Professional Documents
Culture Documents
Akut Sinu
Uploaded by
Bryan De HopeOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Akut Sinu
Uploaded by
Bryan De HopeCopyright:
Available Formats
Diagnosing ARIs Series
Acute sinusitis
Graham Worrall MBBS MSC FCFP
ecause children have very small, underdeveloped sinuses, acute sinusitis in children is rarely seen in general practice. This article considers the common type of sinusitis seen in adults.
One Tuesday moming Fred Brown, a 35-year-old accountant, comes to see you. He complains of 2 days of pain in both cheeks and his forehead; he has a runny nose and a slightly sore throat, and he is having a hard time concentrating at work. He does not have afever or a cough. His medical record shows that, apart from a broken arm when he fell off his bike at 15 and acute appendicitis when aged 23, he has had no serious illness. He is not taking any long-term medication. He has come to your office 3 times in the past 5 years: for influenza, for a head cold, and for sinusitis, receiving antibiotics from . a colleague of yours for the sinusis. He is married with 2young children.
toothache, tooth or gum infections, temporomandibular (TM) joint pain, tic doloureux (trigeminal neuralgia), facial herpes simplex, and facial herpes zoster.
Mr Brown says that he gets regular dental checkups, and he believes his teeth and gums to be healthy. The pain is not worse when he is chewing or biting. He has not noticed any pain in his ears, and he can move his face normally. His nose is runny, and his nostrils are partly blocked. He has not noticed a rash; he cannot remember having chickenpox; and he is not prone to cold sores. Before examining Mr Brown, you consider what other more serious illnesses it could be.
Epidemiology and population at risk
Approximately 0.5% of all upper respiratory tract infections are complicated by sinusitis; the incidence of acute sinusitis ranges from 15 to 40 episodes per 1000 patients per year, depending on the setting.''^ It is much more common in adults than it is in children, whose sinuses are not fully developed.^ Acute sinusitis is the second most common infectious disease seen by GPs.^'^ Most acute sinusitis is caused by the same viruses that cause the common cold."^ Although up to one-third of adult patients seen in ears, nose, and throat clinics might have acute bacterial sinusitis (and cultures of antral puncture specimens show Streptococcus pneumoniae and Haemophilus influenzae to be the most common causative bacteria), the proportioh of cases of acute sinusitis due to bacteria is much smaller in primary careprobably less than 2%.' It has been found that 75% or more of patients with sinusitis in the placebo groups of antibiotic trials get better spontaneously within 7 to 10 days."* Complications from acute bacterial sinusitis are very rare; none occurred in the placebo arms of the primary care antibiotic trials.
As Mr Brown has a runny nose and has only experienced facial pain for 2 days, it is likely his symptoms are due to the common cold. His job entails meeting a lot of other people, and he probably picked up an infection from one of them.
Alarm symptoms. Mr Brown reports no fever (more characteristic of acute bacterial infection), and he does not feel particularly ill (degree of illness and slowness of recovery have been found to be associated with more severe illness). There has been no rash on his face (as in herpes simplex or zoster), and there is no pain when he moves his face (as in tic doloureux or TM joint dysfunction). Alarm signs. There might be pus seen in the ostia or the cavity of the nose (suggesting bacterial infection). There might be a high fever. The patient might be constitutionally ill (characteristic of acute bacterial infections or of spread of disease from the sinusitis). Spread . of sinusitis to the central nervous system will produce lethargy or neurologic signs. Herpes simplex and zoster produce characteristic rashes.
Mr Brown has no alarhn symptoms. You proceed to examine him. His temperature is 36.8C; his pulse is 72 beats/min. He has a runny nose, but you do not see any purulent discharge in either nostril or in his pharynx. Palpation reveals slight tenderness over his lefl maxilla, but his ears,' teeth, gums, and TM joints are normal. He has no trouble breathing; findings fiom his chest examination are ncirmal. He is alert and orientated. He has no rash, no swollen glands, and no alarm signs. You are becoming more certain that he probably has acute viral sinusitis complicating a common cold.
What else could it be?
other causes of facial pain (which need to be excluded) include the following:
This article is eligible for Malnpro-MI credits. To earn credits, go to www.cfp.ca and click on the Mainpro link.
VOL 57: MAY MAI 2011 | Canadian Family Physician i e Mdecin de famille canadien 5 6 5
Diagnosing ARIs Series
How sure of the diagnosis are you?
Acute sinusitis is a classic primary care diagnosis, usually made based on history and examination alone. This is because investigations, whether simple (transillumination, plain sinus x-ray scans, or culture of nasal discharge) or more complex (ultrasonography or computed tomography [CT] scans), have been found to be of no diagnostic value in the primary care population with sinusitis." Many attempts have been made to identify a constellation of signs and symptoms that will increase the likelihood of bacterial sinus infection being present.'^"^ The most important signs, symptoms, and test results, as well as their likelihood ratios (LRs) for presence or absence of bacterial sinusitis, are shown in Table I."*
Table 1. Likelihood ratios for the presence or absence ] of bacterial sinusitis :
POSITIVE LIKELIHOOD RATIO NEGATIVE : LIKELIHOOD ' RATIO
nonsinusitis symptoms show mucosal abnormalities,"* and 87% of people with uncomplicated common colds also show sinus abnormalities on CT scan."
The absence ofpurulent nasal discharge, fever, prolonged illness, and severe illness, plus only a moderate degree of sinus tenderness, all make it likely that Mr Brown is sufferingfiom a common cold with sinus congestion. You inform him that he likely has viral sinusitis and that it is a self-limiting disease for which antibiotics will not provide any benefit.
Is it likely to get worse?
In otherwise healthy people, viral sinusitis is usually selflimiting and rarely produces serious after-effects. Most patients vAW get better without treatment in 7 to 10 days. In the control groups in the trials of antibiotics for sinusitis, 90% of untreated patients were completely better by the end of 1 week, about the same as the proportion of those treated with antibiotics.'^ When symptoms persist beyond 7 days, and when the patient experiences a "second sickening," the possibility of bacterial sinusitis increases, but serious complications from bacterial sinusitis are very rare.
SIGNS, SYMPrOMS, AND TEST RESULTS
Symptoms Purulent rhinorrhea Unilateral face pain Pain in teeth 2-phase illness No relief from decongestants Signs Purulent nasal secretion Pain on stooping Transillumination Tender maxillary sinus Blood test results ESR >10 mm/h CRP level > 10 mg/L 2.9 1.8 0.70 0.45 5.5 1.6 1.6 0.75 1.5 1.8 2.5 2.1 2.1 0.26 1.3 0.66 0.43 0.7
Deciding on the best treatment
In Europe and North America, more than 90% of patients with diagnoses of "acute sinusitis" in primary care receive prescriptions for antibiotics." This occurs despite the selflimiting natural history of untreated sinus infections and the results of the many antibiotic trials, which show that most patients in the placebo groups get better almost as quickly as those who receive antibiotic treatment. Many patients (like Mr Brown on a previous visit) have received antibiotics before and have an expectation that they should receive them when they have sinusitis again. There have been relatively few trials of antibiotics for adults with acute sinusitis in the primary care setting; in gerieral, those that have been done show that although antibiotics clear up the colour of the purulent mucus, they have little effect on the duration or severity of the illness. The best systematic review'^ found that the beneficial effects, if any, were so small that the number needed to treat for 1 patient to benefit slightly was about 16 patients, a number greater than that needed to produce an antibiotic side effect (approximately 10). Unfortunately, one study has clearly shown that no combination of symptoms and signs can predict which patients are likely to have more prolonged illness or if a particular patient is one of the small minority who might benefit from antibiotic treatment." Another review suggests that if an antibiotic is used the best one in primary care is probably a cheap broad-spectrum one such as amoxicillin,' and that a 5-day course is probably as effective as a 10-day course.^" Because of the disappointing response to antibiotics, perhaps it is better to concentrate on relieving the
0.45
0.33 NA 1.54
I
; ; '
CRP-C-reactive protein, ESR-erythrocyte sedimentation rate, NA-not applicable. Data from Lindbaek and Hjortdahl."
It is Striking that all the LRs, both positive and negative, are low. The only one that approaches a value that would substantially change a physician's estimate of the likelihood of disease is the positive LR for the presence of purulent nasal secretion. Because of the low LRs associated with these symptoms, signs, and test results, there is currently no evidencebased decision rule that is useful for the diagnosis of acute sinusitis in primary care. The diagnosis is usually clinicalcultures from the nasopharynx do not reflect the organisms causing sinusitis." Transillumination of the sinuses has low sensitivity.^ Ultrasonography has also proven to be of little value for diagnosing sinusitis in primary care populations.'" Although CT scans have been recommended by some experts, 40% of people who have CT scans for
566
Canadian Family Physician Le Mdecin de famille canadien | VOL 57: MAY MAI 2011
Diagnosing ARIs Series
patient's symptoms. Textbooks suggest comfort measures for patients with symptoms of acute sinusitis: maintenance of adequate hydration (to loosen secretions), application of warm facial packs (to help promote drainage of mucus), administration of analgesics (for the localized pain and tenderness), use of decongestants (to increase ostial diameter and promote sinus drainage), and use of saline nose drops (to provide moisture and improve mucociliary function). Unfortunately, no good-quality trials have been done to show that any of these measures are effective. A review suggested that intranasal steroid sprays might be modestly effective for relieving symptoms of acute sinusitis.21 A South African study relieved symptoms with 1-mg betamethaspne tablets daily for 5 days.^^ Unfortunately, these treatments were used concurrently with antibiotics, which made their effects (if any) difficult to quantify. One review found that evidence for the benefit of herbal medicines (whether occidental or oriental) was very limited.^^ A study in the Netherlands found that if a wait-andsee approach were used, 9196 of patients complaining of acute sinus symptoms would get better within 1 week.^" There are no studies to show that intervening in the acute illness has any beneficial effect in preventing chronic sinusitis or the rare acute complications of sinusitis.
You explain to Mr Brown that his sinus symptoms are most likely due to viral infection, and that he is unlikely to benefit fiom antibioticti-eatrnent.His illness will likely last 7 to 10 days, and there should not be any complications. He accepts this, but asks you if there are any medicines other than painkillers or decongestants he can take; in past experience he has found both of these make him drowsy and interfere witii his concenti'ation at work. You explain that there really is not enough evidence to convince you ti^at either steroids or herbal medicines have much effect on the symptoms. Unfortunately, there really is no good treativentfor tiie condition, fhe wants a steroid nasal spray, you are willing to prescribe one.
A Cochrane systematic review" found that, for acute upper respiratory tract infections, use of delayed prescriptions did not result ih patient harm and it reduced antibiotic use. One of the trials reviewed was for acute sinusitis; delaying the aritibiotic prescription made no difference to outcomes. I
You give Mr Brown a prescription for a 5-day course of amoxicillin-davulanate, which he should consider taking if his symptoms do not improve within a few days. '^
Dr Worrall is Honorary Research Professor in the Department of Family Medicine at Memorial University of Newfoundland in St John's. Competing interests None declared Correspondence Dr Graham Worrall, Dr W.H. Newhock Memorial Clinic. Family Medicine. Box 449. Whitbourne, NF AOB 3K0; e-mail gworrallmun.ca References 1. Royal College of General Practitioners, DHSS Office of Population Censuses. Morbidity statistics from general practice 1981-82third National Morbidity Survey. London, UK: HMSO, OfBce for Natiorial Statistics; 1986. 2. Hoogen HJ, Huygen FL, Schellekens jw. Morbidityfiguresftomgeneral practice 19781982. Nijmegen, The Netherlands: Nijmeegs Universitt Huisarten Institut; 1985. 3. Aitken M, Taylor JA. Prevalence of clinical sinusitis in young children followed by primary care physicians. //U/e;gy Clin Immunol 1998;152(3):244-8. 4. McCormick A, Fleming D, Charlton J. Morbidity statisticsfi:omgeneral practicefourth National Morbidi^ Survey 1991-92. London, UK: HMSO, Office for National Statistics; 1995. 5. Australian General Practice Statistics and Classification Centre. The BEACH Project. Ganherra. Australia: Australian Institute of Health and Welfare; 2006. Available from: www.fmrc.org.au/beach. Accessed 2011 Jan 31. 6. Gwaltney JM, Scheid WM, Sande MA, Sydnor A. The microbial aetiology and antimicrobial therapy of adults with acute community-acquired sinusitis: a fifteen-year experience at the University of Virginia and review of other selected studies. ; Allergy Clin Immunol 1992;90(3 Pt 2):457-6l! 7. Puhakka T, Mkel MJ, Alanen A, Kallio T, Korsoff L, Arstila P, et al. Sinusitis in the common co\. J Allergy Clin Immunol l998;102(3):403-8. 8. De Bock GH, Dekker FW, Springer MP, Stolk J, Springer MP, Kievit J, et al. Antimicrobial treatment in acute maxillary sinusitis: a meta-analysis. J Clin Epidemiol 1997;50(8):881-90. ' 9. Low DE, Desrosiers M, McSheny J, Garber G, Williams JW Jr, Remy H, et al. A practical guide for the diagnosis and treatment of acute sinusitis. CMAJ l997;l56(Suppl 6):S1-I4. 10. Alberta Clinical Practice Guidelines Program, The diagnosis and management of acute bacterial sinusitis. Edmonton, AB: AGPGP; 2000. 11. Gwaltney JM Jr. Phillips GD. Miller RD, Riker DK. Gomputed tomographic study of the common co\d. N Engt J Med 1994;330(l):25-30. 12. Williams JW Jr, Aguilar G, Makela M, Gomell J, Holleman DR, Chiquette E, et al. Antibiotics for acute maxillary sinusitis. Cochrane Database Syst Rev 2000;(2):GD000243. Update in: Cochrane Database Syst Rev 2008;(2):GD0OO243. 13. Hansen JG, Schmidt H, Rosborg J, Lund E. Predicting acute maxillaiy sinusitis In a general practice population. BMJ 1995;311 (6999):233-6. 14. Lindbaek M, Hjortdahl P. The clinical diagnosis of acute purulent sinusitis in general practicea review. BrJ Gen Pract 2002;52(479):49l-5. 15. Van Duijn NP. Brouwer HJ, Lamberts H. Use of symptoms and signs to diagnose maxillary sinusitis in general practicecomparison with ultrasonography. BMJ 1992;305(6855):684-7. j 16. Axelsson A, Brorson JE. The correlation between bacterial findings in the nose and maxillary sinus in acute maxillary sinusitis. Laryngoscope 1973;83(12):2003-l 1. 17. Otten FW, Engberts GE, Grote JJ. Ultrasonography as a method of examination in the frontal sinus. Clin Otolaryngol 1991;16(3):285-7. 18. Havas TE, Motbey JA, Gullane PJ. Prevalence of incidental abnormalities on computed tomographic scans of the paranasal sinuses. Arch Otolaryngol Head Neck Surg . 1988;114(8):856-9. 19. De Sutter A. Lemiengre M, Van Maele G, van Driel M, De Meyere M, Ghristiaens T, et al. Predicting prognosis and effect of antibiotic treatment in rhinosinusitis. Ann Fam Med 2006;4(6):486-93. 20. Institute for Glinical Systems Improvement. Health care guideline: acute sinusitis in adults. Bloomington, MN: Institute for Clinical Systems Improvement; 2002. Available from: www.icsi.org. Accessed 2011 Jan 31. 21. Zalmanovici C, Yaphe J. Intranasal steroids for acute sinusitis. Cochrane Database Susi Rev 2OO9;(4):GDOO5I49. 22. Ratau NP, Snyman JR, Swanepoel C. short-course, low-dose oral betamethasone as an adjunct in the treatment of acute infective sinusitis: a comparative study with placebo. Clin DrugInvestig2004;24{\0):577-B2. 23. Guo R, Canter PH, Ernst E. Herbal medicines for the treatment of rhinosinusitis: a systematic review. Otolaryngol Head Neck Surg 2006;135(4):496-506. 24. De Bock GH, van Erkel ER. Springer MP, Keviet J. Antibiotic prescriptions for acute sinusitis in otherwise healthy adults: clinical cure in relation to costs. Scand J Prim Health Care 200\,\9U):S8-63. 25. Spurling GK. Del Mar CB, Dooley L, Foxlee R. Delayed antibiotics for respiratory infections. Cochrane Database Syst Rev 2007;(4):GD0044l7,
Is it safe to wait and see?
In the antibiotic trials, patients in the placebo-control groups were no more ill than those receiving treatment.
Mr Brown is a healthy man, and it is likely that the worst of his infection is over; he will probably be better in a few days. There is no harm in taking analgesics, decongestants, or steroids for a short while. As there are no signs of complications, you suggest that things will improve spontaneously, but he should come back to see you if the condition worser\s or does not improve in a few days, or if he develops a fever Mr Brown mentions that he is due to leave town in 3 days for a business meeting. He is worried that he might get worse while he is away in a sti'ange city. Could he have an antibiotic prescription to take, just in case he gets worse?
VOL 57: MAY MAI 2011 | Canadian Family Physician Le Mdecin de famille canadien
567
Copyright of Canadian Family Physician is the property of College of Family Physicians and its content may not be copied or emailed to multiple sites or posted to a listserv without the copyright holder's express written permission. However, users may print, download, or email articles for individual use.
You might also like
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (120)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- USMLE PathognomicsDocument9 pagesUSMLE PathognomicsMatt McGlothlin94% (18)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- Nclex DietDocument109 pagesNclex DietDanica Chiara Motia100% (4)
- Trigger Point InjectionDocument10 pagesTrigger Point Injectionv_vijayakanth7656No ratings yet
- IMCI Session 3-The Integrated Case Management ProcessDocument67 pagesIMCI Session 3-The Integrated Case Management Processsarguss1480% (5)
- GastritisDocument6 pagesGastritisNader Smadi100% (5)
- Concept of Health and IllnessDocument28 pagesConcept of Health and IllnessCeline Eliz Ang86% (7)
- Atenolol Drug StudyDocument2 pagesAtenolol Drug StudyFranz.thenurse6888100% (2)
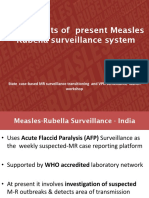
- 07a Ongoing MR Outbreak Surveillance SystemDocument23 pages07a Ongoing MR Outbreak Surveillance SystemDevendra Singh TomarNo ratings yet
- Follow UpDocument2 pagesFollow UpBryan De HopeNo ratings yet
- Anti-Fungal Activity of Capsicum Frutescence and Zingiber Officinale Against Key Post-Harvest Pathogens in CitrusDocument6 pagesAnti-Fungal Activity of Capsicum Frutescence and Zingiber Officinale Against Key Post-Harvest Pathogens in CitrusBryan De HopeNo ratings yet
- Story of My LifeDocument3 pagesStory of My LifeBryan De HopeNo ratings yet
- 4919 13766 1 PBDocument4 pages4919 13766 1 PBBryan De HopeNo ratings yet
- Situasi Kamar GueDocument1 pageSituasi Kamar GueBryan De HopeNo ratings yet
- Razer Cortex Diagnostics ReportDocument8 pagesRazer Cortex Diagnostics ReportBryan De HopeNo ratings yet
- Kistral Guide ArtileryDocument5 pagesKistral Guide ArtileryBryan De HopeNo ratings yet
- Add On MozillaDocument1 pageAdd On MozillaBryan De HopeNo ratings yet
- Me 1Document7 pagesMe 1Bryan De HopeNo ratings yet
- Situasi Kamar GueDocument1 pageSituasi Kamar GueBryan De HopeNo ratings yet
- Application PDFDocument2 pagesApplication PDFBryan De HopeNo ratings yet
- Working Armour Control of Sprains Train Injuries 20251Document30 pagesWorking Armour Control of Sprains Train Injuries 20251Bryan De HopeNo ratings yet
- Add On MozillaDocument1 pageAdd On MozillaBryan De HopeNo ratings yet
- DissertationDocument136 pagesDissertationBryan De HopeNo ratings yet
- Amaurosis Fugax: Alternative NamesDocument2 pagesAmaurosis Fugax: Alternative NamesBryan De HopeNo ratings yet
- Sudden Visual Loss Clinical PresentationDocument8 pagesSudden Visual Loss Clinical PresentationBryan De HopeNo ratings yet
- LirikDocument29 pagesLirikBryan De HopeNo ratings yet
- MUSCULOSKELETAL Sprains Strains Dislocations - NarraDocument4 pagesMUSCULOSKELETAL Sprains Strains Dislocations - NarraBryan De HopeNo ratings yet
- Sprains and Strains FFDocument4 pagesSprains and Strains FFBryan De HopeNo ratings yet
- 86 Normal Low Tension GlaucomaDocument4 pages86 Normal Low Tension GlaucomaBryan De HopeNo ratings yet
- GINA Pocket2013 May15Document0 pagesGINA Pocket2013 May15David BarzalloNo ratings yet
- Sprains and Strains FFDocument4 pagesSprains and Strains FFBryan De HopeNo ratings yet
- Scabies - NarraDocument2 pagesScabies - NarraBryan De HopeNo ratings yet
- Sri An A 0202Document12 pagesSri An A 0202SelviNo ratings yet
- Scabies - NarraDocument2 pagesScabies - NarraBryan De HopeNo ratings yet
- Industry Interventions For Addressing MSD in NZ Meat ProcessingDocument49 pagesIndustry Interventions For Addressing MSD in NZ Meat ProcessingBryan De HopeNo ratings yet
- MUSCULOSKELETAL Sprains Strains Dislocations - NarraDocument4 pagesMUSCULOSKELETAL Sprains Strains Dislocations - NarraBryan De HopeNo ratings yet
- 4919 13766 1 PBDocument4 pages4919 13766 1 PBBryan De HopeNo ratings yet
- Guia Muscul en Angles.v1355478068 2Document25 pagesGuia Muscul en Angles.v1355478068 2Bryan De HopeNo ratings yet
- Guia Muscul en Angles.v1355478068 2Document25 pagesGuia Muscul en Angles.v1355478068 2Bryan De HopeNo ratings yet
- Presentation Slides: Health and Climate ChangeDocument24 pagesPresentation Slides: Health and Climate ChangeSouth East Asia Regional DelegationNo ratings yet
- Slide Chronic Pain-Rudy Hidayat-Iai PDFDocument30 pagesSlide Chronic Pain-Rudy Hidayat-Iai PDFAsri ArrachmanNo ratings yet
- Acute Respiratory InfectionDocument9 pagesAcute Respiratory InfectionStephen FoxNo ratings yet
- Leung and Lam 2018Document9 pagesLeung and Lam 2018Wahida MuntazaNo ratings yet
- FORMAT Discharge PlanDocument5 pagesFORMAT Discharge PlanButchay LumbabNo ratings yet
- Grade 5 Term 1 SchemeDocument203 pagesGrade 5 Term 1 SchemeConistance GatsiNo ratings yet
- Lab Manual VPE311Document40 pagesLab Manual VPE311Friends ZoneNo ratings yet
- Is Pneumonia ContagiousDocument3 pagesIs Pneumonia ContagiousCallMeSashaNo ratings yet
- QuizlewwwDocument90 pagesQuizlewwwnaimNo ratings yet
- A. The Sum of All Chemical Reactions in The Organisms, That Produce Energy or Synthesize Organic MatterDocument5 pagesA. The Sum of All Chemical Reactions in The Organisms, That Produce Energy or Synthesize Organic MatterShane Aileen AngelesNo ratings yet
- The Pathophysiology of LabyrinthitisDocument2 pagesThe Pathophysiology of LabyrinthitisSurya Michael ChanceNo ratings yet
- Venesection: Phlebotomy orDocument20 pagesVenesection: Phlebotomy orVera June RañesesNo ratings yet
- Anger Management JournalDocument1 pageAnger Management JournalRidwan SyafiudinNo ratings yet
- 4th & 5th April-2016-All Papers (1032MCQS) by Amlodipine BesylateDocument61 pages4th & 5th April-2016-All Papers (1032MCQS) by Amlodipine BesylateZohaib Ahmed MemonNo ratings yet
- Parasitology Slide Presentation SET BDocument28 pagesParasitology Slide Presentation SET BNorjetalexis CabreraNo ratings yet
- Preserving Body Image and Self-EsteemDocument47 pagesPreserving Body Image and Self-EsteemGhostNo ratings yet
- Conduction System of HeartDocument2 pagesConduction System of HeartEINSTEIN2DNo ratings yet
- Jeopardy Digestive and Urinary SystemsDocument27 pagesJeopardy Digestive and Urinary Systemsapi-133770097No ratings yet
- IJPN 24 March With DOIDocument252 pagesIJPN 24 March With DOIShrutiMarwahNo ratings yet
- IMCI Orientation and Planning Guidelines For Provinces and DisrictsDocument83 pagesIMCI Orientation and Planning Guidelines For Provinces and DisrictsCAREZAMBIA100% (1)
- Primary and Secondary TuberculosisDocument22 pagesPrimary and Secondary TuberculosisRahul Patil100% (1)
- Cardiac FibromaDocument12 pagesCardiac FibromaBhupendraNo ratings yet