Professional Documents
Culture Documents
Causative Agents Causative Agents: Headache, Myalgia, & Nausea Are Added S/SX For Streptococcal Pharyngitis
Uploaded by
Don Chiaw ManongdoOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Causative Agents Causative Agents: Headache, Myalgia, & Nausea Are Added S/SX For Streptococcal Pharyngitis
Uploaded by
Don Chiaw ManongdoCopyright:
Available Formats
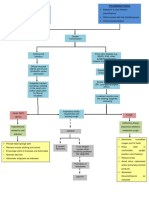
ACUTE PHARYNGITIS Description: - A sudden painful inflammation of the pharynx, the back portion of the throat that includes
the posterior third of the tongue, soft palate, and tonsils. - commonly known as SORE THROAT. Incidence: - Increased during winter and early spring. Pathophysiology: VIRAL (most cases) PREDISPOSING FACTORS - Exposure to viral agents - Poorly ventilated rooms CAUSATIVE AGENTS Adenovirus, influenza virus, Epstein-Barr virus, Herpes simplex virus BACTERIAL (10%) PREDISPOSING FACTORS - Bacterial upper respiratory tract infections
CAUSATIVE AGENTS GABHS, Group A Streptococcus (GAS) or Streptococcus pharyngitis Others: Mycoplasma pneumoniae Neisseria gonorrhoeae, H. influenzae Type B Enters into the system by way of droplets of coughs and sneezes and unclean hands that have been exposed to the contaminated fluids Lodges in the pharynx and initiates an inflammatory response
Pain
Fever Malaise Enlarged and tender (High) cervical lymph nodes
Vasodilation Edema
Tissue damage
Note: Painful sore throat (1-5 days), headache, myalgia, & nausea are added S/Sx for streptococcal pharyngitis.
(Fiery-red) Redness and swelling of the tonsillar pillars, uvula and soft palate (may demonstrate petechiae of the roof of the mouth Formation of creamy exudate in the tonsillar pillars (white-purple exudate)
If untreated COMPLICATIONS:
Common: Sinusitis, Otitis media Bad breathe Peritonsillar abscess, Mastoiditis, Cervical adenitis Rare: Bacteremia, Pneumonia, Meningitis, Rheumatic fever, Nephritis
CHRONIC PHARYNGITIS Description: - Is a persistent inflammation of the pharynx Pathophysiology: Risk factors: Working in dusty surroundings Excessive use of voice Chronic cough Habitual use of alcohol and tobacco General thickening and congestion Of the pharyngeal mucous membrane If it remains untreated and progresses, The membrane becomes thin, whitish, glistening, and at times wrinkled Swollen lymph follicles becomes numerous in the pharyngeal wall
RECURRING INFLAMMATION OF THE PHARYNX
Hypertrophic
Atrophic
Chronic granular clergymans sore throat
constant sense of irritation or fullness in the throat inflam-
mucus collects in the throat (can be expelled by coughing)
difficulty swallowing
intermittent postnasal drip causing minor irritation and mation of the pharynx
TONSILITIS AND ADENOIDITIS Description: - Inflammation of the tonsils and adenoids, often thought as a childhood disorder, but can occur in adults. Pathophysiology: Risk factors: - Alcohol use, smoking, splenectomy, weakened immune system (DM, Chemotherapy, etc.), sinusitis, exposure to someone with tonsillitis. CAUSES: Bacteria GABHS Virus Epstein-Barr virus (90% in adults affected) and Cytomegalovirus
Entry into the system (tonsils and adenoids) and multiplies Inflammatory process sets-in ENLARGED Tonsils Sore throat Fever Snoring Difficulty swallowing Adenoids Mouth-breathing Earache Draining ears Frequent head colds Noisy respiration Fills the space behind the posterior nares Nasal obstruction
If untreated: Complications Infection extends to the middle ears Acute otitis media Rupture of tympanic membrane Deafness Infection extends to the mastoid cells Mastoiditis
PERITONSILLAR ABSCESS Description: - Also known as quincy, a common major suppurative complication of sore throat. Pathophysiology: GABHS Sore throat (an acute tonsillar infection) (as a consequence of previous infections of the tonsils, adenoids, etc.) If untreated: Complications Infection spreads causing the collection of purulent exudate between the tonsillar capsule and the surrounding tissues and soft palate severe sore throat fever raspy voice inflammation of the superior constrictor muscle of the pharynx (severe sensation of burning, squeezing pain while swallowing) Odynophagia Enlarged and tender cervical lymph nodes
inflammation of the medial ptyregoid muscle
pain
spasm
difficulty swallowing (dysphagia) Drooling local cellulitis and abscess formation spreads over the palate, the neck and chest Edema in the palate, neck and chest Respiratory arrest
trismus (inability to open mouth)
pain on lateral head movement
Infection may spread and may cause Mediastinitis, intracranial abscess, Empyemas Further spread of infection
Death
Systemic infection
LARYNGITIS Description: - Inflammation of the larynx. Incidence: - Common during winter (viral laryngitis) Pathophysiology Risk factors: - Voice abuse - Exposure to dust, chemicals, smoke or other pollutants - Upper respiratory infection (allergic rhinitis and pharyngitis) - Infection of the vocal cords - Gastroesophageal reflux (Reflux laryngitis) Predisposing factors: - Exposure to sudden changes in temperature - Dietary deficiencies - Malnutrition - Immunosuppressed state
Causes: - Causative agents for common colds and pharyngitis (bacteria and virus-common cause) Presence of predisposing and risk factors Entry of causative agents Inflammation and infection of the larynx ACUTE Laryngitis Hoarseness of voice or Aphonia (complete loss of voice) Severe cough and dry sore throat Sudden onset made worse by cold dry wind Throat feels tickle in the worst in throat made morning and worse by cold improves when air/liquids in a warmer climate uvula is visibly edematous (if with allergies)
CHRONIC Laryngitis Persistent hoarseness
OBSTRUCTION AND TRAUMA OF THE UPPER RESPIRATORY AIRWAY OBSTRUCTION DURING SLEEP Obstructive Sleep Apnea (OSA) Description: - Is a disorder characterized by recurrent episodes of upper airway obstruction and a reduction in ventilation. - Cessation of breathing (apnea) during sleep usually caused by repetitive upper airway obstruction. Pathophysiology: Risk factors: - Obesity - Male gender - Post-menopausal status - Advanced age - Alterations in the airway (structural changes like tonsillar hypertrophy, abnormal posterior positioning of one or both jaws, and variations in craniofacial structures) that contribute to the collapsibility of the upper airways.
Normally the pharynx is a collapsible tube that can be compressed And during sleep the muscles of the upper airway is reduced Presence of risk factors Reduction in the diameter of the upper airway Obstruction Frequent and loud snoring with breathing cessation for 10 secs or long (5 episodes/hour) Snorting Gasping Choking Apneic episodes reported by the partner Sudden awakening Chronic fatigue Insomnia and difficulty going to sleep DEATH Apnea Hypoxia and hypercapnia Sympathetic response Hypertension Increased risk for MI and Stroke Dysrhythmias in clients with CVD Small amounts of negative pressure are generated during inspiration Upper airway collapse
Hypersomnolence Early morning awakenings (Daytime sleepiness) with an inability to go back to sleep EPISTAXIS Description: - Also known as nosebleed - a hemorrhage from the nose, is caused by the rupture of tiny, distended vessels in the mucous membrane of any area of the nose. Pathophysiology: Risk factors: - Local infections (vestibulitis, rhinitis, sinusitis) - Systemic infections (scarlet fever, malaria) - Drying of nasal mucous membrane - Nasal inhalation of illicit drugs (cocaine) - Trauma (picking the nose, blunt trauma, (fracture, forceful nose blowing) - Arteriosoclerosis - Tumor (sinus or nsapharynx) - Thrombocytopenia - Use of aspirin - Liver disease - Redu-Osler-Weber syndrome (hereditary hemorrhagic telengiectasia) - Hypertension
Presence of any of the risk factors Rupture of any of the following Anterior ethmoidal artery On the forward part of the roof sphenopalatine artery in the posterosuperior region Bleeding NASAL OBSTRUCTION Description: - Obstruction of the nose Pathophysiology: Causes: - Deviation of nasal septum - Hypertrophy of the turbinate bones - Pressure of nasal polyps Obstruction of the nose Difficulty in maintaining an adequate airway Breathing through Sleep deprivation Nasopharyngitis Infection extends to the nasal sinuses Rhinosinusitis internal maxillary branches
the mouth Drainage is obstructed Dryness of the oral mucosa and persistent, dry, cracked lips FRACTURE OF THE NOSE - Is the break in the continuity of the nasal bone. Pathophysiology: Cause: Direct assault on the nose Tearing of the mucous membrane Rupture of blood vessels Trauma to the nasal area Hematoma Break in the continuity of nasal bone Fracture Pain
Nose bleeding Complications: Infection Abscess Avascular or septic necrosis
LARYNGEAL OBSTRUCTION Description: - Obstruction of the larynx Pathophysiology: Precipitating factors: History of allergies, exposure to medications, latex, foods, and bee stings Foreign bodies Heavy alcohol consumption; heavy tobacco use Family history of airway problems Use of ACE-inhibitors Recent throat pain or Recent fever History of surgery or Previous tracheostomy History of nasogastric tube placement anaphylaxis lodges into the larynx causes tumor angioedema angioedema of mucous membranes infectious process subglottic stenosis nasogastric tube syndrome Laryngeal Obstruction Closes off the opening in the larynx Air passage is compromised during inspiration and expiration Lowered oxygen saturation Use of accessory muscles of respiration Retractions in the neck or abdomen during inspirations Respiratory arrest Death edema of larynx
Client may faint or collapse
CANCER OF THE LARYNX Description: Pathophysiology: Etiology of cancer is unknown.
Risk Factors: CARCINOGENS: - Tobacco (smoke or smokeless) - Combined effects of alcohol and tobacco - Asbestos - Secondhand smoke - Paint fumes - Wood dust - Cement dust - Chemicals - Tar products - Mustard gas - Leather and metals OTHER FACTORS: - Straining the voice - Chronic laryngitis - Nutritional deficiencies (riboflavin) - History of alcohol abuse - Familial predisposition - Age (higher incidence after 60 yo) - Gender (more common in men) - Race (more prevalent-African Americans) - Weakened immune system
Failure of the regulatory mechanism of normal cells and growth continues in excess Neoplasia Benign Malignant Uncontrolled growth of cells or cell division Tumor Because malignant cells are not encapsulated Expands into surrounding tissues (Invasion) Lump in the neck Impedes the action of Lack of adhesion and loss of contact inhibition Spreads to distant parts of the body (Metastasis) - Cervical lymph adenopathy
the vocal cords
- Unintentional weight loss - A general debilitated state - Pain radiating to the ear
- Hoarseness (harsh, raspy and low in pitch voice) - Persistent cough or sore throat - Pain and burning in the throat when consuming hot liquids or citrus juices Late symptoms: - Dysphagia - Dyspnea - Persistent hoarseness - Persistent ulceration - Unilateral nasal obstruction/discharge - Foul breath
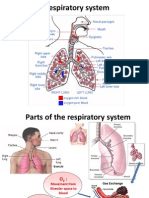
ATELECTASIS Description: - Refers to closure or collapse of alveoli and often described in relation to x-ray findings and clinical signs and symptoms. Pathophysiology: Causes: -Altered breathing patterns -Alterations in small airway functions -Reduced lung volumes due to musculoskeletal or neurologic disorders -Retained secretions -Prolonged supine positioning -Restrictive defects -Pain -Increased abdominal pressure -Specific surgical procedures (i.e. upper abdominal, thoracic or open heart surgery)
Reduced ventilation or blockage that obstructs passage of air to and from the alveoli Alveolar air becomes trapped Trapped air is absorbed into the bloodstream No additional air can enter into the alveoli Patchy infiltrates/consolidated areas in the lungs in the x-ray Alveoli collapse Predisposes to infection Pulmonary infection Hypoxemia Respiratory distress - Tachycardia - Tachypnea - Pleural pain - Central cyanosis - Anxious Acute Respiratory failure Dyspnea Cough Sputum production
Death
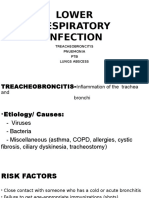
RESPIRATORY INFECTIONS Acute Tracheobronchitis Description: - An acute inflammation of the mucous membranes of the trachea and the bronchial tree of, often follows infection of the upper respiratory tract. Pathophysiology: Causes: Streptococcus pneumoniae Haemophilus influenzae Mycoplasma pneumoniae Fungal infection (Aspergillus)
Enters into the system and initiates inflammatory process Inflammation of the mucosa of trachea and bronchi Dry and irritating cough sternal soreness Expectoration of scanty amount of mucoid spututm As infection progresses Shortness of breath Inspiratory stridor Expiratory wheezes Expectoration of purulent sputum Irritation of the mucosa of airways Blood-streaked secretions Production of mucopurulent sputum - Fever - Chills - Night sweats - Headache - Body malaise
SEVERE ACUTE RESPIRATORY SYNDROME Description: Pathophysiology Predisposing factors: - Living or traveling in places with SARS cases - Close contact with infected people CAUSE Corona virus CAUSE through respiratory droplets which either lodges on mouth, nose, or eyes) touching contaminated objects or surface and then touching ones mucous membranes
Incubation period (2-7 days) Enters into the system and multiplies Inflammatory process sets in (symptoms appear within 10 days) Fever greater that 38 Celcius Cough Difficulty breathing
Poor prognosis if accompanied with the following factors: - Old age - Comorbid condition (DM, COPD and Chronic Hep B) - Atypical symptoms - Elevated serum lactate dehydrogenase on admission - Acute renal failure
PULMONARY TUBERCULOSIS Description:
LUNG ABSCESS Description:
PLEURAL CONDITIONS Description : - Are disorders that involve the membranes covering the lungs (visceral pleura) and the surface of the chest wall (parietal pleura) or disorders affecting the pleural space. PLEURISY Description: - also known as pleuritis, is the inflammation of both layers of the pleurae (parietal and visceral) which is in conjunction with other disorders of the respiratory system. Pathophysiology: Pneumonia Collagen disease After thoracotomy URTI Trauma to the chest Tuberculosis Pulmonary infarction or embolism Primary or metastatic cancer
Inflammation of the parietal and visceral pleura With respiration Rubbing of the two pleural membranes Pleural friction rub upon auscultation (early stage)
Stimulation of the nerve endings on the parietal pleura Severe, sharp, knifelike pain (pleuritic pain) which worsens when taking a deep breath, coughing, or sneezing (usually one sided and becomes absent or minimized when the breath is held)
PLEURAL EFFUSION Description: - a collection of fluid in the pleural space, is rarely a primary disease, usually a secondary to other diseases. Pathophysiology: Causes: (pre-existing conditions) Heart failure
Tuberculosis Pulmonary infections Neoplastic tumors (bronchogenic carcinoma) Pneumonia
Pulmonary infection (viral) Pulmonary embolus Nephrotic syndrome Connective tissue disease
Causing an imbalance in the hydrostatic pressure and oncotic pressure in the lungs Formation and reabsorption of pleural fluid is altered
Inflammation by bacterial products or tumors of the pleural surfaces Extravasation of fluid into tissues or cavity
Effusion of clear fluid Transudate (Meaning pleural membranes are not diseased) Exudate
Decreased/Absent breath sounds Decreased fremitus Dull, flat sound on percussion Small effusion - minimal or no dyspnea Large effusion - Dyspnea (shortness of breath SOB) Malignant effusion - Dyspnea - Difficulty lying flat - Coughing
Acute respiratory distress Tracheal deviation away from the affected side
Note: Signs and symptoms are dependent on the size of effusion, speed of formation, and underlying lung disease (eg. If the cause of the effusion is pneumonia, the client will also exhibit signs and symptoms of pneumonia). EMPYEMA Description: - Is an accumulation of thick, purulent fluid within the pleural space, often with fibrin development and a loculated (walled-off) area where infection is located. Pathohpysiology: Causes: Common cause: As a complication of Bacterial Pneumonia or Lung abscess Other causes: Penetrating chest trauma Hematogenous infection of the pleural space Nonbacterial infections Iatrogenic causes (after thoracic surgery or thoracentesis)
Initial Stage Progression Fibropurulent stage
Pleural fluid is thin
Low leukocyte count
Thick exudative membrane encloses the lung (loculated empyema) Fever Night sweats Pleural pain Cough Dyspnea Anorexia Weight loss
-Decreased or absent breath over the affected area -Decreased fremitus -Dullness on chest percussion
http://nurseslabs.com/pathophysiology/bronchitis-pathophysiology/ http://nurseslabs.com/pathophysiology/chronic-obstructive-pulmonary-disease-copdpathophysiology/
You might also like
- Management of Tuberculosis: A guide for clinicians (eBook edition)From EverandManagement of Tuberculosis: A guide for clinicians (eBook edition)No ratings yet
- Electrolyte Imbalance 1Document3 pagesElectrolyte Imbalance 1Marius Clifford BilledoNo ratings yet
- Community Acquired Pneumonia, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandCommunity Acquired Pneumonia, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- BFCDocument8 pagesBFCIrene GunongNo ratings yet
- PHARYNGITISDocument8 pagesPHARYNGITISWàrìs Ràfìqùé ßàlòçhNo ratings yet
- Pathophysiology of PharyngitisDocument1 pagePathophysiology of PharyngitisKRISTINE BULACAN100% (1)
- Drug Study Pyrantel & CefuroximeDocument2 pagesDrug Study Pyrantel & CefuroximeMikhael Briones ApasNo ratings yet
- Schematic Diagram BA HAP HRDocument2 pagesSchematic Diagram BA HAP HRMika MinsalanNo ratings yet
- Pathophysiology of TuberculosisDocument2 pagesPathophysiology of TuberculosisLeikkaNo ratings yet
- Case PresDocument5 pagesCase PresBeverlyNo ratings yet
- Management of Patients With Oral and Esophageal DisordersDocument14 pagesManagement of Patients With Oral and Esophageal Disordersintotheunknown100% (2)
- Pathophysiology Diagram of Asthma PDFDocument2 pagesPathophysiology Diagram of Asthma PDFYhenlee Rhizelle MarquezNo ratings yet
- Pathophysiology SARSDocument4 pagesPathophysiology SARSStephanie Joy Escala71% (7)
- Urinary Incontinence Nursing ManagementDocument3 pagesUrinary Incontinence Nursing ManagementRnspeakcomNo ratings yet
- Pathognomonic Signs of Communicable Diseases: JJ8009 Health & NutritionDocument2 pagesPathognomonic Signs of Communicable Diseases: JJ8009 Health & NutritionMauliza Resky NisaNo ratings yet
- Acute Bronchitis PathoDocument3 pagesAcute Bronchitis Pathobanyenye25No ratings yet
- Pathophysiology of PneumoniaDocument1 pagePathophysiology of Pneumoniaoxidalaj97% (31)
- Patho PneumoniaDocument2 pagesPatho Pneumoniaailyne_galicia100% (2)
- Nasal PolypsDocument20 pagesNasal PolypsPauleenNo ratings yet
- Pathophysiology of Atrial Septal DefectDocument2 pagesPathophysiology of Atrial Septal Defectbobtaguba50% (2)
- Sample Only Nso - Tracheostomy CareDocument5 pagesSample Only Nso - Tracheostomy CareNader Abdurasad100% (1)
- Pathophysiology of Koch's Disease (Tuberculosis) : Primary InfectionDocument2 pagesPathophysiology of Koch's Disease (Tuberculosis) : Primary InfectionStephanie GapuzNo ratings yet
- Pathophysiology Flow Chart of BronchiectasisDocument2 pagesPathophysiology Flow Chart of BronchiectasisEsmareldah Henry SirueNo ratings yet
- Pathophysiology of Tuberculosis: Group 5 Latosa, Selene Lee, Guk Lim, Johanna Magalona, Stephen Mendoza, ColeenDocument22 pagesPathophysiology of Tuberculosis: Group 5 Latosa, Selene Lee, Guk Lim, Johanna Magalona, Stephen Mendoza, ColeenAlexander Santiago ParelNo ratings yet
- PneumoniaDocument17 pagesPneumoniajustin_saneNo ratings yet
- Teaching Plan PneumoniaDocument4 pagesTeaching Plan PneumoniadeannesemonNo ratings yet
- Discharge Planning PaperDocument5 pagesDischarge Planning Paperapi-283173905No ratings yet
- NCM 112: Care of Client With Inflammatory and Immunologic ResponseDocument10 pagesNCM 112: Care of Client With Inflammatory and Immunologic ResponseNikitaCaitlynLeyaleyNo ratings yet
- Asthma Nanda DiagnosesDocument4 pagesAsthma Nanda DiagnosesZinya RobinsonNo ratings yet
- AmbroxolDocument1 pageAmbroxolPrecious CarmelaNo ratings yet
- Pathophysiology of PneumoniaDocument4 pagesPathophysiology of PneumoniamatrixtrinityNo ratings yet
- Baby Kiran Aged 7 Years Brought To The Emergency Opd Accomp: ScenarioDocument22 pagesBaby Kiran Aged 7 Years Brought To The Emergency Opd Accomp: ScenariobhavanaNo ratings yet
- Drug Study Pedia WardDocument2 pagesDrug Study Pedia WardCayanne ChuaNo ratings yet
- Amoebiasis PathophysiologyDocument3 pagesAmoebiasis PathophysiologyApril CornejoNo ratings yet
- LaryngitisDocument40 pagesLaryngitisMikhail Guidicelli100% (1)
- Case Study of Community Acquired PneumoniaDocument14 pagesCase Study of Community Acquired PneumoniaRachelNo ratings yet
- De Sagun, Leila Camille, A. NCMB312-RLE BSN3Y1-1B Course Task #1Document1 pageDe Sagun, Leila Camille, A. NCMB312-RLE BSN3Y1-1B Course Task #1Carl SantosNo ratings yet
- Copd PathoDocument2 pagesCopd PathoAlvin RamirezNo ratings yet
- CROUP Concept MapDocument3 pagesCROUP Concept Mapingrid50% (2)
- USC Case 04 - SinusitisDocument9 pagesUSC Case 04 - SinusitisDisti Damelia SebayangNo ratings yet
- Pathophysiology of Hansen's DiseaseDocument1 pagePathophysiology of Hansen's DiseaseGrace Lyn Borres ImpasNo ratings yet
- Pneumonia PathoDocument2 pagesPneumonia PathoDerick Nyl PascualNo ratings yet
- Pathophysiology On DementiaDocument2 pagesPathophysiology On Dementiaiamjulzcurtis50% (2)
- Seizure PathophysiologyDocument2 pagesSeizure PathophysiologyqwertyuiopNo ratings yet
- Book-Based: Pathophysiology of Allergic RhinitisDocument2 pagesBook-Based: Pathophysiology of Allergic RhinitisJeraldine Corpuz PascualNo ratings yet
- Predisposing Factors Age Diet Dehydration Precipitating Factors Family or Personal History Digestive Diseases and SurgeryDocument2 pagesPredisposing Factors Age Diet Dehydration Precipitating Factors Family or Personal History Digestive Diseases and SurgeryChloé Jane HilarioNo ratings yet
- Pathophysiology With Anatomy and PhysiologyDocument3 pagesPathophysiology With Anatomy and PhysiologyKaloy KamaoNo ratings yet
- Pathophysiology of Syphilis & GonorrheaDocument14 pagesPathophysiology of Syphilis & GonorrheasourabhNo ratings yet
- Assessment and Management of Patients With Hearing and Balance Disorders WebDocument36 pagesAssessment and Management of Patients With Hearing and Balance Disorders WebStephKirstin Velasco Malapit100% (2)
- ABRUPTIO PLACENTAE PathophysiologyDocument3 pagesABRUPTIO PLACENTAE PathophysiologyBarda GulanNo ratings yet
- 2013 ENDOCRINE PHARMACOLOGY Word Notes PDFDocument52 pages2013 ENDOCRINE PHARMACOLOGY Word Notes PDFNicole Opao100% (4)
- PBL Copd: 1) Mechanics of RespirationDocument34 pagesPBL Copd: 1) Mechanics of RespirationAhmadNo ratings yet
- Pathophysiology of Bronchial AsthmaDocument2 pagesPathophysiology of Bronchial AsthmaFirenze Fil100% (21)
- Kristia Carpio Pulmonary TuberculosisDocument31 pagesKristia Carpio Pulmonary TuberculosiskisNo ratings yet
- Concept Map AsthmaDocument4 pagesConcept Map AsthmaAstrid Moreno De LeonNo ratings yet
- Pathophysiology VolvulusDocument2 pagesPathophysiology VolvulusHyacinth Bueser Bondad0% (2)
- Dental Prob NCPDocument3 pagesDental Prob NCPx483xDNo ratings yet
- Pharyngeal Symptoms Acute &chronic Pharyngitits: Submitted By, Aravind RajanDocument11 pagesPharyngeal Symptoms Acute &chronic Pharyngitits: Submitted By, Aravind RajanVictor EnachiNo ratings yet
- Laringitis Akut Dan KronisDocument37 pagesLaringitis Akut Dan KronisMonika AyuningrumNo ratings yet
- Common Diseases of PharynxDocument72 pagesCommon Diseases of PharynxPinak DeNo ratings yet
- References: Some More Basic Reference Page RulesDocument13 pagesReferences: Some More Basic Reference Page RulesDon Chiaw ManongdoNo ratings yet
- History of Total Quality ManagementDocument3 pagesHistory of Total Quality ManagementDon Chiaw ManongdoNo ratings yet
- Health Information ManagementDocument29 pagesHealth Information ManagementDon Chiaw Manongdo100% (1)
- EMRsDocument2 pagesEMRsDon Chiaw ManongdoNo ratings yet
- Capstone Project FormatDocument6 pagesCapstone Project FormatDon Chiaw ManongdoNo ratings yet
- Preferences For Health Information and Decision-Making: Development of The Health Information Wants (HIW) QuestionnaireDocument9 pagesPreferences For Health Information and Decision-Making: Development of The Health Information Wants (HIW) QuestionnaireDon Chiaw ManongdoNo ratings yet
- UNIT II NotesDocument10 pagesUNIT II NotesDon Chiaw ManongdoNo ratings yet
- Design Thinking Learning ToolDocument2 pagesDesign Thinking Learning ToolDon Chiaw ManongdoNo ratings yet
- IMRADDocument2 pagesIMRADDon Chiaw ManongdoNo ratings yet
- Reflections On Theory DevelopmentDocument3 pagesReflections On Theory DevelopmentDon Chiaw ManongdoNo ratings yet
- The Health Promotion ModelDocument8 pagesThe Health Promotion ModelDon Chiaw Manongdo100% (1)
- Case Study ResearchDocument8 pagesCase Study ResearchDon Chiaw ManongdoNo ratings yet
- Health Promotion Model By: Nola J. Pender: Presented By: Mila MaruyaDocument24 pagesHealth Promotion Model By: Nola J. Pender: Presented By: Mila MaruyaDon Chiaw Manongdo100% (1)
- Filipino TheoristsDocument55 pagesFilipino TheoristsDon Chiaw Manongdo100% (5)
- Uv-Irb Pocedure Flowrevised 81417Document11 pagesUv-Irb Pocedure Flowrevised 81417Don Chiaw ManongdoNo ratings yet
- Notes On PhenomenologyDocument5 pagesNotes On PhenomenologyDon Chiaw ManongdoNo ratings yet
- Review of Resubmitted Study Protocol FormDocument1 pageReview of Resubmitted Study Protocol FormDon Chiaw ManongdoNo ratings yet
- Patient SatisfactionDocument6 pagesPatient SatisfactionDon Chiaw ManongdoNo ratings yet
- Related LiteratureDocument22 pagesRelated LiteratureDon Chiaw ManongdoNo ratings yet
- Remodelling of Nola PenderDocument5 pagesRemodelling of Nola PenderDon Chiaw ManongdoNo ratings yet
- Data Privacy ActDocument8 pagesData Privacy ActDon Chiaw ManongdoNo ratings yet
- Telephonic Nursing Care Delivery ModelDocument2 pagesTelephonic Nursing Care Delivery ModelDon Chiaw ManongdoNo ratings yet
- The Healthy Lifestyle and Personal Control QuestionnaireDocument28 pagesThe Healthy Lifestyle and Personal Control QuestionnaireDon Chiaw Manongdo50% (2)
- Standing Strong in Stress - IndexDocument46 pagesStanding Strong in Stress - IndexDon Chiaw ManongdoNo ratings yet
- Workoverload and StressDocument8 pagesWorkoverload and StressDon Chiaw ManongdoNo ratings yet
- Conflict Management QuestionnaireDocument2 pagesConflict Management QuestionnaireDon Chiaw Manongdo100% (1)
- BronchiectasisDocument25 pagesBronchiectasisDewi PermatasariNo ratings yet
- Patient Assessment and Electrocardiogram: Clinical Case PresentationDocument7 pagesPatient Assessment and Electrocardiogram: Clinical Case PresentationLezahnor CasibangNo ratings yet
- Bhavna KatejaDocument2 pagesBhavna KatejaShahabaz UbaiseNo ratings yet
- BronchiolitisDocument9 pagesBronchiolitisMahmoud FathallaNo ratings yet
- Jurnal Pneumonia AnalisaDocument4 pagesJurnal Pneumonia AnalisaMulyasari LindaNo ratings yet
- IM Concept Map SGD Group 13, Fever and CoughDocument4 pagesIM Concept Map SGD Group 13, Fever and Coughb8gjhmq6rrNo ratings yet
- RespiratoryDocument17 pagesRespiratorykurutalaNo ratings yet
- Presentation Outline Nursing Pulmonary Tuberculosis Revised 1Document10 pagesPresentation Outline Nursing Pulmonary Tuberculosis Revised 1Alfaera Rahma FarestyNo ratings yet
- Ventilator Associated PneumoniaDocument2 pagesVentilator Associated PneumoniaMuzana DariseNo ratings yet
- Pediatric Community-Acquired PneumoniaDocument60 pagesPediatric Community-Acquired PneumoniaIkea Balhon100% (1)
- Nadra VaccineDocument1 pageNadra Vaccineaskari PhotocopyNo ratings yet
- A Child Is Gasping For Breath But Has A Pulse Rate of 100 Per MinuteDocument2 pagesA Child Is Gasping For Breath But Has A Pulse Rate of 100 Per Minuteferri100% (1)
- RS7 InfluenzaDocument6 pagesRS7 InfluenzaGabriella ChafrinaNo ratings yet
- Rencana Pending Bulan OktoberDocument9 pagesRencana Pending Bulan OktoberThey'Were Gethey Ryan SanjayaNo ratings yet
- Lower Respiratory InfectionDocument71 pagesLower Respiratory Infectionpaulyn ramos100% (1)
- Tonsillitis and Adenoiditis: Islamic University Nursing CollegeDocument15 pagesTonsillitis and Adenoiditis: Islamic University Nursing CollegeNinaNo ratings yet
- NCP Bronchila Ashma Dra.Document3 pagesNCP Bronchila Ashma Dra.ЯicaЯdo BautistaNo ratings yet
- Sample of Essay - The FluDocument2 pagesSample of Essay - The FluMerisa WahyuningtiyasNo ratings yet
- End Blok Respi SoalDocument6 pagesEnd Blok Respi Soalanz_4191No ratings yet
- Sakit NovDocument126 pagesSakit NovArda SenjayaNo ratings yet
- Risk For AspirationDocument2 pagesRisk For AspirationGly Mtg100% (6)
- Respiratory System SummaryDocument6 pagesRespiratory System SummaryKiara GovenderNo ratings yet
- Harrison ManuallDocument105 pagesHarrison Manuallale maril100% (1)
- Laporan Registrasi Pasien by ShiftDocument8 pagesLaporan Registrasi Pasien by ShiftDewi DayuntariNo ratings yet
- Communicable Disease QuizDocument2 pagesCommunicable Disease QuizPlacida Mequiabas National High SchoolNo ratings yet
- McqsDocument6 pagesMcqsPinkymekala HasanparthyNo ratings yet
- Country Vaccinations by Manufacturer EditedDocument373 pagesCountry Vaccinations by Manufacturer EditedFriansyahNo ratings yet
- Asthma - FactsDocument24 pagesAsthma - Factsvsvp100No ratings yet
- SuctioningDocument17 pagesSuctioningKandi Issaya100% (1)
- Weekly Influenza Surveillance Update 2020-2021 From The Rhode Island Department of Health.Document29 pagesWeekly Influenza Surveillance Update 2020-2021 From The Rhode Island Department of Health.Frank MaradiagaNo ratings yet
- Love Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)From EverandLove Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)Rating: 3 out of 5 stars3/5 (1)
- ADHD is Awesome: A Guide to (Mostly) Thriving with ADHDFrom EverandADHD is Awesome: A Guide to (Mostly) Thriving with ADHDRating: 5 out of 5 stars5/5 (2)
- The Age of Magical Overthinking: Notes on Modern IrrationalityFrom EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityRating: 4 out of 5 stars4/5 (29)
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionFrom EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionRating: 4 out of 5 stars4/5 (404)
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsFrom EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsNo ratings yet
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedFrom EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedRating: 5 out of 5 stars5/5 (81)
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeFrom EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeRating: 2 out of 5 stars2/5 (1)
- Mindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessFrom EverandMindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessRating: 4.5 out of 5 stars4.5/5 (328)
- The Obesity Code: Unlocking the Secrets of Weight LossFrom EverandThe Obesity Code: Unlocking the Secrets of Weight LossRating: 4 out of 5 stars4/5 (6)
- The Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaFrom EverandThe Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaRating: 4.5 out of 5 stars4.5/5 (266)
- Summary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisFrom EverandSummary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisRating: 4.5 out of 5 stars4.5/5 (42)
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsFrom EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsRating: 4 out of 5 stars4/5 (4)
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsFrom EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsRating: 5 out of 5 stars5/5 (1)
- The Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeFrom EverandThe Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeRating: 4.5 out of 5 stars4.5/5 (253)
- Dark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.From EverandDark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Rating: 4.5 out of 5 stars4.5/5 (110)
- Why We Die: The New Science of Aging and the Quest for ImmortalityFrom EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityRating: 4 out of 5 stars4/5 (5)
- Outlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisFrom EverandOutlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisRating: 4 out of 5 stars4/5 (1)
- Cult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryFrom EverandCult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryRating: 4 out of 5 stars4/5 (45)
- Raising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsFrom EverandRaising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsRating: 4.5 out of 5 stars4.5/5 (170)
- Summary: Thinking, Fast and Slow: by Daniel Kahneman: Key Takeaways, Summary & Analysis IncludedFrom EverandSummary: Thinking, Fast and Slow: by Daniel Kahneman: Key Takeaways, Summary & Analysis IncludedRating: 4 out of 5 stars4/5 (61)
- Manipulation: The Ultimate Guide To Influence People with Persuasion, Mind Control and NLP With Highly Effective Manipulation TechniquesFrom EverandManipulation: The Ultimate Guide To Influence People with Persuasion, Mind Control and NLP With Highly Effective Manipulation TechniquesRating: 4.5 out of 5 stars4.5/5 (1412)
- How to ADHD: The Ultimate Guide and Strategies for Productivity and Well-BeingFrom EverandHow to ADHD: The Ultimate Guide and Strategies for Productivity and Well-BeingRating: 1 out of 5 stars1/5 (1)
- The Marshmallow Test: Mastering Self-ControlFrom EverandThe Marshmallow Test: Mastering Self-ControlRating: 4.5 out of 5 stars4.5/5 (59)