Professional Documents
Culture Documents
Mnemonics
Uploaded by
Mohamoud MohamedOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Mnemonics
Uploaded by
Mohamoud MohamedCopyright:
Available Formats
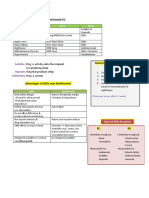
Pulmonary infiltrations inducing drugs "Go BAN Me!
": Gold Bleomycin/ Busulphan/ BCNU Amiodarone/ Acyclovir/ Azathioprine Nitrofurantoin Melphalan/ Methotrexate/ Methysergide
MPTP: mechanism, effect MPTP: Mitochondrial Parkinson's-Type Poison. A mitochondrial poison that elicits a Parkinson's-type effect.
Antimuscarinics: members, action "Inhibits Parasympathetic And Sweat": Ipratropium Pirenzepine Atropine Scopolamine Muscarinic receptors at all parasympathetic endings sweat glands in sympathetic.
Teratogenic drugs: major non-antibiotics TAP CAP: Thalidomide Androgens Progestins Corticosteroids Aspirin & indomethacin Phenytoin
Steroid side effects CUSHINGOID: Cataracts Ulcers Skin: striae, thinning, bruising Hypertension/ Hirsutism/ Hyperglycemia Infections Necrosis, avascular necrosis of the femoral head Glycosuria Osteoporosis, obesity Immunosuppression Diabetes
Beta blockers with CYP2D6 polymorphic metabolism "I Met Tim Carver, the metabolic polymorph": The following beta blockers require dose adjustment due to CYP2D6 polymorphic metabolism: Metoprolol Timolol Carvedilol (in patients with lower or higher than normal CYP2D6 activity)
Beta blockers with intrinsic sympathomimetic activity
Picture diabetic and asthmatic kids riding away on a cart that rolls on pinwheels. Pindolol and Carteolol have high and moderate ISA respectively, making them acceptable for use in some diabetics or asthmatics despite the fact that they are non-seletive beta blockers.
Muscarinic effects SLUG BAM: Salivation/ Secretions/ Sweating Lacrimation Urination Gastrointestinal upset Bradycardia/ Bronchoconstriction/ Bowel movement Abdominal cramps/ Anorexia Miosis
Sulfonamide: major side effects Sulfonamide side effects: Steven-Johnson syndrome Skin rash Solubility low (causes crystalluria) Serum albumin displaced (causes newborn kernicterus and potentiation of other serum albumin-binders like warfarin)
Epilepsy types, drugs of choice: "Military General Attacked Weary Fighters Pronouncing 'Veni Vedi Veci' After Crushing Enemies": Epilepsy types: Myoclonic Grand mal Atonic West syndrome Focal Petit mal (absence) Respective drugs: Valproate Valproate Valproate ACTH Carbamazepine Ethosuximide
Quinolones [and Fluoroquinolones]: mechanism "Topple the Queen": Quinolone interferes with Topoisomerase II.
Beta blockers: B1 selective vs. B1-B2 non-selective A through N: B1 selective: Acebutalol, Atenolol, Esmolol, Metoprolol. O through Z: B1, B2 non-selective: Pindolol, Propanalol, Timolol.
Ribavirin: indications RIBAvirin: RSV Influenza B Arenaviruses (Lassa, Bolivian, etc.) Hypertension: treatment ABCD:
ACE inhibitors/ AngII antagonists (sometimes Alpha agonists also) Beta blockers Calcium antagonists Diuretics
Narcotics: side effects "SCRAM if you see a drug dealer": Synergistic CNS depression with other drugs Constipation Respiratory depression Addiction Miosis Sex hormone drugs: male "Feminine Males Need Testosterone": Fluoxymesterone Methyltestosterone Nandrolone Testosterone
Ca++ channel blockers: uses CA++ MASH: Cerebral vasospasm/ CHF Angina Migranes
Atrial flutter, fibrillation Supraventricular tachycardia Hypertension Alternatively: "CHASM": Cererbral vasospasm / CHF Hypertension Angina Suprventricular tachyarrhythmia Migranes
Disulfiram-like reaction inducing drugs "PM PMT" as in Pre Medical Test in the PM: Procarbazine Metronidazole Cefo (Perazone, Mandole, Tetan).
Delerium-causing drugs ACUTE CHANGE IN MS: Antibiotics (biaxin, penicillin, ciprofloxacin) Cardiac drugs (digoxin, lidocaine) Urinary incontinence drugs (anticholinergics)
Theophylline Ethanol Corticosteroids H2 blockers Antiparkinsonian drugs Narcotics (esp. mepridine) Geriatric psychiatric drugs ENT drugs Insomnia drugs NSAIDs (eg indomethacin, naproxin) Muscle relaxants Seizure medicines
Morphine: side-effects MORPHINE: Myosis Out of it (sedation) Respiratory depression Pneumonia (aspiration) Hypotension Infrequency (constipation, urinary retention)
Nausea Emesis
Therapeutic dosage: toxicity values for most commonly monitored medications "The magic 2s": Digitalis (.5-1.5) Toxicity = 2. Lithium (.6-1.2) Toxicity = 2. Theophylline (10-20) Toxicity = 20. Dilantin (10-20) Toxicity = 20. APAP (1-30) Toxicity = 200.
Diuretics: thiazides: indications "CHIC to use thiazides": CHF Hypertension Insipidous Calcium calculi
Migraine: prophylaxis drugs
"Very Volatile Pharmacotherapeutic Agents For Migraine Prophylaxis": Verpamil Valproic acid Pizotifen Amitriptyline Flunarizine Methysergide Propranolol
Adrenoceptors: vasomotor function of alpha vs. beta ABCD: Alpha = Constrict. Beta = Dilate.
Antiarrhythmics: classification I to IV MBA College In order of class I to IV: Membrane stabilizers (class I) Beta blockers Action potential widening agents
Calcium channel blockers
Opiods: mu receptor effects "MD CARES": Miosis Dependency Constipation Analgesics Respiratory depression Euphoria Sedation
Cancer drugs: time of action between DNA->mRNA ABCDEF: Alkylating agents Bleomycin Cisplastin Dactinomycin/ Doxorubicin Etoposide Flutamide and other steroids or their antagonists (eg tamoxifen, leuprolide)
Busulfan: features ABCDEF:
Alkylating agent Bone marrow suppression s/e CML indication Dark skin (hyperpigmentation) s/e Endrocrine insufficiency (adrenal) s/e Fibrosis (pulmonary) s/e
Tricyclic antidepressants: members worth knowing "I have to hide, the CIA is after me": Clomipramine Imipramine Amitrptyline If want the next 3 worth knowing, the DNDis also after me: Desipramine Norrtriptyline Doxepin
Torsades de Pointes: drugs causing APACHE: Amiodarone Procainamide Arsenium Cisapride Haloperidol Eritromycin
Serotonin syndrome: components Causes HARM: Hyperthermia Autonomic instability (delirium) Rigidity Myoclonus
Tetracycline: teratogenicity TEtracycline is a TEratogen that causes staining of TEeth in the newborn.
Patent ductus arteriosus: treatment "Come In and Close the door": INdomethacin is used to Close PDA.
Physostigmine vs. neostigmine LMNOP: Lipid soluble Miotic Natural Orally absorbed well Physostigmine Neostigmine, on the contrary, is: Water soluble Used in myesthenia gravis Synthetic Poor oral absorption
Beta 1 selective blockers
"BEAM ONE up, Scotty": Beta 1 blockers: Esmolol Atenolol Metropolol
Antirheumatic agents (disease modifying): members CHAMP: Cyclophosphamide Hydroxycloroquine and choloroquinine Auranofin and other gold compounds Methotrexate Penicillamine
Auranofin, aurothioglucose: category and indication Aurum is latin for "gold" (gold's chemical symbol is Au). Generic Aur- drugs (Auranofin, Aurothioglucose) are gold compounds. If didn't learn yet that gold's indication is rheumatoid arthritis, AURActs Upon Rheumatoid.
Antiarrhythmics: class III members Bretylium Ibutilide Amiodarone Sotalol
BIAS:
MAOIs: indications MAOI'S: Melancholic [classic name for atypical depression] Anxiety Obesity disorders [anorexia, bulemia] Imagined illnesses [hypochondria] Social phobias Listed in decreasing order of importance. Note MAOI is inside MelAnchOlIc.
SIADH-inducing drugs ABCD: Analgesics: opioids, NSAIDs Barbiturates Cyclophosphamide/ Chlorpromazine/ Carbamazepine
Diuretic (thiazide)
K+ increasing agents K-BANK: K-sparing diuretic Beta blocker ACEI NSAID K supplement
Reserpine action: Reserpine depletes the Reserves of catecholamines [and serotonin].
Succinylcholine: action, use Succinylcholine gets Stuck to Ach receptor, then Sucks ions in through open pore. You Suck stuff in through a mouth-tube, and drug is used for intubation. Beta-blockers: side effects "BBC Loses Viewers In Rochedale": Bradycardia Bronchoconstriction Claudication
Lipids Vivid dreams & nightmares -ve Inotropic action Reduced sensitivity to hypoglycaemia Cisplatin: major side effect, action "Ci-Splat-In": Major side effect: Splat (vomiting sound)--vomiting so severe that antinausea drug needed. Action: Goes Into the DNA strand.
Vir-named drugs: use"-vir at start, middle or end means for virus": Drugs: Abacavir, Acyclovir, Amprenavir, Cidofovir, Denavir, Efavirenz, Indavir, Invirase, Famvir, Ganciclovir, Norvir,
Oseltamivir, Penciclovir, Ritonavir, Saquinavir, Valacyclovir, Viracept, Viramune, Zanamivir, Zovirax.
Phenobarbitone: side effects Children are annoying (hyperkinesia, irritability, insomnia, aggression). Adults are dosy (sedation, dizziness, drowsiness).
Prazocin: usage Prazocin sounds like an acronym of "praszz zour urine". Therefore Prazocin used for urinary retention in BPH.
Opioids: effects BAD
AMERICANS:
Bradycardia & hypotension
Anorexia Diminished pupilary size Analgesics Miosis Euphoria Respiratory depression Increased smooth muscle activity (biliary tract constriction) Constipation Ameliorate cough reflex Nausea and vomiting Sedation
TB: antibiotics used STRIPE: STreptomycin Rifampicin Isoniazid Pyrizinamide Ethambutol
Phenytoin: adverse effects PHENYTOIN: P-450 interactions Hirsutism Enlarged gums
Nystagmus Yellow-browning of skin Teratogenicity Osteomalacia Interference with B12 metabolism (hence anemia) Neuropathies: vertigo, ataxia, and headache
Narcotic antagonists
The Narcotic Antagonists are NAloxone and NAltrexone. Important clinically to treat narcotic overdose.
Thrombolytic agents USA: Urokinase Streptokinase Alteplase (tPA)
Routes of entry: most rapid ways meds/toxins enter body "Stick it, Sniff it, Suck it, Soak it": Stick = Injection Sniff = inhalation Suck = ingestion
Soak = absorption
Asthma drugs: inhibitor action
zAfirlukast: Antagonist of LT zIlueton: Inhibitor of 5-LO
Direct sympathomimetic catecholamines DINED: Dopamine Isoproterenol Norepinephrine Epinephrine Dobutamine
Anticholinergic side effects
"Know the ABCD'S of anticholinergic side effects": Anorexia Blurry vision Constipation/ Confusion Dry Mouth
Sedation/ Stasis of urine
Atropine use: tachycardia or bradycardia
"A goes with B": Atropine used clinically to treat Bradycardia.
Bleomycin: action "Bleo-Mycin Blows My DNA to bits": Bleomycin works by fragmenting DNA (blowing it to bits). My DNA signals that its used for cancer (targeting self cells).
Aspirin: side effects ASPIRIN: Asthma Salicyalism Peptic ulcer disease/ Phosphorylation-oxidation uncoupling/ PPH/ Platelet disaggregation/ Premature closure of PDA Intestinal blood loss Reye's syndrome Idiosyncracy Noise (tinnitus)
Lupus: drugs inducing it HIP: Hydralazine INH Procanimide
Vigabatrin: mechanism Vi-GABA-Tr-In: Via GABA Transferase Inhibition
Morphine: effects at mu receptor PEAR: Physical dependence Euphoria Analgesia Respiratory depression
Enoxaprin (prototype low molecular weight heparin): action, monitoring EnoXaprin only acts on factor Xa. Monitor Xa concentration, rather than APTT.
Beta-1 vs Beta-2 receptor location "You have 1 heart and 2 lungs": Beta-1 are therefore primarily on heart. Beta-2 primarily on lungs.
SSRIs: side effects SSRI: Serotonin syndrome Stimulate CNS Reproductive disfunctions in male Insomnia
Ipratropium: action Atropine is buried in the middle: iprAtropium, so it behaves like Atropine.
Warfarin: action, monitoring WePT: Warfarin works on the extrinsic pathway and is monitored by PT.
Propranolol and related '-olol' drugs: usage"olol" is just two backwards lower case b's. Backward b's stand for "beta blocker". Beta blockers include acebutolol, betaxolol, bisoprolol, oxprenolol, propranolol.
Depression: 5 drugs causing it PROMS: Propranolol Reserpine Oral contraceptives
Methyldopa Steroids
Lead poisoning: presentation ABCDEFG: Anemia Basophilic stripping Colicky pain Diarrhea Encephalopathy Foot drop Gum (lead line)
Myasthenia gravis: edrophonium vs. pyridostigmine eDrophonium is for Diagnosis. pyRIDostigmine is to get RID of symptoms.
Morphine: effects MORPHINES: Miosis Orthostatic hypotension
Respiratory depression Pain supression Histamine release/ Hormonal alterations Increased ICT Nausea Euphoria Sedation
Inhalation anesthetics SHINE: Sevoflurane Halothane Isoflurane Nitrous oxide Enflurane If want the defunct Methoxyflurane too, make it MoonSHINE.
Cholinergics (eg organophosphates): effects If you know these, you will be "LESS DUMB": Lacrimation Excitation of nicotinic synapses
Salivation Sweating Diarrhea Urination Micturition Bronchoconstriction
Benzodiazapines: ones not metabolized by the liver (safe to use in liver failure) LOT: Lorazepam Oxazepam Temazepam
Benzodiazepines: actions "Ben SCAMs Pam into seduction not by brain but by muscle": Sedation anti-Convulsant anti-Anxiety Muscle relaxant Not by brain: No antipsychotic activity.
Botulism toxin: action, related bungarotoxin Action: "Botulism Bottles up the Ach so it can't be the released":
Related bungarotoxin: "Botulism is related to Beta Bungarotoxin (beta-, not alpha-bungarotoxin--alpha has different mechanism).
Teratogenic drugs "W/ TERATOgenic": Warfarin Thalidomide Epileptic drugs: phenytoin, valproate, carbamazepine Retinoid ACE inhibitor Third element: lithium OCP and other hormones (eg danazol)
Gynaecomastia-causing drugs DISCOS: Digoxin Isoniazid Spironolactone Cimetidine Oestrogens Stilboestrol
Benzodiazepenes: drugs which decrease their metabolism "I'm Overly Calm": Isoniazid Oral contraceptive pills Cimetidine These drugs increase calming effect of BZDs by retarding metabolism.
Anesthesia: 4 stages "Anesthesiologists Enjoy S & M": Analgesia Excitement Surgical anesthesia Medullary paralysis
4-Aminopyradine (4-AP) use"4-AP is For AP": For AP (action potential) propagation in Multiple Sclerosis.
Osmotic diuretics: members GUM: Glycerol Urea Mannitol
Sodium valproate: side effects VALPROATE: Vomiting Alopecia Liver toxicity Pancreatitis/ Pancytopenia Retention of fats (weight gain) Oedema (peripheral oedema) Appetite increase Tremor Enzyme inducer (liver)
Nitrofurantoin: major side effects NitroFurAntoin: Neuropathy (peripheral neuropathy) Fibrosis (pulmonary fibrosis) Anemia (hemolytic anemia) Zafirlukast, Montelukast, Cinalukast: mechanism, usage"Zafir-luk-ast, Monte-luk-ast, Cina-luk-ast": AntiLukotrienes for Asthma. Dazzle your oral examiner: Zafirlukast antagonizes leukotriene-4.
Zero order kinetics drugs (most common ones) "PEAZ (sounds like pees) out a constant amount": Phenytoin Ethanol Aspirin Zero order Someone that pees out a constant amount describes zero order kinetics (always the same amount out)
Hepatic necrosis: drugs causing focal to massive necrosis "Very Angry Hepatocytes": Valproic acid Acetaminophen Halothane
Steroids: side effects BECLOMETHASONE: Buffalo hump Easy bruising Cataracts Larger appetite Obesity
Moonface Euphoria Thin arms & legs Hypertension/ Hyperglycaemia Avascular necrosis of femoral head Skin thinning Osteoporosis Negative nitrogen balance Emotional liability
Amiodarone: action, side effects 6 P's: Prolongs action potential duration Photosensitivity Pigmentation of skin Peripheral neuropathy Pulmonary alveolitis and fibrosis Peripheral conversion of T4 to T3 is inhibited -> hypothyroidism
Monoamine oxidase inhibitors:
Members "PIT of despair": Phenelzine Isocarboxazid Tranylcypromine A pit of despair, since MAOs treat depression
Warfarin: metabolism SLOW: Has a slow onset of action. A quicK Vitamin K antagonist, though. Small lipid-soluble molecule Liver: site of action Oral route of administration. Warfarin
Propythiouracil (PTU): Mechanism It inhibits PTU: Peroxidase/ Peripheral deiodination Tyrosine iodination Union (coupling)
Antibiotics contraindicated during pregnancy MCAT: Metronidazole Chloramphenicol Aminoglycoside Tetracycline
Beta-blockers: nonselective beta-blockers"Tim Pinches His Nasal Problem" (because he has a runny nose...): Timolol Pindolol Hismolol Naldolol Propranolol
Methyldopa: side effects METHYLDOPA: Mental retardation Electrolyte imbalance
Tolerance Headache/ Hepatotoxicity psYcological upset Lactation in female Dry mouth Oedema Parkinsonism Anaemia (haemolytic)
Lithium: side effects LITH: Leukocytosis Insipidus [diabetes insipidus, tied to polyuria] Tremor/ Teratogenesis Hypothyroidism
Respiratory depression inducing drugs "STOP breathing": Sedatives and hypnotics Trimethoprim Opiates Polymyxins
Benzodiazepenes: antidote "Ben is off with the flu": Benzodiazepine effects off with Flumazenil.
PHARMACOLOGY Mechanisms A. Scopolamine Anti-muscarinic Motion Sickness; preoperatively to reduce secretions Anti-muscarinic toxicities (mydriasis & cycloplegia; decreased secretions & sweating; flushing; bradycardia (low doses); tachycardia (high doses); urinary retention; drowsiness, hallucinations, coma) Typical Anti-psychotics (Chlorpromazine, Haloperidol, Thioridazine) Dopamine antagonists Schizophrenia; psychosis Lactation; Extrapyramidal effects (parkinsonism, akathisia (motor restlessness), tardive dyskinesia (lip smacking, jaw movements, etc.)); anti-cholinergic effects (antimuscarinic, alpha-antagonistic (orthostatic hypotension), and anti-histamine (sedation)). Toxicities are a tradeoffhigher extrapyramidal effects coincide with lower anticholinergic effects and vice-versa. The higher the extrapyramidal effects, the higher the potency (haloperidol > chlorpromazine > thioridazine) Atypical anti-psychotics (Clozapine) Dopamine antagonist Schizophrenia; psychosis NO extrapyramidal effects or lactation; agranulocytosis (fatal); Neuroleptic Malignant Syndrome (catatonia, autonomic instability, stupor); anti-cholinergic effects as above B. Opiate Agonists (Morphine, Meperidine, Codeine, Methadone, Heroin, Fentanyl) Act at mu, kappa, delta receptors in CNS Analgesia; Antitussive (Codeine); opiate addiction (Methadone); antidiarrheal (loperamide) CNS depression; nausea; respiratory depression; constipation; urinary retention; dependence Opiate Mixed Agonists-Antagonists (Pentazocine) Same as agonists but will cause withdrawal in those dependent on agonists Opiate Antagonists (Naloxone, Naltrexone) Block opiate receptors Narcotic overdose (no effect if used alone) Erythropoietin Increases RBC production in marrow Anemia associated with renal failure RU486 (Mifepristone) Progestin antagonist Early-term abortion Uterine bleeding, possible incomplete abortion C. Acarbose Alpha-glucosidase inhibitordecreases absorption of glucose NIDDM; adjunct to insulin in IDDM Flatulence; diarrhea; abdominal cramping
D. Losartan Angiotensin II antagonist Hypertension Similar to ACE inhibitors but no cough (decreased bradykinin activation) E. Myasthenia Gravis Drugs Inhibit cholinesterase Diagnosis (edrophonium); long-term treatment (Neostigmine, Pyridostigmine); open-angle glaucoma; reversal of non-depolarizing nm blockade Fasciculations & weakness F. desensitization of pituitaryLeuprolide GnRH analog decreased FSH, LH secretion Prostate Cancer receptor Transient excess testosterone production (prevent by combining with flutamide); impotence, hot flashes, tumor flare G. Flutamide Blocks inhibitory effects of testosterone on GnRH release Combo with leuprolide H. Aminoglutethimide pregneneloneInhibits Cholesterol conversion (like metyrapone) Metastatic breast cancer (decreased estrogen) Induces P450; transient CNS depression; rash I. Metformin Decreases gluconeogenesis; improves lipid profile (HDL rises, LDL falls) NIDDM lower risk of hypoglycemia GI side effects; lactic acidosis (rare); long-term interference w B12 absorption J. Stool Softeners (psyllium, methylcellulose) Absorbs peristalsis Constipation bulk water and softens stool Mechanism, clinical use, and toxicity of dermatologic agents: CORTICOSTEROIDS: Synthesized in the zona fascilculata of the adrenal cortex. Cortisol and Cortisone produced. 1) Glucocorticoids are catabolic. They influence carbohydrate and fat metabolism to insure adequate delivery of glucose to brain and tissues. 2) Decrease intestinal uptake of calcium; increase renal excretion of calcium (contribute to osteoporosis). 3) Supress the inflammatory response Decrease edema, fibrin deposition, capillary dilatation, leukocyte migration and phagocytic activity. Inhibit prostaglandin and leukotriene production by inhibiting phospholipase A2. 4) Include: Cortisone (short acting), Prednisone (intermediate acting), Prednisolone (similar to prednisone but no hepatic metabolism for activity), Methylprednisolone (similar to prednisolone but better anti-inflamatory and less mineralocorticoid effects), Triamcinolone (5x more potent than cortisol), Dexamethasone (long acting) & Beclomethasone (long acting available as aerosol). 5) Toxicity: a) Skin: hirsutism, skin thinning, poor wound healing, striae, acne and purpura. b) Other: hyperglycemia, hypertension, cataracts, glaucoma, peptic ulcer disease, osteoporosis, and increased susceptibility to infection. RETINOIDS: 1) Used to treat the following dermatologic diseases: Acne, psoriasis, icthyosis and has a potential benefit in early skin cancers (actinic keratosis) 2) Toxicity: in skin it can cause desquamation, dry skin and pruritus, erythema. ANTIFUNGALS: 1) Polyene antibiotics are fungicidal against both filamentous and yeastlike fungi including Histoplasma, Blastomyces, Coccidioides, Cryptococcus, Candida, Aspergillus and Sporothrix. Polyenes interact with sterols in the cytoplasmic membrane of fungi leading to rapid leakage of small molecules and death. Sensitive fungi have ergosterol in their membranes. a) Amphotercin B: Broad spectrum to treat systemic fungal infections. Side effects: Fever, chills,
impaired renal function, anemia, thrombocytopenia. b) Nystatin (Mycostatin): Similar to A but used primarily in topical preparations. Use in Candida infections and prophylaxis. 2) Imidazoles: Block the synthesis of fungal cell membrane ergosterols. a) Miconazole & Clomitrazole: Miconazole is the only imidazole that can be administered IV; clotrimazole is only used topically. i) Intravenous miconazole is rarely used due to toxicity. Treats ringworm, vulvovaginal candidiasis b) Ketoconazole: Oral administration only. Causes gynecomastia. 3) Miscellaneous: a) Flucytosine: Administer with amphotercin B in the treatment of cryptococcal meningitis and other systemic infections (synergistic). b) Griseofulvin: Binds to keratin, treat Tineas (capitis, corporis etc), Other new pharmacologic agents: 1) Erythopoietin (EPO): RBC growth factor. Produced in kindneys. Recombinant form available (epoietin alpha). a) Use for tx of Anemia 2nd to renal failure or zidovudine (AZT) use HIV patients. b) Use for tx of Anemia 2nd to chemo, or to stimulate rbc production prior to surgery or to facilitate autologous donation. c) Side effects: Clotting of dialysis tubing and hypertension. 2) RU486 (Mifrepristone): Abortificen. Blocks progesterone receptors and thereby progesterone support of pregnancy. 80% effective, 95% if used with prostaglandins. a) Complications include incomplete abortion (2%), ongoing pregnancy (1%), hemorrhage during D&C (<1%). Know About...... 1) Complications of empiric antibiotic use: a) Resistance: Must take into account susceptibility patterns of local settings. Must distinguish between community vs. nosocomial infection, and must take into account the patients immune status. b) Fungal Infections: Due to destruction of normal flora. (candidiasis). c) Other complications: C. Diff ototoxicity (must monitorPseudomembranous colitis. Gentamicin allergic reactions. 2)levels), Sulfonamides and Penicillin osteoporosis withSecondary effects of other drugs: a) Heparin chronic use. Thombocytopenia usually transient and mild. b) Hyperlipidemia, hypokalemia. 3) Drugs thatThiazides block/increase hepatic drug metabolism: a) Cimetidine: Histamine analog that cab reduce hepatic blood flow and slow clearance of other drugs and also reduces activity of cytochrome p-450 b) Ethanol: Chronic use induces hepatic microsomal enzymes and may enhance metabolism of other drugs. c) Phenobarbital: Increased phenobarbital levels in patients that have ethanol, chloramphenicol or valproic acid on board, since it has microsomal enzyme metabolism. d) Phenytoin (Dilantin): same as Metabolized by microsomal enzymes. e)Phenobarb and ETOH Rifampin: Causes jaundice and hepatotoxicity, also interacts with C p450 system. 4) Fundamental Pharmacodinamics: a) Partial agonists/agonist: Drugs that bind to receptors and stimulate them. b) Antagonists: are drugs that bind to receptors and decrease or block the effect of an agonist. They do not stimulate the receptors. i) Competitive antagonist: Reversibly binds to the receptor and prevents binding of the agonist. ii) Non competitive antagonist: Usually binds to the receptor irreversibly and prevents any agonist action. c) Efficacy: Maximal effect produced by a drug. d) Potency: Activity of a drug compared to a reference standard; depends on the drugs ability to reach the receptors and its affinity to the receptor. 5) Drug efficacy and potency as demonstrated on dose-response curves: a) ED50 (effect dose)- Dose which produces half-maximal response (ie., observed effect seen in 50% of patients); used as a measure of potency (the lower the ED50, the more potent the drug). b) TD50 (toxic dose)- Minimum dose which produces a specific toxic effect in 50% of individual (or animals). c) LD50 (lethal dose)- Minimum dose which kills 50% of animals. d) Therapeutic
index- Ratio of dose required to produce a toxic effect to the dose needed for a therapeutic effect. Used as an indication of drug safety. Expressed as : TI= TD50 or TI= LD50 You want drugs with a high therapeutic index (low ED 50 ED50 side effects at usual doses). 6) Pharmacogenetics: drugs whose metabolism is affected by inheritance: a) Isoniazid: Most commonly used drug for the treatment of TB. i) Inhibits biosynthesis of mycolic acids. ii) Metabolized in the liver (acetylated); speed of acetylation and consequently isoniazids half life is genetically determined (fast vs. slow acetylators). 7. Treatment of Anemia A. Anemia is due to increased destruction or decreased production. B. Microcytic anemia 1. Iron absorbed in the duodenum and proximal jejunum. Iron deficiency seen in premature infants, pregnant and lactating women. Ferrous oral salts can be given; give for 3-6 months to replenish iron stores. IV iron can also be given. 2. Iron toxicity a. N/V, cramps, constipation, diarrhea dose-related so decrease the dose b. Acute toxicity seen in kids, necrotizing gastroenteritis followed by shock, lethargy, dyspnea c. Chronic iron toxicity - hemochromatosis C. Megaloblastic anemia lack of vitamins needed for normal DNA synthesis, so the RBC gets biggger (macrocytic) 1. Vitamin B12 (normally obtained in meats), requires intrinsic factor for absorption (pernicious anemia decreases absorption), gastrectomy also decreases absorption. B12 is stored in the body (years supply) a. B12 deficiency also shows nervous defects b. B12 shots can be given if oral absorption is a problem c. Folate will NOT correct neurological features, but WILL help with the anemia 2. Folic Acid from green leafy veggies, body stores of folate are lower (1-6 months) a. Deficiency doesnt have neurological deficits b. Folic acid is well absorbed orally D. Decreased production 1. Erythropoietin used for renal failure, bone diseases, chemotherapy a. Toxicity too rapid increase in hematocrit can lead to HTN, thrombotic complications 2. Colony stimulating factors (G-CSF, GM-CSF) a. Increase recovery after myelosuppressive chemotherapy or BMT 8. Prevention/treatment of cerebrovascular disease K. Aspirin 1. Irreversibly blocks cyclooxygenase, = inhibits thromboxane (TxA2) formation from platelets 2. Only requires a small daily dose L. Ticlopidine 1. Inhibits platelet aggregation (inhibits ADP pathway) 2. Decreases TIAs, completed strokes, unstable angina pectoris 3. Diarrhea in 20%, leukopenia in 1% (must monitor white count) M. Thrombolytics catalyze formation of plasmin, a generalized lytic state in body is produced 1. Streptokinase cheap, allergic reactions possible 2. Urokinase 3. Tissue plasminogen activators (t-PA) expensive, from recombinant DNA 9. Treatment of rheumatoid arthritis A. Drugs that alter Pain 1. Aspirin 1st line drug, GI problems 2. NSAIDS - 3. COX-2 inhibitors less GI problems B. Drugs that Decrease Progression 1. Methotrexate and immunosuppressives more toxic side effects 2. Gold dermatitis is common side effect 10. Vaccines: indications, potential side effects A. Indications 1. Active immunization antigen is given so host develops antibodies (long protection) a. Give to children 2. Passive immunoglobins are given (short term protection) a. Give to those recently exposed (Tetanus, Botulinum, HBV, Rabies) or to travelers (Polio, tetanus, Measles, diphtheria) B. Side Effects 1. Giving live attenuated vaccines may cause the disease (eg. Polio vaccine) 2. Killed vaccine will not cause the disease 3. Allergic reactions are possible 11. Chemotherapeutic agents: risk of possible secondary cancer
You might also like
- Pharma MnemonicsDocument10 pagesPharma MnemonicsMuhammad Ali Aziz100% (4)
- Pharmacology: Teratogenic CarcinogenicDocument13 pagesPharmacology: Teratogenic CarcinogenicSherlock HolmesNo ratings yet
- Whole Pharmacology Classification: Adrenergic Antagonists Alpha Adrenergic Antagonists Alpha 1 AntagonistsDocument17 pagesWhole Pharmacology Classification: Adrenergic Antagonists Alpha Adrenergic Antagonists Alpha 1 AntagonistsFlorina TrutescuNo ratings yet
- Therapeutic IndexDocument8 pagesTherapeutic IndexMary Jennel RosNo ratings yet
- List of Look-Alike MedicationsDocument5 pagesList of Look-Alike MedicationsAhmad TaramsyNo ratings yet
- NS Review: Brain, Spinal Cord, Peripheral NervesDocument12 pagesNS Review: Brain, Spinal Cord, Peripheral Nervesitsme_rizaNo ratings yet
- Drug of Abuse (Table) PDFDocument2 pagesDrug of Abuse (Table) PDFtchanochNo ratings yet
- Pharmacology - Use of Beta-Blockers & Arbs in Cardiovascular Disease Treating HypertensionDocument5 pagesPharmacology - Use of Beta-Blockers & Arbs in Cardiovascular Disease Treating HypertensionDana20SNo ratings yet
- Pharmacology Drug ChartDocument50 pagesPharmacology Drug ChartEssentialForLivingNo ratings yet
- Antiseizure, Sedative & HypnoticsDocument8 pagesAntiseizure, Sedative & HypnoticsThulasi tootsieNo ratings yet
- Pharmacology FirecrackerDocument37 pagesPharmacology FirecrackerRehan Usman100% (1)
- Fluid Overload Student PagesDocument4 pagesFluid Overload Student PagesJess OswaldNo ratings yet
- Drugclasses Pharmacologypart 1 PDFDocument25 pagesDrugclasses Pharmacologypart 1 PDFSutanya100% (2)
- Pharm Expansion 17 NDFDocument1 pagePharm Expansion 17 NDFNokz M. Raki-inNo ratings yet
- Bot Med Final CHARTDocument33 pagesBot Med Final CHARTapi-26938624100% (3)
- List of Antidotes: No. Drugs AntidoteDocument3 pagesList of Antidotes: No. Drugs AntidotearjumandNo ratings yet
- (Pha) Le 5Document19 pages(Pha) Le 5Gabby TanNo ratings yet
- Drug Classificati On Indications Action Route/Dos e Side Effects Patient Teaching Nursing ImplicationsDocument7 pagesDrug Classificati On Indications Action Route/Dos e Side Effects Patient Teaching Nursing ImplicationsJenny NguyenNo ratings yet
- Assessment by Body SystemsDocument2 pagesAssessment by Body SystemsPat McGarryNo ratings yet
- REVISED-Med TaperingDocument3 pagesREVISED-Med TaperingDwi HerawatiNo ratings yet
- 2014antiepileptics 131129145211 Phpapp01 PDFDocument50 pages2014antiepileptics 131129145211 Phpapp01 PDFshravaniNo ratings yet
- Type 2 Diabetes Treatment Options ExplainedDocument2 pagesType 2 Diabetes Treatment Options ExplainedSafiya JamesNo ratings yet
- Integumentry PDFDocument17 pagesIntegumentry PDFMehul RathoreNo ratings yet
- DRUG SUMMARY TABLE - Anticoagulantes y AntiagregantesDocument3 pagesDRUG SUMMARY TABLE - Anticoagulantes y AntiagregantesManuel BetancurNo ratings yet
- Pharmacology and Treatment of AlcoholismDocument41 pagesPharmacology and Treatment of AlcoholismVarsha Shende Khobragade100% (2)
- Endocrine SystemsDocument1 pageEndocrine SystemsRean T. DeAndreasNo ratings yet
- Respi DrugsDocument36 pagesRespi DrugsLady Mae RamosNo ratings yet
- Parkinson's Disorder - Classification and MechanismDocument1 pageParkinson's Disorder - Classification and MechanismVương TúNo ratings yet
- Drugs in Blood DisordersDocument1 pageDrugs in Blood DisordersSantosh patelNo ratings yet
- Epilepsy Is Due To Sudden, Excessive Depolarization Of: Some or All Cerebral NeuronsDocument19 pagesEpilepsy Is Due To Sudden, Excessive Depolarization Of: Some or All Cerebral NeuronsMourian AmanNo ratings yet
- Physiology Clinical Diagnosis Treatment: TSI AntibodiesDocument10 pagesPhysiology Clinical Diagnosis Treatment: TSI Antibodies85robertNo ratings yet
- Drug Classes and Brand NamesDocument6 pagesDrug Classes and Brand Namesremyde07No ratings yet
- Combined Hormone Pill, Patch, Ring Progestin Only Mini Pill, Depo-Provera, IUDDocument1 pageCombined Hormone Pill, Patch, Ring Progestin Only Mini Pill, Depo-Provera, IUDnkuligowskiNo ratings yet
- Adrenergic AgentsDocument45 pagesAdrenergic AgentsAmit ShahNo ratings yet
- Anxiolytic Sedative-Hypnotic DrugsDocument31 pagesAnxiolytic Sedative-Hypnotic DrugsRoman MamunNo ratings yet
- 8B - Antianginal DrugsDocument70 pages8B - Antianginal Drugslalitrajindolia100% (1)
- Hypertension Drugs Cheat Sheet: by ViaDocument3 pagesHypertension Drugs Cheat Sheet: by ViaGulzaib KhokharNo ratings yet
- Drug CardsDocument3 pagesDrug CardsDave HillNo ratings yet
- Sodium Imbalances (Hyponatremia Vs Hypernatremia)Document17 pagesSodium Imbalances (Hyponatremia Vs Hypernatremia)Angel FiloteoNo ratings yet
- LECTURE 22: Antipsychotic Agents & Lithium: OutlineDocument5 pagesLECTURE 22: Antipsychotic Agents & Lithium: OutlineRosa PalconitNo ratings yet
- Classification of The DrugsDocument50 pagesClassification of The DrugsGlena SalamNo ratings yet
- Neurology VertigoDocument5 pagesNeurology VertigoJenny LauvitaNo ratings yet
- Acetylcholine Bioassay MethodsDocument1 pageAcetylcholine Bioassay MethodsSangi RajNo ratings yet
- EndocrineDocument2 pagesEndocrineUnclePorkchopNo ratings yet
- Paediatric Neurological ExaminationDocument13 pagesPaediatric Neurological ExaminationPrashant PalNo ratings yet
- SNS and PNS Drugs (Cholinergics and Adrenergics)Document5 pagesSNS and PNS Drugs (Cholinergics and Adrenergics)Whitney Krabbenhoft100% (1)
- Dka Guidelines - 2012Document4 pagesDka Guidelines - 2012djizhieeNo ratings yet
- Nursing and PharmacologyDocument9 pagesNursing and PharmacologyJennifer ViciosoNo ratings yet
- Pharmacology test tasks on cardiac glycosides and antiarrhythmic drugsDocument19 pagesPharmacology test tasks on cardiac glycosides and antiarrhythmic drugsBlessing NwosuNo ratings yet
- Table of Sedative, Hypnotic, AntianxietyDocument4 pagesTable of Sedative, Hypnotic, AntianxietyirfanzukriNo ratings yet
- Pharm C Exam 10 Drug ListDocument2 pagesPharm C Exam 10 Drug ListVokdadaNo ratings yet
- Drugs SummaryDocument23 pagesDrugs Summaryapi-3832811100% (1)
- An Easy Guide To Head To Toe Assessment Vrtis 2011-1 PDFDocument6 pagesAn Easy Guide To Head To Toe Assessment Vrtis 2011-1 PDFkatherine dayagNo ratings yet
- Pharmacology A - NSAIDSDocument14 pagesPharmacology A - NSAIDSselflessdoctorNo ratings yet
- PG PREPARATION - Mnemonics in PharmacologyDocument12 pagesPG PREPARATION - Mnemonics in PharmacologyRaveen KumarNo ratings yet
- Drug Guideline For Iron Polymaltose InjectionDocument7 pagesDrug Guideline For Iron Polymaltose Injectionmirza_baig_46No ratings yet
- Medication: Captopril (Capoten) Is An ACE Inhibitor and A Common Antihypertensive. Captopril Generic Name Contents (Hide)Document43 pagesMedication: Captopril (Capoten) Is An ACE Inhibitor and A Common Antihypertensive. Captopril Generic Name Contents (Hide)Kath Rubio0% (1)
- Bam Slam Drug CardDocument4 pagesBam Slam Drug CardLeticia GonzalezNo ratings yet
- Nemotecnias Step1Document18 pagesNemotecnias Step1Leon PaulNo ratings yet
- Mnemonic PharmaDocument13 pagesMnemonic Pharmamanoj kumarNo ratings yet
- Villaconstructionandwaterworks CompanyprofileDocument11 pagesVillaconstructionandwaterworks CompanyprofileMohamoud MohamedNo ratings yet
- Acute Kidney Injury (AKI) : Abdirahman Nour Mmed Internal MedicineDocument48 pagesAcute Kidney Injury (AKI) : Abdirahman Nour Mmed Internal MedicineMohamoud MohamedNo ratings yet
- Ethics Manual SDFDFDocument73 pagesEthics Manual SDFDFmattpiano535No ratings yet
- $overview of Amoud TeachingDocument2 pages$overview of Amoud TeachingMohamoud MohamedNo ratings yet
- Systemic SymptomsDocument1 pageSystemic SymptomsMohamoud MohamedNo ratings yet
- Abdo and HerniaDocument3 pagesAbdo and HerniaENNo ratings yet
- DischargeDocument1 pageDischargeMohamoud MohamedNo ratings yet
- Blood PressureDocument1 pageBlood PressureMohamoud MohamedNo ratings yet
- Acute Kidney Injury: DR Hodan Ahmed Dept of Pediatrics and Child Health Amoud Medical School, AUDocument32 pagesAcute Kidney Injury: DR Hodan Ahmed Dept of Pediatrics and Child Health Amoud Medical School, AUMohamoud MohamedNo ratings yet
- Abdo and HerniaDocument3 pagesAbdo and HerniaENNo ratings yet
- Hypokalemia Hyperkalemia CKD PresentationsDocument2 pagesHypokalemia Hyperkalemia CKD PresentationsMohamoud MohamedNo ratings yet
- Multiple MyelomaDocument27 pagesMultiple MyelomaMohamoud MohamedNo ratings yet
- Surgical Anatomy of the Stomach and DuodenumDocument75 pagesSurgical Anatomy of the Stomach and DuodenumMohamoud MohamedNo ratings yet
- Systemic Surgery Outline 2Document4 pagesSystemic Surgery Outline 2Mohamoud MohamedNo ratings yet
- Para Protein Emi ADocument14 pagesPara Protein Emi AMohamoud MohamedNo ratings yet
- Pediatric Obesity ProblemDocument77 pagesPediatric Obesity ProblemMohamoud MohamedNo ratings yet
- HemolysisDocument22 pagesHemolysisMohamoud MohamedNo ratings yet
- I.Def Anemia: DR Mukhtar Jama Nour, MBBS Amoud University For Health and Science InstituteDocument32 pagesI.Def Anemia: DR Mukhtar Jama Nour, MBBS Amoud University For Health and Science InstituteMohamoud MohamedNo ratings yet
- Oral Cavity 1Document14 pagesOral Cavity 1Mohamoud MohamedNo ratings yet
- Hemoglobinopathies: DR Mukhtar Jama Nour, MBBS Amoud University For Health and Science InstituteDocument32 pagesHemoglobinopathies: DR Mukhtar Jama Nour, MBBS Amoud University For Health and Science InstituteMohamoud MohamedNo ratings yet
- Canadian Diabetes Association Clinical Practice Guidelines Foot CareDocument19 pagesCanadian Diabetes Association Clinical Practice Guidelines Foot CareMohamoud MohamedNo ratings yet
- World Mothers ReportDocument70 pagesWorld Mothers Reportdwhite8No ratings yet
- Neck Traingles 44Document23 pagesNeck Traingles 44Mohamoud MohamedNo ratings yet
- Rehabilitation of Lower Limb AmputeeDocument53 pagesRehabilitation of Lower Limb AmputeeMohamoud Mohamed100% (2)
- STIs: Learn About Chlamydia, Gonorrhea, HPV, Hepatitis B, Herpes, HIV and Syphilis (35 charactersDocument25 pagesSTIs: Learn About Chlamydia, Gonorrhea, HPV, Hepatitis B, Herpes, HIV and Syphilis (35 charactersMohamoud MohamedNo ratings yet
- FirsrDocument43 pagesFirsrMohamoud MohamedNo ratings yet
- Eyes Anf EarsDocument62 pagesEyes Anf EarsMohamoud MohamedNo ratings yet
- Rehabilitation of Lower Limb AmputeeDocument53 pagesRehabilitation of Lower Limb AmputeeMohamoud Mohamed100% (2)
- Inguinal RegionDocument2 pagesInguinal RegionMohamoud MohamedNo ratings yet
- Pediatric ObesityDocument30 pagesPediatric ObesityMohamoud MohamedNo ratings yet
- Grounding Systems and Safety Practices AnalysisDocument29 pagesGrounding Systems and Safety Practices AnalysisFaiz MangalasseryNo ratings yet
- The Long Suffering of Frederic ChopinDocument7 pagesThe Long Suffering of Frederic ChopinDaniel CiobanuNo ratings yet
- Instructional Design HypertensionDocument8 pagesInstructional Design HypertensionGeoffrey OnyanchaNo ratings yet
- ISD1700Document24 pagesISD1700Kevin De La CruzNo ratings yet
- Complete Blood Count (CBC) Normal Laboratory Study Values: DefinitionDocument6 pagesComplete Blood Count (CBC) Normal Laboratory Study Values: DefinitionGlare RhayneNo ratings yet
- Chartering Terms ExplainedDocument49 pagesChartering Terms Explainedbrett1856No ratings yet
- Practicing Oil AnalysisDocument62 pagesPracticing Oil AnalysisCristian SNo ratings yet
- Specification SG 15CDocument3 pagesSpecification SG 15CJohan AlvarezNo ratings yet
- Crepe Paper 2017-05-29-FINALDocument2 pagesCrepe Paper 2017-05-29-FINALPruthvi KrishnaNo ratings yet
- Timing k4jDocument8 pagesTiming k4jCryy73No ratings yet
- Report of Mechanics of Machines 1Document12 pagesReport of Mechanics of Machines 1muhammaduzairNo ratings yet
- Lake Lanao Policy StudyDocument30 pagesLake Lanao Policy StudyGodfrey MordenoNo ratings yet
- BRP-1 Final Report Borjan Private LimitedDocument38 pagesBRP-1 Final Report Borjan Private LimitedArsalan IqbalNo ratings yet
- Silo Surface Area CalculationDocument3 pagesSilo Surface Area CalculationVIC EngineersNo ratings yet
- Fiche New FM Airbus enDocument2 pagesFiche New FM Airbus enCrystal LiuNo ratings yet
- Jacques-Émile Blanche - Cahiers D'un Artiste 1916Document247 pagesJacques-Émile Blanche - Cahiers D'un Artiste 1916matwashereNo ratings yet
- 526Document13 pages526jeas grejoy andrewsNo ratings yet
- Astm C62 05Document2 pagesAstm C62 05altaaeealaa0No ratings yet
- OBGYN Form 3 Answers KeyDocument2 pagesOBGYN Form 3 Answers KeyGrace0% (1)
- Micro Gear WheelDocument4 pagesMicro Gear WheelMuhammad Alep JamianNo ratings yet
- Godrej Group Is An Indian Conglomerate Headquartered in MumbaiDocument4 pagesGodrej Group Is An Indian Conglomerate Headquartered in MumbairahulbastyNo ratings yet
- NSL Hollow Core Slabs 12jul16 - 2016 Edition PDFDocument24 pagesNSL Hollow Core Slabs 12jul16 - 2016 Edition PDFjohnkoh9950% (2)
- BGMEA University of Fashion & Technology (BUFT)Document9 pagesBGMEA University of Fashion & Technology (BUFT)RIFAT HASANNo ratings yet
- History of CFD Work in IndiaDocument10 pagesHistory of CFD Work in IndiajoemonjacobNo ratings yet
- Estimation of The ProjectDocument89 pagesEstimation of The ProjectNaga PrasanthNo ratings yet
- Clerical Exam Sample PaperDocument21 pagesClerical Exam Sample PaperSarbjit Singh100% (1)
- Dubai UAE InformationDocument28 pagesDubai UAE InformationsefdeniNo ratings yet
- First Periodical Mapeh 9Document5 pagesFirst Periodical Mapeh 9Juvy Singian100% (1)
- False Teachings TodayDocument7 pagesFalse Teachings TodayobinwanneNo ratings yet