Professional Documents
Culture Documents
What Is Primary Complex
Uploaded by
Mary CruzOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
What Is Primary Complex
Uploaded by
Mary CruzCopyright:
Available Formats
What is Primary Complex?
Children exposed to Mycobacterium tuberculosis may sometimes develop a tuberculosis (TB) infection called Primary Complex. The most common route of infection is through inhalation. A person with active TB coughs up the germ and it is inhaled by a healthy child. The TB then travels to the lungs. The immune system kicks in and quarantines the germ at the local site and at the neighboring lymph nodes (this forms the walled-in complex).The child remains healthy and usually has no symptoms. They may remain symptom free until their immune system declines and the disease becomes active. How do you diagnose Primary Complex? As most patients have no symptoms, they only find out they have Primary Complex through a tuberculin skin test (also called a Mantoux test or PPD test). A small amount of purified protein derivative (a.k.a. PPD) of the TB germ is injected superficially into the forearm. An itchy, raised, red reaction past a certain size (this changes depending on other conditions) is considered positive. In 20% of cases, a PPD test will be negative in patients with TB infection. Other times, children will have a falsely positive PPD test because they had the BCG BCG (Bacillus Calmette-Guerin) vaccine. Should Primary Complex be treated? Yes. If primary complex is left untreated, it may eventually evolve into active tuberculosis. Drug treatment choices vary depending on the drug resistance to tuberculosis. Is Primary Complex contagious? No. As the infection is walled-in it cannot be spread. How do you prevent Primary Complex? Avoid symptomatic (coughing) individuals that are high risk to have tuberculosis. There is also a vaccine for TB that has mixed results as to whether it actually prevents the disease. It is known to prevent severe disseminated or dispersed TB infection. Make sure to include household help as well when getting tested for Primary Complex. So anyways, here are the 3 things you need to know when battling Primary Complex. Primary Complex is not contagious. Dont ever make your kids feel that what they have is something to be embarrassed about. Based on my readings and from my pedia, Primary Complex is now common here in the country. Its not as scary as it used to be ten years ago and it can be easily cured. Primary Complex is a form of Tuberculosis on kids. They got it from an adult. When an adult suffering from Tuberculosis made contact to a kid through cough and sneeze, the mycrobacteria M. tuberculosis is transferred to the kid. Primary Complex is a 6 month long treatment. Not lesser. You need to make sure that you give the meds everyday religiously for 6 months. If not, the bacteria will just evolve and will develop into a more med resistant kind. When treating Primary Complex, here are some tips that may come in handy: During the first 4 months, your kids need to take in 3 types of medicines (photo above). On the 5th and 6th month based on the advise of your pedia, the meds may be lessen to two kinds. It is best to give them meds on the morning, 30 minutes before eating but you can also give it during lunch time (just make sure that you give it 30 minutes before meal time). Also take note of the time you give the meds, it should be the same time all through out the treatment period.
The three meds have different consistencies. If your kids are a bit hard when it comes to medicine, you should give them the pink med first as this is the most ill tasted. This is done so that whenever the kid refused to swallow it up or throw it up, they hadnt taken in the other meds yet. Give the yellowish next and give the red one last. The red one is the most difficult to swallow, hence they will need a lot of water to consume it. You should give it to them last because they would be full from drinking water to help them swallow the red one. Stick to the meds your doctor gave you. I tried buying the cheaper kit but it turns out that though I save on money, my kids did not like the taste of the cheaper kind. The photo above is the set from Unilab. Trust them to be childs tongue friendly (TasteRite technology). If you child gains weight easily, you might wanna consult your pedia every month for the dosage as its effectiveness rely on the weight of the kid. How much is Primary Complex Treatment? In order for you to know if your kid is suffering from Primary Complex, they will have to undergo two kinds of test, XRAY and PPD (purified protein derivative) or tuberculin skin test. XRAY test can vary from 300 Philippine Pesos to more than 1K depending on your hospital. In some hospitals, this is shouldered by your HMO, in some it is not. PPD or Tuberculin Skin test ranges from 600 Pesos to more than 1k, again, depending on your provider and this is NOT shouldered by HMO. The HRZ Kit (Isoniazid + Rifampicin + Pyrazinamide) from Unilab was less than 500 the last time I bought, so that was last year. A kid can consume 1 to 2 (or 1 to 2 big HRZ kit) bottle a month depending on his weight. It is best to buy it in pack (HRZ kit) as you can save a lot than buying the medicine per bottle. Trust me, I have been there, spend time computing it to see where I can save more. (I will try to update this when I got the prize of each meds). Rimafed or the red one will be consumed more than the other two. Rimafed is given in more ml than the other two that is why. The total amount of Peso you will have to spend when treating Primary Complex (if you have a kid that is less than 15 kilos) is around (cost of xray and ppd not included) 5000 Pesos. Stage 1 Exposure has occurred, implying that the child has had recent contact with an adult who has contagious TB. The child has no physical signs or symptoms and has a negative tuberculin skin test (TST) result (see Tuberculin Skin Test). Chest radiography does not reveal any changes at this stage. Not all patients who are exposed become infected, and the TST result may not be positive for 3 months. Unfortunately, children younger than 5 years may develop disseminated TB in the form of miliary disease or TB meningitis before the TST result becomes positive. Thus, a very high index of suspicion is required when a young patient has a history of contact. Go to Miliary Tuberculosis, and Tuberculous Meningitis for more information on these topics. Stage 2 This second stage is heralded by a positive TST result. No signs and symptoms occur, although an incidental chest radiograph may reveal the primary complex.
Stage 3 In stage 3, TB disease occurs and is characterized by the appearance of signs and symptoms depending on the location of the disease. Radiographic abnormalities may also be seen. Stage 4 Stage 4 is defined as TB with no current disease. This implies that the patient has a history of previous episodes of TB or abnormal, stable radiographic findings with a significant reaction to the TST and negative bacteriologic studies. No clinical findings suggesting current disease are present. Stage 5 TB is suspected, and the diagnosis is pending.
TB is difficult to diagnose in children because it is hard to confirm the diagnosis by culture even where laboratory facilities are good. The presence of HIV makes the task even more difficult, resulting in some children being misdiagnosed as having TB and given treatment, while others with TB may be falsely negative and not receive treatment. The current international TB control strategy focuses on active pulmonary TBthe source of most TB infection in childrenbut does not address children and adolescents as vulnerable sub-groups. Furthermore, vaccination of infants with BCG is no longer believed to prevent active TB in adulthood, although it can protect children from the disseminated forms of the disease, for example, tuberculosis meningitis. Children are exposed to TB primarily through contact with infectious adultswith special risk in high TBHIV settingsand will continue to be at risk for TB as long as those adults remain untreated. Curing TB and preventing its spread in the wider community is thus one important strategy to reducing children s vulnerability to TB. No vaccine yet exists that is truly effective against pulmonary disease. BCG vaccine (Bacillus Camille Guerin) was invented in 1921. It is useful in preventing certain types of TB, namely miliary and meningeal tuberculosis occurring in the first year of life, but is not effective in preventing the development of pulmonary TB in adulthood. Children are also vulnerable to the direct and indirect impacts of other family members having TB. Already marginal households that lose income or incur debt due to TB will experience even greater poverty as budgets are cut and assets sold. If their primary care giver is ill or is preoccupied with caring for other ill family members, the childs care and education may be neglected. If the principal family provider is ill and cannot work, children risk malnutrition, which increases susceptibility to TB and brings with it lifelong deleterious effects on both health and education. Children are especially vulnerable if their mother becomes sick and dies. There is a strong correlation between maternal survival and child survival to age 10. One study in Bangladesh revealed that whereas a fathers death increased child mortality rates by 6 per 100 000 for both boys and girls, a mothers death was associated with increases of 50 per 100 000 in sons and 144 per 100 000 in daughters. Children in households with TB may also be taken out of school or sent to work. Both scenarios deprive them of their right to education and put them in situations that may expose them to more prolonged contact with persons with active TB. In rural Uganda, for example, 32 patients were interviewed about the economic costs of TB. Five of their children had had to be withdrawn from school because fees could not be paid. Even if not removed from school, children from poor or marginalized communities where poor nutrition and ill-health prevail have a below-average school enrolment and attendance rate and, as a result, lower-than-average educational attainment. Lack of education correlated negatively with access to health services, and the neglect of the right to education on childrens current and future health can be profound.
Reasons why children have a high risk of developing active TB disease The immune system of young children is less developed than that of an adult and the risk of developing active TB disease is therefore higher in young children. The chance of developing TB disease is greatest
shortly after infection. When children present with active tuberculosis disease their family members and other close contacts should be investigated for TB to find the source of the disease and treat them as necessary. Therefore a good TB control programme, which will ensure early diagnosis and treatment of adults with infectious form of TB is the best way to prevent TB in children. In HIV infected children the risk is very high to develop TB meningitis with often devastating results for the child like deafness, blindness, paralysis and mental retardation as some of the consequences. Tuberculosis and malnutrition often go together, and a child with TB disease may present as failure to gain weight with loss of energy and a cough lasting for more than three weeks.
Tuberculosis immunology in children: Diagnostic and Therapeutic challenges and opportunities Tuberculosis (TB) is one of the most important causes of infectious morbidity and mortality worldwide. Young children are more likely to develop severe disease from the causative agent Mycobacterium tuberculosis. These clinical observations likely reflect fundamental differences in the immune systems of young children and adults. Essential to effective TB immunity are functioning macrophages, dendritic cells, strong Th1-type T-cell immunity and a relative absence of Th2-type T-cell immunity. Critical differences between adults and children relevant to TB immunity include deficiencies in macrophage and dendritic cell function, deficiencies in the development of Th1-type T-cells in response to pathogens, and the propensity for infants and young children to develop Th2-type CD4+ T-cells in response to immunogens. In this article, knowledge about the requisite components of protective immunity, differences between the immune systems of children and adults relevant to pediatric tuberculosis, M. tuberculosis-specific T-cell immunity in children, and potential application to immunodiagnostics and vaccine development will be reviewed. Identifying TB in Children Vaccination has been the primary TB prevention method in children. In fact, BCG is the most widely used vaccine in the world. Although it is relatively ineffective in preventing infectious forms of TB, it does prevent more serious forms of TB disease in children. Nevertheless, a quarter of a million children still develop TB every year: Particularly vulnerable to infection from household contacts, many of them have been infected in their own homes, by parents or other relatives with active, infectious TB. Diagnosis of TB in children is notoriously difficult, as the early symptoms and signs are easily missed. Most national TB control programmes have little in the way of services for children. TB in the family also has a serious impact on children. In India alone, 300,000 children are taken out of school every year to care for a parent sick with TB. Tuberculosis (TB) is a serious infection caused by the bacteria Mycobacterium tuberculosis. Unfortunately, the incidence of tuberculosis has been increasing in recent years and there are an increasing number of cases of multi-drug resistance tuberculosis. Routine testing for TB with a tuberculin skin test is now only recommended in children who are at high risk for having the illness. Risk factors include being exposed to an infected adult, contact with someone
who has been in prison, contact with the homeless, and travel to countries with a high rate of tuberculosis, including Mexico, India, Vietnam, China, Philippines, and many countries in Latin America, Asia, the Middle East and Africa. Adopted children from any high risk area should also be tested, including Romania and Russia. Also, all contacts of a person with a positive tuberculin skin test should also be tested. Even with a negative test, some younger children may need a chest x-ray and treatment if they were recently exposed to someone with tuberculosis and that person was thought to be contagious. Negative skin tests may need to be repeated in three months. Testing for tuberculosis is by the tuberculin skin test, which is usually a Mantoux test with 5 units of purified protein derivative (PPD). Other forms of testing are not recommended. After being placed on a child's forearm, the tuberculin skin test should be read 48-72 hours later by experienced personnel. Interpretation depends not only on the type of reaction after the test, but also the child's risk of having tuberculosis. A child over 4 years of age with no risk factors may have a small reaction (5-14mm of induration) and not have a tuberculosis infection, while a child who has had close contact with someone with tuberculosis will be considered infected even with a very small reaction (greater than or equal to 5mm induration). Even children who have received the BCG vaccine can have skin testing done. Children exposed to someone with tuberculosis will likely develop a positive tuberculin skin test about 212 weeks later. Some children, especially with immune system problems, can have a negative tuberculin skin test and still be infected with tuberculosis. Most children with tuberculosis do not have symptoms. They have a positive PPD, a normal chest x-ray and no signs or symptoms of tuberculosis and are said to have a tuberculosis infection or a latent tuberculosis infection. Even though they do not have symptoms, people with a positive PPD need treatment, which usually consists of 9 months of isoniazid. If the infection is thought to be resistant to isoniazid, then rifampicin may be used for 6 months. Children with symptoms of tuberculosis, a positive tuberculin skin test and/or a positive chest x-ray are said to have tuberculosis disease. This is more serious than just have a tuberculosis infection. If untreated, children with a tuberculosis infection can develop tuberculosis disease (usually within six months to two years), with symptoms including a cough, fever, night sweats, swollen glands, decreased appetite and activity, weight loss and difficulty breathing. In addition to the tuberculin skin test, children with tuberculosis disease should have additional testing to try and culture the tuberculosis bacteria so that it can be determined which drugs the infection is sensitive to. Because tuberculosis is a slow growing bacteria, culture can take as long as ten weeks for a final result. To obtain a culture, unless the child has a productive cough and can produce a sputum sample, cultures may need to be obtained from a gastric aspirate in the early morning. Children with tuberculosis disease should also be tested for HIV. In the lungs, tuberculosis causes the formation of cavitary lesions, pleural effusions and enlarged lymph nodes. These can usually be seen on a chest x-ray. In addition to the pulmonary symptoms described above, tuberculosis can also cause meningitis and infections of the ear, kidney, bones and joints.
Treatment of tuberculosis is with long-term use of a combination of antibiotics, depending on whether or not it is resistant to commonly used drugs. Treatment should be coordinated with the local health department and/or a pediatric infectious disease specialist. Treatments for tuberculosis disease involving the lungs consists of 6 or 9 months regimens including isoniazid, rifampin and pyrazinamide. Another drug, either ethambutol or streptomycin may be needed for multi-drug resistant TB. Extrapulmonary tuberculosis (either meningitis or infections of the bones or joints) usually includes a 9-12 month regimen of three or four drugs, depending on resistance. Most people with tuberculosis disease need to undergo directly observed therapy (DOT) in which treatment is observed by a health care worker, either in person or sometimes by video. Adults with tuberculosis disease are contagious for at least a few weeks after beginning proper treatment. Children with tuberculosis disease are not as contagious, because they usually have smaller lung lesions and do not cough as much.
Children at greater risk for Tuberculosis Some groups of children are at greater risk for tuberculosis than others. These include: Children living in a household with an adult who has active tuberculosis Children living in a household with an adult who is at high risk for contracting TB Children infected with HIV or another immunocompromising condition Children born in a country that has a high prevalence of tuberculosis Children from communities that are medically underserved
Tuberculosis in children is a grossly neglected area Potentially one of the most devastating infectious diseases in the world, tuberculosis accounts for 2 million deaths a year, including over 250,000 children. Tuberculosis in children suffers from an appalling lack of investigation, which leaves many unanswered questions. What is required? There is an urgent need for child-specific TB prevention and care strategies integrated within national TB control programmes.
Children are highly susceptible to tuberculosis. It has been estimated that as many as one third of the world's population is infected with TB with an estimated 20-50% of children who live in households with active tuberculosis become secondarily infected. Children are particularly vulnerable to infection from household contacts as they are often held close and breathed on. Consider the risk for children in high-burden tuberculosis countries in the developing world where family size is large, living quarters are crowded and more than half the population are children. What is required?
The current DOTS strategy is geared to identifying adults with tuberculosis and treating them under direct observation. The World Health Organization recommends that once an adult has been diagnosed with tuberculosis, the child contacts should be identified and treated under the same program as the adult. Standard tuberculosis drugs are inexpensive and well-tolerated by children.
A better vaccine is needed. The TB vaccine, BCG, addresses the tuberculosis problem in children partially, but not adequately. It limits the severe, disseminated forms of tuberculosis which are unique to young children with tuberculosis, but does not prevent them all. Tens of thousands "immunized" children in the developing world still suffer from tuberculosis meningitis and other disseminated forms of disease. What is required? There is an urgent need to establish an international research agenda for childhood tuberculosis and to work towards establishing research programs for better vaccines. Traditional diagnosis of TB in children is ineffective. A vast number of children infected remain undiagnosed. These silently infected children create a reservoir of future adult disease. Early symptoms and signs of tuberculosis in children are common and easily missed. They include failure to thrive, weight loss, fever, and lethargy. What is required? Early diagnosis can be made with skin testing, even with prior BCG immunization, or with chest X-rays. This must be made more available in the developing world.
Introduction to TB Tuberculosis (TB) is at least as old as mankind and the history of this disease is intertwined with the history of civilization. Like no other illness, TB has taken its toll of human life over the millennia and has spread worldwide. Due to its worldwide incidence and prevalence, it has been referred to as "White Plague". Robert Koch first described the tubercle bacillus in 1882.They are slender, rod-shaped, aerobic, nonspore forming and non-motile bacteria. One of the most striking feature of these bacilli is the acidfastness i.e: difficult to stain. But once stained, they strongly retain the dye, which is not removed even by acid alcohol. These can also be stained with fluorescent dyes. These are 2 - 4 micrometer long and 0.2 -0.5 micrometer wide in size. TB is an infection, often of long term duration caused by 2 species of family Mycobacteriaceae, Order Actinomycetales-- M. tuberculosis and M. bovis which is the main cause of TB in humans, transmitted through unpasteurized milk. These mycobacteria can cause disease in virtually every organ system in the body predominantly in the lungs. The disease is characterized histologically by granuloma formation. TB-Disease How does the tuberculosis spread ? TB is contagious. TB is spread through the air by a person suffering from TB. A single patient can infect 10 or more people in a year. M. tuberculosis infection occurs due to inhalation of droplet nuclei i.e. infectious particles aerosolized by coughing, sneezing or talking. These are sufficiently small to dry while airborne, remain suspended for long periods and reach terminal air passages of the lungs. It has been observed that a cough from an infected person produces 3000 infectious droplet nuclei. Accordingly, the air in a room occupied by him may remain infectious even during his temporary absence. TB-Symptoms Common symptoms of tuberculosis are: Cough for three weeks or more, sometimes with blood-streaked sputum Fever, especially at night Weight loss Loss of appetite Risk factors Malnutrition, immunosuppression and AIDS greatly favour progression of infection to active disease.
TB-Diagnosis Tuberculin Skin Test (TST) The TST is widely used as a supportive second line test to identify patients actively infected with tuberculosis. It has remained more or less unchanged for the last 60 years and has been in existence for more than 100 years. There are three types of tuberculin skin test but the most common is the Mantoux test. The skin test works by injecting Purified Protein Derivative (PPD) into the skin. PPD is a collection of mixed proteins and other materials filtered from killed M. tuberculosis cultures. The test works on the basis that if the body has been exposed to infection with TB it will recognise the proteins and mount an immune response to it. This response would take the form of a lump, swelling or blister at the site of injection. If there is a lump (called an induration) then this may mean that the person is infected. Unfortunately, the skin test has a poor sensitivity (the ability to detect infection if it is present). This sensitivity falls further if the person being tested has had the BCG vaccination earlier in life or if they have a depressed immune system (immunocompromised) due to other illness or medical treatment. TB skin test is also known as Mantoux test. It is the most widely used test in which graded doses of tuberculin are injected intradermally on the forearm using a tuberculin syringe. Koch's tuberculin was an impure extract of boiled culture of tubercle bacilli. In 1934, Siebert made a simple protein precipitate of the old tuberculin (one prepared by Koch) and named it as purified protein derivative (PPD). During 1970, it was recognized that PPD in solution adheres to glass to the extent that 20% of its potency can be lost in 30 minutes and 80% in 24 hours. This can be prevented by addition of Tween 80. Procedure: 0.1 ml of the 5 TU of PPD is injected intradermally on the forearm. On examination after 48-72 hours a positive reaction is indicated by erythema and in duration of > 10 mm size. Erythema(Redness) alone is not taken as positive reaction. Tuberculin skin testing is used as an aid in diagnosing active infection in infants and young children, to measure the prevalence of infection in a community and to select susceptible or high risk patients for BCG vaccination. All persons with prior infection with tubercle bacilli will exhibit a positive response. Some of the common problems doctors and nurses encounter with the skin test are described below: False positives As the active ingredient used in the skin test contains a whole series of proteins that are shared with the BCG vaccine and other mycobacterium common in the environment, the skin test is commonly falsely positive in people who have had no exposure to TB. Common causes of false positive results are prior BCG vaccination and infection with other types of bacteria that are similar to TB. As a large percentage of the world's population is BCG vaccinated this causes considerable problems; it is currently estimated that almost one third of people positive to the TST do not actually have TB infection.
False negatives The sensitivity of the skin test is estimated to be only around 70% in known active TB cases; so the test misses up to 30% of the people who are infected. This sensitivity decreases to as low as 30% in the immunocompromised (which means the error rate can climb to 70% in these people). This makes it very difficult for a doctor to be able to make the right medical decisions because the reliability of the result is so poor. Subjectivity and variability The skin test is difficult to administer correctly as small variations in the way it is done vary the amount of PPD delivered into the skin and thus the resulting size of the reaction. Furthermore, the measurement of the reaction is highly subjective; the variations in diagnosis based on different clinicians reading the same bump in different ways is well documented. Boosting A common problem in those people who are regularly screened for TB infection using the skin test (e.g. Healthcare Workers) is that they start to become immunised to PPD by the repeated administrations of it. This is called 'boosting' and results in a false positive reaction to the skin test. Convenience & Resources The skin test is not patient friendly as it can result in painful blistering at the injection site and result in a scar. It also requires two patient visits - one to inject the tuberculin and one to read the induration (although it is estimated that a third of people never return to have the test read). This is inconvenient for the clinician and patient alike
Sputum Smear Microscopy (SSM) The simplest laboratory test is the examination of sputum (matter thrown up from the lungs) for the detection of a certain type of bacteria. It is cheap and is performed in minutes. This test is based on the principle of Ziehl Neelsen diagnostic technique of direct smear microscopy of sputum. The unique properties of bacterial cell wall of Mycobacterium tuberculosis allows it to retain the primary stain even after exposure to strong acid solutions, they are called acid-fast. In the Ziehl Neelsen staining procedure, using carbol fuschsin and methylene blue, the acid-fast organisms appear red. Learn More on Acid Fast Direct Microscopy Acid-Fast Direct Smear Microscopy- A Laboratory Training Program TECHNICAL GUIDE on Sputum Examination for Tuberculosis by Direct Microscopy in Low Income Countries, Fifth edition 2000 International Union Against Tuberculosis and Lung Disease However, the WHO estimates that it only identifies 35% of patients with active TB. As the test is based on sputum, it has particular difficulty in detecting non-pulmonary TB. This test will also identify certain types of bacteria that are not M. tuberculosis and so it cannot always distinguish between TB and other infections. Despite these shortcomings, it is still the front line tool for active TB diagnosis, partly because
the more definitive culture techniques take longer and partly because it can help determine if a person is infectious. It is argued that as long as bacteria are found in the sputum the patient can continue to pass on the disease to other people. Sputum smear is therefore one method that can be used to monitor an active TB patient's response to treatment.
Chest X-ray Chest x-rays are used to check for lung abnormalities in people who have symptoms of TB disease, but the chest X-ray cannot confirm that a person has active TB, especially if the infection is not in the lungs as in 40% of all cases of active TB. The chest X-ray also has a poor ability to detect infection in the early stages of disease, the damage to the lungs may not yet have become sufficiently marked to be detectable by chest X-ray and thus people who have active TB can be missed. Further, scarring in the lungs remains after a previous TB disease (even if the patient is completely cured) and therefore it is difficult to distinguish past cured TB from current active disease.
Polymerase Chain Reaction (PCR) This technique detects the presence of DNA-type (genetic) material from bacteria by effectively amplifying the measurable amount. Polymerase chain reaction (PCR), is a relatively new development in active TB testing. Even though PCR techniques can magnify even the smallest amounts of genetic material, the sample used still has to contain a certain number of TB bacteria and this is not always possible, particularly with non-pulmonary TB where sensitivity can be as low as 60%. To increase the number of bacteria, and hence improve the sensitivity of the test, the laboratory will often culture the sample, to allow the bacteria to multiply, before carrying out the PCR test. This can take several days or weeks. The test is also relatively complicated to run in the laboratory, is prone to cross contamination and can be expensive. The main use of PCR is not to diagnose TB per se , but to rule out other types of infection in a sputum smear positive patient, before culture results are known.
Culture Cell culture techniques (where live bacteria are grown on a plate in the laboratory) are still seen as the gold standard for active TB as they are extremely sensitive if live mycobacteria can be obtained in the sample. M. tuberculosis can be cultured (grown) from a variety of specimens and can be used to detect pulmonary as well as extra-pulmonary disease. By assessing the effect of antibiotics on the cultured bacteria, this technique can also provide data on likely effectiveness of certain antibiotics. However, it is not always possible to obtain bacteria in the sample, especially in non-pulmonary TB and the test is therefore not always reliable. A drawback of this test is the time to result, which can be anything from two to six weeks.
Blood Test for TB detection QuantiFERON-TB Gold http://www.cellestis.com/IRM/content/home/QFT-GOLDFactSheet.pdf http://www.cdc.gov/mmwr/preview/mmwrhtml/rr5415a4.htm T-SPOT TB Test http://www.oxfordimmunotec.com/products_services/uses.html TB-Tratment Options Treatment of tuberculosis include use of 4 drugs: Rifampicin ( R ) Isoniazid ( H ) Ethambutol ( E) Pyrazinamide ( Z) In some cases of TB it is use of Streptomycin (S ) is recommended. These drugs are known as 1st line drugs for TB. MDR TB TB remains one of the worlds leading infectious causes of adult deaths; furthermore, multidrugresistant strains of the disease are emerging as a considerable threat to human health and a danger to TB control in numerous hot spots throughout the world.
Definition Strains of M.tuberculosis resistant to both isoniazid and rifampicin with or without resistance to other drugs have been termed multidrug-resistant strains. Multidrug-resistant tuberculosis (MDR-TB) is among the most worrisome elements of the pandemic of antibiotic resistance because TB patients that fail treatment have a high risk of death. While resistance to either isoniazid or rifampicin may be managed with other first-line drugs, resistance to both isoniazid and rifampicin (MDR-TB) demands treatment with second-line drugs. These drugs have limited sterilising capacity and are not suitable for short course treatment. Thus, patients with MDR-TB require prolonged treatment with drugs that are less effective and more toxic1. Therefore, it is necessary to distinguish MDR-TB from mere drug-resistant tuberculosis by performing mycobacterial culture and sensitivity testing because the therapeutic implications are different. Overview of the global situation of MDR TB According to WHO, resistance to tuberculosis drugs is probably present everywhere in the world. Certainly, MDR-TB is present in five continents, a third of the countries surveyed having levels above 2% among new patients. In Latvia 30% of all patients presenting for treatment had MDR-TB. The region of Russia surveyed had 5% of TB patients with MDR-TB. In the Dominican Republic, 10% of TB patients had
MDR-TB. In Africa, Ivory Coast has also witnessed the emergence of MDR-TB. Preliminary reports from Asia (India and China) show high levels of drug resistance as well. In the State of Delhi, India, 13% of all TB patients had MDR-TB.
Scenario In South- East Asia India Analysis of various studies in India has shown that the levels of drug resistance in newly detected cases have remained less than 5%. A retrospective analysis of various randomized clinical trials conducted by Tuberculosis Research Centre (TRC) with various rifampicin containing regimens in the intensive phase and with and without rifampicin in the continuation phase revealed an overall emergence of resistance to rifampicin in only 2% of patients, despite a high level (18%) of initial resistance to isoniazid either alone or in combination with other anti-TB drugs.10 Similar results were obtained in prospective studies conducted by NTI in patients on DOTS regimen in Bangalore. Thailand In Thailand the drug resistance status in 19992002 based on 1505 patients with no history of previous treatment was 9.5% for isoniazid, 8.2% to streptomycin and MDR-TB was 0.9%. Nepal For the same period, for Nepal corresponding figures for 755 patients were 5.4%, 8.9% and 1.9% respectively. Philippines Data from Makati Medical Centre DOTS Clinic (2003) indicates high incidence of MDR TB. Approximately 30% of isolates tested were resistant to all five first line drugs, 39.4% to four, 16.8% to three, 12.1% to two. Fluroquinolone resistance was noted in 40.9% isolates. While MDR-TB afflicts countries with poor health infrastructure, it is just as likely to break out in industrialized economies. During the late 1980s and early 1990s outbreaks of MDR-TB in North America and Europe killed over 80% of those who contracted it. The major TB outbreak in New York in the early 1990s was primarily a MDR-TB epidemic, with one in ten cases being drug-resistant. For more information on the Global Scenario of MDR TB see: http://www.who.int/tb/publications/who_htm_tb_2004_343/en/index.html http://whqlibdoc.who.int/hq/2000/WHO_CDS_TB_2000.278_intro.pdf http://www.tballiance.org/2_1_2_MDR_TB.asp Guidelines for Surveillance of Drug Resistance in Tuberculosis
http://whqlibdoc.who.int/publications/2003/9241546336.pdf Key factors for the management of MDR TB are as follows: Diagnosis of MDR TB Reliable susceptibility testing Prevention of MDR TB In new cases In old cases Designing an appropriate regimen Essential Drugs Second line Drugs Cross resistance Ranking with respect to Efficacy, Cost, Tolerance Reliable drug supply of second line drugs
Treatment of MDR TB It is important for the clinician to identify whether the patient is suffering from Drug resistant TB ( resistance to either INH or rifampicin ) or from MDR TB( resistance to both INH and rifampicin). This differentiation is important in order to decide the treatment regimens for the patient. While resistance to either isoniazid or rifampicin may be managed with other first-line drugs, resistance to both isoniazid and rifampicin (MDR-TB) demands treatment with second-line drugs . These drugs have limited sterilising capacity and are not suitable for short course treatment. Thus, patients with MDR-TB require prolonged treatment with drugs that are less effective and more toxic. Therefore, it is necessary to distinguish MDR-TB from mere drug-resistant tuberculosis by performing mycobacterial culture and sensitivity testing because the therapeutic implications are different. Principles to be followed while treating MDR-TB patients: Starting MDR-TB drug regimen Check the history of the patient carefully for previous treatment regimens. Check whether all drugs in the previous regimens have been taken and for how long. Determine the status of sputum smears at all junctures (in terms of positivity ,conversions and sensitivities if available). Confirmed/ Strongly suspect MDR TB Counsel the Patient and family members
Send Tissue / sputum for culture and sensitivity testing (if available)
Start MDR Regimen See the Guidelines for the management of Drug resistant Tuberculosis at http://www.who.int/docstore/gtb/publications/gmdrt/PDF/tb96_210.pdf Choice of drugs Add at least 3 new drugs. Preferably have an aminoglycoside (Streptomycin / Kanamycin / Amikacin/ Capreomycin). One fluoroquinolone (Ofloxacin / Ciprofloxacin / Levofloxacin). Ethionamide or Prothionamide Any one of the following: Cycloserine, PAS, Clofazimine or Moxifloxacin The treatment of MDR TB has been increasingly successful over the last decade, with reported cure rates over 80% in many settings. This is especially true when fluoroquinolones and adjuvant surgical therapy are used.
EXTRA PULMONARY TB Extra-pulmonary tuberculosis (EPTB) refers to disease outside the lungs. It is sometimes confused with non-respiratory disease. Disease of the larynx for example, which is part of the respiratory system, is respiratory but extra-pulmonary. Extra-pulmonary TB may be characterized by swelling of the particular site infected (lymph node), mobility impairment (spine),or severe headache and neurological dysfunction (TB meningitis) etc. Extrapulmonary TB is not accompanied by a cough because it does not occur in the lungs. It is equally important that both the infectious and non-infectious forms of TB are diagnosed and treated as both can be fatal. Development of extra-pulmonary disease At the time primary infection occurs blood or lymphatic spread of tubercle bacilli to parts of the body outside the lung may occur. In the fully immunocompetent host these bacteria are probably destroyed. If some immune deficit is present some may concentrate at a particular site where they may lie dormant for months or years before causing disease. Bacteria may be coughed from the lungs and swallowed. By this route they may enter the lymph nodes of the neck or parts of the gastro-intestinal (GI) tract. Before milk was routinely pasteurised cattle infected with M. bovis, the bovine variant of tuberculosis could pass disease to humans who drank infected milk. Transmission by this route would also give rise to GI diseases. The commonest sites of infection are: Lymph glands and abscesses particularly around the neck. Orthopaedic sites such as bones and joints. The spine is affected in about half such cases.
GU tract - In women uterine disease is probably the most common while in men the epididymis is the site most frequently affected. Both sexes are affected by renal , ureteric or bladder disease equally. Abdomen - This may affect the bowel and or peritoneum. Meningitis - which may be rapidly fatal if not, treated in time Pericardium- which causes constriction to the heart Skin - which can take a number of forms, most notably Lupus vulgaris where changes of the facial skin was supposed to give patients a wolf-like appearance
Clinical presentation Clinical presentation is characteristically chronic with pain and swelling being the principal features. Lymph glands of the neck may develop singly or in chains. They become swollen painful and may have a rubbery texture. They may break down to give abscess formation. These may discharge onto the skin giving a very unsightly combination of swelling a pus around the neck. Bony disease causes pain and swelling of the affected part. Spinal disease may cause paraplegia if enough of the vertebrae are destroyed to cause instability of the spine. Abdominal disease characteristically causes pain and constipation. If advanced it may cause complete obstruction of the bowel. Tuberculous meningitis (TBM) Tuberculous meningitis (TBM) may cause a wide variety of symptoms. A single cranial nerve may be affected resulting in double vision. There may be mental confusion developing over days or weeks. If not detected and treated coma may develop. If treated soon enough recovery may be complete but long term sequelae are likely if the treatment is delayed. TBM has the highest mortality of all complications of tuberculosis. Diagnosis The diagnosis at any site should be confirmed by obtaining specimens for bacteriology wherever possible. This means that fluid aspirated or biopsies taken should be placed in a medium such as saline which will not kill the bacteria. Too often still biopsy specimens are placed in formalin so that bacteriological confirmation including sensitivity testing cannot be done. Treatment Treatment is as for pulmonary disease with isoniazid, rifampicin, pyrazinamide and ethambutol for two months followed by isoniazid and rifampicin for four months, except for CNS disease when treatment should be continued for a full year. Steroids may be used in pericardial and meningeal disease. Surgery is usually unnecessary especially where lymph glands and abscess are pesent as long term discharging sinuses may result. Surgery is sometimes necessary in spinal TB where there is instability and may be needed to overcome strictures in GU or GI disease. Occasionally pericardectomy may be required when pericardial disease causes tamponade. It is surprising how the most destructive lesion can be healed with drug treatment alone.
Tuberculosis in Special Populations Tuberculosis in children has not been given much attention until 1993 when the World Health Organization recognized the burden of tuberculosis in children. Most cases in children are due to the spread of tuberculosis from sputum positive adults. In industrialized countries, the frequency of tuberculosis will be less than 10 per 100,000 population, though in slum dwellers, this may rise to 60/100,000. In the Philippines, a prevalence study in a rural community involving 240 children showed that 52.1% who got exposed to sputum positive adults and only 43.1% with exposure to adults with PTB based on positive chest x-ray findings, were positive purified protein derivative (PPD) reactors.1 1 Tanchuan GA, Tanchuan N, Bautista MS. A prevalence study of tuberculosis infection among children who are contacts of adults diagnosed to have pulmonary tuberculosis in rural communities. UERMMMC Journal of Health Sciences 1998; 3 (2): 48-54. History of Tuberculosis Control in the Philippines (1910-1950) 1910: Mortality rate due to Tuberculosis was 487 per 100,000 The Philippine Islands Anti-Tuberculosis Society (now known as the Philippine Tuberculosis Society Inc or PTSI) was founded on July 29,1910 by Governor Cameron Forbes. Mrs Eleanor Franklin Egan was its first President and Honorable Sergio Osmea was its first Vice-President 1911: San Jan del Monte Sanitarium was opened with 14 nipa hut cottages to admit TB cases 1918: Santol Sanitarium opened. Treatment consisted of fresh air, sunshine, nutritious food, bed rest and isolation Radiologic services began with fluoroscopy as initial test for case finding 1932: Mortality rate due to TB was 223.85 per 100,000 1932: TB Commission was created (Act No. 3743) 1933: Powers and duties of TB Commission transferred to Bureau of Health 1934: Sweepstakes Law (RA 4130) established the Philippine Charity Sweepstakes Office (PCSO) to fund Societys operations 1938: Santol Sanatorium was renamed as Quezon Institute The name of society was changed to Philippine Tuberculosis Society Inc, PTSI. 1944: Streptomycin (SM) was first used as part of the treatment for TB 1947: Mainstays of TB treatment were pneumotherapy, thoracoplasty and prolonged hospitalization 1948: Quezon Institute was rehabilitated after WWII 1949: First case of pneumonectomy in a far-advanced case
You might also like
- Nursing Care Related To Psychological and Physiologic Changes of PregnancyDocument6 pagesNursing Care Related To Psychological and Physiologic Changes of PregnancyKristineeeNo ratings yet
- The Child With Hematologic DisordersDocument149 pagesThe Child With Hematologic DisordersNics FranciscoNo ratings yet
- Signs of LaborDocument5 pagesSigns of Labormarianne_07No ratings yet
- MECONIUM Aspiration SyndromeDocument37 pagesMECONIUM Aspiration SyndromekamalaNo ratings yet
- Abortion BSN 0PR-2: Case Study of BelleDocument27 pagesAbortion BSN 0PR-2: Case Study of BellekervinNo ratings yet
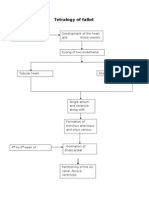
- Tetralogy of FallotDocument3 pagesTetralogy of FallotJohn Mark PocsidioNo ratings yet
- Pregnancy Discomforts/ Minor Disorders of Pregnancy:: Nausea and VomitingDocument5 pagesPregnancy Discomforts/ Minor Disorders of Pregnancy:: Nausea and VomitingNatalie Pemberton100% (1)
- Pre-eclampsia Case ScenarioDocument6 pagesPre-eclampsia Case Scenariogwyne laguardiaNo ratings yet
- PHYSIOLOGICAL CHANGES DURING PREGNANCY1may 20222Document12 pagesPHYSIOLOGICAL CHANGES DURING PREGNANCY1may 20222Pragati BholeNo ratings yet
- Benefits of BreastfeedingDocument20 pagesBenefits of BreastfeedingIan FordeNo ratings yet
- CMCA LEC 12-IntrapartumDocument189 pagesCMCA LEC 12-IntrapartumCarl Josef C. GarciaNo ratings yet
- Assessment of A Pregnant FamilyDocument4 pagesAssessment of A Pregnant FamilyLuna Sang-anNo ratings yet
- (MIOMIO) ALL Types of Position (Breastfeeding)Document12 pages(MIOMIO) ALL Types of Position (Breastfeeding)Juliet Marie MiomioNo ratings yet
- TSU Nursing Case Analysis PneumoniaDocument4 pagesTSU Nursing Case Analysis PneumoniaKrisianne Mae Lorenzo FranciscoNo ratings yet
- Prevalence of Protein Energy Malnutrition Among UnderDocument6 pagesPrevalence of Protein Energy Malnutrition Among UnderagungNo ratings yet
- High Risk NewbornDocument4 pagesHigh Risk NewbornHanna AligatoNo ratings yet
- Nursing Care of Postpartal Family PRINTABLE NOTESDocument4 pagesNursing Care of Postpartal Family PRINTABLE NOTESLyndee May CarnacerNo ratings yet
- History of Nursing Informatics in The PHDocument15 pagesHistory of Nursing Informatics in The PHSMNo ratings yet
- Family Coping Index..Document3 pagesFamily Coping Index..Lharra Cagulada-PostranoNo ratings yet
- Hydrocephalus NCP - DayanghirangDocument2 pagesHydrocephalus NCP - DayanghirangEdnar DayanghirangNo ratings yet
- PrematurityDocument37 pagesPrematurityNishaThakuriNo ratings yet
- 6-Health Problems Common in PreschoolerDocument36 pages6-Health Problems Common in PreschoolerPam Lala100% (2)
- Assessing Neonate Vitals, Growth, ReflexesDocument16 pagesAssessing Neonate Vitals, Growth, ReflexeslouradelNo ratings yet
- Pneumonia in Children: Symptoms, Causes, TreatmentDocument4 pagesPneumonia in Children: Symptoms, Causes, TreatmentkuterinbatNo ratings yet
- Gastrointestinal DrugsDocument45 pagesGastrointestinal DrugsCindy MaslagNo ratings yet
- Treating Pneumonia in Children Under 5Document38 pagesTreating Pneumonia in Children Under 5Arjumand AliNo ratings yet
- ProcreationDocument55 pagesProcreationRoshin TejeroNo ratings yet
- AbortionDocument2 pagesAbortionIden ParfanNo ratings yet
- Breast FeedingDocument11 pagesBreast FeedingJoana Marie GuanNo ratings yet
- Mechanism of LaborDocument2 pagesMechanism of Laborgerold m chuaNo ratings yet
- Aklan State University Nursing Readings on Pyloric StenosisDocument5 pagesAklan State University Nursing Readings on Pyloric Stenosisensoooooooooo100% (1)
- Pathologic Jaundice: A Case Analysis OnDocument22 pagesPathologic Jaundice: A Case Analysis Onfrozen loombandsNo ratings yet
- Infants Diabetic MothersDocument17 pagesInfants Diabetic MothersJaya PrabhaNo ratings yet
- Case Study - Incomplete Abortion Related To APSDocument8 pagesCase Study - Incomplete Abortion Related To APSRomeo ReyesNo ratings yet
- Nursing Care of a Toddler and FamilyDocument6 pagesNursing Care of a Toddler and FamilyIan Mendez100% (1)
- Newborn Physical Assessment by Ms. Mevelle L. AsuncionDocument91 pagesNewborn Physical Assessment by Ms. Mevelle L. AsuncionRizzamwah CatagueNo ratings yet
- Neonatal Respiratory Distress SyndromenhschoicesDocument6 pagesNeonatal Respiratory Distress SyndromenhschoicessehatkanNo ratings yet
- Hyperemesis Gravidarum Case StudyDocument7 pagesHyperemesis Gravidarum Case StudyJose Carmelo JaramillaNo ratings yet
- Intervention of Plan Nursing Intervention Method of Nurse-Family Contact Resources RequiredDocument4 pagesIntervention of Plan Nursing Intervention Method of Nurse-Family Contact Resources RequiredteuuuuNo ratings yet
- High Risk PregnancyDocument6 pagesHigh Risk PregnancyIyah Nicole100% (1)
- Meconium Aspiration Syndrome: Causes, Symptoms and TreatmentDocument13 pagesMeconium Aspiration Syndrome: Causes, Symptoms and TreatmentSANANo ratings yet
- Report - For MaamDocument7 pagesReport - For MaamSherchen Antonio-CortesNo ratings yet
- Febrile SeizuresDocument4 pagesFebrile Seizuresmgonzalez_29No ratings yet
- Myoma Final Power PointDocument45 pagesMyoma Final Power Pointicesexy100% (1)
- Hirschsprung's DiseaseDocument3 pagesHirschsprung's DiseaserjalavazoNo ratings yet
- Nursing Care of A Postpartal Woman and FamilyDocument44 pagesNursing Care of A Postpartal Woman and FamilyEvelyn Medina100% (1)
- Placenta Abruptio - Topic OverviewDocument8 pagesPlacenta Abruptio - Topic OverviewLei AbellarNo ratings yet
- Breast Feeding Teaching PlanDocument2 pagesBreast Feeding Teaching Planapi-355719147No ratings yet
- CroupDocument20 pagesCroupFariezuan HamidNo ratings yet
- Newborn Care EssentialsDocument3 pagesNewborn Care EssentialsShiela Joy DuquezNo ratings yet
- Assisting: Venous Cut DownDocument4 pagesAssisting: Venous Cut DownJimnah Rhodrick BontilaoNo ratings yet
- Shoulder Dystocia: Case AnalysisDocument16 pagesShoulder Dystocia: Case AnalysisKurt Rovic Matza100% (1)
- Drug Study CHN 2Document6 pagesDrug Study CHN 2Raymond Christopher LimNo ratings yet
- Active Management of Normal LabourDocument16 pagesActive Management of Normal LabourjincyneeleshNo ratings yet
- Case Study PTBDocument3 pagesCase Study PTBApril Imperial Tordecillas100% (1)
- Learning Objective Content Teaching Strategy Time Alloted EvaluationDocument3 pagesLearning Objective Content Teaching Strategy Time Alloted EvaluationAmera DimatingcalNo ratings yet
- Hiatal HerniaDocument6 pagesHiatal HerniaElaine Jean UayanNo ratings yet
- The Expanded Program On ImmunizationDocument4 pagesThe Expanded Program On Immunizationapi-3745792100% (3)
- EndometriosisDocument6 pagesEndometriosissalamredNo ratings yet
- Philippine Initiatives in Health InformaticsDocument52 pagesPhilippine Initiatives in Health InformaticsMary Cruz100% (4)
- Peri-Op Nsg.Document73 pagesPeri-Op Nsg.Mary CruzNo ratings yet
- Using Educ Media Effectively (Part 3 of 3)Document10 pagesUsing Educ Media Effectively (Part 3 of 3)Mary CruzNo ratings yet
- Group 8 Manuscript Print (UTI)Document17 pagesGroup 8 Manuscript Print (UTI)Mary CruzNo ratings yet
- Using Educ Media Effectively (Part 1 of 3)Document9 pagesUsing Educ Media Effectively (Part 1 of 3)Mary CruzNo ratings yet
- Using Educ Media Effectively (Part 2 of 3)Document5 pagesUsing Educ Media Effectively (Part 2 of 3)Mary CruzNo ratings yet
- Power Point Presentations Tips (Informatics)Document21 pagesPower Point Presentations Tips (Informatics)Mary CruzNo ratings yet
- Still Birth Case Presentation by BSN2BDocument152 pagesStill Birth Case Presentation by BSN2BMary Cruz60% (5)
- Anatomy and Physiology - Respiratory Mary)Document1 pageAnatomy and Physiology - Respiratory Mary)Mary CruzNo ratings yet
- IntroductionDocument4 pagesIntroductionMary CruzNo ratings yet
- Medical ManagementDocument5 pagesMedical ManagementMary CruzNo ratings yet
- Pathophysiology of Tuberculosis (Edited)Document2 pagesPathophysiology of Tuberculosis (Edited)사이맄 진No ratings yet
- CBC FinalDocument3 pagesCBC FinalMary CruzNo ratings yet
- Introduction 2Document5 pagesIntroduction 2Mary CruzNo ratings yet
- UrinalysisDocument1 pageUrinalysisMary CruzNo ratings yet
- UrinalysisDocument1 pageUrinalysisMary CruzNo ratings yet
- Acute Glomerulonephritis GCDocument70 pagesAcute Glomerulonephritis GCMary Cruz100% (2)
- Medications For Primary ComplexDocument8 pagesMedications For Primary ComplexMary CruzNo ratings yet
- PTB (Mark) CBCDocument3 pagesPTB (Mark) CBCMary CruzNo ratings yet
- NCP 2Document1 pageNCP 2Mary CruzNo ratings yet
- Name: J.A.S Age:1yr Old Medical Diagnosis: Primary Complex Pulmonary Tuberculosi Short Term Goal: Long Term GoalDocument1 pageName: J.A.S Age:1yr Old Medical Diagnosis: Primary Complex Pulmonary Tuberculosi Short Term Goal: Long Term GoalMary Cruz100% (1)
- Intro To Pharmacology Study GuideDocument93 pagesIntro To Pharmacology Study GuideMichelle Morgan LongstrethNo ratings yet
- Importance of avoiding eight factors during and after Panchakarma therapyDocument2 pagesImportance of avoiding eight factors during and after Panchakarma therapy21 RakshitNo ratings yet
- Cyanide PoisoningDocument5 pagesCyanide Poisoningriz04_fortitudessa5178No ratings yet
- Chiba 2018Document9 pagesChiba 2018Fred MeyerNo ratings yet
- Yakima Co (WA) Protocols 2010Document117 pagesYakima Co (WA) Protocols 2010Anthony James-Hartwell100% (1)
- Kidney Stones, UTI, Bladder Control: Causes, Symptoms, Prevention/TITLEDocument24 pagesKidney Stones, UTI, Bladder Control: Causes, Symptoms, Prevention/TITLEIsabella Alycia Lomibao100% (1)
- HNS 107Document95 pagesHNS 107claudette1882No ratings yet
- Crushing and Liquid ARV FormulationsDocument18 pagesCrushing and Liquid ARV FormulationsKumar BhaiNo ratings yet
- Jurnal SyringomaDocument16 pagesJurnal SyringomaNajibah Zulfa Assa'diyahNo ratings yet
- Zirconia ImplantsDocument15 pagesZirconia ImplantsmusatiiNo ratings yet
- Core StiffnessMcGill 2015Document12 pagesCore StiffnessMcGill 2015Hugo TintiNo ratings yet
- Bladder Infection Nursing CareDocument8 pagesBladder Infection Nursing CareJoseph Anthony Benitez VerzosaNo ratings yet
- Enviro-Flo, Inc. Enviro-Chlor Tablet Chlorinator: Installation & Owner'S ManualDocument7 pagesEnviro-Flo, Inc. Enviro-Chlor Tablet Chlorinator: Installation & Owner'S ManualSteve DennisNo ratings yet
- Outpatient Medicine Reimbursement Form - 002 PJVDocument4 pagesOutpatient Medicine Reimbursement Form - 002 PJVPJ ValenciaNo ratings yet
- BDD Module 2 - Maintenance2 PDFDocument14 pagesBDD Module 2 - Maintenance2 PDFHemant KumarNo ratings yet
- Preventing Illness and Living With Ill HealthDocument11 pagesPreventing Illness and Living With Ill HealthMonique MavronicolasNo ratings yet
- Trauma FocusedCognitive BehavioralTherapy (TF CBT)Document2 pagesTrauma FocusedCognitive BehavioralTherapy (TF CBT)Joel RamosNo ratings yet
- Heaven & Earth Spa Treatments Under 40Document2 pagesHeaven & Earth Spa Treatments Under 40Janhavi SoniNo ratings yet
- Jung's Collected WorksDocument6 pagesJung's Collected WorkskarinadapariaNo ratings yet
- Pentagon Reviewer Med SurgDocument31 pagesPentagon Reviewer Med SurgKathy Real VillsNo ratings yet
- Betamethasone (Drug Study)Document4 pagesBetamethasone (Drug Study)Franz.thenurse6888100% (1)
- Oxygen InsuffiencyDocument21 pagesOxygen InsuffiencyAntony Raj Culandai Swamy100% (1)
- Prepare Sponge and CakesDocument30 pagesPrepare Sponge and Cakesmarilyn rosilNo ratings yet
- Complete Urinalysis: A. Physical Characteristics of UrineDocument8 pagesComplete Urinalysis: A. Physical Characteristics of UrineKryza Dale Bunado BaticanNo ratings yet
- MCQsDocument25 pagesMCQsdrstraoNo ratings yet
- First Aid Box ChecklistDocument6 pagesFirst Aid Box ChecklistAbel Angel AblangNo ratings yet
- Drug Interactions in Psychiatry, 3rdDocument454 pagesDrug Interactions in Psychiatry, 3rdKhaled AbdelNaserNo ratings yet
- Best Personality Development Course Navi MumbaiDocument2 pagesBest Personality Development Course Navi MumbaiGurpreet SinghNo ratings yet
- Tetracycline HCl study drugDocument4 pagesTetracycline HCl study drugCheezy BreadNo ratings yet
- DentistryDocument16 pagesDentistryMeka Syahputra56% (9)