Professional Documents
Culture Documents
Medical Surgical Nursing - Respiratory
Uploaded by
Christian EstevesCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Medical Surgical Nursing - Respiratory
Uploaded by
Christian EstevesCopyright:
Available Formats
PAMANTASAN NG LUNGSOD NG MAYNILA (University of the City of Manila) Intramuros Manila
College of Nursing
A Case Study of Pneumonia
In partial fulfillment for the requirement in Medical-Surgical Nursing I
Submitted By: ESTEVES, Christian C. BSN III-1
Submitted To: Professor Enrico P. de Jesus, RN, RM
July 7, 2011
I. CASE INTRODUCTION Pneumonia is an inflammation or infection of the lungs most commonly caused by a bacteria or virus. Pneumonia can also be caused by inhaling vomit or other foreign substances. In all cases, the lungs' air sacs fill with pus , mucous, and other liquids and cannot function properly. This means oxygen cannot reach the blood and the cells of the body. Below is a presentation of case on Pneumonia.
CASE REPORT This is a case of an 18 year-old, non-hypertensive, non-diabetic single male, Filipino, who is currently residing at Pandacan, Manila, and admitted at Santa Ana Hospital on July 2, 2011 diagnosed with Pneumonia, with chief complaint of Difficulty of Breathing, fever, and chest pain. Upon admission, patient had positive signs and symptoms of cough, yellowish phlegm, persistent fever, chest and back pain. Having a minimal knowledge on diseases, he and his family self-medicated him with Paracetamol. However, he noticed no changes and experienced difficulty of breathing. On examination, the patient exhibits adventitious sounds upon auscultation, more efforts and unequal chess wall expansion when inhaling, dull on percussion, and has presence of wound in the left leg and presence of tattoo in the left deltoid.
II. SCHEMATIC DIAGRAM OF PATHOPHYSIOLOGY Virulent Microorganism Streptococcus Pneumoniae
Microorganism eneters the nose( nasal passages)
Passes through the larynx, pharynx, trachea
Microorganism enters and affects both airway and lung parenchyma
Airway damage
Lung invasion
Infiltration of bronchi
flattening of epithelial cells
Infectious organism lodges
macrophages and leukocytes
mucus and phlegm production Stimulation in bronchioles Alveolar collapse Narrowing of Air Passage Increase pyrogen in the body DIFFICULTY OF BREATHING FEVER necrosis of bronchial tissues COUGHING
III. DIAGNOSTIC PROCEDURES AND LABORATORY ANALYSIS NURSING HEALTH HISTORY Past Health History Upon interview, the patients mother was asked about the history of illness of her son, she verbalized that her son had cough, dyspepsia, and cold hands. The patients immunization is hardly remembered. The patient has no history of allergies, and no hospitalization records. According to the mother, she gave Biogesic (Paracetamol) and Loiscol (Carbocisteine). Present Health History Prior to admission, the patients mother verbalized that the patient is experiencing cough, and cold since June 24, 2011, and since June 26, 2011, she observed that the patients chest expansion has more effort, and she perceives it as if the patients is experiencing Difficulty of Breathing. Family Health History There is no history of illness in the immediate family. On his fathers side, there is a history of Pneumonia in his grandfather, uncle, auntie. On his mothers side, there is a history of Hypertension. X-RAY Result C/C: Cough, phlegm, fever Exam Requested: Chest AP > There are reticolunodular opacities on both lungfields with upward traction of left hilus. There are dilated thick walled bronchi noted on both lower lobes. Heart is not enlarged. Aortic knob is sclerotic other visualized structures are unremarkable. Findings are suggestive of Extensive PTB, Bilateral with cicatrical changes, left upper lobe.Bacteriologic correlation is suggested. Figure 1. The radiograph of the patient.
Hemoglobin Erythrocyte Volume Leukocyte count Platelet Count Segmenter Lymphocyte
HEMATOLOGY Normal Value 14-16 gms% 42-50% 5,000-10,000 mm3 150,000-400,000 mm3 36-66% 22-40
Results 11.3 gms% 34 vol% 11,800mm3 200,000 mm3 74% 26
Interpretation Low Low High Normal High Normal
A low hemoglobin level may indicate lower synthesis of erythropoietin, which is needed to stimulate the red bone marrow to produce red blood cell. The erythrocyte volume is lower than the normal value. It may be due to less oxygen that binds with the iron portion to form oxyhemoglobin. Leukocyte count is higher than the normal value since the patients body needs to combat pathogens by phagocytosis and immune response. Other components of the blood are within the normal range.
Color Transparency Specific Gravity Sugar Reaction (pH) Sterility
URINALYSIS Normal Value Pale Yellow Amber Transparent 1.010-1.025 Not Present 4.5-8 pH No microorganism present
Results Light Yellow Cloudy 1.005 Negative 4.1 pH (+) Bacteria
Interpretation Normal Not Normal Low Not Normal Low Not Normal
The patients urine is cloudy, has low specific gravity, and has a presence of bacteria. There may be a presence of white blood cells, bacteria, pus, or contaminants such as prostatic fluid that is causing cloudy urine. Diluted urine has a lower specific gravity thus, causing almost clear or pale yellow color. The patient may have a mild Urinary Tract Infection.
IV. MEDICAL-SURGICAL MANAGEMENT
Organism-specific antibiotic therapy. Administration of initial drug therapy such as broad spectrum antibiotics. Oxygen should be administered. Administration of bronchodilator medications, postural drainage, chest physiotherapy, and nasotracheal suctioning for maintain airway patency Light diet that will not excite the cough in swallowing or increase dyspnea by distention of the stomach, or augment the en-feeblement of the heart action by overtaxing digestion. Starch-rich, and saccharine-rich foods must be withheld.
V. NURSING MANAGEMENT Administer prescribed medications. Promote infection-control measures, especially droplet precautions as indicated. Keep the client in an upright position during feedings and for 30 minutes afterward. Check for residual gastric contents Encourage increased fluid intake to promote internal rehydration. Teach and supervise in coughing, turning and deep breathing techniques. Position the client in side-lying positions, to prevent aspiration. Provide psychological support and restful environment to reduce anxiety and promote rest. Perform respiratory assessment every 4 hours, including determination of rate and characteristics of respirations auscultate the chest, and document findings. Monitor Arterial Blood Gas.
NURSING CARE PLAN PATIENT: Patient X ASSESSMENT Subjective Cues: Dinala naming sya dito sa ospital kasi nilalagnat, nahihirapan huminga tska inuubo na may kasamang dugo, as verbalized by the patients mother Objective Cues: HR: 110 bpm RR: 31 cpm Temp: 38.3 C (+) fever (+) chills (+) dyspnea (+) cough (+) hemoptysis (+) sputum production (+) fatigue (+) crackles (+) tachypnea NURSING DIAGNOSIS Ineffective airway clearance due to inflammation and secretions AGE: 18 years old INFERENCE Invasion of affecting organism (Streptococcus Pneumoniae) Inhalation of organism in the alveolus Multiplication of S. Pneumoniae in the alveolus Invasion in the alveolus epithelium Inflammation of airways Inflammatory exudates fills the alveolar spaces PLANNING Goal: Maintain adequate, and patent airway SPECIFIC OBJECTIVES: Within 8 hours of nursing intervention, the patient will report increased airway patency as manifested by: - Respiratory rate decreased or within the normal range - Maintain Normal Body Temperature - Decreased cough - Decreased sputum production (-) dyspnea (-) crackles GENDER: Male INTERVENTION >Establish rapport with the patients significant other >Monitor vital signs q4 >Monitor respirations and breath sounds, noting rate and sounds >Encourage increased fluid intake >Teach and supervise effective coughing, turning and deep breathing techniques Diagnosis: Pneumonia RATIONALE >To gain cooperation and trust >To obtain baseline data >To indicate respiratory distress or accumulation of secretions >To promote internal rehydration >To help the patient develop a sense of normality without creating undue respiratory distress EVALUATION GOAL MET. Within 8 hours of nursing intervention, the patient reported an increased airway patency, as manifested by: - RR: 23cpm - Temp: 37.5C - Decreased cough - Decreased sputum production (-) dyspnea (-) crackles (-) tachypnea
Lung consolidation Ineffective gas exchange Alveolar exudates consolidates S/Sx Fever, Dyspnea, Sputum Production, Cough, Hemoptysis
>Position the client in side-lying position >Evaluate patients cough/ gag reflex and swallowing ability >Keep environment allergen-free >Administer bronchodilators as ordered >Provide a positive and quiet environment
>To prevent aspiration >To determine the patients ability to protect the airway >To avoid the allergencausing microorganisms >To relax bronchial muscles >To lessen the stress felt by the patient
PATIENT: Patient X ASSESSMENT Subjective Cues: Nananakit yung dibdib tska nahihirapan akong huminga, as verbalized by the patient. Objective Cues: HR: 110 bpm RR: 31 cpm Temp: 38.3 C (+) chest pain (+) dyspnea (+) tachypnea; bradypnea (+) pursed-lip breathing (+) nasal flaring (+) cyanosis NURSING DIAGNOSIS Ineffective Breathing Patterns due to Pneumonia, as manifested by: (+) chest pain (+) dyspnea (+) tachypnea; bradypnea (+) pursed-lip breathing (+) nasal flaring
AGE: 18 years old INFERENCE Invasion of affecting organism (Streptococcus Pneumoniae) Inhalation of organism in the alveolus Multiplication of S. Pneumoniae in the alveolus Invasion in the alveolus epithelium Inflammation of airways Inflammatory exudates fills the alveolar spaces Lung consolidation
GENDER: Male OBJECTIVES INTERVENTION >Establish rapport with the patients significant other > Monitor vital signs q4 > Auscultate chest
Diagnosis: Pneumonia RATIONALE > To gain cooperation and trust > To obtain baseline data >To evaluate presence/ character of breath sounds or secretions > To indicate if there is a possibility of obstruction > Anxiety may be causing acute or chronic hyper ventilation > To diagnose presence/seve rity of lungs disease. EVALUATION GOAL MET. Within 8 hours of nursing intervention, the patient verbalized an improvement in his breathing pattern as manifested by: > decreased chest pain > normal breathing patterns > RR: 23cpm > (-) nasal flaring > (-) cyanosis
Goal: The patient will experience effective respiratory pattern SPECIFIC OBJECTIVES: Within 8 hours of nursing intervention, the patient will verbalize an improvement in his breathing pattern as manifested by: > decreased chest pain > normal breathing patterns > RR within normal range > (-) nasal flaring > (-) cyanosis
> Evaluate cough or presence of secretion > Note emotional responses
> Assist with/ review results of necessary testing
Ineffective gas exchange Alveolar exudates consolidates S/Sx Tachypnea; Bradypnea Nasal flaring Chest pain Cyanosis
>Administer oxygen at lowest concentration as ordered
>For management of underlying pulmonary conditions, respiratory diseases >To limit the level of anxiety >To promote deeper respiration and cough >To limit fatigue
>Maintain calm attitude while dealing with client >Administer Analgesics as ordered >Encourage adequate rest periods between activities >Teach the client on how to splint the chest wall with a pillow
>To provide comfort during coughing
NAME: PATIENT X ASSESSMENT Subjective data: Nakakaramdam ako ng pagod at hirap sa paghinga, as verbalized by the patient Objective data: HR: 110 bpm RR: 31 cpm Temp: 38.3 C (+) restlessness (+) pallor (+) cyanosis (+) fatigue (+) tachypnea
AGE: 18 years old
GENDER: Male INTERVENTION >Establish rapport with the patients significant other > Maintain airway patency
Diagnosis: Pneumonia RATIONALE > To gain cooperation and trust > To ensure opyimal oxygenation and ventilation >To enhance sense of wellbeing > To sustain motivation EVALUATION GOAL MET. Within 8 hours of nursing intervention, the patient participated willingly in necessary/ desired activities, as manifested by: (-)restlessness (-)pallor (-)cyanosis (-)fatigue RR=23cpm
NURSING INFERENCE OBJECTIVES DIAGNOSIS Activity Invasion of Goal: The Intolerance affecting patient will due to fatigue, organism demonstrate a febrile illness, (Streptococcus decrease in hypoxemia, Pneumoniae) physiological and increased signs of work of Inhalation of intolerance breathing, as organism in manifested by: the alveolus SPECIFIC Respiratory OBJECTIVES: Rate Multiplication Within 8 hours decreased or of S. of nursing within the Pneumoniae in intervention, normal range. the alveolus the patient will (+)restlessness participate (+) pallor Invasion in the willingly in (+) cyanosis alveolus necessary/ (+) fatigue epithelium desired (+) tachypnea activities, as Inflammation manifested by: of airways (-)restlessness (-)pallor Inflammatory (-)cyanosis exudates fills (-)fatigue the alveolar RR within spaces normal range Lung consolidation Ineffective gas
>Encourage client to maintain positive attitude > Give client information that provides evidence of daily/weekly progress >Provide referral to other disciplines, such as exercise physiologist, psychological counseling/therapy, etc. > Provide positive atmosphere, while acknowledging difficulty of the situation of the client
> To develop individually appropriate therapeutic regimens.
> To help minimize frustration and rechannel energy.
exchange Alveolar exudates consolidates S/Sx Tachypnea Restlessness Cyanosis Fatigue
>Plan care to carefully balance rest periods
>To reduce fatigue
Generic Name
Brand Name
Classifica tion Antiinfective
Action Interferes with or inhibits protein synthesis in bacteria by binding to 50S ribosomal subunit
Dosa ge 300g IV thru 50 cc solus et every 6 hr
Indication Treatment of rickettsial infection
Chloromphe Chloromy nical cetin
Adverse Reaction s Doserelated bone marrow depressio n& aplastic anemia, GI disturbanc es
Nursing Consideration > Assess lung sounds, respiratory pattern, pulse and blood pressure before administration and during peak of medication > Monitor pulmonary function tests before initiating therapy and periodically throughout course to determine effectiveness of medication > Observe patient for drug tolerance and rebound bronchospasm. If condition occurs, withhold medication and notify physician immediately > Administer medicine at the time specified or as close to that time as possibleif there is a delay, document it.
Paracetamo l
Omol Syrup
Antipyretic Analgesic
reducing the activity of the cyclooxygenase (COX) enzyme; this enzyme participates in the production of prostaglandins
125/v ol 5ml every 6 hrs
Relief of pain & for rapid lowering of fever in bronchitis
Allergic reactions, GI disturbanc es
Flexotide
Flixotide Accuhale
Antiinflammati on
which in turn are involved in the pain and fever processes controls the signs and symptoms of asthma that are responsive to orally inhaled corticosteroids
neb.
Treatment of acute exacerbations of asthma
sneezing attacks immediate ly after use; irritation and burning in the nose
Salbutamol
Ventolin Syrup
2 adrenocep tor agonist
Acetylcystei ne
Fluimucil
Mucolytic Agent
acts on the 2 adrenoceptors of bronchial muscle, with little or no action on the -1 adrenoceptors of the heart. Decreases viscosity of secretions, promoting secretion removal through coughing, postural
1 tbsp 3x a day
Bronchospasm & excessive secretions of tenacious mucus (e.g. bronchial asthma, chronic asthma, chronic bronchitis)
Hypokale mia, tachycardi a, tremor, muscle cramps
> Administer only the drug that you prepare > If patient refuses medication, ask a relative to assist in administering the medications. > Evaluate client's condition and medication compatibility > Administer medicine at the time specified or as close to that time as possibleif there is a delay, document it. > Evaluate client's condition and medication compatibility >dilute with normal saline solution or sterile water for injection. >Administer the ff drugs separately because they are incompatible with acetylcysteine:
6 to 10 ml of 10% soluti on or 3 to 5 ml of
in adjunctive treatment of acute and chronic bronchopulmonary disease
Nausea, rhinorrhea , bronchosp asm especially in asthmatic
drainage, and mechanical means. In acetaminophen overdose, maintains and restores hepatic glutathione, needed to inactivate toxic metabolites.
20% soluti on three or four times daily.
s, stomatitis, and urticaria.
tetracyclines, hydrogen peroxide, trypsin. >Use water to remove residual drug solution on the patients face after administration by face mask. >Inform patient that nebulization may produce an initial disagreeable odor, but will soon disappear. >Give daily before 9AM to mimic normal peak diurnal corticosteroid levels and minimize HPA suppression. >Space multiple dose evenly throughout the day. >Use minimal dose for minimal duration to minimize adverse effects. >Use alternate day maintenance therapy with short acting corticosteroids whenever possible.
Hydrocortis one Sodium succinate
SoluCortef
Shortacting Corticoste roid
Suppresses inflammatory and immune responses, mainly by inhibiting migration of leukocytes and phagocytes and decreasing inflammatory mediators
100m g IV, q6 hours
Replacement therapy in adrenal cortical insufficiency Hypercalcemia; associated with cancer Short term inflammatory disorders
Vertigo, headache, hypotensi on, shock, thin, fragile skin, petechiae, amenorrh ea, muscle weakness
You might also like
- Med-Surg Nusing BulletsDocument65 pagesMed-Surg Nusing BulletsHarley C. Tan100% (1)
- COMPREHENSIVE NURSING ACHIEVEMENT TEST (RN): Passbooks Study GuideFrom EverandCOMPREHENSIVE NURSING ACHIEVEMENT TEST (RN): Passbooks Study GuideNo ratings yet
- Medical Surgical Nursing - DiabetesDocument4 pagesMedical Surgical Nursing - Diabetestripj33100% (2)
- NURSING CARE OF ADULTS I: Passbooks Study GuideFrom EverandNURSING CARE OF ADULTS I: Passbooks Study GuideNo ratings yet
- Nursing Lecture RespiratoryDocument13 pagesNursing Lecture RespiratoryAedge010100% (1)
- Principles of Medication AdministrationDocument22 pagesPrinciples of Medication AdministrationTina TalmadgeNo ratings yet
- Community Focused Nursing: Passbooks Study GuideFrom EverandCommunity Focused Nursing: Passbooks Study GuideNo ratings yet
- Abdominal Paracentesis.Document4 pagesAbdominal Paracentesis.Sukh Preet100% (1)
- Medsurg 2007Document15 pagesMedsurg 2007WisdomIsMisery100% (1)
- Mechanical Ventilation For NursingDocument55 pagesMechanical Ventilation For NursingAmira AttyaNo ratings yet
- Career Clarity for Nurses: Navigating Nursing Through Challenging TimesFrom EverandCareer Clarity for Nurses: Navigating Nursing Through Challenging TimesRating: 1 out of 5 stars1/5 (1)
- Concept Map 1Document5 pagesConcept Map 1api-396919069No ratings yet
- NURSING CARE OF ADULTS II: Passbooks Study GuideFrom EverandNURSING CARE OF ADULTS II: Passbooks Study GuideNo ratings yet
- Patient NursingDocument7 pagesPatient Nursingsahilchaudhary7No ratings yet
- Medical Surgical Nursing Review NotesDocument75 pagesMedical Surgical Nursing Review NotesMary Ann Comia RañolaNo ratings yet
- Nursing ProcessDocument12 pagesNursing Processgrey26No ratings yet
- Transition to the Registered Professional Nurse Role: Passbooks Study GuideFrom EverandTransition to the Registered Professional Nurse Role: Passbooks Study GuideNo ratings yet
- Asepsis and Infection Control Nursing SchoolDocument20 pagesAsepsis and Infection Control Nursing Schoolleonardo orozco100% (1)
- Nursing Concept Map 1Document3 pagesNursing Concept Map 1Norah Okafor Ezike67% (3)
- ANEMIADocument48 pagesANEMIAjomcy0% (2)
- ABG Analysis NCLEX ExamDocument5 pagesABG Analysis NCLEX ExamAngie MandeoyaNo ratings yet
- Study Guide Med Surg #1Document22 pagesStudy Guide Med Surg #1cfunk929No ratings yet
- How To Calculate Drug Dosage AccuratelyDocument7 pagesHow To Calculate Drug Dosage AccuratelyAiramCeszDelaCruzNo ratings yet
- HESI Women's Health:Newborn DrugsDocument8 pagesHESI Women's Health:Newborn Drugsisapatrick8126No ratings yet
- Adult Health III Final Study GuideDocument12 pagesAdult Health III Final Study GuideRyanne JNo ratings yet
- Basic Nursing Fundamentals EliminationDocument35 pagesBasic Nursing Fundamentals Eliminationlisa100% (1)
- Fundamental Hesi Review NotesDocument2 pagesFundamental Hesi Review NotesMike Burgess50% (2)
- NursingDocument61 pagesNursingMrs Rehan50% (2)
- Bowel EliminationDocument67 pagesBowel EliminationPhyu Lin100% (1)
- Med Surg Test 4 Study GuideDocument29 pagesMed Surg Test 4 Study GuideJessNo ratings yet
- Chapter 036Document9 pagesChapter 036Neverends201160% (5)
- Musculoskeletal Note1Document34 pagesMusculoskeletal Note1FreeNursingNotes100% (4)
- CCM Study Guide Foundations of NursingDocument46 pagesCCM Study Guide Foundations of NursingAlexandra BrowneNo ratings yet
- RN Lesson 2 Safety & Infection Control PracticeDocument39 pagesRN Lesson 2 Safety & Infection Control PracticeRuthmarie CatarajaNo ratings yet
- Nursingprocess Assessing 111105015609 Phpapp01Document71 pagesNursingprocess Assessing 111105015609 Phpapp01ALmik HussinNo ratings yet
- Arterial LinesDocument13 pagesArterial LinesberhanubedassaNo ratings yet
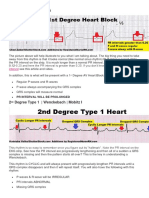
- Heart BlocksDocument3 pagesHeart BlockslhenNo ratings yet
- Chapter 19 Heart Marie BDocument29 pagesChapter 19 Heart Marie BomarNo ratings yet
- MedSurg GIDocument4 pagesMedSurg GIZachary T HallNo ratings yet
- 50 Shades of Practice QuestionsDocument11 pages50 Shades of Practice QuestionsAmie Ray100% (1)
- OxygenationDocument56 pagesOxygenationHerald Clarence M. AmbayecNo ratings yet
- Respiratory AssessmentDocument38 pagesRespiratory AssessmentNisha MwlzNo ratings yet
- Exam 3 Review Med SurgDocument18 pagesExam 3 Review Med SurgCarol ReidNo ratings yet
- Med-Surg LEWIS 47 Final Foofed UpDocument10 pagesMed-Surg LEWIS 47 Final Foofed Uphariniliaankhen100% (1)
- Hesi Gerontology Age-Related Risks PDFDocument14 pagesHesi Gerontology Age-Related Risks PDFAna BienneNo ratings yet
- Nursing Process QuestionsDocument12 pagesNursing Process QuestionsSritama Ghosh100% (1)
- Medication Calculation - Commonly Used FormulasDocument1 pageMedication Calculation - Commonly Used FormulasAaron AntonioNo ratings yet
- Ob Exam Study Guide The Bible 001 49pgsDocument50 pagesOb Exam Study Guide The Bible 001 49pgsVin Lorenzo CampbellNo ratings yet
- Thorax, Skin, Hair, Nails ObjectivesDocument3 pagesThorax, Skin, Hair, Nails Objectivesctramel001100% (1)
- NCLEX Practice QuestionsDocument12 pagesNCLEX Practice QuestionsDane WrightNo ratings yet
- Acid Base Balance: Carol Johns, MSN, RNDocument36 pagesAcid Base Balance: Carol Johns, MSN, RNkatrinasdNo ratings yet
- Fundamentals Kaplan ReviewDocument94 pagesFundamentals Kaplan Reviewymitchell7No ratings yet
- Nursing Test Taking Strategy IDocument20 pagesNursing Test Taking Strategy Iicy431100% (1)
- OxygenationDocument19 pagesOxygenationdlneisha61100% (3)
- Hello, ScribdDocument1 pageHello, ScribdChristian EstevesNo ratings yet
- Recommendation LetterDocument5 pagesRecommendation LetterChristian EstevesNo ratings yet
- HelloDocument19 pagesHelloChristian EstevesNo ratings yet
- St. Perpetua Was Young, Beautiful and Well-Educated Noblewoman of Carthage, North AfricaDocument7 pagesSt. Perpetua Was Young, Beautiful and Well-Educated Noblewoman of Carthage, North AfricaChristian EstevesNo ratings yet
- Pcs LogoDocument1 pagePcs LogoChristian EstevesNo ratings yet
- Bed SpacerDocument1 pageBed SpacerChristian EstevesNo ratings yet
- St. Perpetua: (A Project in CLED) Submitted By: 6 - St. Perpetua Submitted ToDocument1 pageSt. Perpetua: (A Project in CLED) Submitted By: 6 - St. Perpetua Submitted ToChristian EstevesNo ratings yet
- Esteves, Rolyn Mae C.: MathematicsDocument2 pagesEsteves, Rolyn Mae C.: MathematicsChristian EstevesNo ratings yet
- Travelbee&WeidenbachDocument9 pagesTravelbee&WeidenbachChristian EstevesNo ratings yet
- Rle FormDocument1 pageRle FormChristian EstevesNo ratings yet
- Deed of AssignmentDocument2 pagesDeed of AssignmentChristian EstevesNo ratings yet
- CHED Memorandum Order # 5 (2008)Document121 pagesCHED Memorandum Order # 5 (2008)wiredpsyche100% (69)
- CHED Memorandum Order # 5 (2008)Document121 pagesCHED Memorandum Order # 5 (2008)wiredpsyche100% (69)
- Medical Surgical Nursing - NeuroDocument19 pagesMedical Surgical Nursing - NeuroChristian EstevesNo ratings yet
- Bed SpacerDocument1 pageBed SpacerChristian EstevesNo ratings yet
- Case StudyDocument16 pagesCase StudyChristian EstevesNo ratings yet
- Clinical TeachingDocument25 pagesClinical TeachingChristian EstevesNo ratings yet
- Values WRDocument1 pageValues WRChristian EstevesNo ratings yet
- Fluids and Electrolytes NOTESDocument3 pagesFluids and Electrolytes NOTESChristian EstevesNo ratings yet
- BACON B - Bowel EliminationDocument4 pagesBACON B - Bowel EliminationChristian EstevesNo ratings yet
- Values WRDocument1 pageValues WRChristian EstevesNo ratings yet
- FecalDocument29 pagesFecalChristian EstevesNo ratings yet
- Case History For 2nd Year StudentsDocument4 pagesCase History For 2nd Year StudentsAkshit SharmaNo ratings yet
- Pediatrics CWU Year 5Document7 pagesPediatrics CWU Year 5anon_67984147No ratings yet
- PNEUMONIADocument8 pagesPNEUMONIARica ParcasioNo ratings yet
- Diagnosis and Management of Cystic Fibrosis: Rosalind L SmythDocument6 pagesDiagnosis and Management of Cystic Fibrosis: Rosalind L SmythMuhammadShahzadNo ratings yet
- History Taking of Respiratory SystemDocument24 pagesHistory Taking of Respiratory SystemNadiya Elfira BilqisNo ratings yet
- AEBA QUESTIONS-WPS OfficeDocument2 pagesAEBA QUESTIONS-WPS OfficeMarj Castor LisondraNo ratings yet
- NCM 112 LEC Topic 2 Oxygenation Current Health History Physical Examination Normal Abnormal Breath Sounds Breathing PatternsDocument7 pagesNCM 112 LEC Topic 2 Oxygenation Current Health History Physical Examination Normal Abnormal Breath Sounds Breathing PatternsViviene Faye FombuenaNo ratings yet
- Pulmonary Tuberculosis Nclex QuestionsDocument3 pagesPulmonary Tuberculosis Nclex Questionssheen100% (6)
- SDA Catalog For July-Aug - Sept-2021Document110 pagesSDA Catalog For July-Aug - Sept-2021Be HeroSmartNo ratings yet
- Evaluation Checklist Case 7 Bronchial AsthmaDocument7 pagesEvaluation Checklist Case 7 Bronchial AsthmaChristian MendiolaNo ratings yet
- Cuprum MetallicumDocument6 pagesCuprum MetallicumKamalNo ratings yet
- Deborah Hellyer AsthmaDocument86 pagesDeborah Hellyer AsthmaGiorgi PopiashviliNo ratings yet
- Organic Wellness Healthy & Organic ProductDocument18 pagesOrganic Wellness Healthy & Organic Productorganic wellnessNo ratings yet
- OCCUPATIONAL DISEASES Clinical cases 2015 англ 2Document28 pagesOCCUPATIONAL DISEASES Clinical cases 2015 англ 2kjk100% (1)
- Introduction To Community Health: What Is Community Health and Why Is It Important?Document35 pagesIntroduction To Community Health: What Is Community Health and Why Is It Important?Mark Johnson Dela PeñaNo ratings yet
- Assessment of Respiratory FunctionDocument4 pagesAssessment of Respiratory FunctionCristine Dominique E. DonaireNo ratings yet
- BBCR RepertoryDocument189 pagesBBCR Repertoryjaydeeppanchala24No ratings yet
- History of Present IllnessDocument2 pagesHistory of Present IllnessReylan GarciaNo ratings yet
- Common Illnesses in Family PracticeDocument234 pagesCommon Illnesses in Family Practicetmle100% (2)
- IV. Data Presentation, Interpretation and AnalysisDocument43 pagesIV. Data Presentation, Interpretation and AnalysisMaykel JekNo ratings yet
- John Murtaghs General Practice Companion Handbook 7Th Edition John Murtagh Full Chapter PDF ScribdDocument67 pagesJohn Murtaghs General Practice Companion Handbook 7Th Edition John Murtagh Full Chapter PDF Scribdderrick.ayala232100% (5)
- Nursing Diagnosis Nursing Intervention Rationale Exchange: Prioritized Nursing Problem For Choanal AtresiaDocument9 pagesNursing Diagnosis Nursing Intervention Rationale Exchange: Prioritized Nursing Problem For Choanal AtresiaJinaan MahmudNo ratings yet
- AnaesthesiaDocument121 pagesAnaesthesiaSandeep Bhangale100% (1)
- COPD CaseDocument73 pagesCOPD CaseTony DawaNo ratings yet
- POCKET GUIDE GOLD 2023 Ver 1.2 17feb2023 - WMVDocument55 pagesPOCKET GUIDE GOLD 2023 Ver 1.2 17feb2023 - WMVMARISOL FERNANDA GÓMEZNo ratings yet
- Chapter 54 Drugs Acting On The Upper Respiratory TractDocument44 pagesChapter 54 Drugs Acting On The Upper Respiratory TractHannah Lorraine GamayonNo ratings yet
- Med-Surg HESI Study GuideDocument13 pagesMed-Surg HESI Study GuideTravis Hargett93% (14)
- Sample NCP in Format Color CodedDocument4 pagesSample NCP in Format Color CodedinsadauNo ratings yet
- Alternative and Complementary Medicine: AlterativeDocument9 pagesAlternative and Complementary Medicine: AlterativemuhammadriazNo ratings yet
- Postural, DrainageDocument7 pagesPostural, DrainageJames ThompsonNo ratings yet