Professional Documents
Culture Documents
Position Paper-RH Bill-Dr Manalo
Uploaded by
CBCP for LifeOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Position Paper-RH Bill-Dr Manalo
Uploaded by
CBCP for LifeCopyright:
Available Formats
REPRODUCTIVE HEALTH ACT: MEDICAL & ETHICAL ISSUES By Maria Fidelis C. Manalo, MD, MSc.
Consultant and Faculty, Department of Community & Family Medicine, Far Eastern University - Nicanor Reyes Medical Foundation, Fairview, Quezon City 1119, Philippines. Email: mcmanalo@feu-nrmf.ph
It is the objectives of this position paper: 1) to increase the awareness and sensitivity of our legislators to ethical problems that they confront as they propose to make reproductive health care a priority program of the government and to make it into one of the laws of the land; 2) to develop an understanding of bioethical concepts and principles and be able to apply them in the analysis of bioethical issues in reproductive health care; and 3) to help the Filipino public develop a mature reasoning and to act according to sound ethical judgment. There are many instances when healthcare matters require an ethical approach. We cannot follow the principle: Everything that can be done ought to be done. Medical practice is subject to certain ethical limitations. Human dignity must be the central value for the financing of development. A true concern for the development of peoples cannot afford to be reductionistic, but must respect the genuine claims of both economics and morality. Such an authentic concern must prize the close relationship between the centrality of the human person and economic activity, stressing the subjective character of human work and its place in human creativity. The matter of Reproductive Health Care and the provisions of the house bills pertaining to it will be evaluated based on the following bioethical principles: beneficence & non-maleficence, justice and autonomy. PRINCIPLES OF BENEFICENCE AND NON-MALEFICENCE The bioethical principles of beneficence and non-maleficence require of health service providers to do things for the patients benefit and to avoid doing him harm. The Hippocratic Oath says thus: I will use treatment to help the sick according
to my ability and judgment, but will never use anything to injure or wrong them. The health care professionals have the duty to do or promote good and the duty to remove or prevent evil or harm. 1. Reproductive Health and Population and Development Act of 2010 (House Bill HB 96 and Senate Bill SB 2378) is about education & promotion of safe sex and use of modern contraceptive devises. (Sec. 13, Mandatory Age-Appropriate Reproductive Health and Sexuality Education, HB 96 and SB 2378) What is wrong with safe sex and the use of contraceptives? 1. Contraceptives are not effective in blocking out STDs. The inherent naturally occurring flaws in natural rubber (latex) are up to 5 microns inches in size. The average sperm is about 50 microns in diameter, and the average AIDS virus is about 0.1 micron in size. An AIDS virus can pass through a latex flaw. (Dr. C. Michael Roland of the U.S. Naval Research Lab, Washington D.C, Rubber World, June, 1993) The greater danger of infection lies in the propensity of condoms to burst, tear and slip off frequently. (Brian Clowes, http://www.lifeissues.net/) There is no absolute guarantee that one will not get sexually transmitted diseases (STDs) and HIV even when condom is used. Most experts believe that the risk of getting HIV/AIDS and other sexually transmitted diseases can be greatly reduced if a condom is used consistently and correctly. In other words, sex with condoms isn't totally "safe sex," but it is "less risky" sex. The most reliable ways to avoid transmission of STDs are to abstain from sexual activity, or to be in a long-term mutually monogamous relationship with an 2
uninfected partner. (Centers for Disease Control (CDC) & US FDA) 2. Some contraceptives are abortifacient. Birth control pills are synthetic steroid hormones that mimic the way real estrogen and progestin works in a woman's body. The pill prevents ovulation - no new eggs are released by a woman on the pill since her body is tricked into believing she is already pregnant. Although the primary mechanism of oral contraceptives (OC) is inhibition of ovulation, other alterations include changes in the cervical mucus, which increase the difficulty of sperm entry into the uterus, and changes in the endometrium, which reduce the likelihood of implantation. (Physicians Desk Reference & Drug Facts and Comparisons) "Family planning" experts have always recognized that the high failure rate of contraceptives would lead to more abortions. Oral contraceptives (OCs) have a method failure rate of 0.3 % and user failure rate of 8% during the first year. As such, if a woman uses the combined pill or the minipill, she has a 34% chance of an unintended pregnancy in five years and a 57% chance of a pregnancy in 10 years. Abortion statistician Christopher Tietze stated that: "The safest regimen of control for the unmarried and for married child-spacers is the use of traditional methods [of contraception] backed up by abortion; but if this regimen is commenced early in the child-bearing years, it is likely to involve several abortions in the course of her reproductive career for each woman who chooses it." (Brian Clowes, The Facts of Life, http://www.hli.org/) Many women present for emergency contraception following consensual but unprotected sexual intercourse and in some cases aggravated
sexual assault. Hormonal emergency contraception (morning-after pill or Yuzpe method) is supposed to substantially decrease the likelihood of an unwanted or unintended pregnancy when taken within 24-72 hours of unprotected intercourse. Similar to the other hormonal contraceptives, the major mechanism is inhibition or delay of ovulation (US Food and Drug Administration, 1997). Other mechanisms include sperm penetration, tubal motility, and alteration of the endometrium (post-fertilization effect). Established pregnancies are supposedly not harmed. (Williams Obstetrics, 22nd Ed, 2005) EllaOne a new five day morningafter pill that claims to be emergency contraception can in fact act as an abortion-inducing drug. It can prevent an embryo from receiving nourishment from its mothers womb, thereby aborting the pregnancy. The drugs chemical composition and function are nearly identical to a commonly used abortion drug known as RU-486. The drug has been on sale in the UK for a year and has been approved by the US Food and Drug Administration earlier this year. (Lifesitenews.com, 18 October 2010) In IUD users, the low recovery of ova from the uterus, as well as the lack of hCG rise in more recent studies of IUD users, suggest that the major postfertilization effect is destruction of the early embryo in the Fallopian tube, in the same way that the major prefertilization effect is likely to be destruction of sperm and ova. For the copper IUD, this embryocidal effect may be more a result of inflammation and direct toxicity, whereas with the progestin IUDs it may result more from inhibition of transport through the Fallopian tube, along with prevention of implantation, preventing long-term viability of the embryo. (Stanford and Mikolajczyk, American Journal of Obstetrics & Gynecology, December 2002) 3
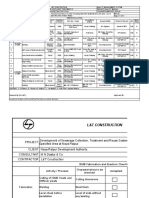
3. Contraceptives harm the body in numerous ways. (see Table 1) Table 1. Adverse Effects of Contraceptive Methods
Contraceptive Methods
Oral contraceptives
Adverse Effects
increased risk of thromboembolic disorders (deep vein thrombosis, pulmonary embolism), stroke, hypertension, increased risk of myocardial infarction in smokers, migraine headache, aberrations in the levels of several nutrients, stimulatory effect on some cancers, other metabolic effects same as oral contraceptives
Injectable Contraceptives (Depo-Provera) and Progestin Implants (Norplant) Hormonal Emergency Contraception (morning-after pill or Yuzpe method) Intrauterine devices (IUDs)
nausea and vomiting
uterine perforation and abortion, uterine cramping and bleeding, menorrhagia, infection, ectopic pregnancies; if theres pregnancy with IUD in utero late abortion, sepsis, preterm birth effective up to 17 days after intercourse (Weiss, 1993) nausea, vomiting, gastrointestinal cramping, hemorrhage due to partial expulsion of pregnancy, intra-abdominal hemorrhage from an early unsuspected ectopic pregnancy
Mifepristone (RU 486)
Tubal sterilization
anesthetic complications, inadvertent injury of adjacent structures, pulmonary embolism (rare), failure to produce sterility with subsequent development of ectopic pregnancy an almost twofold risk of prostatic cancer in men less than 55 years old (Lesko et al, 1999)
Vasectomy
(Williams Obstetrics - 22nd ed (2005) McGraw Hill Professional)
The best evidence continues to suggest that the increased risk of cardiovascular side effects (especially venous thromboembolism or VTE, manifesting as deep venous thrombosis of the leg or pulmonary embolism), in oral contraceptive (OC) users is a class effect, dependent on the estrogen dose and duration of use, and independent of the progestogen used. (Shapiro & Dinger. J Fam Plann Reprod Health Care. 2010 Jan) In a national cohort study in Denmark from 1995 to 2005 involving Danish women aged 15-49 with no history of cardiovascular or malignant disease, a total of 4,213 venous thrombotic events were observed, 2, 045 of which were in current users of oral contraceptives. The overall absolute risk of VTE per 10 000 woman years in current users of oral contraceptives was 6.29, vs. 3.01 in nonusers. (Lidegaard et al, British Medical Journal. 2009 Aug) In a population based case-control study in the Netherlands of 1,524 patients and 1,760 controls, involving premenopausal women <50 years old who were not pregnant, not within four weeks postpartum, and not using a hormone excreting intrauterine device or depot contraceptive, results showed that currently available oral contraceptives increased the risk of VTE fivefold compared with non-
use. The risk clearly differed by type of progestogen and dose of estrogen. (van Hylckama Vlieg, British Medical Journal, 2009) 2. Reproductive Health and Population and Development Act of 2010 is about classifying making family planning supplies as essential medicine (Sec. 9, Family Planning Supplies as Essential Medicines, HB 96 and SB 2378) What is wrong with classifying family planning supplies as essential medicines? The National Drug Committee, the body in charge of developing the Formulary, followed a systematic process in deciding on the drugs list. With the support of the Action Programme on Essential Drugs, guidelines were first developed in 1990 for selecting drugs, based on the WHO Technical Report Series No.825, The Use of Essential Drugs. Criteria included relevance to prevalent diseases, efficacy and safety and quality. In cases where national standards are not established, the WHO Certification Scheme on the Quality of Pharmaceutical Products Moving in International Commerce is requested. The cost of treatment regimen is also taken into account, as are the capabilities of health workers at different levels of health care; and benefit/risk ratio (see Table 2).
Table 2. Criteria for Drug Selection into Essential Drug List & National Drug Formulary
Criteria
Relevance to disease Quality
indicated in the treatment of prevalent diseases must meet adequate quality control standard including stability and when necessary bioavailability; compliance with WHO Certification Scheme on the Quality of Pharmaceutical Products Moving in International Commerce product manufactured in accordance with CGMP and records whether or not the product has been approved for marketing in the country of origin.
Cost of treatment regimen Appropriateness to the capability of health workers at different levels of health care. Local health problems Benefit/Risk ratio 5
Most normal, low-risk pregnancy, per se, is not a disease, and as such does not need medicines, except for iron and folic acid-multivitamin supplementation. Hence, the only essential medicines during pregnancy would be ferrous sulfate and folic acid-multivitamins. Hormonal contraceptives (and injectables) are not safe, as has already been shown by meta-analysis of case-control studies. Use of oral contraceptives (OCs) was associated with almost twofold statistically significant increased risk of premenopausal breast cancer in general and across various patterns of OC use. The association between OC use and breast cancer risk was greatest for parous women who used OCs 4 or more years before first full term pregnancy. (Kahlenborn et al, Mayo Clinic Proceedings. 2006). Contraceptive hormone use is linked to cardiovascular disease. Newer generation oral contraceptives (OC) indicate a persistent increased risk of venous thromboembolism for current users. Current guidelines indicate that, as with all medication, contraceptive hormones should be selected and initiated by weighing risks and benefits for the individual patient. Women 35 years and older should be assessed for cardiovascular risk factors including hypertension, smoking, diabetes, nephropathy, and other vascular diseases, including migraines, prior to OC use. (Shufelt & Bairey Merz, J Am Coll Cardiol. 2009 Jan) Depot medroxyprogesterone acetate (DMPA) suppresses pituitary gonadotrophin output, thus, suppressing ovulation. Estrogen production from the ovary is also strongly inhibited, and the resulting estrogen deficiency has a detrimental impact on bone. DMPA may be particularly detrimental in young women, as it may impede attainment of peak bone mass. (Albertazzi et al, Contraception. 2006 Jun) DMPA use seemed to be associated with a statistically significant increased risk of fractures, in a
case control study among Danish women (Vestergaard et al, Contraception. 2008 Dec) Intrauterine devices (IUDs) are not safe. During the use of a copper IUD, menstruation tends to be longer with a greater loss of blood; in 70% of women who use a hormonal IUD oligomenorrhea or even amenorrhoea develops. In the first weeks after IUD insertion, there is an increased risk of pelvic inflammatory disease (PID). (Summary of the practice guideline 'The intrauterine device' from the Dutch College of General Practitioners, 2009) A World Health Organization multicentre study established that pelvic inflammatory disease (PID) risk is temporally related to IUD insertion procedures. (Shapiro, Reprod Health Matters. 2004 May) In 15 studies comparing IUD performance in parous vs. nulliparous women, nulliparous women had higher rates of expulsion and removals due to bleeding and pain. (Hubacher, Contraception. 2007 Jun) Uterine perforation is a rare yet serious complication and is usually seen during insertion of the IUD. (Koltan et al, J Chin Med Assoc. 2010 Jun) There are about 70 cases in the literature of IUDs that have migrated into the bladder. The resulting bladder perforation can be complete or partial. (Istanbulluoglu et al, J Chin Med Assoc. 2008 Apr) There is a reported case of a colon penetration by a copper IUD. (Arslan et al, Arch Gynecol Obstet. 2009) Various contraceptive methods or reproductive patterns may play a role in the etiology of cancer. There is an association of contraceptive methods, including oral contraceptives (OC) and tubal sterilization (TS), with overall and site-specific cancer. In a large prospective cohort study from 1996 to 2006 of 66,661 Chinese women in Shanghai, 76.7% of whom used contraception, 2,250 women were diagnosed 6
with cancer during a median follow-up time of 7.5 years. Use of any contraceptive method was associated with increased risk of rectal cancer and reduced risk of thyroid cancer. Risk of gallbladder cancer increased with ever use of oral contraceptives (OC). Ever having a tubal sterilization (TS) was associated with increased uterine body cancer and decreased risk of stomach cancer. There are no findings of any contraceptive method being related to the risk of ovarian cancer but the analyses were based on few events. (Dorjgochoo et al, Int J Cancer. 2009 May)
Distributive justice is the aspect of justice that pertains to a fair scheme of distributing societys benefits and burdens to its members. The presumed benefits are receiving medical care and treatment. The presumed burdens are paying for care and partaking in experimental research.
PRINCIPLE OF JUSTICE The principle of justice includes respect or recognition of a right that belongs to others, either to God or to fellowmen. It demands giving to others what is due them.
3. Reproductive Health and Population and Development Act of 2010 is about promoting a program to achieve equitable allocation of resources (Sec. 3, Guiding Principles, HB 96), when problems pertaining to lack of reproductive health is not as prevalent or as life-threatening as our other health problems. The governments health programs should address and give priority to the top 10 leading causes of morbidity and mortality. (see Table 3)
Table 3. The 10 leading causes of death by broad income group (2004) according to the World Health Organization Low-income countries
Lower respiratory infections Coronary heart disease Diarrheal diseases HIV/AIDS Stroke and other cerebrovascular diseases Chronic obstructive pulmonary disease Tuberculosis Neonatal infections Malaria Prematurity and low birth weight
Deaths in millions
2.94 2.47 1.81 1.51 1.48 0.94 0.91 0.90 0.86 0.84
% of deaths
11.2 9.4 6.9 5.7 5.6 3.6 3.5 3.4 3.3 3.2
What is wrong with giving priority to reproductive health? In the Philippines, eight of the 10 leading causes of morbidity are caused by infections. They are: acute lower respiratory tract infection and pneumonia; acute watery diarrhea; bronchitis/ bronchiolitis; influenza; tuberculosis; malaria; acute febrile illness; and dengue fever. Among these communicable diseases, pneumonia and tuberculosis continue to be among the 10 leading causes of mortality, causing a significant number of deaths across the country. (World Health Organization-WHO-Western Pacific Region Report) Former Department of Health (DOH) Secretary Dr. Manuel M. Dayrit, has commented: While we have all become accustomed to the longstanding situation in which donated contraceptives were widely distributed free-of-charge, this may not necessarily have been the best approach for the nation to take in addressing the needs of the people. Statistics will show that the prevalence of contraceptive use has long since leveled off, and there is really no massive clamor among the Filipino people to have more and more free contraceptives. Financial resources allotted by foreign donors to assist the Philippine Governments programs could actually be better spent in other pursuits than purchasing contraceptives. It is also of value to demystify our perceptions about the role of contraceptives in womens health, womens rights, and healthy families. To equate access to contraceptives with the reduction in maternal morbidity and mortality is simplistic. (Philippine Daily Inquirer, 9/20/04) The principle of justice demands equal distribution of burdens. Justice demands that giving undue burden to an individual requires his informed consent, he must understand what is involved in the burden and voluntarily accept it. Often it involves the virtue of charity. However,
should the reproductive health bill be passed into a law, it will guarantee universal access to health care services, methods, devices and supplies. If efforts are not made to ensure informed consent from the prospective users of artificial contraceptives, eventually, it will be the poor and uneducated who will suffer more from the burden of their adverse effects. The rich and the educated would know better. When did the birth control movement begin? It began during the late 18th century, when people started questioning the earth's ability to sustain a large population. Prior to the 1800s, the death rate had offset the birth rate, so the overall population of the Earth remained the same. However, scientific advances during the 18th and 19th centuries resulted in better food supplies, control of diseases, and safer work environments for people living in developed countries. The result of these advances were longer life spans and an increase in the world's population. Thus birth control came to be regarded as a solution to overpopulation. In the early 1900s Margaret Higgins Sanger (18831966) founded what became known as the birth control movement in the United States. While working as a nurse in
the poor neighborhoods of New York City, she came to be aware of the effects of
unplanned and unwelcome pregnancies. Her mother's health had suffered as she bore eleven children. She came to believe in the importance to women's lives and women's health of the availability of birth control, a term which she's credited with inventing. In 1912, Sanger gave up nursing work to dedicate herself to the distribution of birth control information. In 1916, Sanger set up the first birth control clinic in the United States. In 1927 Sanger helped organize the first World Population Conference in Geneva. During the 1930s, it was discovered that hormones prevented ovulation in rabbits. In 1950, while in her 80s, Sanger underwrote the research necessary to create 8
the first human birth control pill. Sanger raised $150,000 for the project. The birth control pill was introduced to the public in the early 1960s. According to Dr. Alan F. Guttmacher, president of the Planned Parenthood World-Wide Association, it was Mrs. Sanger who convinced America and the world that control of conception is a basic human right and like other human rights must be equally available to all. Sanger's American Birth Control League, established in 1921, became the Planned Parenthood Federation of America in 1946 and led to the establishment of more than 250 Planned Parenthood Centers in 150 cities throughout the country. The movement is now worldwide, with 38 member organizations and projects in 88 countries. Planned Parenthood is the largest abortion provider in the world. The eugenics circle held that some races and individual members of the human species were genetically superior to others These superior members should be encouraged to reproduce, while the births of inferior members such as the poor or minorities were to be regulated. Their ultimate solution to the problem of poverty was simple: Eliminate the poor. In Birth Control Review May 1919, Sanger wrote, "More children from the fit, less from the unfit - that is the chief aim of birth control." The Birth Control Review November 1921 edition declared, "Birth control: to create a race of thoroughbreds." Sanger outlined her philosophy in her 1922 book Pivot of Civilization. In it she sharply criticized philanthropists who provided free maternity care to poor mothers. According to Sanger, these acts of generosity "encourage the healthier and more normal sections of the world to shoulder the burden of unthinking and indiscriminate fecundity of others; which brings with it, as I think the reader must
agree, a dead weight of human waste. Instead of decreasing and aiming to eliminate the stocks that are most detrimental to the future of the race and the world, it tends to render them to a menacing degree dominant. The founder of Planned Parenthood saw contraception, sterilization and eventually abortion as the panacea for eliminating all human suffering. In Margaret Sanger: Father of Modern Society, author Elasah Drogin observed: "Through the 284 pages of Pivot of Civilization, there is not one word written about fair labor laws, fair housing requirements, a more equitable distribution of wealth, or even the simple responsibility of caring for one's neighbor." Sanger's disdain for certain members of society was not confined to the poor, whom she often referred to as "human weeds." It targeted minorities such as blacks. In a private letter to Clarence Gamble dated Oct. 19, 1939, she revealed her ultimate goal toward blacks and how it could best be attained. "The most successful educational approach to the Negro is through a religious appeal," she wrote. "We do not want word to go out that we want to exterminate the Negro population, and the minister is the man who can straighten out that idea if it ever occurs to any of their more rebellious members." The following lines from Pivot of Civilization allow a particularly telling glimpse of Sanger's "compassion" and her motives. "Remember our motto: if we must have welfare, give it to the rich, not to the poor . ... We are paying for and even submitting to the dictates of an everincreasing, unceasingly spawning class of human beings who never should have been born at all." Sanger's views naturally led her to strike out against the institution of marriage and the family. "The marriage bed," she 9
wrote, "is the most degenerating influence in the social order." Sanger advocated instead a "voluntary association" between sexual partners. She thus sought to supplant the family as the most fundamental unit of society with relationships directed toward the sexual gratification of cooperating individuals. (Walter Schu, National
4. Reproductive Health Population and Development Act of 2010 is about ensuring peoples access to medically safe, legal, effective, quality and affordable reproductive health goods and services. (Implementing Mechanisms, Sec. 20, HB 96 AND Sec. 17, SB 2378) What is wrong with access to reproductive health goods and services? Former Department of Health (DOH) Secretary Dr. Manuel M. Dayrit, MD is known to have commented: Equally flawed is the much-publicized argument that women are accorded the rights they deserve when they are made to use contraceptives. Majority of women who use these products are not wholly aware of the many effects they have on their health and lives, and of the other approaches that are available to them. It is our belief that womens rights, reproductive rights, and the right to health could only be realized within an environment of informed choice. (Philippine Daily Inquirer, 9/20/04) Indiscriminate access to reproductive health goods and services without full disclosure of the potential for post-fertilization effects of hormonal contraceptives constitutes a violation of informed consent. The available evidence supports the hypothesis that when ovulation and fertilization occur in women taking oral contraceptives (OCs), post-fertilization effects are operative on occasion to prevent clinically recognized pregnancy. Oral contraceptives directly affect the endometrium. These effects have been presumed to render the endometrium relatively inhospitable to implantation or to the maintenance of the preembryo or embryo prior to clinically recognized pregnancy. (Larimore & Stanford, Archive of Family Medicine, Feb 2000)
Catholic Register, May, 1999)
Are the proponents and supporters of the Reproductive Health Bills aware of these historical facts?
PRINCIPLE OF AUTONOMY
The principle of autonomy upholds the patients option to choose based on respect for his free will. A patient has the moral right, as an individual person, to determine what is good for himself. This right of self-determination include the right to informed consent, informed decision, informed choice and the tight to refusal of treatment. It is the duty of the physician to perform or omit an action corresponding to the patients right. The rights to informed consent, decision and choice guarantees the patients right to receive all necessary information concerning diagnosis and medical intervention, before that treatment is administered, in order to be able to give willing and uncoerced consent based on his/her value system. The elements of informed consent include disclosure by the health professional of the nature of the intervention, its expected risks, and benefits and alternatives available, comprehension, and competence of the patient . According to the Patients Bill of Rights: The patient has the right to refuse treatment to the extent permitted by law and to be informed of the medical consequences of his action. A patient may refuse medical treatment because their religious convictions prohibit them from doing so.
10
Indiscriminate access to reproductive health goods and services without full disclosure of the potential for post-fertilization effects of hormonal contraceptives constitute a violation of the patients right to refuse treatment. Physicians should understand and respect the beliefs of patients who consider human life to be present and valuable from the moment of fertilization. Patients should be made fully aware of this information so that they can consent to or refuse the use of oral contraceptives. (Larimore & Stanford, Archive of Family Medicine, Feb 2000) Women who believe that human life begins at fertilization and those who consider it is important to distinguish between natural and induced embryo loss are less likely to consider the use of a method with post-fertilization effects. In a cross-sectional survey of 755 women, aged 18-49, from Primary Care Health Centers in Pamplona, Spain, 40% of women would not consider using a method that may work after fertilization but before implantation and 57% would not consider using one that may work after implantation. (de Irala et al, Biomed Central Women's Health 2007) Among 618 women ages 1850 in family practice and obstetrics and gynecology clinics in Salt Lake City, Utah, and Tulsa, Oklahoma, USA, 34% reported they believed that life begins at fertilization and would not use any birth control method that acts after fertilization. (Dye et al, Biomed Central Women's Health 2005)
What are the arguments and the evidence on abstinence only vs. comprehensive sex education programs?
Comprehensive Sex Education or Abstinence-Plus Education: Includes discussions of issues such as perception of personal risk, costs and benefits of preventive behaviors, sexual decision making, refusal skills, and condom use for safe sex Explores the context for and meanings involved in sex Acknowledges that many teenagers will become sexually active Teaches and promotes contraception Discussion topics include substance abuse, contraception, abortion, and AIDS/STDs Emphasizes avoidance of unprotected sex through abstinence or using protection
Abstinence Education:
Includes discussions of values, character building, and, in some cases, refusal skills Encourages abstinence from high-risk behavior, including sexual activity Discussion topics include friendship, love and dating, self-respect, decision-making, alcohol abuse, drug abuse, physical fitness and nutrition, and AIDS/STDs
5. The Reproductive Health and Population and Development Act of 2010 is about mandatory age-appropriate reproductive health and sexuality education. (Sec. 13, HB 96 and SB 2378).
11
What is wrong with age-appropriate mandatory reproductive health and sexuality education? The harmful effects of early sexual activity are well documented. They include sexually transmitted diseases, teen pregnancy, and out-of-wedlock childbearing. As well, teen sexual activity is linked to emotional problems, such as depression, and increased risk of suicide. Abstinence education programs, which encourage teens to delay the onset of sexual activity, are effective in curbing such problems. Opponents of abstinence education, however, claim that abstinence programs dont work and that there has been no scientific evidence that abstinence programs are effective. (Pardue, Web Memo, May 2005) The ill effects of sex education programs that merely promote "safe sex" were made evident in a study published in 2004. In England, the governments TeenAge Pregnancy Units strategy involves explicit sex education in schools, often conducted by nurses without teachers present. It also hands out free condoms and send birthday cards when girls reach 14 asking them to attend confidential health checks without their parents. In Scotland, sex education programs were introduced to distribute free morning-after pills and condoms. These approaches have failed to tackle the rise in STDs, unwanted conceptions, and abortion levels. (Abstinence education shows its wisdom, zenit.org, Oct 9, 2004) At least 10 studies have shown the positive effects of abstinence programs. The study by Dr. Robert Lerner published in the Institute for Youth Developments peer-reviewed journal Adolescent & Family Health in 2004
evaluated the effectiveness of the Best Friends abstinence education program which began in 1987 and currently operates in more than 100 schools across the United States. Its curriculum consists of a character-building program for girls in the fifth or sixth grade, including at least 110 hours of instruction, mentoring, and group activities throughout the year. A companion program for boys, Best Men, began in 2000. Junior-high and middle school-aged girls who participated in the Best Friends program, when compared to their peers who did not participate, were: Six-and-a-half times more likely to remain sexually abstinent; Nearly two times more likely to abstain from drinking alcohol; Eight times more likely to abstain from drug use; and Over two times more likely to refrain from smoking
In an analysis of the causes of the decline in non-marital birth and pregnancy rates for teens from 1991 to 1995, increased abstinence among 15- to 19-year-old teens accounted for at least two-thirds (67%) of the drop in teen pregnancy rates. Increased abstinence also accounted for more than half (51%) of the decline in teen birthrates. (Mohn et al, Adolescent and Family Health, April 2003) In a study looking at the changes in sexual behaviors among high school students and the decline in teen pregnancy rates in the 1990s, results showed that 53 percent of the decline in teen pregnancy rates can be attributed to decreased sexual experience among teens aged 15- 17 years old, while only 47 percent of the decline is attributed to increased use of contraception among teens. (Santelli et al. Journal of Adolescent Health, August 2004)
12
In a poll on what parents want taught in sex education programs, the overwhelming majority of parents (91%) want schools to teach that adolescents should be expected to abstain from sexual activity during high school years. Only 7 percent of parents believe that it is okay for teens in high school to engage in sexual intercourse as long as they use condoms, which is the predominant theme of comprehensive sex education. (Rector et al, Backgrounder, January 2004) Teens themselves welcome the abstinence message and appear to be heeding it. A poll by the National Campaign to Prevent Teen Pregnancy found that a clear majority of adolescents (69%) agree that it is not okay for high school teens to engage in sexual intercourse. (With One Voice, December 2004) The Centers for Disease Controls (CDC) Youth Risk Behavior Survey (YRBS) shows that the number of teens who have ever had sexual intercourse has fallen seven percent in the last 12 years, from 54 percent in 1991 to 46 percent in 2003. (Youth Online: Comprehensive Results http://apps.nccd.cdc.gov/yrbss)
Since the State, in accordance with the provisions of the Philippine constitution, recognizes and guarantees the exercise of the universal basic rights of every man, including that of the unborn, regardless of gender, religious convictions and cultural beliefs, then major amendments to the proposed RH Bill have to be made before they can even be deliberated upon by our lawmakers, much less approved and passed as a law. The end of meeting the Millennium Development Goals (MDG) by 2015 does not and cannot justify the means of providing universal access to reproductive health care services and methods when these have not been proven medically safe, legal and licit in all aspects. All licensed medical practitioners swear by the Hippocratic Oath which says: I will not accede to pretensions that are directed to the administration of poison nor induce to anyone suggestions of the kind. I will abstain from administering abortifacients to women. While I continue keep this Oath unviolated, may it be granted to me to enjoy life and the practice of the art and science of medicine with the blessing of the Almighty and respected by my peers and society, but should I trespass and violate this Oath, may the reverse be my lot. Indeed, should policy makers impose on healthcare providers to trespass and violate the Hippocratic Oath which abides by the bioethical principles of beneficence, non-maleficence, justice, and autonomy when they render reproductive health care, may they be accountable for this act before God and before the Filipino people whom they are supposed to serve. "The moral causes of prosperity ... reside in a constellation of virtues: industriousness, competence, order, honesty, initiative, frugality, thrift, spirit of service, keeping ones word, daring -- in short, love for work well done. No system or social structure can resolve, as if by magic, the problem of poverty outside these virtues." 13
Summary of the Evidence & Recommendations
The available evidence as presented supports the valid opposition of those against the Reproductive Health and Population and Development Act of 2010 on the grounds that the provisions of the RH Bill as such could constitute violations of the bioethical principles cited and the practice of sound medicine on the part of the health service providers. Physicians and policy makers should understand and respect the beliefs of patients who consider human life to be present and valuable from the moment of fertilization.
(John Paul II, Address to the U.N. Economic Commission for Latin America and the Caribbean, April, 1987)
14
You might also like
- Benefits & Issues With Birth Control - Based On The Teachings Of Dr. Andrew Huberman: A Double-Edged Sword – Discovering The Positives And PitfallsFrom EverandBenefits & Issues With Birth Control - Based On The Teachings Of Dr. Andrew Huberman: A Double-Edged Sword – Discovering The Positives And PitfallsNo ratings yet
- RH BillDocument13 pagesRH BillDr. Liza ManaloNo ratings yet
- Contraception for the Medically Challenging PatientFrom EverandContraception for the Medically Challenging PatientRebecca H. AllenNo ratings yet
- ReportDocument13 pagesReportapi-663135887No ratings yet
- Preconception Health and Care: A Life Course ApproachFrom EverandPreconception Health and Care: A Life Course ApproachJill ShaweNo ratings yet
- Summary Afp-2.Rh BillDocument30 pagesSummary Afp-2.Rh BillRyanna Ang-angcoNo ratings yet
- Long Life Strategy: A guidebook for living a longer, healthier, and more fulfilling lifeFrom EverandLong Life Strategy: A guidebook for living a longer, healthier, and more fulfilling lifeNo ratings yet
- ReportDocument13 pagesReportapi-663410827No ratings yet
- Life-Long Health: Learn How to Control Your Genes to Stay Young With AgeFrom EverandLife-Long Health: Learn How to Control Your Genes to Stay Young With AgeNo ratings yet
- RHBill - A Deeper Look at ..Document8 pagesRHBill - A Deeper Look at ..CBCP for LifeNo ratings yet
- Finaldraft AbortionDocument9 pagesFinaldraft Abortionapi-281584433No ratings yet
- Belisa AliyiDocument10 pagesBelisa AliyijonamarekefaleNo ratings yet
- Contraceptives: Abortifacient or NotDocument6 pagesContraceptives: Abortifacient or NotCamille LlorenteNo ratings yet
- Article Campaign About Infertility Science 3rd GradingDocument5 pagesArticle Campaign About Infertility Science 3rd GradingJerson GenerNo ratings yet
- ContraceptionDocument10 pagesContraceptionLolPaolulNo ratings yet
- What Is ContraceptionDocument10 pagesWhat Is ContraceptionLolPaolulNo ratings yet
- Senior Research ProjectDocument11 pagesSenior Research Projectapi-244845748No ratings yet
- Infertility, A Basic InformationDocument15 pagesInfertility, A Basic InformationRajesha KodagNo ratings yet
- Brunke T n332 EthicalpaperDocument13 pagesBrunke T n332 Ethicalpaperapi-260168909No ratings yet
- Javon WitherspoonDocument6 pagesJavon Witherspoonapi-445367279No ratings yet
- The Reproductive Health Bill 5043Document4 pagesThe Reproductive Health Bill 5043delacruzg63No ratings yet
- Oral Contraceptives and Their Effect On Women in The Modern SocietyDocument10 pagesOral Contraceptives and Their Effect On Women in The Modern SocietyDorotea ŠvrakaNo ratings yet
- Debate GUIDE PDFDocument8 pagesDebate GUIDE PDFBlesse PateñoNo ratings yet
- Advances in Male Contraception: Stephanie T. Page, John K. Amory, and William J. BremnerDocument29 pagesAdvances in Male Contraception: Stephanie T. Page, John K. Amory, and William J. BremnerLinguumNo ratings yet
- 5the Pill Byron Mar 2006Document2 pages5the Pill Byron Mar 2006Veronica CristeaNo ratings yet
- Conttraception AssignmentDocument10 pagesConttraception AssignmentMaria Hazel AbayaNo ratings yet
- Bio Project CorrectedDocument35 pagesBio Project CorrectedSABARI SRINIVAS ANo ratings yet
- DP 203Document63 pagesDP 203charu parasherNo ratings yet
- Reproductive Health: in Urban TerritoriesDocument16 pagesReproductive Health: in Urban TerritoriesSiddharth JainNo ratings yet
- Chapter 3Document2 pagesChapter 3Bhavnesh ChoudharyNo ratings yet
- wp3 2Document10 pageswp3 2api-457368313No ratings yet
- NSG 106Document12 pagesNSG 106Anipah AmintaoNo ratings yet
- In Partial Fullfilment in Requirements in Practical Research 2Document7 pagesIn Partial Fullfilment in Requirements in Practical Research 2Famella JaneNo ratings yet
- © Ncert Not To Be Republished: Reproductive HealthDocument10 pages© Ncert Not To Be Republished: Reproductive HealthMothi KarunaNo ratings yet
- Research Paper 3Document12 pagesResearch Paper 3api-534311862No ratings yet
- Anticipating PGDDocument10 pagesAnticipating PGDArlin Chyntia DewiNo ratings yet
- Concept Tutorial: Presented byDocument35 pagesConcept Tutorial: Presented byBhavna SinghNo ratings yet
- Bio Infertility EditedDocument9 pagesBio Infertility EditedSABARI SRINIVAS ANo ratings yet
- ResearchDocument12 pagesResearchHannahNo ratings yet
- 12th Class Biology Ncert Chap-4Document10 pages12th Class Biology Ncert Chap-4Prathyusha MannemNo ratings yet
- Camp Testimony 2011-01-12Document6 pagesCamp Testimony 2011-01-12rosieNo ratings yet
- SandraDocument27 pagesSandraapi-289502576No ratings yet
- Best Practice & Research Clinical Obstetrics and GynaecologyDocument12 pagesBest Practice & Research Clinical Obstetrics and GynaecologyAndhika MaulinaNo ratings yet
- New Advances in Contraceptive Methods: ISSN 2347-3614Document10 pagesNew Advances in Contraceptive Methods: ISSN 2347-3614ArumaiselviNo ratings yet
- New Advances in Contraceptive Methods: ISSN 2347-3614Document10 pagesNew Advances in Contraceptive Methods: ISSN 2347-3614ArumaiselviNo ratings yet
- Who 2011 Lagman RequestDocument5 pagesWho 2011 Lagman RequestMulat Pinoy-Kabataan News NetworkNo ratings yet
- Capstone Final Paper MasterDocument24 pagesCapstone Final Paper Masterapi-667931371No ratings yet
- Research Project GodwinDocument51 pagesResearch Project GodwinBless UgbongNo ratings yet
- Ational Ublic Ealth Ction Lan: N P H A PDocument26 pagesAtional Ublic Ealth Ction Lan: N P H A PAbhay RanaNo ratings yet
- Family Planning 2 LessonDocument50 pagesFamily Planning 2 LessonAhmed AcxNo ratings yet
- Abortion and Womens Health - April 2017Document28 pagesAbortion and Womens Health - April 2017Gabriel SantosNo ratings yet
- AnnotationDocument2 pagesAnnotationJannah Monaliza BambaNo ratings yet
- Biology ProjectDocument9 pagesBiology ProjectNitesh JaiswalNo ratings yet
- Notes 230606 103749 FebDocument5 pagesNotes 230606 103749 FebAadilNo ratings yet
- Presentation and Report Mai ConsDocument3 pagesPresentation and Report Mai ConsLama El NajdiNo ratings yet
- Global Perspective Research PaperDocument7 pagesGlobal Perspective Research Paperpyt.jaraiii123No ratings yet
- Biology Class-12 Chapter-4Document5 pagesBiology Class-12 Chapter-4mokanrajan141106No ratings yet
- Essay 2 MartinezDocument6 pagesEssay 2 Martinezapi-644311691No ratings yet
- Late Termination of Pregnancy. Professional Dilemmas: Isack Kandel and Joav MerrickDocument11 pagesLate Termination of Pregnancy. Professional Dilemmas: Isack Kandel and Joav Merrickvyola chaniaNo ratings yet
- Ob Study Guide #1Document10 pagesOb Study Guide #1Leah ElizabethNo ratings yet
- Aleluya, Credo, Prayer of The Faithful (MVF, SJ) Papal MassDocument1 pageAleluya, Credo, Prayer of The Faithful (MVF, SJ) Papal MassCarmina Dullas LucatinNo ratings yet
- Supreme Court Temporary Restraining Order On The Implementation of RA 10354Document4 pagesSupreme Court Temporary Restraining Order On The Implementation of RA 10354CBCP for LifeNo ratings yet
- SWS Opinion Survey On DivorceDocument10 pagesSWS Opinion Survey On DivorceCBCP for LifeNo ratings yet
- 2 PageSummary RH Decision 2Document2 pages2 PageSummary RH Decision 2CBCP for LifeNo ratings yet
- House Bill 5373 - RH Law Repeal ActDocument3 pagesHouse Bill 5373 - RH Law Repeal ActCBCP for LifeNo ratings yet
- Supreme Court Temporary Restraining Order On The Implementation of RA 10354Document4 pagesSupreme Court Temporary Restraining Order On The Implementation of RA 10354CBCP for LifeNo ratings yet
- 109th Plenary Assembly - FINAL Pastoral Guidance On The Implementation of The RH LawDocument4 pages109th Plenary Assembly - FINAL Pastoral Guidance On The Implementation of The RH LawCBCP for LifeNo ratings yet
- TanDem Complaint Impeachment AquinoDocument13 pagesTanDem Complaint Impeachment AquinoCBCP for LifeNo ratings yet
- Texts of The Magisterium On The Subject of The Divorced and Remarried FaithfulDocument55 pagesTexts of The Magisterium On The Subject of The Divorced and Remarried FaithfulCBCP for LifeNo ratings yet
- DAP ProjectsDocument19 pagesDAP ProjectsJojo MaligNo ratings yet
- A Primer On The Beliefs of The Iglesia Ni KristoDocument20 pagesA Primer On The Beliefs of The Iglesia Ni KristoRev. Fr. Jessie Somosierra, Jr.0% (1)
- Justice Brion Separate Concurring OpinionDocument43 pagesJustice Brion Separate Concurring OpinionCBCP for LifeNo ratings yet
- An Act Prohibiting Discrimination On The Basis of Sexual Orientation and GenderDocument6 pagesAn Act Prohibiting Discrimination On The Basis of Sexual Orientation and GenderCBCP for LifeNo ratings yet
- 109th Plenary Assembly - FINAL Pastoral Letter On Papal VisitDocument4 pages109th Plenary Assembly - FINAL Pastoral Letter On Papal VisitCBCP for LifeNo ratings yet
- Justice de Castro Concurring Opinion PDFDocument54 pagesJustice de Castro Concurring Opinion PDFCBCP for LifeNo ratings yet
- Office of The Solicitor General Reply For DOH & FDA On IUD 02 July 2014Document1 pageOffice of The Solicitor General Reply For DOH & FDA On IUD 02 July 2014CBCP for LifeNo ratings yet
- 109th Plenary Assembly - FINAL Pastoral Exhortation (The JOY of INTEGRITY)Document5 pages109th Plenary Assembly - FINAL Pastoral Exhortation (The JOY of INTEGRITY)CBCP for LifeNo ratings yet
- Justice Reyes Concurring and Dissenting Opinion PDFDocument32 pagesJustice Reyes Concurring and Dissenting Opinion PDFCBCP for LifeNo ratings yet
- Pastoral Guide On The Christian Understanding of Health Vs RH LawDocument5 pagesPastoral Guide On The Christian Understanding of Health Vs RH LawCBCP for LifeNo ratings yet
- Prolife Letter To DOH On IUDDocument3 pagesProlife Letter To DOH On IUDCBCP for LifeNo ratings yet
- G.R. 204819 Reproductive Health (RH) Law Dissenting Opinion Justice Marvic LeonenDocument90 pagesG.R. 204819 Reproductive Health (RH) Law Dissenting Opinion Justice Marvic LeonenHornbook RuleNo ratings yet
- RH Law Concurring Opinion Justice CarpioDocument3 pagesRH Law Concurring Opinion Justice CarpioHornbook RuleNo ratings yet
- Justice Bernabe Concurring and Dissenting Opinion PDFDocument14 pagesJustice Bernabe Concurring and Dissenting Opinion PDFCBCP for LifeNo ratings yet
- Prolife Letter To FDA On IUDDocument3 pagesProlife Letter To FDA On IUDCBCP for LifeNo ratings yet
- Justice Del Castillo Concurring and Dissenting OpinionDocument72 pagesJustice Del Castillo Concurring and Dissenting OpinionCBCP for LifeNo ratings yet
- Imbong vs. Judge Ochoa, JRDocument106 pagesImbong vs. Judge Ochoa, JRPeterD'Rock WithJason D'ArgonautNo ratings yet
- Justice Abad Concurring Opinion PDFDocument22 pagesJustice Abad Concurring Opinion PDFCBCP for LifeNo ratings yet
- Annex AAADocument10 pagesAnnex AAACBCP for LifeNo ratings yet
- IRR RA 10354 RH LawDocument81 pagesIRR RA 10354 RH LawCBCP for LifeNo ratings yet
- Annex AAADocument10 pagesAnnex AAACBCP for LifeNo ratings yet
- Republic of The Philippines Division of Bohol Department of Education Region VII, Central VisayasDocument6 pagesRepublic of The Philippines Division of Bohol Department of Education Region VII, Central VisayasJOHN MC RAE RACINESNo ratings yet
- CCDocument5 pagesCCnazmulNo ratings yet
- Engineering DrawingDocument1 pageEngineering DrawingDreamtech PressNo ratings yet
- Science and Technology in Ancient India by NeneDocument274 pagesScience and Technology in Ancient India by NeneAshok Nene100% (1)
- Crisis of The World Split Apart: Solzhenitsyn On The WestDocument52 pagesCrisis of The World Split Apart: Solzhenitsyn On The WestdodnkaNo ratings yet
- SICHEM Brochure 2023Document8 pagesSICHEM Brochure 2023krishnarao badisaNo ratings yet
- Cool Fire Manual 45M620N2UK 01 PDFDocument198 pagesCool Fire Manual 45M620N2UK 01 PDFPaun MihaiNo ratings yet
- Play ClawDocument2 pagesPlay ClawFrenda SeivelunNo ratings yet
- Bioinformatics Computing II: MotivationDocument7 pagesBioinformatics Computing II: MotivationTasmia SaleemNo ratings yet
- Healthymagination at Ge Healthcare SystemsDocument5 pagesHealthymagination at Ge Healthcare SystemsPrashant Pratap Singh100% (1)
- International Freight 01Document5 pagesInternational Freight 01mature.ones1043No ratings yet
- Low Speed Aerators PDFDocument13 pagesLow Speed Aerators PDFDgk RajuNo ratings yet
- Ismb ItpDocument3 pagesIsmb ItpKumar AbhishekNo ratings yet
- Community Architecture Concept PDFDocument11 pagesCommunity Architecture Concept PDFdeanNo ratings yet
- Xtype Power Train DTC SummariesDocument53 pagesXtype Power Train DTC Summariescardude45750No ratings yet
- Project Chalk CorrectionDocument85 pagesProject Chalk CorrectionEmeka Nicholas Ibekwe100% (6)
- Enzymes IntroDocument33 pagesEnzymes IntropragyasimsNo ratings yet
- Beyond Models and Metaphors Complexity Theory, Systems Thinking and - Bousquet & CurtisDocument21 pagesBeyond Models and Metaphors Complexity Theory, Systems Thinking and - Bousquet & CurtisEra B. LargisNo ratings yet
- How To Add Attachment Using JAVA MappingDocument4 pagesHow To Add Attachment Using JAVA MappingmvrooyenNo ratings yet
- Stonehell Dungeon 1 Down Night Haunted Halls (LL)Document138 pagesStonehell Dungeon 1 Down Night Haunted Halls (LL)some dude100% (9)
- SecurityFund PPT 1.1Document13 pagesSecurityFund PPT 1.1Fmunoz MunozNo ratings yet
- Environmental Science 13th Edition Miller Test BankDocument18 pagesEnvironmental Science 13th Edition Miller Test Bankmarykirbyifsartwckp100% (14)
- The Great Muslim Scientist - Imam Jaffer Sadiq (ADocument78 pagesThe Great Muslim Scientist - Imam Jaffer Sadiq (ASalman Book Centre100% (2)
- Paul Spicker - The Welfare State A General TheoryDocument162 pagesPaul Spicker - The Welfare State A General TheoryTista ArumNo ratings yet
- Digital Electronics Chapter 5Document30 pagesDigital Electronics Chapter 5Pious TraderNo ratings yet
- Chief Complaint: History TakingDocument9 pagesChief Complaint: History TakingMohamad ZulfikarNo ratings yet
- Daily Lesson Log Quarter 1 Week 1Document5 pagesDaily Lesson Log Quarter 1 Week 1John Patrick Famadulan100% (1)
- Extract The .Msi FilesDocument2 pagesExtract The .Msi FilesvladimirNo ratings yet
- Erosional VelocityDocument15 pagesErosional VelocityGary JonesNo ratings yet
- Summative Reflection CommDocument5 pagesSummative Reflection Commapi-546460750No ratings yet
- The Obesity Code: Unlocking the Secrets of Weight LossFrom EverandThe Obesity Code: Unlocking the Secrets of Weight LossRating: 4 out of 5 stars4/5 (6)
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsFrom EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsNo ratings yet
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeFrom EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeRating: 2 out of 5 stars2/5 (1)
- The Age of Magical Overthinking: Notes on Modern IrrationalityFrom EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityRating: 4 out of 5 stars4/5 (24)
- The Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaFrom EverandThe Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaRating: 4.5 out of 5 stars4.5/5 (266)
- Summary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisFrom EverandSummary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisRating: 4.5 out of 5 stars4.5/5 (42)
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedFrom EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedRating: 5 out of 5 stars5/5 (80)
- ADHD is Awesome: A Guide to (Mostly) Thriving with ADHDFrom EverandADHD is Awesome: A Guide to (Mostly) Thriving with ADHDRating: 5 out of 5 stars5/5 (1)
- Self-Care for Autistic People: 100+ Ways to Recharge, De-Stress, and Unmask!From EverandSelf-Care for Autistic People: 100+ Ways to Recharge, De-Stress, and Unmask!Rating: 5 out of 5 stars5/5 (1)
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsFrom EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsRating: 5 out of 5 stars5/5 (1)
- Outlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisFrom EverandOutlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisRating: 4 out of 5 stars4/5 (1)
- Dark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.From EverandDark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Rating: 4.5 out of 5 stars4.5/5 (110)
- Gut: the new and revised Sunday Times bestsellerFrom EverandGut: the new and revised Sunday Times bestsellerRating: 4 out of 5 stars4/5 (392)
- Why We Die: The New Science of Aging and the Quest for ImmortalityFrom EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityRating: 4 out of 5 stars4/5 (3)
- Raising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsFrom EverandRaising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsRating: 4.5 out of 5 stars4.5/5 (169)
- Cult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryFrom EverandCult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryRating: 4 out of 5 stars4/5 (44)
- Mindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessFrom EverandMindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessRating: 4.5 out of 5 stars4.5/5 (328)
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsFrom EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsRating: 3.5 out of 5 stars3.5/5 (3)
- When the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisFrom EverandWhen the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisRating: 3.5 out of 5 stars3.5/5 (2)
- Sleep Stories for Adults: Overcome Insomnia and Find a Peaceful AwakeningFrom EverandSleep Stories for Adults: Overcome Insomnia and Find a Peaceful AwakeningRating: 4 out of 5 stars4/5 (3)
- Gut: The Inside Story of Our Body's Most Underrated Organ (Revised Edition)From EverandGut: The Inside Story of Our Body's Most Underrated Organ (Revised Edition)Rating: 4 out of 5 stars4/5 (378)
- To Explain the World: The Discovery of Modern ScienceFrom EverandTo Explain the World: The Discovery of Modern ScienceRating: 3.5 out of 5 stars3.5/5 (51)
- The Marshmallow Test: Mastering Self-ControlFrom EverandThe Marshmallow Test: Mastering Self-ControlRating: 4.5 out of 5 stars4.5/5 (58)