Professional Documents
Culture Documents
Cirrhosis Outline
Uploaded by
Stephanie TalbotOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Cirrhosis Outline
Uploaded by
Stephanie TalbotCopyright:
Available Formats
CIRRHOSIS OUTLINE: A.
CIRRHOSIS- diffuse destruction & fibrotic regeneration of hepatic cells which decreases blood flow, scar tissue formation decreased liver fxn B. TYPES: 1. LAENNECs ak.a ALCOHOLICS, NUTRITIONAL, PORTAL CIRRHOSIS i. Fatty liverfull of fat cells, leukocytes & lymphocytes 2. POSTNECROTIC- due to autoimmune hepatitis- diffuse bands fibrotic tissue 3. BILIARY- due to biliary obstructionjaundice w/ fibrosis 4. CARDIAC- due to right-sided heart failure (core Pulmonale)liver becomes reservoir for venous blood heart cant circulate, becoming anoxicfibrosis C. MOST COMMON CAUSE---ALCOHOL INGESTION D. ETIOLOGY 1. Formation fibrotic bands of connective tissue 2. Formation of nodular appearance which blocks bile & blood flow 3. Decrease liver fxn increase liver enzymes, disturbed metabolic fxn & disturbed circulatory pathways 4. Uncompensated or compensated liver fxn E. CAUSES 1. Alcohol ingestion 2. Hepatitis 3. Biliary/cardiovascular dx 4. Drugs & toxins F. EARLY S/S CIRROSIS 1. Anorexia 2. Weight loss 3. N&V 4. Dyspepsia 5. Flatulence 6. Diarrhea/constipation
7. Fever 8. Lassitude 9. Enlarged liver & spleen, palpable liver 10. Abdominal pain
G. LATE S/S CIRRHOSIS 1. Jaundice 6. Endocrine problems: 2. Peripheral edema gynecomastia, amenorrhea, 3. Ascites hyperaldosteronism 4. Skin lesions: palmar erythema, 7. Fetor hepaticas spider angiomas, striae, 8. Asterixis ecchymosis 9. Protruding umbilicus 5. Hematologic problems: 10. Hepatic encephalopathy thrombocytopenia, leukocytopenia, anemia H. COMPLICATIONS: 1. Portal HTN and esophageal & gastric varacies- due to dilation veins of esophagus, stomach, intestines & rectum from increased sinusoid pressure 2. Peripheral edema & ascites- due to decreased colloid pressure and increased hydrostatic pressure 3. Hepatic neuropathy- due to livers inability convert ammoniaurea to be excreted in urine 4. Hepatorenal syndrome- renal failure due hepatic failureno output
I.
LABS & DIAGNOSTICS: 1. Liver fxn : i. Increased AST, ALT, alkaline phosphatase, PTT, serum bilirubin & globulin ii. Decreased total protein, albumin, cholesterol, & urobilirubin in stool 2. Liver biopsy 3. EGD 4. Angiography (percutaneous transhepatic portographyPTP) 5. CT scan 6. Ultrasound 7. Serum e-lytes, CBC 8. Guaiac stool 9. Barium swallow J. COLLABORATIVE CARE 1. DIET THERAPY i. NA2+ restriction ii. High carb, mod protein, low fat diet iii. Admin B-complex vitamins: thiamine, folate, cobolamin 2. REST- to pull fluid from 3rd space 3. DRUG THERAPY i. Diuretic therapy- Spironolactone (Aldactone), Diuril, Lasix to excrete fluid from 3rd space 1. i/o, daily weight, abdominal girth, e-ltyes, low Na2+ antacids ii. Paracentesis 1. Explain procedure & informed consent 2. VS, weight, allergies 3. Void before procedure 4. Assist upright position w/ feet resting comfortably 5. During monitor: VS q15, measure 7 record drainage, position semi-fowlers & maintain bedrest till VS stable iii. COMFORT MEASURES 1. Elevate HOB 2. Encourage sitting chair w/ feet up iv. PERITONOVENOUS SHUNT if indicated 1. Pre-op- Vit K & fresh frozen plasma to treat coag probs, correct e-lyts, PRBC on hand for surgery 4. MANAGE ESOPHOGEAL VARACIES i. Gastric intubation to lavage stomach (ice NS) until fluid clear ii. Esophagogastric balloon tamponade to compress bleeding 1. Deflate Q8-12hrs to prevent necrosis 2. Check balloon for leaks, keep tube taped & secure 3. Check resp distress, cut balloon ports if in distress iii. Administer blood/blood products iv. Administer vasopressin & b-blocker to reduce portal HTN v. Injection sclerotherapy 1. Assess VS & chest pain 2. Administer pain meds 3. Assess lung sounds vi. Endoscopic band ligation procedure vii. Transjugular Intrahepatic portal systemic shunt 5. MANAGE HEPATIC ENCEPHALOPATHY i. Administer antibiotics ex. Neomycin to decrease intestinal flora ii. Admin Lactulose to promote fecal excretion of fecal ammoniadilute w/ fruit juice, want 2-5 soft stools daily, watery diarrhea= too much Lactulose
K. NURSING MANAGEMENT: 1. HEALTH PROMOTION i. Avoid alcohol, Tylenol & other hepatotoxic drugs, treat alcoholism ii. Adequate nutrition iii. Tx acute hepatitis, biliary dx & r-sided heart failure 2. ACUTE INTERVENTIONS i. Rest ii. Oral hygiene before meals iii. Tx jaundice w/ Cholestyramine iv. Note colour urine & stool v. I/O, daily weight, measure girth & extremities vi. Air pressure mattress for edema, turn q2hr, cough/deep bx, ROM, elevate lower extremities vii. Diuretics 1. Check Na+, K+, Cl- & bicarb levels 2. Check s/ s fluid retention & for hypokalemia viii. Monitor bleeding tendencies: melena, hematemesis, hemorrhage, anemia, increased risk infection.
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (120)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Myles Textbook For Midwives, 15th Edition: Journal of Obstetrics and GynaecologyDocument3 pagesMyles Textbook For Midwives, 15th Edition: Journal of Obstetrics and Gynaecologyintan wahyuNo ratings yet
- Prioritization, DelegationDocument5 pagesPrioritization, DelegationStephanie Talbot100% (1)
- Daily OrganizationDocument4 pagesDaily OrganizationStephanie TalbotNo ratings yet
- CardiacDocument43 pagesCardiacStephanie TalbotNo ratings yet
- BRY's Biology, 1st SemesterDocument93 pagesBRY's Biology, 1st SemesterStephanie TalbotNo ratings yet
- Structural Defects Upper GIDocument15 pagesStructural Defects Upper GIStephanie TalbotNo ratings yet
- Principles of DelegationDocument16 pagesPrinciples of DelegationStephanie Talbot100% (1)
- PUD OutlineDocument4 pagesPUD OutlineStephanie TalbotNo ratings yet
- Ulcerative Colitis OutlineDocument3 pagesUlcerative Colitis OutlineStephanie TalbotNo ratings yet
- Module 10.3: Children Who Have Alterations in Tissue PerfusionDocument23 pagesModule 10.3: Children Who Have Alterations in Tissue PerfusionStephanie TalbotNo ratings yet
- Reproductive System For Female OutlineDocument2 pagesReproductive System For Female OutlineStephanie Talbot100% (1)
- STD'S BacterialDocument2 pagesSTD'S BacterialStephanie TalbotNo ratings yet
- Hiatal Hernia OutlineDocument2 pagesHiatal Hernia OutlineStephanie TalbotNo ratings yet
- TPN OutlineDocument1 pageTPN OutlineStephanie TalbotNo ratings yet
- Reproductive CancersDocument2 pagesReproductive CancersStephanie TalbotNo ratings yet
- Laboratory Tests GI SystemDocument1 pageLaboratory Tests GI SystemStephanie TalbotNo ratings yet
- Neurovascular AssessmentDocument5 pagesNeurovascular AssessmentStephanie TalbotNo ratings yet
- OBESITY OutlineDocument2 pagesOBESITY OutlineStephanie TalbotNo ratings yet
- Module 7.2 Drug ChartDocument1 pageModule 7.2 Drug ChartStephanie TalbotNo ratings yet
- Module 7.3 Drug ChartDocument1 pageModule 7.3 Drug ChartStephanie Talbot100% (1)
- Musculoskeletal System OutlineDocument3 pagesMusculoskeletal System OutlineStephanie TalbotNo ratings yet
- Intestinal Obstruction OutlineDocument2 pagesIntestinal Obstruction OutlineStephanie Talbot100% (1)
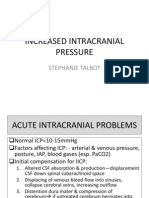
- Increased Intracranial PressureDocument13 pagesIncreased Intracranial PressureStephanie Talbot100% (1)
- Module 7.1 Drug ChartDocument2 pagesModule 7.1 Drug ChartStephanie TalbotNo ratings yet
- Musculoskeletal TraumaDocument3 pagesMusculoskeletal TraumaStephanie TalbotNo ratings yet
- Hepatitis OutlineDocument3 pagesHepatitis OutlineStephanie TalbotNo ratings yet
- Gynocological ProblemsDocument3 pagesGynocological ProblemsStephanie TalbotNo ratings yet
- Diverticulosis OutlineDocument3 pagesDiverticulosis OutlineStephanie TalbotNo ratings yet
- Cholecystitis Cholelithiasis OutlineDocument2 pagesCholecystitis Cholelithiasis OutlineStephanie TalbotNo ratings yet
- Crohns OutlineDocument4 pagesCrohns OutlineStephanie TalbotNo ratings yet
- Podiatry Dissertation ExamplesDocument7 pagesPodiatry Dissertation ExamplesBestOnlinePaperWritersUK100% (1)
- Indices and Measurement of Dental CariesDocument19 pagesIndices and Measurement of Dental Cariesmaher0% (1)
- Chapter 012Document5 pagesChapter 012lukeNo ratings yet
- Tropocells 4 Pages PDF Format January 2011Document4 pagesTropocells 4 Pages PDF Format January 2011robertoblumandradeNo ratings yet
- Antiaritmice Clasa I A MedicamentDocument3 pagesAntiaritmice Clasa I A MedicamentAndreea ElenaNo ratings yet
- Medical Report For Foreign Worker Health ScreeningDocument7 pagesMedical Report For Foreign Worker Health ScreeningP Venkata SureshNo ratings yet
- Jaw Opening Exercises Head and Neck Cancer - Jun21Document2 pagesJaw Opening Exercises Head and Neck Cancer - Jun21FalconNo ratings yet
- Stable Bleaching PowderDocument1 pageStable Bleaching PowderAbhishek SharmaNo ratings yet
- Plaque ControlDocument52 pagesPlaque ControlIbrahim AbdelHadi100% (1)
- ,previewDocument57 pages,previewhoàng đình sơn60% (5)
- PneumoniaDocument20 pagesPneumoniaKartika RezkyNo ratings yet
- Sleep Gauge - Sleep Quality ScoreDocument1 pageSleep Gauge - Sleep Quality ScoreMike UyNo ratings yet
- Cerebellopontine Angle Tumors: Guide:Dr Suchitra Dashjohn Speaker: DR Madhusmita BeheraDocument20 pagesCerebellopontine Angle Tumors: Guide:Dr Suchitra Dashjohn Speaker: DR Madhusmita Beheraasish753905No ratings yet
- 5090 w12 QP 11Document20 pages5090 w12 QP 11mstudy123456No ratings yet
- History of HypnosisDocument3 pagesHistory of HypnosisashvinNo ratings yet
- Motor Control TheoriesDocument19 pagesMotor Control Theoriessridhar_physio50% (2)
- Bioethics OutlineDocument30 pagesBioethics OutlineJason KeithNo ratings yet
- Writing Nursing Sample Test 2 2014Document4 pagesWriting Nursing Sample Test 2 2014Praveen B S PrasadNo ratings yet
- Blood Gas InterpretationDocument36 pagesBlood Gas InterpretationMary Charmaine DivinagraciaNo ratings yet
- Freedman Goldberg Reichmann The Radical Act of Inward LookingDocument35 pagesFreedman Goldberg Reichmann The Radical Act of Inward LookingSantharaj KuppuswamyNo ratings yet
- PharmDocument16 pagesPharmEi SetteNo ratings yet
- Genxraver Girl Interrupted Usmle Step 2 Notes PDFDocument259 pagesGenxraver Girl Interrupted Usmle Step 2 Notes PDFughbuzzoffNo ratings yet
- Vieillard-Baron2018 Article DiagnosticWorkupEtiologiesAndMDocument17 pagesVieillard-Baron2018 Article DiagnosticWorkupEtiologiesAndMFranciscoNo ratings yet
- Intracanal Medicaments and IrrigantsDocument85 pagesIntracanal Medicaments and IrrigantsAmit Abbey100% (1)
- cc11046 PDFDocument189 pagescc11046 PDFNurfadhilah YusufNo ratings yet
- MSDS - Dust SuppressantDocument3 pagesMSDS - Dust SuppressantJc RamírezNo ratings yet
- Survanta PiDocument10 pagesSurvanta PiBas BaylonNo ratings yet
- 30 - Gag Reflex - Causes and ManagementDocument4 pages30 - Gag Reflex - Causes and ManagementNadiyah Rizqi ANo ratings yet
- Emotionally Focused Therapy (Eft) and Emotionally Focused Family Therapy (Efft) : A Challenge/opportunity For Systemic and Post-Systemic TherapistsDocument5 pagesEmotionally Focused Therapy (Eft) and Emotionally Focused Family Therapy (Efft) : A Challenge/opportunity For Systemic and Post-Systemic TherapistsEFTcouplesNo ratings yet