Professional Documents
Culture Documents
Exam 1 Study Guide Module Nursing Art Science
Uploaded by
itschloebOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Exam 1 Study Guide Module Nursing Art Science
Uploaded by
itschloebCopyright:
Available Formats
Exam 1 Study Guide-Module
Chloe Nguyen
1.1- Chapter 1, 2, 3, 4, 6, 11 Discuss nursing as both an art and a science As a professional nurse you will learn to deliver care artfully w/ compassion, caring, and respect for each pt's dignity and personhood. As a science nursing practice is based on a body of knowledge that is continually changing with new discoveries and innovations. Trace the roots of nursing as a profession from ancient to modern times Nurses were nuns from the catholic and Anglican churches. It was started in the Crimean and Civil War. Discuss the contributions of Florence Nightingale as Originator of contemporary nursing- she developed the first organized program for training nurses, the Nightingale Training School for Nursing at St. Thomas hospital in London Pioneer in modern health care principles- Philosophy based on health maintenance and restoration State the definition of nursing according to Virginia Henderson Defines nursing as " assisting the individual, sick or well, in the performance of those activities that will contribute to health, recovery, or a peaceful death and that the individual would perform unaided if he or she had the necessary strength, will, or knowledge. Describe the focus of definitions of nursing The focus is on providing safe, patient-centered health care to the global community. Define the 4 main aims of nursing Promoting wellness-educating and teaching patients about caring for themselves to achieve a healthier lifestyle Preventing illness-helping pts get better whenever they are sick starting with holistically. Nurses main focus is to help the pt to get back to as good as normal health as possible. Trying the least invasive procedures first then more invasive if need be. 1
Restoring health-medicating pts Facilitating coping-rehabilitation. Rehab centers and physical therapy
Discuss nursing as a Discipline-as a nurse you work under an overhead where you have to follow certain policies, rules, and guidelines. You must work within your scope of practice. Profession- to act professionally you administer quality pt-centered care in a safe, conscientious, and knowledgeable manner. You are responsible and accountable to yourself and your pts and peers. List, define, and discuss: Various roles traditional and expanded roles for nurses o a higher level of being a maid And expanded roles would be advocator, caregiver, communicator, and educator. Members of the health care team o Physicians o Physical therapist o Pharmacy o Anyone that come in contact with the that has to do with care of the pt Specialty certification- certification in a specific area of nursing practice. Minimum practice requirements are set, based on the certification the nurse seeks. National nursing organizations such as the ANA have many types of certification to enhance your career such as certification in medical surgical or geriatric nursing. After passing the initial examination, you maintain your certification by ongoing continuing education and clinical or administrative practice. Describe the educational preparation for nursing levels of basic and advanced preparation AA-2 years of basic sciences, theory and clinical courses
BA-4 years of education including basic sciences, theoretical nursing courses, clinical courses, as well as social science, arts, and humanities in supporting nursing theory. Masters- provides advance clinician with strong skills in nursing science and theory with emphasis on the basic sciences and research-based clinical practice. Important degree for the roles of nurse educator and nurse administrator. REQ for advance practice registered nurse (APRN) And doctorate- prepares graduates to apply research findings to clinical nursing. Continuing education-Continuing education involves formal, organized educational programs offered by universities, hospitals, state nurses associations, professional nursing organizations, and educational and health care institutions. An example is a program on caring for older adults with dementia offered by a university or a program on safe medication practices offered by a hospital. Continuing education updates your knowledge about the latest research and practice developments, helps you to specialize in a particular area of practice, and teaches you new skills and techniques In-service education-An in-service program is held in the institution and is designed to increase the knowledge, skills, and competencies of nurses and other health care professionals employed by the institution. Often in-service programs are focused on new technologies such as how to correctly use the newest safety syringes. Many in-service programs are designed to fulfill required competencies of an organization. For example, a hospital might offer an in-service program on safe principles for administering chemotherapy or a program on cultural sensitivity.
Discuss nursing professional organizations American Nurses Association (ANA)-Our union- the body that bargains for us National League for Nursing (NLN)- the body that accredits schools Specialty organizations-Professional nursing organizations deal with issues of concern to specialist groups within the nursing profession. 3
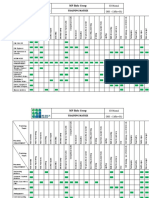
Describe the types of health care settings including Inpatient-acute care/ hospitals Outpatient-dr's office Home care-nursing care provided for pts in their own home Day care-a place where elderly adults can go while their caregivers are busy working Intervention centers- Crisis intervention and alcohol intervention centers Hospice-a service for the terminally ill pts Discuss primary, secondary, and tertiary prevention
Levels
Definition
Examples Health education Smoking cessation Weight loss programs Dental exams etc...
Primary
Activities directed at health promotion Activities directed at diagnosis / prompt intervention Activities directed at rehabilitation
Secondary
Mammograms Prostate exams Colonoscopies Early treatment Rehabilitation services; speech, occupational, physical
Tertiary
Discuss the theoretical basis for nursing practice that has evolved from other disciplines General systems theory-these are made up of separate interrelated components which share a common purpose. We work as a open system- anything external from the body. The chemical reaction within a test tube is a closed system because it does not interact with the environment Change theory4
Adaptation theory- the process through which the patient creates a positive response to the environmental changes. An example is a pt with weakness on the right side learns to use a walker. Developmental theories of Erickson's theory of psychosocial development pg 132
and Maslow hierarchy of needs- page 69 5
Define health and illness across the health Illness continuum o As you go away from the neutral point (equilibrium) you become more sick or well. If you start going to the left you start experiencing signs, then symptoms, then disability, and eventually if not treated, premature death. The more you go to the right of the scale, the healthier you are, starting with being aware of your health and doing something about it, then you educate yourself and then you grow from that and optimally you reach high level of wellness State and define the stages of illness behavior Stage 1- symptoms experiences- something the patient experiences themselves, such as headaches. Stage 2- assumption of the sick role- believing you are sick and acting the part Stage 3- medical center contact-you go to the doctor for further help or self medicate Stage 4- dependent client role- someone takes over your normal roles b/c you are too sick Stage 5- Recovery or rehabilitation- you get better
4.3- Chapter 39 List the functions of the skin Protection Sensation Temperature regulation Excretion and secretion Produces and absorbs vitamin d in conjunction with ultraviolet rays from the sun Factors influencing the skins condition Illness Culture Health state Age Personal preferences
Basic principles that guide practices to skin care Skin is the bodys first line of defense against infections Skin sensitivity to irritation and injury varies among individuals and in accordance with their health. Moisture in contact with the skin for more than a short time can result in bacteria growing Body odor is caused by resident skin bacteria acting on body secretions
Assess the integumentary system and adequacy of self-care of hygiene. Note texture, color, turgor, hydration, temperature, and thickness of the skin, note any lesions, pigmented spots, excoriations or abrasions o A healthy persons skin is smooth, warm, and supple with good turgor. Assess pts. muscle strength, flexibility, balance, visual acuity, and ability to detect thermal and tactile stimuli. o Pts. with limited upper-extremity mobility, reduced vision, fatigue, or inability to grasp small objects will need assistance. 7
o Assess for ROM of the joints o Assess for fatigue and presence of pain and need for analgesics Discuss how personal hygiene practices may vary widely from person to person and culture to culture Different cultures hold different personal ideas about how self care is maintained. Some cultures (western) bath everyday and use deodorant vs cultures in Europe where they bathe less freq and use no deodorant. Identify factors affecting skin condition and personal hygiene Illness Culture Health states- elderly is usually weak Age young and elderly Personal preference
Identify how hygiene is scheduled throughout the day in a hospital setting Early AM-getting the pt ready for breakfast, any scheduled test or early morning surgery. RN offers bedpan or urinal if pt isnt ambulatory, washing the pts hand and face, and assisting with oral care. Morning Care-after breakfast, offer bedpan or urinal to pts confined to bed, PROVIDE BATH or SHOWER, incl. perineal care and oral, foot, nail, and hair care, give back rub, change pts gown or pajamas, change bed linens, and straighten pts bedside unit. AKA Complete AM care. Afternoon care-incl. washing of the hands and face, assisting with oral care, offering bedpan or urinal and straighten bed linen HBS Care (hour before sleep) (PM care)-help pt relax and promote sleep. Often incl changing of soiled linens, gowns or pajamas, helping pts wash the face and hands, provide oral care, give back massage (rub downwards; shoulders down), offer bedpan or urinal. 8
Some pts enjoy a beverage before bed such as juice; check diet to determine which beverage is allowed. Describe the priorities of scheduled hygienic care A Pts condition influences your priorities for hygiene care. Seriously ill pt usually needs a daily bath bc body secretions accumulate and the pt is unable to perform hygiene care for themselves. A pt with incontinence may need perineal care with every episode of soiling. Plan for necessary assistance for pts who are weakened and possess poor coordination. Timing is also important. Being disrupted in the middle of a bath often frustrates and embarrasses the pt.
Distinguish between the different classifications of hygiene assistance required Self-care- Pt is able to do things on their own. Youre there to mostly supervise and help with heading them things if needed. Partial care-Bed bath that consists of bathing only body parts that would cause discomfort if left unbathe such as the hands, face, axillae, and perineal area. Partial bath may also include washing back and providing back rub. Provide a partial bath to dependent patients in need of partial hygiene or self-sufficient bedridden patients who are unable to reach all body parts. Complete care- bath giving to totally dependent pts in bed
List the purposes of bathing Cleanses skin Skin conditioner Relaxation Promote circulation Musculoskeletal exercise Promote comfort Sensory input improves self image Nurse / pt relationship (communication enhancer) 9
Health care teaching Assessment
Identify the nursing responsibilities involved in hygiene care regarding: tub or shower baths for ambulatory patients-reqs a more thorough washing and rinsing than a bed bath. Pt still needs nurses assistance. Some facilities have lifting devices to help position dependent patience safely in the bath. bed baths for self-care patients- help pts with whatever they need such as gathering supplies and handing them things but allow them to do it on their own to promote independence. bed baths for partial-care patients- help pt with hard to reach areas. Remember to wear gloves if coming in contact with body fluids. Practice safety and privacy for pt at all times
Identify the aspects of oral care for both Conscious patients-make sure they take out denture before oral care if there are any. Brush the teeth and rinse mouth with mouth rinse. Unconscious patients- position in semi fowlers position and check for gag reflex. Let pt know what you are doing at all times. Make sure to suction water so that the pt doesnt drown.
Identify aspects of care of dentures Handle dentures with care because they break easily and theyre expensive. They should be removed at night so the gums can rest and prevent bacteria buildup. The dentures should be brushed, flossed and placed in a labeled solution filled container placed in the bedside drawer away from the table top where someone can knock them over. Rinse mouth and dentures after meals to prevent denture-induced stomatitis.
State technique for care of the eyes 10
Wash eyes with a clean moist washcloth. NO SOAP. Wiping from the inner canthus to the outer canthus. Unconscious pts need more frequent eye care because they secretions usually collect along the edge of the eye when the blink reflex is absent. If the eye doesnt close completely place, an eye patch over the eye to prevent corneal drying and irritation. Apply lubricating eye drops according to the HCPs orders.
Discuss technique and legal aspects for care of the hair Need physicians order to shampoo and cut Shaving- consider personal preferences Nails- physicians order to cut toenails. Some gender depending on their culture only one same gender nurses to assist them
Discuss technique and psychological aspects for care of the perineal area for males and females Always remember to assess for irritation, excoriation, inflammation, swelling, excessive discharge, odor, pain or discomfort, presence of urinary or fecal incontinence, recent rectal or perineal surgery, presence of indwelling catheter, perineal-genital hygiene practices, self-care abilities o Each pt might prefer a same sex nurse to provide perineal care for them. o Provide privacy is a priority when performing perineal care. o For males. If the pt is uncircumcised retract the foreskin and clean the meatus and REMEMBER to return the foreskin or else it will result in circulation being cut off and can cause gangrene and then the amputation of the penis o For females. As a nurse you should wash the least contaminated to the most contaminated area. Front to back. Identify nursing responsibilities for the care of a patient with Thrombo Embolic Deterrent Stockings (TEDS) Reqs physician order 11
Measure for proper fit Apply with pt laying down Do NOT massage leg Check heel position Loosen toes Remove q shift for 30 mins Launder prn/ re-use
Discuss the implications of the back rub To help with relaxation, circulation, touch is important, gives nurse a chance to check the skin for breakdown. Lotion is used. No more than 3-5 mins to complete. Nurses arent allowed to do back rubs anymore. Its only ok to relax the pt for a couple minutes. Only stroke from top of the shoulder down is allowed.
Identify safety features of a typical hospital bed Position changes Safety features- 2 rails, controls, locks, brakes Mattresses specialty, pressure reducing, air mattress overlays, etc
State guidelines for bed making for both Unoccupied beds-pt is out of bed. o Use gloves to remove the soiled linen. Hold away from your body. o Place linen in linen hamper o Remove gloves and make the clean bed. o Make sure there are not creases Identify Occupied beds- pt is in bed the components of a bedside unit Bed Overbed table Bedside table
State the elements of a safe bedside unit 12
Call light in reach Bed in lowest position, brakes LOCKED Side rails up, 2 upper if possible o Any more than 2 needs a doctors order Uncluttered walkway Personal items in reach so pt doesnt try to reach for something they need and fall over and hurt themselves
Develop nursing diagnoses related to deficient hygiene measures Activity intolerance Bathing self-care deficit Dressing self-care deficit Impaired physical mobility Impaired oral mucous membrane Ineffective health maintenance Risk for infection
13
2.4- Chapter 28 Explain the relationship of the chain of infection to the transmission of infection If the chain of infection is uninterrupted the transmission of infection has a higher chance to becoming an infection. Discuss the six components of the chain of infection Infectious agent-are microorganisms such as bacteria, viruses, fungi, and protozoa. Reservoir-is a place where the microorganisms survive, multiply, and await to transfer to a susceptible host. Portal of exit- these incl blood, skin, and mucous membranes, respiratory tract, genitourinary tract, gastrointestinal tract, and trans placental. Mode of transmission-is the way a microorganism is transferred such as airborne, droplet, or contact. They can also be transferred indirectly through inanimate objects (needles or sharp objects, dressings, environment), vehicles (water, drugs, solutions, blood, food), and vectors (mosquito, louse, flea, and tick). Portal of entry- the organisms can enter the same routes they used for exiting. Host- if the hosts immune system is compromised the pt will be susceptible to being infected. It depends on the degree of the infection and how the pts immune system is.
Describe nursing interventions used to break the chain of infection HAND HYGIENE!! Esp for c diff and neutropenic infection- low wbc Alcohol base Identify patients at risk for developing an infection and the bodys normal defenses against infection Age- the very young and the very old Hereditary Those who are physically and emotionally stressed Nutritional status Medical therapy 14
Diagnostic procedures Medications Disease process
Identify factors that reduce the incidence of nosocomial infection Meticulous hand hygiene Use of chlorhexidine washes Identify situations in which hand washing is indicated ALL the time! When your hands are soiled. When dealing with immune compromised pts such as neutropenia pts and chemo or cancer pts the components of proper hand washing Control the water, as warm as you can stand Wet hand Get soap Lather for a good 15 seconds Rinse with finger pointing down Wipe hand with a dry paper towel from fingers to wrist and discard when it hits the wrist and grab another towel to finish drying off hands Use a dry towel to turn faucet off
Identify
Discuss normal flora that are found on the hands Transient bacteria- It is bacteria that it is in the surface of the skin and therefore come and goes as we touch things and as we move around. Resident flora- encompasses a wide variety of microorganisms, and the interactions between microbes and host creates a mutualistic relationship that both entities benefit from
Identify nursing diagnoses associated with a patient who has an infection or is at risk of developing an infection Risk for infection 15
Imbalanced nutrition: less than body requirements Impaired oral mucous membrane Risk for impaired skin integrity Social isolation Impaired tissue integrity Readiness for enhanced immunization status
Differentiate between types of techniques and protocols for isolation Contact precautions: Used for direct and indirect contact with patients and their environment. Direct contact refers to the care and handling of contaminated body fluids. An example includes blood or other body fluids from an infected patient that enter the health care worker's body through direct contact with compromised skin or mucous membranes. Indirect contact involves the transfer of an infectious agent through a contaminated intermediate object such as contaminated instruments or hands of health care workers. The health care worker may transmit microorganisms from one patient site to another if hand hygiene is not performed between patients Droplet precautions: Focus on diseases that are transmitted by large droplets expelled into the air and travel 3 to 6 feet from the patient. Droplet precautions require the wearing of a surgical mask when within 3 feet of the patient, proper hand hygiene, and some dedicated-care equipment. An example is a patient with influenza. Airborne precautions: Focus on diseases that are transmitted by smaller droplets, which remain in the air for longer periods of time. This requires a specially equipped room with a negative air flow referred to as an airborne infection isolation room. Air is not returned to the inside ventilation system but is filtered through a high-efficiency particulate air (HEPA) filter and exhausted directly to the outside. All health care personnel wear an N95 respirator every time they enter the room. Protective environment: Focuses on a very limited patient population. This form of isolation requires a specialized room with positive airflow. The airflow rate is set at greater than 12 air exchanges per hour, and all air is filtered through a HEPA filter. 16
Patients are not allowed to have dried or fresh flowers or potted plants in these rooms When using the isolation guidelines of the CDC, refer to additional CDC documents to prevent health careassociated aspergillosis and Legionnaires disease in immunocompromised patients and the spread of multidrug-resistant organisms Regardless of the type of isolation system, follow these basic principles: o Use thorough hand hygiene before entering and leaving the room of a patient in isolation. o Dispose of contaminated supplies and equipment in a manner that prevents spread of microorganisms to other persons as indicated by the mode of transmission of the organism. o Apply knowledge of a disease process and the mode of infection transmission when using protective barriers. o Protect all persons who might be exposed during transport of a patient outside the isolation room.
Identifying equipment needed and nursing responsibilities for each standard Precautions (Tier One)- always don gloves transmission Categories (Tier Two)o Airborne precautions-always don N95 measles, chickenpox (varicella), disseminated varicella zoster, pulmonary or laryngeal TB o Droplet precautions- always don mask Diphtheria (pharyngeal), rubella, streptococcal pharyngitis, pneumonia, or scarlet fever in infants and young children, pertussis, mumps, Mycoplasma pneumonia, meningococcal pneumonia or sepsis, pneumonic plague. o Contact precautions- always don gloves and gown Varicella zoster disseminated MRSA VRE C diff 17
Reverse or protective isolation: Discuss the psychological implications of isolation for the patient Reverse isolation is when I protect myself from the patient Protective isolation is when I protect the pt from me. o Private room; positive airflow with 12 or more air exchanges per hour. HEPA filtration for incoming air. o Some psychological implications of isolation for the pt are Pt can feel lonesome bc normal social relationships are disrupted This can be psychologically harmful, esp for children. These pts suffer more depression and anxiety and were less satisfied with their care
Describe techniques for medical and surgical asepsis Medical is a cleaning technique Surgical is when you want absence of all organisms for surgery or invasive procedures etc
Define medical and surgical asepsis Medical asepsis- technique to reduce or prevent the spread of microorganisms. Objects referred to as clean ( Absence of ALMOST ALL microorganisms). Surgical asepsis-technique that keeps an area or object FREE from ALL microorganisms. Objects are referred to as STERILE ( absence of microorganisms) Identify areas and occasions when surgical asepsis is used Used in procedures involving sterile areas of the body. o OR o Labor and delivery rooms o And when inserting IV and catheters o And special diagnostic areas GI prep 18
State the nurses responsibility in maintaining sterility Anticipate patient sneezing so offer them a mask Patient prep Ask the pt about toileting Not to talk, sneeze, etc while setting up a sterile field
List the principles of sterile technique and state the rationale for each Sterile object touches only sterile object o Bc non sterile objects are contaminated Only sterile object placed on sterile field o Bc any other item is contaminated when wet, open, or punctured Sterile object or field out of range of vision or below waist is contaminated o Nurses should never turn their back to a sterile field bc you never know what could have fell into the sterile field while you were not looking. Any thing below the waist is contaminated because it cannot be viewed at all times Sterile object or field contaminated by prolonged exposure to air o Microorganisms can travel by droplet through the air into the area of the sterile field. o Do not cough, laugh, or sneeze when preparing a sterile field Sterile surface comes in contact with wet, contaminated surface is contaminated o Can contaminate other sterile objects in the field via capillary action. Fluid flows in direction of gravity o To avoid contamination during a surgical hand scrub, hold your hands above your elbows. This allows water to flow downward without contaminating your hands and fingers. Edges of sterile field contaminated (1 inch) o Because it is exposed to the air after being opened
19
State the techniques for Handling sterile objects o Sterile object touches only sterile object o Only sterile object placed on sterile field o Sterile object or field out of range of vision or below waist is contaminated o Sterile object or field contaminated by prolonged exposure to air o Sterile surface comes in contact with wet, contaminated surface is contaminated o Fluid flows in direction of gravity o Edges of sterile field contaminated Pouring sterile solutions o Pour over the sterile field not too far up but not to close to the sterile field to contaminate it o Hold the bottle outside the edge of the sterile field o Label is always faced up so that you dont get solution on the label and deface it Opening and adding sterile supplies to a sterile field o Open with both hand while still holding the sterile supplies in the wrapper that it came in and drop it into the sterile field carefully to not knock it off or spill anything.
20
2.2- Chapter 29 State the components that constitute vital signs. Temperature (96.8-100.4F) Pulse (60-100 beats) Respirations (12-20 breaths/min) Blood pressure (100/60-119/79 mmhg) Pain (0-10) subjective Oxygen saturation (95-100 SpO2) Discuss parameters for frequency of vital-sign measurement. Upon admission (as part of physical exam) Routine schedule in a hospital Before & after surgical/diagnostic procedures Before, during & after blood administration Before & after certain medications Changes in a patients physical condition Before & after interventions that influence VS Subjective complaint Gather a baseline
Identify the nurses responsibility for vital-sign measurement Nurse assigned to client is responsible not the UAP Nurse should make sure equipment is functional and appropriate for accurate assessment Evaluate against pts baseline vs standard book values To help make intervention as needed Make sure the equipment is correct size Check medications that pt is taking Control external factors Document any major changes
Discuss body temperature How temperature is regulated o Hypothalamus controls the body temp Anterior hypothalamus controls heat loss 21
Posterior hypothalamus controls heat production Methods of heat loss o Radiation-transfer of heat between two objs WITHOUT physical contact o Conduction- transfer of heat WITH physical contact o Convection- transfer of heat away by air movement o Evaporation-transfer of heat energy when liquid (sweat) is turned in to gas Methods of temperature measurement o Orally- make sure pt hasnt smoke, ate, or drank anything in the last 15 minutes o Axillary- make sure the site is dry o Rectally- remember to LUBERCATE the probe. Only go in 11.5 inch o Temporallyo Tympanic-for adults pull pinna backward, up, and out point probe towards midline between eyebrow and side burns. For kids older than three, pull pinna up and back. Locations o Mouth o Underarm o Anus o Forehead o Ears Equipment o Glass thermometers o Electronic thermometers o Electronic tympanic thermometers o Disposable thermometers-sweat impairs adhesion Contraindications o Oral Contraindicated in infants, small children, or confused, unconscious, or uncooperative pts Contraindicated following oral surgery, trauma, history of epilepsy, or shaking chills o Rectal 22
Contraindicated in newborns and other conditions Expected values at each location o Oral & tympanic 98.6F (37C) o Rectal 99.5F (37.5C) o Axillary 97.7F (36.5C)
Recognize the terms associated with temperature Febrile-with fever Afebrile-without fever Pyrexia- Fever 100.4F due to infectons; pyrogens Hyperpyrexia-elevation of the body temp above 106F Hyperthermia-100.4F due to external factors Hypothermia-decreased body temp Malignant hyperthermia- a hereditary condition of uncontrolled heat production
Discuss basic information related to the patients pulse Physiology of the pulseo Arterial walls expand each time left ventricle contracts to eject blood into the aorta o Expansion can be felt as an artery travels over a bony prominence, called a pulse Developmental changes associated with normal pulse rate o Babies have a faster pulse at 100-160 beats/min o Males have a slower rate than females o People who are thin have a slower rate o Increased age may be associated with a slower pulse Terms associated with pulse including o Tachycardia- Rapid beating >100 o Bradycardia- Slow beating <60 Factors that will increase pulse rate o Medications o Pain 23
o Strong emotions (fear, anger, anxiety, or surprise) o Exercise o Application of heat for a long period o Decreased in BP o Elevated temperature o Any condition resulting in poor oxygenation or blood Decrease pulse rate o Some meds digoxin o Person just woke up or is resting o People who are thin o Older people o Males have slower rates than females Characteristics of pulse including o Rhythm-is the pattern of the pulsations and the pauses between them o Amplitude Reflects the volume of blood ejected against the arterial wall with each contraction and the condition of the arterial vascular system leading to the pulse site May be graded or described as strong, weak, thready, or bounding 0 Absent pulse or not felt 1+ Thready/Weak, not easily felt, slight pressure occludes it 2+ Normal 3+ Bounding, stronger than normal e.g. after increased activity
Assessment sites temporal-side of forehead carotid-side of neck, under chin apical- between 4th and 5th intercostal space radial-at wrist on thumb side brachial-in the antecubital space femoral- groin area popliteal behind the knee 24
posterior tibia- ankle area dorsalis pedis-top of foot, towards the inside
Apical-radial pulse assessment Method o Locate the mitral valve loudest sound S1 at 4th and 5th intercostal space mid-clavicular line o Count with a stethoscope for 60 seconds Indications as to when to take apical pulse o When the radial pulse is irregular. o When knowing the central pulse is essential for treatment/meds (i.e. Digoxin). o To determine presence of pulse deficit (2 nurses count at same time, using same watch). Pulse deficit- the difference between the radial and the apical pulse
Discuss respirations Physiology of respirations o Movement of air in and out of lungs o CO2 -out and O2 -in Developmental changes associated with the normal respiration rate o Children seem to breath faster than adults Factors that will increase or decrease respiratory rate o Exercise (I) o Acute pain (I) o Anxiety (I) o Smoking (I) o Body positions (I) (D) o Medications Opioids, analgesics, general anethetics and sedative hypnotics DEPRESS rate and depth Amphetamines and cocaine sometimes INCREASE rate and depth Bronchodilators DECREASE rate by causing airway dilation 25
o Neurological injury- impairs respiratory center and inhibits respiratory rate and rhythm o Hemoglobin function Decreased hemoglobin levels (anemia) increase respiratory rate because of the reduced oxygen carrying capacity of the blood. Increased altitude lowers the amt of saturated hemoglobin which increases the respiratory rate and depth Abnormal blood cell function (sickle cell disease) reduces the ability of hemoglobin to carry oxygen which increases respiratory rate and depth. terms associated with respiration o Apnea- without breath o Dyspnea- difficulty breathing o Orthopnea- difficulty breathing when laying down o Tachypnea-rapid breathing o Bradypnea-slow breathing o Cheyne-Stokes- The pattern of breathing with gradual increase in depth and sometimes in rate to a maximum, followed by a decrease resulting in apnea; the cycles ordinarily are 30 seconds to 2 minutes in duration, with 530 seconds of apnea Discuss blood pressure Terms associated with blood pressure o Systolic pressure- Maximum pressure is exerted upon left ventricular contraction or systole, thus the highest pressure is the systolic measure o Diastolic pressure- When the heart rests between beats the pressure is at its lowest point and is referred to as the diastolic measure o Pulse pressure-the difference between systolic and diastolic measurements. Eg: BP 120/80 = pulse pressure of 40 o Hypertension-asymptomatic; most common alteration in BP 26
Dx in adults: when 2 or more readings on at least 2 subsequent visits indicates diastolic pressure > or =90 mmhg or systolic pressure > or =140 mmhg Prehypertension- systolic is between 120-130 or diastolic is between 80-89 Stage 1 systolic is between 140-159 or diastolic is between 90-99 Stage 2- systolic is >160 or diastolic is>100 o Hypotension-systolic falls below 100 or lower Symptoms: pallor, skin mottling, clamminess, confusion, dizziness, chest pain, increase HR, and decreased urine output Life threatening o Orthostatic (postural) hypotension- low blood pressure assoc. with weakness or fainting when one rises to an upright position (sitting or standing) o Factors responsible for maintaining blood pressure Medication Exercise Diet o Factors responsible for deviations of blood pressure Disease Race Gender Stress Age Time Obesity o Contraindications for site selection Usually, one should avoid obtaining a blood pressure in the same arm in which an arteriovenous fistula (such as used in hemodialysis) is present, or where lymphadema exists or if there has been a mastectomy done. Furthermore, caution should be used if the patient is at high risk for developing lymphedema (such as after lymph node dissection for treatment of breast cancer). 27
In these instances, using the other arm is recommended; if bilateral arteriovenous fistulas or lymphedema exist, then obtaining a lower extremity blood pressure is recommended 2.3- Chapter 30 Describe the purpose of nursing history and physical assessment Gather baseline data about the clients health status Supplement, confirm, or refute data obtained in the nursing history Confirm & identify nursing diagnoses Make clinical judgments about a clients changing health status & management Evaluate the physiological outcomes of care
Discuss psychological and physical preparation of the patient. Psychological Preparation Tips: o Provide an explanation regarding the purpose and steps of the examination o Use simple, understandable terms o Encourage client questions o Inform client to tell you if there is any discomfort o Professional yet relaxed demeanor o Observe for client emotional responses Physical Preparation Tips: o Comfort for client is essential o Before beginning assessment ask client if they need to use the toilet o Client is dressed & draped appropriately o Provide privacy for the examination o Use towels & linens to drape client for privacy as well as warmth o Frequently inquire about client comfort List and describe the four primary assessment techniques Inspection-youre assessing the pt by looking at them 28
Palpation-uses the sense of touch. Youre feeling for any abnormalities Percussion-involves tapping the body with the fingertips to evaluate o Size o Borders o Consistency of body organs o Fluid filled cavities Auscultation- act of listening to sound produced by the body o With or without stethoscope
Discuss the components of the general overview Should include the following o Sex & race o Body build, posture & gait, movements o Hygiene & grooming, dress o Signs of illness o Affect: attitude, mood, speech o Cognitive status (orientation, memory) o VS, weight & height Identify the techniques, anatomy, and expected findings of the basic physical assessment of the adult patient, system-by-system, head-to-toe. Skin: define and discuss Flushing-reddened appearance of the skin Cyanosis-blueness of the skin- increased amt of deoxygenated Hgb ( assoc w/ hypoxia) Jaundice-yellow/orange color change as a result of increased bilirubin in tissue Pallor-decrease in color, reduced amt of oxyhemoglobin, may be due to anemia or shock Ecchymosis-(bruise) collection of blood in the tissue Petechiae-small red ecchymotic changes that occur due to capillary rupture in the dermis Turgor-the fullness or elasticity of the skin and is usually assessed on the sternum or under the clavicle. 29
Diaphoresis-(sweating) when the entire skin is moise (usually cool in temp as well) Edema-characterized by swelling, with taut and shiny skin over the edematous area. Nails- should be 160 degrees and no more than that Head o Hair and scalp- should have not masses, depressions, or lesions o Ears- pinna shouldnt be lower than eye level; if it is lower and has a deviation in alignment it can be a form of down syndrome Face- should be symmetrical, with some slight deviations but not major. Bells palsy will be a major deviation o Check sinuses Nose- check smell CN 1. Check for patency- one nostril at a time. Eyes, identify o PERRLA- Pupil, Equal, Round, Reactive to Light, Accommodating o EOM- extra ocular muscle Neck o o o Convergence Assess: ROM Lymph nodes- check for any masses that are palpable usually lymph nodes arent palpable Trachea- listen for breathe sounds and adventitious soundstrachea will have bronchial sounds Carotid pulse- assess the pulse one at a time Listen to the pulse with the bell and diaphragm to
assess any bruits Chest-check ap diameter, note any masses or bulging or retraction of ICS Lungs: define: o Normal breath sounds: o Bronchial sounds- should be around neck and trachea region; high pitch, long and loud expiration 30
o Bronchovesicular- heard over major bronchi and over upper right posterior lung field; moderate in pitch and intensity. Inspiration=Expiration o Vesicular- over entire lung field, heard over lesser bronchi, bronchioles, and lobes; low pitch, low intensity, soft and short expiration o Adventitious Crackles-heard during inspiration. Discontinuous. High pitch. The cause is the random and sudden inflation of groups of alveoli. Disruptive passage of air through small airways Rhonchi- heard on insp and expiration. Rumbling course sound, like a snore. Mainly heard over trachea and bronchi. If loud enough it can be heard over lung fields. Cleared with cough. Continuous. o When auscultating lung fields The vesicular lung sounds is the only one to be heard when assessing it laterally. Heart. Locate and discuss: listen with bell and diaphragm o S1lub- is the sound of mitral and tricuspid valves closing. Mitral is located between 4th and 5th Intercostal space midclavicular Tricuspid is at the 4th intercostal space left of sternum o S2dub- the sound of the pulmonic and aortic valves closing Aortic is located at the 2nd intercostal space to the right of the sternum Pulomonic is located at the left side 2nd intercostal space left of sternum Auscultation sites for aortic valve- right of sternum 2nd intercostal space, pulmonic valve- left of sternum 2nd intercostal space, tricuspid valve- left of sternum 4th ICS , and mitral valve 5th ICS midclavicular o Erbs point-3rd ICS left of sternum o PMI- between 4th and 5th intercostal space midcalvicular o Apex-5th intercostal space o Breasts31
o Axillao Abdomen- aortic, renal, iliac, and femoral regions o Bowel sounds- LR, UR, UL, LL Pain assessment of the abdomeno Pattern of characteristics of pain help determine source. o If pt has tender areas- assess those areas last Detecting ascitesGenitaliao Male Remember to return the foreskin to original position to prevent phimosis o Female Know Gravida- number of pregnancies Parity- number of births MusculoskeletalNervousPeripheral vascular- Assess the pulse points for similar rhythm and rate. Check bilaterally.
Identify common abnormal findings associated with each system
Discuss the documentation of findings in narrative nursing notes format, identifying acceptable terminology and abbreviations and following head-totoe forma
32
1/14/2013 6:14:00 PM
33
You might also like
- Evolution of Nursing BulletsDocument3 pagesEvolution of Nursing Bulletstorque15100% (1)
- Periods of Nursing HistoryDocument38 pagesPeriods of Nursing HistoryJeny Pearl Hijosa0% (1)
- History of World NursingDocument62 pagesHistory of World Nursingmikmik006No ratings yet
- Fundamentals of NursingDocument44 pagesFundamentals of Nursingtheglobalnursing100% (2)
- Fundamentals of NursingDocument2 pagesFundamentals of NursingIann Reuben Favie RosalNo ratings yet
- A Spiritual History of NursingDocument9 pagesA Spiritual History of NursingMarimiel Pagulayan100% (1)
- Evo of NursingDocument5 pagesEvo of NursingFrancis ObmergaNo ratings yet
- History of NursingDocument13 pagesHistory of NursingEileenAquinoMacapagal100% (1)
- Fundamental's FinalDocument21 pagesFundamental's FinalShaunn Diesto Caberto100% (1)
- Presented By: Anjani.S.Kamal 1 Year MSC (N)Document23 pagesPresented By: Anjani.S.Kamal 1 Year MSC (N)shubham vermaNo ratings yet
- Nursing ProcessDocument12 pagesNursing Processgrey26No ratings yet
- Medical Surgical Nursing Review 1Document31 pagesMedical Surgical Nursing Review 1jeshemaNo ratings yet
- Fundamentals of Nursing (Part 1)Document11 pagesFundamentals of Nursing (Part 1)Louie ParillaNo ratings yet
- Manila's First Hospital Nursing SchoolDocument21 pagesManila's First Hospital Nursing Schooljaelrian jaelrianNo ratings yet
- History of Nursing (Part 1)Document56 pagesHistory of Nursing (Part 1)Joseph TheThirdNo ratings yet
- Incontinence Case StudyDocument26 pagesIncontinence Case StudyRose AnnNo ratings yet
- Scope and Practice of Emergency With LectureDocument34 pagesScope and Practice of Emergency With LectureArvie ReyesNo ratings yet
- Health Assessment Intro, Nsg. Process, Interviwe, RosDocument216 pagesHealth Assessment Intro, Nsg. Process, Interviwe, RosHyacinth Jane Dela PeñaNo ratings yet
- Vital Signs: Carol Mitchell, RN, MSNDocument56 pagesVital Signs: Carol Mitchell, RN, MSNokaciaNo ratings yet
- History of NursingDocument2 pagesHistory of NursingalexNo ratings yet
- Cardiovascular System: By: Marc Anthony Liao RNDocument59 pagesCardiovascular System: By: Marc Anthony Liao RNloveseeker06No ratings yet
- Test BankDocument6 pagesTest BankKazama SmithNo ratings yet
- Bio 235 Midterm 1 NotesDocument53 pagesBio 235 Midterm 1 NotesNita JosephNo ratings yet
- StatementDocument5 pagesStatementtrinity_brannonNo ratings yet
- Professional Adjustment Final 2Document41 pagesProfessional Adjustment Final 2lielani_martinezNo ratings yet
- Fundamentals of Nursing: Definitions, History, RolesDocument35 pagesFundamentals of Nursing: Definitions, History, RolesJesler ChioNo ratings yet
- Anatomy Reproductive SystemDocument8 pagesAnatomy Reproductive SystemjisooNo ratings yet
- References: NCSBN's Review For The NCLEX-PN ExaminationDocument5 pagesReferences: NCSBN's Review For The NCLEX-PN Examinationbapimirab6540% (1)
- Chapter 26Document46 pagesChapter 26meeeenonNo ratings yet
- Period of Nursing in History of Nursing NewDocument258 pagesPeriod of Nursing in History of Nursing NewAnonymous aqeaNUn100% (1)
- History of Nursing PDFDocument21 pagesHistory of Nursing PDFFouziaShahzad100% (3)
- Nursing ResumeDocument3 pagesNursing Resumeapi-430800277No ratings yet
- Fragile X SyndromeDocument11 pagesFragile X SyndromeMartinNo ratings yet
- Maternal Ob NotesDocument103 pagesMaternal Ob NotesBoris OrbetaNo ratings yet
- Nursing in EmergenciesDocument5 pagesNursing in EmergenciesAvisheel KalsiNo ratings yet
- Nursing Documentation's Legal ImportanceDocument52 pagesNursing Documentation's Legal ImportanceAlyssa Azucena100% (1)
- Clinical ExemplarDocument5 pagesClinical Exemplarapi-252750576No ratings yet
- Fundamentals in NursingDocument9 pagesFundamentals in NursingWendy EscalanteNo ratings yet
- Health AssessmentsDocument76 pagesHealth AssessmentsAtashia Rain GaguiNo ratings yet
- Fundamentals of Nursing p.1-37Document38 pagesFundamentals of Nursing p.1-37Wik Wik PantuaNo ratings yet
- Chapter 20: Postpartum Physiologic Changes Lowdermilk: Maternity & Womens Health Care, 11th EditionDocument11 pagesChapter 20: Postpartum Physiologic Changes Lowdermilk: Maternity & Womens Health Care, 11th EditionNurse UtopiaNo ratings yet
- Chapter 18: Nursing Management of The NewbornDocument37 pagesChapter 18: Nursing Management of The NewbornJ15No ratings yet
- Think Nursing! ReportDocument20 pagesThink Nursing! ReportRobert Fraser RNNo ratings yet
- Diagnosis Schizophrenia 2Document1 pageDiagnosis Schizophrenia 2Bukola OgunnaikeNo ratings yet
- Philosophy of NursingDocument8 pagesPhilosophy of Nursingapi-430575435No ratings yet
- Np1 - Fundamentals of Nursing: Nursing During The Philippine RevolutionDocument48 pagesNp1 - Fundamentals of Nursing: Nursing During The Philippine RevolutionKate TergaNo ratings yet
- ActiveLearningTemplate SysdisDocument1 pageActiveLearningTemplate SysdisCovey delacruzNo ratings yet
- Cardiac FT: ResultsDocument26 pagesCardiac FT: ResultsBillynTarplainNo ratings yet
- Fundamentals of Nursing History and EvolutionDocument38 pagesFundamentals of Nursing History and EvolutionDane RamosNo ratings yet
- Ne 35 4 2010 04 16 Smith 200117 SDC1Document28 pagesNe 35 4 2010 04 16 Smith 200117 SDC1Agung NohuNo ratings yet
- Pre Hos TraumaDocument11 pagesPre Hos TraumaGel OmugtongNo ratings yet
- Care and Management of The Client With Cardiac Alterations: Presented By: Jessaly Joyce SiosonDocument38 pagesCare and Management of The Client With Cardiac Alterations: Presented By: Jessaly Joyce SiosonJoyce SiosonNo ratings yet
- Pharmacology Test 1: Questions and RationalesDocument52 pagesPharmacology Test 1: Questions and RationalesElla ReyesNo ratings yet
- 5395 Nursing DesertationDocument35 pages5395 Nursing Desertationdouglas gacheru ngatiiaNo ratings yet
- Disaster NursingDocument9 pagesDisaster NursingKimberly Louise LopezNo ratings yet
- Nursing Final BookDocument137 pagesNursing Final BookJagdish RajanNo ratings yet
- Main drug therapy for ulcerative colitis is sulfa for one yearDocument4 pagesMain drug therapy for ulcerative colitis is sulfa for one yearcathyNo ratings yet
- NURSING CARE OF ADULTS II: Passbooks Study GuideFrom EverandNURSING CARE OF ADULTS II: Passbooks Study GuideNo ratings yet
- COMPREHENSIVE NURSING ACHIEVEMENT TEST (RN): Passbooks Study GuideFrom EverandCOMPREHENSIVE NURSING ACHIEVEMENT TEST (RN): Passbooks Study GuideNo ratings yet
- Greek MathemaDocument6 pagesGreek MathemaSebastian GhermanNo ratings yet
- RUDDER PLATING DIAGRAMDocument1 pageRUDDER PLATING DIAGRAMMuhammad Ilham AlfiansyahNo ratings yet
- 72 Names of God in HasidimDocument16 pages72 Names of God in HasidimFrancesco VinciguerraNo ratings yet
- Audit Reveals Optimization Opportunities for Cement Ball Mill SystemDocument19 pagesAudit Reveals Optimization Opportunities for Cement Ball Mill SystemVijay Bhan100% (2)
- AREADocument10 pagesAREAhaipm1979No ratings yet
- World Ranking For Industrial Trucks DHF 2015Document2 pagesWorld Ranking For Industrial Trucks DHF 2015MA TotalforkliftNo ratings yet
- Elcometer Wet-Film Gage 115 Spec SheetDocument2 pagesElcometer Wet-Film Gage 115 Spec SheetMary CasillasNo ratings yet
- Reference UMDNS Codes PDFDocument69 pagesReference UMDNS Codes PDFPumps RnDNo ratings yet
- Experimental Validation of The BAC Factor Method For Lighting SystemsDocument5 pagesExperimental Validation of The BAC Factor Method For Lighting SystemsJireh AngNo ratings yet
- Assignment 1 Systems Analysis - EME5601Document7 pagesAssignment 1 Systems Analysis - EME5601Travis GrantNo ratings yet
- Minicap FTC260, FTC262: Technical InformationDocument20 pagesMinicap FTC260, FTC262: Technical InformationAmanda PorterNo ratings yet
- Dr. Kumar's Probability and Statistics LectureDocument104 pagesDr. Kumar's Probability and Statistics LectureAnish KumarNo ratings yet
- MP Birla Group: Training MatrixDocument3 pagesMP Birla Group: Training MatrixAprilia kusumaNo ratings yet
- Estudio CarmenaDocument11 pagesEstudio CarmenaAlfredo BalcázarNo ratings yet
- IMG - 0092 PSME Code 2012 90Document1 pageIMG - 0092 PSME Code 2012 90Bugoy2023No ratings yet
- IOM Paquetes DX Precedent RT-SVX22U-EN - 03072018Document82 pagesIOM Paquetes DX Precedent RT-SVX22U-EN - 03072018Mario Lozano100% (1)
- Eko 75 Spare Part ListDocument23 pagesEko 75 Spare Part ListРустам Хайретдинов100% (1)
- 02 - AFT - Know Your Pump & System Curves - Part 2ADocument8 pages02 - AFT - Know Your Pump & System Curves - Part 2AAlfonso José García LagunaNo ratings yet
- BS en 10108-2004Document14 pagesBS en 10108-2004Martijn GrootNo ratings yet
- Heidegger On Destruction - Chung ChinDocument16 pagesHeidegger On Destruction - Chung ChinAprilo DielovaNo ratings yet
- Mathematics: Full Marks Zero Marks: 0 in All Other CasesDocument31 pagesMathematics: Full Marks Zero Marks: 0 in All Other CasesAbhishek KumarNo ratings yet
- Mtech Geotechnical Engineering 2016Document48 pagesMtech Geotechnical Engineering 2016Venkatesh ThumatiNo ratings yet
- Mcu-R4nek0n+submittal 04212020Document2 pagesMcu-R4nek0n+submittal 04212020Jaime A. AlvarezNo ratings yet
- EM 385-1-1 Chapters 20-26Document179 pagesEM 385-1-1 Chapters 20-26MusabNo ratings yet
- Anatomy Mckinley PPT Chapter 1Document65 pagesAnatomy Mckinley PPT Chapter 1Rosa AlcantarNo ratings yet
- DVRP Newsletter Resilience Vol. 2, Issue 2Document6 pagesDVRP Newsletter Resilience Vol. 2, Issue 2Lucius Doxerie Sr.No ratings yet
- W2AEW Videos (Apr 29, 2017) Topics Listed NumericallyDocument12 pagesW2AEW Videos (Apr 29, 2017) Topics Listed Numericallyamol1agarwalNo ratings yet
- Improving MV Underground Cable Performance - Experience of TNB MalaysiaDocument4 pagesImproving MV Underground Cable Performance - Experience of TNB Malaysialbk50No ratings yet
- Reservoir Engineering Handbook Tarek Ahmed Solution ManualDocument36 pagesReservoir Engineering Handbook Tarek Ahmed Solution ManualMohamad Hasen japerNo ratings yet