Professional Documents
Culture Documents
Pathophysiology of Angina
Uploaded by
Philip SimanganCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Pathophysiology of Angina
Uploaded by
Philip SimanganCopyright:
Available Formats
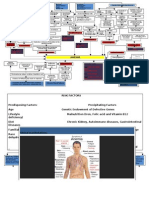
PATHOPHYSIOLOGY
Predisposing Age- 73 years old Hereditary- HPN, DM Gender- female Hx of Cholecystectomy (NMMC; 1995) Menopause (starts at age 42 years old; Menarche starts at age 13 yrs.old.) DM II (1999; usual glucose level: 140-160mg/dL; highest level: 300mg/dL) Precipitating >HPN (37 yrs old; usual BP 140/90; highest BP is 200/110mmHg) >Inc. serum Cholesterol level: 231mg/dL >Lack of exercise/activity >Obesity (BMI of 27 kg/m2, IBW: 48.96kg)
Increase shearing force of the arterial wall by the condition of the blood Nonspecific injury to arterial wall (endothelial injury) in the coronary artery
Diagnostic: CBC: Eosinophils-16.4%(0.006.00) Diagnostic: Blood Chemistry: Cholesterol-231 mg/dl (0-200 mg/dl) Triglycerides-191 mg/dL (0-150 mg/dl) Medication: >Atorvastatin Calcium (Lipitor)80mg 1 tab OD @ HS (Antilipidemics) >Enoxaparine Sodium (Lovenox)-o.6ml SC q12 (Antilipemics) >Aspirin (Aspilet EC)-80mg 1tab od (Nonopioid analgesics and antipyretics; antiplatelet) >Clopidogrel (Platexan) 75mg/tab, 4tabs now, then OD (Adenosine diphosphate (ADP) receptor antagonist
Desquamation of endothelial lining and stimulation of Mast cells to produce inflammation Increase permeability/adhesion molecules, Lipids (LDL, VLDL) and activation of platelets assimilation into the area Oxidized LDL attracts monocytes and macrophages to the site and plaques begin to form from cells and smooth muscle cells develop to form foam cells into thrombus
Diagnostic: >X-Ray Report (Chest AP- Sitting) Impressions: Medication: Atherosclerosis thoracic aorta. > >Amlodipine Besylate (Norvasc)Color Flow Doppler 50mg 1 tab Rupture of atherosclerotic plaque Conclusion: OD (Calcium-channel (cap) and Increase adhesion of a) blockers; Antianginals)motion abnormality Segmental wall >Nitroglycerin (Glyceryl these molecules and increase indicative of coronary artery disease Signs/ symptoms: Signs/ b) Trinitrate)-10mg Patch scleroses. Aortic and mitral thrombus/blood clot formation Right& left subcostal Coronary Ischemia and Ischemia symptoms: c) (Nitrates/Vasodilators; Aortic regurgitation, 1+ margin chest pain-5-6/10 Antianginals)regurgitation, trivial >Cold, by d) Mitral of tissue in the region supplied Diagnostic: pain scale; pain occur >Isosorbide Mononitrate (Imdur) Clammy skin Medication: Interventions: Diagnostic: >ECG tracing: the artery Occlusion and stenosis/narrowing of the even during exertion or 30mg 1 tab OD >prolonged/d> Metoprolol Tartrate >Obtained a 12 rest; heaviness and Clinical Chemistry: ST-depression & Signs/ symptoms: at lead ECG as coronary artery and leads to coronary (Nitrates/Vasodilators; ecreased Signs/ prescribed tightness of chest with (Toprol-XL) 50mg 1tab Decreased Calcium refill of 5 T wave >decreased capillary Antianginals) vasoconstriction Diagnostic:Signs/ symptoms: Interventions: symptoms: >Administered O2 inhalation via nasal 8.3 mg/dl inversion capillary refillBID (beta-adrenergic secs dyspnea; pain radiates 1tab of 5 secondsChemistry: Interventions: Signs/ Signs/ symptoms: >Jugular Increase demand for oxygen and glucose in the >Aspirin(Aspilet EC) 80mg cannula at 2L/min Clinical blockers, Dysrhythmias(bradycardia; >O2 therapy via nasal vein (8.4 10.2 mg/dl) >Clinical >RR: 26 cpm; tachypneic up to the neck and chin; od (Nonopioid analgesics) >increased Anti-dysrhythmics) >O2 therapy via Interventions: andAltered repolarization of nitrogensymptoms: cannula at 2L/min >tachycardia; PR:49-59bpm; tachycardia; distention >Advised to perform deep breathing Decreased Peripheral Anaerobic metabolism tissues leads to diminishedUrea Chemistry: myocardial >dyspnea >Diazepam (Valium)-5mg 1 tabIncrease guarding behavior, facial BP 22mg/dl (7-cell nasal cannula at (JVD)(Sept.4PR:130-150bpm NPO at 8cm Stimulation of sympathetic Increased Stimulation of cardiac sensory nerve exercises andgrimace; pursed-lip of used Acid production >Spironoloctone(Aldac Hypokalemia and Cardiac Increase >bradycardia; vasoconstriction and the myocardium that altered PR 130-150bpm); causedLactic of tachycarsia by increased oxygenation, Cellular hypoxia of can >use of accessory muscles to BID (Anxiolytics) 170/110mmHtone) 25mg 1tab OD 5,2009) except >palpitations noted decreased blood flowdecreased 17mg/dL) palpitations; dizziness Decreased Increase system to stimulate 2L/min myocardial release of breathingkinins,for O2 & glucose preload nervous PR: 49-59bpm endings to transmit 130-150bpm; ions, with techniquecentral mild to the potassium nervous Output to demand Unstable Angina breathe oxygen membrane lead 3.0 mmoL/L integrity > Metoprolol Tartrate (Toprol-XL) g Decreased norepinephrine and left ventricular >Elevated HOB P.O meds Increased after Increased Heart >maintained anxiety; body weakness relaxing environment (Potassium Sparing (3.5- 5.1 contractility needs adrenal medulla system to cause pain Pectoris prostaglandins >nasal flaring to the kidneys cardiac output 50mg 1tab BID (beta-adrenergic in the tissues/hypoxia Atherosclerosi s
Medication: >Losartan Potassium (Cozaar)-100mg 1tab OD (Angiotensin II antagonists) >Captopril(Capoten)-25mg tab BID (Angiotensin II antagonists)
Renin (released from kidneys) to split off angiotensinogen to form angiotensin I Angiotensin-converting enzyme (ACE) removes and converts Angiotensin I into Angiotensin II which promotes vasoconstriction Antidiuretic hormone Sodium retention by released from Angiotensin II stimulates kidneys and promotes an hypothalamus to increase adrenal cortex releaseby increased plasma reabsorption of water aldosterone osmotic to increased blood kidneys pressure
Medication: >Spironoloctone (Aldactone) 25mg 1 tab OD (Distal Tubule Diuretics/ Potassium Sparing Diuretics)
Constipation prior to admission (resolved Sept 1,2009)
Medication: Semma cone (Senokot)-30ml OD PO Lactulose (Chephulac)-30ml od PO Diarrhea resolved (Sept. 3, 2009)
Increased blood pressure
Overloading of blood in the ventricles of the heart
Interventions: Hold laxatives 2xday as indicated
for
BM
Signs/ symptoms: >BP170/110mmHg(hypertensive) >temp-36.8C >Dizziness(10 days prior to admission until assessment day >faintness(10days prior to admission)
Excessive stretch and decreased contraction occur
Increase workload of the heart
Diagnostic: >Echocardiography Conclusion: Concentric left ventricular hypertrophy with left ventricular diastolic dysfunction
Thickening of the cardiac muscle that leads to Left Ventricular Hypertrophy
Hypertensive Cardiovascular Disease (HCVD)
COMPLICATIONS: Myocardial Infarction Dysrhythmias Cardiogenic shock Pulmonary embolism Recurrent Myocardial Infarction Ventricular aneurysms Rupture of the heart Pericarditis Death
You might also like
- Pathophysiology of Hypertension, Diabetes, Ubm, BPHDocument3 pagesPathophysiology of Hypertension, Diabetes, Ubm, BPHCarly Beth Caparida LangerasNo ratings yet
- Anemia Pathophysiology All in 1 by Francis OliverosDocument3 pagesAnemia Pathophysiology All in 1 by Francis Oliverosfrancis00090No ratings yet
- Management of Hypertension: Affan Syafiqi - Nurul Husna - Audi RahmanDocument77 pagesManagement of Hypertension: Affan Syafiqi - Nurul Husna - Audi RahmanRavi K. ShuklaNo ratings yet
- ACS SchematicDocument2 pagesACS Schematicswish27No ratings yet
- B. Pathophysiology A) Schematic Diagram (Book - Based) : Wasting Blood Glucose LevelDocument2 pagesB. Pathophysiology A) Schematic Diagram (Book - Based) : Wasting Blood Glucose LevelCarl Elexer Cuyugan Ano50% (2)
- ACS PathophysiologyDocument2 pagesACS PathophysiologyFerliza OblenaNo ratings yet
- Non-St Segment Elevation Myocardial Infarction (Nstemi)Document24 pagesNon-St Segment Elevation Myocardial Infarction (Nstemi)MHIEMHOINo ratings yet
- ConceptMap AMLDocument1 pageConceptMap AMLnursing concept mapsNo ratings yet
- GERD PathophysiologyDocument35 pagesGERD PathophysiologyKathlea Noble-dc100% (1)
- PathophysiologyDocument1 pagePathophysiologyHazel PalomaresNo ratings yet
- Nstemi: How To Risk Stratify?Document32 pagesNstemi: How To Risk Stratify?dhannibernadetNo ratings yet
- NCP Chronic Renal FailureDocument15 pagesNCP Chronic Renal FailureNurul BariyyahNo ratings yet
- Pleural EffusionDocument12 pagesPleural EffusionWan HafizNo ratings yet
- Heart Valve DiseaseDocument9 pagesHeart Valve DiseaseChaturangaNSenerathNo ratings yet
- Colorectal Concept Map Group 2Document2 pagesColorectal Concept Map Group 2Maria CristinaNo ratings yet
- Burns Pathophysiology 2Document1 pageBurns Pathophysiology 2Monique Ann DanoyNo ratings yet
- PonstanDocument5 pagesPonstanYou know whoNo ratings yet
- NPDADocument52 pagesNPDAAlondra MangandogNo ratings yet
- Congestive Heart FailureDocument19 pagesCongestive Heart FailureIlavenil PanduranganNo ratings yet
- DM Case StudyDocument21 pagesDM Case StudyBern TolentinoNo ratings yet
- Concept MapDocument1 pageConcept Mapapi-252910411No ratings yet
- Pathophysiology of Congestive Heart Failure NarrativeDocument4 pagesPathophysiology of Congestive Heart Failure NarrativeAlfred BucabucaNo ratings yet
- Pa Tho Physiology of ParkinsonDocument2 pagesPa Tho Physiology of Parkinsoncuriosity_killsNo ratings yet
- 2 Acute Myocardial InfarctionDocument15 pages2 Acute Myocardial InfarctionpauchanmnlNo ratings yet
- Cerebrovascular Accident: "A Case Study Presentation"Document35 pagesCerebrovascular Accident: "A Case Study Presentation"Kristine YoungNo ratings yet
- Concept Map - Colon CancerDocument2 pagesConcept Map - Colon Cancerbea pegadNo ratings yet
- Nootropil: Qualitative and Quantitative CompositionDocument12 pagesNootropil: Qualitative and Quantitative CompositionMuhammad TalhaNo ratings yet
- Chronic Obstructive Pulmonary Disease (COPD) and Bronchial AsthmaDocument16 pagesChronic Obstructive Pulmonary Disease (COPD) and Bronchial AsthmaAngel Joy CatalanNo ratings yet
- Propranolol 1 PresentationDocument17 pagesPropranolol 1 Presentationapi-284092317100% (1)
- Case Presentation: Patient Chart - Mary JohnsonDocument12 pagesCase Presentation: Patient Chart - Mary Johnsonivoneeh_16100% (1)
- Omeprazole DSDocument2 pagesOmeprazole DSjenniferducaoNo ratings yet
- 4th Yr. Med Cardio Module Question - Copy-1Document11 pages4th Yr. Med Cardio Module Question - Copy-1Sheda BondNo ratings yet
- Chronic Obstructive Pulmonary Disease (COPD) : Sultan Chaudhry Benny Dua Eric WongDocument7 pagesChronic Obstructive Pulmonary Disease (COPD) : Sultan Chaudhry Benny Dua Eric Wongjamil aldasriNo ratings yet
- Addison's Disease. FinalDocument10 pagesAddison's Disease. FinalAnn KelseaNo ratings yet
- PathophysiologyDocument2 pagesPathophysiologyKarla Karina Dela CruzNo ratings yet
- PATHODocument9 pagesPATHOj_averilla2012No ratings yet
- (MED1) 3.04 Approach To Hypertension (Dr. Bago-Azares)Document11 pages(MED1) 3.04 Approach To Hypertension (Dr. Bago-Azares)NoreenNo ratings yet
- What Is Acute Pancreatitis?Document5 pagesWhat Is Acute Pancreatitis?leonard1971No ratings yet
- Case Study #5Document2 pagesCase Study #5Jenny Jenders100% (1)
- Acute Exacerbation of COPDDocument33 pagesAcute Exacerbation of COPDRalphE.BouDeleh100% (1)
- CKD + HPN Concept Map DRAFTDocument1 pageCKD + HPN Concept Map DRAFTInah Floresta BesasNo ratings yet
- DB31 - Pathophysiology of Diabetes Mellitus and HypoglycemiaDocument5 pagesDB31 - Pathophysiology of Diabetes Mellitus and HypoglycemiaNeil Alcazaren かわいいNo ratings yet
- Nephrolithiasis PDFDocument16 pagesNephrolithiasis PDFApriany Cordias Arlita SilalahiNo ratings yet
- Pathophysiology ErDocument3 pagesPathophysiology ErAlexa A. AldayNo ratings yet
- Hypertensive Cardiovascular DiseaseDocument5 pagesHypertensive Cardiovascular DiseaseAna Katrina OcanaNo ratings yet
- Hypertension Pathophysiology and Treatment PDFDocument6 pagesHypertension Pathophysiology and Treatment PDFBella TogasNo ratings yet
- Liver CancerDocument3 pagesLiver CancerMichael John F. NatividadNo ratings yet
- Concept Map Meningitis TheoryDocument3 pagesConcept Map Meningitis TheoryMia AuliaNo ratings yet
- Addison'sDocument4 pagesAddison'sKoRnflakesNo ratings yet
- Pathophysiology of Angina PectorisDocument1 pagePathophysiology of Angina PectorisCheryl100% (1)
- Drug StudyDocument14 pagesDrug StudyHannah Philene D. CalubNo ratings yet
- PT EducationDocument4 pagesPT Educationapi-248017509No ratings yet
- Myxedema ComaDocument14 pagesMyxedema Comabc3bhat6206No ratings yet
- Addison's Disease (Primary Adrenal Insufficiency)Document5 pagesAddison's Disease (Primary Adrenal Insufficiency)sunnnydayNo ratings yet
- Case 1 - Pneumonia (Final)Document4 pagesCase 1 - Pneumonia (Final)Joegie ArioNo ratings yet
- Neurogenic ShockDocument3 pagesNeurogenic ShockGlaizalyn Fabella TagoonNo ratings yet
- Left-Sided Heart FailureDocument3 pagesLeft-Sided Heart FailureKhalid Mahmud ArifinNo ratings yet
- Cardiotonic Drugs: Endang Martiniani Dra. M.PharmDocument44 pagesCardiotonic Drugs: Endang Martiniani Dra. M.PharmYUSRIL ZUMADINSYAHNo ratings yet
- Angina Pectoris PathophysiologyDocument4 pagesAngina Pectoris Pathophysiologyteddydeclines1467% (6)
- Antiangina and Hipolipidemic AgentsDocument83 pagesAntiangina and Hipolipidemic AgentsFaridah Yuwono 28No ratings yet
- Oncology Handouts PDFDocument21 pagesOncology Handouts PDFPhilip Simangan100% (1)
- Gastro Ibd Test DrillsDocument10 pagesGastro Ibd Test DrillsPhilip SimanganNo ratings yet
- Endocrine: Common Lab Tests For Endocrine and Hormonal DisordersDocument19 pagesEndocrine: Common Lab Tests For Endocrine and Hormonal DisordersPhilip SimanganNo ratings yet
- Endo and Git HandoutsDocument20 pagesEndo and Git HandoutsPhilip Simangan100% (1)
- Nursing Board Review CardioDocument16 pagesNursing Board Review CardioPhilip Simangan100% (1)
- Research Ps 2013Document42 pagesResearch Ps 2013Philip SimanganNo ratings yet
- Periop HandoutsDocument4 pagesPeriop HandoutsAileen Grace DulnuanNo ratings yet
- Complicated Obsterics FinalDocument14 pagesComplicated Obsterics FinalSteam LcNo ratings yet
- Growth and Development FinalDocument14 pagesGrowth and Development FinalGlenn Daryll SantosNo ratings yet
- Oncology Nursing: I. Epidemiology, Etiology, TermsDocument7 pagesOncology Nursing: I. Epidemiology, Etiology, TermsGlenn Daryll SantosNo ratings yet
- CHN NotesDocument17 pagesCHN NotesJohnny Yao JrNo ratings yet
- Safety and InfectionDocument7 pagesSafety and Infectionrhimineecat71No ratings yet
- Emergency FinalDocument8 pagesEmergency FinalGlenn Daryll SantosNo ratings yet
- Leadership and Managementfinal Nursing ReviewerDocument23 pagesLeadership and Managementfinal Nursing ReviewerPhilip Simangan100% (5)
- Ms HandoutsDocument11 pagesMs HandoutsPhilip SimanganNo ratings yet
- Perioperative NursingDocument10 pagesPerioperative NursingChin ChanNo ratings yet
- Peptic Ulcer DiseaseDocument3 pagesPeptic Ulcer DiseasePhilip SimanganNo ratings yet
- PediaDocument138 pagesPediaPhilip SimanganNo ratings yet
- RESEARCH Nursing ReviewerDocument9 pagesRESEARCH Nursing ReviewerPhilip SimanganNo ratings yet
- Nursing Board Review Medical SurgicalDocument9 pagesNursing Board Review Medical SurgicalPhilip Simangan0% (1)
- Community Health NursingDocument49 pagesCommunity Health NursingTaypen ArchieNo ratings yet
- 75 Items MS Random Questions With Answers and Rationale NLEDocument12 pages75 Items MS Random Questions With Answers and Rationale NLEAr-jay Jubane100% (7)
- Endocrine Drugs 2003Document61 pagesEndocrine Drugs 2003Philip SimanganNo ratings yet
- Dilation and CurettageDocument21 pagesDilation and CurettagePhilip SimanganNo ratings yet
- Anatomy and Physiology of Anatomy SystemDocument2 pagesAnatomy and Physiology of Anatomy SystemPhilip SimanganNo ratings yet
- UpdatesDocument4 pagesUpdatesPhilip SimanganNo ratings yet
- Patho PTBDocument3 pagesPatho PTBRenalyn Domingo JoseNo ratings yet
- Child Development Milestone ChartDocument21 pagesChild Development Milestone ChartPhilip SimanganNo ratings yet
- VELARDE-Pharmacology Notes Unit B-Cardiovascular System-2019Document19 pagesVELARDE-Pharmacology Notes Unit B-Cardiovascular System-2019j blNo ratings yet
- ACE INHIBITORS & ARBsDocument31 pagesACE INHIBITORS & ARBsMaria khurshidNo ratings yet
- Oestradiol As Hemihydrate + DrospirenoneDocument15 pagesOestradiol As Hemihydrate + Drospirenoneddandan_2No ratings yet
- NCP For HypertensionDocument6 pagesNCP For HypertensionJaic Ealston D. Tampus0% (2)
- Drug StudyDocument23 pagesDrug StudyJoyce Anne SupnetNo ratings yet
- SSC CGL Special Edition General Awareness NotesDocument130 pagesSSC CGL Special Edition General Awareness NotesRajdeepSenNo ratings yet
- Canine AscitesDocument7 pagesCanine AscitesGabriel Coelho GimenesNo ratings yet
- ICU Masterclass - Inotropes and Vasopressors HandbookDocument79 pagesICU Masterclass - Inotropes and Vasopressors HandbookRj PolvorosaNo ratings yet
- Fluid & ElectrolyteDocument26 pagesFluid & Electrolytesanjana bhatia100% (1)
- PathophysiologyDocument137 pagesPathophysiologyAhmed S. Hamid0% (1)
- CVD and HTNDocument60 pagesCVD and HTNZsazsa100% (1)
- CH 18 Endocrine3Document65 pagesCH 18 Endocrine3adamaditya666No ratings yet
- Fluids and Electrolytes A Fast and Easy Way To Understand Acid-Base Balance Without MemorizationDocument195 pagesFluids and Electrolytes A Fast and Easy Way To Understand Acid-Base Balance Without MemorizationNayely MoralesNo ratings yet
- Concept MapDocument5 pagesConcept MapRon OpulenciaNo ratings yet
- Flash Pulmonary EdemaDocument11 pagesFlash Pulmonary EdemaEda SopNo ratings yet
- ESRD PathophysiologyDocument2 pagesESRD PathophysiologyMark Ronhel Gallardo PerenalNo ratings yet
- Renal ' Renal ' Section Iii: Renal-Physiology Renal-AnatomyDocument20 pagesRenal ' Renal ' Section Iii: Renal-Physiology Renal-AnatomyLuis Jose VelazquezNo ratings yet
- Hypertension PathophysiologyDocument1 pageHypertension PathophysiologyTiffany Blanca Evangelista RaiNo ratings yet
- Study Guide PathoPhysiology UCLA N 230 ADocument27 pagesStudy Guide PathoPhysiology UCLA N 230 ATracy Pope100% (1)
- Chapter 5Document6 pagesChapter 5Shiny ChenNo ratings yet
- Vasodilators by Hiren PatelDocument28 pagesVasodilators by Hiren PatelHiren_Patel_2427No ratings yet
- Disease of Blood VesselsDocument5 pagesDisease of Blood VesselsKeshant SamarooNo ratings yet
- Answers RAAS WorksheetDocument2 pagesAnswers RAAS WorksheetParis ParisNo ratings yet
- Endo 3 Notes PDFDocument9 pagesEndo 3 Notes PDFDilNo ratings yet
- PathoPhysiology of Renal Failure (Overview)Document7 pagesPathoPhysiology of Renal Failure (Overview)Tiger Knee100% (3)
- Human Biological Science 2 BIOL122: National Workshop Manual 2019Document78 pagesHuman Biological Science 2 BIOL122: National Workshop Manual 2019Huge Lovely SmileNo ratings yet
- Circulation Seqs With Keys Edu Apnafort ComDocument10 pagesCirculation Seqs With Keys Edu Apnafort ComᎷᏒ ᏗᏒᎩᏗᏁ ᏦᏂᏗᏁNo ratings yet
- Renal PhysiologyDocument193 pagesRenal Physiologyramadan100% (1)
- Excretion & OsmoregulationDocument41 pagesExcretion & OsmoregulationSAGAR PADALKARNo ratings yet
- 10 - AutacoidsDocument67 pages10 - AutacoidscchatrumaNo ratings yet