Professional Documents
Culture Documents
CTO Retrograde Technique
Uploaded by
Niranjan ReddyOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
CTO Retrograde Technique
Uploaded by
Niranjan ReddyCopyright:
Available Formats
JACC: CARDIOVASCULAR INTERVENTIONS 2012 BY THE AMERICAN COLLEGE OF CARDIOLOGY FOUNDATION PUBLISHED BY ELSEVIER INC.
VOL. 5, NO. 1, 2012 ISSN 1936-8798/$36.00 DOI: 10.1016/j.jcin.2011.10.011
STATE-OF-THE-ART PAPER
The Retrograde Technique for Recanalization of Chronic Total Occlusions
A Step-by-Step Approach
Dominique Joyal, MD,* Craig A. Thompson, MD, J. Aaron Grantham, MD, Christopher E. H. Buller, MD, Stphane Rinfret, MD, SM Montreal and Quebec City, Quebec, and Toronto, Ontario, Canada; New Haven, Connecticut; and Kansas City, Missouri
Chronic total occlusion recanalization still represents the nal frontier in percutaneous coronary intervention. Retrograde chronic total occlusion recanalization has recently become an essential complement to the classical antegrade approach. In experienced hands, the retrograde technique currently has a high success rate with a low complication prole, despite frequent utilization in the most anatomically and clinically complex patients. Since its initial description, important changes have occurred that make the technique faster and more successful. We propose a step-by-step approach of the technique as practiced at experienced centers in North America. Because the technique can vary substantially, we describe the different alternatives to each step and offer what we perceived to be the most efcient techniques. (J Am Coll Cardiol Intv 2012;5:111) 2012 by the American College of Cardiology Foundation
In addition to angina relief, chronic total occlusion (CTO) recanalization may provide additional benets, including avoidance of bypass surgery and enhanced survival (1). To achieve such clinical benets, the procedure has to be technically successful, and complications must be avoided. Historically, success rates have been limited to 60% to 70% with the antegrade approach (1). Knowledge and expertise in the retrograde techniques have become an essential adjunct for CTO operators to improve success. Using collateral channels (CCs)
From the *Jewish General Hospital, McGill University, Montreal, Quebec, Canada; Institut Universitaire de Cardiologie et de Pneumologie de Qubec, (Quebec Heart and Lung Institute), Laval University, Quebec City, Quebec, Canada; St-Michaels Hospital, Toronto, Ontario, Canada; Yale University School of Medicine, New Haven, Connecticut; and the Saint Luke Hospital, Kansas City, Missouri. All authors reported having received honorariums from Abbott Vascular (which distributes Asahi products in North America) for teaching or proctorship of CTO PCI. Drs. Rinfret and Thompson have received honorariums from Terumo for past lectures. None of these relationships are felt to be conicted with the content of this article. Manuscript received July 25, 2011; revised manuscript received October 3, 2011, accepted October 14, 2011.
to reach the distal end of the occlusion subsequently allows for the use of combined antegrade and retrograde subintimal tracking techniques to connect the dots from both ends of the occluded segment when conventional antegrade wire crossing is ineffective, unsafe, or inefcient. Retrograde CTO percutaneous coronary intervention (PCI) was rst mastered by Japanese operators (2,3), which opened new perspectives through the use of small CCs. The technique has evolved rapidly, resulting in shortened procedural time and reduced radiation, compared with the early days (4). Important modications of the retrograde technique have occurred since earlier descriptions, notably the advent of the channel dilator (Corsair, Asahi Intecc, Nagoya, Japan) that substantially streamlines the procedure and has modied the crossing techniques (5). The purpose of this review is to summarize and provide a contemporary, updated step-by-step guide for operators wishing to embark on retrograde recanalization of CTO. For the purpose of this review, only supporting equipment available in North America will be discussed.
Joyal et al. Retrograde Recanalization of CTO
JACC: CARDIOVASCULAR INTERVENTIONS, VOL. 5, NO. 1, 2012 JANUARY 2012:111
This paper absolutely cannot replace proper proctorship through live exchanges and in-laboratory work. Therefore, we discourage embarking on these complex procedures without proper training and proctorship. However, we hope that this paper serves to demystify and clarify some of the complex steps of the procedure. Step 1: Angiographic Film and CC Analysis Careful analysis of the diagnostic lms and review of the indications are crucial before considering the technique. Lesion length is important to estimate, although it is much less of a negative predictor of success than in the classic antegrade approach. Even when robust ipsilateral CCs are present, better imaging is obtained with dual injections. Even weak contralateral support can be competitive with the ipsilateral CCs, and thereAbbreviations fore optimal angiography is and Acronyms only obtained with complete lling of the distal collateral CART controlled bed from all feeding sources. antegrade and retrograde subintimal tracking Sufcient injection ow and CC collateral channel several view angles are crucial for better understanding of colCTO chronic total occlusion lateral sourcing and maximizing IVUS intravascular visualization. Lower magnicaultrasound tion and avoiding panning conLAD left anterior siderably helps in evaluating descending coronary artery CCs, as CC lling will invariLCX left circumex ably occur in a dissimilar time PCI percutaneous frame from the epicardial vescoronary intervention sels. It is often the circumstance PDA posterior descending that a single frame or 2 in an artery entire series of angiograms will PL posterolateral relay the appropriate informaRAO right anterior oblique tion to determine therapeutic strategy. Other critical informaRCA right coronary artery tion gained from the diagnostic angiograms are the distal vessel size, estimated amount of myocardium jeopardized, lesion calcication, side branches and morphology of the proximal cap and distal end of the CTO, and presence or absence of ambiguity in the course of the vessel within its occluded segment. Frequently, the distal vessel from the CTO is either underlled or hypoplastic from lack of ow, but will have an apparent large lumen gain acutely post PCI and/or positive remodeling through intermediate follow-up. The distal end of the occlusion, submitted to lower collateral ow pressure, is often more favorable in terms of shape (tapered entry from retrograde direction) and softer (more easily penetrated with guidewires) than the proximal cap, submitted to systemic diastolic blood pressure. Therefore, when several classical risk factors for antegrade failure, such as blunt cap, long occlusion, severe calcications, tortuosity, and side branches at cap
level, are present, the retrograde approach becomes benecial to increase success. Such classical risk factors are not independent predictors of failure in the retrograde era (6). Analysis of the potential donor artery is also important in terms of size and extent of atherosclerosis. Analysis of all potential CCs is critical. There are 2 types of CCs: septal and epicardial CCs. Septal CCs are the safest and should be the default choice whenever possible. One must pay attention to the course of the CC from its origin to the distal connection. Severe septal tortuosity is a severe limitation to wire advancement, whereas size is less so. It has been learned that straight, faintly visible or even invisible septal CCs can often be crossed, especially with surng with the guidewire, as described later. From the right anterior oblique (RAO) cranial view, the classic septal CC connecting the left anterior descending coronary artery (LAD) to the posterior descending artery (PDA) has a classic b-shape distal turn near its connection (Fig. 1). This
Figure 1. Favorable LAD to PDA Septal Collateral Before (A) and after (B) wire passage. Please note the b-shape turn of the wire, when looking from the RAO cranial view. LAD left anterior descending coronary artery; PDA posterior descending artery; RAO right anterior oblique.
JACC: CARDIOVASCULAR INTERVENTIONS, VOL. 5, NO. 1, 2012 JANUARY 2012:111
Joyal et al. Retrograde Recanalization of CTO
course should be looked for when advancing the wire. The RAO cranial view may, however, overestimate the turn. A straight RAO or an RAO caudal view is helpful to obtain the perpendicular view of the distal turn. In general, the less tortuous septal CC that seems to connect should be considered as a rst candidate. Epicardial CC assessment includes length, tortuosity, and size. In general and as opposed to septal CCs, the main criteria for epicardial CCs is adequate size and not extent of tortuosity. Epicardial CCs are almost always tortuous; this is not a contraindication, especially in the Corsair era. Epicardial CCs are longer than septal CCs in general, and this needs to be taken into account before selecting the proper guide catheter equipment. As epicardial rupture is more serious than septal rupture, and because epicardial use may be associated with procedural ischemia, these CCs should be used only if no septal CCs are suitable. One exception is the use of epicardial CCs in patients who had previous coronary bypass artery grafts (CABG) surgery; because of the lack of pericardial space and the presence of a very strong and adherent pericardium, epicardial CCs can be used more safely, as perforation is extremely unlikely to cause tamponade in these patients. Traditional epicardial CCs are between the right ventricular branch and LAD, between the distal LAD and PDA, and between diagonal branches and LAD. Posterolateral (PL) CCs, a type of epicardial CC, may be located on the PL left ventricular wall (connection between the distal left circumex coronary artery and PL branch of the right coronary artery [RCA]). We use the Werner classication of CC (7). This classication is germane to stratication of retrograde techniques as well as overall evaluation for CTO PCI with prediction for ischemia (and subsequent ischemia reduction) based on CC size; CC0 being a CC with no visible connection to the recipient artery, CC1 being tiny or faint CC connections, and CC2 being small vessel-like connection. CC0 and tortuous CC vessels have been associated with increased failure, although we believe such small CCs (specically CC0 septal CCs) should not discourage attempts to cross using a gentle surng technique if there is distal lling of the collateral bed. General determinants of successful epicardial CC wiring include epicardial size versus tortuosity (pitch ratio) in which larger, less tortuous CCs are more successful than those that are small with severe tortuosity (Fig. 2). Size appears to be less of a determinant for successful septal CC wiring with the septal surng (trial and error) technique, where greater relative magnitude of branching becomes more of a limiting issue. Step 2: Setting Up the Procedure Dual arterial access is essential with the retrograde technique. Arterial access is generally performed using transfemoral or transradial approaches. A combination of 1 radial
Figure 2. Favorable and Unfavorable Epicardial CCs (A) Favorable LCX to right PL epicardial collateral with minimal tortuosity and adequate size. (B) Unfavorable LAD to RCA epicardial collateral with extreme tortuosity. However, the LCX to PL CC is more favorable. CC collateral channel; LAD left anterior descending coronary artery; LCX left circumex; PL posterolateral; RCA right coronary artery.
and 1 femoral approach can be used to mitigate some of the bleeding risk associated with CTO PCI and allow for more options with antegrade 7-F or 8-F catheters, if needed. The bilateral femoral approach has therefore been advocated by the pioneers, especially in the era of septal balloon dilation. Bilateral transradial approach limits the operator to the use of a smaller 6-F to 7-F catheter but is associated with a much reduced risk of bleeding and better patient comfort (8). It is known that larger catheters can provide more passive support. However, retrograde procedures often lead to deep engagement of the retrograde guide after externalization (described
Joyal et al. Retrograde Recanalization of CTO
JACC: CARDIOVASCULAR INTERVENTIONS, VOL. 5, NO. 1, 2012 JANUARY 2012:111
later), which can be potentially catastrophic with large catheters, especially in the donor artery. Hence, the use of a bilateral femoral or radial approach is a matter of operator preference and experience, and acknowledgment of risks/ benets of both approaches is important. Importantly, we discourage the use of 6-F antegrade catheters in the United States as only 7-F compatible covered stents are available. In Canada, 6-F compatible covered stents allow a safer use of 6-F antegrade catheters. Use of short guide catheters, specically for the retrograde limb, is highly recommended; 90-cm guide catheters (commercially available in 6-, 7-, and 8-F) allow the possibility of externalization of the wire with less concern about equipment length. This is especially crucial if use of an epicardial CC is planned. Regular 100-cm guide catheters can be manually shortened and connected to a 1-F smaller introducer sheath (9). Removing 10 cm is usually sufcient. Shortening catheters manually offers the advantage of using the ideal catheter curve for support after the proper position was conrmed within the patient and reducing inventory needs. Strategies to reduce bleeding are essential especially because we use unfractionated heparin at higher doses than
usual. In this respect, the use of 1 or both radials offers a clear advantage. Because of its reversibility, heparin is the antithrombotic of choice in CTO-PCI. Bivalirudin or glycoprotein IIb/IIIa inhibitors are not recommended, because of concerns in case of perforation. An activated clotting time of 300 to 350 s should be targeted, especially when the retrograde equipment is in place, to reduce the risk of catheter-induced thrombosis. It should be veried every 20 to 30 min. Step 3: Retrograde CC Access and Crossing The selected CC is rst wired proximally with a workhorse wire, shaped to navigate the donor vessel and to access the CC. Currently, the microcatheter of choice is the Corsair catheter (Asahi Intecc). It is an over-the-wire hydrophilic catheter composed of 8 thin wires wound with 2 larger ones that serves as a CC dilator while providing exceptional CC tracking and crossing as well as retrograde guidewire control (Fig. 3). The authors favor the 150-cm version. The maximum outside diameter is 0.93 mm (2.8-F), and its unique tapered-tip entry prole is 0.015 inch. These features make it a channel dilator, which has considerably
Figure 3. Corsair Catheter Reprinted, with permission from Elsevier, from Tsuchikane et al. (5).
JACC: CARDIOVASCULAR INTERVENTIONS, VOL. 5, NO. 1, 2012 JANUARY 2012:111
Joyal et al. Retrograde Recanalization of CTO
simplied CC crossing by virtue of its excellent tip exibility and lubricity. Currently, the Corsair catheter circumvents septal CCs balloon dilation with a small balloon (1.25 to 1.5 mm) in most cases. Hence, after wire access to the selected CC, the Corsair catheter is positioned at the proximal portion of the CC. Once the position is secured, the workhorse wire is exchanged for a polymer-jacketed wire to cross the CC. Appropriate wires are the nontapered polymer-covered guidewires with small distal tip load. We favor the Fielder FC (Asahi Intecc) or the Pilot 50 (Abbott Vascular, Santa Clara, California), although the tapered-tip Fielder XT (Asahi Intecc) can sometimes help to track very tiny CCs. The distal tip of the wire is shaped with the traditional CTO tip shape consisting of a very distal 1-mm 30 to 45 bend. After we have positioned the guidewire at the tip of the Corsair, we proceed with CC surng in the cases of septal CCs. This consists of gently advancing the guidewire and observing the path of least resistance within the septal channels. We look for a smooth passage to the distal artery, with the previously described course (Fig. 1). We often do nonselective CC visualization from guide catheter injection. However, poor distal visualization because of the occlusion of the CC with the Corsair is often encountered. If septal surng fails to access the CTO vessel, we may assess the distal path and microconnections through selective injections from the Corsair catheter positioned in the proximal portion of the septal CC. The downside of selective visualization is the increased risk of septal rupture, which makes the septal CC unusable, and creates a septal hematoma. We thus use selective injection as a last resort after several attempts at surng have failed. Furthermore, it is safest to inject from the LAD to RCA than the reverse as the CCs near the RCA are much smaller and more prone to rupture. CC rupture is seldom problematic, although it ends the chance of crossing the selected CC. In most instances, a persistent stain is noticed that rarely grows when assessing with nonselective injections. We usually pursue the procedure with alternative CCs. When performing septal surng, identication of the wrong path is also assessed by the appearance of wire buckling. We then retract and modify slightly the trajectory. On occasion, the wire appears to op freely distally and this usually indicates entry into a cardiac chamber. Wire advancement into the left or right ventricles is common, as natural communications between coronaries and heart cavities exist. Such events are totally benign as long as the Corsair is not advanced. Alternatively, one can prefer to use, at the very beginning of the retrograde attempt, a microcatheter such as the Terumo FineCross (Terumo, Somerset, New Jersey) or the SuperCross (Vascular Solutions, Minneapolis, Minnesota). Such microcatheter, which has a smaller tip prole on a longer length, allows one to more deeply engage very small septal CCs. Use of the FineCross or SuperCross also avoids
the unnecessary use of the more expensive Corsair in case of retrograde failure, and can be used again from the antegrade side. However, if the polymer-jacketed guidewire crosses through the septal CC, the catheter should be exchanged for the Corsair, which is far more performant in crossing the CC. Once across into the distal recipient artery, the wire classically has a to-and-fro movement implying intravascular position. This to-and-fro movement conrms that the wire can move freely within its path from the donor to the recipient vessel, with heart beats. Proper position will then be conrmed by nonselective retrograde guide injection. The wire is then advanced far enough to provide support for the Corsair catheter advancement. This is performed by 5 to 10 alternating clockwise and counterclockwise rotations while providing forward tension. In the presence of very tortuous or severely angulated CCs, the Corsair catheter may become resistant to rotation. Advancement of the Corsair will be more effective with counterclockwise rotations. Exchange for a new Corsair is required if the Corsair cannot be advanced despite several minutes of rotation in both directions. The Corsair is then advanced and positioned near the distal end of the occlusion. In case of epicardial CC crossing, surng is not performed as the wire is manipulated to follow the path of the channel. Diverging from the observed path potentially leads to perforation, which is far more problematic than septal ruptures. We usually shape the wire with a small distal bend although a more proximal bend can ease crossing tortuous loops. We thus gently advance the guidewire until any resistance is felt. Advancement of the Corsair is made with the same previously described techniques, although it is helpful to advance the Corsair halfway through the collateral path to provide support for better wire crossing to the distal recipient vessel or to modify the shape of the CC for additional wire manipulation. Although currently unavailable in North America, the Sion guidewire (Asahi Intecc) has been increasingly used by Japanese and European operator with high success and low perforation rates. The epicardial CC often loses temporarily its tortuous shape after crossing with the Corsair, which can lead to ischemia. Therefore, we suggest using epicardial CCs as a last resort and when additional CCs are present to prevent ischemia. Step 4: Crossing the CTO The objective is to cross retrograde into the proximal true lumen by taking advantage of the softer or more favorable characteristics of the distal end, whenever possible. We tend to limit our choices to a set of 4 guidewires; Fielder XT, Fielder FC (Asahi Intecc) (or Pilot 50), Pilot 200 (Abbott Vascular), and Conanza Pro 12 (Asahi Intecc). Features of those guidewires, with others, are presented in Table 1. A tapered distal cap can be crossed with Fielder XT, Fielder
Joyal et al. Retrograde Recanalization of CTO
JACC: CARDIOVASCULAR INTERVENTIONS, VOL. 5, NO. 1, 2012 JANUARY 2012:111
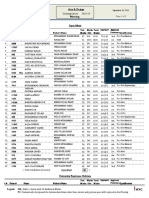
Table 1. Most Commonly Used Guidewires for CTO Recanalization
Guidewires Collateral surng Pilot 50 Fielder FC CTO crossing Fielder XT Pilot 200 Conanza Pro 12 Externalization Pilot 200 (300 cm) Rotablator wire (325 cm) Abbott Vascular Boston Scientic 0.014/0.35 0.009/0.23 shaft 0.014/0.35 tip 0.014/0.35
chronic total occlusions; nr
Manufacturers
Wire Diameter (inch/mm)
Tip Load (g)
Hydrophilicity
Notes
Abbott Vascular Asahi Intecc Corporation
0.014/0.35 0.014/0.35
1.5 1.5
Hydrophilic tip hydrophobic shaft Hydrophilic tip hydrophobic shaft
Collateral surng Collateral surng
Asahi Intecc Corporation Abbott Vascular Asahi Intecc Corporation
0.014/0.33 shaft 0.009/0.23 tip 0.014/0.35 0.014/0.35 shaft 0.009/0.23 tip
0.8 6 12
Hydrophilic tip hydrophobic shaft Hydrophilic tip hydrophilic shaft Hydrophobic tip hydrophilic shaft
Microchannel present; tapered cap; good for small knuckle Microchannel present; tapered cap; progress in plaque; good for powerful knuckle Blunt cap; reverse-CART
6 nr nr
not relevant.
Hydrophilic tip hydrophobic shaft nr nr
Good choice with short guides Less friction but kinkable Longest wire; strongest shaft
ViperWire Advance (330 cm) Cardiovascular System
CART
controlled antegrade and retrograde subintimal tracking; CTO
FC (or Pilot 50), or Pilot 200. Fielder XT and Pilot 200 are felt to be the best suited to progress within the plaque, with or without a knuckle at their tip. However, for rm plaque with an understood CTO trajectory and good target, we prefer the Conanza Pro 12. The Conanza Pro family has the characteristics of hydrophilic coating except for the 1-mm distal tip, which is hydrophobic. The Conanza Pro 12 has a tapered tip of 0.009 inch with 12 g of tip load. We favor initially the approach of positioning our retrograde wire as far as possible within the occlusion (either within the lumen or the subintimal space) with attempts to cross using a rapid wire escalation strategy. We can provide a landmark for the retrograde wiring using an antegrade wire. We generally do not employ kissing or marker wire strategies to meet wires in the lesion with the intent to cross, as the success of these methods is time inefcient. Poor maneuverability of the retrograde wire is one limitation of primary retrograde wire crossing. To overcome this problem, the Corsair catheter should be used as the supporting catheter for the retrograde wire because of its strong backup support. Corsair is frequently advanced into the CTO to improve the wire maneuverability in retrograde vessel tracking. Another important issue is to avoid wire perforation in retrograde vessel tracking. If the retrograde wire escalation strategy technique fails, or if the CTO lesion length is long or its course poorly understood (also called vessel ambiguity), we usually proceed with the knuckle-wire technique (Fig. 4). This entails creating a small loop with the retrograde polymer jacketed (Fielder XT or Pilot 200) wire to dissect the subintimal/subadventitial space, and hence prepare an opportunity to connect the proximal lumen with a distal false lumen within the CTO segment using reverse controlled
antegrade and retrograde subintimal tracking (CART) (10) or standard CART technique (2). The knuckle-wire technique is thus our second approach after unsuccessful pure retrograde crossing and enables a different base of operation for eventual wire crossing. Rotation of a knuckle-wire may cause wire knotting, making it impossible to retrieve. Therefore, knuckled wire should be pushed, never rotated. In many instances, both wires are advanced within the subintimal/subadventitial space but fail to meet in the same plane. The wires are seen as parallel to each other in multiple views. We then proceed with the reverse CART technique. The different variations of the CART technique were developed to connect the antegrade and retrograde subintimal/subadventitial or true lumen spaces. In the classic CART, a balloon (1.25 to 2.5 mm) is positioned in the CTO and inated over the retrograde wire into the retrograde subintimal space, parallel to the antegrade wire. The antegrade wire is manipulated to connect with the enlarged retrograde subintimal space to ultimately exit into the distal true lumen. The classic CART is rarely performed in North America nowadays since the introduction of the Corsair catheter. The reverse CART has the same basic concept as CART. A rapid exchange balloon is inated on the antegrade wire to enlarge the antegrade subintimal/ subadventitial space (Fig. 5). If the balloon cannot reach a plane within the vicinity of the retrograde Corsair, a Tornus (Asahi Intecc) catheter can be used to enlarge the track to subsequently deliver the antegrade balloons, for reverse CART. The retrograde wire is then manipulated to enter the enlarged antegrade space. The concept is that 4 fates exist for the wires/catheters in the antegrade and retrograde CTO spaces. 1) Antegrade wire is positioned in a segment that used to be the lumen, as is the retrograde wire.
JACC: CARDIOVASCULAR INTERVENTIONS, VOL. 5, NO. 1, 2012 JANUARY 2012:111
Joyal et al. Retrograde Recanalization of CTO
Objective is either to advance the retrograde or the antegrade wire, using the other wire as a landmark (kissing wire). Alternatively, antegrade dilation can be performed to increase the chance of connecting the two wires. If such a strategy fails, intentionally penetrating the subintimal/ subadventitial plane either from the retrograde or the antegrade side increases success. 2) Both antegrade and retrograde systems reside within the circumferential subintimal/subadventitial plane, and therefore will easily be connected when the space is enlarged. This is an ideal
Figure 5. Reverse-CART Technique (A) A balloon is inated on the antegrade wire within the subintimal/subadventitial space. A retrograde wire, supported by the Corsair catheter, is aimed at the space created. (B) Illustration of the technique. Note the more funnel shape of the distal end of the occlusion as oppose to the more blunt proximal cap. CART controlled antegrade and retrograde subintimal tracking.
Figure 4. Knuckle-Wire Technique (A) A knuckle is created on the retrograde wire with support from the Corsair catheter. (B) Illustration of the technique. Note the position of the wire within the subintimal/subadventitial space, which is expended by the knuckle.
situation. 3) The retrograde system is in the subintimal/ subadventitial plane, and the antegrade one is inside of what used to be the lumen; therefore, a larger layer of tissue resides between the 2 systems. With appropriate antegrade balloon ination, the CTO tissue and vessel wall can be broken up to the subintimal/subadventitial space, for the retrograde wire to engage the space and then the antegrade true lumen. A stiff wire, such as the Conanza Pro 12, is used to re-enter from the retrograde subintimal/ subadventitial space to the true proximal lumen. 4) The antegrade system is in the subintimal/subadventitial space and retrograde is inside of what used to be the lumen. In such a situation, advancing a retrograde knuckled guidewire will likely reach the same subintimal/subadventitial space, which will connect the antegrade and retrograde spaces
Joyal et al. Retrograde Recanalization of CTO
JACC: CARDIOVASCULAR INTERVENTIONS, VOL. 5, NO. 1, 2012 JANUARY 2012:111
when enlarged with antegrade dilation. Experience has taught us that balloons sized within the presumed or intravascular ultrasound (IVUS)-measured adventitial borders can safely be used to open the space, especially when the antegrade wire is perceived to be surrounded by all the vessel wall layers. The width of the antegrade or retrograde knuckle can help to guide the selection of a properly sized balloon. One problem that is often encountered is the immediate recoil of the subintimal space, despite use of large balloons. To counter this, on occasion, we attempt to aim at the antegrade inated balloon with the tip of the retrograde wire. Several alternative techniques have also been described. The Stent reverse CART technique involves deploying a stent within the antegrade dissected plane to create an open target for retrograde crossing. We prefer the use of the GuideLiner mother-in-child catheter (Vascular Solutions, Minneapolis, Minnesota) inserted into the space to help connect the retrograde wire to the antegrade guide. Of note, after antegrade dilation, we avoid as much as possible antegrade injections and rely solely on retrograde visualization. The intent is to avoid propagation of hydraulic dissections, which can signicantly complicate the procedure. To prevent accident, we usually cover the antegrade manifold or unhook the contrast syringe until stents have been deployed. The use of IVUS has been advocated (10). We nd that the most helpful use of IVUS is in determining the size of the artery, location of the antegrade and retrograde systems in the vessel structure, and distance from the wire to the outside wall when performing reverse CART. This ensures proper expansion of the subintimal space and minimizes risk of perforations. However, we believe that reverse CART can be performed in most instances without IVUS guidance, to reduce procedure cost and expedite the technique, particularly when using knuckle-wire techniques that tend to safely remain within the vessel structure.
horse wire into the distal vessels and branches conrms true lumen positioning. In most instances, it is the retrograde wire that crosses into the proximal true lumen. The goal at this point is to orient the retrograde wire into the antegrade guide. Coaxial alignment of the antegrade guide to the ostial segment of the CTO vessel is helpful for wiring the antegrade guide catheter. When possible, we advance the Corsair through the occlusion. Anchoring the tip of the retrograde wire in the antegrade guide with an antegrade balloon (anchoring technique with a 2.5 mm in a 7- or 8-F guide, 2.0 mm in a 6-F guide) can provide sufcient backup for Corsair advancement. If this fails, the Corsair should be exchanged for a long 1.5- or 1.25-mm over-the-wire balloon, which usually has a smaller crossing prole than the Corsair, to perform retrograde CTO dilation. If this step succeeds, antegrade ow can usually be restored, and a wire can be advance to the distal bed from the antegrade guide. At this point, the procedure is converted to an antegrade fashion, and the retrograde equipment can be removed.
Externalization
Step 5: Wiring the Antegrade Guide, Snaring, and Externalization If the occlusion is crossed antegrade, for example after the knuckle wire or a kissing-wire technique, the procedure is performed over the antegrade wire, and the retrograde equipment is removed. Care must be taken to ensure that the distal end of the antegrade wire is in the distal true lumen with contralateral injection. We discourage distal contrast injection through a microcatheter, or an overthe-wire balloon lumen, which can provoke distal dissection. As soon as a microcatheter, an over-the-wire balloon, or an antegrade Tornus catheter has crossed the lesion, the CTO wire should be exchanged for a safer workhorse guidewire. Easy advancement of the work-
If the retrograde guidewire and Corsair enter the antegrade guide catheter, externalization should be the next step. The short retrograde wire used to cross the occlusion is removed, and exchanged for a long wire, advanced through the opposite hemostatic valve with the objective of converting the recanalization procedure to an antegrade fashion. Several workhorse wires come in 300 cm, although we prefer using a 300-cm Pilot 200 guidewire, as the plastic jacket eases progression of the wire within the Corsair and out into the antegrade guide. For extra length, the Rotablator oppy wire (Boston Scientic, Natick, Massachusetts) is 325 cm; however, its shaft is only 0.009 inch in diameter, and easily kinkable. The ViperWire Advance guidewire (Cardiovascular Systems Inc., St Paul, Minnesota) has emerged as an ideal guidewire for externalization. It is 335 cm long, the longest of 0.14-inch wires available, and passes very easily through the Corsair to the antegrade hemostatic valve. With septal CCs, as the wire and the Corsair are subjected to the contraction of the septum myocardium, we advance the wire slowly and notice systolic resistance to the advancement of the wire. Use of the ViperWire substantially shortens this step, because its strong shaft eases pushing the wire across all resistances. After signicant advancement, one can use uoroscopy over the opposite access to visualize wire position. We externalize just enough of the wire (10 to 15 cm) to be able to introduce rapid exchange gear over it. Because the distal tip of the wire comes out of the patients heart and not the reverse, the gear can be advanced or pulled out despite no proximal control of the wire. As the externalized wire brings tension within the coronaries, extreme care should be taken to avoid deep seating (especially when
JACC: CARDIOVASCULAR INTERVENTIONS, VOL. 5, NO. 1, 2012 JANUARY 2012:111
Joyal et al. Retrograde Recanalization of CTO
retrograde gear is pulled) and unintentional advancement of the guide catheters, mostly the retrograde one, which can lead to donor artery dissection. Use of 6-F catheters from the retrograde side likely reduces the risk of donor artery dissection. Moreover, care should be taken not to lose the proximal end of the long guidewire into the Corsair, from the retrograde side; it is wise to leave a torquing device on the wire or a clamp to avoid this. If the retrograde wire is positioned into the aorta, a fast alternative is to exchange the short guidewire for a 300-cm Pilot 200 in order to snare its tip for and snare a long wire. We favor the 3-loop En Snare 18- to 30-mm Endovascular System (Merit Medical Systems, South Jordan, Utah), which works considerably faster than the conventional gooseneck snares. The standard En Snare is 6- and 7-F compatible, as long as its long sheath is not used (Fig. 6). The antegrade guide is pulled back in the aorta above the distal position of the retrograde wire. The wire is rst advanced through one of the 3 loops, and then snared and pulled into the guide, preferably on the soft part of the wire. We then gently reposition the antegrade guide at the ostium of the coronary. As the wire is carefully externalized, backward tension is provided on the retrograde guide catheter as this step promotes deep seating of the guide. Once the tip of the wire is out of the opposite connector, its tip is secured and the folded part cut with surgical scissors. Alternatively, there may be situations where retrograde angioplasty must be performed, especially in the setting of ipsilateral CC crossing when using smaller guiding catheters. This involves removing the Corsair and introducing an over-the-wire or a rapid exchange balloon over the retrograde wire. Because the septal CC has already been dilated by the Corsair, further dilating the channel is usually not required. Once sufcient passage for an antegrade wire has been created by retrograde angioplasty, the procedure is continued in an antegrade fashion. Step 6: Opening the Occlusion We rst withdraw the Corsair to the distal portion of the artery. A rapid exchange balloon is introduced on the distal tip of the retrograde wire, from the antegrade guide. The balloon usually easily crosses the occlusion because the externalized wire provides great support. Care must be taken to never let the tips of the balloon and the Corsair touch each other as they can become entrapped due to dissimilar tip sizes and powerful forces generated working on the same wire. It is also crucial to maintain the Corsair in the CC as long as the retrograde wire is in position. Because the externalized retrograde wire can exert signicant shear stress or tension, especially in a septal CC, the Corsair protects the CC and the septum against being transected, as a cheese cutting effect.
Figure 6. Snaring a Retrograde 300-cm Pilot 200 Wire With a Triple-Loop System (A) Wire enters one loop. (B) The snare is pulled to engage the guidewire into the antegrade guide catheter.
Once the balloon has opened the occlusion, 2 options are available. One is to continue with ballooning and stenting the vessel over the externalized retrograde wire. This provides excellent support for passage of long stents. Alternatively, an antegrade workhorse wire can be advanced through the newly opened vessel. Once proper wire position is conrmed by contralateral injections, the Corsair and its wire are removed. To do so, we reposition the Corsair forward up to the opposite ostium near the antegrade guide. At this point, we slowly pull the retrograde wire back, remove the wire from the Corsair, followed by pulling out
10
Joyal et al. Retrograde Recanalization of CTO
JACC: CARDIOVASCULAR INTERVENTIONS, VOL. 5, NO. 1, 2012 JANUARY 2012:111
Figure 7. Description of Recanalization of a Proximal LAD Occlusion From RCA Septal Collaterals Septal connections are identied (A) followed by septal engagement (B), septal surng (C), engagement of LAD and advancement of Corsair catheter (D), advancement of retrograde wire within distal occlusion (E), crossing of occlusion and advancement of Corsair catheter within antegrade guide catheter (F), positioning of an antegrade balloon after externalization (G), positioning and deployment of stent (H), conrmation of vessel patency before Corsair removal (I), and nal picture (J). Note the inconsequential septal staining from septal surng. Abbreviations as in Figure 2.
the Corsair. As with its insertion, we favor alternating clockwise/anticlockwise rotations of the Corsair until it reaches the retrograde guide catheter (Fig. 7). We have learned not to overtreat distal lesions, particularly small vessels without angiographic atherosclerotic plaque or small dissection. The distal bed disease, which has been chronically underperfused, tends to be overestimated, and the vessel frequently vasodilates and remodels with restoration of antegrade ow. Also, as we position our stents, we use contralateral injections to avoid propagation of antegrade hydraulic dissections. Step 7: Final Pictures Upon removal of the Corsair, we assess for potential CC damage. Contrast staining in the septum is not infrequent and seldom lead to hemodynamic compromise. In the
recent J-CTO registry, the incidence of perforations resulting in cardiac tamponade was only 0.4% (11). Often, distal CCs are less opacied at the end of the procedure; it does not mean dissection or thrombosis but simply less recruitment secondary to restoration of antegrade ow. In addition, we also assess for donor artery patency. Donor artery dissection is very rare and would need to be treated in a standard fashion. The nal assessment from the antegrade injections usually shows distal competitive ow. This gradually disappears at follow-up as CCs are shut down. Conclusions Retrograde recanalization of CTO represents the last frontier in interventional cardiology. We have provided an updated step-by-step approach to demystify the procedure. In a substantial population of patients previously labeled as
JACC: CARDIOVASCULAR INTERVENTIONS, VOL. 5, NO. 1, 2012 JANUARY 2012:111
Joyal et al. Retrograde Recanalization of CTO
11
unrevascularizable, retrograde recanalization of CTO offers a valuable option. It can now be performed, in experienced hands, with a high degree of success, safety, and efciency.
Reprint requests and correspondence: Dr. Stphane Rinfret, Clinical and Interventional Cardiology, Multidisciplinary Cardiology Department, Institut Universitaire de Cardiologie et de Pneumologie de Qubec (Quebec Heart and Lung Institute), 2725, chemin Ste-Foy, Quebec City, Quebec G1V 4G5, Canada. E-mail: stephane.rinfret@criucpq.ulaval.ca.
REFERENCES
1. Joyal D, Alalo J, Rinfret S. Effectiveness of recanalization of chronic total occlusions: a systematic review and meta-analysis. Am Heart J 2010;160:179 87. 2. Surmely JF, Tsuchikane E, Katoh O, et al. New concept for CTO recanalization using controlled antegrade and retrograde subintimal tracking: the CART technique. J Invasive Cardiol 2006;18:334 8. 3. Surmely JF, Katoh O, Tsuchikane E, Nasu K, Suzuki T. Coronary septal collaterals as an access for the retrograde approach in the percutaneous treatment of coronary chronic total occlusions. Catheter Cardiovasc Interv 2007;69:826 32. 4. Thompson CA, Jayne JE, Robb JF, et al. Retrograde techniques and the impact of operator volume on percutaneous intervention for coronary chronic total occlusions an early U.S. experience. J Am Coll Cardiol Intv 2009;2:834 42.
5. Tsuchikane E, Katoh O, Kimura M, Nasu K, Kinoshita Y, Suzuki T. The rst clinical experience with a novel catheter for collateral channel tracking in retrograde approach for chronic coronary total occlusions. J Am Coll Cardiol Intv 2010;3:16571. 6. Rathore S, Katoh O, Matsuo H, et al. Retrograde percutaneous recanalization of chronic total occlusion of the coronary arteries: procedural outcomes and predictors of success in contemporary practice. Circ Cardiovasc Interv 2009;2:124 32. 7. Werner GS, Ferrari M, Heinke S, et al. Angiographic assessment of collateral connections in comparison with invasively determined collateral function in chronic coronary occlusions. Circulation 2003;107: 19727. 8. Rinfret S, Joyal D, Nguyen CM, et al. Retrograde recanalization of chronic total occlusions from the transradial approach; early Canadian experience. Catheter Cardiovasc Interv 2011;78:366 74. 9. Wu EB, Chan WW, Yu CM. Retrograde chronic total occlusion intervention: tips and tricks. Catheter Cardiovasc Interv 2008;72: 806 14. 10. Rathore S, Katoh O, Tuschikane E, Oida A, Suzuki T, Takase S. A novel modication of the retrograde approach for the recanalization of chronic total occlusion of the coronary arteries intravascular ultrasoundguided reverse controlled antegrade and retrograde tracking. J Am Coll Cardiol Intv 2010;3:155 64. 11. Morino Y, Kimura T, Hayashi Y, et al. In-hospital outcomes of contemporary percutaneous coronary intervention in patients with chronic total occlusion insights from the J-CTO Registry (Multicenter CTO Registry in Japan). J Am Coll Cardiol Intv 2010;3:14351.
Key Words: chronic total occlusion coronary interventions.
percutaneous
You might also like
- Parental Alienation, DSM-V, and ICD-11Document113 pagesParental Alienation, DSM-V, and ICD-11Talia Schwartz67% (6)
- Interactive Medical Acupuncture Anatomy. 2016 Narda G. RobinsonDocument1,167 pagesInteractive Medical Acupuncture Anatomy. 2016 Narda G. RobinsonVasily Zabelin100% (7)
- TriageDocument95 pagesTriageEduardo FriasNo ratings yet
- Careers in Biomedical ScienceDocument24 pagesCareers in Biomedical ScienceEncik LaLaNo ratings yet
- Unit 6 Cardiac Catheterization and AngiographyDocument28 pagesUnit 6 Cardiac Catheterization and AngiographyJack Tomar100% (1)
- Guidelines TAVI TAVRDocument15 pagesGuidelines TAVI TAVRRossellaDisalvo100% (1)
- Tavi 150923155743 Lva1 App6892Document157 pagesTavi 150923155743 Lva1 App6892Zhivka KostadinovaNo ratings yet
- Down SyndromeDocument20 pagesDown SyndromeJessa DiñoNo ratings yet
- CV WritingDocument6 pagesCV WritingFatima SiddiquiNo ratings yet
- Mr. Jose Ferdinand M. Rojas Ii: FPCP, FPSMO, Recommended Her To Undergo Chemotherapy For Her Spinal Column WhichDocument3 pagesMr. Jose Ferdinand M. Rojas Ii: FPCP, FPSMO, Recommended Her To Undergo Chemotherapy For Her Spinal Column Whichglenn padernalNo ratings yet
- PhototherapyDocument26 pagesPhototherapyJOSLIN0% (1)
- Pacemaker Timing & IntervalsDocument124 pagesPacemaker Timing & IntervalsNiranjan Reddy100% (1)
- TeleHealth Final ManuscriptDocument127 pagesTeleHealth Final ManuscriptMaxine JeanNo ratings yet
- Letters Combined (11 Referral, 2 Discharge, 1 Transfer)Document49 pagesLetters Combined (11 Referral, 2 Discharge, 1 Transfer)Faisal ImtiazNo ratings yet
- Chn-Jessie DaclisDocument3 pagesChn-Jessie DaclisJasmine JarapNo ratings yet
- PCI or PTCADocument30 pagesPCI or PTCAMelissa KanggrianiNo ratings yet
- Glomus CcarotidasDocument8 pagesGlomus CcarotidasJuan TijerinaNo ratings yet
- Review Article: Computed Tomography in The Evaluation For Transcatheter Aortic Valve Implantation (TAVI)Document13 pagesReview Article: Computed Tomography in The Evaluation For Transcatheter Aortic Valve Implantation (TAVI)Paul SchoenhagenNo ratings yet
- IVL Meta-Analysis 2021 MayDocument10 pagesIVL Meta-Analysis 2021 MayPraveenVeeraNo ratings yet
- De Maria Et Al 2019 Management of Calcific Coronary Artery LesionsDocument14 pagesDe Maria Et Al 2019 Management of Calcific Coronary Artery LesionsVimal NishadNo ratings yet
- CathSap BDocument153 pagesCathSap BSajjad HussainNo ratings yet
- Transcatheter Aortic Valve-In-Stentless Surgical Aortic Valve Insertion: Hype or Hope?Document2 pagesTranscatheter Aortic Valve-In-Stentless Surgical Aortic Valve Insertion: Hype or Hope?a f indra pratamaNo ratings yet
- CTO: Current Technique: Cover StoryDocument6 pagesCTO: Current Technique: Cover Storymoche_raulNo ratings yet
- Core Curriculum Subadventitial Techniques For Chronic Total Occlusion Percutaneous Coronary InterventionDocument10 pagesCore Curriculum Subadventitial Techniques For Chronic Total Occlusion Percutaneous Coronary InterventiongunaoNo ratings yet
- Acs 07 04 463Document7 pagesAcs 07 04 463GuadaNo ratings yet
- Anaortic, Off-Pump Coronary Artery Bypass Using Multiple Arterial Grafts: Surgical TechniqueDocument15 pagesAnaortic, Off-Pump Coronary Artery Bypass Using Multiple Arterial Grafts: Surgical TechniqueWilliam MakdinataNo ratings yet
- Original ArticlesDocument8 pagesOriginal ArticlesHugoNo ratings yet
- Modified Selective Aortic RootDocument7 pagesModified Selective Aortic RootDm LdNo ratings yet
- DCO After TAVRDocument12 pagesDCO After TAVRBogdan BotezanNo ratings yet
- DISRUPT CAD Pooled Analysis - Kereiakes JACC Intv 2021Document12 pagesDISRUPT CAD Pooled Analysis - Kereiakes JACC Intv 2021PraveenVeeraNo ratings yet
- Catheter Ablation of Intramural Outflow Tract Premature Ventricular Complexes - A Multicentre StudyDocument9 pagesCatheter Ablation of Intramural Outflow Tract Premature Ventricular Complexes - A Multicentre Studyahmed mostafaNo ratings yet
- Central Venous Catheter - StatPearls - NCBI BookshelfDocument11 pagesCentral Venous Catheter - StatPearls - NCBI BookshelfsafrinaNo ratings yet
- Clinical and Procedural Impact of Aortic Arch Anatomic Variants in Carotid Stenting ProceduresDocument10 pagesClinical and Procedural Impact of Aortic Arch Anatomic Variants in Carotid Stenting Procedureshud6427No ratings yet
- Subclavian Vein Catheter Extravasation-Insufficient Catheter Length As A Probable Causal FactorDocument7 pagesSubclavian Vein Catheter Extravasation-Insufficient Catheter Length As A Probable Causal Factorwouter PieteraerensNo ratings yet
- Extracorporeal Membrane Oxygenation Bridge To Adult Heart TransplantationDocument6 pagesExtracorporeal Membrane Oxygenation Bridge To Adult Heart TransplantationОлег ПоздняковNo ratings yet
- J Jacc 2020 09 603Document12 pagesJ Jacc 2020 09 603Alejandro Alberto Garcia de la RochaNo ratings yet
- IVUS OCT Guidance of IVL 2020 Mateissi, Mamas Et Al.Document7 pagesIVUS OCT Guidance of IVL 2020 Mateissi, Mamas Et Al.PraveenVeeraNo ratings yet
- OSTIALLESIONS Final PDFDocument25 pagesOSTIALLESIONS Final PDFwasimNo ratings yet
- Chronic Total OcclusionsDocument37 pagesChronic Total OcclusionsValentin CHIONCELNo ratings yet
- Treatment of CLI 2011 PDFDocument17 pagesTreatment of CLI 2011 PDFvas25No ratings yet
- KJP 60 237Document8 pagesKJP 60 237Tri RachmadijantoNo ratings yet
- Mitral Annular CalcificationDocument8 pagesMitral Annular CalcificationJiawei ZhouNo ratings yet
- Endovascular Treatment of Femoropopliteal Arterial Occlusive Disease - Current Techniques and LimitationsDocument10 pagesEndovascular Treatment of Femoropopliteal Arterial Occlusive Disease - Current Techniques and Limitationsafso afsoNo ratings yet
- 489 FullDocument9 pages489 FullHellenaNo ratings yet
- Coronaries PowerpointDocument96 pagesCoronaries PowerpointnrzmcbmprhNo ratings yet
- CANULADocument12 pagesCANULAAlejandro Salazar TorresNo ratings yet
- Pen Surgery For Thoracoabdominal Aortic Aneurysm-Is It Still A Horrible SurgeryDocument11 pagesPen Surgery For Thoracoabdominal Aortic Aneurysm-Is It Still A Horrible SurgeryJonathan Frimpong AnsahNo ratings yet
- Material 1 Primary AngioDocument25 pagesMaterial 1 Primary AngioBeatrice KühnNo ratings yet
- CT Support of Cardiac Structural Interventions: Review ArticleDocument12 pagesCT Support of Cardiac Structural Interventions: Review ArticlefibiaNo ratings yet
- Radial Artery Harvesting in Coronary Artery Bypass Grafting Surgery-Endoscopic or Open Method? A Meta-AnalysisDocument20 pagesRadial Artery Harvesting in Coronary Artery Bypass Grafting Surgery-Endoscopic or Open Method? A Meta-Analysisosve91No ratings yet
- Cit0515 F4 SteinbergDocument5 pagesCit0515 F4 SteinbergNasru llahNo ratings yet
- Acute Stroke AssessmentDocument7 pagesAcute Stroke AssessmentHanh NguyenNo ratings yet
- ANGIOLOGIADocument13 pagesANGIOLOGIAAnnette ChavezNo ratings yet
- JCCR 08 00278Document3 pagesJCCR 08 00278ekafithraNo ratings yet
- Unlicensed-A-V Fistula CareDocument29 pagesUnlicensed-A-V Fistula CareMuhammad HaneefNo ratings yet
- Zhao 2018Document7 pagesZhao 2018Alexandru PusneiNo ratings yet
- Safety and Ef Ficacy of An Endovascular-First Approach To Acute Limb IschemiaDocument9 pagesSafety and Ef Ficacy of An Endovascular-First Approach To Acute Limb IschemiaSisca Dwi AgustinaNo ratings yet
- CTO - The Algorithms Within The Algorithm - Riley2018Document12 pagesCTO - The Algorithms Within The Algorithm - Riley2018Evandro Martins FilhoNo ratings yet
- The Radial Artery For Percutaneous Coronary Procedures or Surgery?Document9 pagesThe Radial Artery For Percutaneous Coronary Procedures or Surgery?Deebanshu GuptaNo ratings yet
- Anatomical Considerations and Emerging StrategiesDocument21 pagesAnatomical Considerations and Emerging StrategiesPatus QuakusNo ratings yet
- Literature Review On Central Venous CatheterDocument4 pagesLiterature Review On Central Venous Catheterafdtsdece100% (1)
- Arterial Trauma During Central Venous Catheter Insertion: Case Series, Review and Proposed AlgorithmDocument8 pagesArterial Trauma During Central Venous Catheter Insertion: Case Series, Review and Proposed AlgorithmJuan Jose Velasquez GutierrezNo ratings yet
- Active Versus Conventional Side Branch Protection Strategy For Coronary Bifurcation LesionsDocument8 pagesActive Versus Conventional Side Branch Protection Strategy For Coronary Bifurcation LesionsLuis Rafael Suárez U.No ratings yet
- Lee Et Al. 2017 Am J Cardiol OA vs. RADocument4 pagesLee Et Al. 2017 Am J Cardiol OA vs. RAPraveenVeeraNo ratings yet
- Peripherally Inserted Central Venous Acces - 2021 - Seminars in Pediatric SurgerDocument8 pagesPeripherally Inserted Central Venous Acces - 2021 - Seminars in Pediatric Surgeralergo.ramirezNo ratings yet
- RCA OstijalnaDocument8 pagesRCA Ostijalnaediz71No ratings yet
- 0068KJR - KJR 20 1546Document8 pages0068KJR - KJR 20 1546Joshua AmenNo ratings yet
- Carotid Artrey DiseaseDocument6 pagesCarotid Artrey DiseaseOnon EssayedNo ratings yet
- Vascular Closure Device in Cardiac Cath Laboratory: A Retrospective Observational StudyDocument5 pagesVascular Closure Device in Cardiac Cath Laboratory: A Retrospective Observational StudypatelNo ratings yet
- Scalamogna Et Al. 2022 - CRM - IsAR-CALC-2 DesignDocument6 pagesScalamogna Et Al. 2022 - CRM - IsAR-CALC-2 DesignPraveenVeeraNo ratings yet
- New Approaches For The Assessment of Vessel Sizes in Quantitative (Cardio-) Vascular X-Ray AnalysisDocument14 pagesNew Approaches For The Assessment of Vessel Sizes in Quantitative (Cardio-) Vascular X-Ray AnalysisIrfan IbrahimNo ratings yet
- Aortic RegurgitationFrom EverandAortic RegurgitationJan VojacekNo ratings yet
- Congenitial Echo ModelDocument1 pageCongenitial Echo ModelNiranjan ReddyNo ratings yet
- QP DNBDocument9 pagesQP DNBNiranjan ReddyNo ratings yet
- 1057Document12 pages1057Niranjan ReddyNo ratings yet
- Trans Catheter Therapies For Mitral and Aortic Valve ReplacementDocument9 pagesTrans Catheter Therapies For Mitral and Aortic Valve ReplacementNiranjan ReddyNo ratings yet
- Echoecho Followup After Valve ReplacementDocument12 pagesEchoecho Followup After Valve ReplacementNiranjan ReddyNo ratings yet
- Usefulness of The Valvuloarterial Impedance To Predict AdverseDocument11 pagesUsefulness of The Valvuloarterial Impedance To Predict AdverseNiranjan ReddyNo ratings yet
- Revison de Proyecto Tunning LatinoamericaDocument13 pagesRevison de Proyecto Tunning LatinoamericaJorge Solar RosselNo ratings yet
- P. Ameldev and P.V. TresamolDocument4 pagesP. Ameldev and P.V. Tresamolelif bayramNo ratings yet
- ESTAVILLO, Karen G. (FEVER UTI, CONSTI)Document4 pagesESTAVILLO, Karen G. (FEVER UTI, CONSTI)Karen EstavilloNo ratings yet
- Varicose Veins Diagnosis and TreatmentDocument7 pagesVaricose Veins Diagnosis and Treatmenthossein kasiriNo ratings yet
- Heart Failure Core MeasuresDocument8 pagesHeart Failure Core MeasuresDocRNNo ratings yet
- The Montreal Definition and Classification of GERDDocument22 pagesThe Montreal Definition and Classification of GERDAndrew WongkarNo ratings yet
- Northwestern Medicine Thinkfirst For KidsDocument2 pagesNorthwestern Medicine Thinkfirst For KidsJimNo ratings yet
- Medicinecomplete Clark Drug and PoisonDocument25 pagesMedicinecomplete Clark Drug and PoisonArménio SantosNo ratings yet
- Explanation 2020 1Document315 pagesExplanation 2020 1Reshma Shaji PnsNo ratings yet
- Exercise Based Cardiac Rehabilitation For Coronary Heart Disease 2021Document266 pagesExercise Based Cardiac Rehabilitation For Coronary Heart Disease 2021Josemi Del Castillo MolinaNo ratings yet
- 2018 Intravenous CannulationDocument37 pages2018 Intravenous CannulationCathy PingoyNo ratings yet
- Primary HyperparathyroidismDocument9 pagesPrimary HyperparathyroidismJamesNo ratings yet
- EpiPen CaseDocument5 pagesEpiPen CaseTanvi RastogiNo ratings yet
- Contoh Pico Terbaru-Blok EndokrinDocument3 pagesContoh Pico Terbaru-Blok EndokrinIndra ArdiansyahNo ratings yet
- Developmental Coordination DisorderDocument3 pagesDevelopmental Coordination DisorderQina Nugroho, pts.100% (1)
- Studi Kasus: Kehamilan Dengan: Dengan Katub Jantung Prostetik Mekanik Dan Penggunaan AntikoagulanDocument10 pagesStudi Kasus: Kehamilan Dengan: Dengan Katub Jantung Prostetik Mekanik Dan Penggunaan AntikoagulanMonyet...No ratings yet
- 282173Document75 pages282173Shirley MoNo ratings yet
- MeritListFinal (2018) 7 PDFDocument71 pagesMeritListFinal (2018) 7 PDFFaisal AmeenNo ratings yet
- AXA - Sales Brochure Qatar - ALL - ENDocument10 pagesAXA - Sales Brochure Qatar - ALL - ENAhmad MuhammadNo ratings yet