Professional Documents
Culture Documents
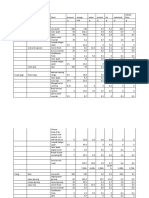
NCP IDNT Diagnosis-Etiology Matrix
Uploaded by
kapetaeOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
NCP IDNT Diagnosis-Etiology Matrix
Uploaded by
kapetaeCopyright:
Available Formats
Nutrition Diagnosis Etiology Matrix
Below are the etiology categories and their definitions. Etiologies are grouped by the type of cause or contributing risk factor. In two specific instances, Access and Behavior etiologies, these alone may be the cause or contributing risk factor of the nutrition diagnosis or the practitioner may determine a more specific root cause, e.g., Belief-Attitudes of the problem. Etiology Category BeliefsAttitudes Etiologies Definition Cause or contributing risk factors related to the conviction of the truth of some nutrition-related statement or phenomenon; feelings or emotions toward that truth or phenomenon and activities. Cause or contributing risk factors related to the patient/clients values, social norms, customs, religious beliefs and/or political systems. Cause or contributing risk factors impacting the level of understanding about food, nutrition and health, or nutrition-related information and guidelines. Cause or contributing risk factors related to physical ability to engage in specific tasks, may be cognitive in nature. Cause or contributing risk factors related to medical/health status that may have a nutritional impact (excludes psychological etiologiessee separate category). Cause or contributing risk factors related to a diagnosed or suspected mental health/psychological problem (Diagnostic and Statistical Manual of Mental Disorders, DSM) Cause or contributing risk factors associated with the patient/clients personal and/or social history. Cause or contributing risk factors related to medical or surgical treatment or other therapies and management or care. Cause or contributing risk factors that affect intake and the availability of safe, healthful food, water, and food/nutrition-related supplies. A more specific root cause of Access Etiologies may not be known but may eventually reveal Beliefs-Attitudes, Cultural, Knowledge, Physical Function, Psychological, SocialPersonal, or Treatment Etiologies. Cause or contributing risk factors related to actions which influence achievement of nutrition-related goals. A more specific root cause of Behavior Etiologies may not be known but may eventually reveal Beliefs-Attitudes, Cultural, Knowledge, Physical Function, Psychological, Social-Personal, or Treatment Etiologies.
Cultural Etiologies
Knowledge Etiologies
Physical Function Etiologies
PhysiologicMetabolic Etiologies
Psychological Etiologies
SocialPersonal Etiologies
Treatment Etiologies
Access Etiologies
Behavior Etiologies
1
Supplemental material for International Dietetics and Nutrition Terminology (IDNT) Reference Manual, Third Edition. Copyright 2011American Dietetic Association.
Category Beliefs-Attitudes Beliefs-Attitudes
Etiology Altered body image Food preference
Diagnosis Poor nutrition quality of life (NQOL) (NB-2.5) Limited food acceptance (NI-2.9), Excessive fat intake (NI-5.6.2), Inappropriate intake of fats (specify) (NI-5.6.3), Undesirable food choices (NB-1.7) Not ready for diet/lifestyle change (NB-1.3) Harmful beliefs/attitudes about food or nutritionrelated topics (NB-1.2) Harmful beliefs/attitudes about food or nutritionrelated topics (NB-1.2) Less than optimal enteral nutrition (NI-2.5), Less than optimal parenteral nutrition (NI-2.8) Disordered eating pattern (NB-1.5)
Beliefs-Attitudes Beliefs-Attitudes Beliefs-Attitudes Beliefs-Attitudes Beliefs-Attitudes
Denial of need to change Desire for a cure for a chronic disease through the use of alternative therapy Disbelief in science-based food and nutrition information End-of-life care if patient/client or family do not desire nutrition support Familial, societal, biological/genetic, and/or environmental related obsessive desire to be thin Food faddism
Beliefs-Attitudes
Imbalance of nutrients (NI-5.5), Excessive protein intake (NI-5.7.2), Inappropriate intake of proteins or amino acids (specify) (NI-5.7.3), Excessive mineral intake (NI-5.10.2) Inadequate oral intake (NI-2.1), Limited food acceptance (NI-2.9), Excessive energy intake (NI-1.5), Inadequate oral intake (NI-2.1), Excessive oral intake (NI-2.2), Limited food acceptance (NI-2.9), Excessive alcohol intake (NI-4.3), Imbalance of nutrients (NI5.5), Excessive fat intake (NI-5.6.2), Inappropriate intake of fats (NI-5.6.3), Excessive protein intake (NI-5.7.2), Inappropriate intake of protein or amino acids (specify) (NI-5.7.3), Excessive fiber intake (NI-5.8.6), Excessive mineral intake (NI5.10.2), Underweight (NC-3.1), Food- and nutrition-related knowledge deficit (NB-1.1), Not ready for diet/lifestyle change (NB-1.3), Physical inactivity (NB-2.1), Excessive physical activity (NB-2.2), Limited access to food and/or water (NB3.2) Breastfeeding difficulty (NC-1.3) Not ready for diet/lifestyle change (NB-1.3), Limited adherence to nutrition-related recommendations (NB-1.6), Poor nutrition quality of life (NQOL) (NB-2.5)
Beliefs-Attitudes Beliefs-Attitudes
Limited food acceptance due to food aversion Harmful beliefs/attitudes about food, nutrition, and nutrition-related information
Beliefs-Attitudes Beliefs-Attitudes
Irritability Lack of self-efficacy for making change or demoralization from previous failures at change
2
Supplemental material for International Dietetics and Nutrition Terminology (IDNT) Reference Manual, Third Edition. Copyright 2011American Dietetic Association.
Category Beliefs-Attitudes
Etiology Lack of value for behavior change or competing values
Diagnosis Excessive energy intake (NI-1.5), Excessive oral intake (NI-2.2), Excessive alcohol intake (NI-4.3), Excessive fat intake (NI-5.6.2) Inappropriate intake of fats (specify) (NI-5.6.3), Self-monitoring deficit (NB-1.4), Limited adherence to nutrition-related recommendations (NB-1.6), Physical inactivity (NB-2.1), Inability or lack of desire to manage selfcare (NB-2.3) Undesirable food choices (NB-1.7)
Beliefs-Attitudes Beliefs-Attitudes Beliefs-Attitudes
Lacks motivation and or readiness to apply or support systems change
Negative impact of current or previous medical Poor nutrition quality of life (NQOL) (NB-2.5) nutrition therapy (MNT) Not ready for diet/lifestyle change Overweight/Obesity (NC-3.3), Self-monitoring deficit (NB-1.4), Inability or lack of desire to manage self-care (NB-2.3), Poor nutrition quality of life (NQOL) (NB-2.5) Breastfeeding difficulty (NC-1.3)
Beliefs-Attitudes Beliefs-Attitudes
Perception of inadequate milk supply Perception that lack of resources (e.g., time, financial, or interpersonal) prevent: Selection/food choices consistent with recommendations Changes
Undesirable food choices (NB-1.7) Not ready for diet/lifestyle change (NB-1.3), Limited adherence to nutrition-related recommendations (NB-1.6) Physical inactivity (NB-2.1) Self-monitoring deficit (NB-1.4), Inability or lack of desire to manage self-care (NB-2.3)
Sufficient level of activity Self-monitoring Beliefs-Attitudes Unwilling or disinterested in: Learning/applying information
Food- and nutrition-related knowledge deficit (NB1.1), Not ready for diet/lifestyle change (NB-1.3), Limited adherence to nutrition-related recommendations (NB-1.6), Undesir-able food choices (NB-1.7), Inability or lack of desire to manage self-care (NB-2.3) Excessive energy intake (NI-1.5) Excessive oral intake (NI-2.2) Inappropriate intake of proteins or amino acids (specify) (NI-5.7.3) Self-monitoring deficit (NB-1.4) Inadequate fiber intake (NI-5.8.5) Disordered eating pattern (NB-1.5)
Reducing energy intake Reducing intake Modify protein or amino acid intake Tracking progress Unwillingness to purchase or consume fiber-containing foods Weight regulation/preoccupation significantly influences self-esteem
3
Supplemental material for International Dietetics and Nutrition Terminology (IDNT) Reference Manual, Third Edition. Copyright 2011American Dietetic Association.
Category Cultural Cultural Cultural
Etiology Culture of overeating Practices that affect nutrient intake Cultural practices that affect ability to: Access to food, fluid, nutrients
Diagnosis Predicted excessive energy intake (NI-1.7) Predicted suboptimal nutrient intake (specify) (NI5.11.1)
Inadequate energy intake (NI-1.4), Inadequate oral intake (NI-2.1), Inadequate fluid intake (NI-3.1), Malnutrition (NI-5.2), Inadequate proteinenergy intake (NI-5.3), Inadequate protein intake (NI5.7.1), Inadequate carbohydrate intake (NI-5.8.1), Inadequate vitamin intake (specify) (NI-5.9.1), Inadequate mineral intake (specify) (NI-5.10.1), Unintended weight loss (NC-3.2) Inadequate fat intake (NI-5.6.1) Breastfeeding difficulty (NC-1.3) Food- and nutrition-related knowledge deficit (NB-1.1), Undesirable food choices (NB-1.7) Inability or lack of desire to manage self-care (NB-2.3) Excessive carbohydrate intake (NI-5.8.2) Inappropriate intake of proteins or amino acids (specify) (NI-5.7.3) Inconsistent carbohydrate intake (NI-5.8.4) Inappropriate intake of types of carbohydrates (specify) (NI-5.8.3) Self-monitoring deficit (NB-1.4) Inadequate energy intake (NI-1.4), Excessive energy intake (NI-1.5), Excessive oral intake (NI2.2), Inadequate fluid intake (NI-3.1), Excessive fluid intake (NI-3.2), Inadequate bioactive substance intake (NI-4.1), Excessive bioactive substance intake (NI-4.2), Excessive alcohol intake (NI-4.3), Malnutrition (NI-5.2), Inadequate proteinenergy intake (NI-5.3), Imbalance of nutrients (NI-5.5), Excessive fat intake (NI-5.6.2), Inadequate protein intake (NI-5.7.1), Inadequate carbohydrate intake (NI-5.8.1), Inadequate fiber intake (NI-5.8.5), Excessive mineral intake (specify) (NI-5.10.2), Overweight/obesity (NC3.3), Self-monitoring deficit (NB-1.4), Inability or lack of desire to manage self-care (NB-2.3), Poor nutrition quality of life (NQOL) (NB-2.5), Limited access to food or water (NB-3.2), Limited access to nutrition-related supplies (NB-3.3)
Make appropriate food choices Breastfeed Learn/apply information Manage self-care Reduce carbohydrate intake Regulate types of protein or amino acids consumed Regulate timing of carbohydrate consumption Regulate types of carbohydrate consumed Track personal progress Knowledge Food and nutrition knowledge deficit
4
Supplemental material for International Dietetics and Nutrition Terminology (IDNT) Reference Manual, Third Edition. Copyright 2011American Dietetic Association.
Category Knowledge
Etiology Food and nutrition knowledge deficit concerning: Sufficient oral food/beverage intake Consumption of an appropriate variety of foods Potentially unsafe food Proper infant feeding, food/feeding preparation and storage Adequate energy intake Appropriate amount or types of dietary protein or amino acids
Diagnosis
Inadequate oral intake (NI-2.1) Excessive mineral intake (specify) (NI-5.10.2) Intake of unsafe food (NB-3.1) Intake of unsafe food (NB-3.1) Underweight (NC-3.1) Malnutrition (NI-5.2), Inadequate proteinenergy intake (NI-5.3), Inadequate protein intake (NI5.7.1), Inappropriate intake of proteins or amino acids (specify) (NI-5.7.3) Inadequate proteinenergy intake (NI-5.3), Inadequate fat intake (NI-5.6.1), Excessive fat intake (NI-5.6.2), Inappropriate intake of fats (NI5.6.3) Excessive carbohydrate intake (NI-5.8.2), Inappropriate intake of types of carbohydrates (specify) (NI-5.8.3) Inconsistent carbohydrate intake (NI-5.8.4) Inconsistent carbohydrate intake (NI-5.8.4)
Appropriate amount or type of dietary fat
Appropriate amount and types of dietary carbohydrate Appropriate timing of carbohydrate intake Physiological causes requiring careful timing and consistency in the amount of carbohydrate Physiological causes requiring use of modified carbohydrate Physiological causes requiring use of modified carbohydrate intake Desirable quantities of fiber Correct enteral formula needed Food and supplemental sources of vitamins Food and supplemental sources of minerals Recommended dose of vitamin and mineral supplements Management of diagnosis requiring mineral restriction Management of diagnosed genetic disorder altering mineral homeostasis
Inappropriate intake of types of carbohydrates (specify) (NI-5.8.3) Excessive carbohydrate intake (NI-5.8.2) Inadequate fiber intake (NI-5.8.5), Excessive fiber intake (NI-5.8.6) Inadequate enteral nutrition infusion (NI-2.3) Inadequate vitamin intake (specify) (NI-5.9.1), Excessive vitamin intake (specify) (NI-5.9.2) Inadequate mineral intake (specify) (NI-5.10.1) Imbalance of nutrients (NI-5.5) Excessive mineral intake (specify) (NI-5.10.2) Excessive mineral intake (specify) (NI-5.10.2)
5
Supplemental material for International Dietetics and Nutrition Terminology (IDNT) Reference Manual, Third Edition. Copyright 2011American Dietetic Association.
Category Knowledge
Etiology Food and nutrition knowledge deficit concerning, contd: Correct amount of enteral/parenteral formula Correct parenteral nutrition components Appropriate/correct access for delivering EN/PN Health benefits of physical activity How to make nutrition-related changes Food-drug interactions On the part of the caregiver
Diagnosis
Excessive energy intake (NI-1.5) Excessive parenteral nutrition infusion (NI-2.7) Inadequate parenteral nutrition infusion (NI-2.6), Less than optimal parenteral nutrition (NI-2.8) Inadequate enteral nutrition infusion (NI-2.3), Inadequate parenteral nutrition infusion (NI-2.6) Physical inactivity (NB-2.1) Limited adherence to nutrition-related recommendations (NB-1.6) Food-medication interaction (NC-2.3), Predicted food-medication interaction (NC-2.4) Excessive enteral nutrition infusion (NI-2.4), Excessive parenteral nutrition infusion (NI-2.7), Less than optimal enteral nutrition (NI-2.5), Less than optimal parenteral nutrition (NI-2.8) Imbalance of nutrients (NI-5.5) Food- and nutrition-related knowledge deficit (NB1.1) Food- and nutrition-related knowledge deficit (NB1.1), Harmful beliefs/attitudes about food or nutrition-related topics (NB-1.2), Self-monitoring deficit (NB-1.4), Undesirable food choices (NB1.7), Inability or lack of desire to manage self-care (NB-2.3) Physical inactivity (NB-2.1) Excessive energy intake (NI-1.5) Breastfeeding difficulty (NC-1.3)
Consumption of high-dose nutrient supplements Infant/child hunger cues Lack of prior exposure to accurate nutritionrelated information
Lack of prior exposure to accurate information regarding physical activity Failure to adjust for lifestyle changes or restricted mobility and decreased metabolism Physical function Physical function Irritability
Physiological difficulty causing inability to Self-feeding difficulty (NB-2.6) physically: Bend elbow at wrist Grasp cups and utensils Sit with hips square and back straight Support neck and/or control head and neck Coordinate hand movement to mouth Lack of self-feeding ability Diminished ability to shop Unintended weight loss (NC-3.2) Limited access to food and/or water (NB-3.2), Limited access to nutrition-related supplies (NB3.3) Self-feeding difficulty (NB-2.6) Overweight/Obesity (NC-3.3)
6
Physical function Physical function
Physical function Physical function
Limited physical strength or range of motion Physical inactivity
Supplemental material for International Dietetics and Nutrition Terminology (IDNT) Reference Manual, Third Edition. Copyright 2011American Dietetic Association.
Category Physical function Physical function PhysiologicMetabolic PhysiologicMetabolic
Etiology Change in physical activity anticipated Voluntary or involuntary physical activity/movement Age-related demands Alteration in gastrointestinal tract Decreased functional length of GI tract
Diagnosis Predicted suboptimal energy intake (NI-1.6), Predicted excessive energy intake (NI-1.7) Increased energy expenditure (NI-1.2) Inadequate protein intake (NI-5.7.1)
Increased nutrient needs (specify) (NI-5.1), Malnutrition (NI-5.2), Altered gastrointestinal (GI) function (NC-1.4), Increased nutrient needs (specify) (NI-5.1), Malnutrition (NI-5.2), Altered gastrointestinal (GI) function (NC-1.4), Inadequate fat intake (NI-5.6.1) Limited food acceptance (NI-2.9), Inadequate bioactive substance intake (NI-4.1), Excessive bioactive substance intake (NI-4.2), Increased nutrient needs (specify) (NI-5.1), Malnutrition (NI5.2), Inadequate fat intake (NI-5.6.1), Altered gastrointestinal (GI) function (NC-1.4) Altered gastrointestinal (GI) function (NC-1.4) Increased nutrient needs (specify) (NI-5.1), Altered gastrointestinal (GI) function (NC-1.4) Impaired nutrient utilization (NC-2.1) Decreased nutrient needs (specify) (NI-5.4) Breastfeeding difficulty (NC-1.3) Excessive fat intake (NI-5.6.2), Inappropriate intake of fats (specify) (NI-5.6.3) Inadequate fluid intake (NI-3.21) Biting/Chewing (masticatory) difficulty (NC-1.2) Overweight/Obesity (NC-3.3)
Alteration in GI anatomical structure
Alteration in GI function
Change in GI tract motility Change in GI related organ function Compromised endocrine function PhysiologicMetabolic PhysiologicMetabolic PhysiologicMetabolic PhysiologicMetabolic PhysiologicMetabolic PhysiologicMetabolic PhysiologicMetabolic Altered cholesterol metabolism/regulation Breast or nipple abnormality Changes in taste, appetite Conditions leading to excess fluid loss Craniofacial malformations Decreased energy needs
Decreased ability to consume sufficient energy, Inadequate energy intake (NI-1.4), Inadequate oral nutrients intake (NI-2.1), Inadequate proteinenergy intake (NI-5.3), Inadequate protein intake (NI-5.7.1), Inadequate vitamin intake (specify) (NI-5.9.1), Inadequate mineral intake (specify) (NI-5.10.1), Unintended weight loss (NC-3.2) Decreased nutrient needs related to low activity Excessive enteral nutrition infusion (NI-2.4), levels due to chronic disease or organ failure Excessive parenteral nutrition infusion (NI-2.7), Excessive vitamin intake (specify) (NI-5.9.2)
PhysiologicMetabolic
7
Supplemental material for International Dietetics and Nutrition Terminology (IDNT) Reference Manual, Third Edition. Copyright 2011American Dietetic Association.
Category PhysiologicMetabolic PhysiologicMetabolic PhysiologicMetabolic PhysiologicMetabolic PhysiologicMetabolic PhysiologicMetabolic PhysiologicMetabolic PhysiologicMetabolic PhysiologicMetabolic PhysiologicMetabolic
Etiology Developmental delay Difficulty chewing or swallowing high-fiber foods Difficulty latching on Excessive energy intake Food allergies and aversions impeding food choices consistent with guidelines Food intolerances Genetic predisposition to overweight/obesity Heart failure
Diagnosis Limited food acceptance (NI-2.9) Inadequate fiber intake (NI-5.8.5) Breastfeeding difficulty (NC-1.3) Overweight/Obesity (NC-3.3) Undesirable food choices (NB-1.7) Decreased nutrient needs (specify) (NI-5.4) Predicted excessive energy intake (NI-1.7) Decreased nutrient needs (specify) (NI-5.4)
Illness causing unexpected weight gain because Unintended weight gain (NC-3.4) of head trauma, immobility, paralysis or related condition Impaired cognitive ability, including learning disabilities, neurological or sensory impairment, and dementia Inadequate fluid intake (NI-3.1), Food- and nutrition-related knowledge deficit (NB-1.1), Not ready for diet/lifestyle change (NB-1.3), Selfmonitoring deficit (NB-1.4), Undesirable food choices (NB-1.7), Inability or lack of desire to manage self-care (NB-2.3), Impaired ability to prepare foods/meals (NB-2.4), Self-feeding difficulty (NB-2.6), Limited access to food or water (NB-3.2) Underweight (NC-3.1) Breastfeeding difficulty (NC-1.3) Underweight (NC-3.1) Physical inactivity (NB-2.1)
PhysiologicMetabolic PhysiologicMetabolic PhysiologicMetabolic PhysiologicMetabolic PhysiologicMetabolic PhysiologicMetabolic
Inadequate energy intake Inadequate milk supply Increased energy needs Injury, condition, physical disability or limitation that reduces physical activity or activities of daily living Intolerance of EN/PN Kidney, liver, cardiac, endocrine, neurologic, and/or pulmonary dysfunction
Inadequate enteral nutrition infusion (NI-2.3), Inadequate parenteral nutrition infusion (NI-2.6) Limited food acceptance (NI-2.9), Excessive fluid intake (NI-3.2), Biting/ Chewing (masticatory) difficulty (NC-1.2), Altered nutrition-related laboratory values (specify) (NC-2.2) Inability or lack of desire to manage self-care (NB2.3)
PhysiologicMetabolic
Lack of developmental readiness to perform self-management tasks
8
Supplemental material for International Dietetics and Nutrition Terminology (IDNT) Reference Manual, Third Edition. Copyright 2011American Dietetic Association.
Category PhysiologicMetabolic PhysiologicMetabolic PhysiologicMetabolic PhysiologicMetabolic PhysiologicMetabolic PhysiologicMetabolic PhysiologicMetabolic PhysiologicMetabolic PhysiologicMetabolic PhysiologicMetabolic PhysiologicMetabolic PhysiologicMetabolic PhysiologicMetabolic PhysiologicMetabolic PhysiologicMetabolic PhysiologicMetabolic PhysiologicMetabolic PhysiologicMetabolic
Etiology Lethargy, sleepiness Limited vision Limited food acceptance Liver dysfunction
Diagnosis Breastfeeding difficulty (NC-1.3) Self-feeding difficulty (NB-2.6) Inadequate oral intake (NI-2.1) Decreased nutrient needs (specify) (NI-5.4), Excessive protein intake (NI-5.7.2), Inappropriate intake of amino acids (specify) (NI-5.7.3) Excessive oral intake (NI-2.2) Increased nutrient needs (specify) (NI-5.1), Breastfeeding difficulty (NC-1.3) Breastfeeding difficulty (NC-1.3) Swallowing difficulty (NC-1.1), Biting/ Chewing (masticatory) difficulty (NC-1.2) Inappropriate intake of protein or amino acids (specify) (NI-5.7.3) Excessive protein intake (NI-5.7.2), Inappropriate intake of amino acids (specify) (NI-5.7.3) Impaired nutrient utilization (NC-2.1) Impaired nutrient utilization (NC-2.1) Swallowing difficulty (NC-1.1) Breastfeeding difficulty (NC-1.3) Altered nutrition-related laboratory values (specify) (NC-2.2) Biting/Chewing (masticatory) difficulty (NC-1.2) Impaired ability to prepare foods/meals (NB-2.4), Limited access to food or water (NB-3.2) Excessive carbohydrate intake (NI-5.8.2), Inappropriate intake of types of carbohydrates (NI5.8.3), Inconsistent carbohydrate intake (NI-5.8.4)
Loss of appetite awareness Malnutrition/malabsorption Mastitis and/or painful breasts, nipples Mechanical issues such as inflammation, surgery, stricture, or oral, pharyngeal and esophageal tumors, mechanical ventilation Inborn errors of metabolism Metabolic abnormality Metabolic disorders Metabolic disorders Motor causes related to neurological or muscular disorders Oral pain Other organ dysfunction that leads to biochemical changes Partial or complete edentulism Physical disability Physiologic causes requiring modified amount or timing of carbohydrate intake
9
Supplemental material for International Dietetics and Nutrition Terminology (IDNT) Reference Manual, Third Edition. Copyright 2011American Dietetic Association.
Category PhysiologicMetabolic
Etiology Physiological causes increasing nutrient needs due to: Accelerated growth or anabolism
Diagnosis
Increased energy expenditure (NI-1.2), Inadequate enteral nutrition infusion (NI-2.3), Inadequate parenteral nutrition infusion (NI-2.6), Increased nutrient needs (specify) (NI-5.1), Inadequate mineral intake (specify)(NI-5.10.1) Inadequate fluid intake (NI-3.1), Increased nutrient needs (specify) (NI-5.1), Inadequate protein intake (NI-5.7.1), Inadequate carbohydrate intake (NI5.8.1), Inadequate vitamin intake (specify) (NI5.9.1), Inadequate mineral intake (specify) (NI5.10.1), Predicted suboptimal nutrient intake (specify) (NI-5.11.1), Malnutrition (NI-5.2), Inadequate proteinenergy intake (NI-5.3), Unintended weight loss (NC-3.2) Inadequate enteral nutrition infusion (NI-2.3), Inadequate parenteral nutrition infusion (NI-2.6), Inadequate fluid intake (NI-3.1), Increased nutrient needs (specify) (NI-5.1), Malnutrition (NI-5.2), Inadequate proteinenergy intake (NI-5.3), Inadequate protein intake (NI-5.7.1), Inappropriate intake of proteins or amino acids (specify) (NI5.7.3), Inadequate vitamin intake (specify) (NI5.9.1), Unintended weight loss (NC-3.2) Increased energy expenditure (NI-1.2), Inadequate fluid intake (NI-3.1) Inadequate energy intake (NI-1.4), Inadequate oral intake (NI-2.1), Inadequate fluid intake (NI-3.1), Malnutrition (NI-5.2), Inadequate proteinenergy intake (NI-5.3), Inadequate protein intake (NI5.7.1), Inadequate vitamin intake (specify) (NI5.9.1), Inadequate mineral intake (specify) (NI5.10.1), Unintended weight loss (NC-3.2) Predicted excessive energy intake (NI-1.7), Predicted excessive nutrient intake (NI-5.11.2) Breastfeeding difficulty (NC-1.3) Altered nutrition-related laboratory values (NC2.2) Decreased nutrient needs (specify) (NI-5.4), Excessive protein intake (NI-5.7.2), Inappropriate intake of amino acids (specify) (NI-5.7.3) Underweight (NC-3.1)
Altered absorption or metabolism
Disease/condition
Maintenance of body temperature Prolonged catabolic illness
PhysiologicMetabolic PhysiologicMetabolic PhysiologicMetabolic PhysiologicMetabolic PhysiologicMetabolic PhysiologicMetabolic
Altered metabolism Poor sucking ability Prematurity Renal dysfunction
Small for gestational age, intrauterine growth retardation/restriction and/or lack of progress/appropriate weight gain per day Soft tissue disease (primary or oral manifestations of a systemic disease)
Biting/Chewing (masticatory) difficulty (NC-1.2)
10
Supplemental material for International Dietetics and Nutrition Terminology (IDNT) Reference Manual, Third Edition. Copyright 2011American Dietetic Association.
Category PhysiologicMetabolic PhysiologicMetabolic Psychological Psychological Psychological Psychological Psychological
Etiology Swallowing difficulty, and altered suck and breathing patterns in infants Xerostomia Alcohol or drug addiction Addictive personality Mental illness, confusion, or altered awareness Mental illness, confusion, or altered awareness Psychological causes such as depression and disordered eating
Diagnosis Swallowing difficulty (NC-1.1), Breastfeeding difficulty (NC-1.3) Biting/Chewing (masticatory) difficulty (NC-1.2) Excessive alcohol intake (NI-4.3), Impaired nutrient utilization (NC-2.1) Excessive physical activity (NB-2.2) Intake of unsafe food (NB-3.1), Excessive oral intake (NI-2.2) Intake of unsafe food (NB-3.1), Excessive oral intake (NI-2.2) Inadequate energy intake (NI-1.4), Inadequate oral intake (NI-2.1), Inadequate fluid intake (NI-3.1), Excessive fluid intake (NI-3.2), Malnutrition (NI5.2), Inadequate proteinenergy intake (NI-5.3), Inadequate fat intake (NI-5.6.1), Inadequate protein intake (NI-5.7.1), Inadequate carbohydrate intake (NI-5.8.1), Excessive carbohydrate intake (NI-5.8.2), Inappropriate intake of types of carbohydrates (NI-5.8.3), Inconsistent carbohydrate intake (NI-5.8.4), Inadequate fiber intake (NI-5.8.5), Inadequate vitamin intake (specify) (NI-5.9.1), Excessive vitamin intake (specify) (NI-5.9.2), Inadequate mineral intake (specify) (NI-5.10.1), Unintended weight loss, (NC-3.2) Undesirable food choices (NB-1.7), Excessive physical activity (NB-2.2), Limited access to food or water (NB-3.2), Limited access to nutrition-related supplies (NB-3.3) Breastfeeding difficulty (NC-1.3), Physical Inactivity (NB-2.1) Breastfeeding difficulty (NC-1.3), Not ready for diet/lifestyle change (NB-1.3), Self-monitoring deficit (NB-1.4), Limited adherence to nutritionrelated recommendations (NB-1.6), Physical inactivity (NB-2.1), Inability or lack of desire to manage self-care (NB-2.3), Poor nutrition quality of life (NQOL) (NB-2.5) Predicted excessive energy intake (NI-1.7) Overweight/Obesity (NC-3.3), Predicted suboptimal energy intake (NI-1.6), Predicted excessive energy intake (NI-1.7) Predicted suboptimal energy intake (NI-1.6), Predicted excessive energy intake (NI-1.7), Predicted suboptimal nutrient intake (NI-5.11.1)
Social-Personal Social-Personal
Lack of role models Lack of social support for implementing changes
Social-Personal Social-Personal
Family or social history of overeating Increased psychological/life stress
Social-Personal
Change in living situation
Social-Personal
Living in a geographic location with danger for Predicted suboptimal nutrient intake (specify) (NIenvironmental emergency 5.11.1)
11
Supplemental material for International Dietetics and Nutrition Terminology (IDNT) Reference Manual, Third Edition. Copyright 2011American Dietetic Association.
Category Treatment Treatment Treatment Treatment Treatment
Etiology Accidental vitamin and/or mineral overdose from oral, enteral or parenteral sources Calories unaccounted for from IV infusion and/or medications Changes in taste, appetite Changes in GI tract motility
Diagnosis Excessive vitamin intake (specify) (NI-5.9.2), Excessive mineral intake (specify) (NI-5.10.2) Excessive energy intake (NI-1.5) Excessive fat intake (NI-5.6.2), Inappropriate intake of fats (specify) (NI-5.6.3) Altered gastrointestinal (GI) function (NC-1.4)
Chronic use of medications known to cause Unintended weight gain (NC-3.4) weight gain, such as use of certain antidepressants, antipsychotics, corticosteroids, certain HIV medications Difficulty chewing or swallowing high-fiber foods Excessive energy intake Food intolerances High level of fatigue or other side effect of therapy Inadequate fiber intake (NI-5.8.5) Overweight/Obesity (NC-3.3) Decreased nutrient needs (specify) (NI-5.4) Undesirable food choices (NB-1.7), Impaired ability to prepare foods/meals (NB-2.4)
Treatment Treatment Treatment Treatment Treatment
Improvement in patient/client status, allowing Less than optimal enteral nutrition (NI-2.5), Less return to total or partial oral diet; changes in the than optimal parenteral nutrition (NI-2.8) course of disease resulting in changes in nutrient requirements Inadequate energy intake Infusion volume not reached or schedule for infusion interrupted Insufficient electrolyte replacement when initiating feeding (PN/EN, including oral) Lack of, compromised, or incorrect access for delivering EN/PN Mechanical issues such as inflammation, surgery, stricture, or oral, pharyngeal and esophageal tumors, mechanical ventilation Medications that increase appetite Medications that increase nutrient needs Medications that that affect nutrient metabolism Medications that increase fluid needs or decrease thirst Misused specialized protein products Misdiagnosis of lactose intolerance/lactase deficiency Underweight (NC-3.1) Inadequate enteral nutrition infusion (NI-2.3), Inadequate parenteral nutrition infusion (NI-2.6) Imbalance of nutrients (NI-5.5) Inadequate enteral nutrition infusion (NI-2.3), Inadequate parenteral nutrition infusion (NI-2.6) Swallowing difficulty (NC-1.1), Biting/ Chewing (masticatory) difficulty (NC-1.2) Excessive energy intake (NI-1.5), Excessive oral intake (NI-2.2), Increased nutrient needs (specify) (NI-5.1) Impaired nutrient utilization (NC-2.1) Inadequate fluid intake (NI-3.1) Inappropriate intake of protein or amino acids (specify) (NI-5.7.3) Inadequate mineral intake (specify) (NI-5.10.1)
Treatment Treatment Treatment Treatment Treatment
Treatment Treatment Treatment Treatment Treatment Treatment
12
Supplemental material for International Dietetics and Nutrition Terminology (IDNT) Reference Manual, Third Edition. Copyright 2011American Dietetic Association.
Category Treatment
Etiology Nutrient/nutrient interaction and/or drug/nutrient interaction
Diagnosis Inadequate intake from enteral/parenteral (EN/PN) nutrition infusion (NI-2.3), Inadequate parenteral nutrition infusion (NI-2.6), Inadequate vitamin intake (specify) (NI-5.9.1), Inadequate mineral intake (specify) (NI-5.10.1), Food-Medication Interaction (NC-2.3), Predicted food-medication interaction (NC-2.4) Excessive energy intake (NI-1.5) Predicted suboptimal energy intake (NI-1.6), Predicted suboptimal nutrient intake (NI-5.11.1) Predicted excessive energy intake (NI-1.7), Predicted excessive nutrient intake (NI-5.11.2) Predicted suboptimal energy intake (NI-1.6), Predicted suboptimal nutrient intake (NI-5.11.1) Inadequate fiber intake (NI-5.8.5) Unintended weight loss (NC-3.2) Decreased nutrient needs (specify) (NI-5.4), Excessive protein intake (NI-5.7.2), Inappropriate intake of amino acids (specify) (NI-5.7.3) Biting/Chewing (masticatory) difficulty (NC-1.2) Excessive vitamin intake (specify) (NI-5.9.2) Limited access to food or water (NB-3.2), Limited access to nutrition-related supplies (NB-3.3) Limited access to food or water (NB-3.2), Limited access to nutrition-related supplies (NB-3.3)
Treatment Treatment
Overfeeding of parenteral/enteral nutrition (PN/EN) Planned procedure, therapy or medication predicted to increase energy expenditure or nutrient need Planned therapy or medication predicted to reduce energy/nutrient need or metabolic rate/metabolism Planned procedure, therapy or medication predicted to decrease ability to consume sufficient energy or nutrients Prolonged adherence to a low-fiber or lowresidue diet Prolonged hospitalization Renal dysfunction
Treatment
Treatment
Treatment Treatment Treatment
Treatment Access Access
Xerostomia Access to foods and supplements in excess of needs Caregiver intentionally or unintentionally not providing access to food or nutrition-related supplies Community and geographical constraints for shopping and transportation
Access Access
Environmental causes, e.g., inadequately tested Inadequate mineral intake (specify) (NI-5.10.1) nutrient bioavailability of fortified foods, beverages, and supplements; inappropriate marketing of fortified foods, beverages, supplements as a substitute for natural food source of nutrient(s) Exposure to contaminated water or food, e.g., community outbreak of illness documented by surveillance and/or response agency Intake of unsafe food (NB-3.1)
Access
Access
Failure to participate in federal food programs Limited access to food or water (NB-3.2) such as WIC, National School Breakfast/Lunch Program, food stamps Financial constraints that may prevent sufficient level of activity (e.g., to address cost of equipment or shoes or club membership to gain access)
13
Access
Physical inactivity (NB-2.1)
Supplemental material for International Dietetics and Nutrition Terminology (IDNT) Reference Manual, Third Edition. Copyright 2011American Dietetic Association.
Category Access
Etiology Lack of, or limited access to: Adaptive foods or eating devices conducive for self-feeding Available and safe exercise environment and/or equipment Fluid Fortified foods and beverages Specialized protein products Food or artificial nutrition
Diagnosis
Self-feeding difficulty (NB-2.6) Physical inactivity (NB-2.1) Inadequate fluid intake (NI-3.1), Inadequate fiber intake (NI-5.8.5) Inadequate mineral intake (specify) (NI-5.10.1) Excessive protein intake (NI-5.7.2) Inadequate energy intake (NI-1.4), Inadequate oral intake (NI-2.1), Malnutrition (NI-5.2), Inadequate protein-energy intake (NI-5.3), Inadequate fat intake (NI-5.6.1), Inadequate protein intake (NI5.7.1), Inadequate carbohydrate intake (NI-5.8.1), Inadequate vitamin intake (specify) (NI-5.9.1), Inadequate mineral intake (specify) (NI-5.10.1), Underweight (NC-3.1), Unintended weight loss (NC-3.2), Poor nutrition quality of life (NQOL) (NB-2.5) Inadequate fiber intake (NI-5.8.5) Inadequate bioactive substance intake (NI-4.1) Excessive energy intake (NI-1.5), Excessive oral intake (NI-2.2), Excessive fat intake (NI-5.6.2), Inappropriate intake of fats (specify) (NI-5.6.3) Undesirable food choices (NB-1.7) Limited access to food or water (NB-3.2) Excessive bioactive substance intake (NI-4.2) Intake of unsafe food (NB-3.1) Intake of unsafe food (NB-3.1) Inability or lack of desire to manage self-care (NB-2.3), Limited access to nutrition-related supplies (NB-3.3) Limited access to food or water (NB-3.2), Limited access to nutrition-related supplies (NB-3.3)
Fiber-containing foods Food that contains a bioactive substance Healthy food choices
Recommended foods Sufficient quantity or variety of culturally appropriate healthful food/water Safe and/or clear and accurately labeled food supply Food storage equipment/facilities Self-management tools or decision guides or other nutrition-related supplies Access Limited, absent, or failure to participate in community supplemental food programs such as food pantries, emergency kitchens, or shelters, with a sufficient variety of culturally appropriate healthful foods or nutrition-related supplies Schools lacking nutrition/wellness policies or application of policies ensuring convenient, appetizing, competitively priced culturally appropriate healthful foods at meals, snacks, and school sponsored activities
Access
Limited access to food or water (NB-3.2)
14
Supplemental material for International Dietetics and Nutrition Terminology (IDNT) Reference Manual, Third Edition. Copyright 2011American Dietetic Association.
Category Behavior Behavior Behavior Behavior Behavior Behavior
Etiology Addictive behavior Consumption of high-dose nutrient supplements Eating behavior serves a purpose other than Excessive energy intake Excessive physical activity Food and nutrition compliance limitations
Diagnosis Excessive exercise (NB-2.2) Imbalance of nutrients (NI-5.5) Harmful beliefs/attitudes about food or nutritionOverweight/Obesity (NC-3.3) Underweight (NC-3.1) Excessive carbohydrate intake (NI-5.8.2), inappropriate intake of types of carbohydrates (specify) (NI-5.8.3), Inconsistent carbohydrate intake (NI-5.8.4) Poor nutrition quality of life (NQOL) (NB-2.5)
Behavior Behavior
Food or activity behavior-related difficulty
Food preparation or eating patterns that involve Excessive fiber intake (NI-5.8.6) only high-fiber foods to the exclusion of other nutrient-dense foods Disordered eating pattern Frequent intake of foods containing bioactive substances Limited food acceptance due to behavioral issues Inability to limit or refuse offered foods Inadequate energy intake Lack of focus and attention to detail, difficulty with time management and/or organization Lifestyle change that reduces physical activity or activities of daily living Over consumption of a limited variety of foods Poor or inappropriate food planning, purchasing and preparation practices Reluctance or avoidance of self-feeding Excessive physical activity (NB-2.2), Underweight (NC-3.1), Overweight/Obesity (NC-3.3) Excessive bioactive substance intake (NI-4.2) Inadequate oral intake (NI-2.1) Excessive oral intake (NI-2.2) Underweight (NC-3.1) Self-monitoring deficit (NB-1.4) Physical inactivity (NB-2.1) Excessive mineral intake (specify) (NI-5.10.2) Excessive oral intake (NI-2.2), Inadequate fiber intake (NI-5.8.5), Limited access to food or water (NB-3.2) Self-feeding difficulty (NB-2.6)
Behavior Behavior Behavior Behavior Behavior Behavior Behavior Behavior Behavior
Behavior
15
Supplemental material for International Dietetics and Nutrition Terminology (IDNT) Reference Manual, Third Edition. Copyright 2011American Dietetic Association.
You might also like
- Eat Right, Live Well Understanding the Science of NutritionFrom EverandEat Right, Live Well Understanding the Science of NutritionNo ratings yet
- 2015 Terminologi Domain Perilaku LingkDocument27 pages2015 Terminologi Domain Perilaku LingkNanda Raisya Yandara PutriNo ratings yet
- Domain Diagnosa Gizi-Intake 2013-4Document58 pagesDomain Diagnosa Gizi-Intake 2013-4Ilmi Dewi A100% (1)
- NCP InterventionDocument17 pagesNCP InterventionNurul Huda HekmutiarNo ratings yet
- PATOBIOLOGI GIZIDocument13 pagesPATOBIOLOGI GIZIDewiNo ratings yet
- Food Frequency Questionnaire (FFQ)Document23 pagesFood Frequency Questionnaire (FFQ)Novita SariNo ratings yet
- 2015 Nutrition Diagnosis Terminologi 2015Document9 pages2015 Nutrition Diagnosis Terminologi 2015Vivin Syamsul ArifinNo ratings yet
- Appenix19 - IDNT Terminology PDFDocument6 pagesAppenix19 - IDNT Terminology PDFAkiara KazuiNo ratings yet
- Jurnal Pangan Dan GiziDocument65 pagesJurnal Pangan Dan GiziUmi Kalsum IdrusNo ratings yet
- Toxi Medik-2Document39 pagesToxi Medik-2Wahyu MargariniNo ratings yet
- Nutrition Counseling During Pregnancy On Maternal Weight GainDocument4 pagesNutrition Counseling During Pregnancy On Maternal Weight GainAbha AyushreeNo ratings yet
- Nutrition Therapy For Upper Gastrointestinal Disorders Case QuestionsDocument11 pagesNutrition Therapy For Upper Gastrointestinal Disorders Case QuestionspeytonNo ratings yet
- MEDICAL NUTRITION THERAPY FOR ANEMIADocument39 pagesMEDICAL NUTRITION THERAPY FOR ANEMIAYanuarti PetrikaNo ratings yet
- Pengaruh Penambahan Tepung Daun Kelor Terhadap Daya Terima Dan Kadar Protein Mie BasahDocument6 pagesPengaruh Penambahan Tepung Daun Kelor Terhadap Daya Terima Dan Kadar Protein Mie BasahVina SoumokilNo ratings yet
- Hubungan Pengetahuan Gizi Aktivitas FisikDocument5 pagesHubungan Pengetahuan Gizi Aktivitas FisikshofiNo ratings yet
- PES StatementsDocument6 pagesPES Statementsdoniazad13112No ratings yet
- Metabolic Stress Case StudyDocument10 pagesMetabolic Stress Case StudydakotaNo ratings yet
- Nutrition For Athletes - CSUDocument5 pagesNutrition For Athletes - CSUherkamayaNo ratings yet
- Nutrition Services Screening Assessment (NSSA) SebagaiDocument8 pagesNutrition Services Screening Assessment (NSSA) SebagaiEko RistiyantoNo ratings yet
- Enteral Nutrition Administration Inconsistent With Needs (NI-2.6)Document2 pagesEnteral Nutrition Administration Inconsistent With Needs (NI-2.6)Hasna KhairunnisaGIZINo ratings yet
- NUTRITION Program PlanningDocument5 pagesNUTRITION Program PlanningDr Rajan Dubey100% (1)
- 01.0 Nutrition Assessment & Monitoring & Evaluating TerminologyDocument5 pages01.0 Nutrition Assessment & Monitoring & Evaluating TerminologyYuznia Sari Andhika PutriNo ratings yet
- Nutrition Management For AthleteDocument10 pagesNutrition Management For AthleteMahayu Firsty RamadhaniNo ratings yet
- Introduction To Writing Pes StatementsDocument3 pagesIntroduction To Writing Pes Statementsapi-434982019No ratings yet
- Case Studies - Type 1 DiabetesDocument4 pagesCase Studies - Type 1 Diabeteszenagit1234560% (2)
- Artikel MelaDocument14 pagesArtikel MelaRobi UcibeNo ratings yet
- Gizi Seimbang VegetarianDocument17 pagesGizi Seimbang VegetarianroropujiNo ratings yet
- Oncology AdimeDocument2 pagesOncology Adimeapi-299929867No ratings yet
- Chronic Kidney Disease Case StudyDocument5 pagesChronic Kidney Disease Case Studyhailey guzzoNo ratings yet
- Medicine and Nutrition Case StudyDocument5 pagesMedicine and Nutrition Case Studyapi-384113918No ratings yet
- TM 1 - Formulasi & Fortifikasi Gizi AJDocument91 pagesTM 1 - Formulasi & Fortifikasi Gizi AJKyoumi OfficialNo ratings yet
- Study Evaluates Food Waste and Food Costs for Patients at Two Makassar HospitalsDocument5 pagesStudy Evaluates Food Waste and Food Costs for Patients at Two Makassar HospitalsDaraa Ananda100% (1)
- Menu Sehari 1800 Kkal ETPTDocument4 pagesMenu Sehari 1800 Kkal ETPTAzizaNo ratings yet
- Form Pg-Sga PDFDocument2 pagesForm Pg-Sga PDFzain syalsabila0% (1)
- A S P E N Clinical Guidelines - Nutrition Support of The Critically Ill ChildDocument56 pagesA S P E N Clinical Guidelines - Nutrition Support of The Critically Ill ChildPaulina Kristiani BangunNo ratings yet
- Pes Statements SamplesDocument19 pagesPes Statements SamplesJennie ManobanNo ratings yet
- ESPEN Guidelines On Parenteral Nutrition. Intensive Care 2009Document38 pagesESPEN Guidelines On Parenteral Nutrition. Intensive Care 2009ERINSONNo ratings yet
- Medical Nutrition TherapyDocument4 pagesMedical Nutrition TherapycjgregoryNo ratings yet
- Medical Nutrition Therapy For Renal Disease 2016Document39 pagesMedical Nutrition Therapy For Renal Disease 2016Steven FongNo ratings yet
- The Evaluation of Antihypertensive Drug Usage Toward Hypertension Patients with Complications at Hospital X Surakarta 2014Document15 pagesThe Evaluation of Antihypertensive Drug Usage Toward Hypertension Patients with Complications at Hospital X Surakarta 2014Ghea RofifahNo ratings yet
- Modifikasi Resep Brownis Untuk Makanan Selingan Penderita Diabetes MellitusDocument5 pagesModifikasi Resep Brownis Untuk Makanan Selingan Penderita Diabetes MellitusRegitaand PutNo ratings yet
- Case Study 30Document6 pagesCase Study 30api-276551783No ratings yet
- Case Study 19Document3 pagesCase Study 19api-533641139No ratings yet
- 3458 7242 1 SM PDFDocument9 pages3458 7242 1 SM PDFJuhariah Aring RNo ratings yet
- Case Study31Document5 pagesCase Study31api-276551783No ratings yet
- Reading Comprehension DeviDocument6 pagesReading Comprehension DeviDevi Rahma YuniNo ratings yet
- (Spmi) KELOMPOK 1 - Menu Panti AsuhanDocument12 pages(Spmi) KELOMPOK 1 - Menu Panti Asuhanputri n.kNo ratings yet
- Soal 1Document7 pagesSoal 1shofiNo ratings yet
- Drug-Nutrient Interaction in Prescriptions ForDocument7 pagesDrug-Nutrient Interaction in Prescriptions ForRafika DitaNo ratings yet
- fshn420 - Cancer Case StudiesDocument5 pagesfshn420 - Cancer Case Studiesapi-703153445No ratings yet
- Nutrition Support Internship Case Study 1Document5 pagesNutrition Support Internship Case Study 1api-457873289No ratings yet
- Master Tabel SpssDocument3 pagesMaster Tabel SpssIrene Sri Malem SembiringNo ratings yet
- Nutrition Diagnosis Etiology Matrix PDFDocument16 pagesNutrition Diagnosis Etiology Matrix PDFLaura BrownNo ratings yet
- Nutrition Diagnosis Etiology Matrix (ADANCP)Document16 pagesNutrition Diagnosis Etiology Matrix (ADANCP)Firman WayNo ratings yet
- Nutrition Diagnosis Etiology Matrix: (Diagnostic and Statistical Manual of Mental DisordersDocument13 pagesNutrition Diagnosis Etiology Matrix: (Diagnostic and Statistical Manual of Mental DisordersVivin Syamsul ArifinNo ratings yet
- NutritionDiagnosisEtiologyMatrix 2013 PDFDocument16 pagesNutritionDiagnosisEtiologyMatrix 2013 PDFMuhammad YunusNo ratings yet
- Nutrition Diagnosis Domains and Terms: Behavior: Knowledge and BeliefDocument6 pagesNutrition Diagnosis Domains and Terms: Behavior: Knowledge and BeliefIlmi Dewi ANo ratings yet
- Spain Usa ExtraditionDocument2 pagesSpain Usa ExtraditionAdrian BirdeaNo ratings yet
- AMU2439 - EssayDocument4 pagesAMU2439 - EssayFrancesca DivaNo ratings yet
- Deforestation Contributes To Global Warming: Bruno GERVETDocument11 pagesDeforestation Contributes To Global Warming: Bruno GERVETMajid JatoiNo ratings yet
- Maheshwar Handlooms Cluster Diagnostic StudyDocument15 pagesMaheshwar Handlooms Cluster Diagnostic Studyumang31390100% (3)
- Business Plan Presentation ON Air Conditioner: Presented By-V.Sowmith REG NO-2121BM010112Document16 pagesBusiness Plan Presentation ON Air Conditioner: Presented By-V.Sowmith REG NO-2121BM010112Kavya Madanu100% (1)
- JKFBDDocument2 pagesJKFBDGustinarsari Dewi WNo ratings yet
- Training Plan JDVP 2020 - BPP (40days)Document36 pagesTraining Plan JDVP 2020 - BPP (40days)Shallimar Alcarion100% (1)
- Case Digest For Labor Relations 2Document40 pagesCase Digest For Labor Relations 2zeigfred badanaNo ratings yet
- Apple Mango Buche'es Business PlanDocument51 pagesApple Mango Buche'es Business PlanTyron MenesesNo ratings yet
- Doulci Activator For IOS 9Document2 pagesDoulci Activator For IOS 9Syafiq Aiman100% (2)
- TAFJ-H2 InstallDocument11 pagesTAFJ-H2 InstallMrCHANTHANo ratings yet
- Present Tense Exercises. Polish A1Document6 pagesPresent Tense Exercises. Polish A1Pilar Moreno DíezNo ratings yet
- Compilation of Activities UBCVDocument13 pagesCompilation of Activities UBCVRenell Vincent RamosNo ratings yet
- Jhansi Aptc Form 40 A 1Document1 pageJhansi Aptc Form 40 A 1Siva KumarNo ratings yet
- PNP TELEPHONE DIRECTORY As of JUNE 2022Document184 pagesPNP TELEPHONE DIRECTORY As of JUNE 2022lalainecd0616No ratings yet
- Cast Copper Alloy Solder Joint Pressure Fittings: ASME B16.18-2018Document41 pagesCast Copper Alloy Solder Joint Pressure Fittings: ASME B16.18-2018crescon designNo ratings yet
- Drama For Kids A Mini Unit On Emotions and Character F 2Document5 pagesDrama For Kids A Mini Unit On Emotions and Character F 2api-355762287No ratings yet
- HED - PterygiumDocument2 pagesHED - Pterygiumterry johnsonNo ratings yet
- Issues and Concerns Related To Assessment in MalaysianDocument22 pagesIssues and Concerns Related To Assessment in MalaysianHarrish ZainurinNo ratings yet
- AIESEC - Exchange Participant (EP) GuidebookDocument24 pagesAIESEC - Exchange Participant (EP) GuidebookAnonymous aoQ8gc1No ratings yet
- Reaction PaperDocument1 pageReaction Papermarvin125No ratings yet
- Unit 2 - BT MLH 11 - KeyDocument2 pagesUnit 2 - BT MLH 11 - KeyttyannieNo ratings yet
- Script For The FiestaDocument3 pagesScript For The FiestaPaul Romano Benavides Royo95% (21)
- Eng 188 Change in Ap, Ae, and ErrorsDocument5 pagesEng 188 Change in Ap, Ae, and Errorsmkrisnaharq99No ratings yet
- Scholarship For Yemeni StudentsDocument45 pagesScholarship For Yemeni Studentshilal_lashuel80% (10)
- The Ramayana and The Sacred Palm Trees of Sumeria, Mesopotamia, Assyria and PhoeniciaDocument7 pagesThe Ramayana and The Sacred Palm Trees of Sumeria, Mesopotamia, Assyria and PhoeniciaNeeta RainaNo ratings yet
- Dukic WarehouselayoutsDocument14 pagesDukic Warehouselayoutsrohitkamath7No ratings yet
- Calvo, G (1988) - Servicing The Public Debt - The Role of ExpectationsDocument16 pagesCalvo, G (1988) - Servicing The Public Debt - The Role of ExpectationsDaniela SanabriaNo ratings yet
- Module 1 in Contemporary Arts First MonthDocument12 pagesModule 1 in Contemporary Arts First MonthMiles Bugtong CagalpinNo ratings yet