Professional Documents
Culture Documents
VSO Our Side of The Story Uganda
Uploaded by
VSOOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
VSO Our Side of The Story Uganda
Uploaded by
VSOCopyright:
Available Formats
Our Side of the Story
Coalition for Health Promotion and Social Development
Ugandan health workers speak up
HEPS-Uganda, The Coalition for Health Promotion and Social Development
Established in 2000, HEPS-Uganda, the Coalition for Health Promotion and Social Development, is a health rights organisation that advocates for increased access to affordable essential medicines for poor and vulnerable people in Uganda. HEPS promotes pro-people health policies and carries out campaigns at local, national and regional levels. It also initiates and conducts research necessary for health and human rights advocacy. Since 2007, HEPS-Uganda has actively promoted health rights within seven local government districts, addressing maternal health and equitable access to healthcare. Working in some of the most disadvantaged rural areas of Uganda, HEPS has trained community representatives to spread the word about health rights and how to exercise them. It also promotes the responsible use of healthcare resources and effective ways of communicating with health workers. For more details, visit: www.heps.or.ug
VSO Uganda
VSO Uganda volunteers are currently working in the central, western and northern regions of the country, in the fields of participation and governance, disability, health, education and livelihoods. Poor and disadvantaged people in Uganda are badly affected by preventable diseases. Health service provision and access is low, and staff retention is a challenge. VSO is supporting the Ugandan Government in implementing the Health Sector Strategic Plan (HSSP) to improve health systems in the context of a decentralised health delivery system at district level. HSSP focuses on working with communities and the implementation of primary and preventive healthcare services, as well as good-quality, accessible clinical services as stipulated in the minimum healthcare package. It has a particular emphasis on reaching the majority of the population, over 80% of whom live in rural areas, where the people tend to be poorer than in urban settings. For more details, visit: www.vsointernational.org/where-we-work/uganda.asp
VSO
VSO is different from most organisations that fight poverty. Instead of sending money or food, we bring people together to share skills and knowledge. In doing so, we create lasting change. Our volunteers work in whatever fields are necessary to fight the forces that keep people in poverty from education and health through to helping people learn the skills to make a living. We have health programmes in 11 countries, with plans to open further health programmes in the coming years. From extensive experience supporting health and HIV programmes in developing countries, VSO believes that in order for health systems to improve, more health workers must be recruited and retained. They must be of good quality, in the right places, well trained and with access to the basic equipment and drugs needed. They also need to be well supported placed in the right location, treated fairly and managed well. Through our Valuing Health Workers research and advocacy project, VSO identifies the issues that affect health workers ability to deliver quality healthcare. These findings will support partners to carry out further research and make a significant contribution to improvements in the quality of health worker recruitment, training and management. For more details visit: www.vsointernational.org/what-we-do/advocacy
Our Side of the Story: Ugandan health workers speak up
Acknowledgements
The Valuing Health Workers research and advocacy project is the initiative of VSO International. This report is based on research in Uganda in partnership with HEPS-Uganda, the Coalition for Health Promotion and Social Development, and with support from VSO Uganda. Thanks are due to Rosette Mutambi, executive director of HEPS-Uganda, Sarah Kyobe, VSO Uganda health programme manager, and Stephen Nock, VSO International policy and advocacy adviser, for their practical support and encouragement. Stacey-Anne Penny brought to the project her drive to explore and understand the lived experience of Ugandan nurses and her invaluable contribution as co-researcher up to August 2010. HEPS-Uganda colleagues provided a supportive and friendly working environment. The following HEPS staff played practical roles in managing consultative workshops, facilitating access to fieldwork sites and co-convening and transcribing focus group discussions: Prima Kazoora, Phiona Kulabako, Aaron Muhinda and Kenneth Mwehonge. This report would not have been possible without the willing participation of 122 health workers across Uganda. Thank you to them for voicing the rewards and challenges of their daily lives. Thank you to local managers for making staff available, and to patients for their forbearance while their health workers gave time to the research. Not least, thanks are due to the representatives of organisations concerned with health worker and health consumer interests, for their participation in workshops and interviews.
Patricia Thornton
Text: Patricia Thornton Field research: Patricia Thornton, Stacey-Anne Penny, Prima Kazoora, Phiona Kulabako, Aaron Muhinda and Kenneth Mwehonge Editing: Stephen Nock, Diane Milan, Stephanie Debere and Emily Wooster Layout: www.revangeldesigns.co.uk Photography: Cover photo Matthew Oldfield/Science Photo Library All other images: VSO/Ben Langdon Please note that none of the photographs in this publication are of the hospitals or health centre sites visited for the research fieldwork.
VSO 2012 Unless indicated otherwise, any part of this publication may be reproduced without permission for non-profit and educational purposes on the condition that VSO is acknowledged. Please send VSO a copy of any materials in which VSO material has been used. For any reproduction with commercial ends, permission must first be obtained from VSO. The views expressed in this report belong to individuals who participated in the research and may not necessarily reflect the views of HEPS-Uganda, VSO Uganda or VSO International.
ISBN: 978 1903697 139
Our Side of the Story: Ugandan health workers speak up
The VSO Valuing Health Workers initiative
What is life like working in healthcare in a low-income country? What prompts nurses, midwives and doctors to take up their professions and what are the rewards? What do health workers say about the barriers they face in providing access to healthcare? What in their view needs to change? And how can their voices be heard? VSOs Valuing Health Workers initiative is listening to the experiences of health workers and gathering evidence to advocate for change. VSO recognises that health workers voices must be heard and acted on to improve access to healthcare and to help achieve the Millennium Development Goals. It therefore started participatory research in four countries in Africa and Asia, in partnership with in-country non-governmental organisations (NGOs). In Uganda, research was carried out in partnership with HEPS-Uganda, the Coalition for Health Promotion and Social Development, from February 2010 to February 2011. VSO will support local partners to use the research findings to advocate for health workers, and will gather the research evidence to advocate on a global level. In Uganda, negative images of health workers are projected in the media, political speeches, policy documents, healthcare user research and health consumer advocacy projects. The overriding message is that health workers attitudes, behaviour and practices present barriers to accessing healthcare. The Valuing Health Workers research in Uganda set out to explore with frontline health workers and their managers the conditions underlying accusations of unethical behaviour and service inadequacies. The overall objective was to give opinion-formers and healthcare service users a realistic picture of what life is like as a health worker in Uganda, to increase understanding and modify expectations. Ugandan civil society organisations will use the findings to help build mutual understanding and promote harmonious relationships between healthcare users and workers, as well as to advocate for improved conditions for health workers in Uganda. This short report documents the experiences and views of 122 health workers medical doctors, clinical officers, nurses, midwives and nursing assistants. They include frontline workers, facility managers and local government district health officers. Through small group discussions and individual interviews in the workplace, the researchers encouraged health workers to speak freely in response to open questions, having been promised that identities would not be revealed. The facility-based participants worked at 18 hospitals and health centres across seven local government districts in all regions of Uganda and in the capital city, Kampala. The selection of facilities took account of region, the extent to which the district was easy or hard to serve, the level of hospital and health centre, location (urban or rural) and ownership (government, not-for-profit or private sector). Many participants drew on their prior experiences from training or working in different sectors and levels of healthcare facility. In addition, 24 stakeholders from civil society organisations, trade unions, professional associations and regulatory councils contributed their perspectives through workshops and individual interviews. A full report gives further details of the research approach. It includes a comprehensive overview of the Ugandan healthcare context, along with extensive references. It can be accessed at: http://www.vsointernational.org/what-we-do/health.asp
Our Side of the Story: Ugandan health workers speak up
Contents
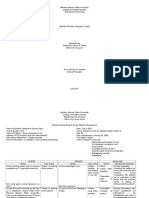
Healthcare in Uganda: challenges and provision Challenging working conditions The rewards Benefiting others Job satisfaction Being recognised, appreciated and valued Appreciative and supportive management and colleagues 6 7 8 8 8 9 9
Reasons for becoming a health worker: the right heart and the wrong heart 10 A passion for the patients 10 They join for the wrong reasons 11 Workload The impact on health workers The impact on attitudes, behaviour and practices The impact on community relations Factors contributing to understaffing and work overload Facility infrastructure The impact on health workers The impact on attitudes, behaviour and practices The impact on community relations Equipment and medical supplies The impact on health workers The impact on attitudes, behaviour and practices The impact on community relations Medicine supplies The drug supply situation The impact on health workers and the quality of care The impact on community relations Pay The impact on health workers The impact on attitudes, behaviour and practices Poor pay, turnover and loss to Uganda The way forward Raising the voices of health workers Speaking through professional associations, unions and regulatory councils Changing public perceptions of health workers Bridging communities and healthcare facilities and staff Summary of participants recommendations References 12 12 13 14 14 16 16 17 17 18 18 19 19 20 20 20 22 24 24 26 27 28 28 28 30 31 32 34
Our Side of the Story: Ugandan health workers speak up
Healthcare in Uganda: challenges and provision
A major challenge for the Ugandan healthcare system is posed by a rapidly growing population, with the third-highest growth rate in the world, a strikingly high birth rate (especially among teenage women) and a very young profile. A further challenge is to serve the exceptionally high proportion of the population residing in rural areas, who have extremely poor access to electricity and low access to improved water supplies. Although declining somewhat, maternal, infant and under-five death rates are still not under control. Malaria is the main sickness and a major cause of childhood deaths. Uganda has only one doctor per 10,000 people, and only 14 health workers (doctors, nurses and midwives) per 10,000 people. This is significantly below the level of 23 health workers per 10,000 recommended by the World Health Organization (WHO). Only four other countries have poorer provision of hospital beds than Uganda. Only 16 countries worldwide spend smaller proportions of their gross domestic product on health. Although the Government is committed under the Abuja Declaration to apportion 15% of its budget to health, its health spending has never exceeded 10% of total public expenditure. Most healthcare in the formal system is delivered at health centres and at hospitals at national, regional and district levels. One in five local government districts had no hospital when an official inventory of the then 80 districts was drawn up in 2010. Each sub-district should have a level IV health centre, headed by a medical doctor and providing emergency surgery. Five of the 80 districts in the inventory had no health centre IV at all and a further 23 had just one. The situation is likely to have worsened as districts go on being created, reaching a total of 112 in mid-2010. One in four facilities is classified as a health centre III and should provide maternity, inpatient and laboratory services. Two-thirds of health facilities are classed as health centre II, intended for preventive services and outpatient curative care. Three in ten of these are in the capital city. The Government runs 60% of the hospitals and health centres. Not-for-profit organisations (mostly faith-based) run just under 20%. Private for-profit organisations run just over 20% of the officially classified healthcare facilities, mainly in urban areas. There are also innumerable unrecognised small private units. Fewer than four in ten Ugandans turn to health centres or hospitals when they fall sick. The rural population use health centres more than urban dwellers, while the urban population use hospitals more than people in rural areas. The poorer you are in Uganda, the more likely you are to go to a government health centre. Children and pregnant women are the largest groups of health facility patients. Over 25% of Ugandans live more than 5km from their nearest health facility. Nine in ten walk or cycle to their government health centre. The available data on the make-up of the Ugandan health workforce show extreme shortfalls in the most highly qualified occupational groups and maldistribution across the country. Although the aim is to phase them out, Uganda has relied heavily on nursing assistants, especially in rural areas. Medical doctors and the most highly qualified midwives and nurses are concentrated in urban areas, especially in and around Kampala. An estimated 40% of the facility-based workforce are in the government sector, 30% in the not-for-profit sector and 30% in the private sector. Medical doctors are concentrated in the private sector, although there are high rates of dual employment, with medical doctors working in both private and government sectors. Half the medical doctors and four in ten nurses employed in government facilities work in the regional and national referral hospitals.
A queue of people waiting to see a doctor. A doctor in Uganda serves an average of 10,000 people.
Our Side of the Story: Ugandan health workers speak up
Challenging working conditions
Staffing shortfalls
Almost half (48%) of approved posts at health centres and hospitals are vacant, a shortfall of 25,506 staff. The situation is worst in the lower-level health centres, yet health centre IVs and general hospitals respectively lack 45% and 38% of their approved staff complements. (Matsiko, 2010) Hospitals at regional level are missing 30% of the staff they should have. There are gross disparities across local government districts. In four districts, less than 30% of posts are filled, while only ten districts filled more than 70% of posts. (Oketcho et al, 2009) Health centre IVs have an acute shortage of medical doctors: 64% of these posts were vacant across the two-thirds of health centre IVs that provided data. Across the 42 general hospitals reporting, four in ten medical doctor posts and four in ten nursing positions were not filled. (Ministry of Health, 2010)
Deficits in equipment and medical supplies
The Ministry of Health acknowledges a shortage of basic equipment in health facilities and that only 40% of equipment in place is in good condition. (Ministry of Health, 2010) An independent survey reveals a gross lack of equipment for the diagnosis and treatment of malaria: half of health centre IIIs and a fifth of health centre IVs and hospitals in the survey lack a functional microscope, 86% of health centre IIs and IIIs had no rapid diagnostic tests, and 60% of all facilities surveyed were not equipped to measure haemoglobin. (Achan et al, 2011) Other evidence suggests that only one in 20 facilities has a vacuum extractor (used for assisted vaginal delivery) and only one in ten a dilation and curettage kit (needed to remove a retained placenta). (Ministry of Finance, Planning and Economic Development, 2010)
Non-availability of essential medicines
The percentage of health facilities registering stock-outs in essential medicines has consistently been over 60% for the last ten years. (Ministry of Finance, Planning and Economic Development, 2010) Not one of 40 essential medicines was available in every government facility in a sample survey in the second quarter of 2010, and only eight of the 40 essential medicines were found in all the not-for-profit facilities surveyed. (Uganda Country Working Group, 2010) Essential medicines were on average out of stock for 73 days of the year in government facilities and seven days in not-for-profit facilities, according to a 2008 sample survey. (Ministry of Health, 2008a) Only one in three respondents surveyed in 2008 agreed that their nearest government facility usually had all the medicines the household needed. (Ministry of Health, 2008b)
Uganda has only one doctor per 10,000 people, and only 14 health workers (doctors, nurses and midwives) per 10,000 people
Dilapidated infrastructure
Most facilities are in a state of disrepair. (Ministry of Health, 2010) Many health centre IVs lack crucial infrastructure to make them fully functional: half those reporting to the Ministry of Health have an incomplete or non-functional operating theatre or no theatre at all. (Republic of Uganda, 2010) Only one in four health facilities has electricity or a backup generator with fuel routinely available during service hours. Only 31% have year-round water supplied in the facility by tap or available within 500m. (Ministry of Finance, Planning and Economic Development, 2010) Less than half of all facilities can transport a patient to a referral site in maternal emergencies. (Ministry of Finance, Planning and Economic Development, 2010) Only 6% of health facilities have information and communication technology mobile phone, radio, TV or computer. (Ministry of Health, 2010)
Low pay
Monthly starting salaries in public service in 200910 were: 353,887 UGX (Uganda shillings) for a registered nurse (US$191) 657,490 UGX for a medical officer (US$354) 840,749 UGX for a senior medical officer (US$453)1 (Matsiko, 2010). In contrast, high court judges received 6.8 million UGX per month (US$3,664) Ugandan nurses and doctors salaries are the lowest in East Africa.
1. 1,856 Uganda shillings = 1 US dollar at 31 March 2010
Our Side of the Story: Ugandan health workers speak up
The rewards
Ugandan health workers rarely get the chance to speak about the positives of what they do the rewards and satisfactions and participants welcomed the opportunity the research gave them. The most satisfying aspects of their work were helping others, doing a good job and being valued for what they did. Positive practice environments were by no means commonplace, however some participants were so discouraged by working conditions that they struggled to find anything good to say about being a health worker. For a few, the only positives were the material benefits of a regular salary and a free house.
Benefiting others
Participants told of feeling happy carrying out their vocation, helping their people, giving something back, delivering care and comfort, helping those unable to help themselves and saving lives. Strikingly, the benefits to the community, to individual patients and to families were the chief sources of satisfaction, even in the harshest working environments.
Midwives spoke of the rewards of working for the welfare of two people live mother and a live baby and achieving something positive with neither mother nor baby lost.
I love it when someone comes in ill and goes back happy
Benefiting families
The nurse is the most important person in the family. Especially for nurses in rural settings or from rural families, it was hugely rewarding to be able to deal with family health problems. Knowing how to prevent and treat illness in your immediate family, as well as how to protect yourself, encouraged a commitment to nursing which would last up to and beyond retirement: You will be a nurse until you die. Nurses at some rural health centres mentioned the advantages to their family and themselves of quick access to free treatment. The nurse could use his or her knowledge to treat a relative and save the costs of referral to a health centre or hospital. It was said in some facilities that staff and their family members received free medication.
Benefiting the wider community
Health workers liked sharing their knowledge and skills with communities in order to counter harmful traditional beliefs and practices, educate people about ways of preventing disease and encourage take-up of health services. Seeing more women delivering babies in health units, diseases controlled through immunisation programmes, or reduced reliance on harmful traditional remedies brought great satisfaction. Health workers were especially pleased when they were involved in new programmes and could see their impacts, such as a nutrition clinic, a mental health unit or the prevention of mother-to-child HIV transmission. Satisfaction came from being part of a health facility that put patients first. Especially in rural areas, health workers were happy to use their knowledge to help informally outside working hours and around their homes. For an off-duty nurse, it was good to socialise with inpatients, hear their family problems and have the chance to give some health education.
Job satisfaction
Linked to the happiness of seeing someone recover is the satisfaction of knowing your own contribution, especially among medical doctors and clinical officers: I feel happy when I give treatment to my patients and they get well. I feel so proud, I feel very fine, and I can see the difference I have made, thats very important. Introducing new treatments and bringing about change in a challenging environment was hugely satisfying: What others thought was so difficult, I have been able to do. Maternity workers spoke of their joy when they safely delivered a healthy baby, when everyone is smiling, and the satisfaction of seeing that baby grow.
Benefiting patients
Participants highlighted the visible results of care and treatment. They expressed their delight at the benefits to patients. Nurses and medical doctors spoke of the joy and pride they felt when a patient who arrived sick, even on the verge of death, went home recovered: I love it when someone comes in ill and goes back happy. Seeing life enhanced was also hugely rewarding: Making people happy makes me happy. Just seeing some improvement in a patient was cheering.
Our Side of the Story: Ugandan health workers speak up
Having done good nursing work treating a very ill patient who improved and was discharged gave a kind of job satisfaction and encourages me to care for patients a little more. For nurses, it was good to have done something, no matter how little, to help save a life. Achieving successes is not easy in Uganda, and an occasional victory, such as when a sick child recovers, was something to live for that makes you do what you do. Participants took satisfaction in doing a good job when there was enough equipment, other medical supplies and medicines to enable proper care: Most of what you need for a patient is available, so your job is not much interfered with, and You cannot forget your skills. Elsewhere health workers commented on the satisfaction of just being able to play their part and do their duty the best they could, despite many shortcomings in supplies and equipment and staffing shortfalls. Some spoke of pride in working efficiently to treat patients or caring tenderly where they could. Particularly for younger participants, opportunities to learn through work and to experience managing different kinds of medical condition were highly valued. While not commonly reported, opportunities to learn new skills, such as counselling, were valued for their benefits to patients. In the few instances where workplace-based education programmes were in place, participants spoke enthusiastically about how they shared their learning with other staff and developed new communication skills.
pleasure of helping was enough, whether praised or not: I feel it inside my heart. As well as appreciation, recognition of their expertise was important to nurses: Their confidence in you boosts your own confidence. Midwives are delighted when a baby is given their name. Nursing staff and medical doctors emphasised how recognised and appreciated they felt when a past patient greeted and thanked them warmly or showed off your baby. Being remembered by patients was seen as a mark of trust and boosted the nurses own confidence. For some nurses, respect and trust on the part of patients or caregivers opened up disclosure of confidences and opportunities for further help.
Appreciative and supportive management and colleagues
Appreciation on the part of managers was a huge positive, although not widely reported: When you are recognised that you are doing good work, I think that is important, it motivates. Simply being told thank you was not necessarily very satisfying in difficult working conditions. Health workers valued the provision of more tangible tokens of appreciation, such as open internet access, Christmas and Easter presents and staff parties. Rare, and especially valued, was facility sponsorship of further training, with a job to return to. Uniquely in the study, participants in a local government hospital praised management who appreciate us so much. Certificates of appreciation, staff parties, presents, financial contributions to costs of burials and operations, help with costs of further study, days off to recover from illness, interest in their work and responsiveness to problems staff identified were cited as proof of this appreciation. Health workers felt valued by good, supportive managers who created opportunities for them to raise their concerns, were always willing to discuss a problem, and sought and implemented solutions. Nurses spoke of the satisfaction of working cooperatively with other staff, having someone to consult if needed, sharing ideas and reaching solutions. Teamwork also meant helping each other out, such as an off-duty nurse caring for another nurses sick child and willingness to extend hours to cover for a nurses delayed arrival at work. Where working conditions were especially challenging, nurses valued being part of a support network where everyone understood the difficulties.
Being recognised, appreciated and valued
Community recognition
Some nurses in rural settings liked being acknowledged and known in the community: When you go out you are respected, or You are famous. Being a nurse meant being seen as an educated person; it was gratifying to be called a small doctor. Nurses sometimes felt their training set them apart from other people, conferring a certain prestige, especially when they could use their knowledge to help outside their formal work. Nursing was also valued as a way to meet different types of people, get to know many people and make friends.
Patients appreciation, trust and respect
Health workers valued being liked, appreciated, praised, respected and trusted by patients. It was noted that expressing thanks was not the norm in some parts of Uganda, and health workers spoke enthusiastically about the boost a thank you from a patient gave them: You feel very happy after your work when they say thank you. So you keep on, because you are enjoying it. For some, the
Our Side of the Story: Ugandan health workers speak up
Reasons for becoming a health worker: the right heart and the wrong heart
Participants explained what prompted them to become healthcare professionals. The urge to help, prevent suffering and save lives stood out. The overriding impression emerged of a heartfelt desire to make a difference as a nurse, midwife, clinical officer or medical doctor, rather than merely to earn a living. It is a mark of their professional commitment that almost all participants said they would still choose to become a health worker. Participants observed that some people joined the health professions, notably nursing, for the wrong reasons. This, in their view, was one explanation for poor attitudes and unethical behaviour, and they put forward suggestions for improving the calibre of recruits. The recommendations also include other stakeholders views.
A passion for the patients
For many health workers, the strong need to give to others was born of childhood experience. It had been common in rural areas to see close family and members of the local community suffer and die in pain, with no proper medical care. Participants recounted how siblings and parents had died of mysterious illnesses that, they later realised, were due to preventable epidemics or treatable with modern medicine. Training as a nurse, clinician or medical doctor would bring to the community essential knowledge to help prevent illnesses, discourage harmful traditional healing practices and save lives: They were really suffering, people were dying, there were no doctors, no nurses, nobody to give them an idea about their health. I wanted to help my people. Others spoke of atrocities in conflict areas and the need for medical skills to rebuild communities. Health workers spoke warmly of positive experiences undergone when they or family members were in hospital. The gentle and caring touch and the healing words of nursing staff left a lasting impression. They wanted to be that person, to give in that caring way, to stop others pain. Growing up, they learnt how the skills of the medical staff had saved the life of someone close to them, or even their own life, and they wanted to give something in return. Some were encouraged by a parent who, gratefully remembering a midwife, urged that their child become a midwife too. Not all impressions were good. Negative experiences of healthcare services fuelled a desire to raise the standard of medicine in Uganda. Young men and women said they felt compelled to join their professions because they believed that professional neglect had contributed to the deaths of a parent, siblings or a newborn baby, or because they perceived the limitations of Ugandan medical expertise in the face of a
life-threatening condition. Unsympathetic handling prompted a wish to improve the quality of nursing, and the shouts of women abandoned in labour evoked a desire to help. Women spoke of only ever wanting to be a nurse from as early as primary school stage. They saw themselves as naturally kind, a helping sort of person, with an urge to relieve suffering: I just had it in me, or I had that heart. Some women found they developed the heart as young adults when they had to nurse a family member. Not-for-profit sector participants especially cited a desire to love and serve the patients or to care for the needy, spoke of coming closer to God or explained they had a call or were chosen by God. Health workers emphasised giving, and spoke less about what they had expected to gain from their profession, though the prospect of knowledge to care for and treat ones family and oneself was important, especially among lesser-qualified women in rural areas. Nurses happiness when a patient recovered was mentioned, as was the respect people gave to a local nurse. The nurse had status as a life saver, a person of importance to call on in an emergency. Young girls who went on to be nurses had been greatly attracted by the dress and deportment of nurses, their smart, clean uniforms, shoes and gloves and the way they walked, which set them apart from other people. Among would-be medical doctors there was some admiration of smart white coats and acknowledgement of the prestige attached to being a doctor. Financial gain was not a driving force, though earning in a steady job was certainly a better option than digging in vegetable gardens and relying on uncertain harvests. In the most remote rural area, the health facility was the only source of training and employment locally, and so a magnet for school-leavers.
10
Our Side of the Story: Ugandan health workers speak up
For most participants, the decision to become a health professional was positive and informed. Time spent at hospitals or health centres as a patient, relative of a patient or just as a curious child allowed to sit with nurses had shown how nurses worked with patients, and helped stimulate an interest. Empathy for patients sometimes developed when touched by their condition. Having a father, mother, sister, brother or aunt in a nursing or medical field gave some insight into the work, through visiting their place of work, living in staff quarters or listening to their accounts of day-to-day happenings. A close relatives positive attitude, humility or empathy for patients attracted young women to nursing. For many of these participants, the example of their relative was the main reason for entering a nursing or medical profession. With little career guidance at school, it was natural to do what members of the family were doing. Others were expected by their family to take up a profession and saw health work as a more appealing option than teaching, secretarial or business occupations, even rebelling against fathers who insisted on a teaching course. Some older participants had been encouraged by adults at school or family friends, such as priests and nuns, to apply for a medical or nursing course. Others from that generation had been recruited to nursing by agents of the Ministry of Health, or had followed family wishes or suggestions in complete ignorance of what nursing involved. Clinical officers and medical doctors told of expectations on them as the brightest school students to enter one of the prestigious professions. Engineering and medicine were the prime alternatives if they excelled in science subjects. So the path towards medicine could be set in early years when top students were pushed towards sciences. Faced with a choice of career direction, financial security was something younger men had taken into account, in the context of many qualified professionals chasing too few jobs: At least you can always find a job. But nobody said they joined the nursing or medical profession purely for that reason. Among doctors, the choice of medical training over another sciencebased profession was in some cases influenced by the prospect of professional advancement and mobility, self-employment and private practice. Not all those who had decided on a career in the medical field entered via the course of their choice. Lacking financial backing from their families, uncertain about getting the grades, or failing to gain entry, would-be medical doctors had to settle for clinical officer training or a nursing course, and aspiring clinical officers became nurses. It was sometimes hard at first to accept a substitute course, especially when other people said nursing is for failures.
They join for the wrong reasons
There were widespread beliefs among nursing and midwifery professionals that poor attitudes and unethical behaviours are linked to joining nursing for the wrong reasons. It was thought that more recent recruits joined because they had no other option, because nursing was a last resort when they failed to qualify for more prestigious professions or because parents pushed them into it. Pursuing pay, looking only at the job market and even aspiring to leave the country were other presumed reasons for joining nursing. Older nurse managers had noted very few nurses come with a sense of vocation now. There was a widespread view that people enter nursing with the wrong heart. It was believed that as a result, unhappy, disinterested and self-serving recruits resort to bad habits, become rude and forget their ethics and accountability to patients. There were also some comments by managers about medical doctors questionable attitudes to work when they seemed to lack that inner drive. Yet more than one nurse, and also a medical doctor, said they came to love their profession only when in practice. A story was told of how a lecturer inspired an enthusiasm for nursing in a student whose sole ambition had been to train as a doctor. Indeed, some of those most critical of motives for joining were staff who had developed an interest in their profession after they started work. Participants recommendations include: career guidance for school students and arrangements between schools and health facilities for work experience tighter admission procedures for nurse training, to probe reasons for applying improvements to standards of nurse training schools, including more and better-quality tutors, smaller class sizes and more attention to the practical application of professional ethics integration of health and human rights training into the curricula improvements to the community-based education component of pre-qualification training the establishment of more training schools in rural areas, to produce health workers adapted to rural lifestyles and bind health workers to the community a review of the value of the Nurses and Midwives Council registration interviews.
11
Our Side of the Story: Ugandan health workers speak up
Workload
Concerns about understaffing and workload were most marked among health workers and managers in government facilities at all levels. At some not-for-profit and private facilities the concern barely surfaced, while at others it was a key issue for participants. Overload was reported even in well-staffed hospitals within the not-for-profit sector. Not surprisingly, health workers dwelt on the consequences for them of understaffing and heavy workloads. But also they spoke passionately about the damaging effects on patients and on community perceptions of health workers.
The impact on health workers
Unmanageable workloads
Overwhelmed was a word widely used by nurses speaking about unmanageable workloads in many government hospitals and a not-for-profit hospital: How can you manage? It does something to you. Nurses spoke of being affected mentally and destroyed to the extent of becoming ill: One nurse running a full ward, with patients sleeping on the floor as well, the overwhelming number can affect the nurse psychologically. With a nurse off sick, the workload became even harder to manage.
Working day and night
Health workers in government health centres told of working day and night, often alone, due to understaffing and staff absences. It was pointed out that clinical officers, midwives, nurses and nursing assistants had stayed on duty round the clock or even longer, contrary to government rules and codes of conduct. They said they kept on in the face of fatigue because of their commitment to helping others: If God were not calling, you could not do this work 24 hours. Health centre midwives suffered especially. Midwives in rural health centres told of working alone day and night, sleeping with their children in disused wards, always on call to deal with expectant mothers often arriving in late stages of labour. A manager acknowledged that a midwife had worked alone and on call for five months. In a private sector health centre, scheduled time off had to be forgone for the sake of the patients: If a doctor prescribes care for 24 hours, we have to stay and then work again next day.
Too many tasks and responsibilities
In government health centres, midwifery and nursing staff said they were stretched to the limit by too many tasks: You have to run the antenatal clinic, conduct deliveries, carry out post-natal, do the ward round, one person. Then you have to run most of the young child clinic. Burnout resulted: You have to do the counselling, take blood, see the patients, prescribe for them and do everything. When you leave at the end of the day, you are burnt down completely. Among nurses in government hospitals there were complaints about having to take on doctors duties: I dont know when a ward round was last done. We review patients, even prescribe. The non-availability of a doctor caused dilemmas for midwives, who feared blame if they undertook a medical procedure beyond their scope of duty. Health centre nurses believed they did the work of a clinical officer. Government hospital nursing assistants complained about doing work which should be done by nurses. Working in a team had been one of the attractions of nursing as a career choice. It was frustrating and disheartening when cooperation was lacking, such as when a relief worker failed to turn up: No teamwork at all, and when it is an emergency and they delay, you really feel bad. You know what the outcome will be, but you cant help.
Over-long shifts and too little time off
Among not-for-profit hospital nurses there were complaints about being forced into working 12-hour shifts. Taking up the option of working shorter hours would reduce days off from two to one, a hard choice for nurses with children and homes to look after. Days off duty are important times to do your own things and should be an entitlement. Yet it seemed taken for granted that nurses and nursing assistants living on site in staff accommodation would turn out in their off time to fill staffing gaps in some health centres. Even a not-for-profit hospital with clearly specified conditions of service was reported not to give good time off because of understaffing.
When you leave at the end of the day you are burnt down completely
12
Our Side of the Story: Ugandan health workers speak up
Impacts on health
Among nursing staff in government health centres and general hospitals there were concerns about the effects on health of forgoing or delaying meals because of work pressure. Not eating on schedule was a key concern when suffering from diabetes, and eating well was important to maintain immunity against infection from patients. Even taking a drink was not easy because how would it look when they are in pain? It was even hard to make a quick toilet visit without being reprimanded by hospital managers.
The impact on attitudes, behaviour and practices
Hospital nurses acknowledged that overload damaged the quality of work: At the end, you are very tired and no quality of work is done. Participants employed outside the government sector were especially outspoken about the impact on the quality of nursing in a large government hospital where they had seen performance drop and patients needs neglected. Personal distress made things worse, they felt: Understaffed in a ward full of patients, on top of family worries, they find they cant perform, miss things and cannot provide all the services patients need. The nursing role should be much more than taking routine observations and giving treatment, but it was impossible for an overworked nurse to find time to talk with patients, uncover their problems and deal with the whole picture. Consequently task-oriented nursing was unavoidable and even routine tasks were hard to complete: With two nurses for 50 patients, you are reduced to troubleshooting, its not nursing.
Restricted professional development
Managers concerns included the impact on clinical officers development when they lacked the opportunity to work under the guidance of a medical doctor, and the professionally isolating consequences for staff with no supporting teamwork: Nobody to consult when you are stuck, nobody to delegate to when you are unable. A nursing assistant had been put in a role that took her away from direct patient care, to fill gaps in the professional staff complement: I want to learn more from the patients, but I have no choice. There were views that opportunities for further study were blocked because the facility would not be able to recruit a replacement if the nurse left.
As a human being you can get irritated and lose your temper because of fatigue
Hospital nurses torn apart by patients calling for attention found it hard to make patients understand that they had to wait their turn. They recognised they could lose their temper in such stressful situations and forget their basic good intentions: You become different. Medical staff had seen the effects of tiredness: The tone of voice changes, and The nurses end up losing it, when they are already frustrated by poor pay. Managers were generally understanding: As a human being you can get irritated and lose your temper because of fatigue, or What do you expect with only half the nurses you should have? They become rude. Participants working in well-staffed private and not-for-profit hospitals had seen the consequences of work overload in the government sector. Managers observed that lack of opportunity to fulfil their proper professional role demotivates nurses, who then adapt to a culture of poor standards of care in their work environment. A dont care attitude resulted: By the time she is 30 she is used up. Already tired due to understaffing, she has run out of compassion and the patients say she is not caring. They said that overwhelmed nurses skip out from work, ask to be transferred and run away to the private sector where patients do not complain they are neglected.
Failing the patients
Among health centre IV workers, the lack of a medical doctor was one of the biggest concerns, more important to them than frustrations about individual workload and personal consequences: I can get demoralised seeing someone dying in my hands because we are missing a doctor, and It really hurts a lot when a patient is dying and you know what should be done. You even go home depressed.
I can get demoralised seeing someone dying in my hands because we are missing a doctor
Health workers who expressed these feelings were adamant that they kept on turning up for work to stop the next persons suffering: If Im depressed because someone has died and I say I am not going to work the next day, then we are going to lose more.
13
Our Side of the Story: Ugandan health workers speak up
Midwife behaviour towards patients changed as a result of working alone all day and all night, especially with no peace of mind due to personal and family worries: So you become tough with the mother so that she understands and you get a live baby and a live mother. Managers were well aware of the unacceptably long hours midwives put in and spoke openly about the effects they had seen: As time goes by, because of the fatigue and perpetual calling, somehow as a human being you tend to deteriorate. Midwives no longer in the government sector understood how over-tired midwives were forced to escape from 24-hour work in health centres, to make contact with their families. For midwives, perpetual responsibility for the lives of mothers and babies was a burden and it was hard to stay patient with the mothers. Nurses discussed the knock-on effects on their patients of their having to do too many things at once: You find you are stressed and are rude to patients unknowingly. There were some strong views that the workload in some large hospitals was increased by senior staff malingering or not pulling their weight. A view from the private sector was that frustrated junior nurses in the government sector took it out on the patients. Long, tiring shifts led to overworked nurses being short with patients, not interacting with them and conveying disinterest through attitude and expression. Managers and frontline doctors had seen how hunger made nursing staff bad-tempered and rude to patients. It was said that long shifts, together with poor pay, made nurses look for ways of escaping not turning up for duty and leaving work early. It was also said that even after 12-hour shifts, some nurses went on to other nursing jobs just to survive financially, and so developed bad habits.
Health centre workers realised that no respite in long shifts led to community complaints about harsh language: We work the whole day without resting, and in the late afternoon we get tired and then we change face. Staff working set hours had met some hostility from local people who assumed the health centre was closed to outpatients when they saw health workers socialising together towards the end of the working day. The staff there pointed out that they worked hard to serve outpatients quickly and so deserved some rest-time after patients had stopped arriving. It was also hard to make waiting patients understand that health workers were not resting when they sat completing paperwork. Health workers in sole charge of patients faced a dilemma: go hungry or leave the patients alone? Doing the latter was reported to have brought unfortunate consequences for staff who were arrested for neglect of duty. The arrests were said to be motivated by local political candidates seeking to gain electoral favour by discrediting ruling politicians with oversight of the facility. Clinical officers can be left alone to cover an entire health centre, running from one department to another. So, it was deeply upsetting when a patient arrived, assumed no staff were available, and called on a local leader who then complained to higher authorities. The lack of a medical doctor rebounded on other staff: When the patient dies, the community look on you as a bad person who refused to treat the patient. Lack of a midwife or qualified nurse meant that nursing assistants carried out deliveries. They found it hard to convince patients to put their trust in them, especially as they themselves recognised they lacked the full range of knowledge to save pregnant women in difficulty.
The impact on community relations
Aggressive or demanding outpatients were a particular concern for medical doctors and clinical officers. With so many patients waiting for attention it was important to prioritise their treatment. But patients either did not understand the triage system or believed they deserved priority. Such challenges to professional judgment were especially hard to handle when aggrieved patients called on local leaders to intervene on their behalf. Midwives working round the clock were distressed by patients accusing them of not working when they had found a little time to rest. This misperception was said to fuel community hostility towards health workers.
Factors contributing to understaffing and work overload
It is not necessarily the case that there is a shortage of health workers available in the labour force. Some government sector managers were aware of huge numbers of applicants for advertised vacancies, while others said they had failed to recruit. Among managers at district level, views were expressed that decentralisation of the health system was to blame for the uneven distribution of health workers in local government.
Recruitment barriers
Government sector managers explained that financial allocations for salaries stood in the way of recruiting more staff: there was simply no money in the pot to pay more health workers. Even if funds were made available to fill authorised posts, vacancies remained due to bureaucratic procedures and the absence of a District Service Commission tasked with recruiting health personnel to the district.
When the patient dies, the community look on you as a bad person who refused to treat the patient
14
Our Side of the Story: Ugandan health workers speak up
Managers explained why remote and rural facilities found it hard to recruit and retain medical doctors, nurses and midwives. They sympathised with new recruits who turned round and left for want of something to do in a village: They post someone out there in the wilderness and they expect them to work! With no electricity for TV and internet, people were not connected to the world. Poor roads and no public transport at night left staff stuck. Free staff accommodation was widely believed to make it easier for nurses and medical doctors to leave behind the amenities of town life. Poor-quality staff quarters, on the other hand, were a deterrent to taking up and staying in posts. An example was cited of rented accommodation of so poor a standard that it was not safe to raise a child there, leading to a nurse leaving her post. Health workers living in towns spoke along similar lines, adding that food was expensive in remote areas and educational standards poor. It was remarked that medical doctors dislike working in villages because of the lack of opportunity for learning and career advancement. It was also said that medical doctors avoid jobs at district level because local politicians misuse health service resources and interfere in treatment decisions.
Paradoxically, staff scarcity was a barrier to holding public sector health workers to account for their absences. Turning a blind eye was preferable to starting disciplinary procedures which would likely lead to a transfer. It would be suicide to lose someone, as the remaining few staff would be more overburdened and blame the manager. Managers noted wryly that they had little leeway to dictate to medical doctors and midwives in understaffed facilities: They hold you to ransom, they know they have power because they can just go and get work somewhere else. A frontline doctor echoed the point: You work in a relaxed environment. They dont want to pressure you too much and push you away. It is reported elsewhere that Ugandan facility managers have no authority to discipline staff. Scarcity was similarly a barrier to the redistribution of staff within a district. While in theory a district health manager could move a nurse or midwife from a better-served health centre to ease understaffing at another centre in the district, in practice the manager met resistance: They wont go because they know they are marketable.
Local management factors
In the local government sector, the problems of overwork and too little time off stemmed in part from limited management capacity to draw up fair duty rosters. Poorly planned rosters scheduled nurses to work back-to-back day and night shifts. The view among nurses was that properly organised time off would motivate them to work. Concerned health centre managers said they recognised the need to manage staff hours fairly, but with so few staff that was almost impossible. Government sector managers explained how unexpected absences increased the load on nursing staff. When staff failed to turn up for work, and especially when they did not communicate their intent, managers struggled to find workers to fill the gaps and patients were left waiting. While there was sympathy for the personal and family problems that kept staff from work, managers felt that the reasons offered were not always genuine. In the Ugandan culture it was hard to question whether family sickness or burials had actually occurred, and hard to enforce a requirement to produce sick notes. Sometimes managers suspected, or even knew, that absent staff were moonlighting or pursuing a side income, doing other things to survive. Managers and frontline workers commented that staff who lived on site were rarely absent, unless they were sick or a relative had a problem, as they would be ashamed when patients came looking for them at home. Participants working in government health centres explained how their hours and workload increased at short notice when senior colleagues were called away to workshops and meetings. They rarely questioned why these activities took priority over clinical and management duties at the facility, though the attraction of attendance allowances was alluded to.
Task-shifting
It is clear from workers accounts that work overload, stress and poor community relations result from doing work for which they are not qualified or trained. Such task-shifting has been found in government healthcare facilities elsewhere in Uganda. Managers and frontline workers expressed concerns about staff working beyond their scope of practice, when a nursing assistant acted as a nurse, a nurse as a midwife and a midwife as a medical doctor. This is necessitated by shortages and absences of suitably qualified staff. However, it seems that task-shifting was also a deliberate strategy to save money by employing less-qualified staff. Participants recommendations to reduce the impact of staff shortages include: the introduction of standards for patient/nurse and patient/ doctor ratios, so that health worker overload is transparent and quantifiable educating the public, through better-informed news media, about financial and bureaucratic obstacles to recruiting more health workers centralising management of health worker recruitment and deployment, to address the problem of unfilled posts and uneven distribution of health workers providing good-quality staff accommodation, equipped with electric lighting and clean water supply, suitable for families.
15
Our Side of the Story: Ugandan health workers speak up
Facility infrastructure
Government sector workers in rural hospitals and health centres bore the brunt of dilapidated conditions: non-functioning operating theatres, erratic or non-existent electric power, unreliable access to clean water, blocked sewers, broken-down transport and no communication technology. They told of damaging effects on job satisfaction, risks to themselves and deeply felt harm to patients.
Government facility managers and district health officers wondered why more health centres were being constructed when existing facilities did not work as they should. Facility managers in the government sector told of struggling with inadequate budgets to repair or replace decades-old infrastructure: The only borehole, you pump for 30 minutes and then it stops for two hours. Pumping water only every second day and encouraging rainwater collection in jerrycans and drums was a partial solution. Elsewhere, the best that could be hoped for was to be earmarked for rehabilitation at least we are in a programme or that a Good Samaritan would help connect to a distant water source. On the other hand, external funding coupled with well-managed in-house technical services allowed a not-for-profit hospital manager to speak with pride of rainwater conservation and solar power systems. There was a marked contrast between a hospital where wards were cleaned three times a day and one which had no water supplies for years. hard, yet: We just have to bear with it for the betterment of our community. Nurses working in bad light felt they were failing in their duty to patients in need of scheduled treatments during night hours. Hospital communication systems do not work without power, and midwives can be left to bear the brunt when a doctor cannot be called.
Risks to health workers
Working with no power or water, health workers were naturally worried about the risks to themselves: We are risking our lives. Maternity workers emphasised the risk of contamination from infected blood when working in the dark. Nurses feared being assaulted when working alone in unlit wards or crossing dark compounds, a risk increased by lockless doors, breaches in compound fences and inadequately equipped or absent guards: We fear to answer the door when somebody knocks for help. Lack of a functioning flush toilet at the workplace forced a dangerous walk home through a snake-infested compound.
The impact on health workers
The condition of the working environment is one of the biggest challenges. So that people can work with a smile, wake up in the morning and be happy going to work. You enjoy your work and your profession.
Risks to patients
Midwives and maternity nurses emphasised the risks to women giving birth at night. Assisting deliveries by the light of a mobile phone or a candle begged from a patient, they were forced to delay repairing episiotomies until daylight. Unable to read the patients case notes at night, midwives could not tell if she had HIV and thereby reduce the risk to the baby. Only a donors gift of lamps relieved months of suffering delivering in the dark. Infection control was near impossible when nursing staff had to beg the little water spared by patients attendants to wash their hands, so as to avoid passing on infections to the patients.
Low job satisfaction
A major concern was the state of operating theatres at health centre IVs. Government sector managers spoke of theatres that did not function because of poor design or shoddy construction. They said that when a theatre was unusable, or lacked proper equipment or anaesthetists, underemployed medical doctors lost interest and left. Doctors blamed the lack of opportunity to practise surgery for unwillingness to take up a medical doctor post at a health centre IV. For nurses working with only one paraffin lamp and limited fuel, proper care of night-time emergency admissions was impossible: How can you manage to put in the intravenous line with a dim light? Sharing one paraffin lamp across three wards was very
Just yesterday we were doing an operation and we had to complete stitching by torchlight
16
Our Side of the Story: Ugandan health workers speak up
Participants told how expensive fuel for electricity generators ran out at crucial moments: Just yesterday we were doing an operation and we had to complete stitching by torchlight. Sterilisation was a huge challenge. As generator power must be conserved it could not be used routinely for precious equipment, such as an ultrasound machine which mostly stood idle despite having a trained operator. Limited generator power did not allow refrigerated blood storage and patients could rarely afford the costs of travel to the referral hospital, to the distress of health workers: I feel so sympathetic and sorry. Transport is essential if the referral system is to work as intended, and is crucial when a facility cannot provide the intended services because of lack of infrastructure, power, equipment, supplies or qualified staff. Health workers showed pride in their facility when it had a functioning ambulance to transport referred patients or could rely on an ambulance sent on request from a higher-tier facility. On the other hand, working in a facility with no patient transport was deeply upsetting because many patients just could not afford to pay their own transport costs: They say they will go to the hospital but they go home and later you find out that they died. Health workers distress was acute when a health centre patient was referred direct to a distant regional referral hospital. They knew that patients were deterred not only by the travel costs but also by the prospect of a strange hospital and an alien language. Commonly, budgets did not stretch to fuel the vehicle for referrals. It was widely acknowledged that patients were asked to pay towards fuel but that was often beyond the reach of people in poor communities. The negative impact on nurses and midwives cannot be exaggerated. They came into nursing to save lives, to use their knowledge to benefit their communities. For them it was very hard and frustrating to stand by unhappy and helpless, knowing that a mother and baby would die because the vehicle lacked fuel. Nor was it a good experience to see patients return to the facility in a terrible condition and very weak or with complications because of the lack of fuel for referral. Health workers also found it frustrating when mechanical problems were left unattended. A managerial concern in the government sector was that effective referral systems require a means of communication from lower- to higher-level facilities. Health workers seemed resigned to using their personal mobile phones and paying for calls from their own pockets to contact referral hospitals.
Because of the constraints on providing transport, it was unusual to hear of a vehicle being used to bring patients to a health facility. Staff in a government sector hospital were proud that it provided an ambulance service to bring in emergency patients, and noted how relations with the community benefited as a result. There was also praise and gratitude expressed for a project that supported pregnant womens transport costs, resulting in more facility-based deliveries.
The impact on attitudes, behaviour and practices
Health workers spoke of their distress over how a lack of electric power, water and transport affected the quality of service. They wanted to do their best for patients but had to protect themselves too. They explained how patient perceptions of rudeness arose from the lack of power and water. The fear of infection influenced their approach to patients: Sometimes we come in with a scared heart or Sometimes you shy away from risk and the patient thinks you are rude, but it is the working conditions. They also acknowledged that the frustrations of working in the dark caused impatience and delays that patients construed as neglect.
The impact on community relations
It was said that patients refused to be admitted for treatment when the toilets did not work and they were not able to bathe, thus damaging the reputation of the facility. A lack of toilets forced staff to return home, fuelling patients beliefs they were not at work, and putting them at risk of being blamed by local political leaders for leaving the workplace while on duty. Recommendations from participants include: investment in good operating theatre facilities and their staffing in a small number of health centre IVs, and showcasing them as good practice before embarking on more building and rehabilitation work meetings between management and frontline staff to identify and act on infrastructure deficits that can be remedied locally staff involvement in direct action to remedy infrastructure problems.
17
Our Side of the Story: Ugandan health workers speak up
Equipment and medical supplies
Health workers praised facilities with good diagnostic equipment, such as X-ray and ultrasound, and a commitment to a well-equipped establishment: Its a good place, thats why I have stayed so long. Elsewhere, working with inadequate equipment was a huge challenge, damaging workers professional fulfilment, the quality of services and community relationships. The difficulties were acute in the government sector, but present too in parts of the not-for-profit sector.
The impact on health workers
Government sector medical doctors and nurses told of interruptions in supplies of oxygen and blood; missing canulas, needles, giving sets and sutures; minimal availability of urinetesting kits and family planning supplies; insufficient dressing packs; and absent or faulty diagnostic equipment. Rural midwives in the government sector told how they struggled to provide a service with no delivery kit, cord clamp, sucker, gauze or cotton wool and just one pair of scissors. Working without protective wear gloves, aprons, gumboots, shoes, masks was a huge risk, especially for midwives working in the dark: You are bathed in blood. Lacking gloves, midwives even used their own clothes and plastic bags to grasp the baby during delivery. Workers in some rural facilities in the government sector provided their own work clothes as, it was said, the Ministry of Health no longer supplied uniforms. In the government sector there was widespread frustration at not being able to work effectively: What really hinders my work is lack of some equipment and The equipment does not allow you to do what you are supposed to do. Nurses spoke about thwarted professional fulfilment. Willing to work to the best of their ability, they felt handicapped and disappointed. As a result, work was neither enjoyable nor happy: If I am provided with what I am supposed to use, I can enjoy the work or You cant really be happy in such conditions, but would be happier with equipment to do your best. Frontline medical doctors spoke of struggling with the minimum and of feeling deflated by poorly maintained equipment such as X-ray machines with blown bulbs or no chemical to print the film: You wake up and have the same problem, you go home, you come back and it has not changed. Doctors wanting the satisfaction of doing their best for their patients spoke of frustrations such as a lack of diagnostic equipment or facility for blood counts. Managers recognised that medical doctors eventually lose morale when they are unable to operate on a patient because oxygen or sutures are missing, and that being unable to apply knowledge was very demotivating.
Failing their patients greatly distressed nurses and doctors. Patients died because of the lack of essential supplies: We would have saved that life if we had oxygen. It stresses you. A lack of diagnostic equipment cost lives too: The patient probably would have survived if you were able to investigate. Government sector workers faced a dilemma when the facility ran out of supplies. User charges were abolished in 2001 in all government facilities except private wings in hospitals, and health workers told of prohibitions on asking patients to go and buy missing items: It is very annoying, you go home dissatisfied. The medical doctor has a duty towards the patients health: What do you do? Ask the patient to buy or see them get worse? The other option was to be kind and refer the patient to a higher-level facility. Participants spoke against the policy: I dont feel it wrong to ask a patient to buy needles in order to help them, and it was clear that patients in some facilities were being asked to buy supplies. It was hard to ask a patient to buy items that should have been provided free of charge: I dont want to be the one to say go and look for a canula. Participants in facilities with relatively good supplies welcomed relief from the stresses of telling patients to buy their own. They also expressed pride in a facility that did not force patients to spend what money they had on intravenous fluids, canulas, gloves, dressings and the like. There was praise for imaginative management that solved temporary supply problems by borrowing from other facilities.
The impact on attitudes, behaviour and practices
Participants working in the private and not-for-profit sectors spoke frankly about the effects of shortages they had seen during their time in government facilities. They told of nurses forgetting what they had been taught in training schools and some not working as a result, thus projecting a bad image to the community which in turn made nurses feel not respected and prompted them to leave. Participants in the government sector did not identify these effects. However, there was a suggestion that nurses were reluctant to come to work and
18
Our Side of the Story: Ugandan health workers speak up
face patients and their relatives knowing that essential supplies were lacking: Staff dont want to come in and look at a mother with a dying child and no canula to give intravenous fluids.
The impact on community relations
Health workers felt blamed for the lack of supplies and resented accusations of theft. The patients attitude changed when asked to buy supplies: You feel bad when somebody is not appreciating what you are doing. Patients carers were sometimes angry and violent, such as the husband who hit a midwife when asked to buy gloves. There were fears of personal repercussions if the rule was disregarded and the patient was asked to buy supplies: The Government is going to see you as a bad person. Staff in one facility were stressed by the arrest of a health worker who asked a patient to buy essential supplies. The view there was that local political candidates had set the arrest in motion to discredit the incumbent leader. Participants recommendations include: encouragement to international donors to supply large items of equipment directly more attention to the maintenance of essential equipment management consultation with frontline workers to identify and act on equipment shortfalls, alongside empowerment of workers through educating them on how the supply system works.
Attending a weekly mother-and-baby group. Children and pregnant women are the largest groups of health facility patients.
19
Our Side of the Story: Ugandan health workers speak up
Medicine supplies
Medicine shortages and stock-outs emerged as one of the biggest challenges for government health workers. Unable to give their patients the drugs they needed, health workers grieved for their patients suffering and became demoralised by the futility of their roles. They struggled with disappointed or angry patients and their limited understanding of the reasons for shortfalls in supplies. They were deeply hurt by accusations of stealing drugs, the lack of trust the public had in health facility staff, apparent press hostility and by what they saw as politically motivated moves to discredit them.
The drug supply situation
Outside the government sector, medicine supplies were generally thought adequate to treat most conditions. A sufficient supply brought health workers the satisfaction of working effectively, as well as pride in an efficient facility that logged all movements of medicines. The not-for-profit sector was not immune to shortages, however; in one facility shortages were said to be due to loss of revenue because it gave impoverished patients drugs on credit. In parts of the government sector there was some acknowledgement that government efforts to improve the delivery system of the central medical store had brought improvements in supplies of essential medicines. It was also noted that drug supply increased after a government stamp on packets was introduced. There was enthusiasm that better supplies now benefited patients: Now we have enough drugs, I would not say all drugs, and inpatients get the drugs the doctors prescribe. There was a sharp contrast between praise for medicine supplies in better-stocked facilities and disgruntlement among workers elsewhere. Health workers said some essential drugs were used up in a matter of weeks, or even days: They bring one tin of quinine tabs for the whole unit and Just five tins of Panadol which the department can use up in one day. Complaints centred on undersupply for population demand; shortfalls in supply where deliveries did not match orders; erratic deliveries, such as oversupply of condoms but no anti-malaria drugs; and irregular deliveries which did not conform to promised quarterly schedules. Shortages were said to be made worse by patients taking unfair advantage of brief periods of plenty, but with no testing equipment it was hard to refuse drugs to patients who claimed the common complaint of malaria. And it had been noted that patients turned up with a different patient record book every day of the week in order to stock up with drugs at home.
Government facilities typically could not stretch their budgets to purchase drugs in the private market, and were forced to sit and wait for the next delivery from the central medical store. However, one hospital dedicated a quarter of its private wing income to medicines.
The impact on health workers and the quality of care
Health workers said they felt disappointed and that the lack of drugs demoralises them. Job satisfaction suffered when they were unable to give patients the drugs they needed. Their presence in the workplace sometimes seemed futile: You are here, and there is nothing to give the patients. You are just sitting waiting for them, then tell them to go back as there is no drug. Especially hard to bear was being forced to tell poor patients to buy their medication in the private market: I hate the situation of being helpless before the patient when they cant afford to buy drugs and You feel you have not done much for the patient when they have to buy. It seemed like fobbing off the patient: You tell them to buy, but the patient is expecting answers. It was hard to be seen as letting down patients keen to have family planning supplies who could barely afford the transport to the facility: You feel so bad, it seems as if you are deceiving them and they lose confidence. Self-esteem suffered when drugs were not available: They look at you and think the health workers are bad, and yet it is the government not us or Their eye looks at the nurse and that doesnt make me able to be the nurse I want to be. The biggest source of distress for health workers was the impact on patients, and they spoke emotionally about how they felt for their patients when no medicines were available. In the case of antiretroviral drugs against HIV, which should be taken for the rest of a persons life, it was very hard to see patients go for up to six months without treatment.
A patient at Masindi district hospital, Uganda. Working with inadequate and missing equipment is a huge challenge for health workers.
20
Our Side of the Story: Ugandan health workers speak up
21
Our Side of the Story: Ugandan health workers speak up
Health workers cared passionately about the consequences for poor patients: Few can afford even 2,000 shillings [US$1], so day after day they walk here and wait. Walk 15, 20km despite the pain. They felt the pain too when patients became more unwell while waiting for their families to raise money to purchase medication. Hospital doctors spoke of how they were forced to refer admitted patients who could not afford to buy medicines, or just keep them in a bed without medication. The quality of care also suffered when the patient could afford only cheaper, inferior drugs which then failed to improve their condition, resulting in referral, an option many patients could not afford.
What kinds of drugs can we steal? Paracetamol? Because thats the only drug in the hospital!
There was widespread indignation at accusations of stealing non-existent medications: What are they supposed to be stealing? or What kinds of drugs can we steal? Paracetamol? Because thats the only drug in the hospital! and How can they take things that are not there! Health workers felt that local leaders and politicians made matters worse when they failed to present the true picture to complaining patients, and even accused health workers in front of the patients: It is making us lose morale for what we are supposed to do. Health workers resented negative stories in the print media, TV and radio, believing that journalists blew up single incidents unfairly to give an exaggerated picture of the extent to which frontline health workers were guilty of pilfering drugs. A stakeholder concurred: We cant brand all health workers as thieves just because someone has stolen a tin of aspirin. Stakeholders noted that press stories about health workers stealing drugs had increased with the work of the Medicines and Health Supplies Delivery Monitoring Unit, an autonomous unit set up in October 2009 within the Presidents Office. While there was support for its efforts to expose poor working conditions as well as abuses, the view was expressed that it was unhelpful to create a media story around every case of wrongdoing the unit uncovered: They tried to create publicity instead of dealing with the real issue of what is causing the stock-outs. There was also hurt and indignation when top public figures spoiled the professions reputations by stating publicly that health workers are thieves: How can any patient value a doctor, value a nurse, when they say such things about us! It was felt that government conspired to make out that all health workers were thieves although, in the opinion of health workers, top managers and not frontline workers were the chief culprits. Public accusations by the President were especially damaging to health workers self-esteem. Patients get angry because the politicians tell them drugs are provided. Views were expressed that politicians deliberately mislead the public: Government makes them believe they have sent drugs and The public is being hoodwinked! But for a public servant it would be suicide to contradict political masters.
The impact on community relations
It puts a lot of strain on community relations. Health workers said it was hard to make patients and other community members understand why drugs were not always available. They acknowledged that people sick and in pain had little appetite for words of explanation, and that the complexities of the supply system were beyond the understanding of some people without education. But they also told of angry, bitter patients who cursed them and refused to listen. In the past, Ugandan healthcare users maintained a belief that government health facilities lacked medicines even when receipts increased. According to health worker participants, there now appears to be a prevailing belief that health facilities are well supplied with medicines: People say why dont you give us drugs? A particular problem arose when a health facility changed ownership from not-for-profit to government and the previously superior supply of medicines could not be maintained. Health workers said that communities served by government facilities assumed health workers took the drugs: Patients think you steal and patients call us thieves. They said that patients believed that health workers took government supplies to stock their own clinics and drug shops, to which patients were then sent to buy medicines. It was acknowledged that such abuses had occurred. Indeed, good supplies in one hospital were attributed to the fact that few of its nurses ran private clinics and drug shops. Health workers regretted the lack of trust put in them and the effect on community attitudes: When drugs are not there, they tend to hate nurses. In contrast, it had been observed that patients attitudes towards health workers improved when given supplies of drugs to last several days. It was especially upsetting to be directly accused of theft when a patient demanded a drug that the clinician knew was not appropriate for their condition.
22
Our Side of the Story: Ugandan health workers speak up
Participants recommendations include: improved transparency at the point of medicine delivery, with the opening of boxes witnessed by the chairperson of the health unit management committee, the elected chair of the local community, the government internal security officer, police and patients supportive paperwork to show what has been ordered and delivered efforts to inform local leaders about the supply situation and ensure they use the information responsibly outreach to communities to explain the real situation through Village Health Teams, staff visits such as child immunisation days and talks to patient groups at the facility.
Politicians stop playing games on the right to health
A story is often told of a politician who delivered a truck laden with medicines to a health centre in his constituency. The truck was reportedly containing all the medicines that this health centre needed at the time. In a country where getting medicines in public facilities is intermittent and health workers are reviled for stealing medicines, this politician was an angel straight from heaven. Now, long after the speeches and pleasantries had ended, and the MP had gone, it was time to open the boxes. But alas, the boxes were full of saline solution. [] There was no way medics at the facility would tell people the next day that there was no medicine. To the politician he had scored a political goal. But in the process, the health workers had been put in a tight position.
Daily Monitor, 16 February 2011
How can a patient value a doctor, value a nurse, when they say such things about us!
23
Our Side of the Story: Ugandan health workers speak up
Pay
The frontline workers and managers participating in the research said they did not join their professions just for the money. They wanted to use their training to help others, prevent and cure illness and save lives: I became a nurse not so much because I am interested in money, though money is also important. I feel it really was a vocation. In any case, salaries were simply not attractive enough: With so little money, nurses must want to care and help patients, just to keep going. Money was never an overriding factor for job satisfaction, though among frontline doctors there were expectations of earning enough to help build yourself up and feel good about helping people at the same time. Yet there were some strongly held views among participants that some of the recent generation of health workers entered the profession with no genuine vocation for it and became disaffected because salaries were so low.
Staff in rural health facilities said that despite long working hours with little chance to rest, they worked over weekends and on public holidays for the sake of the patients. They even volunteered their help unpaid on top of their regular work, out of commitment to patients welfare, for instance in HIV clinics. Low salaries were of course a concern, and there were many calls for better financial compensation. But it is very striking that when asked about what had to change to make things better for them, health workers emphasised improvements in the infrastructure that would result in better care and treatment for patients. Frustration with equipment and supplies outstripped frustration over salaries. Nursing staff spoke heatedly about their struggles to survive on low pay and support their dependants, see their children through education, pay for a roof over their heads, settle essential bills and afford transport to work. Financial worries added to the stresses of long hours and little rest, the burden of having too many patients, the frustrations of not having enough medical supplies and lack of appreciation in the workplace: If better paid, a nurse will work with patients with love and happiness knowing that rent and bills are paid. In areas where demand for housing had pushed up rents, health workers found housing costs hard to meet or were forced to pay high transport costs to reach more affordable accommodation. Paying US$1.50 or more a day for transport was very hard to afford on a nursing assistants salary. In Uganda, income is needed not just to meet daily living costs. There are extended families to support: participants had up to 15 children depending on them. One of the satisfactions of earning is being in a position to support the study costs of a family member. As educated people, health professionals naturally want a good education for their children. Public primary and secondary education is free, but schools often impose fees for lunch, uniforms and building development, and many Ugandans favour the private schools that comprise over a quarter of the secondary education sector. Worry about school fees pervaded health workers lives. A participant spoke heatedly about the impossibility of affording university fees of US$900 a semester with three children and a monthly salary of US$330.
The impact on health workers
Health workers felt undervalued because salary levels did not match their needs and social expectations. The pay was felt to be unfair and not to represent an appropriate return for what they put in.
Money worries
Health workers said salaries were not enough to cover the costs of ordinary daily living, to allow them to pursue a career or to meet social expectations. They said that money worries got in the way of doing their best work and even contributed to bad practices. Managers said inadequate pay was one of the biggest challenges to healthcare delivery.
Society expects so much from you. Its impossible to convince people that you dont have money when you are a doctor
24
Our Side of the Story: Ugandan health workers speak up
Failing to meet social expectations
As a health professional there are also social expectations to meet. Family, friends and social associates assume you are well off, and it was shaming to reveal how meagre the salary actually was. Medical doctors especially felt embarrassed when they could not afford to contribute large sums of money at functions held to raise funds for wedding or funeral expenses. They were also expected to help with school fees or medical costs: Society expects so much from you. Its impossible to convince people that you dont have money when you are a doctor. The pressure came from the community expecting a nurse or doctor to be at a certain level and seeing them as not responsive to community problems. It was also hard for doctors to face the disbelief of patients begging them to pay for life-saving treatment that should have been freely available: You look in their eyes and see the hurt and the disappointment. Medical doctors and senior nurses spoke of unaffordable lifestyle aspirations such as a house that befits their status. Doctors wanted to be in a position to afford a decent house rather than put up with low-standard government sector accommodation on site.
Unfair pay
Participants regularly voiced strong opinions that the pay was unfair and undervalued health workers. Nurses complained that their salaries did not reflect the years of study they had put in. They pointed to other medical jobs that required the same length of training yet were more highly paid: Nursing is one of the lowest-paid medical professions. Doctors pointed to the much higher salaries of other professionals: We send our children to the same schools, buy our food at the same markets. It was dispiriting to see their university contemporaries earning so much more yet working less hard. The fact that medical doctors are paid less than secretaries and drivers in some statutory agencies underscored the lack of value attached to the medical profession in Uganda. There were some strong feelings, notably among managers and practising doctors, that low pay reflected a lack of political will at ministerial and presidential level to invest in healthcare. There was some anger about public spending on political campaigns, the military and a presidential jet, and about wastage through corruption, while healthcare was grossly underfunded. Salaries were doubly unfair because they did not reflect the long hours many health workers put in: You can give your family neither time nor money. Nor did salary levels take account of the risks of infection health workers faced. Not being rewarded for doing the same work as higher-grade staff was thought grossly unfair. It sometimes seemed to hospital nurses that doctors did little while they did all the work. Nurses complained that after paying for additional training to upgrade their skills, they lingered for years on their previous salary until promotion was granted. Another area of perceived unfairness was the disparity in salaries offered by the government, not-for-profit and private sectors. Not-for-profit sector workers pointed to their longer hours, and it was commented that unlike some government health workers they worked the hours they were paid for. It was pointed out that not-for-profit and private facilities were free to decide their own salary levels and acknowledge seniority in their own way, resulting in lower pay than in government settings. A particular grievance was the absence of a senior clinical officer grade in a not-for-profit facility. A further concern was that the governments salary enhancement for employment in hard-to-reach areas seemed not to have been adopted systematically in the not-for-profit sector.
Disrespect
In Uganda respect comes with how much you earn. It was said that patients look down on nurses when they know how little they are paid. Rural nursing assistants who were especially poorly paid said this would be a barrier to enlisting the help of the local community to advocate for higher salaries: Its our secret.
Thwarted professional ambitions
A widespread and serious concern was unaffordable further training: I have to sponsor my own study yet I am serving the nation! Health workers spoke, often passionately, about thwarted ambitions to improve their skills and knowledge. Nursing assistants wanted to train as enrolled nurses or midwives, and enrolled nurses and midwives to train as registered nurses and midwives. Registered nurses wished to add midwifery to their qualifications or go to degree level. Doctors wished to bring their knowledge up to date and train as specialists.
25
Our Side of the Story: Ugandan health workers speak up
Rarely was it said outright that health workers are exploited, although there were views that unfair advantage is taken of their professional ethics and dedication to patients: Nurses are trained to love and serve, to forswear hard conditions, and no matter how little we are paid we have to have that love. Indeed, among managers there was some intolerance of frontline workers complaints about low salaries and an attitude that commitment to the work regardless of the pay was praiseworthy: Patients have to get a service, poorly paid or not. Yet managers were among the most vocal critics of salary levels: The salary is deplorable! Overall, participants appeared more resigned than militant about unfair pay, though there was some anger that the Government cited the Hippocratic Oath to prevent doctors from protesting.
workers thought that pilfering of medicines happened only on a small scale and that drugs were taken for personal or family needs and not to sell. But there were also views that helping yourself had become a habit, with reports of staff openly justifying selling supplies on the grounds that the facility did not reward them well enough. Participants with experience of closely managed facilities spoke of tighter administrative practices that helped to safeguard medicines. Workplace cultures that accepted stealing were also noted. The suggested solutions were tighter management to reduce opportunities for abuse, and holding staff to their codes of employment. Peer influence to change behaviour was seldom proposed. Taking money from patients is a sensitive topic which some health workers were understandably reluctant to discuss. Soliciting bribes from patients was thought to be rare and was unacceptable because it would add to patients poverty. If it did occur, it was attributable to low pay: If paid a satisfactory salary I think they would not get money from the patients. There was also a view that worries about surviving on retirement pensions drove health workers to ask for bribes. It was observed that in some settings patients expected to give staff some inducement to attend to them. Such mistrust was hurtful and offensive, and it was suggested that the distance between workers and patients widened as a result. Participants told of scams whereby patients were robbed of their money by conmen masquerading as health workers, and of angry patients subsequently attacking legitimate staff. Health workers distinguished accepting appreciation from demanding money and some acknowledged a temptation to accept unsolicited money from patients as compensation for ill-paid, exhausting work. It was suggested that some see health workers accepting appreciation and wrongly conclude that a bribe has been taken. It was widely believed that urban health workers were forced to work in two or even three jobs to make ends meet, with government sector employees also working in private clinics or private hospitals. One unfortunate consequence, it was said, was to reinforce patients suspicions that health workers steal drugs from their workplace to sell in private clinics. Moonlighting was often known, or suspected, to explain absences: Most people, when they dont turn up for work you find they are running a clinic somewhere. It was said that absenteeism was not a problem in areas where private treatment or drugs were unaffordable. Exhaustion from doing too many jobs was thought to cause behaviour patients saw as rude. Rural areas were said to offer many fewer opportunities for side employment, but there it seemed that health workers were sometimes forced to take time out to tend crops to feed their families. It was noted that before decentralisation, rural workers regularly saw to their vegetable gardens before leaving for work, when salaries arrived late or not at all. It was suggested that this habit continued.
The impact on attitudes, behaviour and practices
Health workers and managers were encouraged to say what in their view explained behaviour regularly criticised in the Ugandan media, including being rude to patients, stealing medicines and supplies, not turning up or coming late to work, and taking money from patients. Health workers acknowledged that these bad practices did happen in some places: Its poverty. You get a salary of US$200, you pay school fees of around US$150, you get stuck. You dont have transport to take you to work, you dont have food in the house, you dont have anything, children are crying, your parents need you to keep them. Thats what drives people to do those things. But they also argued that the media exaggerated the scale of such practices by unfairly generalising a single instance to all health workers: It spoils the reputation of all nurses, it pains and discourages us so much.
If the pay was more, the nurses would respect their work more
One of the hottest topics in the Ugandan media is the apparent disappearance of essential medicines and medical supplies between the central store and patients in government health facilities. Theft on the part of health workers is only one explanation for shortfalls in supplies. Participants acknowledged that theft did occur within some health facilities. In their view, the explanation lay with low pay and money worries: They are not stealing medicines because they are evil their income does not satisfy their needs. Delays in salary payment were implicated too: They steal for survival. In no way was stealing condoned. Some participants were upset that patients were deprived of already scarce supplies. Others were bewildered that health workers could put their own interests before those of patients. Only rarely did participants believe that greed led health workers to steal. Some health
26
Our Side of the Story: Ugandan health workers speak up
There were beliefs that absence from the workplace was encouraged by lump sums given notionally to cover transport and attendance at workshops, and there were some grievances about perceived unfair selection of participants: They only want the big people. The more junior staff valued the learning and professional contacts that workshops offered. Effort at work was affected by low pay, managers felt. Views were expressed that nurses put in minimal effort because they feel they are not getting what they are worth. It was observed that because nurses are paid so little, they take out their frustrations on patients, arrive late, fail to monitor patients and are unkind to them. It was noted how hard it was to get people to work when they lacked the basic minimum, and that with no incentive of a decent wage it was impossible to retain skilled and interested workers. Occasionally in managers eyes, low morale was related to low pay. Low pay was also argued to contribute to doctors questionable attitude to work. Things would change with better pay: When you are paid highly you are more motivated and If the pay was more, the nurses would respect their work more and respect the job that pays them.
For others, nursing abroad was a real aspiration, and there were one or two stories about disappointments. Nurses reasons for considering working outside Uganda counter the widely held perception that the lure of money pulls nurses to lucrative jobs in other countries. Better pay was not an overriding consideration. Nurses explained they were looking for an environment where theres respect for what you do and where they could learn about different medical conditions, use equipment they were trained to use, update their skills and have the chance to advance professionally. Individual advancement was not the sole driving factor: I would bring my skills back to share with Ugandan nurses and I would bring back the knowledge to my people. Among participants with medical qualifications there were beliefs that medical doctors left the country in large numbers for greener pastures, as well as claims that few of their graduate contemporaries were still in Uganda, though the lack of hard facts on the extent of emigration was also acknowledged. The prevailing assumption was that doctors moved in pursuit of money. When questioned about their own intent, doctors spoke about the attraction of a better income. Yet opportunities to work with proper equipment and love what you do also were important not simply a good salary. Doctors were interested in working in highly regarded, well-resourced hospitals in other East African countries or in Southern Africa. African countries were attractive because they are close to home, but the USA and Europe were not ruled out. Not all doctors wanted to leave for better working conditions and there were also keen ambitions to take their skills to countries even more in need of medical doctors than Uganda, such as Sudan or Somaliland. Participants recommendations include: increased basic salaries, a minimum wage, revision of salary scales to recognise university degrees and alignment of salary scales across the government, not-for-profit and private sectors overtime payments and an allowance to recognise responsibility when in sole charge of a ward free accommodation of a good standard, with electricity and water paid for donations of free food for the household, tea and snacks provided at work, Christmas and Easter gifts and contributions towards extraordinary personal expenses, to show that health workers are valued allowances for risk, housing, transport, responsibility and study, as well as hardship wider use of income from the private wings of government hospitals to benefit staff.
Poor pay, turnover and loss to Uganda
The research participants were, of course, stayers in their profession. Career histories showed a fair amount of mobility from one health facility to another, but only very exceptionally did a participant speak of leaving their profession, and that was to earn more. The consensus was that the biggest turnover was among medical doctors. There were firm beliefs that Ugandan-trained doctors left the government sector to work for NGOs, prestigious not-for-profit hospitals or the private sector. Private sector work was appealing as a way to make more money and avoid the frustrations of government hospitals. Managers and practising doctors told how young doctors run away from hard-to-fill rural posts because of poor salaries. Yet practising doctors explained that for many young doctors, a year or two gaining experience in a rural setting, even in deprived circumstances, was a step towards acceptance for specialist training. Staying longer meant passing the age limit for scholarships. Specialism was then the gateway to private practice and considerably higher earnings. In any case, district-level facilities could rarely support the costs of a specialist who wished to return after training. Participants were asked if they had thought about working abroad and why. For some nurses, the possibility was remote: family responsibilities came first, the barriers to getting a nursing job abroad were just too high, or they had not even realised it was allowed.
27
Our Side of the Story: Ugandan health workers speak up
The way forward
Work overload, poor infrastructure and the lack of medical equipment, supplies and medicines frustrated and distressed health workers. They felt unrewarded for the work they do and undervalued. Their accounts show that working conditions were the root causes of bad practices and unethical behaviour, and that health workers bore the brunt of the blame for system failures. The research revealed a vicious circle: impoverished working environments, along with low pay, affected the quality of patient care; patients blamed the health workers; the wider community then distrusted health workers, whose level of stress increased. The situation was made worse by negative media stories and political leaders criticisms of health workers, which fuelled public distrust, damaged the standing of the health profession, added to workers distress and, most importantly, raised the barriers to access to healthcare.
Raising the voices of health workers
The view of civil society organisations, and of some managers, was that frontline health workers are not empowered to speak up. Indeed the concept of voice was unfamiliar, and the idea that they might speak out and gain support to improve poor working conditions and the quality of care was new to many frontline health worker participants. The research identified barriers to individual health workers voicing their concerns and their preferences for advocacy by representative organisations. There were views among frontline workers that responsibility for improvements lies with facility managers, district management or the Ministry of Health. Stakeholders noted that where decisions are made with no staff involvement the staff are afraid for their jobs, they fear to speak up. Anxiety about reprisals was a barrier to speaking out in public. It was explained that in Uganda there is a lot of fear of being pinpointed if you talk out about your problems. The low esteem accorded to health workers was a further barrier. It was said that nurses do not speak out because of the stigma attached to the profession: The moment you stand up and say you are a nurse, people see you as a person who kills patients, they assume you are a bad nurse, a failure. A lack of respect from management undermined nurses. Those with experience in large urban hospitals told of senior nurse managers and administrators who sat on, barked at and belittled them in front of patients. They also spoke of doctors who publicly ignored and disparaged their
knowledge and contributions as mere nurses: I have quite often heard doctors tell a nurse she is stupid. Such behaviour coloured patients respect for nursing staff and damaged their reputation in the wider community: They think a nurse barked at is nothing. They said management blamed nurses unfairly, failed to investigate problems and made their lives miserable. Oppressed and voiceless in the workplace, it is not surprising that nurses had little appetite for championing their profession. This report has shown that rural workers in government facilities have faced disappointed, distrustful and sometimes angry patients, interfering and bullying local politicians and politically engineered attacks on health workers credibility. Hostile environments and impoverished workplaces drained any will they had to do more than meet patients needs the best they could. Moreover, health workers had few chances to meet with people from other healthcare facilities to exchange experiences and build solidarity. Nurses spoke enthusiastically about a forum organised by a health sub-district which discussed solutions to common problems.
Speaking through professional associations, unions and regulatory councils
Health worker participants favoured channelling concerns to the Ministry of Health, Government or Parliament through bodies that spoke for them as, unlike individual health workers, such bodies know the way. Awareness of professional organisations and trades unions was not widespread and there was some confusion over their names, how their status differed and which body did what.
We never show why we should be valued
28
Our Side of the Story: Ugandan health workers speak up
Some health workers felt unions were doing a good job, evidenced by salary increases and the successful legal defence of individual workers. Health workers saw advantages in the protection of a union and the pursuit of individual complaints. A union had the advantage over an association of registration with the Ministry of Labour and permission to negotiate with the government. Male frontline workers spoke most enthusiastically about the potential of unions as a collective voice, and saw a need for local organisation and meetings at district level. They also identified a role for unions to strengthen advocacy within health facilities and talk to management on behalf of the workers: They need to bring in people from above and help
us at a lower level to improve things. Women too saw the potential strength of the nurses union if all nurses joined collectively, paid subscriptions and attended meetings. There was some confidence that more involvement in unions would get nurses listened to at the national level. Supporters of the nurses union acknowledged that nurses were not currently well informed about it. It was suggested that professional associations might do more to bring members together, such as convening annual meetings to discuss challenges facing the profession. Opportunities to attend professional association conferences were few but highly valued, and there were calls for them to be held locally.
Young woman collecting water, Kampala, Uganda. Under one-third of Ugandan health facilities have tap water or a clean source within 500m.
29
Our Side of the Story: Ugandan health workers speak up
However, there were also doubts about the value of the unions and professional associations. It was pointed out that bodies did not do enough to inform their memberships about their activities or call them to meetings. A lack of feedback, of tangible benefits and of evidence of proper financial management, alongside rumours of power struggles, deterred workers from spending part of their small salaries on subscriptions to remote associations and unions. There were also suspicions that those at the top of the organisations had different agendas from workers on the frontline. The effectiveness of representative bodies was also questioned, given a history of government suppression. There were conflicting interpretations and some misunderstanding of the remit of the regulatory councils. Some health workers saw their council as equivalent to a union, with a role to advocate for their constituency. Others perceived a punishing attitude, and complained that the Nurses and Midwives Council was down on nurses and investigated only serious, high-profile cases of irregular behaviour. Concerns were voiced that the council did little to defend nurses accused of stealing medicines and that no action had been taken against politicians who beat up nurses. The nurses council was seen as remote from nurses on the ground, preoccupied with meetings, disinclined to inform members of what they discussed and not independent enough of government. It was suggested that it would be better if representatives of professional associations, unions and regulatory councils were less remote from workers on the ground. In particular, there were calls for people up there to visit health facilities, talk with health workers and learn about their difficulties first-hand, so that the right voices were taken to the top. Recommendations among managers were that representative organisations compare reports from different places and compile strong collective arguments to improve conditions in the workplace, rather than simply address individual grievances and traditional welfare issues. Representatives of associations and unions acknowledged shortcomings and weaknesses. They were understaffed and severely under-resourced, with poor office facilities. The consensus among stakeholders was that individual associations and unions were not yet strong voices for health workers and that working in an alliance would be more effective. It was recognised that much would have to be done to align the efforts of multiple and sometimes competing professional unions and associations.
Health workers interests fall mainly to the professional organisations. Coalitions rarely bridge the two sets of interest. The Health Workforce Advocacy Forum Uganda is a coalition of health professional associations, unions and health rights organisations. A membership organisation largely made up of health workers, it has recently campaigned for a positive practice environment for health workers. The Valuing Health Workers research found consensus that a way forward would be for all civil society organisations concerned about limits on access to healthcare to join with the Health Workforce Advocacy Forum Uganda, to support and strengthen its advocacy on behalf of health workers.
Changing public perceptions of health workers
Participants were hugely affected by the persistently negative portrayal of health workers in Uganda: I feel like I am a professional being abused. Members of civil society and professional organisations identified priority actions to reverse that image through targeting the media. Strong views were expressed by health workers that the public must hear their story: We havent gone to the radio to tell people the problem is not us. We should be talking about our side of the story. The public must be told the real causes: Papers always blame the person, saying nurses are rude, etc, but theres a need to dig and find what really causes it. People must see the contributions health workers make: We never show why we should be valued. Participants said that reporters working for the national media are inadequately informed about the health worker situation and are overly reliant on official briefings for their information. It is important to increase the capacity of civil society and health worker organisations to write press releases, hold press conferences and build relationships with individual reporters and media houses, so that the key campaign messages hit home. It is similarly important to engage with local reporters and try to moderate the tendency to create sensational stories from isolated incidents. The Uganda Health Communication Alliance is an important ally. While it was widely understood that the media look for bad news, there was scope for positive human interest features, such as profiles of individual health workers and the work they do. It will be important to avoid suspicions of favouritism in selection of the health workers featured.
An advocacy alliance
In Uganda countless small civil society organisations work to promote health rights. Dependent on financial support from a patchwork of sources (mainly development partners), they gain strength through loose, generally informal coalitions based on common aims. They are broadly aligned to consumers interests.
We should be talking about our side of the story
30
Our Side of the Story: Ugandan health workers speak up
Local language radio is highly popular in Uganda and is a vehicle often used by civil society advocacy organisations. Radio call-in shows attract health users voicing complaints about local services: You hear them on the radio, it makes us uncomfortable. While health workers are restricted in what they can say publicly, civil society organisations have the opportunity to put complaints in the wider context and speak up for health workers.
but health workers reported favourable effects when a top local politicians family used maternity services at a local government facility. Seeing the challenges encouraged the politician to understand their root causes. A more general recommendation was to invite politicians to spend time in facilities alongside staff to see what the work is really like.
Bridging communities and healthcare facilities and staff
There seemed, from health workers accounts, to be places where relationships between patient communities and facilities worked well. These were places which ignored status so they dont feel you are greater than them and welcomed patients on the same level; where off-duty nurses mixed socially with patients; where Village Health Team workers visited the facility and had direct phone contact with the facility head and other staff; where people called for an ambulance and it came; where local people volunteered to clean the facility and look after the compound; where facility management listened to what the local community wanted from it and where the community saw the facility as their own. At district level, managers told of ongoing efforts to build or repair bridges with communities. There was a role for members of Village Health Teams (where they were functional) as go-betweens to explain to people in their own homes the problems health workers faced. Outreach, where facility-based health workers took services such as immunisation to the community, was thought a good opportunity to talk with people on their own ground, though limited by a lack of transport. There were hopes that empowered health unit management committees would tell the community the truth. The aim was for committee members to explain how facilities work for example, how supplies are ordered and staff disciplined as well as to encourage people to use their services. But funds were short to cover the expenses of village health workers, outreach and health unit management committee members. Community dialogue meetings were recommended to bring together service users, local leaders and those involved in providing services: If there can be community dialogue meetings in each village, then we can discuss with them their problems. We tell them what we do, they express their problems, how we go wrong, I also tell them where they go wrong. Community dialogues also meant that district managers learnt community views about individual health workers. There were places where the distance between communities and facilities appeared hard to bridge. Patients arrived expecting staff not to help, and health workers came to work fearing that patients would complain: They dont respect the nurses needs, we dont respect each other. Interfering and demanding politicians seemed an intractable problem,
They dont understand what we go through, that sometimes nurses are rude due to the working conditions
Mutual respect and understanding
Health workers understood what life is like for patients, they felt the pain that patients feel and they wanted better conditions to improve things for patients. It was exceptional to hear that patients empathised with health workers: Patients also feel badly when they see us with no way to help them. They dont blame us. When you explain, they understand. More commonly health workers said that patients did not understand what life is like for health workers: They dont understand what we go through, that sometimes nurses are rude due to the working conditions. Patients seemed not to realise that health workers, like any other people, get tired, need to eat and fall sick. Health workers said they tried to get them to understand we are human beings. Civil society organisations have been working to create common cause between health workers and patients. Early projects learnt that empowering community members to exercise their health rights must go hand in hand with valuing health workers. Otherwise there is a real risk of adversarial relationships between healthcare workers and users. Indeed, early experiences were that community members, fired up with new knowledge about violations of their health rights, reprimanded workers they perceived to be rude, while health workers complained of harassment and threatened to resign. Subsequently, community-based training has enabled health workers to speak out about the structural problems, with service users coming to appreciate the reasons behind health worker behaviour they object to. Now the focus of community-based training has moved towards fostering mutual understanding and communication through participatory methods involving health workers and community members together.
31
Our Side of the Story: Ugandan health workers speak up
Summary of participants recommendations
The findings identified two priorities for action
1. Value health workers for their contributions to the health of Ugandans. 2. Expose the poor working conditions that prevent health workers from providing good-quality healthcare.
Four enabling strategies emerged from health workers accounts and stakeholder advice
1. 2. 3. 4. Improve the quality and relevance of training. Raise the voices of health workers through representation. Change public perceptions through the media. Build bridges with patient communities.
Priorities
1. Value health workers for their contributions to the health of Ugandans
Health worker terms and conditions of service Review salary scales to determine whether increases in basic salaries are possible. Reform government salary scales to recognise first and postgraduate degrees, in order to attract degree nurses to public sector jobs and ensure their education is used to support patient care directly. Consider the establishment of a minimum wage and the feasibility of imposing the same salary structure in all sectors (government, not-for-profit and private). Overtime and responsibility payments Explore a system for remunerating health workers for overtime. Consider implementing a responsibility allowance paid when a nurse has sole charge of a ward. Small financial motivations Incentivise staff through small items of personal support, such as food for the household, snacks at work, and Christmas and Easter gifts. Contributions towards family burials, medical operations and provision of cloth for uniforms are well received. Review current allowances for risk, hardship, housing, transport, responsibility and study, to ensure consistency and fairness across all facilities. Use the income from local government hospitals private wings to benefit staff, by supplementing salaries or allowances.
2. Ensure working conditions enable health workers to provide good-quality healthcare
Health worker/patient ratios Introduce standards for patient/nurse and patient/doctor ratios, so that health worker overload is transparent and quantifiable, and managers have information to help reduce pressure on overloaded staff. Recruitment blockages Manage health worker recruitment and deployment centrally, to address the problem of unfilled posts and uneven distribution of health workers. Decent staff accommodation The Government should follow through on its strategy to provide decent and safe accommodation for health workers at health facilities, especially in remote areas. Civil society organisations should continue to monitor implementation of this strategy and press for concrete targets. Facility infrastructure Ensure regular meetings between management and department heads, at which facility-related problems can be raised and decisions taken on actions needed. Invest in good theatre facilities and their staffing in a small number of level IV health centres, and showcase them as good practice before embarking on further investment. Equipment, medical and medicine supplies Give much more attention to the maintenance and quick repair of medical equipment, including systems for monitoring equipment maintenance and adequate stocks of spare parts. Hold regular formal consultations with frontline workers to enable them to participate in decision-making about equipment and supplies, and to improve transparency in equipment procurement processes. Encourage international donors to provide large items of equipment directly.
32
Our Side of the Story: Ugandan health workers speak up
Enabling strategies
1. Improve the quality and relevance of health worker training
Career guidance and early contact Ensure well-motivated trainees, for example through more talks at schools and work experience placements. Training schools admission procedures Reject applicants who seem to be applying for the wrong reasons, including those allocated to a university course which is not their first or second choice. Developing and sustaining the right heart in training schools Return oversight of training to the Ministry of Health from the Ministry of Education and Sports. Reduce nursing and midwifery class-sizes and improve tutor capacity, to ensure the right attitudes and practical understanding of the ethical code are encouraged throughout pre-qualification training. Health and human rights training Expand existing partnerships between training institutions and health consumer advocacy organisations. Improve nursing course content to make sure that students take on board the role of the nurse as a patients advocate. De-urbanise health worker training Increase the number of training schools and residency programmes in rural areas to produce staff already adapted to rural environments and connected to the local community. Improve the community service element in medical curricula and increase the exposure of urban health students to rural settings with increased fieldwork. Nurses and Midwives Council registration interviews The Nurses and Midwives Council should weigh up the advantages of screening interviews held as a prerequisite for registration post-qualification against detrimental effects on nurse morale.
Professional associations and unions should do more to bring members together, for instance at local general meetings, and make greater efforts to visit facilities and talk with health workers so that the right voices can be taken to the top. They should compile strong collective arguments to improve conditions in the workplace, as well as addressing individual grievances and traditional welfare issues. The Health Workforce Advocacy Forum Uganda (a coalition of health professional associations, unions and health rights organisations) should expand its membership and continue its campaign for a positive practice environment for health workers.
3. Change public perceptions by influencing the media
Inform journalists about the obstacles to health worker recruitment and discourage them from writing sensationalist or negative stories in the media. Put complaints on local language radio call-in shows into a wider context. Encourage the running of positive human interest features, such as profiles of individual health workers and the work they do. Work with the Uganda Health Communication Alliance. Improve the capacity of civil society and health worker organisations to write press releases, hold press conferences and build relationships with individual reporters and media houses, so the key campaign messages hit home.
4. Build bridges between patient communities, healthcare facilities and staff
Transparency on drug availability Use well-managed public opening of medicine deliveries to help convince communities that medicines are not in stock, and to counter accusations of theft. Call on local notables, police or patients to witness the opening of boxes. Support with paperwork to show what has been ordered and delivered. Ensure that local leaders are fully informed through regular meetings about the demand for and supply of drugs and that they use this information responsibly. Connecting communities and facilities Use opportunities to talk with people on their own ground and explain the problems health workers face, for instance through Village Health Teams, facility-based health workers providing outreach immunisation services, and talks to women awaiting prenatal checks. Promote community dialogue meetings bringing together service users, local leaders and health unit management teams. Increase funds to cover these activities. Invite top local politicians to spend time in facilities alongside staff to see what the work is really like. Civil society organisations should continue their work to create common cause between health workers and patients.
2. Raise the voices of health workers
Sharing of experience and common approaches Encourage staff to meet with people from other healthcare facilities to discuss solutions to common problems and communicate them to sub-district level managers. These managers could also be encouraged to instigate similar forums. Speaking through professional associations, unions and regulatory councils Channel health worker concerns to the Ministry of Health, Government or Parliament through bodies that speak for them, such as professional organisations and trade unions.
33
Our Side of the Story: Ugandan health workers speak up
References
Achan J, et al (2011) Case Management of Severe Malaria A Forgotten Practice: Experiences from health facilities in Uganda, PLoS ONE 6, 3. Matsiko C (2010) Positive Practice Environments in Uganda: Enhancing health worker and health system performance, International Council of Nurses, International Pharmaceutical Federation, World Dental Federation, World Medical Association, International Hospital Federation and World Confederation for Physical Therapy. Ministry of Finance, Planning and Economic Development (2010) Millennium Development Goals Report for Uganda 2010. Special theme: Accelerating progress towards improving maternal health, Kampala: Ministry of Finance, Planning and Economic Development. Ministry of Health (2008a) Pharmaceutical Situation Assessment Level II, Health Facilities Survey in Uganda: Report of a survey conducted JulyAugust 2008, Kampala: Ministry of Health. Ministry of Health (2008b) Access to and Use of Medicines by Households in Uganda: Report of a survey conducted 2008, Kampala: Ministry of Health. Ministry of Health (2010) Health Sector Strategic and Investment Plan: Promoting peoples health to enhance socio-economic development 2010/112014/15, Kampala: Ministry of Health. Oketcho V, Namaganda G and Matsiko C (2009) Human Resources for Health Planning In Uganda: Practice and lessons, Uganda Capacity Program, IntraHealth International, Uganda. Republic of Uganda (2010) Annual Health Sector Performance Report Financial Year 2009/2010, Kampala: Ministry of Health. Uganda Country Working Group (2010) Medicine Price Monitor Uganda No 9 AprJune 2010, Kampala: Uganda Country Working Group.
34
ISBN 978-1-903697-13-9
9 781903 697139
Valuing Health Workers is VSOs research and advocacy initiative, which supports the achievement of the health-related Millennium Development Goals. Valuing Health Workers research is currently underway in four countries. Following on from the research, advocacy strategies will be created, which will include the development of volunteer placements in civil society coalitions, professional associations and health ministries. VSO works with the Health Workforce Advocacy Initiative (HWAI). HWAI is the civil-society led network of the Global Health Workforce Alliance (GHWA) and engages in evidence-based advocacy with the goal of enabling everyone to access skilled, motivated and supported health workers who are part of well-functioning health systems. www.healthworkforce.info/HWAI/Welcome.html VSO works with Action for Global Health a cross-European network of health development organisations. The network calls on European Governments and the European Commission to act now to support developing countries to achieve the health-related Millennium Development Goals. www.actionforglobalhealth.eu For more information please contact: advocacy@vso.org.uk If you would like to volunteer with VSO please visit: vsointernational.org/volunteer In addition to this publication, the following research and publications may also be of interest: Participatory Advocacy: a Toolkit for Staff, Volunteers and Partners this manual is an easily accessible guide to lobbying and campaigning, and can be used by health activists and other campaigners for social justice. Ugandan Health Workers Speak: The Rewards and the Realities a report of initial findings of the Valuing Health Workers research in Uganda. Valuing Health Workers in Cambodia a short briefing on the research approach in Cambodia. Valuing Health Workers: Implementing Sustainable Interventions to Improve Health Worker Motivation (Malawi) a report drawing together existing research in Malawi, and identifying recommendations to tackle the HRH crises. Local Volunteering Responses to Health Care: Challenges and Lessons from Malawi, Mongolia and the Philippines this report looks at how community volunteers can be involved in delivering health services. Brain Gain: Making Health Worker Migration Work for Rich and Poor Countries. VSO Briefing: the perspective from Africa. The IMF, the Global Crisis and Human Resources for Health this 2010 report, written with the Stop Aids Campaign and Action for Global Health, shows how the IMF is constraining the fiscal space for developing countries and impeding the recruitment of much-needed new health workers. To access any of these publications, please visit: www.vsointernational.org/health
Carlton House, 27a Carlton Drive Putney, London, SW15 2BS, UK +44 (0) 20 8780 7500 www.vsointernational.org VSO is a registered charity in England and in Wales (313757) and in Scotland (SC039117).
Published January 2012
VSO Bahaginan www.vsobahaginan.org.ph VSO Ireland www.vso.ie VSO Jitolee www.vsojitolee.org
VSO Netherlands www.vso.nl VSO UK www.vso.org.uk
You might also like
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- NORMSDocument236 pagesNORMSpankaj agrawal100% (1)
- VSO Advocacy ToolkitDocument100 pagesVSO Advocacy ToolkitVSONo ratings yet
- Room Pressurization Control Application Guide - A6V10308401 - Us en PDFDocument64 pagesRoom Pressurization Control Application Guide - A6V10308401 - Us en PDFKagitha TirumalaNo ratings yet
- IDBE-WO-YPZZZ-En0001 Onshore Construction Execution Plan, Rev 0Document56 pagesIDBE-WO-YPZZZ-En0001 Onshore Construction Execution Plan, Rev 0Advis100% (2)
- TelemedicineDocument19 pagesTelemedicineecell_iimk100% (1)
- Otolaryngology Mcqs & SBAs 2nd EditionDocument6 pagesOtolaryngology Mcqs & SBAs 2nd EditionJohn M. HemsworthNo ratings yet
- Excerpt of Genius On The Edge by Dr. Gerald ImberDocument18 pagesExcerpt of Genius On The Edge by Dr. Gerald ImberKaplan Publishing100% (1)
- VSO People FirstDocument16 pagesVSO People FirstVSO100% (1)
- VSO Editorial GuidelinesDocument22 pagesVSO Editorial GuidelinesVSONo ratings yet
- VSO Photovoice Facilitators GuideDocument20 pagesVSO Photovoice Facilitators GuideVSO50% (2)
- VSO Stories of Change - MalawiDocument36 pagesVSO Stories of Change - MalawiVSONo ratings yet
- VSO Uganda Strategy 2012-15Document8 pagesVSO Uganda Strategy 2012-15VSONo ratings yet
- VSO Sierra Leone Strategy 2012-15Document8 pagesVSO Sierra Leone Strategy 2012-15VSONo ratings yet
- VSO Nigeria Strategy 2012-15Document8 pagesVSO Nigeria Strategy 2012-15VSONo ratings yet
- VSO Cambodia Strategy 2012-17Document8 pagesVSO Cambodia Strategy 2012-17VSONo ratings yet
- VSO Nepal StrategyDocument8 pagesVSO Nepal StrategyVSONo ratings yet
- VSO Cameroon Strategy 2012-15Document8 pagesVSO Cameroon Strategy 2012-15VSONo ratings yet
- VSO Bangladesh StrategyDocument8 pagesVSO Bangladesh StrategyVSONo ratings yet
- VSO Rwanda Strategy 2012-17Document8 pagesVSO Rwanda Strategy 2012-17VSONo ratings yet
- VSO Tajikistan Strategy 2012-16Document8 pagesVSO Tajikistan Strategy 2012-16VSONo ratings yet
- VSO and Youth Position PaperDocument16 pagesVSO and Youth Position PaperVSONo ratings yet
- VSO Health Volunteers Briefing PackDocument22 pagesVSO Health Volunteers Briefing PackVSONo ratings yet
- VSO 2012 Annual ReportDocument64 pagesVSO 2012 Annual ReportVSO100% (1)
- VSO CWS Position PaperDocument4 pagesVSO CWS Position PaperVSONo ratings yet
- VSO Stories of Change - MalawiDocument36 pagesVSO Stories of Change - MalawiVSONo ratings yet
- VSO Our Side of The Story Uganda - Full ReportDocument68 pagesVSO Our Side of The Story Uganda - Full ReportVSONo ratings yet
- 2187 Optiflo Brochure AW Amended WebDocument2 pages2187 Optiflo Brochure AW Amended WebShalom BhopaleNo ratings yet
- Adaptive Leadership FlyerDocument2 pagesAdaptive Leadership FlyerFauquier NowNo ratings yet
- Director Medical Staff Services in Minneapolis ST Paul MN Resume Lynn SeelingDocument3 pagesDirector Medical Staff Services in Minneapolis ST Paul MN Resume Lynn SeelingLynnSeelingNo ratings yet
- Orthodontist CV PeshawarDocument3 pagesOrthodontist CV PeshawarYasir IsrarNo ratings yet
- Doh HospitalDocument7 pagesDoh HospitalJasmine Montero-GaribayNo ratings yet
- Hospital Data BankDocument6 pagesHospital Data BankBOOKREADER_NOWNo ratings yet
- Humanitarian Assisstance of Mormon Church in SerbiaDocument8 pagesHumanitarian Assisstance of Mormon Church in SerbiaSasa MilosevicNo ratings yet
- Unit 13 Task AnalysisDocument11 pagesUnit 13 Task AnalysisStark ToursNo ratings yet
- Flow and TableDocument7 pagesFlow and TableRainbow DashieNo ratings yet
- 1 Coophealthproviders 091521Document42 pages1 Coophealthproviders 091521ariel DeeNo ratings yet
- Minor Head InjuryDocument2 pagesMinor Head InjurySamer FarhanNo ratings yet
- Tugas Ketua Jabatan Pediatrik KardiologiDocument3 pagesTugas Ketua Jabatan Pediatrik KardiologisjamilmdfauzieNo ratings yet
- In Touch FL27 PDFDocument247 pagesIn Touch FL27 PDFJuanAguileraOlivoNo ratings yet
- Blood Is Thicker Than WaterDocument1 pageBlood Is Thicker Than WaterBalkis Semera Lot UluNo ratings yet
- 98 ExerciseDocument4 pages98 ExerciseMuội LêNo ratings yet
- Measure Vital Signs and Teach Relaxation BreathingDocument5 pagesMeasure Vital Signs and Teach Relaxation Breathingmauludina zahrrohNo ratings yet
- Hospital and Clinical Pharmacy CH 1 Hospital Pharmacy NotesDocument12 pagesHospital and Clinical Pharmacy CH 1 Hospital Pharmacy Notesmaharachandana18No ratings yet
- Grammar ConjunctionsDocument7 pagesGrammar ConjunctionsK PrasadNo ratings yet
- Paediatric RadiographyDocument75 pagesPaediatric RadiographyTapshi SohalNo ratings yet
- Antibiotic Stewardship 508Document34 pagesAntibiotic Stewardship 508Adel AdelNo ratings yet
- Adv2022-0035 Guidelines On Accreditation Renewal For CY 2023Document1 pageAdv2022-0035 Guidelines On Accreditation Renewal For CY 2023Renso De LeonNo ratings yet
- Underwriting PacketDocument9 pagesUnderwriting Packetapi-207980596No ratings yet
- The Hound of BaskervillesDocument128 pagesThe Hound of BaskervillesMljnNo ratings yet
- NPI NCMH StephDocument12 pagesNPI NCMH StephAnonymous 2fUBWme6wNo ratings yet