Professional Documents
Culture Documents
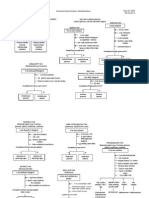
Sensations and Sensory Pathways General Senses Test Procedure Normal Result Abnormal Result Clinical Interpretation
Uploaded by
Abby MataOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Sensations and Sensory Pathways General Senses Test Procedure Normal Result Abnormal Result Clinical Interpretation
Uploaded by
Abby MataCopyright:
Available Formats
Sensations and Sensory Pathways General Senses Test Distribution of Sensory Receptors Procedure Use 9 (5x5mm) small squares
of graphing paper with a hole and place them in the volar surface of the forearm and the back or nape (avoid hairy portion) with the subject blindfolded. Test 5 spots on each square using fine bristle/horse hair, heated pin head, cooled pin head and pin or fine needle Normal Result Distribution of sensations: (Most) Pain result to stimulation of nociceptors(pain receptors) - Fast pain(occurs very rapidly usually within 0.1 second after stimuli is applied, because the nerve impulses propagate along medium-diameter, myelinated A fibers) Light Touch result from stimulation of tactile receptors in skin or subcutaneous layer (mechanoreceptors). - Meissner corpuscles (hairless skin); Hair roor plexuses (hairy skin) Cold result to stimulation thermoreceptors - Cold receptors located in the stratum basale and are attached to medium-diameter, myelinated A fibers. - Activation of receptors occur at 10-40C. Warmth result to stimulation of thermocreceptors - Not as abundant as cold receptors. - Activation of receptors occurs at 32-48C. (Least) At temperatures below 10C and above 48C, pain receptors are stimulated. Left index finger, from ice water, felt hot when placed in tap water; right index finger, from warm water, felt cold Abnormal Result Different distribution of sensations Hypalgesia decreased pain Analgesia absence of pain Hyperalgesia increased pain Hyperthesia decreased touch sensation Anesthesia absent touch Hyperesthesia increased touch sensation Clinical Interpretation Damage to posterior columnmedical leminiscal pathway, specifically the cuneeate fasciculus tract ( conveys nerve impulses for touch, pressure, vibration and conscious proprioception from upper limbs, trunk, neck, posterior head to the cerebral cortex) Damage to anterolateral or spinothalamic pathway (conveys nerve impulses for pain, cold, warmth, itch and tickle from limbs, trunk, neck, and posterior head to the cerebral cortex) Lesion in primary somatosensory area of cerebral cortex (receives nerve impulses for touch, pressure, vibration, itch, tickle, temperature (coldness and warmth), pain and proprioception)
Contrast
a. Fill three beakers with water: 1. B1: warm water (35OC) 2. B2: room temperature
No difference felt between left and right index fingers
Damage to posterior columnmedical leminiscal pathway, specifically the cuneate fasciculus
3. B3: ice water ~0 C b. Place left finger in beaker 3 and right index finger in beaker 1. ~20 seconds, place both fingers simultaneously in beaker 2. Compare the sensations during immersion in beaker 2.
when placed in tap water Successive contrast hot sensation to cold sensation Simultaneous contrast hot and cold sensations are felt at the same time Temperature sensations are not absolute but relative to the baseline previously established by sensory adaption.
tract Damage to anterolateral or spinothalmic pathway Lesion in primary somatosensory area of cerebral cortex.
Summation
Starting from the fingertips up to the wrist gradually immerses one hand in a basin full of war water for 10 seconds.
Extend of Immersion Fingers warm Palm warmer Wrist - warmest
No difference felt in extent of immersion.
Adaptation
Using the same basin the Summation test, immerse the whole hand for 5 minutes Have the subject blindfolded and place a piece of cork on the forearm for a minute or two. Observe,
Intensity of the sensation weakens.
Intensity of sensation remains the same. The sensation of touch or pressure continues to be unaltered.
Damage to posterior medial leminiscal pathway specifically the cuneate fasciculus tract Damage to anterolateral or spinothalmic pathway Lesion in primary somatosensory area of cerebral cortex Damage to anterolateral or spinothalamic pathway Lesion in primary somatosensory area of cerebral cortex.
The sensation of touch of pressure weakens at the end of the second minute. Adaptation characteristic of most sensory receptors - Generator or receptor potential decreases in amplitude during a maintained, constant stimulus. - Causes frequency of nerve impulses in the first order neuron to decrease The subject is able to detect two distinguishable blunt points. Approximate values for this two-point discrimination test :
Two-Point Discrimination
Blindfold the subject. Determine the threshold using two pins on the fintertip, nape, back of hand and tip of tongue. A. Set two points of pins together then
One or none of the two points is felt by the subject
Damage to anterolateral or spinothalamic pathway. Damage to trigeminothalmic pathway (conveys nerve impulses
increase 2 mm at a time until the pints can be discriminated as two. Points should be applied gently, simultaneously and with equal pressure. B. Repeat procedure, but the two points should be above threshold value and should be worked backwards until the two points are felt as one
Aristotles Experiment
Blindfold the subject. Place a small round object between ends of the crossed (middle finger over right index finger) and uncrossed fingers. Let the subject roll the object on the table
Fingers 2-3mm Upper lip 4-5mm Cheek 6mm Nose 7mm Palm 10mm Forehead 35mm Foot 20mm Belly 30mm Forearm 35mm Upper arm 39mm Shoulder 41mm Thigh 42mm Calf 45mm The subject is able to perceive two objects when fingers are crossed. Perceptual Disjunction the brain has failed to take into account that the subject has crossed his/her fingers. - Because the object touches the outside of both fingers at the same time, the brain interprets it as two separate objects. Diplesthesia tactile diplopia - In touch, the illusory experience of two objects when only one is actually present. The subject is able to recognize and differentiate objects even when blindfolded.
for touch, pressure, vibration, pain, cold, warmth and tickle from the face, nasal cavity, oral cavity and teeth). Lesion in primary somatosensory area of cerebral cortex.
The subject is able to perceive only one object
Possible prior cognitive bias.
Stereognosis tests the individuals ability to perceive and integrate a variety of sensory modalities and to interpret the stimuli to identify small objects placed in the hand.) Vibration sense Vibration results from rapidly repetitive sensory signals from tactile receptors
Blindfold the subject. Prepare three objects that the subject needs to identify while blindfolded. Objects are given one at a time in the subjects hand and ask him to identify it. Record the results.
The subject is not able to distinguish objects (Astereognosis)
-Astereognosis of the abnormal hand -Lesion in the somatosensory area of the cerebrum
i. Place the base of a vibrating tuning fork against various bony prominences - the malleoli, patella and styloid processes. Time the duration the vibration can be felt.
-The subject is able to feel the normal vibrating sensations -patient is able to detect when vibration ceases
-not able to detect and feel the vibration
-damage to posterior columnmedial leminiscal pathway -lesion in primary somatosensory area of cerebral cortex for early detection of
Meissner corpuscles (touch) - rapidly adapting - detect lower frequency vibrations -fingertips, hands, eyelids, tip of tongue, lips, nipples, soles, clitoris, tip of penis Pacinian corpuscles (pressure) -rapidly adapting -detect high-frequency vibrations -dermis, hypodermis, submucosal tissue, joints, tendons, muscles, periosteum, mammary glands, external genitalia, pancreas, urinary bladder Muscle and Joint Senses Kinesthesia -sense that detects bodily position, weight, or movement of the muscles, tendons, and joints
ii. Repeat (i) on various muscular regions biceps, triceps, and gastrocnemius
Pallesthesia - ability of body to feel mechanical vibrations on or near the body
demyelinating disease and peripheral neuropathy (damage in peripheral nerves)
i. Blindfold the subject. Place the subjects arms at a certain position and measure the angle made by the arm from the trunk ii. The arm is then dropped to the side and subject is asked to try and duplicate the previously measured position. Measure the angle formed by the arm from the trunk. iii. Record the difference between the two angles measured. This is the angle of error of the subject iv. Repeat the procedure for 5 different angles
Angle difference between blindfolded and not is small
angle difference is large
-low/ no muscle memory -damage to cerebellum -lesion in primary motor area (lesion of parietal cortex or thalamocortical projections to the parietal lobe)
Static Position Sense
i. Ask 3 different subjects to balance themselves on one leg with eyes open. Observe any moments and record the time they are able to keep their balance ii. Ask the subjects to balance themselves on one leg with eyes closed. Observe any movements and record the time they are able to keep their balance iii. With eyes closed, and balanced on one leg, ask the subjects to bend the head to the left side. Observe and record what happens. iv. Repeat (iii) but this time, ask the subjects to bend the head to the right side. Observe what happens.
able to keep balance and posture is correct
excessive postural swaying or loss of balance
-present when eyes are opened or closed = cerebellar deficit or ataxia -present when eyes are closed =proprioceptive deficit Ataxia condition in which the cerebellum Is damaged through the trauma or disease thereby disrupting muscle coordination -Lesion in the primary motor area of cerebral cortex
Gait
i. Draw a straight line on the floor. ii. Let the subject walk on the line, heel to toe, with 1. Eyes open 2. Eyes closed iii. Observe and record what happens
normal walking patterns (can walk heelto-toe in a straight line)
swaying, pattern not in line, steps too far from each other
-myopathic and neuropathic disorders -damage to the cerebellum (ataxia) -lesion in primary motor area of cerebral cortex
You might also like
- Eye HistologyDocument9 pagesEye HistologyGrace Shan BernusNo ratings yet
- (Practical Exam) Physiology Lab Materials For PracsDocument6 pages(Practical Exam) Physiology Lab Materials For PracsKeesha RiveraNo ratings yet
- 2013 - Lower Limb-Fascial Compartments of Thigh - Student VersionDocument28 pages2013 - Lower Limb-Fascial Compartments of Thigh - Student Versionmarina_shawkyNo ratings yet
- Histology of Ear and EyeDocument2 pagesHistology of Ear and EyeAnny Alvrz100% (1)
- Anatomy of Labyrinth by DR Inam Ur RehmanDocument29 pagesAnatomy of Labyrinth by DR Inam Ur RehmanasssadulllahNo ratings yet
- All Histology Semester 2 QuizzesDocument21 pagesAll Histology Semester 2 QuizzesBarwdi ZenNo ratings yet
- Cubital Fossa PDFDocument18 pagesCubital Fossa PDFKyle TongolNo ratings yet
- (Practical Exam) Physiology Lab Practical Cheat ShitDocument11 pages(Practical Exam) Physiology Lab Practical Cheat ShitKeesha RiveraNo ratings yet
- (ANA) 4.01 Abdomen in General - Dr. ElevazoDocument22 pages(ANA) 4.01 Abdomen in General - Dr. ElevazopasambalyrradjohndarNo ratings yet
- 12-Radial & Ulnar NervesDocument14 pages12-Radial & Ulnar NervesHafizah HoshniNo ratings yet
- Anatomy - Pectoral Region and Axilla PDFDocument4 pagesAnatomy - Pectoral Region and Axilla PDFAngel KimNo ratings yet
- 1 Ana Intro Finals September 16 LaygoDocument3 pages1 Ana Intro Finals September 16 LaygombdelenaNo ratings yet
- The Cockroach (Periplaneta Americana, L.): An Introduction to Entomology for Students of Science and MedicineFrom EverandThe Cockroach (Periplaneta Americana, L.): An Introduction to Entomology for Students of Science and MedicineRating: 4.5 out of 5 stars4.5/5 (2)
- Upper Extremity (Anatomy)Document17 pagesUpper Extremity (Anatomy)Margareth Christine CusoNo ratings yet
- Carpal Tunnel SyndromeDocument22 pagesCarpal Tunnel SyndromeAbu 'Ibby' IbrahimNo ratings yet
- Upper Limbs NOTES - BRS Anatomy, Table of Muscles and BRS Questions With Answers ExplainedDocument14 pagesUpper Limbs NOTES - BRS Anatomy, Table of Muscles and BRS Questions With Answers ExplainedJustyna PoznanskaNo ratings yet
- A Physio Midterm SGDDocument7 pagesA Physio Midterm SGDMaryNo ratings yet
- C - VVV VV VVVV VVV - VVV VV - VVVV VV VVDocument3 pagesC - VVV VV VVVV VVV - VVV VV - VVVV VV VVBea Angela Bithao AnonoyNo ratings yet
- Advances in Pathobiology and Management of Paget’s Disease of BoneFrom EverandAdvances in Pathobiology and Management of Paget’s Disease of BoneSakamuri V. ReddyNo ratings yet
- MOCK QUIZ - Head & Neck EmbryoDocument3 pagesMOCK QUIZ - Head & Neck EmbryoLanz RomuloNo ratings yet
- Handbook of Endocrine Research TechniquesFrom EverandHandbook of Endocrine Research TechniquesFlora de PabloNo ratings yet
- Brainstem (Pons, Medulla, Midbrain) : Dr. MariaDocument23 pagesBrainstem (Pons, Medulla, Midbrain) : Dr. MariaMuhammad Mustaqeem100% (1)
- Practicals Histology Prelims ADocument36 pagesPracticals Histology Prelims AShaylla BretañaNo ratings yet
- Mptregulations 2010Document81 pagesMptregulations 2010jayababuNo ratings yet
- Histology of The SkinDocument23 pagesHistology of The Skinshmirtb100% (1)
- Histology of The EyeDocument5 pagesHistology of The EyeshindyNo ratings yet
- ANATOMY: Pelvic 2Document16 pagesANATOMY: Pelvic 2Nur Liyana MohamadNo ratings yet
- Research Surgery and Care of the Research Animal: Surgical Approaches to the Organ SystemsFrom EverandResearch Surgery and Care of the Research Animal: Surgical Approaches to the Organ SystemsNo ratings yet
- SGDDocument7 pagesSGDJanine Vega Calayo100% (1)
- Lower Limb: Front and Medial Aspect of ThighDocument8 pagesLower Limb: Front and Medial Aspect of ThighErnie G. Bautista II, RN, MDNo ratings yet
- Fergusson College (Autonomous) Pune: MicrobiologyDocument15 pagesFergusson College (Autonomous) Pune: MicrobiologyAAANo ratings yet
- Development of Skin Skin Largest Organ Embryonic Origins Vernixcaseosa1%#Document3 pagesDevelopment of Skin Skin Largest Organ Embryonic Origins Vernixcaseosa1%#Jonathan PaghubasanNo ratings yet
- Pyridoxine (Vitamin b6)Document16 pagesPyridoxine (Vitamin b6)Kuzhandai VeluNo ratings yet
- PHYSIOLOGY COMPRE 2nd Yr - 230512 - 233623 1Document9 pagesPHYSIOLOGY COMPRE 2nd Yr - 230512 - 233623 1SANKEPALLI, PAVITHRA REDDYNo ratings yet
- Cranial Nerves ExamDocument58 pagesCranial Nerves ExamTom JenyonNo ratings yet
- Muscles of The Neck PDFDocument1 pageMuscles of The Neck PDFEdreyn DellosaNo ratings yet
- Pharyngeal ApparatusDocument33 pagesPharyngeal ApparatusDeepa BhatNo ratings yet
- Osta Diagrams Facial Part of HeadDocument22 pagesOsta Diagrams Facial Part of HeadslyfoxkittyNo ratings yet
- MUSCLES OINA LavarnDocument20 pagesMUSCLES OINA LavarnStray KidsNo ratings yet
- 3 Hyman Digestive SystemDocument7 pages3 Hyman Digestive SystemJoachimNo ratings yet
- Histology of The SkinDocument48 pagesHistology of The SkinSHARON MARIA SUNNY100% (1)
- Anatomy MCQ - General PDFDocument6 pagesAnatomy MCQ - General PDFNesma MuslehNo ratings yet
- (Practical Exam) Back Row NotesDocument16 pages(Practical Exam) Back Row NotesKeesha RiveraNo ratings yet
- 2 ThoraxDocument7 pages2 Thoraxapi-3757921No ratings yet
- St. Luke's College of Medicine - William H. Quasha Memorial: AnatomyDocument4 pagesSt. Luke's College of Medicine - William H. Quasha Memorial: AnatomyMavic VillanuevaNo ratings yet
- Neural Tube DefectsDocument12 pagesNeural Tube Defectsdaniel_1592No ratings yet
- Axillary Artery: Branches First (1 Branch) Second Part (2 Branches) Third (3 Branches) 1 2 4Document14 pagesAxillary Artery: Branches First (1 Branch) Second Part (2 Branches) Third (3 Branches) 1 2 4foster18No ratings yet
- PONS: NeuroanatomyDocument20 pagesPONS: NeuroanatomyHassan IlyasNo ratings yet
- Anatomy - Skull FeaturesDocument6 pagesAnatomy - Skull FeaturesAkhil BansalNo ratings yet
- Quiz IVDocument5 pagesQuiz IVErvin T MileNo ratings yet
- Histology Notes 2Document13 pagesHistology Notes 2Lukas BüchlerNo ratings yet
- Upper Limb, Pectoral RegionDocument24 pagesUpper Limb, Pectoral Regiongtaha80No ratings yet
- Of These Parts of The Body. Example: What Structure Is Above The Eye?)Document4 pagesOf These Parts of The Body. Example: What Structure Is Above The Eye?)Anonymous QexowtfNo ratings yet
- Study GuideDocument43 pagesStudy GuideWahaj Mujahid100% (1)
- Anatomy LE2 Samplex 2017BDocument7 pagesAnatomy LE2 Samplex 2017BHanako Sasaki AranillaNo ratings yet
- BiostatisticsDocument16 pagesBiostatisticsEsper Soriano100% (1)
- Abnormalities in Cell Growth (Group 1)Document73 pagesAbnormalities in Cell Growth (Group 1)Michal VillanuevaNo ratings yet
- Brachial Plexus Self QuizDocument2 pagesBrachial Plexus Self Quizsan100% (1)
- MictobiologyDocument26 pagesMictobiologySaransh GhimireNo ratings yet
- Hema I Chapter 14 - CSFDocument28 pagesHema I Chapter 14 - CSFTesfaNo ratings yet
- USP Limit Test For LeadDocument2 pagesUSP Limit Test For LeadAbby MataNo ratings yet
- Gastrointestinal DrugsDocument11 pagesGastrointestinal DrugsAbby MataNo ratings yet
- Cholelithiasis AnaphysioDocument12 pagesCholelithiasis AnaphysioAbby MataNo ratings yet
- BiochemDocument3 pagesBiochemAbby Mata100% (1)
- Societal Security and Crisis Management by Per Lægreid, Lise H. RykkjaDocument398 pagesSocietal Security and Crisis Management by Per Lægreid, Lise H. Rykkjasabar odahNo ratings yet
- SHS UCSP Midterm Exam PDFDocument4 pagesSHS UCSP Midterm Exam PDFZllehb BhelayzNo ratings yet
- The Making of Race in Colonial Malaya-Political Economy and Racial IdeologyDocument34 pagesThe Making of Race in Colonial Malaya-Political Economy and Racial Ideologywafiq azmanNo ratings yet
- OriginallyDocument1 pageOriginallyIshita Narsiker100% (1)
- Grade 2 Reading RubricDocument3 pagesGrade 2 Reading Rubricanurag_kapila3901100% (3)
- Critical Book Review 1Document4 pagesCritical Book Review 1Hasri IndahNo ratings yet
- Mr. Pranav Padmanabhan: Email Mobile AddressDocument2 pagesMr. Pranav Padmanabhan: Email Mobile AddressSanju Kumar DPNo ratings yet
- On Color: The Husserlian Material A Priori: Jairo José Da SilvaDocument9 pagesOn Color: The Husserlian Material A Priori: Jairo José Da SilvaVero CohenNo ratings yet
- Empirical Studies Related To TFQ ModelDocument6 pagesEmpirical Studies Related To TFQ ModelapplesbyNo ratings yet
- Ielts Writing Task 2 WorkbookDocument14 pagesIelts Writing Task 2 WorkbookM A Alim Mukul89% (9)
- Adjective To Describe A PersonDocument31 pagesAdjective To Describe A PersonroshankqNo ratings yet
- Time Management Is Key To SuccessDocument19 pagesTime Management Is Key To SuccessbraramanNo ratings yet
- Interpretation of HumphreyDocument42 pagesInterpretation of HumphreyRima Octaviani AdityaNo ratings yet
- Encuesta Nacional Epidemiologia PsiquiatricaDocument16 pagesEncuesta Nacional Epidemiologia Psiquiatricaapi-3707147100% (2)
- Assigment 2Document4 pagesAssigment 2Yuan67% (3)
- Sanity in The World of DarknessDocument11 pagesSanity in The World of DarknessSteampunkObrimosNo ratings yet
- Rudolf Steiner. Mathematics and Occultis PDFDocument9 pagesRudolf Steiner. Mathematics and Occultis PDFJosé Santos PereiraNo ratings yet
- Demo PlanDocument3 pagesDemo PlanSelina HonradoNo ratings yet
- Management Is A Process: P O L CDocument17 pagesManagement Is A Process: P O L CMylene SalvadorNo ratings yet
- Emotional Impact of Typefaces: I. The BackgroundDocument2 pagesEmotional Impact of Typefaces: I. The BackgroundHari MohanNo ratings yet
- The Discourse of Arabic AdvertisingDocument41 pagesThe Discourse of Arabic Advertisingahreiz2009No ratings yet
- MET SpeakingPromptSample 01Document3 pagesMET SpeakingPromptSample 01Lorenzo Mahecha VillaNo ratings yet
- Sublime Metaphysical Illusion - Essay On Nietzsche's Birth of TragedyDocument3 pagesSublime Metaphysical Illusion - Essay On Nietzsche's Birth of TragedysjschuNo ratings yet
- COMM 1010 F2F (Syllabus)Document5 pagesCOMM 1010 F2F (Syllabus)SteveHaslamNo ratings yet
- Talent ManagementDocument14 pagesTalent ManagementPoojitha KottiNo ratings yet
- LACAPRA, D. Emile Durkheim - Sociologist and Philosopher (Em Inglês) PDFDocument301 pagesLACAPRA, D. Emile Durkheim - Sociologist and Philosopher (Em Inglês) PDFRafael50% (2)
- Multicultural Communication WorkbookDocument35 pagesMulticultural Communication WorkbookHugh Fox IIINo ratings yet
- Experimental PsychologyDocument15 pagesExperimental PsychologyAzubuike Chidi100% (1)
- Practical Research Part2Document6 pagesPractical Research Part2Paul VerzosaNo ratings yet
- The Impact of Culture On An OrganizationDocument4 pagesThe Impact of Culture On An OrganizationSivaraman P. S.No ratings yet