Professional Documents
Culture Documents
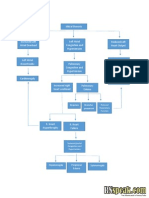
Congestive Heart Failure and Pulmonary Edema Concept Map
Uploaded by
Andrew GodwinOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Congestive Heart Failure and Pulmonary Edema Concept Map
Uploaded by
Andrew GodwinCopyright:
Available Formats
Progression of Illness Positive progression of this disease toward increased functioning and discharge from the hospital includes
the following. Improved symptoms of pulmonary congestion evidenced by lack of dyspnea when weaned from ventilator. Improved pulmonary & extremity edema. Transition from IV to PO fluids. No significant alterations in electrolyte values with special attention paid to creatinine and sodium. No auscultation of crackles and rales in lung fields. Chest x-ray displaying improved ventilation and decrease or absent infiltrates. Patient and family education need have been sufficiently addressed. Echocardiogram displays ejection fraction of at least 40%. Blood pressure is within normal parameters. O2 level greater than 95% on RA or patients norm. Ability to ambulate without exacerbation of symptoms including dyspnea and orthostatis.
Nursing Diagnoses Decreased Cardiac Output Risk for ineffective coping PC: Pulmonary Embolism Risk for infection Ineffective tissue perfusion Acute pain Impaired gas exchange Impaired verbal communication
(Ignatavicius &Workman, 2010; Ackley & Ladwig, 2011).
(Ackley & Ladwig, 2011)
Pathophysiology Heart Failure may present acutely as a result of myocardial ischemia secondary to a MI. The weakened cardiac muscle causes the CO to decrease. The decreasing cardiac output then triggers in increased in systemic vascular resistance and afterload, which only further decreases the CO. Eventually the heart is unable to effectively push against the increased afterload and fluid begins to flow back through the pulmonary veins and fills the lungs. In CHF with acute pulmonary edema this will be the terminal event if the systemic vascular resistance is not promptly reversed. (Ignatavicius &Workman, 2010).
Interventions Continually assess for signs and symptoms of precipitating heart failure. Monitor for signs of bleeding due to anticoagulation and blood thinning therapies. Try to find underlying cause and treat the cause. Monitor ST segment continuously to determine changes in myocardial tissue perfusion. Assess that urine output hourly, alert physician if less than 30 ml/hr. Maintain the patient in the semi-fowlers position to lessen the work of breathing and facilitate venous return. Continuously monitor O2 and assess vital signs.
Congestive Heart Failure and Pulmonary Edema
Medications Loop diuretics such as Lasix should be used to remove excess fluid volume except in the case of severe renal dysfunction. Vasodilators such as nitroglycerin should be used to lower the systemic vascular resistance and therefore decrease the cardiac afterload. Beta-blockers should be used to decrease the preload and afterload placed on the heart. Anticoagulation therapy drugs: coumadin, heparin, lovenox, aspirin. ACE inhibitor regimen should be started because of their effect on slowing even reversing left ventricular remodeling over time. ARDs may be used if ACE inhibitors are not well tolerated.
(Ignatavicius &Workman, 2010; Urden, Stacy, & Lough, 2008)
Signs and Symptoms Fatigue Weakness SOB Distended neck veins Dizziness Decreased exercise tolerance Anxiety Syncope Palpitations Chest pain or discomfort Hypotension Hypertension Pulmonary and extremity edema
Risk Factors Coronary artery disease Male gender History of hypertension, diabetes mellitus, valvular disease, and myocardial infarction. Alcohol, cardiac surgery, kidney conditions, pericarditis, myocarditis, viruses. Congenital heart defects, sleep apnea,
(Ignatavicius &Workman, 2010)
(Ignatavicius & Workman, 2010; Urden et al., 2008)
Treatments The first priority of treatment is airway management. This is judged by the severity of the presenting symptoms. Could include supplemental oxygen via nasal cannula or mask, noninvasive ventilation or in this patients case endotracheal intubation. Urinary catheter should be placed to closely monitor renal function and allow patient to rest. A 12-lead ECG to assess for cardiac abnormalities. IV access to provide prompt medication administration. Frequent vital sign assessments to monitor for a decline in cardiac function.
(Urden et al., 2008)
(Ignatavicius &Workman, 2010; Urden et al., 2008)
You might also like
- RHYTHM CHEAT SHEET: A CONCISE GUIDEDocument1 pageRHYTHM CHEAT SHEET: A CONCISE GUIDEjb cookiesNo ratings yet
- EKG Quick and Dirty - GD v3.0Document2 pagesEKG Quick and Dirty - GD v3.0Sheema Sh100% (1)
- Spotlight On Cardiac DrugsDocument2 pagesSpotlight On Cardiac Drugspauerish100% (2)
- Nursing Diagnosis & Careplan SamplesDocument5 pagesNursing Diagnosis & Careplan SamplesE94% (18)
- Nursing Mnemonics: The Ultimate Tips and Notes For NursesFrom EverandNursing Mnemonics: The Ultimate Tips and Notes For NursesRating: 5 out of 5 stars5/5 (1)
- Digoxin: Andy Samelson's Drug Cards Andy Samelson's Drug CardsDocument57 pagesDigoxin: Andy Samelson's Drug Cards Andy Samelson's Drug Cardssplendidfender76% (17)
- Concept Map HypertensionDocument1 pageConcept Map Hypertensiongeorge pearson0% (1)
- FRACP Cardiology Study Notes Volume 1Document543 pagesFRACP Cardiology Study Notes Volume 1not here 2make friends sorryNo ratings yet
- Shock Comparison ChartDocument2 pagesShock Comparison Chartlinnaete88% (8)
- Drug CardsDocument10 pagesDrug CardsMaria Robustelli100% (3)
- Drug CardsDocument187 pagesDrug Cardsintaaf82% (33)
- Nursing Care Plan For Acute PainDocument5 pagesNursing Care Plan For Acute PainPhilippineNursingDirectory.com100% (9)
- Hypertension Concept MapDocument1 pageHypertension Concept Mapnursing concept maps100% (1)
- Concept Map COPDDocument2 pagesConcept Map COPDJilian McGugan88% (40)
- Dka Case Study Clinical ExampleDocument15 pagesDka Case Study Clinical ExampleVin Lorenzo Campbell100% (2)
- Drug Card LasixDocument2 pagesDrug Card LasixAdrianne Bazo100% (1)
- Nursing Head-to-Toe Assessment Cheat Sheet - Nurseslabs PDFDocument7 pagesNursing Head-to-Toe Assessment Cheat Sheet - Nurseslabs PDFNyeweh Sia Yomba67% (15)
- Nursing Care Plan Mobility SampleDocument6 pagesNursing Care Plan Mobility Samplen2biologyNo ratings yet
- Learning ECGDocument187 pagesLearning ECGPhysiology by Dr Raghuveer100% (2)
- Heart Failure COncept MapDocument2 pagesHeart Failure COncept MapJrBong SemaneroNo ratings yet
- Gerontological Nursing: Scope and Standards of Practice, 2nd EditionFrom EverandGerontological Nursing: Scope and Standards of Practice, 2nd EditionNo ratings yet
- IM SyllabusDocument7 pagesIM Syllabusepah1925100% (1)
- Chronic Kidney Disease: Bobby Laksana D Putri Priela Pembimbing: Dr. Nursamsu, SPPDDocument30 pagesChronic Kidney Disease: Bobby Laksana D Putri Priela Pembimbing: Dr. Nursamsu, SPPDfrostedsurgeonNo ratings yet
- ACS Nursing Care PlanDocument21 pagesACS Nursing Care Planchris_arc90100% (6)
- Ventricular ArrhythmiasDocument33 pagesVentricular ArrhythmiasSamantha DeshapriyaNo ratings yet
- Nursing DiagnosisDocument58 pagesNursing DiagnosisPrecious Santayana100% (3)
- Nursing Concept Map for Diabetes Patient ManagementDocument1 pageNursing Concept Map for Diabetes Patient ManagementSev Kuzmenko0% (1)
- Cirrohsis Case StudyDocument12 pagesCirrohsis Case Studykaitlynne lambertNo ratings yet
- Concept Map of DMDocument2 pagesConcept Map of DMLeslie Marie Rendon100% (9)
- Small Bowel Obstruction System - DisorderDocument1 pageSmall Bowel Obstruction System - DisorderMarina Wasem Netzlaff0% (1)
- Med Surge 2 - RESP SYSTEM NOTESDocument26 pagesMed Surge 2 - RESP SYSTEM NOTESlorrainenxumalo75% (4)
- COPD Care PLAN PDFDocument2 pagesCOPD Care PLAN PDFVanessaMUeller100% (1)
- Cardioversion & Defibrillation ExplainedDocument18 pagesCardioversion & Defibrillation ExplainedJannah Marie A. Dimaporo100% (4)
- Assessment and Management of Patients With Hearing and Balance Disorders WebDocument36 pagesAssessment and Management of Patients With Hearing and Balance Disorders WebStephKirstin Velasco Malapit100% (2)
- Small Bowel Obstruction Care PlanDocument11 pagesSmall Bowel Obstruction Care PlanKatie YarnellNo ratings yet
- PneumoniaDocument1 pagePneumonianursing concept mapsNo ratings yet
- COPD Risk Factors, Signs, Treatments & Nursing CareDocument2 pagesCOPD Risk Factors, Signs, Treatments & Nursing CareJilian McGugan100% (9)
- Lab Normal Value S&Sof S&Sof : Loma Linda University School of Nursing Accepted Lab Values Adapted From KaplanDocument3 pagesLab Normal Value S&Sof S&Sof : Loma Linda University School of Nursing Accepted Lab Values Adapted From KaplanGiacen100% (3)
- Bipolar Concept MapDocument3 pagesBipolar Concept Mapnursing concept maps100% (2)
- Concept Map StrokeDocument1 pageConcept Map StrokeMary GiuntiniNo ratings yet
- STUDENT-Eating - Disorder-F&E-UNFOLDING ReasoningDocument14 pagesSTUDENT-Eating - Disorder-F&E-UNFOLDING ReasoningPeggy100% (12)
- Congestive Heart Failure Schematic DiagramDocument1 pageCongestive Heart Failure Schematic DiagramCyrus De Asis100% (1)
- Hypertension Concept MapDocument1 pageHypertension Concept Mapgfhbgfhgf71% (7)
- Essential Stroke Nursing GuideDocument5 pagesEssential Stroke Nursing GuideAshleigh Johnstone100% (1)
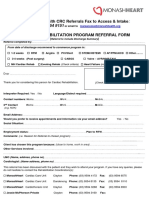
- CRP Referral Form 2016 Monash Heart V5Document1 pageCRP Referral Form 2016 Monash Heart V5Ansari JavedNo ratings yet
- Chronic Renal Failure: PathophysiologyDocument1 pageChronic Renal Failure: PathophysiologyCindy Mae Dela Torre100% (2)
- Concept MapDocument1 pageConcept MapChristine Marie Barce Martinez100% (2)
- Nursing Care Plan For "DYSRHYTHMIAS"Document12 pagesNursing Care Plan For "DYSRHYTHMIAS"jhonroks79% (14)
- ECG Library PDFDocument98 pagesECG Library PDFJayden WaveNo ratings yet
- Hemodialisis KdoqiDocument183 pagesHemodialisis KdoqiMaFer WueRa100% (2)
- Ventricular ArrhytmiaDocument30 pagesVentricular ArrhytmiaIkhsan AmadeaNo ratings yet
- Care Plan For Bowel ResectionDocument4 pagesCare Plan For Bowel Resectionviki840488% (8)
- Colon Cancer Case Study - 64yo Male Diagnosed After Rectal BleedingDocument2 pagesColon Cancer Case Study - 64yo Male Diagnosed After Rectal BleedingDragan Djordjevic100% (4)
- CHF Preparation QuestionsDocument6 pagesCHF Preparation Questionsgenium0689% (9)
- Cellulitis Care PlanDocument6 pagesCellulitis Care PlanNaya Kayala0% (1)
- Peripheral Vascular Disease NursingDocument13 pagesPeripheral Vascular Disease NursingCatlyn Chatpman100% (1)
- Careplan Concept MapDocument1 pageCareplan Concept MapAmanda Simpson100% (3)
- Managing Impaired Gas Exchange in an Elderly COPD PatientDocument23 pagesManaging Impaired Gas Exchange in an Elderly COPD PatientKaren Joyce Costales Magtanong100% (3)
- Concept Map Pleural EffusionDocument1 pageConcept Map Pleural Effusionapi-341263362No ratings yet
- Drugs WorksheetDocument16 pagesDrugs Worksheetninja-2001No ratings yet
- Cellulitis Concept MapDocument3 pagesCellulitis Concept MapBien EstrellaNo ratings yet
- Ricci KeithRN Eating DisorderDocument14 pagesRicci KeithRN Eating DisorderMichelle RicciNo ratings yet
- Intracranial HemorrhageDocument41 pagesIntracranial Hemorrhagedoctormussieaberra100% (1)
- CC-Concept Map 2Document5 pagesCC-Concept Map 2MDCITY50% (2)
- Congestive Heart Failure 1 Concept Map !Document1 pageCongestive Heart Failure 1 Concept Map !Franklin A. Salaum IIINo ratings yet
- TMendoza CriticalCareConceptMap2Document5 pagesTMendoza CriticalCareConceptMap2Theresa Fernandez Mendoza0% (1)
- Diuretic Drugs For Nursing PharmacologyDocument1 pageDiuretic Drugs For Nursing Pharmacologylhayes1234100% (7)
- Pacemakers & AICDs: What You Need to KnowDocument32 pagesPacemakers & AICDs: What You Need to KnowqmmmNo ratings yet
- Jihan Luqmannul Khakim, Dicky Aligheri Wartono, Bagus HerlambangDocument1 pageJihan Luqmannul Khakim, Dicky Aligheri Wartono, Bagus HerlambangazkacantikNo ratings yet
- Cardiac Arrhythmias in Africa: Epidemiology, Management Challenges, and PerspectivesDocument10 pagesCardiac Arrhythmias in Africa: Epidemiology, Management Challenges, and PerspectivesmahsusiyatiNo ratings yet
- Pilipinas: Miss Philippines of Michigan 2008 PageantDocument12 pagesPilipinas: Miss Philippines of Michigan 2008 Pageantstevec74100% (3)
- Acute Coronary Syndrome in Clinical Practice: Firman B. LeksmonoDocument48 pagesAcute Coronary Syndrome in Clinical Practice: Firman B. Leksmonojames klemens phieter phieNo ratings yet
- Etik Dwi Ningsih, Indah Mukarromah, Athi' L Inda YaniDocument9 pagesEtik Dwi Ningsih, Indah Mukarromah, Athi' L Inda YaniMuhamad fajarNo ratings yet
- Nama Nama Yang Tidak Mengumpulkan Soal Ujian Utb 4.1: Akademik Roften CardioDocument8 pagesNama Nama Yang Tidak Mengumpulkan Soal Ujian Utb 4.1: Akademik Roften CardioSyaffira SalsabilaNo ratings yet
- Lifepak CR Plus BrochureDocument20 pagesLifepak CR Plus BrochurenugiexNo ratings yet
- Inter-Rater Reliability of ST-Segment Measurement at A University Hospital in ArgentinaDocument4 pagesInter-Rater Reliability of ST-Segment Measurement at A University Hospital in ArgentinaSholehuddin MunajjidNo ratings yet
- CVS - Charts & DiagramsDocument20 pagesCVS - Charts & DiagramsMamathaNo ratings yet
- 2020 Eagle Practical CardiologyDocument24 pages2020 Eagle Practical CardiologyaeliasgvNo ratings yet
- GlomerulonephritisDocument1 pageGlomerulonephritismaleskunNo ratings yet
- Program SPCCTV 2019 CardiacSurgeryDocument8 pagesProgram SPCCTV 2019 CardiacSurgeryDu SantosNo ratings yet
- Non St-Segment Elevation Acute Coronary Syndrome (Nste-Acs) : EtiologyDocument4 pagesNon St-Segment Elevation Acute Coronary Syndrome (Nste-Acs) : EtiologyKEn PilapilNo ratings yet
- Daftar PustakaDocument9 pagesDaftar PustakaEvan DionesiaNo ratings yet
- Ecg TeachingDocument44 pagesEcg TeachingarvindkanagaratnamNo ratings yet
- Adams-Stokes 1º Sintoma Febre ReumáticaDocument5 pagesAdams-Stokes 1º Sintoma Febre Reumáticacarvalho.tr4270No ratings yet
- Acute Kidney Injury - Mini Lecture: Updated 02/2013Document11 pagesAcute Kidney Injury - Mini Lecture: Updated 02/2013Asmalina AzizanNo ratings yet