Professional Documents
Culture Documents
NCP For Preterm
Uploaded by
jenny_justo9136Original Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
NCP For Preterm
Uploaded by
jenny_justo9136Copyright:
Available Formats
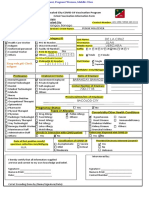
NURSING CARE PLAN ASSESSMENT DIAGNOSISINFERENCEPLANNINGINTERVENTIONRATIONALEEVALUATION Subjective:Bigla na lang humilabangtiyan ko, parang manganganak na ko ( I feel a sudden contraction, I thought
I am in labor ) as verbalized by patient.Objective:
Continued uterine contraction.
Facial mask of pain.
Irritability.
V/S taken as follows:T:37.3 P:84 R:19 Bp: 100/80
Activity intolerance related to muscle or cellular hypersensitivity.
Preterm labor is defined as uterine contractions occurring after 20 weeks of gestation and before 37 completed weeks of gestation. Risk factors include multiple gestation, history of previous preterm labor of delivery, abdominal surgery during current pregnancy, uterine anomaly,
After 8hoursof nursing interventions, the patientwill use identified techniques to enhance activity intolerance. Independent:
Assess status of the client and fetus.
Encourage bed rest with patientin side lying position.
Apply external uterine and fetal monitoring.
Monitor patients vital signs closely, every 15 minutes.
Instruct patient to report any feelings of difficulty of breathing or chest pain, dizziness,
Assessment provides a baseline date for future comparisons.
Bed rest relieves pressure of the fetus on the cervix.
Uterine and fetal monitoring provides evidence of maternal and fetal well being.
Maternal pulse over 120 beats per minute or persistent tachycardia or tachypnea, chest pain, dyspnea and adventitious breath sounds may indicate impending pulmonary edema.
Early recognition of possible adverse effects allows for prompt intervention.
After 8 hours of nursing interventions, the patient was able to use identified techniques to enhance activity intolerance.history of cone biopsy,maternal age younger than 20 or older than age 35. nervousness and irregular heart beats.
Monitor uterine contractions, including frequency and domain.Collaborative:
Obtain diagnostic studies including complete blood count, hemoglobin and hematocrit, urine, vaginal ang cervical cultures as ordered.
Monitor of uterine contractions provides evidence of effective therapy.
Urine, vaginal, and cervical cultures help to rule out infection as a causative factor for preterm labor.
PATIENT: P.F. AGE: 19 years old CUES
CC: Pelvic pressure and abdominal cramps ATTENDING PHYSICIAN: Dr. K.G. S.M. NURSING DIAGNOSIS Ineffective tissue perfusion related to vasoconstriction of blood vessels OBJECTIVE NURSING INTERVENTIONS Independent: > Monitor patients vital signs closely, every 15 minutes. RATIONALE EVALUATION
Subjective: Bigla na lang humilab ang tiyan ko, parang manganganak na ko (I feel a sudden contraction, I thought I am in labor) as verbalized by patient. Objective: Continued uterine contraction. Facial mask of pain. V/S taken as follows: >Temperature:36 C/ax >PR: 83 BPM >RR: 21 BPM >Activity intolerance related to muscle or cellular hypersensitivity.
General: To facilitate maintenance of regulatory mechanisms and functions. Specific: After 8hoursof nursing interventions, the patient will use identified techniques to enhance activity intolerance. > participate in activities that reduce blood pressure or cardiac work load. > minimize edema on upper extremities > client will come quiet or sleep.
Goal partially met. >Maternal pulse over 120 beats per minute or persistent tachycardia or tachypnea, chest pain, dyspnea and adventitious breath sounds may indicate impending pulmonary edema. > Assessment provides a baseline date for future comparisons. > Bed rest relieves pressure of the fetus on the cervix. > Uterine and fetal monitoring provides evidence of maternal and fetal well being. >Early recognition of possible adverse effects allows for prompt intervention. After 8 hours of nursing interventions, the patient was able to use identified techniques to enhance activity intolerance. History of cone biopsy, maternal age younger than 20 or older than age 35. Nervousness and irregular heartbeats.
> Assess status of the client and fetus.
> Encourage bed rest with patient in side lying position. > Apply external uterine and fetal monitoring.
> Instruct patient to report any feelings of difficulty of breathing or chest pain, dizziness, Collaborative: > Monitor uterine contractions, including frequency and domain.
> Obtain diagnostic studies including complete blood count, hemoglobin and hematocrit, urine, vaginal ang cervical cultures as ordered.
> Monitor of uterine contractions provides evidence of effective therapy. >Urine, vaginal, and cervical cultures help to rule out infection as a causative factor for preterm labor.
Secondhand smoke is linked to chronic sinus disease By: Susan Aldridge, medical journalist, PhD Chronic sinus disease is more common a among people who have been exposed to secondhand smoke, according to a new study. There are more than 4,000 compounds in secondhand smoke, including more than 50 that are known to cause cancer or which are suspected of doing so. Previous studies have linked secondhand smoke to many health problems, including lung and ear disease, asthma, heart disease and even some cancers. A team at Brock University, Canada, looked at a group of 306 non-smoking patients who had been diagnosed with chronic sinus disease. That is, they had been diagnosed with having a chronic inflammation of the sinuses for 12 weeks or more. Their exposure to secondhand smoke at home, work, in public places, or at private social functions, during the five years before their diagnosis was compared to that of a group of 306 similar individuals who did not have chronic sinus disease. Those with chronic sinus disease were more likely than the controls to have been exposed to secondhand smoke at home, at work, in public places or at private social functions. There was a doseresponse relationship with those exposed to secondhand smoke in more of the four types of venues being the most likely to develop chronic sinus disease. Overall, it looked as if 40% of cases of chronic sinus disease could be attributed to exposure to secondhand smoke. The researchers are not sure of the underlying mechanism for the connection between secondhand smoke exposure and chronic sinus disease. Exposure might increase susceptibility to upper respiratory infection, or decrease immunity. We already know that exposure to secondhand smoke is linked to other diseases. These new findings suggest that exposure may also cause chronic sinus disease. Therefore, the increasing trend towards banning smoking in public places may help keep your sinuses healthy.
Source: Tammemagi C et al Secondhand smoke as a potential cause of chronic rhinosinusitis Archives of Otolarynology Head and Neck Surgery April 2010;136:327-334
Created on: 05/20/2010 Reviewed on: 05/20/2010
MONDAY, Jan. 10 (HealthDay News) -- Extremely obese people had a significantly greater chance of dying than did others infected with the H1N1 swine flu virus that became a pandemic last winter, a new study reports. Researchers analyzed data from 500 adults hospitalized in California with H1N1 flu during the first four months of 2009 and found that extreme obesity was associated with a nearly three-fold increased risk for death. Extreme obesity is defined as having a body-mass index (BMI) of 40 or greater. BMI is a statistical measure of whether a person is normal, overweight or obese based on whether weight and height are in proportion. The study, published online Jan. 5 and in the Feb. 1 print issue of Clinical Infectious Diseases, did not include data on people who were pregnant or younger than 20. Dr. Janice K. Louie, of the California Department of Health and a study author, said that further research is needed to learn more about why extremely obese people were more likely to die from H1N1 infection. "Extremely obese persons ... should get vaccinated annually for influenza," she said in a news release from the journal. "They should also see their health provider earlier if symptoms of influenza develop so that they can get diagnosed and treated as quickly as possible. This is especially important if the influenza virus is known to be circulating in the community and causing illness." More information The American Lung Association has more about influenza. http://health.usnews.com/health-news/family-health/respiratory-disorders/articles/2011/01/10/for-the-veryobese-h1n1-was-more-apt-to-be-fatal
Seekiing A New Approach To A TB Vaccine Main Category: Tuberculosis Also Included In: Immune System / Vaccines Article Date: 26 Jan 2011 - 5:00 PST
WHAT: A team of U.S. and European researchers have found that a new vaccine strategy tested in mice provides stronger, more long-lasting protection from tuberculosis (TB) infection than the vaccine currently used in humans, known as BCG. Their findings were published online on January 23rd in the journal Nature Medicine. The study was co-funded by the National Institute of Allergy and Infectious Diseases (NIAID), part of the National Institutes of Health, and the Bill & Melinda Gates Foundation. It was coordinated by the NIAIDfunded TB Vaccine Testing and Research Materials program at Colorado State University, an initiative to speed the development of new TB vaccines and treatments. Caused by the bacterium Mycobacterium tuberculosis (Mtb), TB remains one of the major causes of disability and death worldwide, with an estimated 1.7 million deaths in 2009 and increasing rates of drugresistant disease. The BCG vaccine, the only one approved for human use, provides some protection against initial TB illness but does not prevent latent infection, in which Mtb persists in human cells for years and may later develop into active disease. In this study, the researchers combined two proteins previously found to improve the BCG vaccine's effectiveness with a new component, a stress response protein that mice produce throughout the TB infection process. This three-component vaccine, known as H56, was administered to uninfected mice before and after BCG vaccination. Six weeks later, the mice were exposed to Mtb. The multistage strategy not only protected against initial illness, but controlled reactivation of latent infection and reduced Mtb levels in the lungs more effectively than BCG alone. Because of the success of this study, the vaccine candidate is now entering clinical development. Notes: For more information, see the NIAID Tuberculosis Web portal. ARTICLE: C Aagaard et al. A multistage tuberculosis vaccine that confers efficient protection before and after exposure. Nature Medicine. DOI: 10.1038/nm.2285 (2011). WHO: Christine Sizemore, Ph.D., chief of the Tuberculosis, Leprosy and other Mycobacterial Diseases Section at NIAID. Source: Nalini Padmanabhan NIH/National Institute of Allergy and Infectious Diseases
WEDNESDAY, Jan. 19 (HealthDay News) -- Intensive care patients who may be infected with strains of pneumonia that are resistant to many drugs may be more likely to die if current treatment guidelines are followed, a new study suggests. The findings highlight the need to reassess the American Thoracic Society (ATS) and the Infectious Diseases Society of America (IDSA) guidelines, said the researchers. Current guidelines call for immediate antibiotic treatment -- before culture results are known -- of patients at risk for multiple drug-resistant (MDR) infection. The guidelines state that patients should receive a regimen of three antibiotics: two drugs against so-called Gram-negative pathogens and one drug against methicillin-resistant Staphylococcus aureus, or MRSA. The logic in this approach is that at least one drug should be active against any likely infectious agent. However, several studies conducted since the guidelines were released in 2005 have failed to show that dual Gram-negative therapy is better than treatment with a single drug, the researchers noted. For their study, a team led by Dr. Daniel Kett, of the University of Miami Miller School of Medicine, enrolled 303 patients at risk for MDR pneumonia from four academic medical centers in the United States. Of those patients, 129 were treated according to the ATS/IDSA guidelines and 174 received a different treatment. The rate of survival after 28 days was 65 percent in the guidelines-compliant group and 79 percent in the group that didn't adhere to the guidelines, the investigators found. "Our results further question the need for combination Gram-negative empirical treatment for patients with pneumonia, even those who are severely ill and at risk of multi-drug resistant pathogens," the researchers wrote. One expert was not surprised by the findings. "Who gets pneumonia with resistant bacteria? It is a person in such weakened condition that they are vulnerable to pathogens that would otherwise be trivial," noted Dr. Bruce Hirsch, attending physician in the infectious diseases division at North Shore University Hospital in Manhasset, N.Y. "It is a person who has suffered multiple infections already and has been exposed to multiple courses of antibiotics. It is a person with structural lung abnormalities that prevent the lungs from recovering from infections." According to Hirsch, the new study "demonstrates high mortality rates in patients given recommended antibiotics as well as individualized antibiotics. Even in this age of sophisticated and powerful medications, adherence to the best guidelines can fail us." For their part, the study authors "recommend that the planned, revised ATS-IDSA guidelines be reassessed before widespread implementation. Since the most common reason for non-compliance was failure to use a secondary anti-Gram-negative drug, we suggest a comparison of regimens employing MRSA treatment and single versus dual Gram-negative coverage." The study was published in the Jan. 19 online edition of The Lancet Infectious Diseases. More information The American Lung Association has more about pneumonia.
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Essentials of Palliative CareDocument525 pagesEssentials of Palliative Caretaha100% (2)
- Med 02 2023Document19 pagesMed 02 2023Nimer Abdelhadi AliNo ratings yet
- Introduction To Language and Linguistics BIT10703 Ahmad Taufik Hidayah Bin AbdullahDocument5 pagesIntroduction To Language and Linguistics BIT10703 Ahmad Taufik Hidayah Bin AbdullahMuhammad Ikhwan RosmanNo ratings yet
- ACLS Megacode Testing ScenariosDocument12 pagesACLS Megacode Testing Scenariosealm10100% (2)
- Ultrasonography of The EyeDocument8 pagesUltrasonography of The Eyetaner_soysurenNo ratings yet
- Toxicology Rotation ReportDocument36 pagesToxicology Rotation ReportJE AsuncionNo ratings yet
- ADULT Nutrition Screening Questionnaire 2Document1 pageADULT Nutrition Screening Questionnaire 2Alejandra López SalasNo ratings yet
- Physical Therapy Modalities and Rehabilitation Techniques in The Treatment of Neuropathic Pain jpmr.1000124 PDFDocument4 pagesPhysical Therapy Modalities and Rehabilitation Techniques in The Treatment of Neuropathic Pain jpmr.1000124 PDFvinika ChaudharyNo ratings yet
- Patient ProfileDocument19 pagesPatient Profilebangus08No ratings yet
- Daftar Pustaka - 1Document4 pagesDaftar Pustaka - 1Rama YeniNo ratings yet
- Unit-3 BPDocument48 pagesUnit-3 BPShreyas ShreyuNo ratings yet
- 7325-300 C-Peptide & Insulin AccuBind VAST ELISA Rev 6Document2 pages7325-300 C-Peptide & Insulin AccuBind VAST ELISA Rev 6Luisa MaríaNo ratings yet
- Derma BriefDocument7 pagesDerma BriefjeharatNo ratings yet
- Vaccination Form (Sample)Document1 pageVaccination Form (Sample)Godfrey Loth Sales Alcansare Jr.No ratings yet
- Abstracts: Annals of OncologyDocument2 pagesAbstracts: Annals of OncologySanghita BiswasNo ratings yet
- ICD-10 CM All Diagnosis and Trigger Codes - Revised 9-17-2015Document6,507 pagesICD-10 CM All Diagnosis and Trigger Codes - Revised 9-17-2015Puskesmas MakaleNo ratings yet
- Ghai 10ed CompetenciesDocument15 pagesGhai 10ed Competenciesghimansi50No ratings yet
- New School Health FormsDocument42 pagesNew School Health FormsJoanna MarieNo ratings yet
- Neoblade Trial Slides For NCRI Bladder Cancer MeetingDocument10 pagesNeoblade Trial Slides For NCRI Bladder Cancer MeetingProf_Nick_JamesNo ratings yet
- Emergency Drug StudyDocument3 pagesEmergency Drug StudyGrace Santos MirandaNo ratings yet
- Kamagra Tablets Are A Outstanding Treatment For EDwmqrm PDFDocument3 pagesKamagra Tablets Are A Outstanding Treatment For EDwmqrm PDFcherryburn67No ratings yet
- ABC Bone CystDocument43 pagesABC Bone CystIrfan Ullah KhanNo ratings yet
- Breast Cancer ScreeningDocument7 pagesBreast Cancer ScreeninglucaassuntiNo ratings yet
- Transverse MyelitisDocument7 pagesTransverse MyelitisAmr BashaNo ratings yet
- Catheter Ablationin in AF With CHFDocument11 pagesCatheter Ablationin in AF With CHFKristian Sudana HartantoNo ratings yet
- Uji Karsinogenik & MutagenikDocument23 pagesUji Karsinogenik & MutagenikMariadi CaniagoNo ratings yet
- PulpotecDocument5 pagesPulpotecRuel MarmolejoNo ratings yet
- Description of Equipment MIN Unit Cost Total Cost X - Ray: Medical Equipment List For Typical District HospitalDocument60 pagesDescription of Equipment MIN Unit Cost Total Cost X - Ray: Medical Equipment List For Typical District Hospitalramesh100% (1)
- Lab Policies Alkaline Phosphatase C311 Lab 8803Document4 pagesLab Policies Alkaline Phosphatase C311 Lab 8803Valdez Francis ZaccheauNo ratings yet
- Assignment 3 Suicide Prevention ProgramDocument20 pagesAssignment 3 Suicide Prevention Programapi-696109851No ratings yet