Professional Documents
Culture Documents
RESPIRATORY
Uploaded by
RizMarieOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
RESPIRATORY
Uploaded by
RizMarieCopyright:
Available Formats
XI. RESPIRATORY A. Thoracic (Chest) Procedures: 1. Thoracentesis: a.
Pre-procedure: CHEST XRAY and baseline VITAL SIGNS Positioning: Sitting up over the bedside table. Sit in a chair backwards, propped up over the back of the chair. Cant sit up? Lie on UNAFFECTED side with HOB at 45. b. Procedure: Client must be very still, no coughing or deep breaths. The fluid is being removed from the PLEURAL SPACE. As the fluid is removed the lung should RE-EXPAND. Since you are removing fluid, the client could go into fluid volume DEFICIT. Therefore, you should be checking the VITAL SIGNS. c. Post-procedure: Another 150 Hurst Review Services 2. Chest tubes: a. Chest tube Insertion: What has happened that the client needs a chest tube? Lung has COLLAPSED. If the chest tube is placed in the upper anterior chest, (2nd intercostal space) then it is for removal of AIR. If the chest tube is placed laterally in the lower chest, (8th or 9th intercostal space) then it is for DRAINAGE. Why? Air TIGHT and drainage . Can the client have both? YES, THATS WHY IT IS Y CONNECTED. They are y-connected together and attached to a closed chest drainage unit (CDU).
The chest tube is sutured to the chest wall and a vaseline or AIR TIGHT dressing is applied around the chest tube exit site. The chest tube is then connected to a closed chest drainage unit. What is the purpose of the CDU? It is to restore the normal vacuum pressure in the pleural space. The CDU does this by removing all air and fluid in a closed ONE WAY system until the problem is corrected. b. Three chambers of the CDU 1) Drainage collection chamber: The chest tube connects to a 6 foot connection tube that leads to the DRAINAGE collection chamber. What if this chamber fills up? GET A NEW CDU 2) Water seal chamber: What is the purpose of the water seal? To promote ONE WAY flow out of the pleural space which will prevent AIR from moving back up the system and into the chest. The drainage chamber and water seal chamber are connected by a strawlike channel that allows the drainage to remain in the first chamber and the VENTED to go down into the water of the water seal chamber. This chamber contains the 2 cm of water which acts as a oneway valve. In other words we are preventing backflow. You may see when client coughs, sneezes, or exhales. You will see a slight rise and fall of water and the water seal tube as the client BREATHE.
This fluctuation is called TIDALING and is normal. If tidaling stops it usually means that the lung has re-expanded. Any air exists the water seal chamber and enters the third chamber called the suction control chamber. This allows any air to be vented out through the air vent found at the top of the suction control chamber. 3) Suction Control Chamber: If the client needs suction to remove air and fluid, this chamber controls the amount of PRESSURE applied. Sterile water is placed in this chamber up to the 20 cm line. This is the usual prescribed amount. Turn on the wall vacuum suction until you have SLOW gentle continuous bubbling. If a dry suction system is used, water is not used to regulate the pressure, therefore no bubbling. A dial is used to set the desired negative pressure. Once again increasing the vacuum wall suction will not increase the pressure. B. Management of Closed Chest Drainage Systems 1. Assessment: Assess dressing It must be kept TIGHT and INTACT. Listen to lung sounds bilaterally. Monitor pulse oximetry and report anything < LESS THAN 90 PERCENT. Record drainage every hour for 24 hours and then every 8 HOURS. Notify physician of 100ml of drainage or greater in 1st hour, and if there is a change in color to bright RED. Deep breathe, cough, and use incentive spirometer.
Watch for fever, WBCs, and drainage because they could develop an INFECTION at insertion site. Watch daily chest x-rays for RE-EXPANSION. 2. Maintaining CDU: Keep BELOW level of chest If you lift it to high FLUID will go back in. Want gravity drainage. Keep tubing straight and free of KINKS and dependent loops. Tape connections, it must be a CLOSED system. Monitor the water levels in the system. Want to see tidaling (fluctuations)with respirations Fluctuations will STOP when the lung has re-expanded, or kink/clot in tubing, or a dependent loop present in the system. 3. Trouble Shooting: a. What do you do if the tubing becomes disconnected? 1) Another STERILE connector at bedside. 2) Reconnect as fast as you can. b. What if my CDU falls over and my water leaks out or shifts to the drainage compartment? Do whatever you can to REESTABLISH the water seal. Set CDU upright, and fill water seal chamber to 2 cm of water. If there is not water in the water seal chamber then air can do what? Collapse the LUNG. What if the chest tube is accidentally pulled out? Sterile vaseline gauze taped down on 3 sides. OR PUT GLOVES. c. When is bubbling normal? Chest tube connected to suction, gentle CONTINOUS bubbling is expected in the suction chamber. If a client with a pneumothorax is coughing, sneezing, or just taking a deep
breath and exhaling, you may see INTERMITTENT bubbling in the water seal chamber. d. When is bubbling a problem? If there is CONTINOUS bubbling in the water seal chamber, then you have an air leak in the system. Never clamp a chest tube without an order. It could lead to a TENSION pneumothorax. 4. Chest tube removal: Have client take a deep breath and HOLD (valsalva) and place a vaseline gauze over the site. C. Chest Trauma: 1. Hemothorax/Pneumothorax: a. Pathophysiology: Blood or air has accumulated in the PLEURAL SPACE. What has happened to the lung? COLLAPSED b. S/S: SOB Increased HR Diminished breath sounds on the AFFECTED side. LESS movement on the affected side. Chest pain Cough What will show up on the chest x-ray? AIR or BLOOD Subcutaneous emphysema is air trapped in the tissue (usually neck and face). c. Tx: Thoracentesis, chest tubes, daily CXR If a pneumothorax is present and the client has a chest tube what type of bubbling would be expected to see in the water seal chamber? INTERMITTENT BUBBLING RULE: Never pull out a penetrated object.
2. Tension Pneumothorax (Trauma, PEEP): Trauma, PEEP, clamping a chest tube, or taping an open pneumothorax on all 4 sides without air valve. a. Pathophysiology: PRESSURE has built up in the chest/pleural space and has collapsed the lung PRESSURE pushes everything to the opposite side (mediastinal shift). b. S/S: Subcutaneous emphysema, absence of BREATH sounds on one side, asymmetry of thorax, respiratory distress. Can be fatal as accumulating pressure compresses vessels decreases venous return decreases CARDIAC OUTPUT. c. Tx: Large bore needle is placed into the 2nd ICS (by the doctor) to allow excess air to escape, find the cause, chest tube. 3. Open pneumothorax (sucking wound): a. Pathophysiology: Opening through chest that allows air into the CHEST. b. Tx: Have the client inhale and hold or valsalva (take a deep breath and hold) or hummmmm. Both of these will INCREASE the intra-thoracic pressure so no more outside air can get into the body. Then place a piece of petroleum gauze over the areaTape down how many sides? 3 SIDES Fourth side acts like a what? AIR VENT OR FLUTTER VALVE Have client sit up if possible to expand lungs. Trauma clients stay flat, until evaluated for other injuries.
4. Fractures of ribs and sternum: Most common injuries from chest trauma. a. S/S: Pain & tenderness Crepitus (bones gratting together) ShalloW RESPIRATION b. Tx: Non-narcotic analgesic Nerve block to assist with productive coughing. Support injured area with hands. Not recommended to immobilize with chest binders and straps, this could lead to pneumothorax and flail chest. 5. Flail Chest (multiple rib fractures): a. S/S: Pain Paradoxical chest wall movement (see-saw chest); chest sucks inwardly on inspiration and puffs out on expiration. To assess chest symmetry always stand at foot of bed to observe how the chest is rising and falling. Dyspnea, cyanosis Increased pulse b. Tx: Stabilize the area, intubate, ventilate Positive pressure ventilation stabilizes the area. 1) PEEP: Positive End Expiratory Pressure On end expiration the vent exerts a down into the lungs to keep alveoli open. Improves gas exchange and decreases the work of BREATHING. It EXPANDS and realigns the ribs so they can start growing back together. PEEP may also be used to treat pulmonary edema or severe hypoxemia.
The classic reason to use PEEP is Adult Respiratory Distress Syndrome (ARDS). 2) BiPAP: Bi-level Positive Airway Pressure Used a lot with COPD, heart failure, and sleep apnea. Exerts different levels of pressure on inspiration and expiration. 3) CPAP: Continuous Positive Airway Pressure Constant pressure is used for inspiration and expiration. Used for obstructive sleep apnea. Anytime you see PEEP, CPAP, or Bi-PAP, your priority nursing assessment is to check bilateral PNEUMOTHORAX. D. Pulmonary Embolism: 1. Cause: This can occur if a client becomes dehydrated, has venous stasis from prolonged immobility or surgery, or has been taking birth control pills. Clotting disorders or heart arrhythmias like A-Fib. 2. S/S Hypoxemia #1 PO2? LOW Short of breath, cough, RR Increased D-Dimer (increased with pulmonary embolus) Will tell if a clot is located ANYWHERE in the body (not just in the lungs) Positive VQ scan (a ventilation/perfusion scan that can detect an embolus; done in radiology) FOR POST OP Looks at BLOOD FLOW to the lungs, dye is used, remove JEWERLY from chest area so that it will not give false results. A positive spiral CT or CT angiography Hemoptysis COUGHING UP BLOOD Pulse? INCREASE Chest pain (sharp, stabbing)
CXR will show ATELECTASIS. BP in lungs? INCREASE PULMONARY hypertension 3. Tx: Prevent! Ambulate and HYDRATE. Oxygen ABGs Ventilator Decrease pain Heparin sodium, Warfarin (Coumadin), Enoxaparin (Lovenox)
You might also like
- NCLEX-RN Prep Plus: 2 Practice Tests + Proven Strategies + Online + VideoFrom EverandNCLEX-RN Prep Plus: 2 Practice Tests + Proven Strategies + Online + VideoRating: 3 out of 5 stars3/5 (4)
- Hurst BurnsDocument4 pagesHurst BurnsKristin Jones100% (5)
- TOP 30 NCLEX Meds PDFDocument2 pagesTOP 30 NCLEX Meds PDF281175100% (2)
- Testing Strategies: Hurst Review Services 240Document3 pagesTesting Strategies: Hurst Review Services 240reynold100% (1)
- The Chicago Review Press NCLEX-RN Practice Test and ReviewFrom EverandThe Chicago Review Press NCLEX-RN Practice Test and ReviewRating: 4 out of 5 stars4/5 (20)
- Fluids and ElectrolytesDocument6 pagesFluids and ElectrolytesRizMarie100% (1)
- ACIDDocument2 pagesACIDRizMarie100% (2)
- ORTHODocument2 pagesORTHORizMarie50% (2)
- Peds HESI Study GuideDocument5 pagesPeds HESI Study Guidemscostello985367% (9)
- Prado Random FactsDocument377 pagesPrado Random Factsjkrix100% (2)
- Peds ATI TakeawaysDocument4 pagesPeds ATI TakeawaysNiki95% (19)
- HESI PsyDocument16 pagesHESI PsyKrista Howe100% (14)
- PEDS HESI RN Case Studies With Practice TestDocument41 pagesPEDS HESI RN Case Studies With Practice Testbngraham4100% (6)
- Testing StrategiesDocument1 pageTesting StrategiesRizMarie100% (2)
- ORTHODocument2 pagesORTHORizMarie50% (2)
- ACIDDocument2 pagesACIDRizMarie100% (2)
- ENDOCRINEDocument5 pagesENDOCRINERizMarie100% (3)
- BURNSDocument4 pagesBURNSRizMarie100% (2)
- Psychiatric NursingDocument5 pagesPsychiatric NursingRizMarie100% (4)
- PEDIATRICSDocument5 pagesPEDIATRICSRizMarie75% (4)
- NEUROLOGICALDocument3 pagesNEUROLOGICALRizMarie100% (4)
- FINALTHOUGHTSDocument5 pagesFINALTHOUGHTSRizMarieNo ratings yet
- ONCOLOGYDocument6 pagesONCOLOGYRizMarie100% (2)
- Hurst - Content Review - Cardio (Edit)Document8 pagesHurst - Content Review - Cardio (Edit)Elaine NorbergNo ratings yet
- CARDIODocument7 pagesCARDIORizMarie100% (7)
- MANAGEMENTDocument3 pagesMANAGEMENTRizMarie50% (4)
- Common Lab Values With Normals and Critical Values PDFDocument2 pagesCommon Lab Values With Normals and Critical Values PDFRizMarie100% (7)
- Chronic Arterial Vs Chronic Venous PDFDocument1 pageChronic Arterial Vs Chronic Venous PDFRizMarieNo ratings yet
- RN Intense Remedial Packet AnswersDocument53 pagesRN Intense Remedial Packet AnswersAli Resendiz50% (4)
- CNS Stimulants and Depressants PDFDocument5 pagesCNS Stimulants and Depressants PDFRizMarie100% (1)
- Ati 2Document10 pagesAti 2KitesaMedeksa100% (6)
- Sata ListDocument11 pagesSata ListNaidin Catherine De Guzman-AlcalaNo ratings yet
- NCLEX RN Practice Questions 17Document29 pagesNCLEX RN Practice Questions 17clarheena89% (9)
- Key Concepts For An NCLEX-RN Cram SheetDocument3 pagesKey Concepts For An NCLEX-RN Cram Sheetema100% (2)
- Nclex PointersDocument2 pagesNclex PointersKira95% (19)
- Nclex NotesDocument18 pagesNclex Notesmaane1005No ratings yet
- Obstetric Questions: Please State Whether The Following Statements Are TRUE or FALSEDocument8 pagesObstetric Questions: Please State Whether The Following Statements Are TRUE or FALSEjulialeo90% (10)
- Nclex ReviewDocument27 pagesNclex ReviewNicole Chadwick100% (4)
- NCLEX Questions and AnswersDocument16 pagesNCLEX Questions and AnswersJoslyn Gross100% (3)
- ATI Predictor 2010 Topics To ReviewDocument8 pagesATI Predictor 2010 Topics To ReviewJonathon95% (19)
- Compressive Ati PDFDocument9 pagesCompressive Ati PDFsarahjaimeeNo ratings yet
- Mneumonics To PrintDocument22 pagesMneumonics To Printcharitoave100% (2)
- Med Surg Study GuideDocument27 pagesMed Surg Study Guidetrifecta31No ratings yet
- HURST NCLEX Review Facts PDFDocument6 pagesHURST NCLEX Review Facts PDFMikeNo ratings yet
- Select All That Apply SATADocument58 pagesSelect All That Apply SATANicholas TagleNo ratings yet
- Maternity Nclex RN ReviewDocument11 pagesMaternity Nclex RN ReviewKwai Browne100% (7)
- My Nclex Study GuideDocument4 pagesMy Nclex Study GuideLogin Nurse100% (1)
- DEAR TO NCLEX's HEART PDFDocument452 pagesDEAR TO NCLEX's HEART PDFrn msn100% (4)
- NCLEXDocument3 pagesNCLEXEternity RealNo ratings yet
- NCLEX Test Taking TipsDocument3 pagesNCLEX Test Taking TipsjrilleraNo ratings yet
- NATIONAL COUNCIL LICENSURE EXAMINATION FOR REGISTERED NURSES (NCLEX-RN): Passbooks Study GuideFrom EverandNATIONAL COUNCIL LICENSURE EXAMINATION FOR REGISTERED NURSES (NCLEX-RN): Passbooks Study GuideNo ratings yet
- COMPREHENSIVE NURSING ACHIEVEMENT TEST (RN): Passbooks Study GuideFrom EverandCOMPREHENSIVE NURSING ACHIEVEMENT TEST (RN): Passbooks Study GuideNo ratings yet
- 101 Ways to Score Higher on your NCLEX: What You Need to Know About the National Council Licensure Examination Explained SimplyFrom Everand101 Ways to Score Higher on your NCLEX: What You Need to Know About the National Council Licensure Examination Explained SimplyRating: 3.5 out of 5 stars3.5/5 (10)
- Chicago Review Press NCLEX-PN Practice Test and ReviewFrom EverandChicago Review Press NCLEX-PN Practice Test and ReviewRating: 4 out of 5 stars4/5 (4)
- ONCOLOGYDocument6 pagesONCOLOGYRizMarie100% (2)
- CNS Stimulants and Depressants PDFDocument5 pagesCNS Stimulants and Depressants PDFRizMarie100% (1)
- Common Lab Values With Normals and Critical Values PDFDocument2 pagesCommon Lab Values With Normals and Critical Values PDFRizMarie100% (7)
- Asthma 05 2011 Ta PDFDocument3 pagesAsthma 05 2011 Ta PDFRizMarie100% (1)
- MATERNITYDocument6 pagesMATERNITYRizMarie100% (3)
- RenalDocument3 pagesRenalStefanie HenryNo ratings yet
- NELEC2Document2 pagesNELEC2RizMarieNo ratings yet
- Chronic Arterial Vs Chronic Venous PDFDocument1 pageChronic Arterial Vs Chronic Venous PDFRizMarieNo ratings yet
- NEUROLOGICALDocument3 pagesNEUROLOGICALRizMarie100% (4)
- TestDocument6 pagesTestRizMarieNo ratings yet
- FINALTHOUGHTSDocument5 pagesFINALTHOUGHTSRizMarieNo ratings yet
- GASTROINTESTINALDocument5 pagesGASTROINTESTINALRizMarie100% (3)
- MANAGEMENTDocument3 pagesMANAGEMENTRizMarie50% (4)
- NP Test - 350 Items Key AnswerDocument56 pagesNP Test - 350 Items Key AnswerRizMarie100% (1)
- Pathophysiology: Our Lady of Fatima UniversityDocument2 pagesPathophysiology: Our Lady of Fatima UniversityRizMarieNo ratings yet
- CARDIODocument7 pagesCARDIORizMarie100% (7)
- NRes FormDocument1 pageNRes FormRizMarieNo ratings yet
- RizalDocument7 pagesRizalRizMarieNo ratings yet
- Chronic Osteomyelitis (M&R)Document8 pagesChronic Osteomyelitis (M&R)RizMarieNo ratings yet
- Asian CivDocument4 pagesAsian CivRizMarieNo ratings yet
- C CCC CCCCCC C C C (C C+ CCC CC) Cãc CCCCC CC CC, CCCC C (C C) CC CC CCCC CC C CC C C (CC) CDocument5 pagesC CCC CCCCCC C C C (C C+ CCC CC) Cãc CCCCC CC CC, CCCC C (C C) CC CC CCCC CC C CC C C (CC) CRizMarieNo ratings yet
- Adjuncts To Mechanical Ventilation: Tantani SugimanDocument36 pagesAdjuncts To Mechanical Ventilation: Tantani SugimanAndi Upik FathurNo ratings yet
- AQI Bulletin 20201126Document10 pagesAQI Bulletin 20201126Kartik PrabhakarNo ratings yet
- Journal Club DR - MaleehaDocument45 pagesJournal Club DR - MaleehaSYED MUHAMMAD SAMEEDNo ratings yet
- Bio1 11 - 12 Q2 0902 FDDocument16 pagesBio1 11 - 12 Q2 0902 FDKaren May HontiverosNo ratings yet
- Respiratory and Excretory System ReviewDocument27 pagesRespiratory and Excretory System ReviewJoyce Catherine Buquing UysecoNo ratings yet
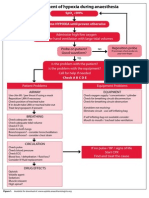
- Management of Hypoxia During AnaesthesiaDocument5 pagesManagement of Hypoxia During AnaesthesiaNurhafizahImfista100% (1)
- Lung Summary LeafletDocument4 pagesLung Summary LeafletDev Ebenezer JohnsonNo ratings yet
- Ventilators, Intensive Care - 052921032909Document9 pagesVentilators, Intensive Care - 052921032909Katlheen KrautzNo ratings yet
- COPDDocument41 pagesCOPDsanalcrazy100% (3)
- Sistema Curativo Por Dieta Amucosa - Arnold Ehret - WWW - Arnoldehret.infoDocument8 pagesSistema Curativo Por Dieta Amucosa - Arnold Ehret - WWW - Arnoldehret.infoLorena CalahorroNo ratings yet
- Mechanical Power FormulaDocument9 pagesMechanical Power FormulaEzeBorjesNo ratings yet
- Overview of Neonatal Respiratory Distress - Disorders of TransitionDocument14 pagesOverview of Neonatal Respiratory Distress - Disorders of TransitionAlfredo Junior Delgado PeláezNo ratings yet
- Diafragmatic Breathing 1Document8 pagesDiafragmatic Breathing 1Veven FeryatamaNo ratings yet
- Technical ManualDocument184 pagesTechnical ManualClaudio Roberto da CostaNo ratings yet
- Brosur Oxylog VE 300Document8 pagesBrosur Oxylog VE 300kentrunqNo ratings yet
- Respiration in PlantsDocument3 pagesRespiration in PlantsHarinarayan MobileNo ratings yet
- GB1 Q2 TosDocument2 pagesGB1 Q2 TosRuby UriarteNo ratings yet
- Respiratory Failure Vs DistressDocument1 pageRespiratory Failure Vs DistressMutiara Annisa AmadeaNo ratings yet
- Case Study 5 (Respiratory) - COPDDocument6 pagesCase Study 5 (Respiratory) - COPDSamantha AquinoNo ratings yet
- PT Case: Copd Exacerbation: DedicationDocument10 pagesPT Case: Copd Exacerbation: DedicationDianaLopezBorjaNo ratings yet
- Respiratory ExaminationDocument59 pagesRespiratory ExaminationNur Hamizah Md FuziNo ratings yet
- BIRD 8400service PDFDocument277 pagesBIRD 8400service PDFmarianoNo ratings yet
- Chapter 2 Respiratory AssessmentDocument9 pagesChapter 2 Respiratory AssessmentKathleen Dela CruzNo ratings yet
- Nueva Ecija University of Science and Technology: Case 7Document7 pagesNueva Ecija University of Science and Technology: Case 7jomariNo ratings yet
- Self Contained Breathing Apparatus: Positive Pressure (Preventing Inward Leaking)Document2 pagesSelf Contained Breathing Apparatus: Positive Pressure (Preventing Inward Leaking)Abraham DeVilliersNo ratings yet
- Anaerobic RespirationDocument10 pagesAnaerobic Respirationnadya munawwarohNo ratings yet
- Chapter 8. Mapleson Breathing SystemDocument37 pagesChapter 8. Mapleson Breathing Systemadham08No ratings yet
- Lesson 1 Human Breathing SystemDocument37 pagesLesson 1 Human Breathing SystemDavid Lawrence GarciaNo ratings yet
- Case ProgressionDocument2 pagesCase Progressionczeremar chanNo ratings yet
- Lesson Plan in Respiratory SystemDocument6 pagesLesson Plan in Respiratory SystemGamol Rieza Shayne100% (1)