Professional Documents
Culture Documents
Assessing Body Temperatur1
Uploaded by
juancristoOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Assessing Body Temperatur1
Uploaded by
juancristoCopyright:
Available Formats
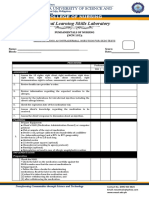
ASSESSING BODY TEMPERATURE (Axillary Temperature) ASSESSMENT: Assess: 1. Clinical Signs of fever.
Onset (Cold or Chill Stage) - Increase heart rate. - Increase respiratory rate and dept. - Shivering - Pallid and cold skin - Complaints of feeling cold - Cyanotic nail beds - gooseflesh appearance of the skin - Cessation of sweating Course - Absence of chills - Warm skin - Photosensitivity - Glassy-eyed - Increase pulse rate and respiratory rate - Increase thirst - Mild to severe dehydration - Drowsiness, restlessness, delirium or convulsion - Herpetic lesions of the mouth - Loss of appetite - Malaise, weakness and aching muscles Defervescence (Fever abatement) - Skin that appear flushed and feels warm - Sweating - Decreased shivering - Possible dehydration PLANNING: 1. Assemble equipment and supplies - Thermometer - Cotton balls with alcohol or alcohol wipes - Tissue/wipes - Watch with a second hand or indicator IMPLEMENTATION: Procedure 1. Check that all equipment is functioning properly. If necessary, shake a glass thermometer down to below 35 degree Celsius (95 degree Fahrenheit) 2. Identify the client properly. 3. Explain to the client what you are going to do, why it is necessary, and how he can cooperate. - To reduce transmission of microorganism 4. Wash hands and observe other appropriate infection control procedures. 5. Provide for client privacy. 6. Place the client in appropriate position. 7. Pat the armpit dry with tissue paper or ask the client to do it if able. 8. Wipe the thermometer from bulb to stem with alcoholized cotton ball. 9. Place the bulb of the thermometer in the center of the axilla on the clients opposite side. 10. Wait for the appropriate amount of time. 6 to 9 minutes for an axillary temperature with a glass - To maintain dignity. - To promote comfort and facilitate the taking of the vital sign. - Moisture can alter or affect axillary temperature.
2. Clinical Signs of Hypothermia. - Decreased body temperature - Severe shivering (initially) - Feeling of cold and chills - Pale, cool, waxy skin - Hypotension - Decreased urinary output - Lack of muscle coordination - Disorientation - Drowsiness progressing to coma 3. Clients readiness for the procedure. Smoking, eating, or drink a hot or cold beverages can alter the reading. In these case, the route of temperature taking must be changed or wait for 20-30 minutes before taking oral temperature. 4. Site most appropriate for measurement. 5. Factors that may alter core body temperature.
Rationale - The indicator fluid will not fall below the starting level if the clients temperature is less than that. - To be sure youre performing the procedure on the correct client. -To lessen anxiety and to promote cooperation.
- The bulb is considered less contaminated than the stem. - To facilitate the reading of body temperature and free the arm nearest to the nurse for the reading of the other vital signs. - To conserve time and energy.
temperature. 11. Remove the thermometer and wipe with a tissue if necessary. 12. Read the temperature. 13. Wipe the thermometer with alcoholized cotton ball from stem to bulb. Return to container. 14. Wash hands. 15. Document the temperature in the clients record. EVALUATION: 1. Compare the temperature measurement with the baseline data, normal range for age of client, and clients previous temperature. Analyze considering time of day and any additional influencing factors and other vital signs. 2. If reading is not within normal range, retake it to eliminate the possibility of inaccuracy. 3. Conduct appropriate follow-up such as notifying the physician, giving a medication, or altering the clients environment. This includes teaching such as increasing fluid intake, coughing and deep breathing or removing heavy coverings.
You might also like
- Atenolol TenorminDocument3 pagesAtenolol TenorminLIEZEL GRACE VELAYONo ratings yet
- Clinical Learning Skills Laboratory: College of NursingDocument3 pagesClinical Learning Skills Laboratory: College of NursingBeverly DatuNo ratings yet
- NCP Risk InfectionDocument1 pageNCP Risk InfectionEni RahmawatiNo ratings yet
- Pharma CardsDocument5 pagesPharma CardsazancheNo ratings yet
- HES 005 P2 Coverage and Drug Study GuideDocument4 pagesHES 005 P2 Coverage and Drug Study GuideXander Jake Asturias TangcalaganNo ratings yet
- Adolescent Nutrition Final CountdownDocument18 pagesAdolescent Nutrition Final CountdownNicole Denise PortugalezaNo ratings yet
- 6) Community Diagnosis 2011Document33 pages6) Community Diagnosis 2011Dinar Kartika HapsariNo ratings yet
- PNS Pain Management Guideline For Nursing CompetencyDocument10 pagesPNS Pain Management Guideline For Nursing Competencyvhon100% (1)
- Fluid Volume Deficit Nursing ManagementDocument5 pagesFluid Volume Deficit Nursing ManagementA.No ratings yet
- Nursing Assessment IIDocument5 pagesNursing Assessment IImyer pasandalanNo ratings yet
- Volume ImpairmentDocument32 pagesVolume ImpairmentAcohCChaoNo ratings yet
- Nursing Process NUTRITIONDocument82 pagesNursing Process NUTRITIONNoci M. FrenkNo ratings yet
- NCM 107-A Lecture 2012Document241 pagesNCM 107-A Lecture 2012Michael Anthony Ermita50% (2)
- Drug StudyDocument8 pagesDrug StudyJay-ar Batara SorianoNo ratings yet
- Chapter 31 HypertensionDocument3 pagesChapter 31 HypertensionVen SemillaNo ratings yet
- Diabetes Mellitus: Rasmussen NPR Concept PlanDocument1 pageDiabetes Mellitus: Rasmussen NPR Concept PlanRoshin TejeroNo ratings yet
- Neuro - Sir Chavez - AS OF 12PMDocument5 pagesNeuro - Sir Chavez - AS OF 12PMCarl JustineNo ratings yet
- Anatomy and PhysiologyDocument4 pagesAnatomy and PhysiologyBeRnAlieNo ratings yet
- Evaluation of Fetal Well BeingDocument22 pagesEvaluation of Fetal Well BeingJoanah Mae AsuncionNo ratings yet
- Competency Appraisal 1Document30 pagesCompetency Appraisal 1mirai desuNo ratings yet
- Nursing DiagnosisDocument9 pagesNursing Diagnosiskhikmatul mu'jizahNo ratings yet
- Assessment Diagnosis Scientific Background Planning Intervention Rationale Evaluation Short Term: IndependentDocument2 pagesAssessment Diagnosis Scientific Background Planning Intervention Rationale Evaluation Short Term: IndependentNE TdrNo ratings yet
- Drug StudyDocument11 pagesDrug StudyJay VillasotoNo ratings yet
- Discharge Plan: Drug/S Indication/S Dosage Route FrequencyDocument3 pagesDischarge Plan: Drug/S Indication/S Dosage Route Frequencymyer pasandalanNo ratings yet
- Nrg203: Care of Mother, Child, and Adolescent: (StudentDocument6 pagesNrg203: Care of Mother, Child, and Adolescent: (Studentmikhaela sencilNo ratings yet
- Term 3 Rationale Pharmacology and MCNDocument35 pagesTerm 3 Rationale Pharmacology and MCNKing KongNo ratings yet
- AFPMC V. Luna General Hospital: Case StudyDocument27 pagesAFPMC V. Luna General Hospital: Case StudyLemuel GuevarraNo ratings yet
- Narratives Case NotesDocument4 pagesNarratives Case NotesKnigh RiderNo ratings yet
- Case Study - Dengue Fever V - S UtiDocument12 pagesCase Study - Dengue Fever V - S UtiHarlene Joyce ReyNo ratings yet
- Nursing Care Plan Case StudyDocument2 pagesNursing Care Plan Case StudyHANIM0% (1)
- PrevacidDocument1 pagePrevacidAdrianne BazoNo ratings yet
- Care of The Clients With Problems in Acute Biologic Crisis: Ateneo de Zamboanga UniversityDocument3 pagesCare of The Clients With Problems in Acute Biologic Crisis: Ateneo de Zamboanga UniversityGrant Wynn ArnucoNo ratings yet
- LOG101 Exercise No. 2 - Types of Definitions 20230217091032Document2 pagesLOG101 Exercise No. 2 - Types of Definitions 20230217091032Daniella TimbolNo ratings yet
- Health Care Ethics Activity 2Document6 pagesHealth Care Ethics Activity 2Kyla BeconiaNo ratings yet
- Nursing Care Plan - MergedDocument13 pagesNursing Care Plan - MergedJuls Flares SycaycoNo ratings yet
- SKILL 8-16 Drawing Blood From A Central Venous Catheter: Key TermsDocument7 pagesSKILL 8-16 Drawing Blood From A Central Venous Catheter: Key TermsElizalde HusbandNo ratings yet
- Bacillary DysenteryDocument32 pagesBacillary Dysenteryapi-199163990% (1)
- Reflective Journal 1Document4 pagesReflective Journal 1api-365605511No ratings yet
- Date Performed: August 18, 2015 Group No. and Section: Group 5 WCDE-A Date Submitted: September 1, 2015 Group MembersDocument28 pagesDate Performed: August 18, 2015 Group No. and Section: Group 5 WCDE-A Date Submitted: September 1, 2015 Group MembersCm MacaliaNo ratings yet
- Gordons 11 Health Pattern Guide Format and Questions Converted 1Document11 pagesGordons 11 Health Pattern Guide Format and Questions Converted 1Kim BadillesNo ratings yet
- Nursing Care To Promote Fetal Maternal HealthDocument3 pagesNursing Care To Promote Fetal Maternal HealthLuna Sang-anNo ratings yet
- Sheena Khan: Biochemistry Generiic Bs NursingDocument22 pagesSheena Khan: Biochemistry Generiic Bs NursingsharmeenNo ratings yet
- Drug StudyDocument24 pagesDrug Studyabulan100% (1)
- HCTZDocument1 pageHCTZSheri490100% (1)
- Glycerin: (Gli-Ser-In)Document2 pagesGlycerin: (Gli-Ser-In)Aryanto DedyNo ratings yet
- STUDENT Sepsis Rapid ReasoningDocument6 pagesSTUDENT Sepsis Rapid Reasoningghodghod123No ratings yet
- Anemia-Careplan For AdultDocument29 pagesAnemia-Careplan For AdultdjbhetaNo ratings yet
- Nursing Skills Output (Nso)Document4 pagesNursing Skills Output (Nso)Julius ElciarioNo ratings yet
- Sterile Perineal Preparation ProcedureDocument1 pageSterile Perineal Preparation ProcedureLewis LyndonNo ratings yet
- Adult HealthDocument28 pagesAdult HealthL1NEDS DNo ratings yet
- ElectrocardiogramDocument3 pagesElectrocardiogramladydreamer_92No ratings yet
- Diabetes OPD ดีมากกกDocument5 pagesDiabetes OPD ดีมากกกPonpimol Odee BongkeawNo ratings yet
- Common ER EquipmentsDocument3 pagesCommon ER EquipmentsApple LlanesNo ratings yet
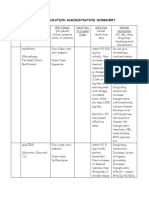
- Medication Administration WorksheetDocument6 pagesMedication Administration WorksheetCheska CarrionNo ratings yet
- Nursing Physical AssessmentDocument5 pagesNursing Physical AssessmentApril Louise PaluganNo ratings yet
- Dietary Computation For Pregnant ClientDocument12 pagesDietary Computation For Pregnant ClientLuis WashingtonNo ratings yet
- Herbal MedicinesDocument2 pagesHerbal MedicinesJan Nicole SeriñaNo ratings yet
- NUR209 WK7 Group Handout Case Study Assessment of Urinary Tract Infection Patient ProfileDocument4 pagesNUR209 WK7 Group Handout Case Study Assessment of Urinary Tract Infection Patient Profileania ojedaNo ratings yet
- Atun Maricris Jorre Ca2 Au Legarda Leadership Managemet Research DownloadableDocument2 pagesAtun Maricris Jorre Ca2 Au Legarda Leadership Managemet Research DownloadableCharissa Magistrado De LeonNo ratings yet
- Top 10 July 2012 Nutritionist-Dietitian Board Exam ResultsDocument1 pageTop 10 July 2012 Nutritionist-Dietitian Board Exam ResultsjuancristoNo ratings yet
- NURS0612 T 10Document3 pagesNURS0612 T 10NonoyTaclinoNo ratings yet
- Performance of Schools August 2012 Occupational Therapist Licensure ExaminationDocument1 pagePerformance of Schools August 2012 Occupational Therapist Licensure ExaminationjuancristoNo ratings yet
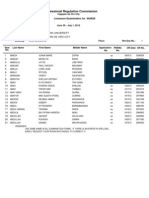
- June 2012 Nle Passers Complete ListDocument557 pagesJune 2012 Nle Passers Complete ListEli Benjamin Nava TaclinoNo ratings yet
- Performance of Schools August 2012 Physical Therapist Licensure ExaminationDocument3 pagesPerformance of Schools August 2012 Physical Therapist Licensure ExaminationjuancristoNo ratings yet
- June 2012 Nurse Licensure Examination Results Performance of Nursing SchoolsDocument19 pagesJune 2012 Nurse Licensure Examination Results Performance of Nursing SchoolsRay Andrew del RosarioNo ratings yet
- Top 10 July 2012 Marine Deck Licensure Examination (Master Mariner)Document1 pageTop 10 July 2012 Marine Deck Licensure Examination (Master Mariner)juancristoNo ratings yet
- Performance of Schools July 2012 Marine Deck Licensure Examination (Chief Mate)Document3 pagesPerformance of Schools July 2012 Marine Deck Licensure Examination (Chief Mate)juancristoNo ratings yet
- Performance of Schools July 2012 Nutritionist-Dietitian Board Exam ResultsDocument3 pagesPerformance of Schools July 2012 Nutritionist-Dietitian Board Exam ResultsjuancristoNo ratings yet
- Top 10 July 2012 Marine Deck Licensure Examination (O.I.C. - N.W.)Document1 pageTop 10 July 2012 Marine Deck Licensure Examination (O.I.C. - N.W.)juancristoNo ratings yet
- Performance of Schools July 2012 Marine Deck Licensure Examination (Master Mariner)Document2 pagesPerformance of Schools July 2012 Marine Deck Licensure Examination (Master Mariner)juancristoNo ratings yet
- Performance of Schools June 2012 Social Worker Board Exam ResultsDocument3 pagesPerformance of Schools June 2012 Social Worker Board Exam ResultsjuancristoNo ratings yet
- Performance of Schools July 2012 Marine Deck Licensure Examination (O.I.C. - N.W.)Document5 pagesPerformance of Schools July 2012 Marine Deck Licensure Examination (O.I.C. - N.W.)juancristoNo ratings yet
- Chief Mate Top 10 PassersDocument1 pageChief Mate Top 10 PassersCoolbuster.NetNo ratings yet
- Board of Real Estate Service - Resolution No. 12 (Series of 2012) - (Brokers) PDFDocument3 pagesBoard of Real Estate Service - Resolution No. 12 (Series of 2012) - (Brokers) PDFjuancristoNo ratings yet
- Vital Signs Procedures ChecklistDocument3 pagesVital Signs Procedures Checklistjuancristo90% (21)
- Performance of Schools July 2012 Ocular Pharmacologist Special Certification Exam ResultsDocument1 pagePerformance of Schools July 2012 Ocular Pharmacologist Special Certification Exam ResultsjuancristoNo ratings yet
- Top 10 July 2012 Real Estate Appraiser Board Exam ResultsDocument4 pagesTop 10 July 2012 Real Estate Appraiser Board Exam ResultsjuancristoNo ratings yet
- Nitroglycerin Drug StudyDocument5 pagesNitroglycerin Drug StudyjuancristoNo ratings yet
- Performance of Schools July 2012 Pharmacist Board Exam ResultsDocument2 pagesPerformance of Schools July 2012 Pharmacist Board Exam ResultsjuancristoNo ratings yet
- Marine Engineer Officers Licensure ExaminationsDocument1 pageMarine Engineer Officers Licensure ExaminationsjuancristoNo ratings yet
- Top 10 June 2012 Social Worker Board Exam ResultsDocument1 pageTop 10 June 2012 Social Worker Board Exam ResultsjuancristoNo ratings yet
- Performance of Schools Real Estate Appraiser Board Exam ResultsDocument7 pagesPerformance of Schools Real Estate Appraiser Board Exam ResultsjuancristoNo ratings yet
- Top 10 July 2012 Pharmacist Board Exam ResultsDocument1 pageTop 10 July 2012 Pharmacist Board Exam ResultsjuancristoNo ratings yet
- Performance of Schools June 2012 Environmental Planner Board Exam ResultsDocument2 pagesPerformance of Schools June 2012 Environmental Planner Board Exam ResultsjuancristoNo ratings yet
- June 2012 Nurse - Tuguegarao RM AssgnmentDocument80 pagesJune 2012 Nurse - Tuguegarao RM AssgnmentTheSummitExpressNo ratings yet
- June - July 2012 Nurse Licensure Examination Room Assignment (Pagadian City)Document50 pagesJune - July 2012 Nurse Licensure Examination Room Assignment (Pagadian City)jamieboyRNNo ratings yet
- Top 10 June 2012 Architect Board Exam ResultsDocument1 pageTop 10 June 2012 Architect Board Exam ResultsjuancristoNo ratings yet
- June - July 2012 Nurse Licensure Examination Room Assignment (CDO)Document112 pagesJune - July 2012 Nurse Licensure Examination Room Assignment (CDO)jamieboyRNNo ratings yet
- Beginner Levels of EnglishDocument4 pagesBeginner Levels of EnglishEduardoDiazNo ratings yet
- What Is A Business IdeaDocument9 pagesWhat Is A Business IdeaJhay CorpuzNo ratings yet
- JKSSB Panchayat Secretary Adfar NabiDocument3 pagesJKSSB Panchayat Secretary Adfar NabiSHEIKHXUNINo ratings yet
- ElectionDocument127 pagesElectionRaviKumar50% (2)
- Brand Zara GAP Forever 21 Mango H&M: Brand Study of Zara Nancys Sharma FD Bdes Batch 2 Sem 8 Brand-ZaraDocument2 pagesBrand Zara GAP Forever 21 Mango H&M: Brand Study of Zara Nancys Sharma FD Bdes Batch 2 Sem 8 Brand-ZaraNancy SharmaNo ratings yet
- Gender Religion and CasteDocument41 pagesGender Religion and CasteSamir MukherjeeNo ratings yet
- Impulsive Buying PDFDocument146 pagesImpulsive Buying PDFrukwavuNo ratings yet
- Remarkings AirportsDocument1 pageRemarkings AirportsJuan Jose CaleroNo ratings yet
- Speech VP SaraDocument2 pagesSpeech VP SaraStephanie Dawn MagallanesNo ratings yet
- Interpret Market Trends and Developments TASk 1Document7 pagesInterpret Market Trends and Developments TASk 1Raí SilveiraNo ratings yet
- Niper SyllabusDocument9 pagesNiper SyllabusdirghayuNo ratings yet
- Gallirei Weekend 2018Document7 pagesGallirei Weekend 2018Reiner Albert BraunNo ratings yet
- InvestMemo TemplateDocument6 pagesInvestMemo TemplatealiranagNo ratings yet
- World War I Almanac Almanacs of American WarsDocument561 pagesWorld War I Almanac Almanacs of American WarsMatheus Benedito100% (1)
- E-Gift Shopper - Proposal - TemplateDocument67 pagesE-Gift Shopper - Proposal - TemplatetatsuNo ratings yet
- مذكرة التأسيس الرائعة لغة انجليزية للمبتدئين?Document21 pagesمذكرة التأسيس الرائعة لغة انجليزية للمبتدئين?Manar SwaidanNo ratings yet
- IC HDL Lab ManualDocument82 pagesIC HDL Lab ManualRakshitha AngelNo ratings yet
- Meditation On God's WordDocument26 pagesMeditation On God's WordBeghin BoseNo ratings yet
- The Concepts and Principles of Equity and HealthDocument18 pagesThe Concepts and Principles of Equity and HealthPaulo César López BarrientosNo ratings yet
- MahayanaDocument26 pagesMahayanaAleza Menorca100% (1)
- 02 - Nature and Role of Science in SocietyDocument10 pages02 - Nature and Role of Science in SocietyMarcos Jose AveNo ratings yet
- Admin Circular 12-Service of SummonsDocument1 pageAdmin Circular 12-Service of SummonsbbysheNo ratings yet
- USA V Rowland - Opposition To Motion To End Probation EarlyDocument12 pagesUSA V Rowland - Opposition To Motion To End Probation EarlyFOX 61 WebstaffNo ratings yet
- Aswini Expert SystemsDocument37 pagesAswini Expert SystemsKarishma Satheesh KumarNo ratings yet
- Rule Against Multiplicity and Child PornoDocument3 pagesRule Against Multiplicity and Child PornoHouston Criminal Lawyer John T. FloydNo ratings yet
- Effect of Boron Content On Hot Ductility and Hot Cracking TIG 316L SSDocument10 pagesEffect of Boron Content On Hot Ductility and Hot Cracking TIG 316L SSafnene1No ratings yet
- Brent Berlin-Covert Categories and Folk TaxonomyDocument10 pagesBrent Berlin-Covert Categories and Folk TaxonomyKawita ChuachengNo ratings yet
- Florida Firearm Bill of SaleDocument4 pagesFlorida Firearm Bill of SaleGeemoNo ratings yet
- Short Tutorial On Recurrence RelationsDocument13 pagesShort Tutorial On Recurrence RelationsAbdulfattah HusseinNo ratings yet
- Chapter 7: Identifying and Understanding ConsumersDocument3 pagesChapter 7: Identifying and Understanding ConsumersDyla RafarNo ratings yet