Professional Documents
Culture Documents
Niacin Therapy For Phosphorus Control in Dialysis
Uploaded by
Marce De LeonOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Niacin Therapy For Phosphorus Control in Dialysis
Uploaded by
Marce De LeonCopyright:
Available Formats
Issues in Renal Nutrition
Focus on Nutritional Care for Nephrology Patients
Ann Cotton, Contributing Editor
Niacin Therapy for Phosphorus Control In Dialysis
Pam Buchholz
or people receiving dialysis, hyperphosphatemia is linked to secondary hyperparathyroidism, bone disease, metastatic calcifications, and cardiovascular risk and mortality (Cheng, Young, Huang, Delmez, & Coyne, 2008). Even with dietary restrictions and the use of phosphorus binders, many individuals with kidney failure will not achieve a phosphorus level of 5.5 mg/dL or less. Niacin is being investigated as another treatment option for phosphorus control because it has been found to inhibit sodium-phosphate co-transport (NaPi2b) in the gastrointestinal tract, thereby decreasing phosphorus absorption (Cheng et al., 2008; Eto, Miyata, Ohno, & Yamashita, 2005). Due to its mode of action, it has the benefit of not relying on mealtimes. Niacin has also been used as an effective treatment of dyslipidemia since the 1950s. Since both hyperphosphatemia and low high-density lipoprotein (HDL) cholesterol are cardiovascular risk factors in the dialysis population, any treatment that could potentially lessen both risk factors with a single medication is worth investigating.
Copyright 2010 American Nephrology Nurses Association Buchholtz, P. (2010). Niacin therapy for phosphorus control in dialysis. Nephrology Nursing Journal, 37(5), 563-564.
flush-free niacin, currently lacks evidence as to effectiveness (Guyton & Bays, 2007).
Studies
Takahashi et al. (2004) used a mean dose of 1080 370 mg/day of nicotinamide, given twice daily in powder form, with 65 individuals on hemodialysis over a period of 12 weeks. Phosphorus binders were stopped, although active vitamin D therapy was allowed to remain constant. Serum phosphorus decreased from 6.9 1.5 to 5.4 1.3 mg/dL. Serum iPTH also decreased from 200 to 150 pg/mL. There was no significant change in serum calcium levels. HDL cholesterol increased from 47.4 14.9 to 67.2 22.3 mg/dL. Sampathkumar, Selvam, Sooraj, Gowthaman, and Ajeshkumar (2006) used extended-release nicotinic acid taken once or twice daily, depending on dose, with 34 individuals on hemodialysis over a period of eight weeks. Phosphorus binders and active vitamin D analogs were stopped during the study. The initial dose was 375 mg/day, with 750 mg/day used if serum phosphorus at the end of two weeks remained above 6 mg/dL. Thirty out of 34 individuals needed only 375 mg/day. Serum phosphorus decreased from 7.7 1.5 to 5.6 1.0 mg/dL. Serum alkaline phosphatase decreased from 107 66 to 82 46 IU/L. Serum calcium increased from 8.1 1.0 to 8.5 1.0 mg/dL. Lipids were not measured. Mller et al. (2007) used a mean dose of 1470 110 mg/day of Niaspan (extended-release nicotinic acid, Abbott Laboratories) with a group of 20 individuals, 19 on hemodialysis and 1 on peritoneal dialysis. Phosphorus binders were stopped, and active vitamin D analogs held steady. The goal was to tolerate at least 1000 mg/day of Niaspan, for which 17 individuals qualified. Of those, 11
Definition
Niacin is a water-soluble vitamin also identified as vitamin B3, with niacin (nicotinic acid) and niacinamide (nicotinamide) being the principle forms. Although nicotinic acid is converted to nicotinamide in the body, they have different modes of action and side effects when used in pharmacological doses. Nicotinic acid has historically been used as an effective treatment of dyslipidemia, while nicotinamide may have some anti-inflammatory effects. Emerging research suggests that nicotinamide may also have a similar effect on dyslipidemia as that of nicotinic acid, most notably the effect of raising HDL cholesterol (Cheng et al., 2008). In the U.S., niacin is available in prescription and overthe-counter formulations: immediate-release (IR), sustained-release (SR), and extended-release (ER). Niacin IR is absorbed most quickly of the three formulations, results in more frequent dosing, and has a higher association with flushing. Niacin SR is absorbed more slowly than the other two formulations but has a higher association with hepatotoxicity. Niacin ER falls between the other two formulations in both absorption rate and metabolic pathways which results in a better safety profile (Berns, 2008; Berra, 2004). Inositol hexanicotinate, often sold as no-flush niacin or
Pam Buchholz, RD, CD, is a Registered Dietitian, DSI Renal, Inc., Greenwood, IN. She may be contacted via e-mail at pbuchholz@dsi-corp.com
The Issues in Renal Nutrition department is designed to focus on nutritional issues for nephrology patients. Address correspondence to: Ann Cotton, Contributing Editor, Nephrology Nursing Journal; East Holly Avenue/Box 56; Pitman, NJ 08071-0056; (856) 256-2320. The opinions and assertions contained herein are the private views of the contributors and do not necessarily reflect the views of the American Nephrology Nurses' Association.
Nephrology Nursing Journal
September-October 2010
Vol. 37, No. 5
563
Niacin Therapy for Phosphorus Control in Dialysis
individuals completed the 12-week study period. Serum phosphorus decreased from 7.2 0.7 to 5.8 0.75 mg/dL. There was no significant change to serum calcium or iPTH levels. Statins were not changed during the study period. An increase in HDL cholesterol from 40 3.2 to 59 5.5 mg/dL was observed. Cheng et al. (2008) completed a randomized, doubleblind, placebo-controlled crossover trial using niacinamide with 33 individuals on hemodialysis. Phosphorus binders, active vitamin D analogs, and calcimimetics were continued without any adjustments unless safety criteria for dosage changes were met. Niacinamide and placebo were packaged in 250 mg capsules, and dosages were titrated from 500 mg/day to 1500 mg/day. After eight weeks, each group underwent a two-week washout period before completing eight weeks with the alternative therapy. Serum phosphorus decreased from 6.26 1.28 to 5.47 1.49 mg/dL with niacinamide; there was no significant change in the placebo group. There were no statistically significant changes to serum calcium or iPTH levels. HDL cholesterol increased from 50 17 to 61 21 mg/dL with niacinamide but not placebo. Restrepo Valencia and Cruz (2008) used Niaspan for eight months with three individuals on hemodialysis and six on peritoneal dialysis. Criteria of both hyperlipidemia and hyperphosphatemia needed to be met to participate. Phosphorus binders and active vitamin D analogs were stopped, but oral statins and gemfibrozil were allowed. After three months, all individuals tolerated 1000 mg of Niaspan. After eight months, serum phosphorus decreased from 6.46 0.53 to 3.94 0.76 mg/dL. Serum calcium increased from 9.63 1.13 to 10.25 0.67 mg/dL. There was no statistically significant change to iPTH levels. HDL cholesterol increased from 45.56 5.62 to 50.22 5.56 mg/dL.
Nausea and vomiting may occur at doses greater than 2000 mg/day. Active peptic ulcer disease is a contraindication for therapy. Niacin may increase uric acid levels, a concern for those with gout, although ER formulations have a smaller impact than IR preparations. Hyperglycemia may result from niacin therapy, but the impact is usually minor (Guyton & Bays, 2007). Conflicting reports concerning thrombocytopenia exist in both frequency and severity.
Conclusion
Based on emerging research, it appears as if both nicotinic acid and nicotinamide decrease serum phosphorus and increase HDL cholesterol levels in individuals undergoing dialysis. Since both hyperphosphatemia and low HDL cholesterol are cardiovascular risk factors for this population, niacin sounds promising. Caution is warranted, however, due to insufficient long-term safety and efficacy data in those receiving dialysis (Berns, 2008). Niacin therapy for phosphorus control should be considered adjunctive therapy at this time, and the healthcare team should closely monitor any person receiving it. References
Berns, J.S. (2008). Niacin and related compounds for treating hyperphosphatemia in dialysis patients. Seminars in Dialysis, 21(3), 203-205. Berra, K. (2004). Clinical update on the use of niacin for the treatment of dyslipidemia. Journal of the American Academy of Nurse Practitioners, 16(12), 526-534. Cheng, S.C., Young, D.O., Huang, Y., Delmez, J.A., & Coyne, D.W. (2008). A randomized, double-blind, placebo-controlled trial of niacinamide for reduction of phosphorus in hemodialysis patients. Clinical Journal of the American Society of Nephrology, 3(4), 1131-1138. Eto, N., Miyata, Y., Ohno, H., & Yamashita, T. (2005). Nicotinamide prevents the development of hyperphosphataemia by suppressing intestinal sodium-dependent phosphate transporter in rats with adenine-induced renal failure. Nephrology Dialysis Transplant, 20(7), 1378-1384. Guyton, J.R., & Bays, H.E. (2007). Safety considerations with niacin therapy. American Journal of Cardiology, 99(6A), 22C31C. Mller, D., Mehling, H., Otto, B., Bergmann-Lips, R., Luft, F., Jordan, J., & Kettritz, R. (2007). Niacin lowers serum phosphate and increases HDL cholesterol in dialysis patients. Clinical Journal of the American Society of Nephrology, 2(6), 12491254. Restrepo Valencia, C.A., & Cruz, J. (2008). Safety and effectiveness of nicotinic acid in the management of patients with chronic renal disease and hyperlipidemia associated to hyperphosphatemia. Nefrologia, 28(1), 61-66. Sampathkumar, K., Selvam, M., Sooraj, Y.S., Gowthaman, S., & Ajeshkumar, R.N. (2006). Extended release nicotinic acid A novel oral agent for phosphate control. International Urology and Nephrology, 38(1), 171-174. Takahashi, Y., Tanaka, A., Nakamura, T., Fukuwatari, T., Shibata, K., Shimada, N., ... Kolde, H. (2004). Nicotinamide suppresses hyperphosphatemia in hemodialysis patients. Kidney International, 65(3), 1099-1104.
Risks and Contraindications
While both nicotinic acid and nicotinamide have doserelated gastrointestinal side effects, only nicotinic acid is associated with flushing. The flushing is a result of prostaglandin-mediated cutaneous vasodilation and is more common in IR than ER formulations (Berra, 2004). Methods to lessen the flushing include starting at low doses and slowly titrating over time. Consistent use will also decrease the frequency and severity of the flushing. Taking a non-steroidal anti-inflammatory drug (NSAID), such as aspirin, 30 minutes to one hour prior to a nicotinic acid dose will help mitigate instances of flushing as will dosing at bedtime (Guyton & Bays, 2007). There has been concern regarding hepatotoxicity with niacin therapy. This is more prevalent with SR than IR or ER formulations, although high enough doses of any preparations may cause problems. Hepatoxicity becomes an issue usually at doses greater than 1500 mg/day for SR formulations and 3000 mg/day or higher for IR formulations (Guyton & Bays, 2007).
564
Nephrology Nursing Journal
September-October 2010
Vol. 37, No. 5
Copyright of Nephrology Nursing Journal is the property of American Nephrology Nurses' Association and its content may not be copied or emailed to multiple sites or posted to a listserv without the copyright holder's express written permission. However, users may print, download, or email articles for individual use.
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5784)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (72)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Doxazosin Mesilate - Martindale 36edDocument1 pageDoxazosin Mesilate - Martindale 36edSvetlana Maiochi LodovicoNo ratings yet
- T1K UpdateDocument24 pagesT1K UpdateolivenanaNo ratings yet
- Colorado Guidelines of Professional Practice For Controlled SubstancesDocument65 pagesColorado Guidelines of Professional Practice For Controlled SubstancesBrian HarrisNo ratings yet
- List of Drug Manufacturers Recognized for ExcellenceDocument2 pagesList of Drug Manufacturers Recognized for Excellencechowder_coronado67% (18)
- Test Farma En-Ro, Ro-EnDocument3 pagesTest Farma En-Ro, Ro-EnIuliaUngurNo ratings yet
- Sinatra ReferenceDocument7 pagesSinatra ReferenceNavisa HaifaNo ratings yet
- BARCODESDocument7 pagesBARCODESChitPerRhosNo ratings yet
- Metoclopramide and Rosuvastatin Nursing ConsiderationsDocument5 pagesMetoclopramide and Rosuvastatin Nursing ConsiderationsDianne NemisNo ratings yet
- Nebu&CPTDocument32 pagesNebu&CPTAbigail Bantayan100% (1)
- The Association Between Stage of Treatment Resistant Depression and Clinical Utility of KetamineesketamineDocument48 pagesThe Association Between Stage of Treatment Resistant Depression and Clinical Utility of KetamineesketamineArgenis SalinasNo ratings yet
- Library G.Pulla Reddy College of Pharmacy Hyderabad: OU - 1705 OU - 1705Document10 pagesLibrary G.Pulla Reddy College of Pharmacy Hyderabad: OU - 1705 OU - 1705A.vidhyavandhanareddyNo ratings yet
- Prescribing Authority TableDocument7 pagesPrescribing Authority TablearifadamjiNo ratings yet
- Curriculum Vitae MTDocument6 pagesCurriculum Vitae MTapi-273097827No ratings yet
- Exotic Hypnosis Inductions - Unusual & Unique Hypnosis TechniquesDocument3 pagesExotic Hypnosis Inductions - Unusual & Unique Hypnosis Techniquesgmeades33% (3)
- Debridement of Large WoundsDocument1 pageDebridement of Large WoundsMeddco helpdeskNo ratings yet
- PPM Arvreferencepricing Table enDocument3 pagesPPM Arvreferencepricing Table enayawe888888No ratings yet
- Review 1. Efficacy and Safety of Cetuximab For CRCDocument13 pagesReview 1. Efficacy and Safety of Cetuximab For CRCcollianairaNo ratings yet
- Cebu Normal University College of Nursing Drug StudyDocument5 pagesCebu Normal University College of Nursing Drug StudyFaye Andrea Francisco100% (1)
- List Harga Quantum UpdateDocument1 pageList Harga Quantum UpdateAde IrawanNo ratings yet
- MMP Handy Chart October 2011 V2Document37 pagesMMP Handy Chart October 2011 V2ColonNo ratings yet
- Netupitant & PalonosetronDocument2 pagesNetupitant & PalonosetronShamim Ahamed ShakilNo ratings yet
- Ventilator The Basic CourseDocument117 pagesVentilator The Basic CourseTputrinya FaniddaNo ratings yet
- 21 AdisaDocument6 pages21 AdisaTri UtariNo ratings yet
- Off-Label Drug Use in Pediatric Patients: ReviewsDocument6 pagesOff-Label Drug Use in Pediatric Patients: ReviewsRestu SNo ratings yet
- Smu066 PDF EngDocument9 pagesSmu066 PDF EngDEREK SANDOVALNo ratings yet
- ΔΤΦ 06082013Document1,140 pagesΔΤΦ 06082013LOUI_GRNo ratings yet
- Telemetry-Intermediate Care Skills ChecklistDocument4 pagesTelemetry-Intermediate Care Skills ChecklistnorthweststaffingNo ratings yet
- 1 PBDocument14 pages1 PBindah marhaniNo ratings yet
- The Morphine Manifesto 2023Document6 pagesThe Morphine Manifesto 2023Fatul Chelseakers ZhinZhaiNo ratings yet
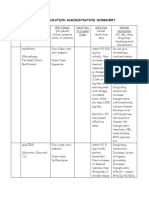
- Medication Administration WorksheetDocument6 pagesMedication Administration WorksheetCheska CarrionNo ratings yet