Professional Documents
Culture Documents
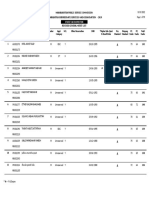
PE Summaries 26
Uploaded by
lj3472Original Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
PE Summaries 26
Uploaded by
lj3472Copyright:
Available Formats
PE Summaries 26/8 Definition of health: A state of complete physical, mental and social wellbeing and not merely the
absence of disease & infirmity. Dimensions of health: Physical, Social, Mental, Emotional & Spiritual Perceptions of health: How your health is perceived. Health continuum is how you measure your perception of your/someone elses health. Inequalities such as socioeconomic status and age can affect these perceptions. Australias perception of health is improving. Social construct: A concept that recognises that people have different views based on their social circumstances and ways of seeing, interpreting, interrelating and interacting with their environment. Impact of the media, peers & family on health: Media raises awareness of health, contributes to misconceptions, laws, heightens perceptions of health. Peers: Influences your idea/behaviours relating to health, influences decisions. Family: Role models of health, their perception of health is passed on, the way you were raised affects perception. Health behaviours of young people: The risk/healthy behaviours youths (12-26) partake in e.g. underage drinking, drugs. Health behaviours of youths has improved over time. Mortality rates decreased due to increased vaccination, safer environments for children. Decline in hospitalisation, improved cancer survival, increases in sporting activities, meeting standards for literacy. Rise in STIs, diabetes, mental disorders and motor vehicle accidents (MVAs). Indigenous people, people in rural areas and people with low SES suffer from significantly poorer health. The reason for these differences is access. Disadvantaged groups have less access to health services, nutritious food etc. Indigenous youths are 2x likely to die, 6x likely to be assaulted and 4x to commit suicide. 10x likely to get STIs, 6x to be a teenage mum, 7x to be in protective services, 15x to be in juvenile detention. Changes in lives of youths in AU: Social changes family types, more mothers in workforce, increased childcare usage. Tech advances: Impact on learning, social interactions. Further study and entering the workforce later, living at home longer. More growing up free from infectious diseases, surviving serious illnesses, increases in obesity, chronic disease, behavioural problems. Determinants of health: The factors that have a negative or positive influence on health at an individual or population level.
Individual determinants of health: Factors unique to each person that determine their health level, e.g. knowledge, skills, attitudes, genetics Socioeconomic determinants of health: Family, peers, media, religion, culture, education, employment, income, environment, geographical location Aboriginal culture: Large influence on health, morbidity/mortality higher, higher unemployment, rural, racism, poor nutrition, inadequate housing, lower education. Aboriginals that change to a western culture have better health. Ethnicity has been shown to be a determinant of the level of participation in sport, with different cultures being the lowest participants in sport. The problems with being rural: Bigger risk of cancer death due to treatments being many hundreds of kilometres away, long distance travel affects family relationships, physically draining Modifiable health determinants: Determinants that can be changed or controlled so they have a different influence on health. e.g. weight. Non-modifiable health determinants: Determinants of health that can not be changed, e.g. age. Individual & socioeconomic determinants: Low SES limits individual ability to buy healthy products. Can influence diet/exercise. Individual factors such as a positive attitude towards health can counter low SES. Low SES also results in low educational opportunities, which harms health status. Individual & environmental determinants: Difficult to manage. Lack of social networks due to geographic isolation, poor hygiene/household management, poor access to health services Individual & sociocultural determinants: Cultural background can have a positive or negative influence. For example, tobacco use is accepted in some cultures, attitudes to sex differ etc. Environmental & socioeconomic determinants: Affects ability to purchase health foods, health services etc., less education levels.
Health promotion: The process that enables people to gain or improve the control they have over their own health. Health promotion involves an individual or group being able to realise aspirations, satisfy needs and change with their environment. Health promotion makes it possible for people to increase control over their determinants of health and hereby improve their health. The world health organisation defines health promotion as the process of enabling people to increase control over their health and improve their health. This definition was incorporated into the Ottawa Charter for Health Promotion. Health promotion approaches & strategies example: Individual focused interventions e.g. posters, health promotion policy (Mental Health Strategy) Harm-minimisation approach: Accepts that some will engage in risktaking behaviour, but aims to reduce adverse health, social and economic consequences of these behaviours by limiting hazards. Zero tolerance approach: Usually associated w/ strict policy. Doesnt consider things like drug use to be a health issue, can lead to victimisation e.g. drug use > HIV Preventative medical approaches: Traditional approaches that regard health as an absence of illness. Public health approaches: Aim to provide max benefit for largest amount of people by preventing disease/injury, promoting health and returning health to communities. Key steps in these approaches include defining & monitoring the problems extent, IDing causes of problem, creating ways of treatment and widely applying treatments. Demand reduction: Encourages people not to use a drug/delay/reduce the use of a drug. Includes info/edu strategies, treatment programs and regulatory controls. Ottawa charter: A health promotion framework developed in 1986 in order to achieve Health For All By the Year 2000. Ottawa Charter has had considerable influence on AU laws, e.g. the Adelaide Declaration 1988. Health promotion supports personal & social development through providing info, education & life skills.
Body in Motion Skeletal system: 206 bones, 650 muscles, 200+ joints. Bones perform 5 main functions. Support, protection, movement, storage of minerals and formation of blood cells.
Major bones: Cranium (skull) sternum humerus (above elbow) scapula (shoulderblade) cervical vertebrae (1-7, from neck down) thoracic vertebrae (8-20, neck down), lumbar vertebrae (21-26) sacrum (in between coccyx & lumbar verts) & coccyx (tailbone) ribs ulna (below elbow, closer to body) radius (below elbow, away from body) pelvis femur (thigh bone) tibia (shin bone) fibula (smaller shinbone, behind tibia) patella (kneecap) tarsals (ankle to toes) metatarsals (tarsals to phalanges) phalanges (end digits, both toes & fingers) carpals (radius/ulna to metacarpals) metacarpals (carpals to phalanges)
Bones can be classified into five categories. Long bones are longer than they are wide, and work in hinge arrangement with other bones, e.g. humerus
Short bones tend to be box shaped, e.g. carpals Flat bones have a broad surface area and play a protective role, e.g. ribs Irregular bones that dont fit into the above three, e.g. vertebrae
Sesamoid bones are bones that are found where tendons pass over a joint, e.g. patella Ligaments: Fibrous bands that connect the articulating bones. Designed to assist stability in joint by restraining movement. Inelastic structure can result in permanent lengthening when overstretched Tendons: Tough inelastic cords of tissue that attach muscle to bone. Further strengthen joints by extending across them and assisting ligaments to hold joints closed. Synovial fluid: Acts as a lubricant, a cushion for blows, provides nutrition for cartilage, carries waste. Amount produced depends on physical activity level, type of joint. Its pumped into the joint space. Viscosity of fluid depends on temperature. Cartilage: Covers bone surfaces to allow bones to move freely over each other. Limited blood supply, receives nourishment from synovial fluid.
Joint actions Flexion: A movement that decreases the angle between the ones at the joint, e.g. bending the leg at the knee Extension: A movement that increases the angle between the bones at the joint, e.g. straightening the leg at the knee Abduction: The movement from a body part away from the midline of the body, e.g. raising arm to the side Adduction: The movement of a body part towards the midline of the body, e.g. lowering arm towards midline Inversion: Rotation of the foot to make the sole of the foot face inwards. Eversion: Rotation of the foot to make the sole of the foot face outwards. Rotation: Moving a body part such as the head or trunk around on its long axis. Circumduction: The circular movement of a body part e.g. rotating your shoulder in a circle Pronation: The rotation of the hand and forearm that causes the hand to face palm downwards Supination: The rotation of the hand and forearm that causes the hand to face palm upwards
Dorsiflexion: This is flexion of the ankle. Pulls top of foot towards tibia. Plantar flexion: Extension of the ankle. A movement that moves top of foot away from tibia
Isometric contractions: Muscle contracts, no movement produced. Length of muscle stays the same Isotonic contractions: The process where the muscle contracts to move an object. Muscle shortens & maintains tension throughout movement. Respiratory system: Responsible for the transfer of oxygen from the air to the blood, and the disposal of CO2. Works in conjunction with the cardiovascular system. Is essential for repeated movements. Lung function: Respiration is gas exchange between cells, blood & atmosphere. Includes pulmonary ventilation (breathing), pulmonary diffusion (exchange of O2 & CO2 between lungs & blood), transport of respiratory gases (transport of O2/CO2 between lungs & tissues of body via. blood) & internal respiration (exchange of gases between capillaries & tissue cells). Inspiration: During inspiration, diaphragm contracts & flattens as the internal intercostal muscles lift the ribs outward & upward. Movement increases chest volume, pulls lung walls outwards which decreases air pressure in lungs. In response to this, air from outside the body rushes into the lungs through air passages. Expiration: Diaphragm relaxes, moves upwards as internal intercostal muscles allow ribs and other structures to return to resting position. Volume of chest cavity decreases, increases lung pressure, air forced out to make pressures equal. Nose: Provides a warm, moist place for air to enter the body Nasal cavity: Situated in nose, contains hair that filets & cleans foreign objects when entering body. Incoming air is warmed. Pharynx (throat): Connects nasal cavity and mouth to larynx. Larynx: Responsible for ensuring food/air goes into proper channels. Epiglottis filters food. Also contains vocal chords that produce voice. Trachea (windpipe): Expels dust and other foreign particles toward pharynx. Divides into two bronchi. Bronchi: Divides into bronchioles, forming a respiratory tree. At the end of bronchioles, tiny air sacs called alveoli exist. Alveoli: The chambers where gas exchange occurs.
Lungs: Encloses the structures of the body responsible for gas exchange.
Circulatory system: Continual supply of food & oxygen that body tissues require is provided by this system. Flows constantly around the body from the heart, to the cells, and back to the heart (circulation). Also known as the cardiovascular system, this system delivers oxygen & nutrients to all parts of the body and removes wastes. It consists of blood, the heart and blood vessels. Blood consists of 55% plasma and 45% red cells, white cells & platelets. Red blood cells carry the protein haemoglobin, which gives blood its colour and can combine with oxygen, which enables blood to carry oxygen to tissues. White blood cells protect the body against bacteria. Platelets are tiny cell fragments which aid in the clotting of blood in event of injury. The heart: Striated muscle fibres, weighs ~300g, 12cm long, 9cm wide, 6cm thick, located in mediastinum, heart wall composed of 3 layers & 4 chambers. Arteries: Carries blood from heart to tissues, thick elastic walls to deal with great pressure. Veins: Carries blood from tissues to heart, smaller vessels at end of veins are called venules, contains valves which prevent blood from going the other way. Capillaries: Connects veins & arteries, nutrients exchanged throughout. A heartrate has two main phases. Diastole as the heart relaxes and refills with blood, and systole the contraction that forces blood around the body.
Health-related components Cardiorespiratory endurance: The ability of the heart, lungs and circulatory system to supply oxygen and nutrients effectively to working muscles and to remove waste. Muscular strength: The greatest maximal force/tension that a muscle group can exert in one maximal contraction. Muscular endurance: The ability to repeat/sustain a muscular effort for a relatively long period of time. Flexibility: The range of movement that can be performed in and around a joint. Body composition: The proportions of various body tissues and influence on body mass. Skill related components Power: The product of strength & speed: the ability to move the human body or an object quickly. Speed: the rate of change in position. Agility: The ability to change the direction or position of body segments or body rapidly & effectively. Coordination: A smooth flow of movement when performing a physical task Balance: A state during which the body is in a stable position/state of equilibrium. Reaction time: The time it takes to respond to a stimulus. Motion, Balance&Stability, Fluid mech & force Linear motion: A straight line movement. Velocity: displacement/time. Allows you to move in any direction. Speed: distance/time. Influences how fast you go. Acceleration: How fast you move between two points. Momentum: mass x velocity. Centre of gravity: Influences your balance to allow stability during movement Line of gravity: References the centre of gravity with a line down to the floor. Base of support: Any body part where weight is being placed upon.
Flotation: Two forces operating on a body in a fluid environment to determine its buoyancy. Centre of buoyancy: The centre of gravity of the water that the swimmer displaces. Drag: The resistance that acts against a body as it moves through a fluid environment. Lift: Occurs perpendicular to the flow of the water over the body when swimming. The Magnus effect: The effect that occurs when a spinning object creates a whirlpool of rotating air or liquid around it.
Newtons 3 laws of motion: Every body continues in its state of rest or motion in a straight line unless compelled to change that state by external forces exerted upon it. The rate of change in motion of a body is proportional to the force causing it, and the change takes place in the direction in which the force acts. For every force that is exerted by one body on another, there is an equal and opposite force exerted by the second body on the first. Applying forces: Enables us to move in a direction, apply force to muscles etc. Absorbing forces: Enables us to resist things like centrifugal force, protects during collisions etc. Applying force to objects: enables us to throw things, kick etc., to accelerate everything. Lactate: A chemical formed during the breakdown of carbohydrates in the absence of sufficient oxygen. Always a small amount of lactate circulating in the blood. Flows freely in blood and increases as the workload increases. High levels of lactate are produced when we exercise and there is low oxygen levels.
DRSABCD: Danger, response, send for help, airways, breathing, compressions, defibrillation. CPR: Cycles of 30 compressions (100/min) and 2 breaths delivered in between navel & collarbone. Depth of compression is 1/3 chest depth. Use one or two hands depending on age/size of casualty, two fingers for infants. S.T.O.P regime: Used to manage sporting injuries. Stop injured person from moving, talk to casualty to find what happened, observe the casualty to see if theres any signs of serious injury (swelling, loss of colour etc.), prevent further injury by monitoring/relocating person. TOTAPS: How to prevent further injury. Talk, observe, touch (feel for swelling/breaks), active movement (ask casualty if they can move injured area), passive movement (try to move area gently), skills test (if passed test return to playing sporting game). Stop assessment if one of these steps can not be performed and wait for medical assistance. PRE: Management of external bleeding. Pressure, restrict movement, elevate site of injury. Shock: The result of the circulatory system not functioning properly. The blood is depressed from circulating through the body and O2 is not being carried to tissue/organs. Signs & symptoms of shock include: pale face, cold skin, weak/rapid pulse, shallow/fast breathing, nausea, fainting/dizzy spells, restlessness, thirst, confusion. Management for shock is: Keep casualty calm, lay them down, follow DRSABCD, control bleeding, raise legs above heart, dress wounds/burns, immobilise fractures/dislocations, keep casualty warm, no food or drink, loosen light clothing, monitor casualty Neck & spinal injuries: Manage with DRSABCD if unconscious, keep calm and immobilise if conscious. Move casualty only if completely necessary and in danger. Loosen tight clothing, stabilise neck/head with cervical collar or something rigid to hold neck in place, seek medical attention. Moving a casualty: Drag by clothes (crackle neck if suspected to be spinal), human crutch method when someone has injured leg/foot and is able to walk with assistance, fourhanded-seat when two first aiders are available to carry. Hold each others wrists firmly in a square shape. Stretcher if possible. When contacting medical services, provide what has occurred, whos injured, how severe the injuries are, where the accident has occurred and what you have done already.
Treating injuries Laceration/abrasion (minor scrapes): Clean wound with saline/sterile water, apply nonadherent dressing Cut (incision) or puncture (penetration): DRSABCD if needed, clean wound w/ saline/sterile water, apply nonadherent dressing, do not remove embedded object Fractures: DRSABCD, control any bleeding, immobilise site, observe and treat shock and seed medical attention Dislocations: DRSABCD, immobilise injured site, apply ice & elevate, seek medical attention Head injuries/concussion: DRSABCD, lay in recovery position if conscious, be aware of spinal injuries, control external bleeding (but dont apply pressure to skull), if fluid coming from ear cover with sterile dressing and allow fluid to drain, seek medical attention Eye injuries: DRSABCD, wash with saline solution, avoid rubbing, seek medical advice Nasal injuries: DRSABCD, breathe through mouth, keep casualty seated w/ head tilted forward, apply finger & thumb pressure to soft area of nostrils, apply cooling to back of neck & forehead for 10min, seek medical advice if bleeding persists Burns: DRSABCD, cool burnt area with cold running water, keep stuck clothing on, cover burnt area w/ nonadherent dressing, minimise shock, do not apply anything or prick blisters Teeth: Straighten tooth, splint with foil and seek dental advice, or if dislodged, rinse in milk or saline solution, replace it correctly in socket, splint and seek dental advice Electrocution: DRSABCD, treat burns with cool water and seek medical attention Chest injuries: DRSABCD, casualty into comfortable position, encourage shallow breathing, pad injured area and seek medical advice Abdominal injuries: DRSABCD, loosen clothing and lay casualty on their back with head and shoulders slightly raised and a rolled up towel or blanket under knees, ensure casualty does not eat or drink, seek medical advice Heartattack: DRSABCD, recovery position and monitor Stroke: DRSABCD, recovery position and monitor
Diabetes: If hypoglycaemia (low blood glucose): give sugary substance and then a carbohydrate rich piece of food, if condition worsens apply DRSABCD. If hyperglycaemic (high blood glucose): apply DRSABCD, give casualty nothing to eat or drink, administer medication Epilepsy: Clear immediate area, seek medical advice, DRSABCD but do not leave patient if severe Asthma: Assure and assist into upright position, help to administer 4 puffs of inhaler, encourage them to relax, repeat medication after 4min if condition doesnt improve, seek medical advice if condition remains bad Anaphylaxes: DRSABCD, use EpiPen, lying/sitting position and observe pulse/breathing, if unconscious check for signs of life and give CPR if necessary Poisoning: If inhaled, move to fresh air, loosen tight clothing. If absorbed, remove contaminated clothing and flush skin with water. If ingested, do not induce vomiting, wash corrosive substance off mouth and face. In all situations, apply DRSABCD, call 000/poisons control if necessary. Bee/wasp stings: DRSABCD, remove sting by scooping out, apply ice and monitor Redback: DRSABCD, keep site clean and apply ice, reassure casualty Funnel-web: DRSABCD, firm pressure immobilisation bandage, call 000 Tick: Grasp part of tick and try to pull out with tweezers, seek medical advice Snake: DRSABCD, call 000, reassure casualty, firm pressure immobilisation bandage, ensure casualty does not move, seek urgent medical advice, record time of bite, when bandage was applied and any snake characteristics, do not elevate injury site Bluebottle: DRSABCD, calm casualty, dont rub site, pick off tentacles, immerse casualty in hot water for 20min (not too hot). Hypothermia: DRSABCD, move to warm place, avoid excessive movement, remove wet clothing and wrap casualty in blankets, place in recovery position. Its important to stabilise body temp. Hyperthermia: DRSABCD, lay casualty in cool and well-ventilated place, loosen tight clothing, sponge with cold water or ice at neck, groin and armpits, give cool drink if conscious, seek medical advice.
You might also like
- Pdhpe Preliminary NotesDocument11 pagesPdhpe Preliminary NotesSimpson100% (9)
- Health Notes Chapter 1-16Document121 pagesHealth Notes Chapter 1-16Stephanie FoleyNo ratings yet
- Notes On Core 1,2,3 & 5Document5 pagesNotes On Core 1,2,3 & 5Charlie BarkerNo ratings yet
- Lecture 1 - Health and Health PromotionDocument46 pagesLecture 1 - Health and Health Promotionkris_fishNo ratings yet
- The Practiceof Promoting and Protecting The Health Of. Populations Using Knowledge From Nursing, Social, and Public HealthsciencesDocument2 pagesThe Practiceof Promoting and Protecting The Health Of. Populations Using Knowledge From Nursing, Social, and Public Healthscienceslola&losa farhanNo ratings yet
- Application of Social Psychology To HealthDocument2 pagesApplication of Social Psychology To HealthNavneet DhimanNo ratings yet
- Chapter1 141020105327 Conversion Gate01Document21 pagesChapter1 141020105327 Conversion Gate01Arild JuliusNo ratings yet
- Health: Health Is The Level of Functional and (Or) Metabolic Efficiency of A Living Being. in Humans, ItDocument7 pagesHealth: Health Is The Level of Functional and (Or) Metabolic Efficiency of A Living Being. in Humans, ItNor Azizah ZainuddinNo ratings yet
- A Doctor's Dozen: Twelve Strategies for Personal Health and a Culture of WellnessFrom EverandA Doctor's Dozen: Twelve Strategies for Personal Health and a Culture of WellnessNo ratings yet
- Components of Health and Global Health IssuesDocument6 pagesComponents of Health and Global Health IssuesSusan HepziNo ratings yet
- PE Definition of HealthDocument3 pagesPE Definition of HealthHahahaNo ratings yet
- Health, Happiness, & Longevity: Eastern and Western ApproachFrom EverandHealth, Happiness, & Longevity: Eastern and Western ApproachNo ratings yet
- Bowel Care And Digestive Disorders: Preventive actions to keep stomach healthy and body disease-freeFrom EverandBowel Care And Digestive Disorders: Preventive actions to keep stomach healthy and body disease-freeNo ratings yet
- Psychology NotesDocument4 pagesPsychology NotesSree Harshitha SiddavatamNo ratings yet
- Introduction To CPH and History of Public Health IDocument6 pagesIntroduction To CPH and History of Public Health IReynajane TugadiNo ratings yet
- Geron - Group 1Document11 pagesGeron - Group 1Potato TomatoNo ratings yet
- Health, Happiness, and Longevity: Health & Spiritual SeriesFrom EverandHealth, Happiness, and Longevity: Health & Spiritual SeriesRating: 5 out of 5 stars5/5 (1)
- Food Counselling. How To Motivate People To Change Eating HabitsFrom EverandFood Counselling. How To Motivate People To Change Eating HabitsNo ratings yet
- Health and Its DeterminantsDocument7 pagesHealth and Its Determinantshardio damselgold.No ratings yet
- ملخصDocument52 pagesملخص7pqj5txhd8No ratings yet
- Health: Needs of Good HealthDocument6 pagesHealth: Needs of Good HealthRahul GuptaNo ratings yet
- Unit - 1Document35 pagesUnit - 1Pela KqbcgrlaNo ratings yet
- Lifespan Perspective On HealthDocument6 pagesLifespan Perspective On HealthYuktiNo ratings yet
- Community Health NursingDocument105 pagesCommunity Health NursingKBDNo ratings yet
- SGD 17Document2 pagesSGD 17Armella AzzahraNo ratings yet
- Social InstitutionsDocument15 pagesSocial Institutionsdorothy kageni100% (1)
- Healthy Diet Health Impact Prevalence Correlates and InterventionsDocument36 pagesHealthy Diet Health Impact Prevalence Correlates and InterventionsGood Boy ᴗ̈No ratings yet
- Medical Definition of BiomedicalDocument4 pagesMedical Definition of BiomedicalRishel Mae Besinga PantallanoNo ratings yet
- Module 11 Health Care Drug Education NSTPDocument30 pagesModule 11 Health Care Drug Education NSTPANNA LEAH FARILLONNo ratings yet
- What Is Health?Document6 pagesWhat Is Health?Respecio MjoyNo ratings yet
- The Building Blocks of Health: How to Optimize Your Wellness with a Lifestyle ChecklistFrom EverandThe Building Blocks of Health: How to Optimize Your Wellness with a Lifestyle ChecklistNo ratings yet
- Health Illness (2022)Document39 pagesHealth Illness (2022)AUDEH AHMADNo ratings yet
- Running Head: Obesity 1Document6 pagesRunning Head: Obesity 1AssignmentLab.com0% (1)
- Health Protection and Promoting Healthy LifestylesDocument3 pagesHealth Protection and Promoting Healthy LifestylesДаніелла АдаменкоNo ratings yet
- Successful Aging and Disease PreventionDocument6 pagesSuccessful Aging and Disease PreventionFriah Mae EstoresNo ratings yet
- Unit 2Document35 pagesUnit 2Shaira Abigail AninoNo ratings yet
- What Are The Determinants of HealthDocument7 pagesWhat Are The Determinants of Healthhiraf247No ratings yet
- Assingement of Psychology and SociologyDocument7 pagesAssingement of Psychology and SociologySurkhali BipanaNo ratings yet
- What Is Health PromotionDocument23 pagesWhat Is Health PromotionPrimalj Pinnaduwa100% (1)
- Healthy LifeDocument9 pagesHealthy LifeMahdie BahmanyarNo ratings yet
- Preventing Illness: Revolutionary StrategiesEmpowering Your Journey to Wellness through Science and Innovation for a Healthier Tomorrow:From EverandPreventing Illness: Revolutionary StrategiesEmpowering Your Journey to Wellness through Science and Innovation for a Healthier Tomorrow:No ratings yet
- One Other Group (Elderly People)Document4 pagesOne Other Group (Elderly People)John XavierNo ratings yet
- Exploring The Determinants Interventions and Dimensions of Health 2023 7 24 5 52 41Document20 pagesExploring The Determinants Interventions and Dimensions of Health 2023 7 24 5 52 41Trailers of moviesNo ratings yet
- Chap 1 Health and WellnessDocument31 pagesChap 1 Health and Wellnessapi-263590842No ratings yet
- How Not to Die: The Code to Your Amazing Life, Living Longer, Safer, and HealthierFrom EverandHow Not to Die: The Code to Your Amazing Life, Living Longer, Safer, and HealthierNo ratings yet
- Year 11 Health PowerpointDocument28 pagesYear 11 Health Powerpointapi-298362079No ratings yet
- Healthand Nutrition PPTDocument19 pagesHealthand Nutrition PPTTrisha Bendaña ReyesNo ratings yet
- Beliefs Representations and Risk - MM - 2013Document23 pagesBeliefs Representations and Risk - MM - 2013Kennedy Absalom ModiseNo ratings yet
- Khamlin Hamad Abdal - Groupa''Document23 pagesKhamlin Hamad Abdal - Groupa''Khamlin NurseNo ratings yet
- T.2 Task 2 ModelsDocument7 pagesT.2 Task 2 ModelsinesNo ratings yet
- Unit 1 Health Awareness and Role and Importance of Yoga: Dr. Rajesh Agrawal Associate Professor, MBICEMDocument22 pagesUnit 1 Health Awareness and Role and Importance of Yoga: Dr. Rajesh Agrawal Associate Professor, MBICEMshrutiNo ratings yet
- Crime Madison L NotesDocument79 pagesCrime Madison L Noteslj3472No ratings yet
- 2008 English Extension 1 NotesDocument3 pages2008 English Extension 1 Noteslj3472No ratings yet
- 2008 English Extension 1 Assessment TaskDocument3 pages2008 English Extension 1 Assessment Tasklj3472No ratings yet
- 2007 English Extension 1 NotesDocument17 pages2007 English Extension 1 Noteslj3472No ratings yet
- Doctoral Experience Capstone PortfolioDocument29 pagesDoctoral Experience Capstone Portfolioapi-595108452No ratings yet
- Final Project DescriptionDocument6 pagesFinal Project DescriptionCahyani DamawatiNo ratings yet
- Antimicrobial ResistenceDocument23 pagesAntimicrobial Resistencelayal mrowehNo ratings yet
- Safety Pocket Guide Web 061808Document534 pagesSafety Pocket Guide Web 061808hombre911100% (1)
- Tipos de Diabetes - Diabetes MonogenicaDocument27 pagesTipos de Diabetes - Diabetes MonogenicaSara AmorimNo ratings yet
- DERMATITISDocument2 pagesDERMATITISKevinJuliusTanadyNo ratings yet
- Mylan EpiPen StatementDocument3 pagesMylan EpiPen StatementCBS This MorningNo ratings yet
- Different Committees in The HospitalDocument8 pagesDifferent Committees in The HospitalShehnaz SheikhNo ratings yet
- The Chameleon Enthusiast by Noelle SenchynaDocument58 pagesThe Chameleon Enthusiast by Noelle SenchynaDragoș DrăniceanuNo ratings yet
- The Extent of Influence of Factors On Cigarette Smoking Among TeenagersDocument4 pagesThe Extent of Influence of Factors On Cigarette Smoking Among TeenagersLESTHER DELA CRUZNo ratings yet
- Pharmacy Job InterviewQuestionsDocument4 pagesPharmacy Job InterviewQuestionsRadha MandapalliNo ratings yet
- Dr. Dan Siegel - Resources - Healthy Mind PlatterDocument4 pagesDr. Dan Siegel - Resources - Healthy Mind PlatterInês Novais100% (4)
- MSDS Aceite CastorDocument6 pagesMSDS Aceite CastorwaddydiNo ratings yet
- Maharashtra Public Service Commission Maharashtra Subordinate Services Main Examination - 2019Document59 pagesMaharashtra Public Service Commission Maharashtra Subordinate Services Main Examination - 2019S KatyarmalNo ratings yet
- Elc590 Informative Speech About InsomniaDocument5 pagesElc590 Informative Speech About InsomniaANGJELLY ALLYA NGAUHNo ratings yet
- NCP Impaired Gas Exhange Related To Alveolar Wall Destruction EMPHYSEMADocument5 pagesNCP Impaired Gas Exhange Related To Alveolar Wall Destruction EMPHYSEMAMa. Elaine Carla Tating50% (2)
- Hirschsprung NCM 109 Case PresentationDocument10 pagesHirschsprung NCM 109 Case PresentationValerie LeddaNo ratings yet
- Pro-Oxidant Strategies - Cancer Treatments ResearchDocument71 pagesPro-Oxidant Strategies - Cancer Treatments ResearchSpore FluxNo ratings yet
- Disability MatrixDocument21 pagesDisability MatrixAngelika MendozaNo ratings yet
- Pappas Bikhazi 2023 Babe Ruth S Anaplastic Epidermoid Carcinoma of The NasopharynxDocument5 pagesPappas Bikhazi 2023 Babe Ruth S Anaplastic Epidermoid Carcinoma of The NasopharynxVinoster ProductionNo ratings yet
- Sarah J. (Englert) Dunham RN, BSN, MS, FNPDocument3 pagesSarah J. (Englert) Dunham RN, BSN, MS, FNPapi-309264509No ratings yet
- GCC Human Drugs Subv2.1Document103 pagesGCC Human Drugs Subv2.1AmrNo ratings yet
- Factitious DisorderDocument6 pagesFactitious DisorderRon JaredNo ratings yet
- Overcoming Obesogenic Environments: A Qualitative Study Exploring Mechanisms of Healthy EatersDocument10 pagesOvercoming Obesogenic Environments: A Qualitative Study Exploring Mechanisms of Healthy EatersCristina Saldias PorrasNo ratings yet
- Job Safety Analysis SOP Rev A 08.2017Document4 pagesJob Safety Analysis SOP Rev A 08.2017AshtosheelatikaNo ratings yet
- IELTS 03 - Listening 01 & Reading 01 - Transcripts & KeysDocument8 pagesIELTS 03 - Listening 01 & Reading 01 - Transcripts & KeysLe Hoang KhaNo ratings yet
- NCPPDocument11 pagesNCPPAngelo Miguel MuñozNo ratings yet
- Rachel Tucker Resume 2020Document1 pageRachel Tucker Resume 2020api-489845523No ratings yet
- Nejmra 2023911Document8 pagesNejmra 2023911Merry LeeNo ratings yet
- Acl Reconstruction Without Meniscus RepairDocument1 pageAcl Reconstruction Without Meniscus Repairsathvik gowdaNo ratings yet