Professional Documents
Culture Documents
Circulatory System
Uploaded by
ahsanshaikh1992Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Circulatory System
Uploaded by
ahsanshaikh1992Copyright:
Available Formats
Blood
55% plasma: carries CO2; glucose, urea, amino-acids, hormones, heat, cells! 45% cells: all made in bone marrow; short life; destroyed in liver; only WBCs have nucleus, reproduce RBCs carry O2; no nucleus; biconcave ( SA); contain haemoglobin; small (8m so SA) WBCs: 3 sorts: Lymphocytes (antibodies); Monocytes (eat bacteria); Granulocytes (many jobs) Platelets: bits of cells vital for blood clotting (and tissue repair)
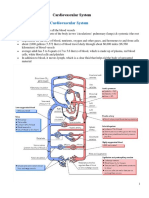
Blood Vessels
Blood pressure falls around system; highest, and varies most, in ventricles; Falls most in arterioles; travels slowest (most resistance) in capillaries; only veins have valves. Heart ventricles arteries arterioles capillaries venules veins heart atria Arteries: aorta (body); carotid (neck); renal (kidney); pulmonary (lungs, O2); hepatic (liver) Veins: vena cava (body); jugular (neck); renal (kidney); pulmonary (lungs, + O2); hepatic portal (gut liver); hepatic (liver). Arteries: thick, muscular walls, help to pump blood along (elastic recoil); narrow lumen (= high pressure); smooth lining (lowers resistance) Arterioles: muscular walls so blood flow follows demand (gut after meal, muscles for exercise, skin for cooling). Supply to brain is constant. Capillaries: site of exchange with cells; walls 1 cell thick (thus leak); high resistance, slow flow; Veins: thin walls, large lumen (thus very low pressure); run between muscle blocks (contraction squeezes blood along); pocket valves ensure blood flows one way ( heart)
Tissue fluid
Fluid surrounding body cells; isotonic with all cells in body Formation: High blood pressure at artery end forces fluid out; low pressure at veinous end not a problem; water and small molecules forced out (10%); proteins and cells remain behind (too big); thus water potential lowers Lower water potential at venous end so water re-enters by osmosis, down water potential gradient. Remaining fluid; drains into lymphatic system. Lymphatic system: Drains tissue fluid no pump; many valves; relies on muscle contraction to force fluid along; collects at lymph nodes = site of lymphocyte production (tonsils); also drain fats from guts in lacteals. Lymph returns to blood just outside the heart (right atrium).
Dual pump; all 4 chambers have same volume; myogenic (does not need nerves to stimulate) Diastole: = filling chamber (low pressure); Systole = contracting chamber (high pressure) Right side deoxygenated, blood from vena cava to lungs; lower pressure (short artery, no gravity) Left side: oxygenated, blood from lungs to body; highest pressure (long trip, problem of gravity) Blood flows: right atrium right ventricle lungs left atrium left ventricle body (aorta) Valves: semi-lunar valves between ventricles and main arteries; open at start of ventricular systole; close at end of ventricular systole (pressure in ventricle < artery) Atrio-ventricular (a-v) valves are between atria and ventricles (L = bicuspid, R = tricuspid) A-V valves open when atria contract (systole); (pressure > than ventricles); A-V valves close when ventricular systole begins (pressure > that in atria)
Diastole Blood returning from the body flows into the right atrium, and oxygenrich blood flowing from the lungs flows into the left atrium.
Atrial systole The right and left atria contract to push blood into the ventricles. The semi-lunar valves close to stop the blood flowing back into the heart.
Ventricular systole The ventricles contract to push blood out of the heart through semi-lunar valves. Both sets of AV valves close to prevent backflow.
Control: regulated by autonomic nerves (vagus, cardiac) and by hormones (adrenalin, insulin) Nerve impulse arrives at sino-atrial node (SAN); impulse travels over atria, causing contraction; to Atrio-ventricular node (AVN); DELAY (allows time for ventricles to fill); impulse down Bundle of His; causes ventricles to contract from bottom (thus fully emptying) Cardiac Output = stroke volume x heart rate (= pulse rate) Heart rate affected by: stress; exercise; drugs (caffeine); hormones; volume of blood returning
You might also like
- Ch18-Ch19 - NotesDocument5 pagesCh18-Ch19 - NotesCj LinceNo ratings yet
- Circulatory System NotesDocument10 pagesCirculatory System Notesdanlayton75% (4)
- Intercellular Control: The CirculationDocument16 pagesIntercellular Control: The CirculationHUAWEI HUAWEINo ratings yet
- General Heart Diagram, Handout Heart Diagram, Vessels HandoutDocument4 pagesGeneral Heart Diagram, Handout Heart Diagram, Vessels HandoutJNo ratings yet
- Paul Cardiac Lecture 2015 OutlineDocument6 pagesPaul Cardiac Lecture 2015 OutlineMichalis KantartzisNo ratings yet
- CVS 1 (Physiological Anatomy) .PDF AfraaDocument36 pagesCVS 1 (Physiological Anatomy) .PDF AfraaEra NewNo ratings yet
- Circulatory System and Gas Exchange Powerpoint CUMMULATIVEDocument55 pagesCirculatory System and Gas Exchange Powerpoint CUMMULATIVEAjay N. SharmaNo ratings yet
- Campbell & Reece Chapter 42 Circulatory System OverviewDocument23 pagesCampbell & Reece Chapter 42 Circulatory System OverviewAlexandra LigpitNo ratings yet
- NPTE CArdio NotesDocument27 pagesNPTE CArdio NotesAubrey Vale SagunNo ratings yet
- PHYSIOLOGY OF THE CARDIOVASCULAR SYSTEMDocument92 pagesPHYSIOLOGY OF THE CARDIOVASCULAR SYSTEMSanti Purnama SariNo ratings yet
- Blood Circ System NoteDocument55 pagesBlood Circ System NoteeyhethNo ratings yet
- The Circulatory SystemDocument3 pagesThe Circulatory SystemBrettnia Angela AradoNo ratings yet
- Multicellular Organisms: Circulatory SystemDocument36 pagesMulticellular Organisms: Circulatory SystemSpidervaitNo ratings yet
- Transport in Animals: The Circulatory SystemDocument6 pagesTransport in Animals: The Circulatory SystemAvyay TopraniNo ratings yet
- 03 CVS PhysiologyDocument55 pages03 CVS PhysiologyMonenus KedirNo ratings yet
- Chapter 11 Cardiovascular SystemDocument6 pagesChapter 11 Cardiovascular SystemClarisse Anne QuinonesNo ratings yet
- Cardiovascular SystemDocument34 pagesCardiovascular Systemurooj100% (1)
- The Cardiovascular System & Physiology of Heart: Presented By: Bhupendra Kumar Integrated M.TechDocument41 pagesThe Cardiovascular System & Physiology of Heart: Presented By: Bhupendra Kumar Integrated M.TechVignesh AshokNo ratings yet
- Powerpoint Thecardiovascularsystem Anatomyandphysiology 141126132329 Conversion Gate01Document75 pagesPowerpoint Thecardiovascularsystem Anatomyandphysiology 141126132329 Conversion Gate01FaridanrlNo ratings yet
- Heart Physiology GuideDocument41 pagesHeart Physiology GuideTheresya Pratiwhy KoniyoNo ratings yet
- 1 Cardiovascular SystemDocument6 pages1 Cardiovascular SystemWaltz PadlanNo ratings yet
- The Heart: Basis of Life .?Document94 pagesThe Heart: Basis of Life .?Diksha AgrawalNo ratings yet
- Anatomy & Physiology Bootcamp NotesDocument51 pagesAnatomy & Physiology Bootcamp Notesgeorgia robinsonNo ratings yet
- 2 Days Training Module 1Document36 pages2 Days Training Module 1ArumNo ratings yet
- Cardiovascular System: Presented by DR Aparna Ramachandran Mds 1 Dept of Public Health DentistryDocument73 pagesCardiovascular System: Presented by DR Aparna Ramachandran Mds 1 Dept of Public Health DentistryAparna RamachandranNo ratings yet
- Cardiovascularsystem 090820055728 Phpapp02Document75 pagesCardiovascularsystem 090820055728 Phpapp02muhammad ijazNo ratings yet
- CirculationDocument11 pagesCirculationRishikaphriya RauichandranNo ratings yet
- Circulatory System NotesDocument31 pagesCirculatory System NotesJMHenry0% (1)
- The Heart: (See An Anatomy Book and Chapter 9 of G&H)Document30 pagesThe Heart: (See An Anatomy Book and Chapter 9 of G&H)raanja2No ratings yet
- The Mammalian Circulatory SystemDocument58 pagesThe Mammalian Circulatory Systemirisgoldcaster100% (1)
- Circulatory System Review: Anatomy, Physiology & FunctionsDocument41 pagesCirculatory System Review: Anatomy, Physiology & FunctionsShayesra-Radina Laja SahibadNo ratings yet
- Circulatory Systems in BiologyDocument42 pagesCirculatory Systems in BiologyAkmal HishamNo ratings yet
- Body Fluids and CirculationDocument10 pagesBody Fluids and CirculationArjun ChristopherNo ratings yet
- Circulatory SystemDocument75 pagesCirculatory SystemSETH VILORIANo ratings yet
- Functional organization of the cardiovascular systemDocument19 pagesFunctional organization of the cardiovascular systemIbtesam Mohammed100% (2)
- Minggu 13 Peredaran DarahDocument11 pagesMinggu 13 Peredaran Darahcuksam27No ratings yet
- Circulation WorksheetDocument3 pagesCirculation Worksheetholagato100% (1)
- Cardiac Diseases and Cardiac RehabilitationDocument49 pagesCardiac Diseases and Cardiac RehabilitationHenri Benedict VillafloresNo ratings yet
- PMLS 2 6-13 (Lec)Document26 pagesPMLS 2 6-13 (Lec)Ricci Gwennmorei TaghapNo ratings yet
- Components of The Cardiovascular SystemDocument23 pagesComponents of The Cardiovascular SystemMr. DummyNo ratings yet
- NCLEX Cardiac ReviewDocument8 pagesNCLEX Cardiac ReviewKaren HutchinsonNo ratings yet
- Biology Chapter 10Document9 pagesBiology Chapter 10wongchengen2006No ratings yet
- Circulatory System PlanDocument95 pagesCirculatory System Plankirsten23No ratings yet
- Cardiac PhysiologyDocument102 pagesCardiac PhysiologyPeter Larsen100% (1)
- Functions of Cardiovascular System:: The Gross AnatomyDocument6 pagesFunctions of Cardiovascular System:: The Gross AnatomyShreyasi PatankarNo ratings yet
- Group 6 "Circulatory System" Circulatory SystemDocument6 pagesGroup 6 "Circulatory System" Circulatory SystemMitchelGramaticaNo ratings yet
- The Cardiovascular SystemDocument50 pagesThe Cardiovascular Systemquiaballares19No ratings yet
- Cardiovascular System: Parts and FunctionDocument14 pagesCardiovascular System: Parts and FunctionkeykeepNo ratings yet
- The Circulatory System: Agriscience 332 Animal Science #8646-A TEKS: (C) (2) (A) and (C) (2) (B)Document111 pagesThe Circulatory System: Agriscience 332 Animal Science #8646-A TEKS: (C) (2) (A) and (C) (2) (B)brdaisyNo ratings yet
- The Circulatory SystemDocument10 pagesThe Circulatory SystemRezki RasyakNo ratings yet
- Blood CirculationDocument42 pagesBlood CirculationAshu kumar100% (1)
- Circulatory SystemDocument111 pagesCirculatory SystemYounas Bhatti100% (1)
- 3 Circulation in ManDocument7 pages3 Circulation in ManAnasatcia Mcpherson 9c FNo ratings yet
- Transport in Animals BIOLOGY bySATRIADocument7 pagesTransport in Animals BIOLOGY bySATRIASatria HalimNo ratings yet
- 2.2 Cardiovascular SystemDocument49 pages2.2 Cardiovascular SystemPratham ChopraNo ratings yet
- Dr. Dini's guide to the cardiovascular systemDocument52 pagesDr. Dini's guide to the cardiovascular systemReni TeeWeeNo ratings yet
- Vertebrate Circulatory System #1Document36 pagesVertebrate Circulatory System #1Josephine Ivy JumalaNo ratings yet
- Animal Transport - IGCSE Biology Notes (2020)Document14 pagesAnimal Transport - IGCSE Biology Notes (2020)Zhi En LeeNo ratings yet
- Human Body Book | Introduction to the Vascular System | Children's Anatomy & Physiology EditionFrom EverandHuman Body Book | Introduction to the Vascular System | Children's Anatomy & Physiology EditionNo ratings yet