Professional Documents
Culture Documents
A New Device For Absolute Anchorage
Uploaded by
imtiyazorthodontistOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
A New Device For Absolute Anchorage
Uploaded by
imtiyazorthodontistCopyright:
Available Formats
ORIGINAL ARTICLES
A new device for absolute anchorage for orthodontics
Michael S. Block, DMD," and David R. Hoffman, DDS b New Orleans, La. A new device has been designed to provide anchorage for orthodontic tooth movement. It is a disk, textured and hydroxylapatite coated on one side, with an internal thread on the other side. It is placed on palatal bone and, after integration, can be connected to teeth for anchorage. This article reviews a dog study demonstrating unilateral tooth movement towards the "onplant" and a monkey study mimicking its use to anchor the molars for anterior retraction. (AM J ORTHOD DENTOFAC ORTHOP 1995; 107:251-8.)
In the late 1970s and 1980s several authors 1-19 thoroughly tested, in animals, the concept of using osseointegrated implants in orthodontic treatment. The implants remained stable when subjected to significant forces for long periods of time. Teeth were moved, palates were widened, and entire maxillae were were protracted 5 to 16 m m with implants as anchorage devices. Histologic sections of the bone implant interface demonstrated a stable nonreactive environment surrounding the implant. The lack of inflammatory or osteoclast cells confirmed the ability of the implant to resist reciprocal m o v e m e n t during orthodontic treatment. In 1989 we designed a thin titanium alloy (6A14V) disk (onplant), textured and coated with hydroxylapatite (HA) on one surface and a threaded hole on the opposite side to be inserted subperiosteally with the H A - c o a t e d side against bone for biointegration. This report describes the use of the onplant as absolute anchorage for orthodontic movements. Since it does not have to be inserted into bone, it can be placed in patients in various states of dental eruption avoiding the unerupted and erupted teeth. The following studies demonstrate the effectiveness of this device and concept in dogs and monkeys.
MATERIALS AND METHODS Onplant device
alloy with an internal threaded hole at its center into which abutments can be placed. The initial onplants were a thin (2 mm thick x 10 mm diameter) disk with a sharp 90 angle at the periphery. This design was modified to a more tapered shape because of the soft tissue dehiscence caused by the sharp edge (Fig. 1).
Canine study
The surface of the onplant that lies against bone is textured and coated with a 75 ~xm thick layer of hydroxylapatite. The surface facing soft tissue is smooth titanium
From the Louisiana State University. ~Associate Professor, Department of Oral and Maxillofacial Surgery. hFormer Clinical Associate Professor, Department of Orthodontics; in private practice in Metairie, La. Copyright 1995 by the American Association of Orthodontists. 0889-5406/95/$3.00 + 0 8/1/48051
The purpose of the dog study was aimed at determining the ability of the onplant, once biointegrated to bone, to remain stable when subjected to orthodontic forces. Four mongrel dogs were used. General anesthesia was induced with an intravenous pentobarbital. After injection of approximately 2 cc of 2% xylocaine with 1 : 100,000 epinephrine, a full thickness mucoperiosteal incision was made in the anterior region of the palate, followed by formation of two subperiosteal tunnels reaching the first molars. Tunneling was used to place the incision away from the onplant. In each dog two onplants were placed onto the palate. The tunnels were conservatively formed to prcvcnt migration of the onplants after they were placed into the desired position. In addition, one onplant was placed over the lateral ramus for mechanical testing in two dogs. After 10 weeks, which were allowed for healing, one of the onplants was exposed by removing a circular patch of palatal tissue directly over the onplant. The healing screw was removed, and a ball-shaped abutment was placed into the internally threaded hole within the onplant. A hole was then created through the maxillary first premolar on the contralateral side of the maxilla. A spring was placed and attached to the ball abutment (Fig. 2). Impressions were taken before placement and after exposure of the onplant for future measurement of the tooth and onplant position. The spring was activated between the tooth and the abutment to exert 11 ounces of force. The springs were checked weekly and reactivated when needed. Impressions were taken every month to compare the initial position of the tooth and subsequent positions. All the dogs were killed after 5 months. The maxillae were retrieved intact and fixed in 10% neutral buffered formalin. After 10 days of fixation, the onplants were
251
252
Block and Hoffrnan
American Journal of Orthodontics and Dentofacial Orthopedics March 1995
Leitz Wetzlar, GMBH, Germany), then stained with Alizarin red.
Monkey study
The purpose of the monkey study was to stimulate an intended use of the onplant to stabilize molars during retraction of the anterior dentition to mimic a situation commonly encountered in clinical orthodontics. Five monkeys were used in the study. One monkey served as a control, and the remaining four had one onplant placed in the middle of the palate opposite the maxillary second molar. The onplant was placed through an incision made anteriorly to prevent placing the incision directly over the onplant. Two onplants had sharp 90 peripheral edges and two had tapered edges. After 12 weeks for healing, the onplants were exposed and the abutments placed. Two of the monkeys had prosthetic abutments inserted into the onplants that were transferred to a model for fabrication of a cast gold transpalatal bar. It was screwed into the abutment in the onplant and soldered to orthodontic bands to the first molar on one side and the second molar on the other side (Fig. 3). The other two monkeys had an abutment placed with a small groove that allowed engagement of a transpalatal wire. A 0.051inch wire was bent to engage the grooved abutment and was soldered to previously adapted orthodontic bands (Fig. 4). The fifth monkey had a palatal bar made from 0.051-inch wire soldered to the molar teeth only (Fig, 5). At the time of onplant placement, the monkeys' first and second maxillary premolars were extracted bilaterally, creating space between the maxillary first molars and the canines. The bar or wire was connected to the first molar on one side and the second molar on the opposite side. Therefore one first molar was "anchored" to the onplant through the bar or wire and the eontralateral first molar was not anchored. Bilateral stainless steel springs were stretched from the canines to the first molars. They exerted a 250 gm reciprocal force between the first molars and the canines. The springs were calibrated weekly to keep the forces as constant as possible. Impressions were taken preoperatively and every 2 months until the conclusion of the study. The monkeys were killed after 6 months. At that time, two of the onplants were removed without difficulty with an osteotome to examine the underlying bone. The remaining three monkeys had the onplants left in place for direct examination after defleshing. The heads of the five monkeys were defleshed to study the movements of the teeth and underlying bone of the maxilla.
Fig. 1. A, Superior smooth surface of onplant with internal thread for placement of transgingival abutment. B, Textured, HA coated surface of onplant that is placed against bone for biointegration. C, Diagram of onplant and abutment. This abutment shown is designed to receive 0.051-inch wire.
RESULTS Canine study
I n o n e of t h e four dogs a large soft tissue d e h i s c e n c e d e v e l o p e d over t h e s h a r p e d g e of the o n p l a n t in which an infection r e s u l t e d . T h i s onp l a n t did n o t i n t e g r a t e . T h e o n p l a n t s o f t h e rem a i n i n g t h r e e dogs i n t e g r a t e d a n d w e r e activated.
carefully resected with accompanying bone and processed for histologic evaluation. The tissue blocks were embedded in plastic and 30 ixm thick sections cut with a Leitz microtome (Ernest
American Journal of Orthodontics and Dentofacial Orthopedics Volume 107, No. 3
Block and H o f f m a n
253
Fig. 2. A, Onplant has been exposed and connected to contralateral second premolar with stainless steel spring activated to deliver 11 ounces of force. Note nonactivated spring to show amount of activation. B, Five months later, second premolar has been moved toward onplant. This tooth moved 8 mm from its original position, without movement of onplant.
Fig. 3. A, Cast bar has been fabricated in laboratory and secured to onplant with screw, and soldered to bands cemented to molar teeth. First molar on one side is anchored by onplant and first molar on opposite side is not anchored. B, Six months later, one can see anchored tooth has not moved. Nonanchored first molar has moved to canine.
According to the measurements of study models of the maxilla, the onplants did not move in relation to the incisors or the molars. However, the premolar attached to the onplant moved toward the onplant in each animal. At the conclusion of the study, one tooth moved 4 mm and the other two teeth had moved 8 mm (Fig. 2, B). The soft tissue
around the onplant was normal in appearance, with slight inflammation consistent with plaque accumulation. Histologic examination of the loaded and unloaded onplants revealed no significant differences between the loaded and unloaded control onplants. In all instances, bone was found directly apposed to
254 Block and Hoffman
American Journal of Orthodontics and Dentofacial Orthopedics March 1995
Fig. 4. A, After exposure of onplant, impression was taken and 0.051-inch wire bent to engage abutment and was also soldered to bands. Then bands were cemented to teeth and springs placed from anchored first molar to canine, and nonanchored first molar to canine. B, Six months later, one sees how 0.051 -inch wire combined with anchorage from wire engaging abutment provided anchorage with less anterior migration of molar.
Fig. 5. A, Control monkey had transpalatal wire soldered to bands similar to animals in Fig. 4. Here first molar on one side is anchored and first molar on opposite side is not anchored by transpalatal wire. B, After 6 months one sees anchored and nonanchored molars moved similarly, without evidence of anchorage reinforcement by transpa!atal wire alone.
the H A coating. In some regions, dense bone was found connecting the palatal bone to the onplant. However, in most regions, trabecular-type bone was found traversing the gap between the underlying palatal bone and the onplant. The coating was intact, without evidence of resorption. Macrophages and osteoclasts were not seen. The cellular response was benign without the presence of inflammatory cells (Fig. 6). The two onplants placed over the ramus were retrieved with their accompanying mandibles and placed into a sterile saline solution. Within 2 weeks, the mandibles were mounted in a Mechanical Testing System 810 (MTS Systems Corp., Eden Prairie, Minn.), and the shear force measured to dislodge the onplants from the underlying mandible. The push off force was 160 and 162 pounds for the two specimens. Examination of the inter-
face after push off revealed separation between the bone over the H A coating and the underlying bone and also between the H A coating and the substrate metal, which was similar to the results of removing the two onplants from the monkeys.
Monkey study
The soft tissue response was different between the sharp and the tapered edge onplants. There was a small soft tissue dehiscence over the two sharp edge onplants but no soft tissue dehiscence over the tapered edge onplants (Fig. 7). All onplants integrated. The anchored molars moved an average of 1 . 2 _ 0.2 mm toward the central incisors. The nonanchored molars moved an average of 4.1 z 1.4 mm toward the central incisors (p < 0.01). The canines on the anchored side moved an average of 1.9 ___ 0.6 mm away from the central incisors, and the canines on the nonanchored side moved an
American Journal of Orthodontics and Dentofacial Orthopedics Volume 107, No. 3
Block and Hoffrnan
255
Fig. 7. This photograph shows soft tissue response after 5 months of loading. Cast gold bar has been removed, allowing direct inspection of healthy palatal tissue around transgingiva[ abutment.
DISCUSSION
Fig. 6. A, 1 : 1 photograph of undecalcified section of onplant with bali attachment demonstrating intimate relationship between textured HA-coated surface of onplant and underlying palatal bone. B, Palatal bone was able to form bone onto textured HA-coated surface. This specimen is 5-month loaded onplant, demonstrating healthy viable bone anchoring device to palate. (Magnification x40, Alizarin red, undecalcified .)
average of 1.9 _+ 0.7 mm away from the central incisors (p > 0.01). As can be seen in Table I, the anchorage was slightly better by using a cast gold bar than with the 0.051-inch wire. Apparently, the wire had space present after cementation of the bands that resulted in small compensatory movements and perhaps a small amount of rotation around the wire. When the animals were killed, an incision was made and the palatal tissue stripped from the onplant revealing the bone onplant interface. When the onplant was placed close to the vertical shelf of the palate, the bone extended over the edge onto the superior surface of the onplant (Fig. 8). When the onplant was gently removed from the bone with an osteotome, the palatal bone under the onplant revealed a textured surface mirroring the textured surface of the onplant (Fig. 9).
The term anchorage is used in orthodontic treatment to describe the resistive value of posterior teeth toward mesial movement. The term reciprocal anchorage implies that the posterior teeth will be allowed to move in accordance with Newtoffs Third Law of " . . . equal and opposite reaction." Maximum anchorage means that additional resistance has been added to the posterior teeth so they will not react to a reciprocal force. Typically, the additional resistance is applied in the form of an extraoral device such as headgear. A headgear delivered force of 12 to 18 ounces will stabilize a molar as long as the device is worn. The problem is that most orthodontic retractive forces are continuous, and the headgear is worn less than 12 hours a day.2 A headgear worn during periods of physical activity can be dangerous. 21 An even greater problem is achieving adequate levels of patient compliance. Grewe and Hermanson22 found little correlation between the severity of the malocclusion and the degree of patients' cooperation. Clemmer found that compliant patients had an internal locus of control, were high achievers, esthetically sensitive, and had a good attitude. 23 Egolt~4 assessed a large group of postorthodontically treated patients and reported that only 4% followed their orthodontist's instruction. An additional 22% complied most of the time. With 74% of the group complying less than half the time, orthodontists welcome treatment schemes that eliminate the need for patient cooperation. One such scheme, first tested nearly 50 years
256
Block and Hoffman
American Journal of Orthodontics and Dentofacial Orthopedics March 1995
Fig. 8. Palatal soft tissue was stripped in this animal after it was killed to inspect bone response to onplant. Here one sees bone modeling over top of onplant. Bone around onplant appeared healthy, which was expected on basis of dog studies.
Fi8. 9. Immediately after they were killed, two monkeys had their onplants removed with aid of osteotome. Note in this photograph textured pattern of bone on palate without loss of bone structure, mirroring surface of onplant.
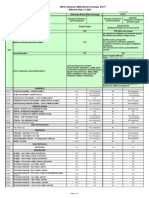
Table I. Tooth movement (mm) in monkey study
Nonanchored Group Number Mo&r Canme Molar Anchored Canine
Cast Bar 0.051-inch wire Combined Control
2 2 4 1
3.5 (0.8) 4.5 (2.1) 4.1 (1.4) 2.9
2.4 (0.7) 1.4 (0.3) 1.9 (0.7) 1.6
1.25 (0.35) 2.30 (1.8) 1.20 (0.2) 2.9
0.85 (0.5) 2.05 (1.1) 1.90 (0.6) 2.0
ago by Gainesforth and Higley, ~5 attempted to harness the stability of devices implanted into the mandible or the maxilla. This was in response to recognizing that compliance was the " . . . biggest problem facing orthodontics." Vitallium screws were inserted into a dog's ramus to secure a spring used to distallize a maxillary canine. All the screws failed in 16 to 31 days. Today we know that titanium is a better material, that good surgical technique is essential, and that adequate healing time must elapse for integration to occur. 26 In 1969 Linkow, 27 reported the use of mandibular blade-vent implants in a person to attach Class II elastics while retracting maxillary incisors. H e subsequently used the implants as bridge abutments to complete the patient's treatment. 28 Beginning with Roberts in 1988, z9'3 a series of authors reported the use of standard endosseous implants in the orthodontic treatment of human beings. 4'23'31-38 The implants were completely successful for providing absolute anchorage for tooth movements. However, since only edentulous areas are suitable for "root form" implants, the site
selection and frequency of opportunity were severely limited. The placement of implants into the ramus is a compromise since other alternatives did not previously exist. Adolescent patients have unerupted teeth preventing placement of an endosseous implant. If placed in a growing person exhibiting considerable vertical alveolar growth, the integrated endosseous implant would behave similar to an ankylosed tooth and become submerged. 39 This onplant device can be used to anchor teeth during orthodontics. The classic orthodontic philosophy that transpalatal bars by themselves serve as anchors is refuted in the control monkey. 4 However, the anchorage from the transpalatal bar and the 0.051inch wire when coupled to the onplant was significant. From a practical point of view, the cast bar is bulky and forces the orthodontist to detour from standard orthodontic practice. The orthodontist does not usually use cast devices. In addition, the use of a screw for retention of the cast bar creates a larger vertical profile of the transpalatal bar and thus would not be well tolerated by the patient.
American Journal of Orthodontics and Dentofacial Orthopedics Volume 107, No. 3
Block and Hoffman 257
T h e g r o o v e d a b u t m e n t for t h e h e a v y 0.051-inch wire allows t h e o r t h o d o n t i s t to use c o n v e n t i o n a l i m p r e s s i o n s picking u p t h e a b u t m e n t a n d t h e b a n d s o n t h e t e e t h to s o l d e r t h e w i r e to t h e b a n d s in a r o u t i n e m a n n e r . T h e n w h e n t h e b a n d s a r e cem e n t e d , t h e t r a n s p a l a t a l wire s h o u l d e n g a g e t h e a b u t m e n t easily. T h e t h i c k wire s h o u l d b e m o r e p r a c t i c a l a n d p r o v i d e lower profile t r a n s p a l a t a l b u l k t h a n t h e cast bar. T h e two a n i m a l s in this s t u d y d e m o n s t r a t e d c o n s i s t e n t a n c h o r a g e . W e recognize t h a t t h e small s a m p l e size p r e c l u d e s statistical verification, c o m p a r i n g a cast b a r with t h e thick wire. D e s p i t e t h e s e limitations, it is a c k n o w l e d g e d throughout the orthodontic community that there is a f u t u r e for i m p l a n t s in o r t h o d o n t i c t r e a t m e n t . A device n e e d e d to b e d e v e l o p e d which was n o t l i m i t e d to e d e n t u l o u s areas, was easy to insert, a n d easy to r e t r i e v e o n c e it was no l o n g e r n e e d e d . T h e a d d i t i o n a l cost o f t h e device w o u l d b e offset by r e d u c e d t r e a t m e n t times, m o r e p r e d i c t a b l e results, a n d less aggravation. CONCLUSIONS 1. T h e o n p l a n t is sufficiently a n c h o r e d to t h e u n d e r l y i n g b o n e to w i t h s t a n d 11 o u n c e s o f c o n t i n u o u s force. It is sufficiently a n c h o r e d by t h e H A - b o n e b i o i n t e g r a t e d i n t e r f a c e to resist u p to 160 p o u n d s of s h e a r force. 2. T h e o n p l a n t can p r o v i d e a b s o l u t e a n c h o r a g e to m o v e a t o o t h t o w a r d it w i t h o u t moving t h e onplant. 3. T h e o n p l a n t can p r o v i d e sufficient a n c h o r age to m o l a r s to p r e v e n t a n t e r i o r m i g r a t i o n w h e n in situations r e q u i r i n g m a x i m u m anchorage. A n e w device has b e e n c r e a t e d to p r o v i d e a n c h o r a g e to t e e t h d u r i n g o r t h o d o n t i c s . This device has b e e n s h o w n in a n i m a l s to p r o v i d e sufficient a n c h o r a g e to successfully m o v e a n d a n c h o r teeth. This o n p l a n t m a y have t h e p o t e n t i a l to largely r e p l a c e h e a d g e a r a n d p r o v i d e o r t h o d o n t i s t s with c o m p l e t e c o n t r o l of a n c h o r a g e r a t h e r t h a n relying on p a t i e n t c o m p l i a n c e . REFERENCES i. Creekmore TA, Eklund MK. The possibility of skeletal anchorage. J Clin Orthod 1983;17:266-9. 2. Gray JB, Steen ME, King CJ, Clark AF. Studies on the efficacy of implants as orthodontic anchorage. AM J ORTHOD 1983;83:311-7. 3. Helm FR, Poon LC, Marshall KJ, Gongloff RJ, Roberts WF.
Bone remodeling response to loading of rigid endosseous implants. J Dent Res 1987;66:186. 4. Kraut RA, Hammer HS, Wheeler JJ. Use of endosteal implants as orthodontic anchorage. Comp Contin Educ Dent 1988;9:796-801. 5. Lubberts R, Turley PK. Force application to bioglass coated alumina implants of various sizes. J Dent Res 1982;61A:339. 6. Mendez-Villamil C, Oliver S, Evans C, Schnittman P. Periodontometric evaluation of mobility changes in stressed vitreous carbon implants. J Dent Res 1980;59A:280. 7, Oliver S, Mendez-Villamil (2, Evans C, Schnitman P, Shulman L. Change in position of vitreous carbon implants subjected to orthodontic forces. J Dent Res 1980;59A:280. 8. Oliver S, Mendez-Villamil C, Heely J, Shulman L Orthodontic stresses and peri-implant alveolar bone in baboons. J Dent Res 1982;61A:281. 9. Paige S, Clark AE, Costa P, King G, Waldron J. Orthodontic stress application to bioglass implants in rabbit femurs. J Dent Res 1980;59A:445. 10. Roberts WE, Smith RK, Zilberman Y, Mozsary P, Smith R. Osseous adaptation to continuous loading of rigid endosseous implants. AM J ORTHOD 1984;86:95-111. 11. Roberts WE, Turley PK, Brezniak N, Fielder P. Bone physiology and metabolism. Calif Dent Assoc J 1987;15(10): 54-61. 12. Roberts WE. Bone tissue interface. J Dent Ed 1988;52(12): 804-9. 13. Sherman AJ. Bone reaction to orthodontic forces on vitreous carbon dental implants. AM J ORTHOD 1978;74:79-87. 14. Smith JR. Bone dynamics associated with the controlled loading of bioglass-coated aluminum oxide endosteal implants. AM J ORTHOD 1979;76:618-36. 15. Turley PK, Shapiro PA, Moffett BC. The loading of bioglass-coated aluminum oxide implants to produce sutural expansion of the maxillary complex in the pigtail monkey (Macaca nemestrina). Arch Oral Biol 1980;25(7):459-69. 16. Turley PK, Roth P. Orthodontic force application to vitallium subperiosteal implants. J Dent Res 1983;62A:681. 17. Turley PK, Gray DW, Kean LJ, Roberts WE, Titanium endosseous and vitallium subperiosteat implants as orthodontic anchors for tooth movement in dogs. J Dent Res 1984;63A:334. 18. Linder-Aronson S, Nordenram A, Anneroth G. Titanium implant anchorage in orthodontic treatment: an experimental investigation in monkeys. Eur J Orthod 1990;12:414-9. 19. Turley PK, Dean C, Schuar J, Stefanac J, Gray J, Hermes J, Poon LC. Orthodontic force application to titanium endosseous implants. Angle Orthod 1988;58:151-62. 20. McDonald FT. The influence of age on orthodontic patient cooperation. Dent Abst 1973;18:52. 21. Booth-Mason S, Birnie D. Penetrating eye injury from orthodontic headgear-A case report. Eur J Orthod 1988;10: 111-4. 22. Grewe JM, Hemanson PC. Influence of severity of malocclusion on the duration or orthodontic treatment. AM J
ORTHOD 1973;63:533-6,
23. Clemmer EJ, Hayes EW. Patient cooperation in wearing orthodontic headgear. AM J ORTHOD 1979;75:517-24. 24. Egolf RJ, BeGole EA, Upshaw HS. Factors associated with orthodontic patient compliance with intraoral elastic and headgear wear. AM J ORTHOD DENTOFAC ORTHOP 1990; 97:336-48. 25. Gainsforth BL, Higtey LB. A study of orthodontic anchor-
258
Block and Hoffman
American Journal of Orthodontics and Dentofacial Orthopedics March 1995
implants: a case report. Comp Contin Educ Dent 1990; 11(9):548-54. Odman J, Lekholm U, Jem T, Br~inemark E Thilander B. Osseointegrated titanium implants a new approach m orthodontic treatment. Eur J Orthod 1988:10:98-105. Van Roekel NB. The use of Br~inemark system implants for orthodontic anchorage: report of a case. Int J Oral Maxiliofac Implants 1989;4:341-4. Arbuckle GR, Nelson CL. Roberts WE. Osseointegrated implants and orthodontics. Oral Maxillofac Clin North Am 1991;3(4):903-19. Shapiro PA, Kokich VG. Uses of implants in orthodontics. Den Clin North Am 1988:32(3):539-49. Odman J, Gr6ndahl K, Lekholm U. Thilunder B. The effect of osseointegrated implants on the dento-alveolar development. A clinical and radiographic study in growing pigs. Eur J Orthod 1991;13:279-86. Stoner MM. Tooth movement. In: Graber TM. ed. Current orthodontic concepts and techniques. Philadelphia: WB Saunders, 1969:449-64.
26.
27. 28. 29.
30.
31. 32.
33.
34.
age possibilities in basal bone. AM J ORrHOD ORAL SURG 1945;31:406-17. Adell R, Lekholm U, Rockler B, Branemark P. A 15-year study of osseointegrated implants in the treatment of the edentulous jaw. Int J Oral Surg 1981;10:387-416. Linkow LI. The endosseous blade implant and its use in orthodontics. Int J Orthod 1969;18:149-54. Linkow LI. Implanto-orthodorltics. J Clin Orthod 1970;4: 685-705. Roberts WE, Marshall KJ, Mozsary PG. Rigid endosseous implant utilized as anchorage to protract molars and close and atrophic extraction site. Angle Orthod 1990;60(2):13552. Roberts WE, Helm RR, Marshall KJ, Gongloff RK. Rigid endosseous implants for orthodontic and orthopedic anchorage. Angle Orthod 1989;59(4):247-56. Douglass JB, Killiany DM. Dental implants used as orthodontic anchorage. J Oral Implantol 1987;13:28-38. Haanaes HR, Stenvik A, Beyer-Olson E, Tryti T, Faehn O. The efficacy of two-stage titanium implants as orthodontic anchorage in the preprosthodontic correction of third molars in a d u l t s - a report of three cases. Eur J Orthod 1991;13:287-92. Higuchi KW, Slack JM. The use of titanium fixtures for intraoral anchorage to facilitate orthodontic tooth movement. J Oral Maxillofac Implants 1992;6(3):338-44. Lanzi GL, Seran CC, Cohen SR. Prosthetic replacement of congenitally missing teeth using single-tooth osseointegrated
35.
36.
37.
38. 39.
40.
Reprint requests to. Dr. Michael S. Block Department of Oral and Maxillofacial Surgery L.S.U. School of Dentistry 1100 Florida Ave. New Orleans, LA 70119
AAO MEETING CALENDAR 1995 1996 1997 1998 1999 2000 San Francisco, Calif., May 12 to 17, Moscone Convention Center
(International Orthodontic Congress)
Denver, Colo., May 11 to 15, Colorado Convention Center Philadelphia, Pa., May 3 to 7, Philadelphia Convention Center Dallas, Texas, May 16 to 20, Dallas Convention Center San Diego, Calif., May 15 to 19, San Diego Convention Center Chicago, Ill., April 29 to May 3, McCormick Place Convention Center
You might also like
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- TADs in Orthodontics: Miniplates for Class III CorrectionDocument18 pagesTADs in Orthodontics: Miniplates for Class III CorrectionimtiyazorthodontistNo ratings yet
- Total Arch Distalization A ReviewDocument4 pagesTotal Arch Distalization A ReviewsmritiNo ratings yet
- Classification of Failure of FPDDocument4 pagesClassification of Failure of FPDrayavarapu sunilNo ratings yet
- Development of Teeth 1Document37 pagesDevelopment of Teeth 1Muli MaroshiNo ratings yet
- Herbst ApplianceDocument21 pagesHerbst Applianceimtiyazorthodontist83% (6)
- A Review of Attachments For Removable Partial Denture Design Part 2 90Document7 pagesA Review of Attachments For Removable Partial Denture Design Part 2 90alioossaNo ratings yet
- Pulp Therapy in ChildrenDocument4 pagesPulp Therapy in ChildrenshahinshamshiriNo ratings yet
- Applications of Orthodontic Mini-ImplantsDocument277 pagesApplications of Orthodontic Mini-ImplantsNicolas Homsi100% (1)
- Are Occulsion and Comprehensive Dentistry Really That ImportantDocument20 pagesAre Occulsion and Comprehensive Dentistry Really That ImportantAhmed HamzaNo ratings yet
- OrthodonticsDocument14 pagesOrthodonticsimtiyazorthodontistNo ratings yet
- Cephalometrics Manual KrothDocument124 pagesCephalometrics Manual Krothimtiyazorthodontist100% (3)
- Ceph Analysis LabDocument23 pagesCeph Analysis LabimtiyazorthodontistNo ratings yet
- KimDocument12 pagesKimIvanna H. A.No ratings yet
- K9 Ve Balista Spring Başarı OranlarıDocument8 pagesK9 Ve Balista Spring Başarı OranlarıRümeysa AydınNo ratings yet
- Occlusal Indices GuideDocument229 pagesOcclusal Indices GuideRajshekhar BanerjeeNo ratings yet
- 1Document11 pages1Gowri KannanNo ratings yet
- Basic Principles of Obturator Design For Partially Edentulous Patients. Part I: ClassificationDocument4 pagesBasic Principles of Obturator Design For Partially Edentulous Patients. Part I: ClassificationArun PrasadNo ratings yet
- Arch Expansion DR SaadDocument41 pagesArch Expansion DR Saadahmed saad100% (1)
- Orthodontist's Perceptions of Smile EstheticsA Questionnaire Based StudyDocument5 pagesOrthodontist's Perceptions of Smile EstheticsA Questionnaire Based StudyInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Biomechanics of the Edentulous StateDocument30 pagesBiomechanics of the Edentulous StateAishwarya SharmaNo ratings yet
- Interrelationship Between Periodontics and Restorative DentistryDocument19 pagesInterrelationship Between Periodontics and Restorative DentistrySuperna TiwariNo ratings yet
- New Clasp Assembly For Distal Extension Removable Partial DenturesDocument17 pagesNew Clasp Assembly For Distal Extension Removable Partial DenturesAli FaridiNo ratings yet
- Biological Considerations in Operative DentistryDocument8 pagesBiological Considerations in Operative Dentistrysheryl teoNo ratings yet
- Jurnal Ilmu Konservasi Gigi: PSA Pada Supernumery RootDocument6 pagesJurnal Ilmu Konservasi Gigi: PSA Pada Supernumery RootAchmad Zam Zam AghazyNo ratings yet
- Historia Diente Ro 01-Cecilia-BacaliDocument5 pagesHistoria Diente Ro 01-Cecilia-BacaliAARON DIAZ RONQUILLONo ratings yet
- PDF PreviewDocument5 pagesPDF PreviewCatalin MNo ratings yet
- Digitally Enhanced Esthetic DentistryDocument3 pagesDigitally Enhanced Esthetic DentistrySMART SMARNo ratings yet
- Maxillary Permanent Central IncisorsDocument68 pagesMaxillary Permanent Central IncisorsAmit Singh100% (1)
- Placa de Acetato BioartDocument5 pagesPlaca de Acetato BioartlenzajrNo ratings yet
- Essential Lines DR ChioderaDocument7 pagesEssential Lines DR ChioderaajiargoputroNo ratings yet
- Periodontal Diseases in Children PedoDocument34 pagesPeriodontal Diseases in Children Pedoarpita7dr9693No ratings yet
- MCS Classicare (MA) Dental Coverage SummaryDocument4 pagesMCS Classicare (MA) Dental Coverage SummaryJessicaNo ratings yet
- Custom Post and Core Case ReportDocument10 pagesCustom Post and Core Case ReportDrAditya BansalNo ratings yet
- Spark Erosion Step by Step GuideDocument4 pagesSpark Erosion Step by Step GuideDentist HereNo ratings yet
- 01 - Introduction To DentistryDocument18 pages01 - Introduction To Dentistrymichal ben meronNo ratings yet
- Intraoral Radiographic Techniques ǁ: by Dr. WajnaaDocument32 pagesIntraoral Radiographic Techniques ǁ: by Dr. WajnaaALI abd-alamamNo ratings yet
- Periodontal Mechanoreceptors Stimulated Study of Human Masseter ReflexDocument6 pagesPeriodontal Mechanoreceptors Stimulated Study of Human Masseter ReflexRakesh KumarNo ratings yet