Professional Documents
Culture Documents
Cefoxitin Sodium Mefoxin
Uploaded by
Kristi WrayCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Cefoxitin Sodium Mefoxin
Uploaded by
Kristi WrayCopyright:
Available Formats
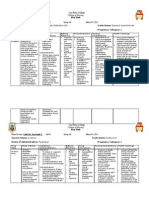
KRISTI WRAY DRUG NAME CLASS/FAMILY MECHANISM OF ACTION Generic: cefoxitin sodium Trade Name: Mefoxin ANTIBIOTIC; SECOND-GENERATION
CEPHALOSPORIN Semisynthetic, broad-spectrum beta-lactam antibiotic classified as secondgeneration cephalosporin; structurally and pharmacologically related to cephalosporins and penicillins. Preferentially binds to one or more of the penicillin-binding proteins (PBP) located on cell walls of susceptible organisms, thus making it bactericidal. It shows enhanced activity against a wide variety of gram-negative organisms and is effective for mixed aerobic-anaerobic infections. Infections caused by susceptible organisms in the lower respiratory tract, urinary tract, skin and skin structures, bones and joints; also intra-abdominal endocarditis, gynecologic infections, septicemia, uncomplicated gonorrhea, and perioperative prophylaxis in prosthetic arthroplasty or cardiovascular surgery. May be cephalosporin of choice for mixed aerobic-anaerobic infections (e.g., Bacteroides fragilis). Possible infection from surgery.
INDICATIONS
WHY IS YOUR PATIENT GETTING THIS MEDICINE ROUTES PATIENT DOSAGE COMMON DOSAGE
IV, IM 1gm IV q6h Moderate to Severe Infections Adult: IV/IM 12 g q68h, up to 12 g/day Child (older than 3 mo): IV/IM 80160 mg/kg/day in 46 divided doses (max: 12 g/day) Surgical Prophylaxis Adult: IV/IM 2 g 3060 min before surgery, then 2 g q6h for 24 h Child: IV/IM 3040 mg/kg 3060 min before surgery, then 3040 mg q6h for 24 h Cesarean Surgery Adult: IV/IM 2 g after clamping umbilical cord
PHARMACOKINETICS
FOR IV MEDS, COMPATIBILITY WITH IV DRIPS AND OR SOLUTIONS
Renal Impairment Dosage Adjustment CrCl 3050 mL/min: 12 g q812h; 1029 mL/min: 12 g q1224h; 59 mL/min: 0.51 g q1224h; greater than 5 mL/min: 0.51 g q2448h Hemodialysis Dosage Adjustment: Dose of 1 2 g post dialysis Peak: 2030 min after IM; 5 min after IV. Distribution: Poor CNS penetration even with inflamed meninges; widely distributed in body tissues including pleural, synovial, and ascitic fluid and bile; crosses placenta. Elimination: 85% unchanged in urine in 6 h, small amount in breast milk. Half-Life: 4560 min. Intravenous IV administration to neonates, infants and children: Verify correct IV concentration and rate of infusion/injection with physician. Prepare: Direct:
Rconstitue each 1 g with 10 mL sterile water, D5W, or NS. Intermittent: Following reconstitution, dilute 12 g in 50100 mL of D5W or NS. Continuous: Dilute large doses in 1000 mL of D5W or NS. Administer: Direct: Give over 35 min. Intermittent: Give over 15 min Continuous: Give at a rate determined by the volume of solution. Reconstituted solution may become discolored (usually light yellow to amber) if exposed to high temperatures; however, potency is not affected. Solution may be cloudy immediately after reconstitution; let stand and it will clear.
Incompatibilities: Solution/additive: AMINOGLYCOSIDES, ranitidine. Y-site: AMINOGLYCOSIDES, cisatracurium, fenoldopam, filgrastim, hetastarch, lansoprazole, pentamidine, vancomycin. After reconstitution, solution is stable for 24 h at 25 C (77 F); 7 days when refrigerated at 4 C (39 F), or 30 wk when frozen at 20 C (4 F). LAB VALUE ALTERATIONS CAUSE BY THIS MED Cefoxitin causes false-positive (black-brown or green-brown color) urine glucose reaction with copper reduction reagents such as Benedict's or Clinitest, but not with enzymatic glucose oxidase reagents (Clinistix, TesTape). With high doses, falsely elevated serum and urine creatinine (with Jaffe reaction) reported. Falsepositive direct Coombs' test (may interfere with cross-matching procedures and hematologic studies) has also been reported. Hypersensitivity to cephalosporins and related antibiotics. History of sensitivity to penicillin or other allergies, particularly to drugs; impaired renal function; coagulopathy; GI disease, colitis; pregnancy ( category B). Drug: Probenecid decreases renal elimination of cefoxitin. Body as a Whole: Drug fever, eosinophilia, superinfections, local reactions: pain, tenderness, and induration (IM site), thrombophlebitis (IV site). GI: Diarrhea, pseudomembranous colitis. Skin: Rash, exfoliative dermatitis, pruritus, urticaria. Urogenital: Nephrotoxicity, interstitial nephritis.
CONTRAINDICATIONS/P RECAUTIONS
INTERACTIONS ADVERSE/SIDE EFFECTS
KRISTI WRAY IMP NURS RESPONSIBILITIES Determine previous hypersensitivity to cephalosporins, penicillins, and other drug allergies before therapy is initiated. Lab tests: Perform culture and sensitivity testing prior to therapy; periodic renal function tests. Inspect injection sites regularly. Report evidence of inflammation and patient's complaint of pain. Monitor I&O rates and pattern: Nephrotoxicity occurs most frequently in patients older than 50 y, in patients with impaired renal function, the debilitated, and in patients receiving high doses or other nephrotoxic drugs. Be alert to S&S of superinfections ( see Appendix F"). This condition is most apt to occur in older adult patients, especially when drug has been used for prolonged period. Report onset of diarrhea (may be dose related). If severe, pseudomembranous colitis (see Signs & Symptoms, Appendix F) must be ruled out. Older adult patients are especially susceptible. Report promptly S&S of superinfection ( see Appendix F"). Report watery or bloody loose stools or severe diarrhea. Report severe vomiting or stomach pain. Report infusion site swelling, pain, or redness.
PT/FAMILY TEACHING
You might also like
- Nifedipine and Prednisone Drug StudyDocument5 pagesNifedipine and Prednisone Drug StudyAllyne GavinoNo ratings yet
- NifedipineDocument3 pagesNifedipineNovi YulianaNo ratings yet
- Dextrose 50 InjectionDocument6 pagesDextrose 50 InjectionLip StickNo ratings yet
- Drug Study FinalDocument5 pagesDrug Study FinalJackie Ann Marie DapatNo ratings yet
- Ranitidine Generic for Zantac Reduces Stomach AcidDocument3 pagesRanitidine Generic for Zantac Reduces Stomach AcidMarychen Cabunas100% (1)
- Drug Study - IbuprofenDocument3 pagesDrug Study - IbuprofenThalia UyNo ratings yet
- EMERGENCY DRUG STUDYDocument3 pagesEMERGENCY DRUG STUDYGrace Santos MirandaNo ratings yet
- Spinal Anes Drug StudyDocument12 pagesSpinal Anes Drug StudyNicosia Mae FerrerNo ratings yet
- DRUG NAME: Hydroxyurea: Synonym (S) : Common Trade Name (S) : ClassificationDocument7 pagesDRUG NAME: Hydroxyurea: Synonym (S) : Common Trade Name (S) : ClassificationDewinta AbutNo ratings yet
- DRUG STUDY - Docx Grand CaseDocument10 pagesDRUG STUDY - Docx Grand CaseAntonette PereyraNo ratings yet
- PrednisoloneDocument2 pagesPrednisoloneKatie McPeekNo ratings yet
- Acetaminophen (Tylenol)Document2 pagesAcetaminophen (Tylenol)amelia hearonNo ratings yet
- Pioglitazone (Actos, Lilly) : May Be Confused With Actidose, ActonelDocument3 pagesPioglitazone (Actos, Lilly) : May Be Confused With Actidose, Actonelshidyakg100% (1)
- FlecainideDocument3 pagesFlecainideAlexandra AntondyNo ratings yet
- Diphtheria and Tetanus Toxoids and Pertussis Vaccine Nursing ConsiderationsDocument2 pagesDiphtheria and Tetanus Toxoids and Pertussis Vaccine Nursing ConsiderationsKasandra Dawn Moquia Beriso100% (1)
- PlasilDocument1 pagePlasilernestjohnNo ratings yet
- CEFOXITINDocument30 pagesCEFOXITINJaessa FelicianoNo ratings yet
- Drug Study CefuroximeDocument2 pagesDrug Study CefuroximeTipey Segismundo100% (1)
- Timolol MaleateDocument3 pagesTimolol MaleateAP TOROBXNo ratings yet
- Drug Analysis CefoxitinDocument2 pagesDrug Analysis CefoxitinNika LoNo ratings yet
- Keppra (Levetiracetam)Document2 pagesKeppra (Levetiracetam)E100% (1)
- Veklury (Remdesivir) Dosing, Indications, Interactions, Adverse Effects, and MoreDocument4 pagesVeklury (Remdesivir) Dosing, Indications, Interactions, Adverse Effects, and MoreRex ChanNo ratings yet
- Enalapril MaleateDocument3 pagesEnalapril MaleatelichunghkNo ratings yet
- BisacodylDocument1 pageBisacodylianecunarNo ratings yet
- Albuterol VentolinDocument3 pagesAlbuterol VentolinKristi WrayNo ratings yet
- Cefazolin (Ancef)Document1 pageCefazolin (Ancef)Adrianne BazoNo ratings yet
- Drug Study Emergency DrugsDocument6 pagesDrug Study Emergency DrugsJhessa Curie PitaganNo ratings yet
- Drug Study March 03 2011Document10 pagesDrug Study March 03 2011zhapper2002No ratings yet
- CimetidineDocument3 pagesCimetidineapi-3797941No ratings yet
- Sulfa Sal AzineDocument2 pagesSulfa Sal Azineikke alma alukaNo ratings yet
- Drug Name Mechanism of Action Administration Indication Contraindication Adverse Effects Nursing ResponsibilitiesDocument1 pageDrug Name Mechanism of Action Administration Indication Contraindication Adverse Effects Nursing ResponsibilitiesIvan Liquiran AvenadoNo ratings yet
- Drug Study Catapres. Losartan, Nootropil Cefuroxime, ArcoxiaDocument2 pagesDrug Study Catapres. Losartan, Nootropil Cefuroxime, Arcoxiajoy_monterubioNo ratings yet
- Effects of atracurium besylateDocument3 pagesEffects of atracurium besylateWidya WidyariniNo ratings yet
- Ateneo de Davao University College of Nursing Drug StudyDocument4 pagesAteneo de Davao University College of Nursing Drug StudyaolbinarNo ratings yet
- Verapamil HCLDocument3 pagesVerapamil HCLMae Ann Bueno CastillonNo ratings yet
- Imipenem Cilastatin (Primaxin)Document1 pageImipenem Cilastatin (Primaxin)ENo ratings yet
- Ceftriaxone medication guideDocument3 pagesCeftriaxone medication guideCiera YoungNo ratings yet
- Drug Study FDocument3 pagesDrug Study FFatima Love Ariate-ArcasetasNo ratings yet
- PHINMA - UNIVERSITY OF ILOILO DRUG STUDY ON ROPIVACAINE/BUPIVACAINEDocument2 pagesPHINMA - UNIVERSITY OF ILOILO DRUG STUDY ON ROPIVACAINE/BUPIVACAINErica sebabillonesNo ratings yet
- Drug Study...Document5 pagesDrug Study...Ezra Dizon ManzanoNo ratings yet
- AmiodaroneDocument2 pagesAmiodaroneanindiawNo ratings yet
- LansoprazoleDocument3 pagesLansoprazoleJody FelizioNo ratings yet
- DrugStudy - CamaristaColeenMaeC (BSN III-G) (Prednisone)Document2 pagesDrugStudy - CamaristaColeenMaeC (BSN III-G) (Prednisone)Coleen Mae CamaristaNo ratings yet
- 3 Drug Study & 1 NCPDocument4 pages3 Drug Study & 1 NCPAnnie Christine RiveraNo ratings yet
- NCP & Drug Study (Tondo Med)Document5 pagesNCP & Drug Study (Tondo Med)Kevin_Remollo_2431No ratings yet
- Assessment Nursing Diagnosis Planning Intervention Rationale EvaluationDocument2 pagesAssessment Nursing Diagnosis Planning Intervention Rationale EvaluationAbigail BascoNo ratings yet
- Drug StudyDocument21 pagesDrug StudyShyla Garnace JavillonarNo ratings yet
- Myonal, Eperisone DrugDocument4 pagesMyonal, Eperisone DrugDhaneswara Adhyatama100% (1)
- Vii. Drug Study Drug Mechanism of ActionDocument7 pagesVii. Drug Study Drug Mechanism of ActionRifa'atul MahmudahNo ratings yet
- LantusDocument1 pageLantusCassie100% (4)
- DRUGSTUDY RANITIDINE, METRONIDAZOLE, CEFUROXIME, KEtorolac NUBainDocument7 pagesDRUGSTUDY RANITIDINE, METRONIDAZOLE, CEFUROXIME, KEtorolac NUBainKyle Cholo CholoNo ratings yet
- Fentanyl SublimazeDocument2 pagesFentanyl SublimazeENo ratings yet
- Cephalexin (Keflex)Document1 pageCephalexin (Keflex)ENo ratings yet
- Drug StudyDocument2 pagesDrug StudyJanina Patricia BuddleNo ratings yet
- Drug Study - CefradoxilDocument13 pagesDrug Study - CefradoxilJohara G'naid0% (1)
- CececeDocument57 pagesCececeBSRT1A BERBANO, IAN JEWEL M.No ratings yet
- Cefotaxime Drug Class, Uses, Side EffectsDocument3 pagesCefotaxime Drug Class, Uses, Side EffectsKristi WrayNo ratings yet
- Cefazolin AncefDocument4 pagesCefazolin AncefAmanda La SalaNo ratings yet
- CefotaximeDocument3 pagesCefotaximeMargotNo ratings yet
- CefoperazoneDocument3 pagesCefoperazoneBaim FarmaNo ratings yet
- Codiene-Acetaminophen Tylenol 3Document1 pageCodiene-Acetaminophen Tylenol 3Kristi WrayNo ratings yet
- Clopidogrel Bisulfate - PlavixDocument2 pagesClopidogrel Bisulfate - PlavixKristi WrayNo ratings yet
- Cefotaxime Drug Class, Uses, Side EffectsDocument3 pagesCefotaxime Drug Class, Uses, Side EffectsKristi WrayNo ratings yet
- Carvedilol KredexDocument2 pagesCarvedilol KredexKristi WrayNo ratings yet
- Clonazepam KlonopinDocument3 pagesClonazepam KlonopinKristi WrayNo ratings yet
- Aspirin ASA BayerDocument2 pagesAspirin ASA BayerKristi WrayNo ratings yet
- Ciprofloxacin CiproDocument1 pageCiprofloxacin CiproKristi WrayNo ratings yet
- Citalopramhydrobromide CelexaDocument3 pagesCitalopramhydrobromide CelexaKristi Wray100% (1)
- Cefepime MaxipimeDocument2 pagesCefepime MaxipimeKristi Wray100% (1)
- Cefazolin Sodium AncefDocument1 pageCefazolin Sodium AncefKristi WrayNo ratings yet
- Aripiprazole AbilifyDocument2 pagesAripiprazole AbilifyKristi Wray100% (2)
- Adderall medication guideDocument2 pagesAdderall medication guideKristi Wray100% (1)
- Aripiprazole AbilifyDocument2 pagesAripiprazole AbilifyKristi Wray100% (2)
- Baclofen drug profileDocument2 pagesBaclofen drug profileKristi WrayNo ratings yet
- Aloe Vera - ZanzibarDocument2 pagesAloe Vera - ZanzibarKristi WrayNo ratings yet
- Alprazolam Dosage, Uses, Side EffectsDocument2 pagesAlprazolam Dosage, Uses, Side EffectsKristi WrayNo ratings yet
- Amblodipine NorvaseDocument2 pagesAmblodipine NorvaseKristi WrayNo ratings yet
- Albuterol AccunebDocument2 pagesAlbuterol AccunebKristi WrayNo ratings yet
- Albuterol VentolinDocument3 pagesAlbuterol VentolinKristi WrayNo ratings yet
- Adacel Tdap VaccineDocument1 pageAdacel Tdap VaccineKristi WrayNo ratings yet
- Aripiprazole AbilifyDocument2 pagesAripiprazole AbilifyKristi Wray100% (2)
- Tylenol for mild to moderate painDocument2 pagesTylenol for mild to moderate painKristi WrayNo ratings yet
- c20Document7 pagesc20Ravi SinghaniyaNo ratings yet
- Pharma Rcs 2000Document9 pagesPharma Rcs 2000tugi_yonoNo ratings yet
- Senior Director Bioprocess Development in Northern California Resume Venkatesh SrinivasanDocument4 pagesSenior Director Bioprocess Development in Northern California Resume Venkatesh SrinivasanVenkateshSrinivasan1No ratings yet
- ECA Biological Raw Materials ExcipientsDocument6 pagesECA Biological Raw Materials ExcipientsBiopharma GuruNo ratings yet
- Absorption of Drugs From Extravascular RoutesDocument11 pagesAbsorption of Drugs From Extravascular RoutesraviNo ratings yet
- Ers 2015Document358 pagesErs 2015Dejan ŽujovićNo ratings yet
- Bromazepam WikiDocument9 pagesBromazepam WikiAndreea PatrascNo ratings yet
- 2016 - Text Book of Clinical Pharmacognosy Dr. Mansoor Ahmad Karachi UiversityDocument600 pages2016 - Text Book of Clinical Pharmacognosy Dr. Mansoor Ahmad Karachi UiversityAmini Mohammad Humayoon100% (1)
- Chapter 21: Introduction To Pharmacology of CNS DrugsDocument19 pagesChapter 21: Introduction To Pharmacology of CNS DrugsJoslin Roz GalileaNo ratings yet
- Gamefowl Medication GuideDocument2 pagesGamefowl Medication Guidechristine goalsNo ratings yet
- As The CEO of Teva, Which Markets Would You Concentrate On Developing Going Forward?Document12 pagesAs The CEO of Teva, Which Markets Would You Concentrate On Developing Going Forward?mGD1993No ratings yet
- Protokol Kemoterapi WilmsDocument5 pagesProtokol Kemoterapi WilmsrantiadrianiNo ratings yet
- DOSAGE CALCULATIONSDocument7 pagesDOSAGE CALCULATIONSShade ElugbajuNo ratings yet
- KCCLDocument18 pagesKCCLAnonymous v6pZ9s9MNNo ratings yet
- Generic Drugs Assessment and Approval Process in India: Dr. H. G. KoshiaDocument41 pagesGeneric Drugs Assessment and Approval Process in India: Dr. H. G. KoshiaPrasoon MishraNo ratings yet
- Pharma GDPI PrepDocument1 pagePharma GDPI PrepPRAJWAL RASTOGINo ratings yet
- Regulatory Affairs - Pharmaceutical GuidelinesDocument2 pagesRegulatory Affairs - Pharmaceutical Guidelinessandro CardosoNo ratings yet
- Herbal Meds JournalDocument10 pagesHerbal Meds Journalnicole alignoNo ratings yet
- CustomersDocument334 pagesCustomersrajeev_snehaNo ratings yet
- Operational Excellence in The Pharmaceutical - Case StudiesDocument7 pagesOperational Excellence in The Pharmaceutical - Case StudiesSivarami VangaNo ratings yet
- Marketing Plan B6 BioconDocument9 pagesMarketing Plan B6 BioconRitvik DineshNo ratings yet
- Screenshot 2019-12-23 at 17.59.49Document1 pageScreenshot 2019-12-23 at 17.59.49Sunil SoniNo ratings yet
- Micro EmulsionDocument39 pagesMicro Emulsionnazeer hasanNo ratings yet
- Clinical Trials of Drug SubstancesDocument9 pagesClinical Trials of Drug SubstancesMahum SohailNo ratings yet
- BNF GuidelinesDocument6 pagesBNF Guidelineselhassia elhassiaNo ratings yet
- Directorio PTS GranadaDocument68 pagesDirectorio PTS GranadaFundación del Parque Tecnológico de la Salud de GranadaNo ratings yet
- PCP Regulations For Pharm.D ProgramDocument21 pagesPCP Regulations For Pharm.D ProgramAdil YousafNo ratings yet
- PDA Points To Consider For Aseptic ProcessingDocument14 pagesPDA Points To Consider For Aseptic ProcessingKevin ZhaoNo ratings yet
- Phytochemical Pharmacognostical and Physicochemical Standardization of Peperomia Pellucida (L.) Hbk.Document4 pagesPhytochemical Pharmacognostical and Physicochemical Standardization of Peperomia Pellucida (L.) Hbk.ayi-zidaneNo ratings yet