Professional Documents
Culture Documents
Inflamation Notes
Uploaded by
Eric EvangelistaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Inflamation Notes
Uploaded by
Eric EvangelistaCopyright:
Available Formats
INFLAMMATORY and IMMUNOLOGIC DISTURBANCES IMMUNITY is the bodys specific protective response to an invading foreign agent or organism; ability
y of the body to fight or conquer infection. IMMUNOPATHOLOGY- the study of diseases that result from dysfunction of the immune system IMMUNE SYSTEM Function: 1. defense against physical injury and infection 2. maintenance of homeostasis, a state of equilibrium of the internal environment ORGANS and tissues of the immune system Bone marrow production site of RBC,s WBC,s and platelets. Its primary function is hematopoiesis (formation of blood cells) Thymus is a single unpaired gland that is located in the mediastinum and is the primary gland of the lymphatic system. Its primary function is allowing the T lymphocytes to develop before migrating to the lymph nodes and the spleen. Lymph nodes and vessels perform several important functions such as: transporting lymph, filtering and phagocytizing antigens, generating monocytes and lymphocytes. Spleen functions include: a. Removing worn out erythrocytes from blood, b. Storing blood and platelets c. Filtering and purifying blood. Tonsils, adenoids and other mucoid lymphatic tissues defend the body against microorganisms. Hematopoietic system(bone marrow) Central and Peripheral Lymphoid Organs CLASSIFICATIONOF IMMUNITY I. SPECIFIC IMMUNITY A. HUMORAL IMMUNITY characterized by production of antibodies by the B lymphocytes in response to a specific antigen. Antibodies are large proteins called immunoglobulins found in the globulin fraction of the plasma proteins. IgG 75% of total Ig in the body
- source: interstitial fluids( serum & tissues)
: passes to neonate thru breastmilk
IgM : 10% IgG Function: assumes major role in bloodborne infections : activates complement system : enhances phagocytosis : crosses placenta IgA - 15% - Source: blood, saliva, tears , breastmilk, prostatic, gastrointestinal and resp. secretions. Source: Serum - Function: protects against GI, GU, and respiratory infections. : prevents absorption of antigen from food reactions : combats parasitic infections ANTIGEN-ANTIBODY REACTION Agglutination antibodies disarmed antigens by Function: allergic and hypersensitivity Source: Intravascular Function: appears as the first Ig produced in response to bacterial and viral infections : activates complement system IgD : 0.2% Source: serum in small amount Function: influences B-lymphocytes but role is unclear IgE : 0.004%
causing them to clamp together Precipitation this reaction occurs when antibody reacts with a soluble antigen resulting in an insoluble complex which then precipitates. Neutralization this occurs when antibody combines with toxins produced by some infectious agents to render them inactive and easier to engulfed and removed from the body. Lysis this is when antibody attacks cell membrane causing microorganisms to rupture. Opsonization in this process, the antigen-antibody molecule is coated with a sticky substance that also facilitates phagocytosis. B. CELLULAR IMMUNITY T- lymphocytes are responsible for cellular immunity. These lymphocytes spend time in the thymus, wherein they are programmed to become T-cells.
causing cell lysis(disintegration) and releasing cytolytic enzymes and cytokines. II. NON-SPECIFIC IMMUNITY
Defenses of the body non selectively directed to foreign substances. 1. Structural certain specialized structures in the body that protect human from microorganisms. EX. Skin, eyebrow, eyelashes 2. Mechanical mechanical processes in the body protects it from foreign bodies. EX. Peristaltic activity, vomiting, diarrhea, tear flow 3. Chemical certain chemicals in the body fights microorganisms. Ex. urine, vaginal secretions, perspiration 4. Biologic these are bacteria that are considered normal flora and are essential for body processes. 5. Inflammatory Response considered as one of the major function of the non-specific immune system. It is the defensive reaction of the body intended to neutralize, control or eliminate the offending agent to prepare the site for repair.
2 major categories of T cells a. Helper T cells are activated upon recognition of antigens and stimulate the rest of the immune system. b. Cytotoxic T cells (Killer T cells) attack the antigen directly by altering the cell membrane and
INFLAMMATION - a biochemical and cellular process that occurs in vascularized tissues - most of the essential components of the inflammatory process are found in the vascularized circulation, and most of the early mediators(facilitators) of inflammation increase the movement of plasma and blood cells from the circulation into the tissues surrounding the injury called as the exudates which defends the host against infection and facilitate tissue repair and healing. CARDINAL SIGNS OF INFLAMMATION
transient vasoconstriction that follows injury Swelling results when vascular permeability increases, and plasma leaked into the inflamed tissues.
Pain results when the pressure of fluids or sealing on nerve endings, and to the irritation of the nerve endings in chemical mediators released at the site
Loss of function related to pain and swelling Loss of function happened when:
Redness (Rubor) Heat (Calor) Swelling (Tumor) Pain (Dolor) Loss of function (Laesa)
Vascular response transient vasoconstriction followed by vasodilation, causing influx of blood to the inflamed area. These fluid pushed into the surrounding sites of injury would consequently become inflammatory exudates which has the following functions as: - dilute toxins released by the bacteria - bring to site certain nutrients necessary for tissue repair
Redness and heat results when vasodilation occurs after
- carry protective cell that would destroy bacteria
a Wall-Off. 2. Cellular response as follows: a. Margination also known as pavementing occurs when leucocytes stick to the walls of the blood vessels. b. Emigration occurs when leococytes multiply and travel to the areas of injury c. Chemotaxis is the directional orientation of leucocytes d. Phagocytosis process where bacteria are engulfed or ingested. 3. Chemical response includes the release of the following chemicals. a. Histamine initiates vascular response by increasing vascular dilation and permeability b. Bradykinin increases vascular permeability c. Prostaglandin also increases vascular permeability. HUMORAL IMMUNITY - one of the two forms of immunity that respond to bacteria and other foreign antigens. It is mediated by circulating antibodies(immunoglobulins IgA, IgB and IgM), which coat the antigens and target them for destruction by polymorphonuclear neutrophils.
CELLULAR IMMUNITY - the mechanism of acquired immunity characterized by the dominant role of T-cell lymphocytes - is involved in resistance to infectious disease caused by viruses and some bacteria and is delayed hypersensitivity reactions, some aspects of resistance to cancer, certain autoimmune diseases, graft rejection and certain allergies. Antibody - an immunoglobulin produced by lymphocytes in response to bacteria, viruses, or other antigenic substances. - it is specific to antigen
4. Fibrin-Barrier Response fibrin forms wall on the inflamed area to prevent invasion of irritants to other tissues. This phenomenon is also known as
- it includes agglutinins, opsonins, and precipitins. Antigen - a substance usually a protein that causes the formation of an antibody and reacts specifically with that antigen.
Specificity of action The unique action of the last 2 properties is its diversity of ability to respond while at the same time responding with specificity of action.
TYPES OF IMMUNITY COMP ARISON OF HUMORAL AND CELLULAR CELL RESPONSE A. NATURAL IMMUNITY innate or genetically or primary HUMORAL IMMUNITY immunity. STAGES OF IMMUNE RESPONSE Recognition stage circulating lymphocytes and macrophages recognize foreign materials or antigens as nonself Proliferation stage sensitized lymphocytes proliferates, differentiate, and mature into T and B cells. Response stage antibody is produced with specific T-cell action. Effector stage antigen is destroyed by antibody, which is produced by B-cell or cytotoxic T-cell action. Properties of immune response Recognition able to recognize self from nonself Memory recalls type of antigen(pick up imprint of the antigen structure) Diversity of action - provides a nonspecific response to any foreign invader, regardless of the invaders composition. - the basis of natural defense mechanism is merely the ability to distinguish between self and nonself B. ACQUIRED IMMUNITY or secondary immunity is an immunologic response acquire during life but not present at birth. 1. ACTIVE ACQUIRED IMMUNITY a. Person develop his own antibodies b. Takes 10 t0 14 days to develop c. Permanent d. Body cells undergo change Active acquired immunity could either be:
* Natural having contact with antigen naturally such as getting sick or frequent exposure to smaller doses of microorganisms like: chickenpox, measles, mumps
globulin
* Artificial acquiring antigen through vaccines or Common diagnostic procedures toxoids like in BCG, DPT and POLIO. WBC count used to suggest the presence of infection, an allergy or leukemia. Used to help monitor the bodys response to various treatments 2. PASSIVE ACQUIRED IMMUNITY: and to monitor bone marrow function. Detects dangerously low number of WBC. a. Person receives preformed antibodies WBC differential count assesses the ability of the body to respond to and eliminate infection. Detects b. Provides immediate immunity the severity of allergic reactions; parasitic and other types of infection and drug reaction. c. Temporary d. No cellular changes INTRADERMAL TEST (MANTOUX TEST) (PPD) given intradermally in the forearm, with 10mm induration significant reaction is positive(+), reading done in 48-72 hours, if positive result, it does not mean that active disease is present, but indicates exposure to Tuberculosis. RADIO IMMUNO ASSAY (RIA) highly sensitive and specific assy method used to determine antibody concentrations or to determine the concentration of any substance against which specific antibody can be produced. ELISA(ENZYME LINKED IMMUNOSORBENT ASSAY
Passive acquired immunity could either be: * Natural acquired naturally during breastfeeding like from colostrum * Artificial having preformed antibodies such as antitoxins, antiserum and gammaglobulin, ex. Immune serum
identifies antibodies specifically against HIV. It does not establish diagnosis of AIDS, rather it indicates that the person has been exposed to or infected with HIV called SEROPOSITIVE. WESTERN BLOT ASSAY used to confirm seropositivity as identified by the ELISA. BONE MARROW BIOPSY assess the quantity and quality of each type of cell produced within the marrow. Used to document infection or tumor within the marrow. Tests to Evaluate Immune Function WBC count and differential Bone marrow biopsy Humoral and cellular immunity tests Phagocytic cell function test Complement component tests Hypersensitivty tests Specific antige
Presence of conditions and disorders: cancer/neoplasm, chronic illness, autoimmune disorders, surgery/trauma Allergies History of infection and immunization Genetic factors Lifestyle Medications and transfusions Pyschoneuroimmunologic factors
Categories of immunologic disorders A. IMMUNODEFICIENCY caused by a defect or deficiency in phagocytic cells, B lymphocytes, T lymphocytes or the complement system. = the clinical results of impaired function of one or more components of the immune or inflammatory response, including B cells, T cells, phagocytic cells and complement. = failure of these self-defense mechanisms to function at normal capacity.
Variables That Affect Immune System Function Age and gender Nutrition
enzyme. Cardinal symptoms of immunodeficiency: 1. recurrent infection 2. infections caused by normal flora 1. bacterial 3. poor response to treatment of infections 2. fungal 4. chronic diarrhea 3. viral infections IMMUNODEFICIENCES: Primary immunodeciency - rare disorder with genetic origins seen primarily in infants and young children - occurs if lymphocyte development is arrested or disrupted in the fetus or embryo. -symptoms usually develop early in life and children witrh these disorders seldom survive childhood. Hyperimmunoglobulinemia (HIE) syndrome a sex-linked recessive disorder found only among male. - characterized by PMN(polymorphonuclear cells) engulfing microorganisms but killing does not take place because PMN lack the necessary digestive 4. deep-seated cold abscess Bruton agammaglobulinemia results from lack of differentiation of B cell precursors into mature B cells. As a result, plasma cells are lacking, and the germinal centers from all lymphatic tissues disappears, leading to a complete lack of antibody production against invading bacteria, viruses and other pathogens. - thymus gland is intact and the response of T cell is normal. Hypogammaglobulinemia or Common Variable immunodeficiency (CVID) - results from lack of differentiation of B cells into plasma cells. - there is general lacking of immunoglobulins Major symptoms of HIE syndrome
in the blood.
- both the B cell and T cell are missing. - there is complete absence of humoral as well as cellular immunity caused by an X-linked or autosomal genetic abnormality.
Agammaglobulinemia the condition in which B cell development are totally or nearly absent. Di Georges syndrome or Thymic hypoplasia a Tcell deficiency that occurs when the thymus gland fails to develop normally during embryogenesis. Presenting signs: 1. recurrent infection 2. hypoparathyroidism 3. hypocalcemia 4. tetany 5. convulsions 6. congenital heart disease 7. renal abnormalities 8. abnormal faces Severe Combined Immunodeciency disease(SCID)
Ataxia telangiectasia characterized by uncoordinated muscle movement(Ataxia) and vascular lesions caused by dilated blood vessels(telangiectasia) usually occurs during the first 4 years of life
Nezelofs Syndrome the individual is born without thymus gland and have various degrees of B-cell immunodeficiency associated with various combinations of increased, decreased or normal immunoglobulin levels.
Wiscott-Aldrich Syndrome an SCID compounded by thrombocytopenia or loss of platelet. 2. Secondary Immunodeciency are common than primary deficiences and frequently occur as a result of underlying disease process or from treatment of these diseases:
Common cause: a. Malnutrition b. Chronic stress c. Burns d. Uremia e. Diabetes mellitus Acquired immunodeficiency Syndrome AIDS - the best known example of an acquired dysfunction of the immune system. - represents a frightening disease because of its extremely high mortality in untreated individuals. Etiology : HIV or retrovirus Risk factors: 1. male homosexual relations 2. intravenous drug use or the injecting drug user. 3. heterosexual relations with an HIV infected
partner 4. sexual relations with infected individuals Mode of transmission 1. Anal intercourse 2. injection of drug direct blood exposure to contaminated needles and syringes. 3. blood and blood products including those persons with hemophilia and other people who are blood recipients. 4. transplacental AIDS transmitted in utero from mother to child. Clinical manifestations: 1. persistent generalized lymphadenopathy characterized by the generalized enlargement of the lymph nodes. 2. lesser AIDS conditions such as oral candidial infection arise and examination of platelet reveals decreased. Most of the patients may be completely asymptomatic. 3. AIDS related complex(ARC:wasting syndrome profound involuntary weight loss of 10%
body weight due to unexplained diarrhea for more than one month or chronic weakness. - intermittent fever
d. Shortness of breath e. Dyspnea f. Occasional chest pain
- splenomegaly - low platelet count and lymphocytes - severe body malaise 2. Mycobacterium Avium Complex(MAC) AIDS SYNDROME Opportunistic infections 1. Pneumocyctis carinii - 60% of the AIDS patients initially manifest PCP. It was thought to be protozoan but recent studies showed that it is a rare fungal infection that cause diseases only to immunocompromised patients: - patients tend to demonstrate the ff: a. Fever b. Chills c. Non-productive cough - a leading bacterial infection in people with AIDS ..Comprising a group of acid fast bacilli, usually causes respiratory infection 3. Tuberculosis - tend to occur in injecting drug users and other groups with with a pre-existing high prevalence of TB infection - TB that occurs late in HIV infection is characterized by absence of a tuberculin test response because of the compromised immune system 4. Oral candidiasis - a fungal infection occurs nearly in all AIDS related conditions. It is characterized by creamy white patches in the oral cavity - Patients may go to respiratory failure within 3 days after onset of symptoms.
-Symptoms: difficult and painful swallowing : retrosternal pain 5. Cryptosporoidal virus - causes diarrhea up to 6L per day resulting to viral infection 6. Cryptococcus neoformans - char by symptoms such as: fever, headache, malaise, stiff neck, nausea and vomiting, seizure 7. Kaposis sarcoma - most common HIV related malignancy involving endothelial layer of the blood and lymphatic vessels - cutaneous lesions appearing anywhere on the body are usually brownish pink to deep purple surrounded by ecchymosis and edema 8. B cell lymphoma(non hodgkins lymphoma - including multiple organ involvement and complications related to opportunistic infection - compromise approximately 11% of all
childhood cancer -a genetic term for a wide spectrum of disorders characterized by the malignant transformation of the lymphoid system. NHL is differentiated from HL by lack of RS (Reed-sternberg cells) and the other cellular changes not characteristics of HL. - the common finding of NHL are alterations in the tumor DNA - arise from single outlaw cell (Monoclonal) and probably develop with accumulation of multiple genetic hits - its most common type of chromosomal alteration is translocation AIDS DEMENTIA COMPLEX - neurologic dysfunction results from the direct effects of HIV or nervous tissue, opportunistic infections, primary neoplasm, CV changes and metabolic encephalopathies. Diagnostic exams: 1. ELISA - test that identifies antibodies directed
aseptically against HIV. It does not establish diagnosis of AIDS, rather indicates that the person has been exposed to infected HIV called seropositive. - or it is a presumptive test
- advice to wear cotton sock to prevent feet from perspiring if lesions are found in the legs
2. Western blot assay with - conformity test of AIDS
- clean peri-anal area every after bowel
non-abrasive soap and water to 3. Immunoflourescent Assay(IFA) - preferred by some physician over the western blot assay since it is more rapid and simple to perform. oral mucosa 1. promote skin integrity - change position every 2 hours - apply medicated lotions, ointments and dressings 2. Promote usual bowel habit -- monitor for pattern of diarrhea and consistency of stools - report abdominal pain and cramping - during periods of acute intestinal inflammation, the patient may be placed on NPO to rest the GIT prevent escoriation - sitz bath to promote comfort - assess frequently for integrity of the Nursing management:
- avoid using adhesive tapes
- encourage increase dietary intake - avoid foods that are irritating to the bowel such as spicy foods, food with extreme temperature and carbonated drinks - administer antispasmodic and anti-diarrheal agents 3. prevent infection - monitor for signs of infection
- monitor respiratory status - encourage intake of 3l per day - administer humidified oxygen 7. relieve pain and discomfort - administer pain relievers - encourage to wear elastic stockings to equalize pressure 8. improve nutritional status
- prevent overcrowded place - monitor daily weight 4. improve activity tolerance - assess factors that may interfere with dietary -assist in activities of daily living 5. maintain thought processes - assess mental status - use simple explanation - provide memory aids - give positive feedbacks for appropriate behavior 6. improve airway clearance intake - control nausea and vomiting with anti-emetic medications - encourage to eat food that are easy to swallow and to avoid rough and spicy foods - encourage to rinse mouth with lidocaine before meals - give food supplements 9. decreased sense of isolation 10. Assist coping with grief
- gaunt looking, apprehensive Mode of Transmission 1. sexual contact 2. blood transfusion 3. contaminated syringes, needles, nipper, razor blades 2. Mental(early stage) - forgetfulness - loss of concentration - loss of libido Signs and Symptoms: 1. Physical - maculo-papular rashes - loss of appetite - weight loss - fever of unknown origin - malaise, persistent diarrhea - TB - esophageal candidiasis - Kaposis sarcoma -pneumocystis carinii pneumonia - apathy - psychomotor - withdrawal 3. Mental(later stage) - confusion - disorientation - seizures - mutism - loss memeory - coma
Prevention: 1. maintain monogous relationship 2. avoid promiscuous sexual contact 3. sterilize needles, syrnges and instruments used in cutting operations 4. proper screening of blood donors 5. rigid examination of blood and other products for transfusion 5. avoid oral, anal contact, swallowing of semen 6. use of condoms and other protective device HIV/AIDS - first occurred in africa and spread in the carribean island. - reported in the USA in 1981 - this sexually transmitted disease spread so rapidly that it is soon occurred in epidemic proportion inseveral countries of the world including the Philippines. It is currently pandemic(occurring throughout the world) - the first case of AIDS in the Philippines was
reported in 1984, as at May 2000, based on Philippines National AIDS council(PNAC) records, there were 1,385 HIV poisitive and 464 AIDS cases. There have been 206 deaths B. GAMMOPATHIES - immunologic disorders pertaining to elevated level of gammaglobulin in the serum. - also known as hypergammaglobulinemia
- Multiple Myeloma is a malignant disease of the most mature form of B lymphocyte which is the plasma cell. - a B cell cancer characterized by the proliferation of malignant plasma cells that aggregate into tumor masses and then become distributed throughout the sleletal systems.
Clinical manifestationof MM 1. Bone pain usually in back and ribs and worsen with rest. The pain is due to a substance secreted by the plasma cells which is the osteoclast activating factor, that stimulates bone breakdown. Thus, lytic lesions and osteoporosis is seen during xrays. 2. Recurrent fractures 3. Hypercalcemia due to escape of calcium ions from the bones 4. Renal failure: large immunoglobulin molecules can damage the renal tubules. 5. Fatigue and weakness due to anemia
2. Xray or Bone scan establishes the degree of bone involvement 3. Bone marrow aspiration detects number of plasma cell in the bone marrow Medical management: - there is no cure for MM, since it is a disease of malignancy, it is treated with chemotherapy and radiation therapy.
Nursing management: 1. administer pain reliever for bone pain 2. maintain hydration to diminish exacerbation of complication 3. prevent from infection C. AUTOIMMUNE DEFICIENCY these disorders involve inappropriate reaction by the immune system in which antibody form against self-antigen. autoimmunity - is a breakdown of tolerance in which the bodys immune system begins to recognize self-antigens as foreign.
Pathophysiology: malignant plasma cells produces MProtein or monoclonal protein release of osteoclast activating factors breakdown of the bone
Diagnostic Exams: 1. Bence Jones Urine Test detects abnormal globulin in the urine
1. Systemic Lupus Erythematous(SLE) a result of disturbed immune regulation that causes exaggerated production of auto-antibodies. - the increase in auto-antibody production is thought to result from abnormal suppressor T-cell function, leading to immune complex deposition and in tissue damage. - seen more often in women especially in the 20 to 40 year old age group - a transient lupus like syndrome that is indistinguishable both clinically and in the laboratory from spontaneously occurring SLE also can develop from prolonged use of drugs, particularly hydralazine(an antihypertensive agent) and procainamide(an antidysrhythmic drug). 11 clinical findings of SLE: 1. facial rash confined to the cheeks(malar rash) 2. discoid rash(raised patches, scaling) 3. photosensitivity(skin rash in sunlight) 4. oral or nasopharyngeal ulcers
5. non-erosive arthritis of at least two peripheral joints 6. serositis(Pleurisy, pericarditis) 7. renal disorders(proteinuria of >0.5 g/day or cellular cast) 8. neurologic disorders(seizures or psychosis) 9. hematologic disorders(hemolytic anemia, leukopenia, thrombocytopenia) 10. immunologic disorders(positive LE cell preparation, anti-DNA, false-positive serologic test for syphilis) 11. presence of antinuclear antibody (ANA) Predisposing Factors SLE: Genetic and hormonal factors onset during the child bearing years. Environmental factors such as sunlight, thermal burns Drugs hydralazine(apresoline), procainamide(pronestyl), INH, chlorphromazine and other anticonvulsant
Clinical manifestations of SLE:
Arthralgia or arthritis 90% of individuals. A common Total Serum Complement the best test to follow the course of presenting features of SLE frequently accompanied by morning disease. stiffness and not deforming in nature. Medical Management: Classic butterfly rash 70% to 80% of individuals. Papulosquamous or annular polycyclic lesion occurs across the NSAID(Non steroidal anti-inflammatory drug) it is useful in bridge of the nose and cheeks. The rashes worsen with treatment of the arthritis associated with SLE sunlight. Pericarditis 30% to 50% of individuals. Most common cardiac Corticosteroid like prednisone ammelurates the mainstay therapy of SLE. Its side effect is to suppress immune system manifestation of SLE thus suppressing body reactions to autoimmune antibodies. Lymphadenopathy and vasculitis 70% to 80% of individuals. Patients manifest papular, erythematous and purpuric lesions Cytotoxic agents arrest autoimmune activity of the SLE on the fingertips, elbows, toes and forearm. These may Plasma-paresis 3-4 liters are exchanged weekly from a progress into necrosis. plasma of a normal donor which is used to remove circulating auto antibody and immune complexes from the blood before Lupus nephritis 40% to 50% of individuals.Occurs as antinuclear antibodies/attaches to the DNA and is deposited in organ and tissue damage occurs. the renal glomerulus. Psychosis and depression Hematologic abnormalities 50% of individuals, with anemia being the most complication Diagnostic exam of SLE: LE cell test test for presence of lupus erythematous Nursing care management: Institute reverse isolation Encourage personal hygiene Maintain clean environment Screen visitor from cold
ANA or anti nuclear antibody test the best definitive test for Avoid drugs such as contraceptives and anticonvulsant SLE since ANA is present in all cases of SLE even in the inactive Avoid unnecessary blood transfusion stage of the disease
Avoid fatigue Discourage pregnancy 2. Rheumatoid arthritis a systemic autoimmune disease that causes chronic inflammation of connective tissue, primarily in the joints. - the joints most commonly affected are: fingers, feet, wrist, elbows, ankles, and knees, but the shoulder, hips, and cervical spine also may be involved, as well as the tissue of the lungs, heart, kidney and skin. - develops most often in women - despite intensive research, the cause of RA remains obscure. It is probably a combination of genetic, environmental, environmental, hormonal and reproductive factors. Clinical manifestation: Joint pain, swelling and warmth Erythema redness or inflammation of the skin Lost of function or joint stiffness especially in the morning lasting for 30 minutes Hand and feet deformities caused by misalignment resulting from swelling, progressive joint destruction or the subluxation
that occurs with a bone slips over another Fever Weight loss Fatigue Edema Lymph node enlargement Raynauds phenomenon intermittent attacks of ischemia of trhe extremities of the body, especialy the fingers, toes, ears, and nose, caused by exposure to cold or by emotional stimuli. - the attacks are characterized by severe blanching of the extremities, followed by cyanosis then redness; usually accompanied by numbness, tingling, burning and often pain. Diagnostic exam of RA: ESR reveals elevated C Reactive Protein positive in RA ANA positive Arthrocentesis synovial fluid shows cloudy, milky or dark yellow and contains numerous inflammatory cells, such as leukocytes and complement. XRAY studies helps monitor progress of the disease
Management of RA: NSAIDS : blocks the enzyme involved in inflammation while leaving the enzyme involved in protecting the stomach lining. (COX-2 inhibitor) Antimalarials, Gold, penicillamine initiated early in treatment; alters cellular metabolism; alter enzyme function and immune response and suppress phagocytic activity Biologic response modifiers such as cytokines Corticoesteroids used when patient has unremitting inflammation and pain or needs a bridging medication while waiting for the slower disease modifying anti-rheumatic agent. Synovectomy excision of synovial membrane Tenorrhapy suturing of tendons Arthrodesis surgical fusion of the joint Arthroplasty surgical repair and replacement of the joint. 3. Hashimotos thyroiditis chronic lymphocytic thyroiditis diagnosed based on the inflammation of the gland. It is not accompanied by pain, pressure symptoms or fever and thyroid activity is normal - cell mediated immunity plays a significant role in the pathogenesis.
- treatment goal: reduction of the size of the gland D. HYPERSENSITIVITY an abnormal, heightened reaction to any type of stimuli.
1. ANAPHYLACTIC TYPE(TYPE I) - is an immediate reaction beginning within minutes of exposure to an antigen and this is mediated by IgE antibodies. anaphylaxis is a clinical immediate immunologic response between a specific antigen and antibody Etilogy: 1. food 2. drugs 3. venom 4. blood products 5. allergen extract 6. diagnostic agents Clinical manifestation of type I
Urticaria Bronchospasm Generalized swelling Hypotension Nausea and vomiting
Clinical manifestations: 1. nasal congestion: clear, watery, nasal discharge 2. intermittent sneezing 3. nasal itching 4. itching of throat and palate
Management: Administer oxygen as indicated Epinephrine as needed Corticosteroids may be given to relieve bronchospasm IV fluids are administered to correct hypotension Atopic allergies 1. Allergic rhinitis/Hay fever inflammation of the nasal mucosa. It is usually induced by airborne pollen or molds. Sensitization begins by ingestion or inhalation of an antigen. On reexposure the nasal mucosa reacts by the slowing of ciliary action, edema formation, and leukocyte infiltration. Histamine is the major mediator of allergic reaction
5. headache 6. pain over paranasal sinuses Management: Administer antihistamine as ordererd May administer adrenergic agents to cause vasoconstriction of the mucosal vessel Mast cell stabilizer like intranasal cromolyn sodium is a nasal spray that inhibits the release of histamine and other mediators of allergic response Advice the client to avoid allergens like dust, hapte-rich foods, etc. 2. Atopic dermatitis most patients have elevated IgE in the serum. Pruritus and
hyperirritability of the skin are the most consistent features and are related to large amount of histamine in the skin. Excessive dryness of the skin results from change in the lipid content, sebaceous gland activity, and sweating.
hypotension, nausea and vomiting, restlessness and shock
3. Urticaria also known as Hives is a type I hypersensitive reaction of the edematous elevations that vary in size and shape, itch and cause local discomfort. It stays from few minutes to hours before disappearing. 2. CYTOTOXIC (TYPE 2) occurs when the system mistakenly identifies a normal constituent of the body as foreign and mediated by whether IgG or IgM.
Nursing Care: - place patient in supine with head elevated at 20-30 degrees - administer fluid, epinephrine and corticosteroids as ordered. - administer mannitol
A. Blood transfusion reaction TYPES: 1. Hemolytic Clinical manifestations - chills, fever, headaches, chest pain, tachycardia, dyspnea, infusing
- insert an indwelling catheter - monitor intake and output - TSB for fever - stop blood transfusion - change IV fluid to prevent from
anymore
- administer IV saline as ordered - obtain blood and urine sample
3. Febrile reaction clinical manifestation: - mild chills
Example: Blood type A individual transfused with a Type B blood mistakenly antigen and antibody reaction agglutination & hemolysis of the RBC hemolyzed blood clogges capillaries unable to carry oxygen and food obstruction of blood flow antihistamine
- fever nursing care: - administer antipyretic and
4. Allergic reaction clinical manifestation:
2. Contaminated blood clinical manifestation: - chills, fever, abdominal pain, nausea and vomiting, diarrhes, hypotension nursing care: - stop BT immediately - administer fluids
- pruritus, urticaria(hives), facial swelling, chills, fever nausea & vomiting, headache, wheezing, laryngeal edema, shock, respiratory distress nursing care: - administer antihistamine, epinephrine or corticosteroids
B. RH incompatibility there is excessive
destruction of RBC which results from antigenantibody reaction and is characterized by hemolytic anemia and hyperbilirubinemia. clinical manifestation of EF Father(Rh+) + Mother (Rh-) incompatible Rh 1. sclera appears yellow before the skin does 2. skin color from light brown to yellow 3. lethargy 4. dark amber concentrated urine 5. poor feeding -subsequent pregnancies, the Rh(+) antibodies will destroy and cause the blood of the fetus to hemolize 6. dark stools Diagnostic evaluation: 1. amniocentesis analysis of bilirubin level in amniotic fluid before birth through the amniotic fluid of the mother. 2. Indirect Coombs test is the direct evaluation of the presence of anti-Rh antibody in maternal circulation. 3. Direct Coombs test this confirms the disease postnatally by detecting antibody attached to circulating lymphocytes of affected infants RHOGAM INJECTION after the first delivery, mother should be given Rhogam within 48 hours to
-During the delivery of the first baby blood of the fetus escape to the body of the mother thru maternal sinuses, causingn Rh antibody towards Rh(+)
- compesatory mechanism: increased production of immature RBC by the fetus
ERYTHROBLASTOSIS FETALIS
prevent the maternal circulation from developing antibody against the opposite Rh factor.
- occurs 24-72 hours after exposure and is mediated by sensitized T cells and macrophages. a. Contact dermatitis a delayed eczematous condition caused by a skin reaction to a variety of irritating or allergenic materials ex. Poison Ivy most common type but soaps, detergents, cosmetics may also cause this type of dermatitis. clinical manifestations: -itching, burning, erythema, skin lesions(vesicles), edema, weeping, crusting and finally drying and peeling of the skin b. Skin graft/Organ rejection - skin graft is a technique in which a section of the skin is detached from its own blood supply and transferred to a free tissue to a distant(recipient) site. These are commonly used to repair defects and cover wound when insufficient skin is available to permit wound closure. TYPES OF GRAFTS 1. isograft/syngeneic - graft exchange between genetically dentical membrane of the same species
3. IMMUNE COMPLEX(TYPE III) - are deposited in tissues or vascular endothelium that contributes to injury, the increase amount of circulating complexes and the presence of vasoactive amines. - the joints and kidneys are the primary susceptible to these type of allergy.
Serum Sickness - this type III hypersensitive reaction is known to be a result of the administration of therapeutic antisera of animal sources for the treatment and prevention of infectious diseases, such as tetanus, pneumoniua and rabies. manifestations: inflammatory reaction at the site of injection of the medication followed by regional and generalized lymphadenopathy. There is usually skin rash and joints are frequently tender and swollen. 4. DELAYED TYPE(TYPE IV)
2. allograft/allogeneic/homograft - graft exchange between individual of the same species 3. autograft/autologous - graft exchange within the same individual 4. xenogeneic - graft exchanged between individuals of different species Rejection of Graft - described as immune complex response leading to rejection by recipient therapy usually due to incompatibility of cell surface antigen - this can be prevented by tissue typing and matching between donor and recipient
Methotrexate a folic antagonist; inhibit folace metabolism and is a potent suppressor of both humoral and cellular immunity 4. antilymphocyte serum serum from animals injected to human results to antibody formation against the lymphocytes. 5. cyclosporina decreases the number of killer T cells without affecting granulocytes - used to suppress rejection If you just found out youre pregnant, one of the first and most important tests you should expect is a blood type test. This basic test determines your blood type and Rh factor. Your Rh factor may play a role in your babys health, so it is important to know this information early in your pregnancy People with different blood types have proteins specific to that blood type on the surfaces of their red blood cells. There are four blood types (A, B, AB and O) Each of the four blood types is additionally classified according to the presence of another protein on the surface of RBC that indicates your RH Factor. If you carry this protein, you are Rh Positive. If you dont
Immunosuppresive therapy are also useful in preventing graft rejection Corticosteroid impairs lymphocyte function, thus suppressing immune response Azathioprine(Imuran) prevent cell-mediated immune response while inactivating Ag receptor sites in T cells
carry the protein, you are Rh negative. Most people about 85% are Rh positive. But if a woman who is Rh negative and a man who is Rh positive conceive a baby, there is the potential for incompatibility The baby growing inside the Rh negative mother may have Rh positive blood, inherited from the father Statistically, at least 50% of the children burn to an Rh negative mother and Rh positive father will be Rh Positive Rh incompatibility isnt a problem if its the mothers first pregnancy because, unless theres some sort of abnormality, the fetuss blood does not normally enter the mothers circulatory system during the course of the pregnancy However, during delivery, the mothers and babys blood usually intermingles. When this happens, the mothers body will begin to produce antibodies(protein molecules in the immune system that recognize, and later work to destroy, any substance foreign to body) against the Rh proteins that have been introduced into her blood. Rh antibodies are harmless until the mothers second or later pregnancies
If she is ever carrying another Rh positive child, her Rh antibodies will now recognize the Rh proteins on the surface of the babys blood cells as foreign Rh antibodies will cross the placenta into the babys bloodstream and attack those cells, causing swelling and rupture of the babys RBC A babys blood count can get dangerously low when this condition, known as hemolytic or Rh disease of the newborn, occur. How is Rh disease of the newborn prevented and treated? - Today, when a woman with the potential to develop Rh incompatibility is pregnant, doctors administer a series of: 2 Rh immune-globulin shots during her first pregnancy - first shot given around 28th wk of pregnancy - 2nd shot given 72 hours after giving birth Rh immune globulin acts like a vaccine, protecting against the development of the Rh antibodies that can cause complications during any future pregnancies.
INFLAMMATION and IMMUNITY
Cell Injury and Inflammation Cell adaptation to injury includes: Adaptive processes H ype rt roph y increase in cell size without cell division H y p e rpl as i a actual increase cell number or density of cells A t ro p h y decrease in tissue or organ size caused by decrease in cell number or cell size Meta plasi a the transformation of one cell type into another Maladaptive responses D y s p l a s i a abnormal differentiation of dividing cells resulting in changes in the size, shape, and appearance of the cells; a precursor to malignancy A n a p l a s i a cell differentiation to a more immature or embryonic form. Malignant tumors are characterized by anaplastic cell growth. Defenses against injury Skin and mucous membrane first line of defense Mononuclear Phagocyte System (MPS) consists of monocytes and macrophages and their
precursor cells known as reticuloendothelial system (RES) Consists of: 1. Fixed phagocytes or macrophages of the liver, spleen, BM, lungs, LN and microglial cells 2. Mobile or wandering phagocytes monocytes (blood) and macrophages found in connective tissues known as histiocytes
Functions of Mononuclear Phagocyte System (MPS) Recognition and phagocytosis of foreign material such as microorganism Removal of old or damaged cells from circulation Participation in the immune response Inflammatory Response Is a sequential reaction to cell injury. It is often but incorrectly used as synonym for the term infection. I n a m m a t i o n is always p r e s e n t wit h infection, but infection is not always present with inflammation. Four Distinct Phenomena in the Inflammatory Response Increased vascular permeability (Vascular response)
Infiltration of leukocytic cells (Cellular response) Formation of exudates Healing process Increased vascular permeability (Vascular Response) After cell injury, the capillaries in the area briefly undergo vasoconstriction After the release of histamine and other chemicals by the injured cells, the vessels dilate (vasodilation) resulting in hyperemia which raises filtration pressure. Capillary Permeability Infiltration of Leukocytic cells (Cellular Response) Neutrophils and monocytes move to the inner surface of the capillaries (margination) and then in amoeboid fashion, through the capillary wall (diapedesis) and to the site of injury. The findings of number of band (immature) neutrophil on circulation is called a shift to the left, which is commonly found in patients with acute bacterial infections (mature neutrophils are called segmented neutrophils, or segs) Chemotaxis and Emigration Mediators of Inflammation response Inflammatory Phases Formation of Exudates
Formed from the fluid and the cells that move to the site of injury. Types of inammatory Exudates: Serous e x u d a t e clear in appearance and can easily reabsorbed with no damage Serosanguinous serous exudate mixed with small amounts of blood from the injured capillaries San gui nou s contains large amount of blood from extensive damage P u r u l e n t results from bacterial invasion and may lead to tissue scarring if cellular necrosis is extensive C a t a r r h a l o r m u c o i d contains mucous secretions and usually results from viral infection of the respiratory tract. Healing Process Refers to the replacement of dead or damaged cells by new and healthy cells derived either from the parenchymal or connective tissue stroma. Includes two (2) major components: Regeneration Scar formation Regeneration This occurs when the injured tissues and cells are
replaced by new cells and tissues that are identical in nature and function to the damaged cells. Scar formation There is a formation of collagenous scar in the healing of tendons, fascia, connective tissues and collagenous structure. This type of repair consists of: Primary healing/union or First Intension repair of clean surgical wound or incision by CT elements Secondary union/ secondary intension repair of a contaminated surgical wound by formation of granulation tissue Tertiary Intension there is delayed primary closure of a wound (DPC) Clinical manifestation of Local Inflammatory Response Local Manifestations of Inflammation
INTRINSIC- begins with the activation of Factor XII (Hageman factor) by contact with abnormal surfaces produced by injury EXTRINSIC- is triggered by trauma, which activates Factor VII (Stable factor) and releases a lipoprotein, called Tissue factor from BV COMMON- conversion of Prothrombin to Thrombin; Fibrinogen to Fibrin FIBRINOLYTIC- conversion of Plasminogen to Plasmin by t-PA (tissue plasmin activator) Fibrin degradation products
Case management Drug therapy Vitamins (Vit A,B,C,D) Antibiotic-Resistant Organisms Reduce risk for Antibiotic-Resistant Infection
Systemic Inammatory Response occurs when bacterial invaders cannot be locally successfully localized and destroyed. Clinical manifestations include fever, leukocytosis, anorexia and nausea, malaise and increased ESR. Systemic inflammatory response COAGULATION PATHWAYS
Alternative meds- Herbal Nutrition therapy Nursing management Drug Therapy for inflammation and Healing Antipyretic drugs: SAN
S alicylates (Aspirin) Acetaminophen (Tylenol) Non steroidal anti-inflammatory drugs (NSAIDs) Ibuprofen (Motrin, Advil) Anti-inammatory drugs: CNS Corticosteroids NSAIDs S alicylates Vitamins (A,B,C,D) Accelerates epithelialization B complex acts as co-enzymes Collagen synthesis D- facilitates Calcium absorption
increase risk for developing resistant infection) Wash your hands frequently Follow directions. (not taking antibiotic as prescribed or skipping can encourage the development of antibiotic resistant bacteria) Finish your antibiotic. (when you stop taking your antibiotic early, the hardest bacteria may survive and multiply. Do not request for an antibiotic for flu or colds. (antibiotics are effective against bacterial infections, but not virus, which cause cold and flu)
Do not take leftover antibiotics. This is dangerous because: T h e l e f t o v e r antibiotic m a y n o t b e appropriate;
Antibiotic-Resistant Organisms: MVP Illness m a y n o t b e a bac teri al infectio n Methicillin Resistant Staphylococcus aureus (MRSA) Vancomycin-Resistant Enterococci (VRE) Penicillin-Resistant Streptococcus (PRSP) Reduce Risk for Antibiotic-Resistant Infection Do not take antibiotics to prevent illness. (might O l d antibiotics m a y h a v e l o s t t h e i r effectiveness and in some case can even be fatal Herbs Used for Healing Clinical uses: used topically for treating minor wounds, including sunburns, cuts and abrasions. (Ex. Aloe, chamomile, Echinacea, evening primerose,
golden seal, St. Johns Worth) Effects: anti-inflammatory actions Nursing implications: herbs should not be used in deep wounds, if used, they should be used after the wound has begun to heal. A l o e c a n b e u s e d safely o n r e c e n t sunburns, minor burns, and superficial cuts and abrasions. Nutrition Therapy High uid intake is needed to replace fluid loss from perspiration and exudate formation. Diet high in CHON, CHO, and Vitamins with moderate Fat intake is necessary to promote health. Protein Needed to correct the negative Nitrogen balance resulting from increased metabolic rate. Necessary for synthesis of immune factors, leukocytes, fibroblast, and collagen. Carbohydrates Needed for the increased metabolic energy required in inflammation and healing. If CHO deficit is present, the body will break down protein, (in replacement of CHO) for the needed energy
Fats Necessary components in the diet to help in the synthesis of fatty acids and triglycerides, which are part of the cellular membrane. Vitamins Vitamin C needed for capillary synthesis, capillary formation, and resistance to infection. Vitamin B-complex necessary as coenzymes for many metabolic reactions. V i t a m i n B deciency m a y r e s u l t s i n disruption of protein and fat, and carbohydrate metabolism will occur. Nursing Management for Inflammation, Infection & Healing Rest and Immobilization promote healing by decreasing the inflammatory process, assisting in the repair process, and decreasing metabolic needs. Elevation will reduce the edema at the inflammatory site and increase venous return Adequate oxygenation of the inflamed area is essential because oxygen promotes the differentiation of fibroblasts and collagen synthesis. O2 is also essential for cell growth and division. Heat and Cold Cold application is usually appropriate at the time of the initial trauma to cause vasoconstriction and decrease swelling, pain and congestion from increased metabolism in the area of
inflammation. Heat may be used later (24-48 hrs) and when swelling has subsided to promote healing by increasing the circulation to the inflamed site and subsequent removal of debris. It is also used to localize the inflammatory agents. Warm, moist heat may help debride the wound site if necrotic material is present. Wound Healing Primary Intention Incision Wound formation Fibrin clot prevents bleeding, acts as glue to hold skin together Inflammatory response builds Blood clot dissolved Granulation tissue forms where clot was Epithelium regenerates
Involves more granulation tissue and regeneration May form underneath a scab May show pinpoint bleeding
Factors Affecting Wound Healing Necrotic or foreign tissue in wound Wound infection Excessive movement Dehiscence breaking open of a surgical wound
Wound Management For wounds that heal by primary intention, it is common to convert the incision with dry, sterile dressings. Medicated sprays that form a transparent film on the skin may be used for dressings on a clean incision on injury. Sometimes a surgeon will leave a surgical wound uncovered. Wound healing management by secondary intention depends on the wound etiology and type of tissue in
Wound Healing Secondary Intention Skin edges cannot be held together Similar to primary intention Takes longer
the wound. (red-yellow-black concept of wound care)
Components of Immune System Specialized blood cells (lymphocytes and macrophages) Specialized structures ( lymph nodes, spleen, thymus, bone marrow, tonsils, adenoids and appendix) Immunity Refers to the bodys capacity to resist invading organisms and toxins, thus preventing tissue and organ damage. It is a state of responsiveness to foreign substances such as microorganisms and tumor proteins. Bone Marrow Components Differentiation and Maturation Three basic defense strategies of Immune system Physical and chemical barrier to infection Inflammatory response Immune response Acquisition of Immunity Natural/Innate Immunity aka primary immune response: refers to the individual who is born with the ability to resist certain types of agents without apparent contact with an antigen (Example: high natural resistance to cold) Acquired immunity aka secondary immune
IMMUNE SYSTEM It is a complex and intricate network of specialized cells, tissues, and organs. It is closely related to the circulatory system, the blood and tissue fluid do not only carry nutrients to the body cells but also carry substances that defend the body against disease. Cells of the immune system seek out and destroy damaged cells and foreign tissue, yet recognize and preserve host cells. (Porth, 2002) Functions of the Immune System Defense - Defending and protecting the body from infection by bacteria, viruses, fungi and parasites by attacking foreign antigens and pathogens. Homeostasis - Removing and destroying damaged or dead cells. Through this mechanism the bodys different cell types remain uniform and unchanged. Surveillance- Identifying and destroying malignant cells, thereby preventing their further development into tumor. (mutations continually arise in the body but are normally recognized as foreign cells and are eventually destroyed.)
response: refers to the resistance of an individual to specific infectious organisms, which develop either actively or passively during the course of an individuals life. Types of Immunity Nonspecific defenses Specific defenses Types of Acquired Specific Immunity ACTIVE Types of Immunity Nonspecic defenses operate in the same way against all disease-causing microorganisms. (SKIN & MUCOUS MEMBRANES) Provides mechanical barrier against the pathogens. Phagocytosis engulfing and digestion of pathogens Interferon - inactivates virus by preventing them from reproducing
1. B-cells 2. T-cells B cells or B lymphocytes Stem cells of bone marrow ------------- B cells Produce antibody and oversee Humoral Immunity An invading antigen causes B cells to divide and differentiate into plasma cells Each plasma cells produces and secretes large amounts of antigen-specific immunoglobulins (Ig) into the bloodstream Immunoglobulins Plasma Cells and Memory B cells and the Humoral Immunity B cells carry the pattern of the non-self antigen to a lymph node B cells then transforms into a plasma cell ---manufacture proteins that exactly fit the non-self surface marker of the antigen. These are antibodies. Each antibody combats just one specific antigen. This antibody is the circulating antibody which moves through the body fluids. When the antigen is located, the antibody hooks on
Specic defenses defend body against specific pathogens. WBC- Lymphocytes Two types of Lymphocytes:
and signals phagocytes to surround and destroy the Helper T cells-( CD4) serve as managers, directing the immune antigen. response. They secrete the chemical called lymphokines that stimulate T cells and B cells to grow, divide and attract A molecule that causes an immune response is an neutrophils and enhance the ability of macrophages to engulf antigen. and destroy microbes. T cell or T lymphocytes Cells that migrate from the bone marrow to the thymus differentiate into T lymphocytes (Thymusdependent cells). T cells live from a few months to the life span of an individual and account for longterm immunity. All mature T cells have the CD3 antigen. T cells and the Cell-Mediated Immunity T cells do not produce circulating antibodies. They carry cellular antibodies on their surface. Once the T cells recognize a non-self marker, the cellular antibodies latch onto an antigen. The T cells then direct the phagocytes to surround and destroy the foreign substances. The T cells can recognize body cells that have been invaded by cancer and certain viruses, thus allowing T cells to launch a defense. Kinds of T cells Fights the non-self markers in the body Cytotoxic T cells- fight diseases by releasing lymphotoxins/ cytolytic substances, which in turn causes lysis of the cell Suppresor T cells- (CD8) inhibit the production of cytotoxic T cells once they are unneeded. Both CD4 and CD8 are involved in the regulation of cell-mediated immunity and the humoral antibody response. T h e h u m a n i m m u n o d e ciency vir us (HIV) invades T helper cells (CD4), thus decreasing their number and function. Therefore individuals with HIV infection do not mount an aggressive response and are at an increased risk for opportunistic infections and malignancies. 4. Natural killer cells are also involved in cellmediated immunity. These cells are not T or B cells, but are large lymphocytes with numerous granules in the cytoplasm. NK cells have a significant role in immune surveillance for malignant cell changes. Altered Immune Response Hypersensitivity Reactions: ACIDS Anaphylactic
Cytotoxic Immune-complex Delayed hypersensitivity S timulatory Types of Hypersensitivity Reactions Type 5: Stimulatory Reactions inappropriate stimulation of normal cells surface Immunodeficiency Abnormality that renders a person susceptible to diseases normally prevented by an intact immune system. Four categories of immune mechanisms: 1. humoral or antibody-mediated immunity; 2. cell-mediated immunity; 3. complement system; 4. phagocytosis Primary Immunodeficiency Disorders Primary immunodeficiency congenital or inherited abnormalities of immune function that render a person susceptible to diseases normally prevented by an intact immune system
Disorders of T-cell function impair the ability to orchestrate the immune response (CD4+ helper T cells) and to protect against fungal, protozoan, viral and intracellular bacterial infections (CD8+ cytotoxic T cells)
Combined T-cell and B-cell immunodeficiency represents a life-threatening absence of immune function that requires bone marrow transplantation for survival States of Immunodeficiency Humoral (B-cell) immunodeficiency
Primary: Transient hypoglammaglobulimia of infancy;
Secondary: Increased loss of immunoglobulins (nephrotic syndrome)
States of Immunodeficiency Cellular (T-cell) Immunodeficiency Primary: DiGeorge syndrome; Nezelof Secondary: Hodgkins disease; AIDS syndrome
Disorders of B-cell function impairs the ability to produce antibodies and defend against microorganisms and toxins that circulate in the body fluids Primary Immunodeficiency Disorders
Combined B-cell and T-cell immunodeficiency Primary: Wiskott-Aldrich syndrome; ataxiatelangiectasia
Secondary: irradiation; Aging
Antipruritic drugs Mast cell-stabilizing drugs
States of Immunodeficiency Complement Disorders Primary: Angioneurotic edema
Antihistamines Best drug treatment for allergic rhinitis and urticaria Sympathomimetic/decongestant drug The major sympathomimetic drug is Epinephrine (Adrenalin), which is the DOC to treat an anaphylactic reaction. Several specific, minor sympathomimetic drugs differ from epinephrine because they can be taken orally or nasally and last for several hours. Used primarily to treat allergic rhinitis. - Phenylephrine (Neo-synephrine) - Pseudoepheride (Sudafed) Corticosteroids Oral
Secondary: Acquired disorders that involve complement utilization
Phagocytic Dysfunction Primary: Chronic granulomatous disease; G6PD Secondary: Drug induced; Diabetes Mellitus
Case Management Drug Therapy: A SCAM Immunotherapy Drug Therapy: A SCAM Antihistamine S ympathomimetic/Decongestant drug Corticosteroids
Nasal nasal corticosteroid spray effective in relieving symptoms of allergic rhinitis Therapeutic Uses Rheumatoid Arthritis SLE Inflammatory Bowel Disease (IBD)
Miscellaneous Inflammatory D/Os Allergic conditions (not acute anaphylaxis) Asthma Dermatologic disorders Neoplams Transplant rejection Preterm infant
Glucocorticoids used for non-Endocrine purposes Pharmacologic Actions Anti-inflammatory and Immune effects Inhibit prostaglandin, leukotriene, and histamine synthesis Suppress infiltration of phagocytes Suppress proliferation of lymphocytes Effects on Metabolism and Electrolytes Glucose levels rise
Immunosuppressive effect Cause lysis of activated B and T cells Sequester T cells Reduce IL-2 production Reduce responsiveness to IL-1 Immunosuppressive doses are large, e.g. Methylprednisolone Anti-immune doses: Anti-inflammatory doses: 500 1500mg (IV) 5 60mg (IV)
Protein synthesis suppressed Fat deposits mobilized Fewer electrolyte effects, but can inhibit calcium absorption
Glucorticoids Adverse Effects Adrenal insufficiency Osteoporosis: long term therapy Infection Glucose intolerance Myopathy
F&E disturbance Growth retardation Psychological disturbances
used with great caution due to associated risk of agranulocytosis Mast cell-stabilizing drugs Inhibit the release of histamines, leukotrienes and other agents from the mast cell after antigen-IgE interaction Used in the management of asthma and treatment of allergic rhinitis Very low incidence of side effects Available as inhalant nebulizer solution, nasal spray, or an oral pill - Cromolyn sodium (Intal, Nasalcrom, Rynacrom
Glucocorticoids Adverse Effects Cataracts and Glaucoma Peptic Ulcer Disease Iatrogenic Cushings Disease Ischemic Necrosis especially caution with ETOH
Antipruritic drugs These drugs protect the skin and provide relief from itching. Over the Counter: Calamine lotion, coal tar solution and camphor Menthol and phenol maybe added to other lotions to produce antipruritic effect More potent drugs that requires Rx: Methdilazine (Tacaryl) Trimeprazine (Temaril)
- Nedocromil (Tilade) Calcineurin Inhibitors Calcineurin is needed to produce IL-2 Without IL-2, T-cells cannot proliferate, so cannot mount an immune response Used for transplant graft rejection Drugs Cyclosporine: nephrotoxicity, infection Kidney, liver, heart transplant Psoriasis, rheumatoid arthritis
Tacrolimus (FK506): same
Tourniquets IV tubing
Cytotoxic Drugs Kill proliferating B and T cells Are non-specific: kill all rapidly dividing cells (red blood cells, skin, epithelial cells) Azathioprine: Adjunct transplant Cyclophosphamide: cancer, SLE, MS Methotrexate: cancer, psoriasis, arthritis Mycophenolate Mofetil: selective, transplant
Syringes Electrode pads O2 masks Tracheal tubes Colostomy and ileostomy pouches Urinary catheters Anaesthetic masks Adhesive tape
Immunotheraphy Involves administration of small titers of an allergen extract in increasing strength until hyposensitivity to the specific allergen is achieved. For best results, the patient should continue to avoid the offending allergen whenever possible because complete desensitization is impossible. Gloves* Latex Allergies
*Latex protein can be aerosolized through powder on gloves and can result in serious reactions when inhaled by sensitized individuals. Two types of Latex Allergies Type 4 allergic contact dermatitis Type 1 allergic reaction Type 4 allergic contact dermatitis Caused by chemicals used in manufacture of latex gloves
Blood pressure cuffs Stethoscopes
Occurs within 6-48 hours Chronic exposure can lead to lichenification, scaling and hyperpigmentation. The dermatitis extend beyond the area of physical contact with the allergen S/Sx: dryness, pruritus, fissuring, cracking of the skin followed by redness, swelling and crusting at 24-48 hours. Type 1 allergic reaction Response to a natural rubber later proteins and occurs within minutes of contact with the proteins. Systemic reactions to latex may result from exposure to latex protein via various routes, including skin, mucous membranes, inhalation or blood. S/Sx: various reactions from skin redness, urticaria, rhinitis, conjunctivitis, or asthma to full-blown anaphylactic shock Recommendations for preventing allergic reactions to latex in the workplace: Ask patient regarding known allergy to latex Use nonlatex gloves for activities that are not likely to involve contact with infectious materials (food preparation, house keeping) Use powder-free gloves with reduced protein content
Do not use oil-based had creams or lotions when wearing gloves After removing gloves, wash hands with mild soap and dry thoroughly Frequently clean work areas that are contaminated with latex containing dust. Know the symptoms of latex allergy, including skin rash, hives, flushing, itching; nasal, eye or sinus symptoms; asthma and shock If symptoms of latex gloves develop, avoid direct contact with latex gloves and products. Wear a medical alert bracelet and carry an epinephrine pen (EpiPen) Inflammation versus Immunity Inflammation is nonspecific, nonadaptive Immunity is specific (to select antigens), adaptive Inflammation allows immunity to happen Immunity controls inflammation
Nursing Diagnoses Risk for infection
Expected outcomes Patient remains free from signs and symptoms of infection Patient maintains adequate respiratory function Patient states ways to prevent infection, including proper handwashing and good personal hygiene. Ineffective coping may be related to perceived or impending personal loss, may be associated with lifethreatening immunodeficiency disorders. Expected outcomes Patient identifies mechanisms for coping effectively Patient demonstrates an active role in self-care activities Patient identifies appropriate resources to maximize his status.
You might also like
- Bio 12 Answer Key CH 8-14Document33 pagesBio 12 Answer Key CH 8-14api-2620290510% (1)
- Analysis of The Short Story of Nick JoaquinDocument2 pagesAnalysis of The Short Story of Nick JoaquinEric EvangelistaNo ratings yet
- Permanent MakeupDocument140 pagesPermanent MakeupNatural Brows AcademyNo ratings yet
- A.D. Pearle - Surgical Technique and Anatomic Study of Latissimus Dorsi and Teres Major Transfers (2006)Document9 pagesA.D. Pearle - Surgical Technique and Anatomic Study of Latissimus Dorsi and Teres Major Transfers (2006)João Pedro ZenattoNo ratings yet
- Cells AliveDocument13 pagesCells Aliveapi-3025396180% (1)
- Renal Physiology MCQDocument12 pagesRenal Physiology MCQTran Dong67% (9)
- Alteration in Inflammatory and Immunologic Response 2012Document22 pagesAlteration in Inflammatory and Immunologic Response 2012Pamela BagabaldoNo ratings yet
- Autoimmune DisordersDocument13 pagesAutoimmune Disordersinah krizia lagueNo ratings yet
- Drug Study CovidDocument5 pagesDrug Study CovidR Hornilla Arcega0% (1)
- MumpsDocument7 pagesMumpsKristine DolatreNo ratings yet
- Tetanus PathophysiologyDocument7 pagesTetanus PathophysiologyWahyu Adhitya PrawirasatraNo ratings yet
- HypersensitivityDocument37 pagesHypersensitivitykiguzonNo ratings yet
- EENT Disorders StudentsDocument26 pagesEENT Disorders StudentsPye Antwan DelvaNo ratings yet
- GDMDocument7 pagesGDMMaica EspañolaNo ratings yet
- Fdar PsycheDocument1 pageFdar PsycheAziil LiizaNo ratings yet
- ChickenpoxDocument4 pagesChickenpoxJen Vizcarra CaminoNo ratings yet
- Anti Emetics 141109072529 Conversion Gate02Document23 pagesAnti Emetics 141109072529 Conversion Gate02sanoozarmNo ratings yet
- Theories of AgingDocument5 pagesTheories of Agingnichtemp1813No ratings yet
- Pediatric Nursing or Child Health NusrsingDocument20 pagesPediatric Nursing or Child Health NusrsingGenynne RagasaNo ratings yet
- ChemotherapyDocument54 pagesChemotherapyPinanto IrwandyNo ratings yet
- DengueDocument6 pagesDengueteabagmanNo ratings yet
- RabiesDocument25 pagesRabiesAdindapauliaNo ratings yet
- Pneumonia and TuberculosisDocument18 pagesPneumonia and TuberculosisVincent QuitorianoNo ratings yet
- Oncologic Nursing Cellular Abberation: Ma - Fe M. Gadayan, RN, MNDocument68 pagesOncologic Nursing Cellular Abberation: Ma - Fe M. Gadayan, RN, MNIsrael AgrisNo ratings yet
- Chronic Myeloid LeukemiaDocument7 pagesChronic Myeloid LeukemiahemendreNo ratings yet
- Assisting: Venous Cut DownDocument4 pagesAssisting: Venous Cut DownJimnah Rhodrick BontilaoNo ratings yet
- Cardiotonic Medications: Drugs Used To For Patients Experiencing Heart FailureDocument28 pagesCardiotonic Medications: Drugs Used To For Patients Experiencing Heart FailureMoxie MacadoNo ratings yet
- July 2012 Pnle Pearls of Success Part 6: Medical and Surgical Health NursingDocument7 pagesJuly 2012 Pnle Pearls of Success Part 6: Medical and Surgical Health NursingNicole OrtegaNo ratings yet
- DrugDocument3 pagesDrugPeace Andong PerochoNo ratings yet
- CD HandoutsDocument80 pagesCD HandoutsMayflor GuiyabNo ratings yet
- Upper Respiratory Tract InfectionDocument9 pagesUpper Respiratory Tract InfectionCHRISTIE MONTANO100% (1)
- Acute Lymphoblastic LeukemiaDocument34 pagesAcute Lymphoblastic LeukemiamtyboyNo ratings yet
- Gastro OooooDocument11 pagesGastro OooooCHLOIE MARIE ROSALEJOSNo ratings yet
- Central Nervous System Infections: Gonzalo B. Roman JR.,MD.,FPSPDocument72 pagesCentral Nervous System Infections: Gonzalo B. Roman JR.,MD.,FPSPBenjamin PrabhuNo ratings yet
- RabiesDocument12 pagesRabieszenNo ratings yet
- Allergy and HypersensitivityDocument73 pagesAllergy and HypersensitivityAdi PomeranzNo ratings yet
- PTBDocument46 pagesPTBJai AdoraNo ratings yet
- Communicable DiseasesDocument24 pagesCommunicable DiseasesJanus de LeonNo ratings yet
- PRELIM CHN LECTURE HandoutsDocument22 pagesPRELIM CHN LECTURE HandoutsJOYCE ANN PEREGRINONo ratings yet
- BRH Drug StudyDocument6 pagesBRH Drug StudyStephanie Dellera AgdanNo ratings yet
- Transcultural Nursing Quiz 2Document2 pagesTranscultural Nursing Quiz 2Jenny AjocNo ratings yet
- Approach To CoughDocument5 pagesApproach To CoughZulaikha HattaNo ratings yet
- STDDocument78 pagesSTDKrupa KarnikNo ratings yet
- SchistosomiasisDocument27 pagesSchistosomiasisNarz Cupahan0% (1)
- Parapneumonic Pleural Effusions and Empyema Thoracis - Background, Pathophysiology, EpidemiologyDocument4 pagesParapneumonic Pleural Effusions and Empyema Thoracis - Background, Pathophysiology, EpidemiologyLorentina Den PanjaitanNo ratings yet
- Basic Concepts in Psychiatric NursingDocument10 pagesBasic Concepts in Psychiatric NursingKhristine Paladan ZernaNo ratings yet
- Midterms ObDocument29 pagesMidterms ObMary Grace Bañes100% (1)
- Typhoid FeverDocument23 pagesTyphoid FeverAs ShahirahNo ratings yet
- Communicable DiseaseDocument22 pagesCommunicable DiseaseheheeheheNo ratings yet
- AntibioticsDocument22 pagesAntibioticsEllen Castillo MarianoNo ratings yet
- Chronic SinusitisDocument12 pagesChronic SinusitisrafiNo ratings yet
- A Study On Evaluation of Factors Affecting Child ImmunizationDocument53 pagesA Study On Evaluation of Factors Affecting Child ImmunizationAbhishek JaluthriaNo ratings yet
- Drug StudyDocument4 pagesDrug StudyCharlyn Mae BirondoNo ratings yet
- Obstetirc NursingDocument36 pagesObstetirc NursingGlenn Daryll SantosNo ratings yet
- Sem2 Anti TB DrugsDocument35 pagesSem2 Anti TB DrugsZijieNo ratings yet
- Complement SystemDocument6 pagesComplement SystemJimit GandhiNo ratings yet
- NCM 109 Cellular AbberationsDocument17 pagesNCM 109 Cellular AbberationsSittie Haneen Tabara100% (1)
- Cardiovascular SystemDocument26 pagesCardiovascular SystemJenny Torreda100% (1)
- Nursing Care of Clients in Emergency Situation 1Document48 pagesNursing Care of Clients in Emergency Situation 1Danica FrancoNo ratings yet
- NCM 112 Fluid and ElectrolytesDocument2 pagesNCM 112 Fluid and ElectrolytesAngeline NavarroNo ratings yet
- S4 L5 SchistosomaDocument5 pagesS4 L5 Schistosoma2013SecBNo ratings yet
- Bio 2 Quiz ReviewerDocument2 pagesBio 2 Quiz ReviewerAlexandra RoderoNo ratings yet
- Inflammatory and Immunologic DisturbancesDocument91 pagesInflammatory and Immunologic DisturbancesRitamaria100% (6)
- Immune System and Lymphatic SystemDocument5 pagesImmune System and Lymphatic SystemEduardson PHNo ratings yet
- Immunologic Disorders FileDocument8 pagesImmunologic Disorders FileBryan Dimen100% (1)
- Drug Study ValiumDocument4 pagesDrug Study ValiumEric EvangelistaNo ratings yet
- Drug Study For Hepatic ABCESSDocument3 pagesDrug Study For Hepatic ABCESSEric EvangelistaNo ratings yet
- Health Teaching Plan FormDocument3 pagesHealth Teaching Plan FormEric EvangelistaNo ratings yet
- Health Teaching Plan FormDocument3 pagesHealth Teaching Plan FormEric EvangelistaNo ratings yet
- Trying It Out: TH THDocument10 pagesTrying It Out: TH THEric EvangelistaNo ratings yet
- NCP For Parent and ChildDocument3 pagesNCP For Parent and ChildEric Evangelista100% (1)
- Lifestyle and Gallstone Disease: Scope For Primary PreventionDocument1 pageLifestyle and Gallstone Disease: Scope For Primary PreventionEric EvangelistaNo ratings yet
- Alternative Media in The Philippines and Beyond. by Eric EvangelistaDocument17 pagesAlternative Media in The Philippines and Beyond. by Eric EvangelistaEric Evangelista0% (1)
- Fixative TableDocument11 pagesFixative TableNicole Kimberly Yu100% (1)
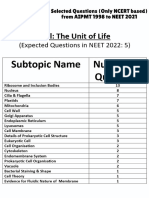
- Cell - The Unit of Life - NCERT Based PYQsDocument9 pagesCell - The Unit of Life - NCERT Based PYQsAkhil singhNo ratings yet
- Neuro Part 2Document6 pagesNeuro Part 2vetthamilNo ratings yet
- CBSE Class 11 Biology Chapter 21 Neural Control and Coordination NotesDocument7 pagesCBSE Class 11 Biology Chapter 21 Neural Control and Coordination NotesShivalgiri Goswami0% (1)
- Ayurvedic Approach To RheumatologicDocument11 pagesAyurvedic Approach To RheumatologicBrad YantzerNo ratings yet
- PlacentaDocument6 pagesPlacentaKishore Singh BasnetNo ratings yet
- Sensory and Motor Nerve EndingsDocument42 pagesSensory and Motor Nerve EndingsMark GanirNo ratings yet
- APCH1 - Single Chain Antibody For Vaccine TargetingDocument6 pagesAPCH1 - Single Chain Antibody For Vaccine TargetingAgustín OstachukNo ratings yet
- Cell AnalogyDocument24 pagesCell AnalogyBOBOBOYS TVNo ratings yet
- Amniotic Fluid 2022Document40 pagesAmniotic Fluid 2022Ogbuefi PascalNo ratings yet
- Extracellular VesicleDocument14 pagesExtracellular VesicleLucas Monteiro LopesNo ratings yet
- Vasculitis Cerebrales: H.A. Arroyo, R.A. Russo, C. RugiloDocument11 pagesVasculitis Cerebrales: H.A. Arroyo, R.A. Russo, C. RugiloCiarol BorbonNo ratings yet
- 2015 Wassce - Biology 2 SolutionDocument9 pages2015 Wassce - Biology 2 SolutionKelvin Yeboah TenkorangNo ratings yet
- Chronic Expanding Hematoma Following AbdominoplastyDocument4 pagesChronic Expanding Hematoma Following AbdominoplastyGabriela Serra del CarpioNo ratings yet
- Pengaruh Pemberian Terapi Latihan Metode SchrothDocument7 pagesPengaruh Pemberian Terapi Latihan Metode SchrothsulaimanNo ratings yet
- The Human Immune SystemDocument24 pagesThe Human Immune Systemmilka berhaneNo ratings yet
- Nle Notes MCNDocument33 pagesNle Notes MCNjosephmary09No ratings yet
- ) Science (Department: Grade (10) Final Revision Worksheet (Biology)Document13 pages) Science (Department: Grade (10) Final Revision Worksheet (Biology)Toto BjNo ratings yet
- Veterinary DermatologyDocument1 pageVeterinary DermatologyCiolacu Victor AdrianNo ratings yet
- CHD 121 Anatomy and Physiology Course OutlineDocument2 pagesCHD 121 Anatomy and Physiology Course Outlinemalenya1No ratings yet
- Cardiorespiratory SystemDocument15 pagesCardiorespiratory SystemDafchen Villarin MahasolNo ratings yet
- 1.4 Selecton of Blood BagDocument3 pages1.4 Selecton of Blood BagBALAJINo ratings yet
- After Effects of COVID 19 and Repair of LungsDocument13 pagesAfter Effects of COVID 19 and Repair of LungsAthenaeum Scientific PublishersNo ratings yet
- Part of BodyDocument4 pagesPart of Bodyanon_535068952No ratings yet
- GRADE 12 LAB - MANUAL 2023 2024 - ApprovedDocument46 pagesGRADE 12 LAB - MANUAL 2023 2024 - ApprovedZainab AlziftawiNo ratings yet