Professional Documents
Culture Documents
Nursing Care Plan 5 Altered Nutrition: Less Than Body Requirements
Uploaded by
dbryant0101Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Nursing Care Plan 5 Altered Nutrition: Less Than Body Requirements
Uploaded by
dbryant0101Copyright:
Available Formats
Case Scenario #4
Pediatric Acute Care
INSTRUCTIONS: For this case scenario, you will develop a Nursing Care Plan using SNL, the Standardized
Nursing Languages of NANDA, NOC and NIC (NNN). You will be completing the blank nursing care plan
that you have printed.
Patient is a 10-month old girl admitted to your unit from the PACU following Laparotomy Nissen
procedure and gastrostomy tube placement. She is sleeping comfortably. VS are WNL. IV of D5/.45
w/10 meq KCL is infusing at 20 cc/hr. Patient is NPO. Gastrostomy tube is ordered to low continuous
suction. Meds include Morphine 0.5 mg q 2-3 hrs.
Functional Health Patterns
Nursing assessment data is organized in Functional Health Patterns. Functional Health Patterns can help direct
the choice of Nursing Diagnoses. The eleven functional health patterns are Health Perception-Health Management;
Cognitive-Perceptual; Nutritional-Metabolic; Elimination; Activity-Exercise; Sleep/Rest; Self-Perception/Self-
Concept; Role/Relationship; Sexuality/Reproductive; Coping/Stress/Tolerance; and Value/Belief.
Ø Health Perception/Management:
Former 32 week Premie with history of multiple occurrences of vomiting, respiratory
distress and pneumonia.
Recently diagnosed with GERD (Gastro-esophageal reflux disease).
Home meds include Cisapride, Zantac, Atrovent and Albuterol.
Parents expect that she will be in the hospital for approximately 5 days and will go home on her
prior feedings. They are unsure of the purpose and care of GT.
Ø Role/Relationship:
Parents accompany child to the unit.
Patient lives with parents and two older siblings, ages 3 and 5.
Both parents work, and patient goes to day care 5 days a week. They will be unable to stay with
the patient during her hospitalization.
Ø Nutrition/Metabolic:
Takes 4-5 oz. of Similac with Fe 5x/day plus 2-3 jars of strained food.
She vomits moderate amount soon after eating 2-3 x/day.
Current weight = 5 kg. She has fallen off the growth curve.
Ø Activity/Exercise:
Patient has become less active especially during occurrences of pneumonia.
Ø Cognitive/Perceptual:
Developmental milestones are at approximately a 6-month-old level.
Sits independently but does not crawl or pull self to standing.
Has no problem with hearing or vision.
Has not been connected with Early Intervention Services.
Nutritional/Metabolic
is the most affected functional health pattern for this patient at this period of time.
.
Ped Acute Care40300
Nursing Diagnosis
Appropriate nursing diagnoses (NANDA) for this patient would include:
Altered nutrition: Less than body requirements
Defining Characteristics:
Reported inadequate food intake
Body weight less than normal
Related factors (Etiology):
Inability to digest nutrients.
Recurrent pneumonia
Pain
Defining Characteristics:
FLACC score >5 (Verbal/coded report)
Related factors (Etiology):
Operative procedure
Knowledge deficit
Defining Characteristics:
Verbalizes lack of information about gastrostomy tube.
Related factors (Etiology):
Unavailability of parents to learn care.
While all these nursing diagnoses are appropriate, for purposes of this exercise let’s use:
Altered nutrition: Less than body requirements.
On the nursing care plan form write in the nursing diagnosis, identifying the defining
characteristics and related factors.
Ped Acute Care40300
Nursing Outcomes (NOCs)
• The next step is to select nursing outcomes that can best affect this nursing diagnosis.
• Listed below are two appropriate nursing outcomes for this patient.
Nutritional Status: Food & Fluid Intake
Indicators:
Oral food intake
Tube feeding intake
Oral fluid intake
IV fluid intake
Nutritional Status: Energy
Indicators:
Growth
Tissue healing
Infection resistance
Endurance
Select one of the above listed nursing outcomes for this care plan exercise, go to the
nursing care plan form and check the indicators that you think will best measure your
patient’s progress towards the outcome that you have chosen. You will need to rate your
patient’s current status for each indicator.
Ped Acute Care40300
Nursing Interventions – NIC
Now that you have chosen your outcome for this patient, you will select the interventions
that will best meet this outcome.
• If you have chosen the NOC, Nutritional Status: Food & Fluid Intake, continue below.
• If you have chosen the NOC, Nutritional Status: Energy, continue to that section.
NOC-Nutritional Status: Food and Fluid Intake
The following two Nursing Interventions are appropriate for this patient. Review the activities
listed below each NIC and select 5 that apply. Write these five on the nursing care plan in the
activity column.
NIC: Fluid Management–Activities 3
(,p.348)
• Weigh daily and monitor • Count or weigh diapers as • Maintain accurate intake and output
trends appropriate record
• Monitor hydration status • Monitor for indications of fluid • Monitor laboratory results relevant to
(e.g., moist mucous overload/retention (e.g., fluid retention (e.g., increased specific
membranes, adequacy of crackles, elevate CVP or gravity, increased BUN, decreased
pulses, and orthostatic pulmonary capillary wedge hematocrit, and increased urine
blood pressure), as pressure, edema, neck vein osmolality levels
appropriate distention, and ascites), as
appropriate
• Assess location and extent • Monitor vital signs, as • Insert urinary catheter, if appropriate
of edema, if present appropriate
• Monitor patient’s weight • Monitor hemodynamic status, • Monitor food/fluid ingested and
change before and after including CVP, MAP, PAP, and calculate daily caloric intake, as
dialysis, if appropriate PCWP, if available appropriate
• Administer IV therapy, as • Monitor nutrition status • Give fluids, as appropriate
prescribed
• Administer prescribed • Administer IV fluids at room • Distribute the fluid intake over 24 hr.,
diuretics, as appropriate temperature as appropriate
• Instruct patient on nothing • Administer prescribed • Promote oral intake (e.g., provide a
by mouth (NPO) status, as nasogastric replacement based drinking straw, offer fluids between
appropriate on output, as appropriate meals, and change ice water routinely),
as appropriate
• Encourage significant other • Offer snacks (e.g., frequent • Restrict free water intake in the
to assist patient with drinks and fresh fruits/fruit presence of dilutional hyponatremia
feedings, as appropriate juice), as appropriate with serum Na level below 130 mEq per
liter
• Monitor patient’s response • Consult physician, if signs and • Arrange availability of blood products
to prescribed electrolyte symptoms of fluid volume excess for transfusion, if necessary
therapy persist or worsen
• Administer blood products (e.g., • Prepare for administration of blood
platelets and fresh frozen products (e.g., check blood with patient
plasma), as appropriate identification and prepare infusion
setup), as appropriate
Ped Acute Care40300
NIC: Enteral Tube Feeding-Activities (p.304) 3
• Insert a nasogastric, • Applying anchoring • Monitor for proper placement of
nasoduodenal, or nasojejunal substance to skin, and the tube by inspecting oral cavity,
tube, according to agency secure feeding tube with checking for gastric residual, or
protocol tape listening while air is injected and
withdrawn, according to agency
protocol
• Request that tube • Monitor for presence of • Monitor fluid and electrolyte status
placement be checked by x- bowel sounds every 4 to 8
ray examination when hr., as appropriate
placement is questionable
• Consult with other health • Elevate head of the bed • Offer pacifier to infant during
care team members in during feedings feeding, as appropriate
selecting the type and
strength of enteral feeding
• Hold and talk to infant • Discontinue feedings 30 • Add blue food coloring to tube
during feeding to simulate to 60 min. before putting feedings to monitor for aspiration
usual feeding activities in a head-down position or fistula
• Irrigate the tube every 4 to • Use clean technique in • Check gravity drip rate or pump
6 hr. during continuous administering tube rate every hour
feedings and after every feedings
intermittent feeding
• Slow tube feeding rate • Monitor for sensation of • Check residual every 4 to 6 hr.
and/or decrease strength to fullness, nausea, and during continuous feedings and
control diarrhea vomiting before each intermittent feeding
• Hold tube feedings if • Keep cuff of endotracheal • Keep open containers of enternal
residual is greater than 150 or tracheostomy tube feeding refrigerated
cc or more than 110% to inflated during feeding, as
120% of the hourly rate in appropriate
adults
• Change feeding and infusion • Wash skin around skin • Check water level in skin level
tubing regularly, according level device daily with mild device balloon, according to
to agency protocol soap and dry thoroughly equipment protocol
• Discard enternal feeding • Refill feeding bag every 4 • Prepare patient for home tube
containers and hr., as appropriate feedings, as appropriate
administration sets every 24
hours
Ped Acute Care40300
NOC-Nutritional Status: Energy
NIC: Weight Gain Assistance-Activities (,p.703) 3
• Refer for diagnostic • Weigh patient at specified • Discuss possible causes of low body
workup to determine intervals, as appropriate weight
cause of being
underweight, as
appropriate
• Monitor for nausea and • Determine cause of nausea • Administer medications to reduce
vomiting and/or vomiting, and treat nausea and pain before eating, as
appropriately appropriate
• Monitor daily calories • Monitor serum albumin, • Encourage increased calorie intake
consumed lymphocyte, and electrolyte
levels
• Instruct on how to • Provide a variety of high- • Consider patient’s food
increase calorie intake calorie nutritious foods from preferences, as governed by
which to select personal choices and cultural and
religious preferences
• Provide oral care before • Provide rest periods, as • Ensure that patient is in a sitting
meals, as needed needed position before eating or feeding
• Assist with eating or • Provide foods appropriate for • Create a pleasant, relaxing
feed patient, as patient: general diet, environment at mealtime
appropriate mechanical soft, blenderized
or commercial formula via
nasogastric or gastrostomy
tube, or total parental
nutrition, as ordered by
physician
• Serve food in a pleasant, • Discuss with patient and • Discuss with patient and family
attractive manner family socioeconomic factors perceptions or factors interfering
contributing to inadequate with ability or desire to eat
nutrition
• Refer to community • Teach patient and family • Teach patient and family how to buy
agencies that can assist meal planning, as appropriate low-cot, nutritious foods, as
in acquiring food, as appropriate
appropriate
• Reward patient for • Chart weight gain progress • Encourage attendance at support
weight gain and post in a strategic groups, as appropriate
location
Ped Acute Care40300
NIC: Nutritional Monitoring-Activities (,p.477) 3
• Weigh patient at • Monitor trends in weight loss • Monitor type and amount of usual
specified intervals and gain exercise
• Monitor patient’s • Monitor parent/child • Monitor environment where eating
emotional response when interactions during feeding, occurs
placed in situations that as appropriate
involve food and eating
• Schedule treatments and • Monitor for dry, flaky skin • Monitor skin turgor, as appropriate
procedures at times with depigmentation
other than feeding times
• Monitor for dry, thin • Monitor gums for swelling, • Monitor for nausea and vomiting
hair that is easy to pluck sponginess, receding, and
increased bleeding
• Monitor skinfold • Monitor albumin, total • Monitor lymphocyte and electrolyte
measurements;triceps protein, hemaglobin, and levels
skinfold, midarm muscle hematocrit levels
circumference, and
midarm circumference
• Monitor food • Monitor growth and • Monitor energy level, malaise,
preferences and choices development fatigue, and weakness
• Monitor for pale, • Monitor caloric and nutrient • Monitor for spoon-shaped, brittle,
reddened, and dry intake ridged nails
conjunctival tissue
• Monitor for redness, • Note any sores, edema, • Note if tongue is scarlet, magenta,
swelling, and cracking of hyperemic and hypertrophic or raw
mouth/lips papillai of the tongue and oral
cavity
• Note significant changes • Initiate a dietary consult, as • Determine whether the patient
in nutritional status and appropriate needs a special diet
initiate treatments, as
appropriate
• Provide optimal • Provide nutritional food and
environmental conditions fluid, as appropriate
at mealtime
Congratulations!
You have successfully completed your first nursing care plan using the standard nursing language
vocabularies of NANDA, NOC, and NIC.
1. If you wish to received CE for this educational activity, please complete the evaluation form and
return along with $10 to:
Carol Williams, MS, RN, C
Educational Services for Nursing
University of Michigan Health System
300 North Ingalls , 6B12
Ann Arbor, Michigan 48109-0436
Ped Acute Care40300
2. If you are working with a coordinator please give your quiz, evaluation and completed nursing care plan to your coordinator.
Pediatric Acute Care
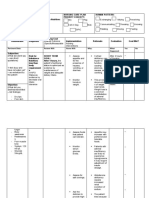
NURSING DIAGNOSIS : Patient Name
Defining Characteristics (Signs & Symptoms)
❏ ❏ ❏
❏ ❏ ❏
❏ ❏ ❏
Related Factors (Etiology)
❏ ❏
❏ ❏
❏ ❏
NOCs (Outcomes)
Measurement Scale Score:
1 = Not adequate
2 = Slightly adequate
Nutritional 3 = Moderately adequate
4 = Substantially adequate
Status:
5 = Totally adequate
Food & ❏ Oral food intake
Liquid ❏ Tube feeding intake
Intake ❏ Oral fluid intake
❏ IV fluid intake
DATE/TIME
INITIALS
Measurement Scale Score:
1 = Extremely compromised
2 = Substantially compromised
3 = Moderately compromised
Nutritional 4 = Substantially compromised
5 = Not compromised
Status:
❑ Growth
Energy ❑ Tissue healing
❏ Infection resistance
❑ Endurance
DATE/TIME
INITIALS
Ped Acute Care40300
NICs (interventions)ACTIVITIES: MODIFICATIONS:
❑
❑
Fluid
❑
Management ❑
❑
DATE/TIME
ACTIVITIES: MODIFICATIONS:
❑:
❏
Enteral Tube
❏
Feeding ❏
❑
DATE/TIME
ACTIVITIES: MODIFICATIONS:
❏
❏
Weight Gain
❏
Assistance ❏
❏
DATE/TIME
ACTIVITIES: MODIFICATIONS:
❏
❏
Nutritional ❏
Monitoring ❏
❏
DATE/TIME
OTHER INTERVENTIONS: SIGNATURE BOXES:
• •
• •
Ped Acute Care40300
You might also like
- Altered Bowel EliminationDocument1 pageAltered Bowel EliminationneoclintNo ratings yet
- NCP PneumoniaDocument28 pagesNCP PneumoniaW'ton Borbe83% (6)
- Nursing Care PlanDocument6 pagesNursing Care Planamang oteiNo ratings yet
- Anatomy and Physiology-Liver CirrhosisDocument2 pagesAnatomy and Physiology-Liver CirrhosisHilmi Ramos100% (3)
- Imbalanced NutritionDocument2 pagesImbalanced NutritionmarielfmerlanNo ratings yet
- Nursing Care Plan Otitis MediaDocument3 pagesNursing Care Plan Otitis Mediaevi nur laili100% (2)
- Ulcerative Colitis FinalDocument13 pagesUlcerative Colitis FinalAngelique100% (1)
- Nursing Care Plan Risk For Urinary RetentionDocument4 pagesNursing Care Plan Risk For Urinary RetentionReginald Julia100% (2)
- Case Study - EmphysemaDocument6 pagesCase Study - Emphysemamackie_041992No ratings yet
- Risk For AspirationDocument1 pageRisk For Aspirationmmcgee01No ratings yet
- Imbalanced Nutrition - Less Than Body Requirements 02Document7 pagesImbalanced Nutrition - Less Than Body Requirements 02AgronaSlaughterNo ratings yet
- Constipation NCPDocument2 pagesConstipation NCPDemilyn Olofernes-Fat100% (1)
- Doenges, Et. Al, (2008) - Nurse's Pocket Guide. 11 Edition. F.A. Davis Company. P. 385Document3 pagesDoenges, Et. Al, (2008) - Nurse's Pocket Guide. 11 Edition. F.A. Davis Company. P. 385Theresa AbrilloNo ratings yet
- NCP Risk For ConstipationDocument1 pageNCP Risk For Constipationjorgeacct50% (4)
- Nursing Process of PneumoniaDocument5 pagesNursing Process of Pneumoniatin2x061275% (8)
- NCP Risk For Fluid Volume DeficitDocument2 pagesNCP Risk For Fluid Volume DeficitJeanineReyes44% (9)
- CellulitisDocument12 pagesCellulitisAlma Bertos-Agub100% (1)
- NCP On Electrolyte ImbalanceDocument4 pagesNCP On Electrolyte Imbalancefreyah_bc67% (3)
- NCP 2 Addison's DiseaseDocument4 pagesNCP 2 Addison's DiseaseRenee RoSeNo ratings yet
- Electrolyte Imbalance NCPDocument8 pagesElectrolyte Imbalance NCPManuel Jacob YradNo ratings yet
- Chronic Obstructive Pulmonary Disease (COPD)Document1 pageChronic Obstructive Pulmonary Disease (COPD)Bheru LalNo ratings yet
- 10 NCP FractureDocument4 pages10 NCP FractureICa Marlina0% (1)
- Case: Liver Cirrhosis Assessment:: Nursing InferenceDocument7 pagesCase: Liver Cirrhosis Assessment:: Nursing InferenceLovelyn GanirNo ratings yet
- Risk For InjuryDocument2 pagesRisk For InjuryRo-anne AkuNo ratings yet
- Nursing Care PlanDocument4 pagesNursing Care PlanSharmaine Grace Florig100% (2)
- Compromised Family Coping NCPDocument2 pagesCompromised Family Coping NCPJamaeka Gotis100% (1)
- NCPDocument4 pagesNCPAndrea BroccoliNo ratings yet
- Subjective and Objective Data Educative (Edx)Document2 pagesSubjective and Objective Data Educative (Edx)Donalyn ReyesNo ratings yet
- Nursing Care PlanDocument15 pagesNursing Care PlanZhel Geron MercadoNo ratings yet
- Nursing Care Plan For "Eating Disorders - Obesity"Document9 pagesNursing Care Plan For "Eating Disorders - Obesity"jhonroks100% (3)
- PTB NCPDocument12 pagesPTB NCPNiel LeeNo ratings yet
- JVJV NCP Risk For Fluid Volume DeficitDocument2 pagesJVJV NCP Risk For Fluid Volume DeficitvicenteturasNo ratings yet
- University of The East: Assessment Diagnosis Planning Intervention Rationale EvaluationDocument3 pagesUniversity of The East: Assessment Diagnosis Planning Intervention Rationale EvaluationPATRICIA JEANNE JABIANNo ratings yet
- Pneumonia Care PlanDocument1 pagePneumonia Care Plantcumurphish67% (3)
- Nursing Care PlanDocument4 pagesNursing Care PlanJobelyn TunayNo ratings yet
- Glaucoma NCPDocument4 pagesGlaucoma NCPChantal CaraganNo ratings yet
- NCP CopdDocument6 pagesNCP Copdjoelette100% (1)
- Nursing Care Plan For Imbalanced Nutrition Less Than Body Req NCPDocument4 pagesNursing Care Plan For Imbalanced Nutrition Less Than Body Req NCPkarthi karthi50% (2)
- Impaired Skin IntegrityDocument2 pagesImpaired Skin IntegritySharewin PulidoNo ratings yet
- NCP For BreathingDocument17 pagesNCP For BreathingCeleste Sin Yee100% (1)
- Nursing Diagnosis For AsthmaDocument6 pagesNursing Diagnosis For AsthmaTINAIDA33% (3)
- NCP Imbalanced NutritionDocument3 pagesNCP Imbalanced NutritionAav Canlas100% (1)
- Nursing Careplan - Rectal CancerDocument5 pagesNursing Careplan - Rectal CancerdrugcardrefNo ratings yet
- Subjective Cues: Independent: On The: "Nahihirapa N Ako Huminga" AsDocument5 pagesSubjective Cues: Independent: On The: "Nahihirapa N Ako Huminga" AsYessaminNo ratings yet
- NCP For CHDDocument2 pagesNCP For CHDMonica Rivera100% (1)
- CHNDocument119 pagesCHNCanny CańasNo ratings yet
- NCP Loss of AppetiteDocument5 pagesNCP Loss of AppetiteStenneli Gumban Trojillo50% (2)
- NCP Copd4Document15 pagesNCP Copd4Alessa Marie Crisostomo Salazar100% (1)
- Ineffective Health Management Related To Mrs. Gama: Provide The Client Enough Knowledge About The ProblemDocument5 pagesIneffective Health Management Related To Mrs. Gama: Provide The Client Enough Knowledge About The ProblemAndrea Albester GarinoNo ratings yet
- Carpenito-Moyet, L. J. (2009) : IndependentDocument3 pagesCarpenito-Moyet, L. J. (2009) : IndependentClint DelacruzNo ratings yet
- Asthma Nanda DiagnosesDocument4 pagesAsthma Nanda DiagnosesZinya RobinsonNo ratings yet
- Nursing Care Plan For "Hepatitis"Document12 pagesNursing Care Plan For "Hepatitis"jhonroks86% (14)
- Intussusception Nursing Care PlanDocument7 pagesIntussusception Nursing Care PlanElli SuñgaNo ratings yet
- NCP Format 3 CKD Chronic Kidney Disease DM Diabetes Mellitus NephropathyDocument3 pagesNCP Format 3 CKD Chronic Kidney Disease DM Diabetes Mellitus NephropathyMichael Baylon Dueñas100% (2)
- Parenteral Nutrition Basic IVT Nov 2008Document53 pagesParenteral Nutrition Basic IVT Nov 2008Crystal Mae Castrodes DaquipilNo ratings yet
- Hainashri MSN ProcedureDocument9 pagesHainashri MSN ProcedureRickjit SadhukhanNo ratings yet
- Parenteral Tube Feeding - (Renad Al-Dousari)Document16 pagesParenteral Tube Feeding - (Renad Al-Dousari)perillantoNo ratings yet
- Nursing Care Plan 4 Gas Exchange, ImpairedDocument9 pagesNursing Care Plan 4 Gas Exchange, Impaireddbryant0101100% (6)
- Acute Glomerulonephritis - CSDocument31 pagesAcute Glomerulonephritis - CSMASIINo ratings yet
- Drug Study 2Document7 pagesDrug Study 2Jediale CarcelerNo ratings yet
- A Hudson Valley Simmons Family Part 3Document124 pagesA Hudson Valley Simmons Family Part 3dbryant0101100% (2)
- The Narragansett Historical Register Vol 3-4 Part 1Document453 pagesThe Narragansett Historical Register Vol 3-4 Part 1dbryant0101No ratings yet
- Game of Life-eBookDocument101 pagesGame of Life-eBookWarrior SoulNo ratings yet
- From The Ashes of Angels 1Document13 pagesFrom The Ashes of Angels 1dbryant0101No ratings yet
- Evanghelia Dupa Iuda CompletaDocument7 pagesEvanghelia Dupa Iuda CompletaciclopulNo ratings yet
- A Hudson Valley Simmons Family Part 1Document124 pagesA Hudson Valley Simmons Family Part 1dbryant010150% (2)
- Gov Henry Bull & DescendantsDocument8 pagesGov Henry Bull & Descendantsdbryant0101No ratings yet
- The Narragansett Historical Register Vol 1-2 Part 2Document238 pagesThe Narragansett Historical Register Vol 1-2 Part 2dbryant0101100% (1)
- Moses Barber 1652-1733 of South Kinston Rhode IslandDocument149 pagesMoses Barber 1652-1733 of South Kinston Rhode Islanddbryant0101100% (3)
- A Hudson Valley Simmons Family Part 4Document123 pagesA Hudson Valley Simmons Family Part 4dbryant0101No ratings yet
- Record of The Rust Family Part 2Document189 pagesRecord of The Rust Family Part 2dbryant0101100% (1)
- An Authentic History of Lancaster County Part 2Document305 pagesAn Authentic History of Lancaster County Part 2dbryant0101100% (6)
- Record of The Rust Family Part 1Document189 pagesRecord of The Rust Family Part 1dbryant0101No ratings yet
- Ness Family History Part 4Document75 pagesNess Family History Part 4dbryant0101100% (1)
- Ness Family History Part 2Document78 pagesNess Family History Part 2dbryant0101100% (1)
- Record of The Rust Family Part 3Document187 pagesRecord of The Rust Family Part 3dbryant0101100% (2)
- Gardner-Gardiner Rhode IslandDocument42 pagesGardner-Gardiner Rhode Islanddbryant0101100% (1)
- Nellis Family HistoryDocument247 pagesNellis Family Historydbryant0101No ratings yet
- Ness Family History Part 3Document78 pagesNess Family History Part 3dbryant0101No ratings yet
- Relating Nursing Diagnoses To Drug TherapyDocument7 pagesRelating Nursing Diagnoses To Drug Therapydbryant0101No ratings yet
- Chronicles of The Family BakerDocument414 pagesChronicles of The Family Bakerdbryant0101100% (2)
- Bouck of Schoharie & OntarioDocument231 pagesBouck of Schoharie & Ontariodbryant010175% (4)
- Nursing Care Plan Acute PainDocument3 pagesNursing Care Plan Acute Paindbryant010199% (69)
- Nursing Diagnosis Keystone of Your Care PlanDocument5 pagesNursing Diagnosis Keystone of Your Care Plandbryant010167% (3)
- Nursing Diagnosis Made SimpleDocument3 pagesNursing Diagnosis Made Simpledbryant0101100% (14)
- Nursing Care Plan Sheet SampleDocument3 pagesNursing Care Plan Sheet Sampledbryant0101100% (5)
- 2nd Book of Records Town of South Amp Ton Long Island NYDocument408 pages2nd Book of Records Town of South Amp Ton Long Island NYdbryant0101No ratings yet
- Baptisms Marriages Methodist Episcopal Church Newburgh NYDocument28 pagesBaptisms Marriages Methodist Episcopal Church Newburgh NYdbryant010180% (5)
- 4th Book of Records Town of South Amp Ton Long Island NYDocument370 pages4th Book of Records Town of South Amp Ton Long Island NYdbryant0101No ratings yet
- Baptisms-Marriage Register of Old Dutch Church of Kingston Ulster Co NYDocument824 pagesBaptisms-Marriage Register of Old Dutch Church of Kingston Ulster Co NYdbryant0101No ratings yet
- Screenshot 2019-10-30 at 12.44.00Document25 pagesScreenshot 2019-10-30 at 12.44.00Miền VũNo ratings yet
- Radiador y Sus Partes, Motor Diesel 504BDTDocument3 pagesRadiador y Sus Partes, Motor Diesel 504BDTRamón ManglesNo ratings yet
- AIPMT 2009 ExamDocument25 pagesAIPMT 2009 ExamMahesh ChavanNo ratings yet
- Evolution Practice Test 2 With AnswersDocument10 pagesEvolution Practice Test 2 With AnswersSuhani SinhaNo ratings yet
- Insurance CodeDocument18 pagesInsurance CodeKenneth Holasca100% (1)
- Management of AsthmaDocument29 pagesManagement of AsthmaAbdullah Al ArifNo ratings yet
- Cardiovascular Pharmacology: DR Muhamad Ali Sheikh Abdul Kader MD (Usm) MRCP (Uk) Cardiologist, Penang HospitalDocument63 pagesCardiovascular Pharmacology: DR Muhamad Ali Sheikh Abdul Kader MD (Usm) MRCP (Uk) Cardiologist, Penang HospitalCvt RasulNo ratings yet
- GCU 0103 Computer PlatformsDocument5 pagesGCU 0103 Computer PlatformsArani NavaratnarajahNo ratings yet
- Lesson 1 Animal CareDocument8 pagesLesson 1 Animal CareLexi PetersonNo ratings yet
- TestDocument233 pagesTestye rightNo ratings yet
- CSF LeaksDocument3 pagesCSF LeaksDrTarek Mahmoud Abo KammerNo ratings yet
- Application of Knowledge QuestionsDocument16 pagesApplication of Knowledge QuestionsElllie TattersNo ratings yet
- PCB Engraver Operator Manual PDFDocument41 pagesPCB Engraver Operator Manual PDFmyoshkeuNo ratings yet
- Eaton Current Limiting FusesDocument78 pagesEaton Current Limiting FusesEmmanuel EntzanaNo ratings yet
- Tool 10 Template Working Papers Cover SheetDocument4 pagesTool 10 Template Working Papers Cover Sheet14. Đỗ Kiến Minh 6/5No ratings yet
- Research Paper DraftDocument45 pagesResearch Paper DraftMelissa SpamNo ratings yet
- Dosage Calculations, CH 10 ProblemsDocument1 pageDosage Calculations, CH 10 ProblemsJacqueline GreerNo ratings yet
- PROJECT PROPOSAL AND PROJECT MANAGEMENT TOOLS GROUPWORK (Situation No. 3 - BSSW 3A)Document21 pagesPROJECT PROPOSAL AND PROJECT MANAGEMENT TOOLS GROUPWORK (Situation No. 3 - BSSW 3A)Hermida Julia AlexandreaNo ratings yet
- Food DirectoryDocument20 pagesFood Directoryyugam kakaNo ratings yet
- CITEC Genesis & GenXDocument45 pagesCITEC Genesis & GenXPutra LangitNo ratings yet
- Msla Business FeesDocument1 pageMsla Business FeesNBC MontanaNo ratings yet
- All Vaccinees Are Requested To Bring Certificate of Dose-II From COWIN Portal Alongwith Registered Mobile Number Before Proceeding For VaccinationDocument7 pagesAll Vaccinees Are Requested To Bring Certificate of Dose-II From COWIN Portal Alongwith Registered Mobile Number Before Proceeding For VaccinationRakesh KumarNo ratings yet
- Midyear Budget ReportDocument402 pagesMidyear Budget Reportcbs6albanyNo ratings yet
- Jis C 8156-2017, EngDocument32 pagesJis C 8156-2017, Eng7620383tlNo ratings yet
- AD Oracle ManualDocument18 pagesAD Oracle ManualAlexandru Octavian Popîrțac100% (2)
- TG Chap. 10Document7 pagesTG Chap. 10Gissele AbolucionNo ratings yet
- CO2 & SelexolDocument18 pagesCO2 & Selexolmihaileditoiu2010No ratings yet
- Supply Chain Logistics Manager in Dallas FT Worth TX Resume Calvin HarperDocument2 pagesSupply Chain Logistics Manager in Dallas FT Worth TX Resume Calvin HarperCalvinHarperNo ratings yet
- Fermentation Media: Agustin Krisna WardaniDocument27 pagesFermentation Media: Agustin Krisna WardaniYosiaNo ratings yet
- Random FactsDocument353 pagesRandom FactsSergio Rivas100% (1)
- Instant Loss On a Budget: Super-Affordable Recipes for the Health-Conscious CookFrom EverandInstant Loss On a Budget: Super-Affordable Recipes for the Health-Conscious CookRating: 3.5 out of 5 stars3.5/5 (2)
- The Beck Diet Solution Weight Loss Workbook: The 6-Week Plan to Train Your Brain to Think Like a Thin PersonFrom EverandThe Beck Diet Solution Weight Loss Workbook: The 6-Week Plan to Train Your Brain to Think Like a Thin PersonRating: 3.5 out of 5 stars3.5/5 (33)
- The Diabetes Code: Prevent and Reverse Type 2 Diabetes NaturallyFrom EverandThe Diabetes Code: Prevent and Reverse Type 2 Diabetes NaturallyRating: 4.5 out of 5 stars4.5/5 (3)
- The Obesity Code: Unlocking the Secrets of Weight LossFrom EverandThe Obesity Code: Unlocking the Secrets of Weight LossRating: 4 out of 5 stars4/5 (6)
- Forever Strong: A New, Science-Based Strategy for Aging WellFrom EverandForever Strong: A New, Science-Based Strategy for Aging WellNo ratings yet
- Body Love Every Day: Choose Your Life-Changing 21-Day Path to Food FreedomFrom EverandBody Love Every Day: Choose Your Life-Changing 21-Day Path to Food FreedomRating: 4 out of 5 stars4/5 (1)
- Find Your Path: Honor Your Body, Fuel Your Soul, and Get Strong with the Fit52 LifeFrom EverandFind Your Path: Honor Your Body, Fuel Your Soul, and Get Strong with the Fit52 LifeRating: 4 out of 5 stars4/5 (3)
- Love Yourself, Heal Your Life Workbook (Insight Guide)From EverandLove Yourself, Heal Your Life Workbook (Insight Guide)Rating: 5 out of 5 stars5/5 (40)
- Grit & Grace: Train the Mind, Train the Body, Own Your LifeFrom EverandGrit & Grace: Train the Mind, Train the Body, Own Your LifeRating: 4 out of 5 stars4/5 (3)
- The Food Lover's Cleanse: 140 Delicious, Nourishing Recipes That Will Tempt You Back into Healthful EatingFrom EverandThe Food Lover's Cleanse: 140 Delicious, Nourishing Recipes That Will Tempt You Back into Healthful EatingRating: 4 out of 5 stars4/5 (3)
- Gut: The Inside Story of Our Body's Most Underrated Organ (Revised Edition)From EverandGut: The Inside Story of Our Body's Most Underrated Organ (Revised Edition)Rating: 4 out of 5 stars4/5 (411)
- Glucose Revolution: The Life-Changing Power of Balancing Your Blood SugarFrom EverandGlucose Revolution: The Life-Changing Power of Balancing Your Blood SugarRating: 5 out of 5 stars5/5 (351)
- Summary of Mary Claire Haver's The Galveston DietFrom EverandSummary of Mary Claire Haver's The Galveston DietRating: 5 out of 5 stars5/5 (1)
- Sugar Crush: How to Reduce Inflammation, Reverse Nerve Damage, and Reclaim Good HealthFrom EverandSugar Crush: How to Reduce Inflammation, Reverse Nerve Damage, and Reclaim Good HealthRating: 4 out of 5 stars4/5 (6)
- Metabolism Revolution: Lose 14 Pounds in 14 Days and Keep It Off for LifeFrom EverandMetabolism Revolution: Lose 14 Pounds in 14 Days and Keep It Off for LifeNo ratings yet
- The End of Craving: Recovering the Lost Wisdom of Eating WellFrom EverandThe End of Craving: Recovering the Lost Wisdom of Eating WellRating: 4.5 out of 5 stars4.5/5 (82)
- Eat Complete: The 21 Nutrients That Fuel Brainpower, Boost Weight Loss, and Transform Your HealthFrom EverandEat Complete: The 21 Nutrients That Fuel Brainpower, Boost Weight Loss, and Transform Your HealthRating: 2 out of 5 stars2/5 (1)
- The Body Book: The Law of Hunger, the Science of Strength, and Other Ways to Love Your Amazing BodyFrom EverandThe Body Book: The Law of Hunger, the Science of Strength, and Other Ways to Love Your Amazing BodyNo ratings yet
- Secrets From the Eating Lab: The Science of Weight Loss, the Myth of Willpower, and Why You Should Never Diet AgainFrom EverandSecrets From the Eating Lab: The Science of Weight Loss, the Myth of Willpower, and Why You Should Never Diet AgainRating: 3.5 out of 5 stars3.5/5 (38)
- The Arm: Inside the Billion-Dollar Mystery of the Most Valuable Commodity in SportsFrom EverandThe Arm: Inside the Billion-Dollar Mystery of the Most Valuable Commodity in SportsRating: 4 out of 5 stars4/5 (49)
- Summary: Fast Like a Girl: A Woman’s Guide to Using the Healing Power of Fasting to Burn Fat, Boost Energy, and Balance Hormones: Key Takeaways, Summary and AnalysisFrom EverandSummary: Fast Like a Girl: A Woman’s Guide to Using the Healing Power of Fasting to Burn Fat, Boost Energy, and Balance Hormones: Key Takeaways, Summary and AnalysisRating: 3 out of 5 stars3/5 (2)
- The Diet Trap Solution: Train Your Brain to Lose Weight and Keep It Off for GoodFrom EverandThe Diet Trap Solution: Train Your Brain to Lose Weight and Keep It Off for GoodNo ratings yet
- Eat to Lose, Eat to Win: Your Grab-n-Go Action Plan for a Slimmer, Healthier YouFrom EverandEat to Lose, Eat to Win: Your Grab-n-Go Action Plan for a Slimmer, Healthier YouNo ratings yet
- Smarter Not Harder: The Biohacker's Guide to Getting the Body and Mind You WantFrom EverandSmarter Not Harder: The Biohacker's Guide to Getting the Body and Mind You WantRating: 3.5 out of 5 stars3.5/5 (2)
- Keto Friendly Recipes: Easy Keto For Busy PeopleFrom EverandKeto Friendly Recipes: Easy Keto For Busy PeopleRating: 3.5 out of 5 stars3.5/5 (2)
- Foods That Cause You to Lose Weight: The Negative Calorie EffectFrom EverandFoods That Cause You to Lose Weight: The Negative Calorie EffectRating: 3 out of 5 stars3/5 (5)
- How to Be Well: The 6 Keys to a Happy and Healthy LifeFrom EverandHow to Be Well: The 6 Keys to a Happy and Healthy LifeRating: 5 out of 5 stars5/5 (1)