Professional Documents
Culture Documents
NCPSFINAL
Uploaded by
Cristina L. JaysonCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
NCPSFINAL
Uploaded by
Cristina L. JaysonCopyright:
Available Formats
NURSING CARE PLANS
PRE OPERATIVE
Problem Identified: Active blood loss Nursing Diagnosis: Risk for Fluid Volume Deficit related to heavy uterine bleeding secondary to myoma Cause Analysis: Fibroids may appear singly or in clusters, and be as small as a grape or as big as an orange. They are comprised of muscle and fibrous tissue, and may cause excessive flow during menstruation or bleeding between periods. Continuous enlargement of tumors can cause distruption of uterine lining and devascularization, wherein capillaries will be injured thus leading to abnormal uterine bleeding. Reference: knettishall.org/xoops/modules Bleeding is one of the main causes of dehydration resulting in decreased blood volume. As a compensatory mechanism, the body pulls the water into the vascular system from other areas, resulting in pallor, or dry mucous membrane. (Hopper, 2003: 47) Cues Subjective: nag dugo japun akoa. 2 pads na ako na consumed. As verbalized by the patient. Objective: Blood Pressure = 110/80 mmHg Pulse rate = 72 bpm Respiratory rate = Objectives Nursing Interventions Short term: Independent: After 4 hours of nursing 1. Monitored and intervention, patient will recorded vital signs be able to understand every 2 hours. condition and identify risk factors potential for further fluid volume deficit. 2. Assessed oral mucous membrane every 4 hours. Long Term: After 3 days of nursing 3. Measured intake intervention, the patient and output per shift. will achieve fluid volume Recorded and at a functional level as reported significant evidenced by stable vital changes. signs and moist mucous membranes. 4. Kept oral fluids at Rationale Tachycardia, dyspnea, or hypotension may indicate fluid volume deficit. (Sparks and Taylor, 2006:111) To check for dehydration. (Sparks and Taylor, 2006: 111) Decreased urine output may indicate reduced fluid volume. It also aids in the estimation of patients fluid balance. (Sparks and Taylor, 2006: 111) This gives patient some Evaluation Short term: Goal met. After 4 hours of nursing intervention, patient was able to understand condition and identify risk factors potential for further fluid volume deficit. Long Term: After 3 days of nursing intervention, the patient achieved fluid volume at a functional level as evidenced by stable vital signs, moist mucous membranes, pinkish conjunctiva and lips.
22 cpm Temperature = 36.0 C Hematocrit = 0.20% N. V: (0.37-0.47%) RBC count = 3.76 1012/L (4-6 1012/L) Hemoglobin = 67 g/L (110-180 g/L) Intake = 1, 200 cc/shift Output = 840 cc/shift Pallor Pale conjuctiva Pale lips Dry mucous
bedside within patients reach and encouraged to increase fluid intake. 5. Explained reasons for fluid loss, and taught patient how to monitor fluid volume by measuring intake and output. Collaborative: 1. Monitored laboratory values and report abnormal findings to doctor. 2. Administered fluids (Plain Normal Saline Solution, 1 liter at KVO), blood or blood products (administered 2 units of PRBC and 1 unit of FWB for 4 hours each), or plasma expanders. Monitored and
control over fluid intake and supplements parenteral fluid intake. (Sparks and Taylor, 2006: 113) This encourages patient involvement in personal care. (Sparks and Taylor, 2006: 112)
Elevated hematocrit and hemoglobin also indicate dehydration. (Sparks and Taylor, 2006: 113) Replaces fluid and whole blood loss; facilitates fluid movement into intravascular space (Sparks and Taylor, 2006: 111)
membrane Weakness
recorded effectiveness and watched out for transfusion reaction.
Problem Identified: Right periumbilical pain Nursing Diagnosis: Acute Pain related to compression of nerve endings secondary to enlarged myoma Cause Analysis: The compressed nerve endings due to enlarged myoma send signal to the brain that causes the patient to feel the pain. (Kozier, et al., 2008: 1189) Cues Subjective: Sakit ni diri dapit bsta mutindog ko as verbalized by patient. Mga 4/10 ang sakit as stated by patient. Objective: Blood Pressure = 110/70 mmHg Pulse rate = 85 bpm Provides baseline for Objectives Short term: After 1 hour of nursing intervention, the patient will carry out appropriate interventions for pain relief Long term: After 8 hours of providing nursing intervention, patient will verbalize decrease in intensity of pain from 4/10 to 2/10 Nursing Interventions Independent: 1. Monitored vital signs during episodes of pain. Rationale Blood pressure, respiratory and heart rate are usually altered in acute pain. (Doenges, 2008: 496) Useful in determining appropriate interventions. (Doenges, 2008. 497) Evaluation Short term: Goal met. After 1 hour of nursing intervention, the patient carried out appropriate interventions for pain relief. Long term: Goal partially met. After 8 hours of providing nursing intervention, patient verbalized a decrease in intensity of pain from 4/10 to 3/10.
2. Reviewed clients previous experiences with pain and methods found either helpful or unhelpful for pain control in the past.
Respiratory rate = 19 cpm Temperature = 36.7 C Presence of myoma (Transvaginal Ultrasound - 08-3112) Grimacing Guarding behavior
3. Ascertained clients knowledge of and expectations about pain management
interventions and teaching, provides opportunity to allay common fears/misconceptions. (Doenges, 2008. 496)
4. Performed pain assessment each time pain occurs. Document and investigate changes from previous reports and evaluate results of pain interventions. 5. Performed comfort measures to promote relaxation, such as massage, bathing, repositioning, and relaxation techniques. 6. Manipulate environment to promote periods of uninterrupted rest.
To demonstrate improvement in status or to identify worsening of underlying condition/developing complications. (Doenges, 2008. 496)
Theses measures reduce muscle tension or spasm, redistribute pressure on body parts, and help patient focus on non-painrelated subjects. (Sparks and Taylor, 2006: 226) This promotes health, wellbeing, and increase energy level important to pain relief. (Sparks and Taylor, 2006: 226)
7. Helped patient into comfortable position and use pillows to splint or support painful areas, as appropriate. Collaborative: 1. Collaborate with patient in administering prescribed analgesics when alternative methods of pain control are inadequate. Monitor and record medications effectiveness and adverse effects.
Reduces muscle tension or spasm and redistributes pressure on body parts (Sparks and Taylor, 2006: 226)
Gaining patients trust and involvement helps ensure compliance and may reduce medication intake. (Sparks and Taylor, 2006: 226)
Problem Identified: Increased urine frequency Nursing Diagnosis: Impaired Urinary Elimination related to compression of bladder secondary to presence of enlarged uterine fibroid. Cause Analysis: Compression of bladder can cause frequent voiding of small quantities of urine. (Kozier, et al., 2008: 1291) Fibroids commonly cause urinary symptoms. They are hard and firm tumors made up of smooth muscle and fibrous tissue. When these tumors are located in the front of the uterus, they can compress the bladder like a paperweight. This does not allow the bladder to fill to its capacity, resulting in increased urinary frequency and nocturia (waking up at night to urinate). (http://www.sharecare.com/question/how-fibroids-causeurinary-symptoms)
Cues Subjective: Patient verbalized, Ika 8 ko nakaihi karon. Patient stated, Usahay makamata kog gbii para mangihi Objective: Nocturia Urination frequency of 8x per shift
Objectives Short term: After 4 hours of nursing intervention, the patient will verbalize understanding of her present condition and participate in measures to compensate for present condition. Long term: After 3 days of nursing intervention, patient will be able to regain her normal urinary elimination as evidenced by absence of nocturia and urinary frequency.
Nursing Interventions Independent: 1. Observed voiding pattern. Document intake and output, and patients daily weight. Report any changes. 2. Encouraged patient to verbalize feelings and concerns related to urologic problem.
Rationale Accurate intake and output measurements are essential for correct fluid replacement therapy. (Sparks and Taylor, 353) Active listening conveys respect for patient; ventilation helps pinpoint patients fear. (Sparks and Taylor, 354)
Evaluation Short term: Goal Met. After 4 hours of nursing intervention, the patient verbalized understanding of her present condition and participated in measures to compensate for defect. Long term: After 3 days of nursing intervention, patient will be able to regain her normal urinary elimination as evidenced by absence of nocturia and urinary frequency.
3. Determined pathology of bladder dysfunction relative to identified medical diagnosis. 4. Explained urologic condition to patient and family members.
Identifies direction for further evaluation/treatment options to discover specifics of individual situation. (Doenges, 2008. 728)
5. Emphasized
Accurate health knowledge increases patients ability to maintain health. Involving family members assures patient that he/she will be cared for. (Sparks and Taylor, 2006: 354)
importance of keeping perineal area clean and dry. 6. Encouraged fluid intake and limit after 7 p.m. 7. Encouraged use of diapers or bedside commode. Collaborative: 1. Insert urinary catheter as a last resort.
Reduces risk for infection and skin breakdown. (Doenges, 2008: 730) To prevent nocturia. (Sparks and Taylor, 2006: 358) Allows the patient to void without the hassle of going to the bathroom.
A patient is catheterized only if necessary because catheterization commonly leads to urinary tract infection. (Smeltzer, 2004: 1290)
Problem Identified: Impaired sleeping pattern Nursing Diagnosis: Sleep Pattern Disturbance related to frequent urination at night Cause Analysis: Sudden urge to void causes patient to become uncomfortable and this can cause him to keep waking up and therefore robs him of his time to rest/sleep. (Smeltzer, 2004: 1278) Cues Objectives Nursing Interventions Rationale Evaluation
Subjective: Paputol-putol akong tulog kay sige kog ihi pgka gabii, as verbalized by patient. Usually matulog ko ay 11:00 sa gabii daun mo mata ko mga 3:00 am. Dili na dayun ko makatulog balik, as stated by patient. Objective: Yawning Dozing Observed lack of energy Sleeping hours = 4 hours (Patients normal sleeping hours = 6-7 hours)
Short term: After 8 hours of nursing intervention, the patient will report an improvement in her sleeping pattern.
Independent: 1. Observed or obtain feedback from client regarding sleeping problems, usual bedtime, routines, number of hours of sleep, time of arising, and environmental needs. 2. Encouraged patient to discuss any concerns that may be preventing sleep. To determine usual sleep pattern and provide comparative base line (Doenges, 2008: 416)
Short term: Goal not met. After 8 hours of nursing intervention, the patient did not report an improvement in her sleeping pattern.
Long Term: After 3 days of nursing intervention, patient will be able to regain her normal sleeping pattern as evidenced by verbalization of 6-7 hours of sleep/day.
Active listening helps you determine causes of difficulty of sleep. (Sparks and Taylor, 2006: 302)
Long Term: After 3 days of nursing intervention, patient regained her normal sleeping pattern as evidenced by verbalization of 6-7 hours of sleep/day.
3. Created quiet environment conducive to sleep. 4. Asked patient to describe in specific terms each morning quality of sleep during previous night. 5. Encouraged use of diapers or bedside
These measures promote rest and sleep. (Sparks and Taylor, 2006: 302) To evaluate effectiveness of intervention (Sparks and Taylor, 2006: 302)
Allows the patient to void without the hassle of going to the bathroom. To reduce need for
commode. 6. Advised patient to limit fluid intake in the evening.
nighttime elimination (Sparks and Taylor, 2006: 358)
POST OPERATIVE:
Problem Identified: pain at the surgical incision
Nursing Diagnosis: Acute pain related to surgical incision at the hypogastric region secondary to total abdominal hysterectomy with bilateral salphingo-oophorectomy Cause Analysis: Nociceptive pain is caused by an injury to the body tissues. The injury may be a cut, a bruise, bone fracture, crush injury, burn or anything that damages tissues. This type of pain is typically aching, sharp, or throbbing. Most pain is nociceptive pain. Pain receptors for tissue injury (nociceptors) are located mostly in the skin or in the internal organs. The pain almost universally experienced after surgery is nociceptive pain. SOURCE: The Merck Manual, p.404 Cues Subjective: Dako akong samad. Ginabutangan pa gain ni ug binder para dili maukab and tahi kay sakit man. Magsige na lang ko higda kay sakit musamot kung mulihok. Tuloy-tuloy iyang pagsakit. Ngut-ngot nga dili masabtan. Objective: -verbalized a pain scale of 6, in a scale of 1-10 with 10 as the most painful -sighing and moaning noted -slowed movement -guarding behavior -positioning to avoid pain Objectives Short Term: After 4 hours of nursing intervention, the patient will: a) verbalize a pain scale of 4-5 and increased comfort b) verbalize and demonstrate nonpharmacologic methods to manage pain such as deep breathing and splinting during cough c) participate in the use of diversional activities such as engaging in conversations to minimize pain Long Term: After 4 days of intervention, the patient Nursing Interventions Independent: 1) Performed comfort measures such as massage, bathing and repositioning. Rationale -these measures reduce muscle tension or spasm; redistribute pressure on body parts and help patient focus on non-pain related subjects Evaluation Short Term: Objectives were fully met. Patient verbalized a pain scale of 4, increased relief and comfort. Patient also demonstrated breathing techniques splinting to minimize pain. She also participated in conversations done to distract her from pain.
2) Helped patient into a comfortable position and use pillows to splint or support the incision area
-to reduce tension and thus reduce pain
3) Manipulated the environment to provide uninterrupted rest
- this promotes health, well-being and increased energy level important to pain relief.
Long Term: At the end of 2 days of intervention, objectives were fully met. The patient verbalized a pain scale of 2 and increased comfort. Whenever mild pain occurred, patient was observed to do deep breathing on her own.
4) Provided diversional
-to help patient focus on
will: a) verbalize a pain scale of 0-2 b) readily integrate non-pharmacologic methods in daily activities whenever pain occurs
activities such as such as encouraging visits of family members and engaging in conversations
non-pain related matters
5) Encouraged use of relaxation techniques such as focused breathing and imaging.
- to distract attention and reduce tension
Collaborative: 1) Administered D5LR 1 liter with Tramadol 50mg at 30gtts/min
-to effectively reduce or eradicate pain
Problem Identified: Disruption of skin surface Nursing Diagnosis: Impaired skin integrity related to mechanical trauma secondary to total abdominal hysterectomy with bilateral salphingooophorectomy as manifested by presence of surgical incision on the hypogastric region. Cause Analysis: Skin, the flexible tissue enclosing the body of vertebrate animals. In humans and other mammals, the skin operates a complex organ of numerous structures serving vital protective and metabolic functions. Surgical incision is a medical procedure involving an incision with instruments; performed to repair damage or arrest disease in a living body. Wound healing is a complex sequence of events initiated by injury to the tissues. The components are coagulation of bleeding, inflammation, epithelization, fibroplasias and collagen metabolism, collagen maturation, scar remodeling and wound contraction. SOURCE: http://www.answers.com/topic/skin Cues Subjective: Dako akong samad. Ginabutangan pa gain ni ug binder para dili maukab and tahi kay sakit man. Katol ako tibuok lawas. Objective: -horizontal incision in the hypogastric region of the abdomen with dressing and abdominal binder noted -redness of surrounding skin noted -pruritus noted in the whole body Objectives Short Term: At the end of 1 hour of nursing intervention, the patient will: a) verbalize and demonstrate appropriate wound dressing procedure b) demonstrate the use splinting and support to protect the wound c) verbalize the need to increase intake of protein and carbohydrates for faster wound healing. Long Term: At the end of 4 days of nursing intervention, the patient will: a) display timely healing of wound without any signs of infection such as Nursing Interventions Independent 1) Inspected skin on a daily basis, describing wound characteristics and changes observed. 2) Instructed the patient and significant others to keep the area clean and dry. 3) Taught patient of proper wound dressing techniques Rationale - To monitor progress of wound healing. Evaluation Short Term: At the end of 1 hour of nursing intervention, objectives were fully met. Patient demonstrated wound dressing appropriately. Patient also demonstrated the use of pillow as splint or support during cough. Patient also verbalized the need to increase protein and carbohydrate intake such as foods as meat, fish, beans and bread. Long Term: At the end of 4 days of nursing intervention, the objectives were fully met. No signs of further infection were noted. No signs of erythema and pus
- To assist bodys natural process of repair.
- this involves the patient in her care and promotes empowerment over her condition. This also prevents infection. -To provide support over the incision area.
4) Instructed patient to apply splint using a pillow when patient coughs or moves.
-these measures promote circulation, reduce pressure and avoid skin
erythema, hyperthermia and pus formation.
breakdown 5) Positioned patient for comfort and minimal pressure on bony prominences. Turn to sides at least every 2 hours.
formation were noted
-Promotes circulation And reduces risks associated with immobility such as thrombus formation and skin ulcers.
6) Encouraged early ambulation or mobilization. -To aid in wound healing.
7) Provided optimum nutrition, and increased protein and carbohydrate intake such as meat, fish and bread. Collaborative: 1. Administered Cefurex 500 mg 1 TAB 2x a day PO
-to aid in faster healing process and in preventing infection.
Problem Identified: Impaired mobility Nursing Diagnosis: Impaired physical mobility related to discomfort at the surgical site Cause Analysis: Insufficient physiological or psychological energy to endure or complete required or desired daily activities due to bleeding from damaged tissues which stimulates inflamamatory response of the body and there will be increased in capillary permeability and leads to cellular exudation then it will cause edema and pain that leads to impaired function. Reference: http://www1.us.elsevierh ealth.com/MERLIN/Gulanick/Constructor/index.cfm?plan=35 Copyright 2009 Mosby Cues Subjective: Dili lagi ko lugos kalihok kay tungod sa kasakit sa samad. Magsige na lang man ko ug higda. Musakit man ug samot pag maglihok-lihok ko Objectives Short term: At the end of 4 hours of nursing intervention, patient will be able to : a) Verbalize understanding of situation and individual treatment regimen and safety measures. b) Demonstrate techniques that enable resumption of activities such as splinting, early ambulation and engaging in self-care activities. Nursing Interventions Independent 1) Instructed patient to splint the wound with a pillow if patient attempts to move. 2) Assisted with self care activities. Rationale -Splinting supports the wound and minimizes the discomfort and pain felt. - improves muscle strength and circulation, enhances patient control in the situation and promotes self directed wellness. -early mobility reduces complications of bed rest. Promotes healing and normalization of organ function. Evaluation Short Term At the end of 4 hours of nursing intervention, the objectives were fully met. The patient verbalized understanding of having myoma and the treatment regimen especially a change in diet to counter the problem. Patient also demonstrated the use of splinting during movement correctly. Patient also performed self-care activities such as dressing, tooth brushing and with assistance
Objective: -difficulty turning to sides noted -slowed movement noted -moaning and sighing noted upon movement
3)Provided assistance with mobility
Long term: After 2 days of nursing intervention, the patient will: a)Regain mobility at the highest possible level with minimal discomfort.
4) Monitored BP with resumption of activity. Note reports of dizziness.
- postural hypotension is common to patients on bed rest and may require interventions like elevation of bed.
Collaborative: 1) Administered Tramal 100 mg 1 TAB BID PO -to perit maximal effort and involvement in activity
Long term: After 2days of nursing intervention, the objectives were fully met. Patient achieved full mobility status little complaints of discomfort.
Problem Identified: Risk for infection Nursing Diagnosis: Risk for infection related to surgical incision Cause Analysis: The location and extent of the surgical site and incision put the patient at risk for contamination of the site and infection and sepsis. The patient is monitored closely for local and systemic signs and symptoms of infection: purulent drainage, redness, increased pain, fever, and an increased white blood count. SOURCE: Medical Surgical Nursing, Brunner, p. 1434 A wound can be infected with microorganisms at the time of injury, during surgery or postoperatively. Surgical infection is most likely to become apparent 2 to 11 days postoperatively. SOURCE: Kozier and Erbs Fundamentals of Nursing. Infection, 8th ed, p. 912 Cues Subjective: Dako akong samad. Ginabutangan pa gain ni ug binder para dili maukab and tahi kay sakit man. Objective: -horizontal incision in the hypogastric region of the abdomen with dressing Objectives Short term: At the end of 30 minutes of nursing intervention a) identify interventions to prevent/risk for infection b) identify the importance of the following the medication regimen. Nursing Interventions Independent 1)Observed for localized signs of infection at sutures or surgical incision wound 2)Noted signs and symptoms of sepsis; fever, chills, diaphoresis 3)Taught patient and SO how to cleanse incision Rationale -To check for any signs of infection -To give necessary interventions -To facilitate wound healing and prevent infection by minimizing Evaluation Short Term: After 30 minutes of nursing intervention, the objectives were fully met. Patient mentioned the importance of hygiene, medication compliance, proper wound dressing and early ambulation to prevent infection.
and abdominal binder noted -redness of surrounding skin noted
Long term: After 2 days of intervention, the client will be able to: a)demonstrate behaviors showing appropriate adaptation to present condition. b)achieve timely wound healing; be free of purulent drainage or erythema; be afebrile c)comply to medication regimen accordingly
site daily and remind the.m to change dressings as needed 4)Encouraged early ambulation and deep breathing ,coughing and position change Collaborative: 1) Administered Cefurex 500 mg 1 TAB 2x a day
growth and spread of microorganisms -Ambulation stimulates lower extremity circulation after caesarean birth
-Premature discontinuation of treatment when client begins to feel well may result in return of infection this is also to avoid parasitic infection -To avoid cross contamination of microorganisms
Long Term: After 2 days of nursing intervention, objectives were fully met. The patient was able to integrate interventions in her daily activities such as wound dressing, coughing and position changes. Patient also complied with the medication regimen.
2)Stressed aseptic or proper handwashing technique by all caregivers
References of the NCPS: Beers et. al.(2003). Merck Manual of Medical Information. 2nd Edition, Merck and Co, Inc. New York.
Doenges, et. al. (2008). Nursing Diagnosis Manual: planning, individualizing and documenting client care. Company: Philadelphia.
2nd Edition, F.A. Davis
Hopper, Paula D. and Linda S. Willams, (2003). Understanding Medical-Surgical Nursing. 2nd edition, F.A. Davis Company: Philadelphia. Kozier, Barbara and Erb, Gleonora, et. al. (2008). Fundamentals of Nursing: Concepts, Process and Practice (7th ed.). Philippines: Pearson Education South Asia Pte. Ltd.
You might also like
- Care Plan Small Bowel ObstructionDocument9 pagesCare Plan Small Bowel Obstructionshaleah80% (5)
- Ugib NCPDocument5 pagesUgib NCPJhuRise Ann Mangana100% (1)
- Actual Nursing Care Plan 2Document16 pagesActual Nursing Care Plan 2Alyanna Evangelista100% (2)
- NCP CholeDocument8 pagesNCP CholeAndrewAlvinTemploNo ratings yet
- CA - Amniotic Fluid EmbolismDocument13 pagesCA - Amniotic Fluid EmbolismRodelen Maraño100% (2)
- SCIATICA EXERCISES Functional BestDocument3 pagesSCIATICA EXERCISES Functional BestMellow Moon RecordsNo ratings yet
- Planning (Nursing Care Plans)Document10 pagesPlanning (Nursing Care Plans)Kier Jucar de GuzmanNo ratings yet
- DengueDocument14 pagesDengueKarenn Joy Concepcion OctubreNo ratings yet
- Example Nursing Diagnosis and Careplan For N205 Mini Careplanspote Ntial ForDocument25 pagesExample Nursing Diagnosis and Careplan For N205 Mini Careplanspote Ntial ForCorina RadulescuNo ratings yet
- Ineffective Tissue PerfussionDocument2 pagesIneffective Tissue Perfussionmonico39No ratings yet
- Cardiovascular Disease Concept MapDocument5 pagesCardiovascular Disease Concept MapRye Anch100% (1)
- NCP TahbsoDocument18 pagesNCP TahbsoKe EjieNo ratings yet
- NCPDocument10 pagesNCPCristina L. JaysonNo ratings yet
- Concept MapDocument6 pagesConcept Mapmenickel3100% (1)
- NCPDocument14 pagesNCPclaidelynNo ratings yet
- NCPDocument13 pagesNCPÍam KristineNo ratings yet
- Lang 2011Document14 pagesLang 2011aungmyintkyawdrNo ratings yet
- Postoperative Hip Answer SheetDocument19 pagesPostoperative Hip Answer SheetCrisha Ann Billones BacutaNo ratings yet
- Management of Dengue Hemorrhagic FeverDocument7 pagesManagement of Dengue Hemorrhagic FeverjoycevillamorNo ratings yet
- Pain N TensDocument19 pagesPain N TensHimanshu YadavNo ratings yet
- DIABETES Nursing ManagementDocument11 pagesDIABETES Nursing ManagementKaloy KamaoNo ratings yet
- Medical History Physical Exam Chest X-Ray Clinical Signs Breath Sounds Fremitus Pleural Friction Rub Egophony TrachealDocument8 pagesMedical History Physical Exam Chest X-Ray Clinical Signs Breath Sounds Fremitus Pleural Friction Rub Egophony TrachealCholo Mercado ManalastasNo ratings yet
- Nursing Care PlanDocument23 pagesNursing Care PlanLorielle HernandezNo ratings yet
- Gynaecology and Acupuncture: Briefing Paper No 4Document9 pagesGynaecology and Acupuncture: Briefing Paper No 4Liliac41No ratings yet
- Case StudyDocument4 pagesCase StudyStar AlvarezNo ratings yet
- Nursing Care Plan For Appendicitis Post OperativeDocument17 pagesNursing Care Plan For Appendicitis Post OperativeOkaRizukiramanNo ratings yet
- PheochromocytomaDocument24 pagesPheochromocytomacamelle sisonNo ratings yet
- NCP JulieDocument14 pagesNCP JulieJulie Mae RubioNo ratings yet
- 4 Phases of IV Fluid Therapy FinalDocument29 pages4 Phases of IV Fluid Therapy FinalLuqmanul Hakim Junaidden100% (1)
- Critical Care - Criteria For Admission & Role of NurseDocument64 pagesCritical Care - Criteria For Admission & Role of NurseProf. Ramsharan MehtaNo ratings yet
- SCR 270 L & D Care PlanDocument5 pagesSCR 270 L & D Care PlanRenzo MarcosNo ratings yet
- Ineffective Tissue Perfusion Related To Decreased HGB Concentration in Blood Secondary ToDocument6 pagesIneffective Tissue Perfusion Related To Decreased HGB Concentration in Blood Secondary Toericke_tanNo ratings yet
- Atuação em DisfagiaDocument4 pagesAtuação em DisfagiaconradNo ratings yet
- Gnur 405 SuzyDocument6 pagesGnur 405 SuzySeth MensahNo ratings yet
- Nursing Diagnosis Impaired Gas ExchangeDocument7 pagesNursing Diagnosis Impaired Gas ExchangeZycon Rodney Ae'zecquel Gachallan50% (2)
- Impaired Tissue IntegritiyDocument2 pagesImpaired Tissue IntegritiyPaolo Martin CuaycongNo ratings yet
- NCPDocument11 pagesNCPJaziel Remo100% (1)
- College of NursingDocument54 pagesCollege of NursingJan VillaminNo ratings yet
- 5NCPDocument4 pages5NCPSara ThorntonNo ratings yet
- Cues Nursing Diagnosis Scientific Rationale Objective Nursing Interventi ON Rationale EvaluationDocument9 pagesCues Nursing Diagnosis Scientific Rationale Objective Nursing Interventi ON Rationale EvaluationTamil VillardoNo ratings yet
- NCPDocument4 pagesNCPEugine Elizabeth Pilarca PerezNo ratings yet
- Extubacion British 2010Document4 pagesExtubacion British 2010fciccioliNo ratings yet
- Pediatrics Care Plan Kawasaki Disease Final Draft and CorrectedDocument9 pagesPediatrics Care Plan Kawasaki Disease Final Draft and CorrectedValencia Vickers50% (4)
- Could Patient Controlled Thirst Driven Fluid Administration 2018 British JouDocument7 pagesCould Patient Controlled Thirst Driven Fluid Administration 2018 British JouSeveNNo ratings yet
- New Born NCPDocument8 pagesNew Born NCPCarl Vincent Marrion Rejuso100% (1)
- Trial of Continuous or Interrupted Chest Compressions During CPRDocument12 pagesTrial of Continuous or Interrupted Chest Compressions During CPRDinar Riny NvNo ratings yet
- Gynecology and ObstetricsvvvvvvvvvvvvvvvvvvvvvvvvvvvvvvvvvvvvvvvvvDocument133 pagesGynecology and ObstetricsvvvvvvvvvvvvvvvvvvvvvvvvvvvvvvvvvvvvvvvvvȚurcan IurieNo ratings yet
- Clinical Decision MakingDocument8 pagesClinical Decision Makingapi-400245000100% (1)
- An Evaluation of Chest Physiotherapy in The Management of Acute Bronchiolitis Changing Clinical Practice PDFDocument6 pagesAn Evaluation of Chest Physiotherapy in The Management of Acute Bronchiolitis Changing Clinical Practice PDFKopi143No ratings yet
- Concept Map 1Document5 pagesConcept Map 1api-396919069No ratings yet
- OBcarestudyDocument9 pagesOBcarestudyJezza Sanchez-Rellita VillariasNo ratings yet
- NCP CalculiDocument8 pagesNCP CalculihailleyannNo ratings yet
- The Active Management of Postpartum Uterine - OJOG - 2016092815312813Document9 pagesThe Active Management of Postpartum Uterine - OJOG - 2016092815312813Stella Putri WandaNo ratings yet
- VIII. Nursing Care PlanDocument12 pagesVIII. Nursing Care PlanNefre Dayap DarrocaNo ratings yet
- NCP PleuralDocument5 pagesNCP Pleuraljanine_valdezNo ratings yet
- Assessment Task-Case Study: Student's Name Institutional Affiliation Course Name and Number Professor's Name DateDocument11 pagesAssessment Task-Case Study: Student's Name Institutional Affiliation Course Name and Number Professor's Name DateleakyNo ratings yet
- Ineffective Tissue PerfusionDocument2 pagesIneffective Tissue PerfusionClaidelyn De Leyola100% (1)
- EVALUATION OF THE INFLUENCE OF TWO DIFFERENT SYSTEMS OF ANALGESIA AND THE NASOGASTRIC TUBE ON THE INCIDENCE OF POSTOPERATIVE NAUSEA AND VOMITING IN CARDIAC SURGERYFrom EverandEVALUATION OF THE INFLUENCE OF TWO DIFFERENT SYSTEMS OF ANALGESIA AND THE NASOGASTRIC TUBE ON THE INCIDENCE OF POSTOPERATIVE NAUSEA AND VOMITING IN CARDIAC SURGERYNo ratings yet
- Top Trials in Gastroenterology & HepatologyFrom EverandTop Trials in Gastroenterology & HepatologyRating: 4.5 out of 5 stars4.5/5 (7)
- Individual Therapy Key PointsDocument9 pagesIndividual Therapy Key PointsCristina L. JaysonNo ratings yet
- New Bon-NleDocument3 pagesNew Bon-NleCristina L. JaysonNo ratings yet
- Mindanao Sanitarium & Hospital College: D.R. Form Actual Delivery FormDocument1 pageMindanao Sanitarium & Hospital College: D.R. Form Actual Delivery FormCristina L. JaysonNo ratings yet
- References For Drug Study and Diagnostic TestsDocument2 pagesReferences For Drug Study and Diagnostic TestsCristina L. JaysonNo ratings yet
- PRC TinaDocument4 pagesPRC TinaCristina L. JaysonNo ratings yet
- Grand Case Presentation InformationDocument7 pagesGrand Case Presentation InformationCristina L. JaysonNo ratings yet
- NCPDocument10 pagesNCPCristina L. JaysonNo ratings yet
- Table 2. Division Family Species Chainforming or SolitaryDocument2 pagesTable 2. Division Family Species Chainforming or SolitaryCristina L. JaysonNo ratings yet
- Project Contract For Phyto Ra-2Document1 pageProject Contract For Phyto Ra-2Cristina L. JaysonNo ratings yet
- 3vital Information: Year) - BSED BioDocument3 pages3vital Information: Year) - BSED BioCristina L. JaysonNo ratings yet
- Imblanced NutritionDocument2 pagesImblanced NutritionCristina L. JaysonNo ratings yet
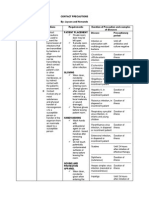
- Contact PrecautionsDocument2 pagesContact PrecautionsCristina L. JaysonNo ratings yet
- Drugs Dosage Nursing Implications: Discharge PlanDocument2 pagesDrugs Dosage Nursing Implications: Discharge PlanCristina L. JaysonNo ratings yet
- A. Identifying Potentially Infectious Patients: V. Transmission-Based PrecautionsDocument2 pagesA. Identifying Potentially Infectious Patients: V. Transmission-Based PrecautionsCristina L. JaysonNo ratings yet
- Radial Neck Fractures in ChildrenDocument4 pagesRadial Neck Fractures in ChildrenAndikaNo ratings yet
- Overuse Injuries and Burnout in Youth Sports A PosDocument17 pagesOveruse Injuries and Burnout in Youth Sports A PosChi Chung CHANNo ratings yet
- 96A0379Document88 pages96A0379flotterotterNo ratings yet
- Head Gestured Automated Wheelchair: Bachelor of Technology Department of MECHANICAL EngineeringDocument42 pagesHead Gestured Automated Wheelchair: Bachelor of Technology Department of MECHANICAL EngineeringNimitesh SinghNo ratings yet
- Small Fragment Set: - Features and Benefits - Indications - Operative Technique - Ordering InformationDocument20 pagesSmall Fragment Set: - Features and Benefits - Indications - Operative Technique - Ordering InformationRicardo_CHES1986No ratings yet
- 20 - Deltoids - Ant, Lat, PostDocument34 pages20 - Deltoids - Ant, Lat, Postbreinfout fotos100% (1)
- Elbow AbnormalDocument21 pagesElbow Abnormalsingle_ladyNo ratings yet
- Atrium Handbook Chest ManagingDocument40 pagesAtrium Handbook Chest ManagingrostaidaNo ratings yet
- Anatomy, Back, Scapula: Paul T. Cowan Matthew VaracalloDocument6 pagesAnatomy, Back, Scapula: Paul T. Cowan Matthew Varacalloaccounts 3 lifeNo ratings yet
- Ergonomics NotesDocument15 pagesErgonomics NotesSarah Abdalla100% (1)
- Turning ABGs Into Childs PlayDocument35 pagesTurning ABGs Into Childs PlayLucyz KlosetNo ratings yet
- List of Rogue WavesDocument6 pagesList of Rogue WavesdescataNo ratings yet
- ZF Repair Manaul Tranmission HBF 15 - 18-II and - 5Document47 pagesZF Repair Manaul Tranmission HBF 15 - 18-II and - 5ahmed_eng_1500100% (2)
- Critical Hits - Teeth & Claws DamageDocument3 pagesCritical Hits - Teeth & Claws DamageМихаил ПотаповNo ratings yet
- Learners With Additional Needs: Module 8Document33 pagesLearners With Additional Needs: Module 8Mary Joy CordoveroNo ratings yet
- MAPEH 9 1st Monthly ExamDocument3 pagesMAPEH 9 1st Monthly Examjohann reyesNo ratings yet
- Orthopedic Manual TherapyDocument56 pagesOrthopedic Manual TherapyWalaa EldesoukeyNo ratings yet
- DM Consunji v. CA. GR No. 137873. Digest.Document1 pageDM Consunji v. CA. GR No. 137873. Digest.Maribel Nicole Lopez100% (1)
- UNIT IV Intentional InjuriesDocument17 pagesUNIT IV Intentional InjuriesLiana Kay RevillozaNo ratings yet
- 04 1 Pengaturan Proses PemasakanDocument79 pages04 1 Pengaturan Proses PemasakanSasqia Annissa P0% (1)
- Right Inguinal Hernia RepairDocument1 pageRight Inguinal Hernia Repairsgod34No ratings yet
- Stretches For Brachial PlexusDocument2 pagesStretches For Brachial PlexusRa RNo ratings yet
- CraniotomyDocument6 pagesCraniotomychaSephNo ratings yet
- Anterior Knee PainDocument11 pagesAnterior Knee PainViswanathNo ratings yet
- Failure of Weaning:: According To The European Respiratory Society (ERS) Task ForceDocument12 pagesFailure of Weaning:: According To The European Respiratory Society (ERS) Task ForceAmr El Taher0% (1)
- SangDocument74 pagesSangEriq GardnerNo ratings yet
- SU99Document52 pagesSU99javicho2006No ratings yet
- Icm SPMRDocument2 pagesIcm SPMRmahmoud4871No ratings yet
- Knee OsteoarthritisDocument3 pagesKnee OsteoarthritispandukajayakuruNo ratings yet