Professional Documents
Culture Documents
Chapter 35 Interventions For Critically Ill Clients With Respiratory Problems
Uploaded by
Tina TalmadgeOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Chapter 35 Interventions For Critically Ill Clients With Respiratory Problems
Uploaded by
Tina TalmadgeCopyright:
Available Formats
Chapter 35: Interventions for Critically Ill Clients with Respiratory Problems Elsevier Inc.
items and derived items 2006, 2002 by Elsevier Inc.
MULTIPLE CHOICE 1. Which client is at greatest risk for the development of a pulmonary embolism? A. 40-year-old woman who has used oral contraceptives for the past 15 years and who had abdominal surgery yesterday for cancer B. 60-year-old man who caught his right hand in a piece of machinery and has five broken fingers, with extensive soft tissue damage C. 30-year-old athlete who lifts weights and was diagnosed with a pneumothorax yesterday D. 50-year-old woman who has fragile capillaries and bruises very easily ANS: A This client has several risk factors. She is at risk for deep vein thrombosis because of oral contraceptive use. The abdominal surgery also increases her risk, as does a diagnosis of cancer. DIF: Cognitive Level: Comprehension TOP: Nursing Process Step: Assessment MSC: Client Needs Category: Physiological Integrity 2. Which client is at greatest risk for development of fat emboli leading to pulmonary embolism? A. 70-year-old man who is easily dehydrated because of drug-induced diabetes insipidus B. 70-year-old woman who has a recurrence of breast cancer C. 36-year-old man who fractured his femur 2 days ago D. 36-year-old woman who is 50 pounds overweight ANS: C The marrow of long bones, including the femur, has a large amount of fat. This fat can be released when the femur is fractured, forming a large fat embolism that can lodge in the blood vessels of the lungs. Unfortunately, there is no way to prevent such an event. DIF: Cognitive Level: Comprehension TOP: Nursing Process Step: Assessment MSC: Client Needs Category: Physiological Integrity 3. Which diagnostic test most specifically confirms the presence of a pulmonary embolism? A. Chest x-ray B. Arterial blood gases
Copyright 2006, 2002 by Elsevier Inc.
C. Pulmonary angiography D. Ventilation-perfusion lung scan ANS: C Pulmonary angiography actually determines the presence of a substance within the pulmonary vasculature. The other tests provide inferential data that are not specific for only pulmonary embolism. DIF: Cognitive Level: Comprehension TOP: Nursing Process Step: Assessment MSC: Client Needs Category: Physiological Integrity 4. Which statement made by a clients spouse indicates the need for more teaching about prevention of a pulmonary embolism at home after major abdominal surgery? A. While he is awake, I will make sure he gets up and walks for at least 5 minutes every 2 hours. B. He is prone to constipation, so I will increase the amount of fiber in his meals every day. C. I will massage his feet and legs twice a day to help blood return. D. I will check his breathing rate and level twice a day. ANS: C It is possible that massaging the feet and legs could promote venous return; however, there is a greater danger of loosening a clot that may have formed in the deep veins of the legs, which would allow it to move. Thus, after surgery, the feet and legs of a client should never be massaged. DIF: Cognitive Level: Application or higher TOP: Nursing Process Step: Implementation/Intervention MSC: Client Needs Category Health Promotion and Maintenance 5. Which set of arterial blood gases would the nurse expect to find in a client who developed a pulmonary embolism 15 minutes ago? A. pH 7.30, HCO3 22 mEq/L, PCO2 60 mm Hg, PO2 66 mm Hg B. pH 7.38, HCO3 22 mEq/L, PCO2 45 mm Hg, PO2 96 mm Hg C. pH 7.47, HCO3 23 mEq/L, PCO2 25 mm Hg, PO2 82 mm Hg D. pH 7.30, HCO3 28 mEq/L, PCO2 65 mm Hg, PO2 75 mm Hg ANS: C
Early changes in blood gases reflect the respiratory alkalosis caused by the hyperventilation due to pain, hypoxia, and anxiety. Such a problem results in excessive loss of carbon dioxide, even though the client is somewhat hypoxic at this time. The reduced partial pressure of carbon dioxide results in a diminished hydrogen concentration and a higher than normal pH. DIF: Cognitive Level: Application or higher TOP: Nursing Process Step: Assessment MSC: Client Needs Category: Physiological Integrity 6. Which set of arterial blood gases would the nurse expect to find in a client who developed a pulmonary embolism 6 hours ago? A. pH 7.30, HCO3 22 mEq/L, PCO2 60 mm Hg, PO2 66 mm Hg B. pH 7.38, HCO3 22 mEq/L, PCO2 45 mm Hg, PO2 96 mm Hg C. pH 7.47, HCO3 23 mEq/L, PCO2 25 mm Hg, PO2 82 mm Hg D. pH 7.30, HCO3 28 mEq/L, PCO2 65 mm Hg, PO2 75 mm Hg ANS: A As this condition of poor gas exchange continues in the client with a PE, blood flowing through the lungs does not receive adequate oxygenation and carbon dioxide is retained, causing an increase in hydrogen ions and a decreased pH indicative of respiratory acidosis. If this condition continues further, the hypoxia results in greater production of carbon dioxide production, resulting in a metabolic acidosis as well as a respiratory acidosis. The bicarbonate level remains normal because not enough time has passed to trigger renal compensation for the acidosis. DIF: Cognitive Level: Application or higher TOP: Nursing Process Step: Assessment MSC: Client Needs Category: Physiological Integrity 7. A client who is 2 days postoperative from a bowel resection tells her nurse that she is having a hard time catching her breath, feels nauseated, and has chest pains when she inhales. The nurse suspects that she is having a pulmonary embolism. What intervention should the nurse perform before notifying the physician? A. Increase the IV flow rate. B. Apply oxygen by mask or nasal cannula at 5 L/min. C. Assess the chest and axillary area for the presence of petechiae. D. Place the client in shock position, with her head and neck flat and her legs elevated. ANS: B
Copyright 2006, 2002 by Elsevier Inc.
If this client is having a pulmonary embolism, she is hypoxic and at risk for other complications and tissue damage. Applying oxygen in this situation can be helpful and is unlikely to cause any problems. Increasing the IV flow rate and assessing for petechiae will not prevent problems. Both of these actions can be performed after the physician is notified. Placing the client in shock position will not improve the hypoxia and may increase the extent of the pulmonary vascular block. DIF: Cognitive Level: Application or higher TOP: Nursing Process Step: Implementation/Intervention MSC: Client Needs Category: Safe, Effective Care Environment; 8. The client is receiving heparin therapy for a pulmonary embolism. Which partial thromboplastin times indicates to the nurse that anticoagulation is adequate? A. The client's PPT is the same as the control value. B. The client's PPT is one half the control value. C. The client's PPT is 5 times the control value. D. The client's PPT is twice the control value. ANS: D Therapeutic PPT values for clients receiving heparin should range between 1.5 and 2.5 times the control value. DIF: Cognitive Level: Application or higher TOP: Nursing Process Step: Evaluation MSC: Client Needs Category: Physiological Integrity 9. A nurse discovers that a physician has prescribed that the client with a pulmonary embolism be started on oral warfarin while still receiving intravenous heparin. What is the nurses best action? A. Administer the medications as prescribed. B. Remind the physician that two anticoagulants should not be administered concurrently. C. Hold the dose of warfarin until the client's partial thromboplastin time is the same as the control value. D. Monitor the client for clinical manifestations of internal or external bleeding at least every 2 hours. ANS: A Although both heparin and warfarin are anticoagulants, they have different mechanisms of action and onsets of action. Because warfarin has such a slow onset, it must be started while the client is still receiving heparin. DIF: Cognitive Level: Application or higher TOP: Nursing Process Step: Implementation/Intervention
MSC: Client Needs Category: Physiological Integrity 10. The client with a massive pulmonary embolism is receiving alteplase (Activase). What is the priority nursing diagnosis or collaborative problem for this client? A. Risk for Impaired Adjustment B. Ineffective Breathing Pattern C. Potential for Anaphylaxis D. Risk for Injury (Bleeding) ANS: D Alteplase is a fibrinolytic agent that dissolves formed clots. The dose of fibrinolytic agents for PE is far higher than the dose used to treat clots in a coronary artery. The drug has an impact on clots outside of the pulmonary embolism and the client is at great risk for hemorrhage and shock. The client with a PE already has an impaired breathing pattern and the alteplase will not worsen this problem. Alteplase, unlike urokinase, is a totally synthetic drug and does not stimulate allergic or anaphylactic reactions. The client may be concerned about his or her family and professional roles but at this time, the risk for bleeding has a higher priority than this psychosocial issue. DIF: Cognitive Level: Application or higher TOP: Nursing Process Step: Analysis MSC: Client Needs Category: Safe, Effective Care Environment; 11. Which intervention should the nurse suggest for the client going home after a pulmonary embolism to reduce the risk for recurrence of a pulmonary embolism? A. Avoid bending over at the waist. B. Avoid prolonged sitting or standing. C. Apply ice immediately to any site of injury. D. Use an incentive spirometer every 2 hours while awake. ANS: B Prolonged sitting or standing contributes to increased venous stasis in the legs, increasing the risk for formation of a thrombus or embolus. DIF: Cognitive Level: Application or higher TOP: Nursing Process Step: Implementation/Intervention MSC: Client Needs Category Health Promotion and Maintenance 12. Which statement made by the client who has respiratory problems indicates the presence of orthopnea? A. I have to stop to catch my breath halfway up a flight of stairs. B. At night, I need to sleep either on three pillows or in my recliner. C. It seems I cant speak a complete sentence without stopping for breath. Copyright 2006, 2002 by Elsevier Inc.
D. When I am eating a meal, I notice my heart usually starts to beat hard and fast. ANS: B Orthopnea is the sensation of dyspnea or breathlessness in the supine position. Clients feel that they cannot catch their breath in the supine position and must rest or sleep in a semisitting position by placing pillows behind their backs or by using a reclining chair. The degree of breathlessness can be roughly measured by the number of pillows needed to make the client less dyspneic (e.g., one-pillow orthopnea, two-pillow orthopnea). DIF: Cognitive Level: Application or higher TOP: Nursing Process Step: Assessment/Analysis MSC: Client Needs Category: Physiological Integrity 13. What precaution should the nurse give in preparation for self-care to a person who will be taking warfarin (Coumadin) for 6 months? A. Decrease your intake of sodium. B. Your blood-clotting time will decrease. C. Increase your intake of multiple vitamins. D. Avoid aspirin and aspirin-containing drugs. ANS: D Warfarin inhibits synthesis of vitamin Kdependent clotting factors. Aspirin inhibits platelet aggregation. These two mechanisms greatly increase the client's risk for uncontrollable bleeding. DIF: Cognitive Level: Application or higher TOP: Nursing Process Step: Implementation/Intervention MSC: Client Needs Category Health Promotion and Maintenance 14. The client with a pulmonary embolism is receiving an intravenous heparin drip. The nurse should make certain which agent is readily available? A. Fresh-frozen plasma B. Protamine sulfate C. Cryoprecipitate D. Vitamin K ANS: B Protamine sulfate is an antidote for heparin. DIF: Cognitive Level: Application or higher TOP: Nursing Process Step: Implementation/Intervention MSC: Client Needs Category: Physiological Integrity
15. Which statement, made by the client who is taking warfarin (Coumadin) daily to prevent blood clots from forming in deep veins, indicates a need for further discussion regarding this therapy? A. I have been eating more salads and other green, leafy vegetables to prevent constipation. B. I have two pairs of antiembolic stockings so that one pair can be washed each day. C. Instead of a safety razor, I have been using an electric shaver to shave. D. On hot days, I make sure I drink at least two quarts of water. ANS: A Vitamin K, present in green, leafy vegetables, enhances blood clotting by increasing the synthesis of specific clotting factors in the liver. Warfarin is a vitamin K antagonist. Ingestion of large amounts of vitamin K can counteract the therapeutic effects of warfarin and reduce the INR until it is no longer within the therapeutic range. This information is critical in preparing a client for self care. DIF: Cognitive Level: Application or higher TOP: Nursing Process Step: Evaluation MSC: Client Needs Category Health Promotion and Maintenance 16. Which client is at greatest risk for ARDS? A. The 62-year-old with COPD who has pneumonia B. The 22-year-old who received 10 units of blood after a motor vehicle crash C. The 78-year-old with chronic congestive heart failure and pulmonary edema D. The 24-year-old with asthma who has not taken any of her asthma medications for 2 weeks ANS: B Extensive trauma alone can cause an excessive release of intracellular enzymes that can damage lung cells and lead to ARDS. The 10 units of blood indicate severe trauma. In addition, with massive transfusions, there is redistribution of large volumes of blood into the pulmonary circulation, which increases pulmonary capillary hydrostatic pressure. This contributes to the movement of fluid into lung tissue, causing noncardiac pulmonary edema. Plasma proteins from this edema start inflammatory processes in the lung tissues that lead to ARDS. DIF: Cognitive Level: Comprehension TOP: Nursing Process Step: Assessment MSC: Client Needs Category: Physiological Integrity 17. The client at risk for acute respiratory distress syndrome (ARDS) has become cyanotic and is diaphoretic. What assessment technique should the nurse perform next? A. Measure pulse oximetry.
Copyright 2006, 2002 by Elsevier Inc.
B. Auscultate breath sounds bilaterally. C. Measure the blood pressure in both arms. D. Compare current ECG tracing with baseline measurement. ANS: A In early ARDS, hypoxemia may be the only abnormal assessment finding and can be life threatening. DIF: Cognitive Level: Application or higher TOP: Nursing Process Step: Implementation/Intervention MSC: Client Needs Category: Physiological Integrity 18. What is the most important intervention for the client with ARDS? A. Antibiotic therapy B. Bronchodilators C. Oxygen therapy D. Diuretic therapy ANS: C Although the client with ARDS may not respond to oxygen therapy to the same degree as clients who have other types of respiratory problems, oxygen is still the most important intervention. Without oxygen therapy, the client with ARDS will always die of respiratory failure. DIF: Cognitive Level: Comprehension TOP: Nursing Process Step: Implementation/Intervention MSC: Client Needs Category: Physiological Integrity 19. The client with respiratory difficulty has a V/Q ratio of 0.5. What is the significance of this value? A. The ratio is low; ventilation is exceeding perfusion. B. The ratio is low; perfusion is exceeding ventilation. C. The ratio is high; ventilation is exceeding perfusion. D. The ratio is high; perfusion is exceeding ventilation. ANS: B
When ventilation and perfusion match, the ratio is or approaches 1. When this ratio is less than 1, ventilation is decreased and is not matched with perfusion. Ventilation and perfusion are not the same throughout, even in healthy lungs. Perfusion is greater at the bases of the lungs and ventilation is greater at the apices of the lungs. Therefore, the normal V/Q ratio for the entire lung is about 0.8. When the V/Q ratio is 0.5, essentially blood flow through some area is occurring, but the blood is not becoming oxygenated because ventilation is less than adequate. DIF: Cognitive Level: Application or higher TOP: Nursing Process Step: Analysis MSC: Client Needs Category: Physiological Integrity 20. What is the priority nursing diagnosis for a client who is in phase 4 of the course of ARDS and is being mechanically ventilated? A. Fatigue B. Risk for Infection C. Risk for Social Isolation D. Impaired Gas Exchange ANS: B Although the client cannot breathe well on his or her own, mechanical ventilation is maintaining adequate oxygenation. However, mechanical ventilation is an invasive intervention and greatly increases the client's risk for infection and sepsis, a common cause of death in this population. DIF: Cognitive Level: Application or higher TOP: Nursing Process Step: Analysis MSC: Client Needs Category: Safe, Effective Care Environment; 21. Which of the following clients could be expected to require mechanical ventilation longterm? A. 27-year-old with status asthmaticus B. 45-year-old with morphine overdose C. 24-year-old with muscular dystrophy D. 65-year-old with bilateral bacterial pneumonia ANS: C Clients who have chronic, progressive neuromuscular diseases that preclude spontaneous ventilation require mechanical ventilation for life. The health problems of status asthmaticus, morphine overdose, and pneumonia are all acute but short-term issues requiring relatively brief ventilatory support. DIF: Cognitive Level: Comprehension TOP: Nursing Process Step: Assessment MSC: Client Needs Category: Physiological Integrity
Copyright 2006, 2002 by Elsevier Inc.
22. What is the main purpose of a negative-pressure ventilator? A. Healing diseased lung tissue B. Relieving hypoxemia by opening obstructed airways C. Assisting ventilation to healthy lungs by mimicking normal chest pressures D. Delivering an individualized preset tidal volume to the lower respiratory tract ANS: C The negative-pressure ventilator is noninvasive and works by changing pressures in the chest cavity rather than by forcing air directly into the lungs. The client is placed in an airtight tube that surrounds either the chest area or the entire body and leaves the head exposed. During inspiration, with the expansion of the chest wall, negative pressure is generated in the chest cavity. Because of the pressure gradient, air moves from the atmosphere (high pressure) into the thoracic cavity (low pressure). At a preset time, negative pressure ceases and expiration occurs. Thus, negative-pressure ventilators create pressure gradients that mimic normal ventilation. DIF: Cognitive Level: Comprehension TOP: Nursing Process Step: Assessment MSC: Client Needs Category: Physiological Integrity 23. A nurse is starting a new shift and assessing the client who has an oral endotracheal tube in place. Which finding requires immediate intervention? A. The client has been intubated for four days. B. The endotracheal tube is midline in the mouth. C. The endotracheal tube is taped to the lower jaw. D. The client has hydrocolloid membrane on the skin of the cheeks. ANS: C The endotracheal tube can be taped to the upper lip but should never be taped to the lower jaw because the lower jaw moves too much. DIF: Cognitive Level: Application or higher TOP: Nursing Process Step: Evaluation MSC: Client Needs Category: Safe, Effective Care Environment; 24. Which situation indicates that a nurse needs to perform endotracheal suctioning of the client who is being mechanically ventilated? A. The client is talking around the endotracheal tube. B. Condensation is present in the ventilator tubing. C. Breath sounds are heard only in one lung. D. Wheezes are auscultated.
ANS: D The presence of wheezes (rhonchi) indicates partial obstruction by secretions. Although the fact that breath sounds are heard only in one lung represents a problem, it cannot be helped by suctioning the endotracheal tube. DIF: Cognitive Level: Application or higher TOP: Nursing Process Step: Implementation/Intervention MSC: Client Needs Category: Safe, Effective Care Environment/Physiological Integrity; 25. The pilot balloon on the endotracheal tube of a client being mechanically ventilated is completely deflated. What is the consequence of this situation? A. The client's lungs may not be receiving the set tidal volume. B. The client has no airway and must be reintubated. C. The endotracheal tube is too small for the client. D. The client's residual volume is too low. ANS: A The pilot balloon indicates whether the endotracheal tube cuff is inflated or deflated. A deflated balloon means that the cuff is also deflated and there is no longer a seal around the tube to prevent air from escaping. Thus, some of the air being moved into the clients airway by the ventilator is escaping through the client's trachea before it reaches the lower airways and alveoli. DIF: Cognitive Level: Application or higher TOP: Nursing Process Step: Analysis MSC: Client Needs Category: Safe, Effective Care Environment/Physiological Integrity; 26. Which intervention promotes a more normal V/Q match for a client receiving mechanical ventilation? A. Administering the prescribed muscle-paralyzing agents B. Positioning the client so that the healthier lung is dependent to the more diseased lung C. Ensuring that the pilot balloon on the endotracheal tube cuff is inflated to its maximal pressure D. Auscultating the lungs bilaterally every 4 hours for the presence of crackles, wheezes, and other abnormal breath sounds ANS: B Clients who are being mechanically ventilated are experiencing a problem in which their normal ventilation is not adequate. (Mechanical ventilation does not improve pulmonary perfusion). The recommended position for clients who have one lung affected by a problem more than the other lung is to place the good lung down, keeping the healthier lung dependent to the less healthy lung. Such positioning allows gravity to keep more blood in the lower lung (healthier lung) and better ventilation in the upper lung. Copyright 2006, 2002 by Elsevier Inc.
DIF: Cognitive Level: Application or higher TOP: Nursing Process Step: Analysis MSC: Client Needs Category: Physiological Integrity 27. Two hours after the client with an endotracheal tube has been extubated, a nurse hears stridor on inhalation. What is the nurses best next action after applying humidified oxygen? A. Document the observation as the only action. B. Ask the client to cough and deep breathe. C. Suction the client's mouth and pharynx. D. Notify the emergency team. ANS: D Stridor on inspiration is caused by laryngospasm or edema and heralds impending airway occlusion. The client's airway is in jeopardy and the physician must take immediate action by prescribing an aerosol vasoconstrictor or by reintubating the client. DIF: Cognitive Level: Application or higher TOP: Nursing Process Step: Analysis MSC: Client Needs Category: Safe, Effective Care Environment/Physiological Integrity; 28. Which assessment finding alerts the nurse to the possibility that the intrathoracic pressure in a mechanically ventilated client is too high? A. Hypotension B. Pulse oximetry value of 96% C. Increased diaphragmatic excursion D. Low-pressure alarm sounds on the ventilator ANS: A Increased intrathoracic pressure can inhibit blood return to the heart and cause decreased cardiac output. DIF: Cognitive Level: Application or higher TOP: Nursing Process Step: Evaluation MSC: Client Needs Category: Safe, Effective Care Environment/Physiological Integrity; 29. The client being mechanically ventilated has become more restless over the course of the shift. What is the nurses best action? A. Darken the room and ask visitors to leave. B. Document the observation as the only action. C. Administer a dose of pain medication or sedative. D. Check the client's oxygen saturation by pulse oximetry.
ANS: D Increasing restlessness in a client being mechanically ventilated may mean that the client is not receiving sufficient oxygen and may be air hungry. It can also be a manifestation of pain. When in doubt, determining the adequacy of ventilation has the highest priority. DIF: Cognitive Level: Application or higher TOP: Nursing Process Step: Implementation/Intervention MSC: Client Needs Category: Physiological Integrity 30. The pressure reading on the ventilator of a client receiving mechanical ventilation is fluctuating widely. What is the correct action to take for this problem? A. Determine whether there is an air leak in the clients endotracheal tube cuff. B. Increase the tidal volume by at least 100 mL or by the clients weight in kg. C. Assess the clients oxygen saturation to determine the adequacy of oxygenation. D. Disconnect the ventilator from the client and use a manual resuscitation bag until the machine has been checked. ANS: C A widely fluctuating pressure reading is one indication of inadequate flow and oxygenation. The client may be air hungry from hypoxia. Check the clients oxygen saturation to determine the adequacy of oxygenation and, if the saturation is less than adequate, increase the flow rate setting on the ventilator. DIF: Cognitive Level: Application or higher TOP: Nursing Process Step: Assessment/Evaluation MSC: Client Needs Category: Physiological Integrity 31. The client sustained an injury to the chest in a motor vehicle crash. Which assessment finding 3 hours later alerts the nurse to a possible pulmonary contusion? A. Dyspnea B. Hemoptysis C. Hyperresonance on percussion D. Increased chest pain with movement ANS: B Interstitial hemorrhage accompanies pulmonary contusion. Bleeding may not be evident at the initial injury, but the client develops hemoptysis and decreased breath sounds up to several hours after injury as bleeding into the alveoli or airways occurs. DIF: Cognitive Level: Application or higher TOP: Nursing Process Step: Analysis MSC: Client Needs Category: Physiological Integrity Copyright 2006, 2002 by Elsevier Inc.
32. What is the priority nursing diagnosis for the client with an uncomplicated rib fracture? A. Ineffective Breathing Pattern B. Impaired Gas Exchange C. Activity Intolerance D. Acute Pain ANS: D Treatment for uncomplicated rib fractures is nonspecific because the fractured ribs unite spontaneously. Movement of the ribs during inhalation (and on exhalation, to some extent) increases the pain. Clients may breathe so shallow to reduce the pain that their breathing pattern becomes ineffective secondary to compensation for the pain. The primary consideration is to decrease pain so that adequate ventilatory status is maintained. DIF: Cognitive Level: Application or higher TOP: Nursing Process Step: Analysis MSC: Client Needs Category: Physiological Integrity 33. The client has experienced left-sided chest trauma 3 hours ago, which included simple fractures of three ribs. The nurse now finds the client to have increased dyspnea, pulse oximetry of 86%, and tracheal deviation to the right. What is the nurses interpretation of these findings? A. Flail chest B. Pulmonary contusion C. Tension pneumothorax D. Acute respiratory distress syndrome ANS: C Blunt chest trauma can cause an air leak into the thoracic cavity, collapsing the lung on the side with the air leak. More air enters the pleural space with each breath, increasing intrathoracic pressure on the affected side, moving the trachea to the unaffected side, and leading to decreased cardiac output. This condition is life threatening without intervention. DIF: Cognitive Level: Application or higher TOP: Nursing Process Step: Analysis MSC: Client Needs Category: Physiological Integrity 34. The client who has experienced blunt trauma to the chest is at risk for developing a hemothorax. Which would the nurse expect to find in a client with a hemothorax? A. Hemoptysis B. Paradoxical chest movements C. Percussion dullness on affected side
D. Hypertympanic sound on affected side ANS: C A hemothorax involves bleeding into the thoracic cavity (not into the pulmonary tree so hemoptysis does not occur), decreasing lung inflation on the affected side. As a result of decreased lung inflation, percussion sounds become duller and less resonant. DIF: Cognitive Level: Application or higher TOP: Nursing Process Step: Assessment MSC: Client Needs Category: Physiological Integrity 35. For the client who has sustained tracheobronchial trauma, which assessment finding alerts the nurse to the possibility of tracheal lacerations? A. Hypertympanic sound on affected side B. Subcutaneous emphysema over the trachea C. Hypotension and decreased capillary refill D. Deviation of the trachea to the affected side ANS: B Lacerations of the trachea cause massive air leaks, which manifest as extensive subcutaneous emphysema and air in the mediastinum. DIF: Cognitive Level: Application or higher TOP: Nursing Process Step: Analysis MSC: Client Needs Category: Physiological Integrity 36. The client in a nursing home became confused and climbed out of bed (over the siderails) without assistance, falling onto a vacuum cleaner temporarily left there by the cleaning staff. Which respiratory assessment finding indicates to the nurse that the client may have a flail chest as a result of this incident? A. Wheezes are present and are heard more loudly when the client inhales compared with what is heard on exhalation. B. An area on the clients left chest is sucked in during inhalation and puffs out during exhalation. C. The client is coughing copious amounts of frothy white sputum. D. The client cannot speak more than six words between breaths. ANS: B
Copyright 2006, 2002 by Elsevier Inc.
Flail chest is the inward movement of the thorax during inspiration, with outward movement during expiration. It usually involves one side of the chest and results from multiple rib fractures caused by blunt chest trauma, leaving a segment of the chest wall loose. The movement of this loose segment becomes paradoxical to the expansion and contraction of the rest of the chest wall. It occurs more commonly in older adults who experience chest trauma. DIF: Cognitive Level: Application or higher TOP: Nursing Process Step: Assessment MSC: Client Needs Category: Physiological Integrity OTHER 1. Indicate which manifestations are associated with a pulmonary embolism. (Select all that apply.) A. Chest pain on inhalation B. Dyspnea C. Hemoptysis D. Muffled heart sounds E. Muscle weakness on one side F. Tachycardia ANS: A, B, C, F Rationale: Not every person with a PE has all manifestations. Most clients have chest pain on inhalation as a result of increased pressure in one area of the chest and possible vasospasms around the embolism. Because the oxygen in the alveoli beyond the area of the clot is not being exchanged into the blood, hypoxia develops. As a result, the client feels short of breath. The cardiac system attempts to compensate for this hypoxia by increasing the heart rate. Hemoptysis may be present if there is bleeding into the alveoli from increased pulmonary vascular pressure in front of the clot. DIF: Cognitive Level: Comprehension TOP: Nursing Process Step: Assessment MSC: Client Needs Category: Physiological Integrity 2. The client is to be extubated from the ventilator after having received mechanical ventilation for 4 days. The client is alert and oriented. Indicate in which order the following steps should be performed. A. Deflate the endotracheal tube cuff. B. Ensure that emergency intubation equipment is at the bedside. C. Explain the entire procedure to the client. D. Give oxygen by face mask or nasal cannula. E. Hyperoxygenate the client. F. Instruct the client to cough. G. Rapidly remove the tube at peak inspiration. H. Suction the endotracheal tube and oral cavity. I. Tell the client to take a deep breath. ANS:
C, B, E, H, A, I, G, F, D Rationale: Extubation is the removal of the endotracheal (ET) tube. The tube is removed when the need for intubation has been resolved. Before removal, explain to the client exactly what is to be done to him or her and what will be expected of the client during the procedure. Such explanations not only reduce anxiety, but they also help ensure the clients cooperation. Set up the prescribed oxygen delivery system at the bedside and bring in the equipment for emergency reintubation. The criteria for extubation are not exact and the client may not be ready for extubation. Keeping reintubation equipment on hand prevents a delay should reintubation become necessary. Hyperoxygenate the client and thoroughly suction both the ET tube and the oral cavity. Suctioning removes any secretions that have collected in or around the tube and ensures that the secretions will not move further down the airway once extubation has been accomplished. Hyperoxygenating the client before extubation prevents hypoxia during the procedure. Then rapidly deflate the cuff of the ET tube and remove the tube at peak inspiration. The cuff must be deflated to prevent injury to the airway tissue. Removal of the tube at peak inspiration, just as exhalation begins, results in less disruption of the normal breathing cycle. Immediately instruct the client to cough. It is normal for large amounts of oral secretions to collect. Give oxygen by face mask or nasal cannula. The fraction of inspired oxygen (FIO2) is usually prescribed at 10% higher than the level used while the ET tube was in place. DIF: Cognitive Level: Application or higher TOP: Nursing Process Step: Assessment MSC: Client Needs Category: Safe, Effective Care Environment;
Copyright 2006, 2002 by Elsevier Inc.
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Principles of Medication AdministrationDocument22 pagesPrinciples of Medication AdministrationTina TalmadgeNo ratings yet
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Urinary Catheterization PrintableDocument8 pagesUrinary Catheterization PrintableThalani NarasiyaNo ratings yet
- Musculoskeletal System Musculoskeletal System: A. SkeletonDocument23 pagesMusculoskeletal System Musculoskeletal System: A. SkeletonTina TalmadgeNo ratings yet
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Chapter 1Document6 pagesChapter 1Tina TalmadgeNo ratings yet
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- Maternal and Child Health Nursing PDFDocument40 pagesMaternal and Child Health Nursing PDFTina Talmadge100% (5)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- COPAR ReviewerDocument6 pagesCOPAR ReviewerRichard Ines Valino94% (16)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- 11.06.2013 Family PlanningDocument84 pages11.06.2013 Family PlanningTina TalmadgeNo ratings yet
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- Normal Spontaneous Vaginal DeliveryDocument41 pagesNormal Spontaneous Vaginal DeliveryTina Talmadge100% (1)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- CNS Drugs TextDocument27 pagesCNS Drugs TextTina TalmadgeNo ratings yet
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- Maternal Child NursingDocument14 pagesMaternal Child NursingTina TalmadgeNo ratings yet
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Body Mechanics and Transfer TechniquesDocument90 pagesBody Mechanics and Transfer TechniquesTina Talmadge100% (1)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Concept of Professional Ethics and BioethicsDocument21 pagesThe Concept of Professional Ethics and BioethicsTina TalmadgeNo ratings yet
- Nursing Skills Procedure ManualDocument154 pagesNursing Skills Procedure ManualTina Talmadge100% (1)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- Gestational WeightDocument139 pagesGestational WeightTina TalmadgeNo ratings yet
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Circulatory SystemDocument51 pagesCirculatory SystemTina TalmadgeNo ratings yet
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Case Study in NutritionDocument27 pagesCase Study in NutritionTina TalmadgeNo ratings yet
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- Neonataljaundice 140128015601 Phpapp02Document39 pagesNeonataljaundice 140128015601 Phpapp02Tina TalmadgeNo ratings yet
- Lydia HendersonDocument20 pagesLydia HendersonTina TalmadgeNo ratings yet
- Circulatory SystemDocument51 pagesCirculatory SystemTina TalmadgeNo ratings yet
- BLOOD TRANSFUSION (BSN 3)Document67 pagesBLOOD TRANSFUSION (BSN 3)Tina TalmadgeNo ratings yet
- Breathing in Simple WayDocument15 pagesBreathing in Simple WayTina TalmadgeNo ratings yet
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Pharma5 CNS DrugsDocument32 pagesPharma5 CNS DrugsTina TalmadgeNo ratings yet
- Basal MetabolismDocument13 pagesBasal MetabolismTina TalmadgeNo ratings yet
- Fats and OilsDocument27 pagesFats and OilsTina TalmadgeNo ratings yet
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
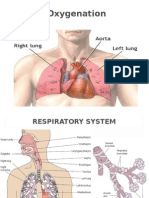
- OXYGENATIONDocument69 pagesOXYGENATIONTina Talmadge100% (4)
- Health Benefits of Functional FoodDocument46 pagesHealth Benefits of Functional FoodTina TalmadgeNo ratings yet
- IV CalculationDocument22 pagesIV CalculationTina TalmadgeNo ratings yet
- Cushings SyndromeDocument51 pagesCushings SyndromeTina TalmadgeNo ratings yet
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (120)
- Health Benefits of Functional FoodDocument46 pagesHealth Benefits of Functional FoodTina TalmadgeNo ratings yet
- CNS Deppressant DrugsDocument7 pagesCNS Deppressant DrugsTina TalmadgeNo ratings yet
- Respiratory SystemDocument13 pagesRespiratory SystemIrica Mae CiervoNo ratings yet
- Anatomy Review RespiratoryDocument8 pagesAnatomy Review RespiratoryHanami AsriNo ratings yet
- Respiratory QuestionsDocument116 pagesRespiratory QuestionsNatukunda Dianah100% (1)
- Management of Hypoxia During AnaesthesiaDocument5 pagesManagement of Hypoxia During AnaesthesiaNurhafizahImfista100% (1)
- Office Spirometry - UpToDateDocument17 pagesOffice Spirometry - UpToDateCamilo HernandezNo ratings yet
- Atelektasis: Penyaji: Martvera SDocument20 pagesAtelektasis: Penyaji: Martvera Saidil ilham100% (1)
- Scan 17-Nov-2021Document6 pagesScan 17-Nov-2021Savita AgrawalNo ratings yet
- Sudqd/Dpd WKH Vhushqw Srzhu: 3udfwlfhDocument2 pagesSudqd/Dpd WKH Vhushqw Srzhu: 3udfwlfhmamoncinNo ratings yet
- Invasive MechanicalDocument8 pagesInvasive MechanicalLTE002No ratings yet
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Nursing Care Plan: Cystic FibrosisDocument4 pagesNursing Care Plan: Cystic FibrosisYael EzraNo ratings yet
- ABG Interpretation Made EasyDocument5 pagesABG Interpretation Made EasyChris Chan100% (2)
- Concept Presentation ON Oxygen InsufficiencyDocument95 pagesConcept Presentation ON Oxygen Insufficiencylumina.sNo ratings yet
- PuritanBennett980Ventilator OperatorsManual en OUS PT00094084A00Document472 pagesPuritanBennett980Ventilator OperatorsManual en OUS PT00094084A00tkAcuNNo ratings yet
- Non-Invasive Respiratory Support, Third Edition - Simonds, Anita K. (SRG) PDFDocument385 pagesNon-Invasive Respiratory Support, Third Edition - Simonds, Anita K. (SRG) PDFCristinaLucanNo ratings yet
- Anatomi Sistem RespirasiDocument80 pagesAnatomi Sistem RespirasialiaNo ratings yet
- 4 High Frequency VentilationDocument40 pages4 High Frequency Ventilationk0601828No ratings yet
- Impaired Gas Exchange Care PlanDocument5 pagesImpaired Gas Exchange Care Planjakifer50% (2)
- Management of The Mechanically Ventilated Patient - Lynelle N. B. PierceDocument5 pagesManagement of The Mechanically Ventilated Patient - Lynelle N. B. Piercezoxigaro0% (1)
- Nursing Care Plan: Valiente, Ana Ambianca S. Maristela, Aony Jamaine Y. Tabora, Elyza M. Quitlong, Jennifer N. BSN 2BDocument6 pagesNursing Care Plan: Valiente, Ana Ambianca S. Maristela, Aony Jamaine Y. Tabora, Elyza M. Quitlong, Jennifer N. BSN 2BAmbianca ValienteNo ratings yet
- 2 NCPDocument2 pages2 NCPJohn CenasNo ratings yet
- ICU One Pager Flow Volume LoopsDocument1 pageICU One Pager Flow Volume LoopsRonald MoralesNo ratings yet
- Why Do You Need To Breathe? - To LiveDocument5 pagesWhy Do You Need To Breathe? - To LiveJuan DavisNo ratings yet
- Chapter 23 Obstructive Lung Disease Chronic Obstructive Pulmonary DiseaseDocument10 pagesChapter 23 Obstructive Lung Disease Chronic Obstructive Pulmonary DiseaseZahra Margrette SchuckNo ratings yet
- Chapter 10 Respiratory System PresentationDocument48 pagesChapter 10 Respiratory System PresentationMary Jane LubricoNo ratings yet
- Respiratory Physiology MCQsDocument25 pagesRespiratory Physiology MCQssk100% (5)
- Nursing Care Plan Name: Group: Group DateDocument5 pagesNursing Care Plan Name: Group: Group DateKen PerezNo ratings yet
- Nueva Ecija University of Science and Technology: Case 7Document7 pagesNueva Ecija University of Science and Technology: Case 7jomariNo ratings yet
- Noninvasive Ventilation in Acute Respiratory FailureDocument6 pagesNoninvasive Ventilation in Acute Respiratory FailureCesar C SNo ratings yet
- Chest Trauma DikaDocument46 pagesChest Trauma DikaOnyedika EgbujoNo ratings yet
- Mechanical Power FormulaDocument9 pagesMechanical Power FormulaEzeBorjesNo ratings yet
- The Obesity Code: Unlocking the Secrets of Weight LossFrom EverandThe Obesity Code: Unlocking the Secrets of Weight LossRating: 4 out of 5 stars4/5 (6)
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsFrom EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsNo ratings yet
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeFrom EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeRating: 2 out of 5 stars2/5 (1)
- The Age of Magical Overthinking: Notes on Modern IrrationalityFrom EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityRating: 4 out of 5 stars4/5 (24)
- The Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaFrom EverandThe Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaRating: 4.5 out of 5 stars4.5/5 (266)
- Summary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisFrom EverandSummary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisRating: 4.5 out of 5 stars4.5/5 (42)
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedFrom EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedRating: 5 out of 5 stars5/5 (80)