Professional Documents
Culture Documents
Lethargy and General Malaise: Clinical Features
Uploaded by
Kinanthi SabilillahOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Lethargy and General Malaise: Clinical Features
Uploaded by
Kinanthi SabilillahCopyright:
Available Formats
20 Symptoms of heart failure GENERAL HF has many causes, as described in Chapter 1.
A high index of suspicion is necessary in patients with predisposing conditions, such as a previous history of MI, diabetes, or hypertension. It is important not to discount the diagnosis of HF in young patients, as dilated cardiomyopathy can occur at any age. If the diagnosis is not considered, such patients may be readily misdiagnosed as having asthma, for example.
Lethargy and general malaise
Clinical features Table 11 Causes of oedema Heart failure Gravitational oedema Hypoproteinaemia Liver disease Nephrotic syndrome Lymphoedema Medications calcium channel blockers, e.g. amlodipine Table 12 Diagnostic sensitivity and specificity of clinical features of heart failure Clinical features Sensitivity (%)
21
For many patients with chronic HF, the most debilitating symptom is tiredness. Patients may have difficulty sleeping due to other symptoms of HF, but lethargy is itself a feature of HF, and has a profound effect on patients exercise capacity and quality of life, over and above that caused by breathlessness and other symptoms. Patients with HF also typically report increased muscle fatigue on exertion, contributing to reduced exercise capacity. Skeletal muscle metabolism has been shown to be abnormal in HF (Table 10). Some patients with HF may present only with feelings of general malaise, and careful questioning may be necessary to detect other symptoms of HF.
Loss of appetite
Patients with heart failure may complain of loss of appetite, which may be due to bowel oedema. Weight loss due to such anorexia may be masked by fluid accumulation, and become apparent only when diuretic therapy is instituted. Poor nutrition due to anorexia combined with reduced absorption from the oedematous bowel eventually results in cardiac cachexia, and the resulting reduction in muscle bulk compounds lethargy and breathlessness. Patients may also complain of right upper quadrant discomfort or pain, caused by liver congestion and capsular stretch. Table 10 Muscle abnormalities in heart failure Wasting Impaired resting blood flow Limited capacity to enhance blood flow on exertion Increased fatigue Abnormal metabolism Early anaerobic metabolism Early intracellular acidosis (From Harlan WR, et al. Ann. Intern. Med. 1977;86:133138.)
BREATHLESSNESS Shortness of breath is the most well known symptom of HF, but is a common symptom of many conditions, and therefore is not very specific for HF. Classically, patients complain of orthopnoea (breathlessness when lying flat), which may be quantified by asking how many pillows the patient uses in bed. Paroxysmal nocturnal dyspnoea (PND; episodic breathlessness waking the patient from sleep) is another classic symptom of HF and, again, the frequency of such episodes can be useful in quantifying severity. Not all patients complain of these symptoms, however, and their absence does not rule out the possibility of a diagnosis of HF. Acute HF most often presents with extreme breathlessness of very sudden onset, such that the patient is often too breathless to talk. Diagnosis in this circumstance relies on clinical examination and investigation, although witnesses may be able to provide some clues. HF should always be considered in the acutely breathless patient. Where there is diagnostic doubt, a trial of a diuretic may result in rapid improvement in the patient with HF. Patients with more insidious onset of HF may describe gradually worsening shortness of breath, and decreasing exercise tolerance over weeks or months. Cough may be an early symptom of HF, and some patients may complain of wheeze, caused by oedema of the bronchial tree, both of which may initially suggest the diagnosis of asthma. PERIPHERAL OEDEMA In some patients, the first symptom of HF may be development of peripheral oedema. The patients usual posture determines the location of oedema: ambulant patients typically initially develop oedema of the ankles which resolves overnight; patients who are immobile may develop oedema predominantly over the sacrum. Oedema has many causes, particularly gravitational in immobile patients. Other causes of oedema may be mistaken for, or coexist with, HF (Table 11). Oedema is classically a sign of right-sided HF, for example in the patient with chronic obstructive pulmonary disease (cor pulmonale), but even in patients with predominant left-sided HF, oedema may be the main presenting feature with breathlessness less apparent. Signs of heart failure In some patients, clinical examination may make the diagnosis clear, but some patients with early HF may have few or no apparent clinical signs. In addition, the signs associated with HF have other
Specificity (%) 52 81 76 80 99 91 93 95 97
43
Breathlessness 66 Orthopnea 21 PND 33 Oedema (history) 23 Tachycardia 7 Pulmonary crackles 13 Oedema (examination) 10 Third heart sound 31 Raised JVP 10 PND: paroxysmal nocturnal dyspnoea; JVP; jugular venous pulsation
44
43 Noonan's syndrome short webbed neck, low-set ears, high nasal bridge; may be subtle and present in adulthood.
44 Atrial septal defect associated with Noonans syndrome.
45
causes which must be considered. Table 12 presents the diagnostic sensitivity and specificity of clinical features of heart failure. GENERAL EXAMINATION Careful general examination may reveal useful information. Although HF is most commonly caused by ischaemic heart disease or hypertension, rarer causes must not be forgotten. Characteristic facies may be present. For example, Noonans syndrome, which is associated with congenital heart disease (43. 44), or tuberose sclerosis (45) which may be associated with cardiac rhabdomyoma, which can be present as HF in
45 Tuberose sclerosis facial angiofibroma.
22 childhood. Systemic disorders such as gout (46, 47), dyslipidaemia (48), scleroderma (49, 50), connective tissue disorders (e.g. EhlersDanlos syndrome [51, 52] or Marfan syndrome [53], both associated with mitral valve prolapse), or neurofibromatosis (Von Recklinghausen syndrome [5457, 76]) may provide clues. Hypothyroidism is associated with HF and the typical myxoedema facies should not be missed (5860). 53 High arched palate in a patient with Marfan syndrome.
Clinical features
53
23
54
46
47
48
55
57 56
46 Chronic tophaceous gout.
47 Chronic tophaceous gout.
48 Cutaneous xanthomata in a patient with dyslipidaemia.
49
50
5456 Von Recklinghausen syndrome caf-au-lait spots. 57 Von Recklinghausens disease showing multiple neurofibromata.
58 59
58 Myxoedema facies. 59 2D echocardiogram showing pericardial effusion due to hypothyroidism (arrow).
49 Scleroderma tight, shiny skin over fingers, loss of finger pulp.
51
50 Skin in scleroderma showing telangiectasia.
52
60 Electrical alternans in a patient with a large pericardial effusion. Alternating large and small QRS complexes caused by the heart swinging within the pericardial fluid.
60
51, 52 EhlersDanlos syndrome demonstration of skin laxity.
24 Carcinoid syndrome is associated with right-sided valvular abnormalities (6163). Patients with chronic HF are often anaemic (64). Anaemia may be due to poor nutrition, or alternatively due to anaemia of chronic disease. Anaemia may be sufficiently severe as to be apparent clinically. Recognition of anaemia is important, as correction may lead to an improvement in functional status. Cachexia may occur in chronic HF (65, 66). Weight loss may be masked by accumulation of oedema, but loss of muscle bulk in the face and upper body may be clearly visible. Cachexia is a poor prognostic sign, and indicates severe HF. Oedema may be the most obvious clinical sign of heart failure. It may range from subtle pitting to pressure over the tibia (67, 68), to gross oedema extending up to the abdomen and genitalia (69). Patients treated with diuretics may become dehydrated even in the presence of persistent oedema. Reduction of skin turgor and reduced urine output may accompany dehydration. During therapy, fluid status can be monitored by weighing.
Clinical features
65
25
66
66 Cachexia note severe loss of upper arm musculature.
65 Patient with advanced heart failure: note pitting oedema, ascites, and cachexia.
61
62
67
68
61 Facial telangiectasia in carcinoid syndrome.
62 Fibrotic tricuspid valve in carcinoid syndrome.
67, 68 Pitting peripheral oedema.
63
64
69
69 All body oedema.
63 Excised carcinoid tricuspid valve.
64 Patient with heart failure and clinical anaemia.
26 Cardiovascular drugs, for example long-term therapy with amiodarone, may induce certain clinical features (70). Certain cardiac conditions may provide features on clinical examination, for example infective endocarditis (7174). CARDIOVASCULAR EXAMINATION Cardiovascular examination is obviously important in the detection of HF, and may provide additional information concerning the underlying cause. Full cardiovascular examination may be difficult in the
Clinical features
27
75
patient with acute breathlessness; in this situation a limited initial examination may be followed by detailed examination once therapy has commenced and symptoms have started to improve.
Pulse
75 Raised jugular venous pulsation.
70
70 Amiodarone facial discoloration (slate-grey appearance).
71
Examination of the pulse often reveals tachycardia (compensating for reduced stroke volume), even in patients who are asymptomatic at rest. In acute HF, the radial pulse may be weak, and tachycardia may be extreme. Atrial fibrillation (AF) is common in HF, and the ventricular rate may be very rapid. Recognition and early treatment of AF may rapidly produce improvement in clinical status.
Jugular venous pulsation
71 Digital gangrene in infective endocarditis.
72
73
The jugular venous pulsation (JVP) is regarded as a barometer of right atrial pressure, and may be raised in HF (75). It should be assessed with the patient lying at 45 degrees. It is useful to differentiate HF clinically from other causes of peripheral oedema (such as hypoproteinaemia, where the JVP is likely to be low), but it has low sensitivity for HF. It may not be visible in the obese patient, or the patient with acute HF and severe breathlessness. The absence of a raised JVP should not rule out the possibility of heart failure.
Palpation
of these signs take time to develop, and may well be absent in patients with HF of acute onset.
Auscultation
Auscultation may be difficult in the breathless patient. Tachycardia may also mask signs. There may be a third or fourth heart sound (due to rapid ventricular filling or atrial contraction against a stiff left ventricle, respectively), or murmurs of underlying valve disease (or functional mitral regurgitation). The presence of a third heart sound is specific for HF, but has a high interobserver variability.
Blood pressure
Valve lesions may be associated with palpable thrills. A right ventricular heave may be present in patients with pulmonary hypertension and right-sided HF (for example, cor pulmonale). Palpation of the cardiac apex may show lateral displacement from the normal position (5th intercostal space, midclavicular line). The character of the apex beat may also be abnormal. A sustained, heaving apex may occur. All 72, 73 Vasculitic spots (Janeway lesion) in infective endocarditis.
74
Blood pressure measurement should be part of cardiovascular examination. High blood pressure should be detected, treated, and controlled. Rarely, unusual causes of hypertension, such as phaeochromocytoma (76, 77) and renal artery stenosis (78) should be considered as causes of HF.
76
77
78
77 MIBG (meta-iodobenzyl guanidine) scan of phaeochromocytoma (arrows).
74 Splinter haemorrhages in infective endocarditis.
76 Renal angiogram showing phaeochromocytoma (arrow) (here associated with Von Recklinghausen syndrome).
78 Renal artery stenosis (arrow) and distal aortic stenosis (arrowhead).
You might also like
- Respiratory Distress - Tintanalli's Emergency MedicineDocument31 pagesRespiratory Distress - Tintanalli's Emergency MedicineRon KNo ratings yet
- Clinical Features and Complications: ABC of Heart FailureDocument4 pagesClinical Features and Complications: ABC of Heart FailureGheavita Chandra DewiNo ratings yet
- Acute Heart FailureDocument9 pagesAcute Heart FailureChen Briones100% (1)
- Background: Congestive Heart FailureDocument5 pagesBackground: Congestive Heart FailureyasayyasayNo ratings yet
- Cardio CHFDocument18 pagesCardio CHFHajime NakaegawaNo ratings yet
- Clinical Features and Complications: ABC of Heart FailureDocument4 pagesClinical Features and Complications: ABC of Heart FailureMohammed Ali Haydar JafferiNo ratings yet
- Cardiomyopathy and myocarditis: Causes, symptoms, diagnosis and treatmentDocument69 pagesCardiomyopathy and myocarditis: Causes, symptoms, diagnosis and treatmentImmanuel100% (1)
- Congestive Heart FailureDocument19 pagesCongestive Heart FailureIlavenil PanduranganNo ratings yet
- PE of The CVS DR ParadoDocument51 pagesPE of The CVS DR ParadoDhrub Chandra PanditNo ratings yet
- Heart Failure DDx and WorkupDocument3 pagesHeart Failure DDx and WorkupAizel ManiagoNo ratings yet
- Internal Medicine (Ans) - M3 Question BankDocument15 pagesInternal Medicine (Ans) - M3 Question BankWu YanlongNo ratings yet
- PVDDocument7 pagesPVDmiss RNNo ratings yet
- Heart Failure Clinical Presentation - History, Physical Examination, Predominant Right-Sided Heart FailureDocument12 pagesHeart Failure Clinical Presentation - History, Physical Examination, Predominant Right-Sided Heart FailureAshutosh SinghNo ratings yet
- Jurnal Print 3Document17 pagesJurnal Print 3Elok ZakiyyaNo ratings yet
- Unit 1 The History and Smmptoms Iovascular Disease: ObjectivesDocument9 pagesUnit 1 The History and Smmptoms Iovascular Disease: ObjectivesbtaleraNo ratings yet
- Usmle World Step 2 NotesDocument241 pagesUsmle World Step 2 NotesAdnan MallickNo ratings yet
- High output heart failure: a reviewDocument7 pagesHigh output heart failure: a reviewChanvira Aria CandrayanaNo ratings yet
- Diastolic DysfunctionDocument39 pagesDiastolic Dysfunctionkaaalifa12No ratings yet
- Congestive Heart Failure/Pulmonary Edema Case FileDocument4 pagesCongestive Heart Failure/Pulmonary Edema Case Filehttps://medical-phd.blogspot.comNo ratings yet
- Heart Failure Clinical Presentation GuideDocument9 pagesHeart Failure Clinical Presentation GuideAizel ManiagoNo ratings yet
- I. Acute Heart Failure: What Every Physician Needs To KnowDocument13 pagesI. Acute Heart Failure: What Every Physician Needs To KnowRubie Ann TillorNo ratings yet
- Embolia PulmonaraDocument3 pagesEmbolia PulmonaraAlina GheNo ratings yet
- KP 2.5.5.3 Cor PulmonaleDocument17 pagesKP 2.5.5.3 Cor Pulmonalenurul ramadhiniNo ratings yet
- Cor Pulmonale: The Disease of the Right HeartDocument40 pagesCor Pulmonale: The Disease of the Right HeartIbtissame BadadNo ratings yet
- Final Anesthesia Reviw Flash CardsDocument217 pagesFinal Anesthesia Reviw Flash Cardsaljuhanita100% (1)
- Heart Failure: Causes, Symptoms, and TreatmentDocument36 pagesHeart Failure: Causes, Symptoms, and TreatmentnathanNo ratings yet
- Causes and evaluation of respiratory failureDocument8 pagesCauses and evaluation of respiratory failurejeanie mae PangapalanNo ratings yet
- Acute Heart Failure and Pulmonary EdemaDocument48 pagesAcute Heart Failure and Pulmonary EdemaSol Gat ChupataNo ratings yet
- Heart Failure & Cor PulmunaleDocument12 pagesHeart Failure & Cor PulmunaleShrestha AnjivNo ratings yet
- Dr Mohammed Jamsheed's Guide to Acute Respiratory Distress Syndrome (ARDSDocument53 pagesDr Mohammed Jamsheed's Guide to Acute Respiratory Distress Syndrome (ARDSavicennax100% (1)
- Congestive Heart Failure: Dr. Asif WazirDocument21 pagesCongestive Heart Failure: Dr. Asif WazirHillary BushnellNo ratings yet
- Chronic Congestive Heart FailureDocument10 pagesChronic Congestive Heart FailureEllappa GhanthanNo ratings yet
- Cardinal Presentations Guide Hsas 21.11.2019Document20 pagesCardinal Presentations Guide Hsas 21.11.2019Nurhafizah IbrahimNo ratings yet
- Cardiovascular Diseases: DR - Priyanka Sharma 1st Year MDS Dept of Public Health DentistryDocument183 pagesCardiovascular Diseases: DR - Priyanka Sharma 1st Year MDS Dept of Public Health DentistryHidayat Abdullah Nya' MakamNo ratings yet
- DR Ali Cardiology-MergedDocument684 pagesDR Ali Cardiology-MergedK PradhanNo ratings yet
- Path o PhysiologyDocument163 pagesPath o PhysiologyDiorella Marie López González100% (2)
- Shock 20231122 213304 0000Document32 pagesShock 20231122 213304 0000Mikella E. PAGNAMITANNo ratings yet
- Clinical Manifestations and Evaluation of The Patient With Suspected Heart Failure PDFDocument23 pagesClinical Manifestations and Evaluation of The Patient With Suspected Heart Failure PDFcristianamihailaNo ratings yet
- Assessment of Breathlessness Clinical Pathway Assessment HandoutDocument8 pagesAssessment of Breathlessness Clinical Pathway Assessment HandoutShivaniNo ratings yet
- 61 Rab Nawaz (Stroke DD)Document23 pages61 Rab Nawaz (Stroke DD)SardarChangezKhanNo ratings yet
- Pitfalls in The Evaluation of Shortness Breath - The ClinicsDocument19 pagesPitfalls in The Evaluation of Shortness Breath - The ClinicsEdgardo Vargas AlvarezNo ratings yet
- Xing Meng Emergency Center of The First Affiliated Hospital of Zhengzhou University, ZhengzhouDocument67 pagesXing Meng Emergency Center of The First Affiliated Hospital of Zhengzhou University, Zhengzhouapi-19916399No ratings yet
- Orthopedic: Complications of FracturesDocument11 pagesOrthopedic: Complications of FracturesDrAyyoub AbboodNo ratings yet
- Acute Respiratory FailureDocument17 pagesAcute Respiratory FailurejulianajosNo ratings yet
- Heart Failure: Abdul Hafiz AliasDocument19 pagesHeart Failure: Abdul Hafiz AliasAbdul Hafiz Alias100% (5)
- Ehad 883Document3 pagesEhad 883nhunhuochachNo ratings yet
- Acute Respiratory Distress Syndrome (Ards) and Sepsis: Frans Abednego Barus Spesialis ParuDocument29 pagesAcute Respiratory Distress Syndrome (Ards) and Sepsis: Frans Abednego Barus Spesialis Paruarif qadhafyNo ratings yet
- Acute Biologic Crisis-ArDocument71 pagesAcute Biologic Crisis-ArJayvee Novenario CasaljayNo ratings yet
- Slow Heart Rate (Bradycardia)Document2 pagesSlow Heart Rate (Bradycardia)Mhar IcelNo ratings yet
- StrokeDocument15 pagesStrokedzulfachriNo ratings yet
- Differential diagnosis of epilepsy and non-epileptic eventsDocument15 pagesDifferential diagnosis of epilepsy and non-epileptic eventsxuexueNo ratings yet
- Acute Pulmonary Edema - NEJMDocument4 pagesAcute Pulmonary Edema - NEJMSuzika Dewi0% (1)
- TachycardiaDocument9 pagesTachycardiaSharlene Anna Natassia OzairsNo ratings yet
- Medicine in Brief: Name the Disease in Haiku, Tanka and ArtFrom EverandMedicine in Brief: Name the Disease in Haiku, Tanka and ArtRating: 5 out of 5 stars5/5 (1)
- Cardiac Care and COVID-19: Perspectives in Medical PracticeFrom EverandCardiac Care and COVID-19: Perspectives in Medical PracticeNo ratings yet
- Finish DHFDocument1 pageFinish DHFKinanthi SabilillahNo ratings yet
- Daftar PustakaDocument1 pageDaftar PustakaAchmad FitrahNo ratings yet
- Sindrom Metabolik Dan Defisiensi Testosteron: Samsul MustofaDocument7 pagesSindrom Metabolik Dan Defisiensi Testosteron: Samsul MustofaKinanthi SabilillahNo ratings yet
- Laporan Tutorial CoverDocument2 pagesLaporan Tutorial CoverKinanthi SabilillahNo ratings yet
- The Steriotypes: Cultural StereotypeDocument8 pagesThe Steriotypes: Cultural StereotypeRosbeyli Mazara ReyesNo ratings yet
- Corporate Law Scope and RegulationDocument21 pagesCorporate Law Scope and RegulationBasit KhanNo ratings yet
- BCIC General Holiday List 2011Document4 pagesBCIC General Holiday List 2011Srikanth DLNo ratings yet
- Explaining ADHD To TeachersDocument1 pageExplaining ADHD To TeachersChris100% (2)
- Italy VISA Annex 9 Application Form Gennaio 2016 FinaleDocument11 pagesItaly VISA Annex 9 Application Form Gennaio 2016 Finalesumit.raj.iiit5613No ratings yet
- The Wild PartyDocument3 pagesThe Wild PartyMeganMcArthurNo ratings yet
- The Serpents Tail A Brief History of KHMDocument294 pagesThe Serpents Tail A Brief History of KHMWill ConquerNo ratings yet
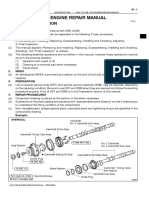
- How To Use This Engine Repair Manual: General InformationDocument3 pagesHow To Use This Engine Repair Manual: General InformationHenry SilvaNo ratings yet
- Ten - Doc. TR 20 01 (Vol. II)Document309 pagesTen - Doc. TR 20 01 (Vol. II)Manoj OjhaNo ratings yet
- (Template) Grade 6 Science InvestigationDocument6 pages(Template) Grade 6 Science InvestigationYounis AhmedNo ratings yet
- De So 2 de Kiem Tra Giua Ki 2 Tieng Anh 8 Moi 1677641450Document4 pagesDe So 2 de Kiem Tra Giua Ki 2 Tieng Anh 8 Moi 1677641450phuong phamthihongNo ratings yet
- Notes Socialism in Europe and RussianDocument11 pagesNotes Socialism in Europe and RussianAyaan ImamNo ratings yet
- PIA Project Final PDFDocument45 pagesPIA Project Final PDFFahim UddinNo ratings yet
- AI Capstone Project Report for Image Captioning and Digital AssistantDocument28 pagesAI Capstone Project Report for Image Captioning and Digital Assistantakg29950% (2)
- Arx Occasional Papers - Hospitaller Gunpowder MagazinesDocument76 pagesArx Occasional Papers - Hospitaller Gunpowder MagazinesJohn Spiteri GingellNo ratings yet
- York Product Listing 2011Document49 pagesYork Product Listing 2011designsolutionsallNo ratings yet
- FOCGB4 Utest VG 5ADocument1 pageFOCGB4 Utest VG 5Asimple footballNo ratings yet
- Prac Research Module 2Document12 pagesPrac Research Module 2Dennis Jade Gascon NumeronNo ratings yet
- IB Theatre: The Ilussion of InclusionDocument15 pagesIB Theatre: The Ilussion of InclusionLazar LukacNo ratings yet
- Sangam ReportDocument37 pagesSangam ReportSagar ShriNo ratings yet
- Kids' Web 1 S&s PDFDocument1 pageKids' Web 1 S&s PDFkkpereiraNo ratings yet
- Pharmaceuticals CompanyDocument14 pagesPharmaceuticals CompanyRahul Pambhar100% (1)
- Business Law Module No. 2Document10 pagesBusiness Law Module No. 2Yolly DiazNo ratings yet
- Aladdin and the magical lampDocument4 pagesAladdin and the magical lampMargie Roselle Opay0% (1)
- Maternity and Newborn MedicationsDocument38 pagesMaternity and Newborn MedicationsJaypee Fabros EdraNo ratings yet
- Irony in Language and ThoughtDocument2 pagesIrony in Language and Thoughtsilviapoli2No ratings yet
- Mari 1.4v2 GettingStartedGuide PDFDocument57 pagesMari 1.4v2 GettingStartedGuide PDFCarlos Vladimir Roa LunaNo ratings yet
- Sound! Euphonium (Light Novel)Document177 pagesSound! Euphonium (Light Novel)Uwam AnggoroNo ratings yet
- DRRR STEM 1st Quarter S.Y.2021-2022Document41 pagesDRRR STEM 1st Quarter S.Y.2021-2022Marvin MoreteNo ratings yet
- International Standard Knowledge Olympiad - Exam Syllabus Eligibility: Class 1-10 Class - 1Document10 pagesInternational Standard Knowledge Olympiad - Exam Syllabus Eligibility: Class 1-10 Class - 1V A Prem KumarNo ratings yet