swallow or crush mebendazole tabletsDocument6 pagesChew, swallow or crush mebendazole tabletsDenvicNo ratings yet
- ImipramineDocument6 pagesImipramineMuhammed Faruk JambazNo ratings yet
- Hypoglycemia, A Simple Guide To The Condition, Treatment And Related ConditionsFrom EverandHypoglycemia, A Simple Guide To The Condition, Treatment And Related ConditionsNo ratings yet
- Naplex Complete Study Outline A Topic-Wise Approach DiabetesFrom EverandNaplex Complete Study Outline A Topic-Wise Approach DiabetesRating: 4 out of 5 stars4/5 (2)
- LeptospirosisDocument17 pagesLeptospirosisStacy MC PelitoNo ratings yet
- Cloxacillin, Sodium: How Should I Take Cloxacillin?Document7 pagesCloxacillin, Sodium: How Should I Take Cloxacillin?Stacy MC PelitoNo ratings yet
- Calcium Gluconate Drug Classification, Dosage and Side EffectsDocument4 pagesCalcium Gluconate Drug Classification, Dosage and Side EffectsStacy MC PelitoNo ratings yet
- Pyramids: King Snefru's Bent PyramidDocument4 pagesPyramids: King Snefru's Bent PyramidStacy MC PelitoNo ratings yet
- Adult Sarcomas: Learning ObjectivesDocument32 pagesAdult Sarcomas: Learning ObjectivesabdullahNo ratings yet
- Farmasi Sosial: Niken N. WidyakusumaDocument14 pagesFarmasi Sosial: Niken N. WidyakusumaNiken Nur WidyakusumaNo ratings yet
- Med Math Practice TestDocument2 pagesMed Math Practice TestTad McDowell100% (1)
- Review 1. Efficacy and Safety of Cetuximab For CRCDocument13 pagesReview 1. Efficacy and Safety of Cetuximab For CRCcollianairaNo ratings yet
- Colorado Guidelines of Professional Practice For Controlled SubstancesDocument65 pagesColorado Guidelines of Professional Practice For Controlled SubstancesBrian HarrisNo ratings yet
- Format Rko 2024Document44 pagesFormat Rko 2024Muhammad_Azzam_BNo ratings yet
- Phenytoin PAR 45Document65 pagesPhenytoin PAR 45Lourdes VictoriaNo ratings yet
- A 21 Year Old Female, 50 KG, Was Scheduled For Excision of Left Breast Mass. VS Are As Follows: BP 100/70, PR 75/min, RR 16/min, Temperature 37°CDocument4 pagesA 21 Year Old Female, 50 KG, Was Scheduled For Excision of Left Breast Mass. VS Are As Follows: BP 100/70, PR 75/min, RR 16/min, Temperature 37°CKat JolejoleNo ratings yet
- Oral Paracetamol Prescribing Guideline Oct 2018 PDFDocument2 pagesOral Paracetamol Prescribing Guideline Oct 2018 PDFBeby SartikaNo ratings yet
- List-of-Drug-Manufacturing 1Document66 pagesList-of-Drug-Manufacturing 1Guru KrupaNo ratings yet
- List of Medicines For Ethiopia: Sixth EditionDocument152 pagesList of Medicines For Ethiopia: Sixth EditionportosinNo ratings yet
- Hospital PharmacyDocument22 pagesHospital PharmacyAkash PawarNo ratings yet
- Elekta Infinity BrochureDocument7 pagesElekta Infinity BrochurebennyNo ratings yet
- Chapter Narcotic Drugs and Psychotropic Substances Act 1985 andDocument4 pagesChapter Narcotic Drugs and Psychotropic Substances Act 1985 andSyrax ImNo ratings yet
- Miconazole Oral Gel and Drug InteractionsDocument4 pagesMiconazole Oral Gel and Drug InteractionsWeng AceNo ratings yet
- 1 - Pharmacokinetics IDocument20 pages1 - Pharmacokinetics IabdallaNo ratings yet
- Pharmacology Case StudyDocument2 pagesPharmacology Case StudyNur SanaaniNo ratings yet
- Lasa Meds List Hqe-1Document2 pagesLasa Meds List Hqe-1Ann CatherynNo ratings yet
- Jco.2022.40.17 Suppl - Lba6003Document1 pageJco.2022.40.17 Suppl - Lba6003Paulo Roberto Zanfolim GarciaNo ratings yet
- Basic Life Support Field GuideDocument56 pagesBasic Life Support Field GuidelmaoheartsNo ratings yet
- 1 - Pharmaceutical Dosage FormsDocument41 pages1 - Pharmaceutical Dosage FormsVaibhav Harish KumarNo ratings yet
- Pharmacology Questions (CNS Drugs) PDFDocument12 pagesPharmacology Questions (CNS Drugs) PDFRuva Oscass JimmyNo ratings yet
- Ayurvedic Package Vasundhara Sarovar Premiere Vayalar Kerala Vby6sqDocument5 pagesAyurvedic Package Vasundhara Sarovar Premiere Vayalar Kerala Vby6sqHarish LakshminarayananNo ratings yet
- SIPDocument6 pagesSIPPutri FebriyaniNo ratings yet
- Preface: Encyclopedia (Marshall Sittig, Noyes Publications, WestwoodDocument4 pagesPreface: Encyclopedia (Marshall Sittig, Noyes Publications, WestwoodJulcon Avanceña AraizNo ratings yet
- 1 PBDocument14 pages1 PBindah marhaniNo ratings yet
- Airway ManagementDocument4 pagesAirway Managementpaveethrah100% (1)
- Reporting Form for Suspected ASU Drug ReactionsDocument2 pagesReporting Form for Suspected ASU Drug ReactionsSachin JadonNo ratings yet
- 02-05 2022 Pharm Pharmacokinetics 2022 R3Document38 pages02-05 2022 Pharm Pharmacokinetics 2022 R3Amira HelayelNo ratings yet
- Instructions - For - Use ValtocoDocument2 pagesInstructions - For - Use Valtocofreebass08No ratings yet