Professional Documents
Culture Documents
Ricketsiae Bacteria
Uploaded by
Ernie G. Bautista II, RN, MDOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Ricketsiae Bacteria
Uploaded by
Ernie G. Bautista II, RN, MDCopyright:
Available Formats
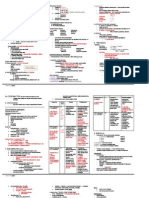
RICKETTSIAE
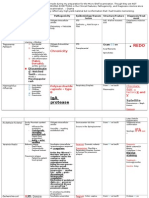
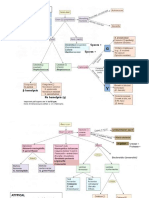
MORPHOLOGY & IDENTIFICATION small (0.3-0.5 x 0.8-2.0 um) gram-negative, pleomorphic, aerobic, obligate intracellular (Energy Parasites) coccobacilli (lack flagella, non-motile) divide by binary fission that may reside in the cytoplasm or within the nucleus of the cell that they invade they metabolize host-derived glutamate via aerobic respiration and the citric acid (TCA) cycle reservoir are animals and arthropds (humans are accidentally infected with these organisms) all are transmitted by arthropod vectors (e.g., ticks, mites, lice or fleas) VECTORS WOOD TICK (Dermacentor andersoni) DOG TICK (Dermacentor variabilis) PATHOGENESIS MOT: inoculated into the dermis of the skin by a tick bite or through damaged skin from the feces of lice or fleas TARGET CELLS: spread through the bloodstream and infect the endothelial cells lining the small blood vessels. Destruction of endothelial cells results in leakage of blood and subsequent organ and tissue damage due to loss of blood into the tissue spaces VIRULENCE FACTORS Adhesins: OmpA (outer membrane protein A)
cytoplasm where they replicate. 3. The mode of exit from the host cell varies depending upon the species - R. prowazekii exits by cell lysis - R. rickettsii get extruded from the cell through local projections (filopodia). F actin in the host cell associates with R. rickettsii and the actin helps to "push" the bacteria through the filopdia - O. tsutsugamushi exits by budding through the cell membrane and remains enveloped in the host cell membrane as it infects other cells. HOST DEFENSES Humoral immunity antibody-opsonized Rickettsia are phagocytosed and killed by macrophages Cell-mediated immunity Delayed type hypersensitivity develops following rickettsial infections. THREE MAJOR GROUPS: (based on clinical characteristics of disease)
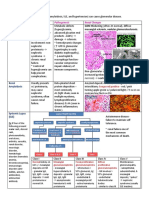
RICKETTSIAL DISEASES (1) ROCKY MOUNTAIN SPOTTED FEVER caused by Rickettsia rickettsii most severe and most frequently reported rickettsial disease in the United States first recognized in 1896 in the Snake River Valley of Idaho and was originally called "black measles" because of the characteristic rash 3-5% mortality (death may occur during the end of the second week due to kidney or heart failure) RESERVOIR: wild rodents(primary) VECTOR: Ixodid (hard) ticks INCUBATION PERIOD: 7 days (range 2-14 days) CLINICAL MANIFESTATIONS: the classic triad of findings for this disease are fever, rash, and history of tick bite severe headache, muscle pain, nausea, vomiting, abdominal pain, and cough The rash typically are painless that appears 2-5 days after onset of illness on the ankles and wrists. Initially begins as small, flat, non-itchy, faint pink 1-5 mm macules that represent a focus of vascular infection and surrounding vasodilation progress to become the characteristic red, spotted (maculopapular) rash of Rocky Mountain spotted fever on the 6th day, owing to the leakage of edema fluid from the affected blood vessels, with the development of a hemorrhage (petechia) in the center of the lesions Early (macular) rash on sole of foot Late (petechial) rash on palm and forearm (2) RICKETTSIALPOX caused by Rickettsia akari RESERVOIR: mite & wild rodents VECTOR: mouse mite INCUBATION PERIOD: 7-24 days CLINICAL SYNDROMES typically a mild disease that has two phases: first phase a papule develops at the site of the mite bite and quickly ulcerates and forms an eschar. This initial phase occurs approximately 1 week after the bite. second phase is characterized by sudden onset of fever, chills headache and myalgia and is followed 2 to 3 days later with a generalized rash. The rash is papulovesicular and crusts over in the later stages. The pox heal within 2 to 3 weeks without scarring. Fatalities are rare
RICKETTSIOSES:
1. Adhere to endothelial cells lining the small blood vessels by parasite-induced phagocytosis 2. Once in the host cell, the bacteria lyse the phagosome membrane with a phospholipase and escape into the host cell
EGBII; 8-15-11
(3)
SCRUB TYPHUS caused by Orientia (Rickettsia) tsutsugamushi occurs in Asia, Australia and the Pacific Islands RESERVOIR: mites and wild rodents VECTOR: chiggers, the larval form of a mite INCUBATION PERIOD: 1-3 weeks CLINICAL SYNDROMES characterized by sudden onset of fever, chills headache and myalgia. maculopapular rash develops 2 - 3 days later. The rash appears first on the trunk and spreads to the extremities (centrifugal spread). Mortality rate in outbreaks are variable.
disease is mild and resolves within 3 weeks even if untreated.
DIAGNOSIS Clinical diagnosis: initial diagnosis Laboratory diagnosis: Direct detection after skin punch tissue biopsy: Giemsa stain Direct/indirect fluorescent antibody test PCR Weil-Felix test (agglutinate OX strains of Proteus vulgaris; no longer recommended) TREATMENT antibiotic treatment should be initiated immediately Doxycycline Drug of choice 100 mg every 12 hours for adults or 4 mg/kg body weight per day in two divided doses for children under 45 kg for a minimum total course of 5 to 10 days Tetracyclines contraindicated in pregnant women because of risks associated with malformation of teeth and bones in unborn children Chloramphenicol is an alternative drug PREVENTION prevention of tick bites protective clothing, insect repellents, etc. tick control no vaccine is available
(4) EPIDEMIC TYPHUS/LOUSE-BORNE TYPHUS caused by Rickettsia prowazekii transmitted by human body louse occurs among people living in crowded, unsanitary conditions such as those found in wars, famine and natural disasters RESERVOIR: humans (primary), squirrel, fleas VECTOR: louse INCUBATION PERIOD: 8 days CLINICAL SYNDROMES Epidemic typhus is characterized by sudden onset of fever, chills, headache, myalgia and arthralgia. After 7 days, maculopapular (can be petechial) rash appears. In contrast to the rash seen with Rocky Mountain Spotted Fever, the rash in epidemic typhus develops on the trunk first and spreads to the extremities (centrifugal spread) Brill-Zinsser disease is recrudescent epidemic typhus. It occurs decades after the initial infection. clinical course of the disease is similar to epidemic typhus but is milder and recovery is faster. The skin rash is rarely seen. diagnosis is made on the basis of a fever with unknown origin and a history of previous exposure to epidemic typhus. (5) MURINE/ENDEMIC TYPHUS caused by Rickettsia typhi occurs worldwide RESERVOIR: rats and cat flea VECTOR: rat flea INCUBATION PERIOD: 1-2 weeks CLINICAL SYNDROMES fever, chills headache and myalgia. rash develops in many but not all cases. The rash begins on the trunk and spreads to the extremities (centrifugal spread).
EGBII; 8-15-11
You might also like
- Herpes, Pox, Rhabdo, Arena VIRUSDocument7 pagesHerpes, Pox, Rhabdo, Arena VIRUSErnie G. Bautista II, RN, MDNo ratings yet
- Antivirals, Rubella, Peecorna VIRUSDocument3 pagesAntivirals, Rubella, Peecorna VIRUSErnie G. Bautista II, RN, MDNo ratings yet
- Parvo BacteriaDocument2 pagesParvo BacteriaErnie G. Bautista II, RN, MDNo ratings yet
- MISC Bacteria (Legionella, Listeria, Gardnerella, Actinobacillus, Bartonella, Calymato-Bacterium, Flavobacterium, Streptobacillus)Document6 pagesMISC Bacteria (Legionella, Listeria, Gardnerella, Actinobacillus, Bartonella, Calymato-Bacterium, Flavobacterium, Streptobacillus)Ernie G. Bautista II, RN, MDNo ratings yet
- Bacteria TableDocument4 pagesBacteria TableBrittany Lynn MyersNo ratings yet
- Major Bacterial Genera TableDocument12 pagesMajor Bacterial Genera TablemojdaNo ratings yet
- Gram Positive BacilliDocument9 pagesGram Positive BacilliRovy JervisNo ratings yet
- Microbiology Key WordsDocument5 pagesMicrobiology Key Wordsmoilo86020% (1)
- Review Parasitology ChartsDocument8 pagesReview Parasitology Chartseezah100% (2)
- Microbiology TablesDocument19 pagesMicrobiology TablesRebecca MarshallNo ratings yet
- Bacterial Virulence FactorsDocument2 pagesBacterial Virulence FactorsJulia IshakNo ratings yet
- Gram Negative Rods GuideDocument8 pagesGram Negative Rods GuideRuel Maddawin100% (1)
- Parasitology TableDocument15 pagesParasitology TableJohn Benedict BondocNo ratings yet
- Parasitic Diseases at a GlanceDocument2 pagesParasitic Diseases at a GlanceStarrie94No ratings yet
- Staphylococcus aureus and Streptococcus viridans Bacteriology ChartDocument13 pagesStaphylococcus aureus and Streptococcus viridans Bacteriology Chartthzone1986No ratings yet
- Mtap - Bacteriology FinalsDocument6 pagesMtap - Bacteriology FinalsMoira Pauline LibroraniaNo ratings yet
- Microbiology: Presented by Alyazeed Hussein, BSCDocument64 pagesMicrobiology: Presented by Alyazeed Hussein, BSCT N100% (1)
- S. Aureus: Bacteriology G Virulence Factors Clinical Diseases Treatment Staphylococcus +Document4 pagesS. Aureus: Bacteriology G Virulence Factors Clinical Diseases Treatment Staphylococcus +MARIA FREDIJEAN CARIÑONo ratings yet
- Sporeforming & Non-Spore Forming BacteriaDocument9 pagesSporeforming & Non-Spore Forming BacteriaErnie G. Bautista II, RN, MD100% (1)
- MICROBIOLOGY LIST BACTERIADocument5 pagesMICROBIOLOGY LIST BACTERIAJaweria Islam Khan BangashNo ratings yet
- Gram staining characteristics and morphologies of common enteric bacteriaDocument4 pagesGram staining characteristics and morphologies of common enteric bacteriakris0% (1)
- Heamtology Reviewer (Midterm)Document15 pagesHeamtology Reviewer (Midterm)Johney DoeNo ratings yet
- Microbiology - Bacteria Summary (Updated)Document26 pagesMicrobiology - Bacteria Summary (Updated)moZZeltovNo ratings yet
- Bacteria Notes SketchyDocument3 pagesBacteria Notes SketchyJayNo ratings yet
- IMS - Immunomodulation & ImmunodeficienciesDocument3 pagesIMS - Immunomodulation & ImmunodeficienciesJeanne RodiñoNo ratings yet
- High Yield - Bacteriology ChartsDocument9 pagesHigh Yield - Bacteriology ChartsAmirsalar EslamiNo ratings yet
- Gram Positive Cocci Reviewer 1Document6 pagesGram Positive Cocci Reviewer 1alianaNo ratings yet
- Biochemical Test MicrobiologyDocument2 pagesBiochemical Test MicrobiologyGab BautistaNo ratings yet
- Gram Positive Cocci Sem 1 1Document45 pagesGram Positive Cocci Sem 1 1Charmaine Corpuz Granil100% (1)
- Microbiology Summary DocumentDocument7 pagesMicrobiology Summary DocumentKNo ratings yet
- ID Bug chart-DKDocument92 pagesID Bug chart-DKNeil M D'SouzaNo ratings yet
- Staphylococci: Streptococcus PyogenesDocument20 pagesStaphylococci: Streptococcus PyogenesPharmacy2015100% (2)
- Structure and Classification of Bacteria: Morpho DifferencesDocument8 pagesStructure and Classification of Bacteria: Morpho DifferencesJaz CNo ratings yet
- Dermatology Resident Roundup Histologic BodiesDocument2 pagesDermatology Resident Roundup Histologic BodiesAreg JosephsNo ratings yet
- A. Staphylococcus Aureus B. Staphylococcus Epidermidis C. Staphylococcus SaprophyticusDocument8 pagesA. Staphylococcus Aureus B. Staphylococcus Epidermidis C. Staphylococcus SaprophyticusRuel MaddawinNo ratings yet
- Antimicrobial Drugs TableDocument19 pagesAntimicrobial Drugs TableLaylee ClareNo ratings yet
- Free Ebook - Microbiology Review Notes by MedpgnotesDocument103 pagesFree Ebook - Microbiology Review Notes by Medpgnotesdr dixit100% (1)
- Family of StreptococcaceaeDocument10 pagesFamily of StreptococcaceaeLovely B. AlipatNo ratings yet
- Micro-Para Practical Exam ReviewerDocument8 pagesMicro-Para Practical Exam ReviewerRA TranceNo ratings yet
- Staph, Strep Bacillus Clostridium Neisseria Pleiomorphic Enterobact-EriceaeDocument2 pagesStaph, Strep Bacillus Clostridium Neisseria Pleiomorphic Enterobact-Ericeaelola100% (1)
- Gram-positive bacteria of medical importance overviewDocument58 pagesGram-positive bacteria of medical importance overviewGx NavinNo ratings yet
- Cocci Rod 4 Main Classifications: Gram Staph, Strep Bacillus Clostridium Neisseria Pleiomorphic Enterobact-EriceaeDocument2 pagesCocci Rod 4 Main Classifications: Gram Staph, Strep Bacillus Clostridium Neisseria Pleiomorphic Enterobact-EriceaeKimberly KanemitsuNo ratings yet
- Pathology B - Gastrointestinal Tract (Esguerra, 2015)Document18 pagesPathology B - Gastrointestinal Tract (Esguerra, 2015)Ars MoriendiNo ratings yet
- Me EnterobacteriaceaeDocument72 pagesMe Enterobacteriaceaewimarshana gamage100% (1)
- Gram Positive BacilliDocument6 pagesGram Positive BacilliSteve ShirmpNo ratings yet
- Navle Master ListDocument60 pagesNavle Master Listhari krishnaa athotaNo ratings yet
- Tables VirusesDocument9 pagesTables VirusesOmphile DansonNo ratings yet
- Subcutaneous Systemic Opportunistic MycosesDocument5 pagesSubcutaneous Systemic Opportunistic MycosesErnie G. Bautista II, RN, MD100% (2)
- Table of Genetic DisordersDocument9 pagesTable of Genetic DisordersjeslymailNo ratings yet
- Antimicrobial Table BasicDocument7 pagesAntimicrobial Table BasicPAschoolstuffNo ratings yet
- Pathology Description/Buzz Words DiseaseDocument5 pagesPathology Description/Buzz Words Diseasebea manzanoNo ratings yet
- The Leukotrienes: Chemistry and BiologyFrom EverandThe Leukotrienes: Chemistry and BiologyLawrence ChakrinNo ratings yet
- Streptococci: S. Pyogenes S. AgalactiaeDocument9 pagesStreptococci: S. Pyogenes S. AgalactiaeChristine BuenNo ratings yet
- Week 7. Renal Pathology Continued.Document9 pagesWeek 7. Renal Pathology Continued.Amber LeJeuneNo ratings yet
- MicrobesDocument12 pagesMicrobesDiMa MarshNo ratings yet
- Antimycobacterial Drugs PDFDocument3 pagesAntimycobacterial Drugs PDFCas BuNo ratings yet
- Genetic and Pediatric Diseases Chapter SummaryDocument16 pagesGenetic and Pediatric Diseases Chapter SummaryJustine HungNo ratings yet
- Bacteria ChartDocument2 pagesBacteria ChartJUSASBNo ratings yet
- Complement SystemDocument4 pagesComplement SystemFait HeeNo ratings yet
- Acne VulgarisDocument49 pagesAcne VulgarisErnie G. Bautista II, RN, MD100% (1)
- Chapter 6 - Immune Diseases (Part II) (Robbins and Cotran Pathologic Basis of Disease)Document3 pagesChapter 6 - Immune Diseases (Part II) (Robbins and Cotran Pathologic Basis of Disease)Ernie G. Bautista II, RN, MD100% (5)
- KCR 2020 Guideline For Scientific ExhibitionDocument2 pagesKCR 2020 Guideline For Scientific ExhibitionErnie G. Bautista II, RN, MDNo ratings yet
- UrolithiasisDocument79 pagesUrolithiasisErnie G. Bautista II, RN, MDNo ratings yet
- Chapter 1 - Cellular Injury, Cell Adaptation & Cell Death (Robbins and Cotran Pathologic Basis of Disease)Document3 pagesChapter 1 - Cellular Injury, Cell Adaptation & Cell Death (Robbins and Cotran Pathologic Basis of Disease)Ernie G. Bautista II, RN, MD91% (34)
- Guide in Reporting Complete Physical Examination (2013) - Source: Bates' Guide To Physical Examination.Document8 pagesGuide in Reporting Complete Physical Examination (2013) - Source: Bates' Guide To Physical Examination.Ernie G. Bautista II, RN, MD100% (6)
- Subcutaneous Systemic Opportunistic MycosesDocument5 pagesSubcutaneous Systemic Opportunistic MycosesErnie G. Bautista II, RN, MD100% (2)
- EnterobacteriaceaeDocument3 pagesEnterobacteriaceaeErnie G. Bautista II, RN, MDNo ratings yet
- Eye and Ear HistologyDocument96 pagesEye and Ear HistologyErnie G. Bautista II, RN, MD100% (1)
- Sporeforming & Non-Spore Forming BacteriaDocument9 pagesSporeforming & Non-Spore Forming BacteriaErnie G. Bautista II, RN, MD100% (1)
- Antimicrobial AgentsDocument3 pagesAntimicrobial AgentsErnie G. Bautista II, RN, MD100% (2)
- AstrocytomaDocument11 pagesAstrocytomaErnie G. Bautista II, RN, MDNo ratings yet
- Histology of Female Reproductive SystemDocument2 pagesHistology of Female Reproductive SystemErnie G. Bautista II, RN, MDNo ratings yet
- Introduction To Nervous SystemDocument4 pagesIntroduction To Nervous SystemErnie G. Bautista II, RN, MD100% (1)
- Histology of Male Reproductive SystemDocument2 pagesHistology of Male Reproductive SystemErnie G. Bautista II, RN, MDNo ratings yet
- Histology of Endocrine SystemDocument1 pageHistology of Endocrine SystemErnie G. Bautista II, RN, MD100% (1)
- Chapter 6 - Immune Diseases (Part I) (Robbins and Cotran Pathologic Basis of Disease)Document6 pagesChapter 6 - Immune Diseases (Part I) (Robbins and Cotran Pathologic Basis of Disease)Ernie G. Bautista II, RN, MD90% (21)
- Histology of Sensory & Motor Nerve EndingsDocument2 pagesHistology of Sensory & Motor Nerve EndingsErnie G. Bautista II, RN, MD100% (1)
- General Sensory PathwaysDocument1 pageGeneral Sensory PathwaysErnie G. Bautista II, RN, MDNo ratings yet
- DiencephalonDocument4 pagesDiencephalonErnie G. Bautista II, RN, MD100% (3)
- Development of Reproductive SystemDocument2 pagesDevelopment of Reproductive SystemErnie G. Bautista II, RN, MDNo ratings yet
- Development of Endocrine SystemDocument1 pageDevelopment of Endocrine SystemErnie G. Bautista II, RN, MDNo ratings yet
- Cranial Nerves (Association & Motor Neurons)Document2 pagesCranial Nerves (Association & Motor Neurons)Ernie G. Bautista II, RN, MD100% (3)
- Lower Limb: Front and Medial Aspect of ThighDocument8 pagesLower Limb: Front and Medial Aspect of ThighErnie G. Bautista II, RN, MDNo ratings yet
- Brainstem & LesionsDocument4 pagesBrainstem & LesionsErnie G. Bautista II, RN, MDNo ratings yet
- TRIUMPHANT COLLEGE COVID-19 TRAINING NewDocument26 pagesTRIUMPHANT COLLEGE COVID-19 TRAINING NewDaniellaNo ratings yet
- Guide To Environmental Microbiological MonitoringDocument29 pagesGuide To Environmental Microbiological MonitoringzyrtylNo ratings yet
- Canine Disobedient, Unruly and ExcitableDocument5 pagesCanine Disobedient, Unruly and ExcitableBrook Farm Veterinary CenterNo ratings yet
- A Concise Review On Nerium Oleander L.Document5 pagesA Concise Review On Nerium Oleander L.tatralor100% (1)
- Acute Pain Abdomen in Surgical PracticeDocument34 pagesAcute Pain Abdomen in Surgical PracticedrakashnardeNo ratings yet
- Chest Rub Ointment ExperimentDocument2 pagesChest Rub Ointment ExperimentIsabel PeraltaNo ratings yet
- Grand Soya Oil 2Document15 pagesGrand Soya Oil 2Yusuf HamidNo ratings yet
- Answers To Questions:: Analysis of SalivaDocument2 pagesAnswers To Questions:: Analysis of Salivaerisseval14No ratings yet
- Double Unders MasteryDocument13 pagesDouble Unders MasterySebastian Hurtado100% (2)
- IV Push MedicationsDocument67 pagesIV Push Medicationsbtalera100% (1)
- Book of Vile DarknessDocument25 pagesBook of Vile Darknessv0idless100% (2)
- Physiology Practice Questions: Parasympathetic Nervous System CharacteristicsDocument4 pagesPhysiology Practice Questions: Parasympathetic Nervous System CharacteristicsGregg ShanksNo ratings yet
- Reducing Waste in ICUDocument10 pagesReducing Waste in ICUzorbini69No ratings yet
- Approach To The Jaundiced Cat - WSAVA 2015 Congress - VINDocument6 pagesApproach To The Jaundiced Cat - WSAVA 2015 Congress - VINdmantsioNo ratings yet
- How To Measure Frailty in Your PatientsDocument1 pageHow To Measure Frailty in Your PatientsZahra'a Al-AhmedNo ratings yet
- The Vanuatu Cooking Project ProposalDocument6 pagesThe Vanuatu Cooking Project ProposalBunga Melur MewangiNo ratings yet
- Chapter 10 Mendilan and Genetics Study GuideDocument16 pagesChapter 10 Mendilan and Genetics Study GuideKing AllanNo ratings yet
- WGW Infographic 2023Document1 pageWGW Infographic 2023PauloNesideCamposNo ratings yet
- Material Safety Data Sheet: 1. Chemical Product and Company IdentificationDocument7 pagesMaterial Safety Data Sheet: 1. Chemical Product and Company IdentificationKun Adi ReksatamaNo ratings yet
- Dengue AccomplishmentDocument4 pagesDengue AccomplishmentKylie GolindangNo ratings yet
- JKNKLKLDocument10 pagesJKNKLKLCyntia AndrinaNo ratings yet
- Benefits of ChocolateDocument13 pagesBenefits of ChocolateMohd Idris MohiuddinNo ratings yet
- Ananda Zaren - Core Elements of The Materia Medica of The Mind - Vol IDocument101 pagesAnanda Zaren - Core Elements of The Materia Medica of The Mind - Vol Ialex100% (2)
- A Pain Education ProgrammeDocument13 pagesA Pain Education Programmeapi-244230664No ratings yet
- Medications and Antidotes ChartDocument2 pagesMedications and Antidotes ChartkNo ratings yet
- Nucleotides, Nucleic Acids, and Heredity: Bettelheim / Brown / Campbell / Farrell / TorresDocument55 pagesNucleotides, Nucleic Acids, and Heredity: Bettelheim / Brown / Campbell / Farrell / TorresMica BernardoNo ratings yet
- Comp ReviewDocument99 pagesComp ReviewTHAO DANGNo ratings yet
- Biology 10Th Edition Raven Test Bank Full Chapter PDFDocument36 pagesBiology 10Th Edition Raven Test Bank Full Chapter PDFlewis.barnes1000100% (12)
- Anticoagulation Options For Intermittent HDDocument10 pagesAnticoagulation Options For Intermittent HDNarinder SharmaNo ratings yet
- Breast Cancer 1Document14 pagesBreast Cancer 1Gînțăgan Denisa GabrielaNo ratings yet