Professional Documents
Culture Documents
Lego Research Paper 1-10-11
Uploaded by
Borja Navas SanchezOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Lego Research Paper 1-10-11
Uploaded by
Borja Navas SanchezCopyright:
Available Formats
T
Trachea, 3-d, tors, transplant
LeGOs 4 the cure
Addy Dinehart, Becca Hennings, Aaron Kitchen, Jamie Kitchen, Tim Nahring, Carlos Roldan Jake Rosenbalm, Virn Warndahl Matt young
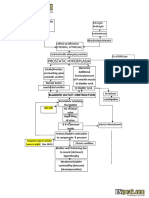
We are the FLL team LEGOs 4 the Cure. This years theme for the FLL competition, body forward, focuses on bioengineering. The subject we chose for our research project is applying current and future technology to help patients who require a tracheal transplant. According to Dr. Lisa Milkowski, and John Janik, the cost of treating patients with organ or tissue failure accounts for approximately 50 percent of total annual healthcare costs in the United States. Also there are many problems with this type of surgery. One question we asked was, why can't we just use an artificial trachea? It turns out that there are several reasons. The survival rate for tracheal prosthesis transplant patients is very low as you can see from this data table and we learned that the surgery takes a long recover from and that some patients require a permanent feeding tube. Organ shortages are also a growing problem. In the last 20 years, kidney shortages have jumped up 75% according to the University of Missouri. We think that this may reflect the amount of other organ
shortages. While coming up with this solution we had to learn about the anatomy of the trachea. The trachea has four layers. The innermost layer is made up of pseudo stratified cilliated columnar epithelial cells. They are covered with mucus and the cilia push the mucus upward in order to remove debris
from the trachea so you can swallow it. The next layer is the submucosa which creates mucus and stores it in goblets cells. The ridges you feel on your trachea is the cartilaginous layer which gives the trachea its form, and the outer layer connects the trachea to the esophagus and the larynx. Our solution is to custom grow a trachea for each patient. Below we will outline our proposed procedure. We would begin by using an MRI machine to scan the patient's trachea. The MRI machine creates an electromagnetic field and uses it to align all the protons in the human body. It uses RF coils, or Radio Frequency coils, to send and record the reaction of the protons thus making a two dimensional cross section. According to the website 3D-Doctor, these cross sections can be combined to create a 3D computer model. This model can then be used by a sterolithography 3D printer to create a biodegradable model that is an exact copy of the inside of the patient's trachea. The 3D printer will use the matrix created by the MRI created model to lay down very thin layers that will create this matrix. Once we have this matrix we can use a bio-printer to print stem cells onto it. Gabor Forgacs and his team from the University of Missouri, have used the bio-printer to create blood vessels, which are layered like the trachea, so it seemed very probable that it would be possible to print a trachea. The University of Missouri separates the cross sections printed with bio-paper. Our idea was to use the model created by the MRI scan and the 3D printer to grow the matrix on. Next we will send hydrogel through the form to allow the cells to sort themselves. The way these cells sort themselves is through the Differential Adhesion Hypothesis. This theory was developed by Malcom Steinberg. It states that similar cells prefer match up with each other. This has been tested
many times, and it is a fact that cells with similar adherent properties prefer to match up with each other. The traditional way stem cell tracheae are grown, is to implant them into the patient's abdomen or arm. This way has worked in many patients, but there are other options if the patient doesn't want to have the trachea implanted in to them. One way is the ORGANIZERtm Series 100 In breath. This bioreactor, developed by Harvard apparatus helps grow tracheae in a more advanced way. It bathes the growing trachea in a solution that feeds oxygen to the cells at the same time it carries away the waste This takes place out of the patient, so the patient doesn't have to worry about damaging their trachea. When the trachea is grown, it can be transplanted using the TransOral Robotic Surgery system, a robot developed originally to work on lungs, but is currently being used for removing cancerous tumors, and helping with sleep apnea. We are somewhat familiar with the TORS system and believe that if it were modified with smaller instruments on the arms, so the arms could get into the trachea, and the arms were at an angle to come in through the throat instead of the abdomen, it could used to preform our surgery. This has many advantages for both the patient and the surgeon. One of the features it has for the surgeon is a console that the robot is controlled allowing the doctor to be anywhere in the world, also the instruments are programed to be precise, and not vibrate, even if the surgeon's hands vibrate. Some of the advantages for the patient is the fact that it requires no incision, instead of breaking the patient's jaw and making an incision from the patient's ear down their neck. Also there is way less recovery time with this type of surgery, and the risk of being required to have a breathing or feeding tube is minimal.
Conclusion We are aware that much of our proposal is based on new but existing technology. We do believe that the way we combine these technologies with our idea of building a bio-degradable custom fit matrix for each patient is new. These ideas combined with using a robotic surgical system to carry out the actual transplant, make our proposal unique.
You might also like
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5795)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1091)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- OncologyDocument67 pagesOncologyCarlos HernándezNo ratings yet
- Research Paper FinalDocument7 pagesResearch Paper Finalapi-643588876No ratings yet
- Benign Prostatic Hyperplasia - BPH - Pathophysiology - Schematic DiagramDocument2 pagesBenign Prostatic Hyperplasia - BPH - Pathophysiology - Schematic DiagramSimran JosanNo ratings yet
- Egypt Cochlear PresentationDocument30 pagesEgypt Cochlear PresentationAhmad Salahuddien100% (1)
- Treatment of Bipolar DisorderDocument20 pagesTreatment of Bipolar DisorderShana Wl100% (1)
- Pulmonary RehabilitationDocument86 pagesPulmonary RehabilitationJuanitoCabatañaLimIIINo ratings yet
- Old Age Psychiatry LectureDocument38 pagesOld Age Psychiatry LectureMo 'Fishpondz' IsmailNo ratings yet
- Hiatus Hernia - Chinese Herbs, Chinese Medicine, AcupunctureDocument6 pagesHiatus Hernia - Chinese Herbs, Chinese Medicine, AcupunctureCarlCordNo ratings yet
- Data Change Template CardivaDocument123 pagesData Change Template CardivaNorilyn FloresNo ratings yet
- Doctor of Veterinary Medicine: 1st Year 1st SemesterDocument4 pagesDoctor of Veterinary Medicine: 1st Year 1st SemesterDexter LagrimasNo ratings yet
- Sri Ramachandra University Application-09Document5 pagesSri Ramachandra University Application-09Mohammed RaziNo ratings yet
- Nonspecific Genital UlcersDocument16 pagesNonspecific Genital UlcersThảo NguyễnNo ratings yet
- Ontario - Schedule of Benefits 2021Document970 pagesOntario - Schedule of Benefits 2021Raj LoganathanNo ratings yet
- Zhang 2021Document8 pagesZhang 2021Magna Fitriani HutasuhutNo ratings yet
- Devry HSM340 Week 7 QuizDocument3 pagesDevry HSM340 Week 7 QuizTSaundersNo ratings yet
- MO Durable Power of AttorneyDocument16 pagesMO Durable Power of Attorneytlayton223No ratings yet
- First Aid: By: Sem. Winmark S. PerdiganDocument18 pagesFirst Aid: By: Sem. Winmark S. PerdiganWinsley RazNo ratings yet
- 1 s2.0 S0883540320304605 MainDocument4 pages1 s2.0 S0883540320304605 MainSavNo ratings yet
- HerbalismDocument15 pagesHerbalismTee R Taylor100% (1)
- Aiims Part IiiDocument104 pagesAiims Part IiiMourian AmanNo ratings yet
- Enfant Cheri Study Centre, Inc. 4 Mid Quarter Examination T.L.E. 7Document2 pagesEnfant Cheri Study Centre, Inc. 4 Mid Quarter Examination T.L.E. 7AR Joy Gardiola TampilNo ratings yet
- Retrospective Study - The Presence of Malassezia in Feline Skin Biopsies. A Clinicopathological Study (Pages 7-14)Document8 pagesRetrospective Study - The Presence of Malassezia in Feline Skin Biopsies. A Clinicopathological Study (Pages 7-14)jenNo ratings yet
- Mantra Systems-Mastering The MDR-White Paper-Edition 4.1Document23 pagesMantra Systems-Mastering The MDR-White Paper-Edition 4.1elias.daood15No ratings yet
- Antipsycotic DrugDocument21 pagesAntipsycotic DrugShashank SatheNo ratings yet
- 5 Drugs 1 IVDocument10 pages5 Drugs 1 IVBianca Nicole Gacad FernandezNo ratings yet
- Martial Arts - Emei Qi Gong-ExercisesDocument3 pagesMartial Arts - Emei Qi Gong-ExercisesSolomon Cosmin Ionut100% (3)
- Assessment and Re-Assessment of Patients According To The Scope of ServiceDocument9 pagesAssessment and Re-Assessment of Patients According To The Scope of Servicegiya nursingNo ratings yet
- DialogDocument2 pagesDialogolga millatNo ratings yet
- Elements of Medical NegligenceDocument4 pagesElements of Medical NegligenceGuevarra RemNo ratings yet
- Upper Extremity Reconstruction: Surgical SolutionsDocument16 pagesUpper Extremity Reconstruction: Surgical Solutionsapi-488115640No ratings yet