Professional Documents
Culture Documents
Oph Ocular Toxoplasmosis DR Michael Wertheim June10
Uploaded by
Yekiko FiraldiOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Oph Ocular Toxoplasmosis DR Michael Wertheim June10
Uploaded by
Yekiko FiraldiCopyright:
Available Formats
U
P D A T E
C L I N I C A L
Ocular toxoplasmosis
By Dr Michael Wertheim, Ophthalmologist. Tel 9312 6033
cular toxoplasmosis should be considered in all patients who present with posterior ocular symptoms, especially immunocompromised patients. The Toxoplasma gondii (T. gondii) parasite has a complex lifecycle; the cat is the definitive host and intermediate hosts include pigs and sheep; humans most commonly contract the disease by ingesting uncooked meat containing tissue cysts. may not be associated with a pigmented scar (Figure 2).
n Fig 1.
Vertical transmission occurs when a pregnant woman contracts a primary infection and passes it on transplacentally. Congenital disease tends to be more severe if acquired in the first trimester but transmission rates are highest in the third trimester. Congenital disease manifests in many ways, from spontaneous abortion to asymptomatic infants that present later in life with ocular scarring or reactivation.
Making the diagnosis
Symptoms may be non-specific and include the onset of new floaters, flashing lights, decreased visual acuity, ocular pain and redness. Ophthalmic examination is often all that is needed to make the diagnosis.
Recognising atypical forms of the disease can be challenging yet definitive diagnosis is essential before starting treatment. The best way to make the diagnosis is by isolating T. gondii PCR from ocular fluid; by an anterior chamber tap or a vitreous biopsy. Blood levels of T.gondii IgM antibodies may help; levels rise during acute acquired toxoplasmosis and typically remain positive for less than a year. (IgG antibodies remain positive for life but are non-specific because a high proportion of the population has a positive IgG for non-ocular infections).
n Fig 2.
near the optic neve, and perhaps associated with an extensive vitritis or very decreased vision.
The appearance of unilateral active retinal toxoplasmosis is classic (Figure 1). Re-activated lesions have a pigmented area (old scar) associated with an adjacent fluffy white lesion (active lesion). There is usually a single lesion evident. In immunocompromised patients, ocular signs are non-specific and may be confused with other retinal inflammation or infection; multiple lesions may be bilateral and may or
Treatment
This is determined mainly by the immune status of the patient and location of the lesion in the retina. All immunocompromised patients need treatment. In immunocompetent patients, the disease is usually self-limiting and, if not sightthreatening, can be closely monitored in clinic. However, all sight-threatening lesions need treatment; lesions within the temporal arcades,
This clinical update is supported by the Eye Surgery Foundation
A 2002 survey of 78 American Uveitis Society specialists revealed 24 different regimens using 9 different parasitic drugs. Only 17% used an oral corticosteroid when treating all cases of ocular toxoplasmosis in immunocompetent patients while others used corticosteroid only for specific indications. So agreement on the ideal treatment is debatable and contentious. The most common drugs used are a combination of pyramenthamine, sulphadiazine, clindamycin and prednisolone. Currently, an effective treatment is a course of azithromycin alone, with or without prednisolone.
You might also like
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Nervous System, NotesDocument6 pagesThe Nervous System, NotesnadshinkNo ratings yet
- Bandhas and MudrasDocument6 pagesBandhas and MudrasMohammed RashidNo ratings yet
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- 7chakra QualitiesDocument8 pages7chakra Qualitiesserby108No ratings yet
- Pediatrics MCQs - DR Ranjan Singh - Part 1Document10 pagesPediatrics MCQs - DR Ranjan Singh - Part 1k sagarNo ratings yet
- Overview Congenital Musculoskeletal DisorderDocument84 pagesOverview Congenital Musculoskeletal DisorderRyan Trian100% (3)
- Ba Duan JinDocument58 pagesBa Duan JinpositivamenteNo ratings yet
- Administering EnemaDocument35 pagesAdministering Enemabajaoc100% (1)
- Goat Housing and Fencing PDFDocument43 pagesGoat Housing and Fencing PDFmary anthoneth bayle100% (1)
- Adoptive Immunotherapy Ludewig Hoffmann (Methods Molec Medicine 109 Humana 2005)Document517 pagesAdoptive Immunotherapy Ludewig Hoffmann (Methods Molec Medicine 109 Humana 2005)Cristian PopaNo ratings yet
- Equine Dental BrochureDocument2 pagesEquine Dental BrochurevetthamilNo ratings yet
- Subcutaneous Infections and True PathogensDocument2 pagesSubcutaneous Infections and True PathogensthescarletpimpernelsNo ratings yet
- Leadfinger GoblinDocument1 pageLeadfinger GoblinBrianNo ratings yet
- 2.manajemen Gawat Nafas Pada Bayi Dan Anak - DrlizaDocument89 pages2.manajemen Gawat Nafas Pada Bayi Dan Anak - DrlizayuniayuNo ratings yet
- SD - Cauda Equina InglesDocument20 pagesSD - Cauda Equina InglesRodriguezNo ratings yet
- Autonomic NsDocument32 pagesAutonomic NsErmias TewoldeNo ratings yet
- Spoof TextDocument9 pagesSpoof TextHeather LeeNo ratings yet
- Anatomy & Physiology: Third EditionDocument74 pagesAnatomy & Physiology: Third EditionTimothy HattoxNo ratings yet
- 15-10-2019, Mr. Jamal, 50 Yo, V.Laceratum Cruris Dextra + Skin Loss + Fraktur Os Fibula, Dr. Moh. Rizal Alizi, M.Kes, Sp. OT-1Document15 pages15-10-2019, Mr. Jamal, 50 Yo, V.Laceratum Cruris Dextra + Skin Loss + Fraktur Os Fibula, Dr. Moh. Rizal Alizi, M.Kes, Sp. OT-1anon_893244902No ratings yet
- Clinical Study: Overjet and Overbite Influence On Cyclic Masticatory Movements: A CT StudyDocument7 pagesClinical Study: Overjet and Overbite Influence On Cyclic Masticatory Movements: A CT Studyarya091193No ratings yet
- CurosurDocument2 pagesCurosuredNo ratings yet
- Health Assessment Form For LearnersDocument2 pagesHealth Assessment Form For LearnersIvy Jessa CandilanzaNo ratings yet
- Diagnosis Dengue Melalui Deteksi Antibodi Imunoglobulin G Spesifik Dalam Sampel Urine Dengan Teknik ELISADocument8 pagesDiagnosis Dengue Melalui Deteksi Antibodi Imunoglobulin G Spesifik Dalam Sampel Urine Dengan Teknik ELISANOVI WULANDARINo ratings yet
- Cory Ne BacteriumDocument25 pagesCory Ne BacteriumSona SandiNo ratings yet
- Efficacy of The Herbal Formulation Av/Epp/14 Against Ectoparasites On PetsDocument3 pagesEfficacy of The Herbal Formulation Av/Epp/14 Against Ectoparasites On PetsAmit Kumar PandeyNo ratings yet
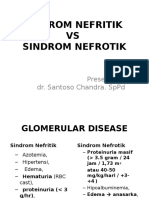
- Sindroma Nefrotik Vs NefritikDocument23 pagesSindroma Nefrotik Vs NefritikihsanNo ratings yet
- Ivtherapybyaakashgupta 170201102953 PDFDocument100 pagesIvtherapybyaakashgupta 170201102953 PDFvvb_frndNo ratings yet
- Neck TrianglesDocument6 pagesNeck TrianglesJay-arh SebusaNo ratings yet
- ArenavirusDocument29 pagesArenavirusRamirez GiovarNo ratings yet
- Anti-Fungal: Tinea Flava, Ringworm, Athlete's Foot and ScabiesDocument2 pagesAnti-Fungal: Tinea Flava, Ringworm, Athlete's Foot and ScabiesShairuz Caesar Briones DugayNo ratings yet