Professional Documents
Culture Documents
Pharmacology Pharmacokinetics Flash Cards
Uploaded by
bobiomeCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Pharmacology Pharmacokinetics Flash Cards
Uploaded by
bobiomeCopyright:
Available Formats
What is the meaning of
pharmacokinetics?
The sutyd of drug movement
throughout the body. lt describes
how the body deals with
medications.
What is the greates barrier
drugs face in reaching their
target cells?
Crossing membranes
What are the four categories of
pharmacokinetics (processes)?
1. absorption
2. distribution
3. metabolism
4. excretion
What 2 ways do drugs cross
body membranes?
1. Active transport (against
concentration/electrochemical
gradient)
2. Diffusion/passive transport
What is absorption?
A process involving the movement of a
substance from its site of administration,
across body membranes, to circulating
fluids.
Which is faster in regard to
absorption--lM
administration or lV
administration? Why?
lV administration because it
enters the bloodstream
directly.
What factors affect
aborption?
Dose of medication
Speed of digestion
Exposure to enzymes (Gl)
Blood flow to site of admin.
Degree of ionization (pH)
Drug/Drug and Food/Drug interactions
ln a basic environment,
aspirin is mostly in what
form? What happens to the
absorption?
lonized form
ln this case, absorption is
prevented.
ls aspirin an acidic or a
basic substance?
Aspirin (ASA) is a weak acid
What is affinity in regard to
pharmacokinetics?
Affinity is the attraction that tissues
have for certain medications.
Only (bound/unbound) drugs can
reach their targe cells or be
excreted by the kidneys.
Unbound (free) drugs
Give examples of two spcial
anatomic barriers that prevent
many chemicals and medications
from entering.
Blood-brain barrier
Fetal-plancental barriers
List some medications that are
readily able to cross the blood-
brain barrier and produce actions
in the CNS.
sedatives
anti-anxiety agents
anticonvulsants
List some substances that easily
cross the plancental barrier and
can potentially harm the fetus.
alcohol
cocain
caffeine
certain Rx meds
What is another name for
metabolism in regard to
medications?
biotransformation
What is the hepatic
microsomal enzyme
system?
The enzyme complex (P-450
system) which inactivates drugs
and acclerates their excretion.
What is the "first-pass"
effect?
This is when drugs absorbed after oral administration
cross directly into the hepatic portal circulation, which
carries blood to the liver before it is distributed to other
body tissues (therefore, some drugs can be completely
metabolized to an inactive form before reaching the
general circulation)
List the steps of the first-
pass effect
1. drugs are abbsorbed
2. drugs enter the hepatic portal circultion and go driectly
to the liver forming...
3. drug conjugates, leaving liver
4. drug is distributed in the general circulation
What are conjugates?
Side chains added to drugs during
metabolism to make them more water
soluble and easily excreted by the
kidneys.
What are prodrugs?
Agents that have no pharmacologic activity
unless first metabolized to their active form by
the body
ie: benazepril (Lorensin)
losartan (Cozaar)
What is enzyme induction?
The process that increases metabolic activity in the liver,
which may require higher doses of meds to achieve the
optimum therapeutic effect.
(ie: phenobarbital causes the liver to synthesize more
microsomal enzymes, therefore increases the rate of its
own metabolism.)
What is excretion?
Drugs being removed from
the body.
What is the primary site of
excretion?
Kidneys
What is the kidney filtration
rate in an average-size
person?
180 L of blood each day
What substances are
filtered at the glomerulus?
Free drugs
Water-soluble agents
Electrolytes
Small molecules
What substances are not
filtered due to large size?
Proteins
Blood cells
Conjugates
Drug-protein complexes
Patients with renal failure will have
(diminished/enhanced) ability to
excrete medications
Diminished, therefore they
may retain drugs for an
extended period of time.
The rate of respiratory excretion is
dependent on factors that affect
gas exchange. List those factors.
Diffusion
Gas solubility
Pulmonary blood flow
What is the relationship between
breathing rate/blood flow to lungs
and excretion?
The faster the breathing rate, the
greater the excretion;
The greater the blood flow into
lung capillaries, the greater the
excretion.
Where are water-soluble
drugs secreted?
Saliva
Sweat
Breast milk
Explain why some patients
experience an "odd" taste when
given lV drugs
This is attributed to the
secretion of agents into the
saliva
Why should nursing mothers
always check with their provider
before taking any Rx, OTC drugs,
or herbal supplements?
Because these agents can be
secreted into breast milk, thus
becoming an exposure risk to the
infant.
What is the minimum
effective concentration?
The amount of drug
required to produce a
therapeutic effect
What is the toxic
concentration?
The level of drug that will
result in serious adverse
effects
The plasma concentration between the
minimum effective concentration and the
toxic concentration is called the what?
Therapeutic range
Define plasma half-life
The length of time required for the
plasma concentration of a medication to
decrease by one-half after administration
(can be a few minutes to hours or days)
What is the relationship
between half-life and
excretion?
The greater the half-life, the longer it takes a
medication to be excreted.
ie: A drug with t 1/2 of 10 hours would take
longer to be excreted than a drug with t 1/2 of 5
hours.
Given the following:
t 1/2 = 14 hours
t 1/2 = 2 days
Which medication would produce
an effect that would last longer in
the body?
The drug with the t 1/2 of 2 days
(longer half-life = longer duration,
longer effect, takes longer to be
excreted)
Drugs with relatively short half-lifes (ie:
aspirin t 1/2 =15-20 min) need to be
given how often? What about drugs with
longer half-lifes (ie: Plendil t 1/2 = 10
hours)?
Aspirin--every 3-4 hours
felodipine
(Plendil)==once/day
lf a patient has extensie renal or hepatic
disease, the plasma half-life of a drug will
(increase/decrease). Explain.
lncrease. The drug concentration
may reach toxic levels, therefore
dosages must be reduced and
meds given less frequently.
How long does it take
(theoretically) to reach even
distribution of continuous
therapeutic level of drug to body
tissues (equilibrium)?
4 half-lives
What is a loading dose?
Maintenance dose?
Loading--higher amount of drug, often given
only once or twice to "prime" the bloodstream
with a sufficient level of drug
Maintenance--given to keep the plasma drug
concentration in the therapeutic range.
Using a routing dosing
schedule with antibiotics,
how long does it take to
reach therapeutic level?
Almost 5 doses (48 hours)
How long does it take to reach
therapeutic level when using a
loading dose of antibiotics?
Level is reached within 12
hours
What can frequency
distribution curves show?
1. The number of patients responding to
a drug action at different doses
2. Represents the safety of a drug (think
median lethal dose)
Give the equation for
Therapeutic lndex
Tl = median lethal dose
divided by median effective
dose
What is the meaning of
therapeutic index?
lt is a measure of the drug's safety
margin: The higher the
therapeutic index, the safer the
medication
How is the median toxicity
dose calculated?
TD50 is the dose that will produce
a given toxicity in 50% of a group
of patients.
How is median lethal dose
calculated?
The LD50 cannot be
experimentally determined in
humans, so it is tested on animals
during the phase trials.
What is the relationship between
the two components of the
equation for therapeutic index?
The larger the difference between
the two doses, the greater the
therapeutic index, thus the safer
the medicine.
Explain potency
A drug that is more potent will
produce a therapeutic effect at a
lower dose, compared with
another drug in the same class.
Explain efficacy
The magnitude of maximal
response that can be produced
from a particular drug.
Which is more important?
Potency or efficacy?
Efficacy is almost always more
important than potency, from a
pharmacotherapeutic perspective.
How do drugs act?
By modulating or changing
existing physiologic and
biochemical processes.
What is a receptor?
The cellular macromolecule to
which a medication binds in order
to initiate its effects
Explain the receptor theory
A drug binds to a receptor to cause a change in body
chemistry or physiology. These receptors do not exist in
the body solely to bind drugs. Their normal function is to
bind endogenous molecules (hormones,
nerotransmitters, growth factors)
What type of substance are
the majority of
macromolecules?
Proteins
Once a drug binds to the
receptor, what happens?
A series of second messenger events within the cell may
be triggered (ie: conversion of adenosine
triphosphate--ATP--to cyclic-AMP) and biochemcial
cascades initiate the drug's action by either stimulating
or inhibiting normal activity of the cell.
How many basic receptor
types exist?
Two--alpha and beta
Both have subtypes (alpha 1&2,
and beta 1&2)
A drug that produces the same
type of response as the
endogenous substance is known
as
an agonist
What is an antagonist?
A drug that occupies a receptor
and prevents the endogenous
chemical from acting.
ls atropine an agonist or an
antagonist?
An antagonist--it inhibits the
effects of acetylcholine by
competing for the binding sites
ls competitive inhibition the
only way antagonists work?
Explain.
No. Functional antagonists inhibit the effects of
an agonist not by competing for a receptor but
by changing the pharmacokinetic factors
(slowing absorption, speeding up metabolism or
excretion, etc.)
Males of Mediterranean and
African descent are more likely to
express a deficiency in the
enzyme glucose-6phosphate
dehydrogenase (G6PD). What
does this result in?
ln administering certain drugs (ie: primaquine,
sulfonamides, nitrofurantoin) an acute hemolysis of red
blood cells occurs and up to 50% of the circulating RBCs
may be destroyed. Nurses must observe patients
carefully following the admin of these meds. Their are
alternative medications.
What are idiosyncratic
reactions?
Unpredictable and
unexplained drug reactions
What is a drug that occupies a
receptor site and prevents
endogenous chemicals from
acting?
An antagonist
Morphine has a greater efficacy than either of the OTC
drugs aspirin or acetaminophen. Based on what a nurse
knows about efficacy, what patient condition might
require a dose of morphine rather than aspirin or
acetaminophen?
A patient in moderate to
severe pain after the otehr
drugs have been ineffective
for pain relief
You read that the drug to be given
to a patient has a "narrow
therapeutic index", this means
The drug has a narrow safety
margin and even a small increase
in dose may produce adverse or
toxic effects.
You might also like
- Acute Renal Failure-Student-Rapid ReasoningDocument4 pagesAcute Renal Failure-Student-Rapid Reasoningapi-268403950No ratings yet
- QF3 Gastrointestinal DrugsDocument2 pagesQF3 Gastrointestinal DrugsNeil Feliciano Espiritu0% (1)
- Nursing Pharmacology Inflammation Study GuideDocument11 pagesNursing Pharmacology Inflammation Study GuideChelsea Smith100% (1)
- Neuro AssessmentDocument13 pagesNeuro AssessmentOrlea Francisco-Sisio100% (2)
- ABC Interpretation and Pulmonary Function TestsDocument21 pagesABC Interpretation and Pulmonary Function TestsbobiomeNo ratings yet
- Endocrine DisordersDocument3 pagesEndocrine DisordersIrish OrleansNo ratings yet
- Introduction to Key Concepts in PharmacologyDocument30 pagesIntroduction to Key Concepts in PharmacologyCandy crush100% (1)
- EndocrineDocument12 pagesEndocrineAna FelNo ratings yet
- Concept Map COPDDocument2 pagesConcept Map COPDnursing concept mapsNo ratings yet
- Pharmacology LectureDocument45 pagesPharmacology LecturebjhilarioNo ratings yet
- Lecture Pharma Part 1 - 2011-2012Document34 pagesLecture Pharma Part 1 - 2011-2012Harley Justiniani Dela CruzNo ratings yet
- 1.introduction To PharmacologyDocument127 pages1.introduction To PharmacologyblacknurseNo ratings yet
- AUTOIMMUNEDocument75 pagesAUTOIMMUNEEva Boje-JugadorNo ratings yet
- Endocrine Disorders TableDocument6 pagesEndocrine Disorders TablebarbaraNo ratings yet
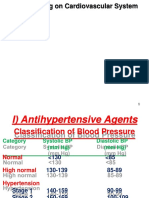
- Drugs acting on the Cardiovascular SystemDocument18 pagesDrugs acting on the Cardiovascular SystemIbrahem AlNo ratings yet
- Drugs Acting On The Respiratory SystemDocument13 pagesDrugs Acting On The Respiratory SystemAlloiBialbaNo ratings yet
- Introduction To Nursing PharmacologyDocument5 pagesIntroduction To Nursing PharmacologyJon Adam Bermudez SamatraNo ratings yet
- Nursing Study Guide Answer KeyDocument174 pagesNursing Study Guide Answer KeyDENNIS N. MUÑOZNo ratings yet
- Cholinergic DrugsDocument11 pagesCholinergic Drugsshivanshpande100% (1)
- Medical Cartoon and The AwesomeDocument2 pagesMedical Cartoon and The Awesomekrrishshrish140% (1)
- Fluids Electrolytes - Acid-Base BalanceDocument11 pagesFluids Electrolytes - Acid-Base BalanceJhosita Flora Laroco100% (1)
- Respiratory System ReviewerDocument7 pagesRespiratory System ReviewerVictoria Ellex TiomicoNo ratings yet
- Diarrhoea Causes, Prevention and TreatmentDocument36 pagesDiarrhoea Causes, Prevention and TreatmentSakshi GargNo ratings yet
- Medical Surgical Nursing - LectureDocument77 pagesMedical Surgical Nursing - LecturePink Majaila GludoNo ratings yet
- Anti Neoplastic and Immunosupressant DrugsDocument29 pagesAnti Neoplastic and Immunosupressant DrugsAshraf Moby100% (1)
- Infectious and Inflammatory Disorders of The Urinary SystemDocument16 pagesInfectious and Inflammatory Disorders of The Urinary SystemBibi Renu100% (1)
- Genitourinary Problem: Nephrotic Syndrome Wilm's Tumor ManagementDocument19 pagesGenitourinary Problem: Nephrotic Syndrome Wilm's Tumor ManagementJayson CruzNo ratings yet
- Aging Perspective and Demography Ncm114 Gerontology Aging PerspectivesDocument19 pagesAging Perspective and Demography Ncm114 Gerontology Aging PerspectivesLeslie CruzNo ratings yet
- NERVOUS SYSTEM Communicable Diseases LEPROSYDocument3 pagesNERVOUS SYSTEM Communicable Diseases LEPROSYFreeNursingNotesNo ratings yet
- Fluid and Electrolyte ImbalanceDocument27 pagesFluid and Electrolyte ImbalanceSimmi Sidhu100% (1)
- Fluid and Electrolyte NotesDocument6 pagesFluid and Electrolyte NotesAshley H Locklear100% (1)
- Assessment of The BreastDocument14 pagesAssessment of The BreastArlyn MendenillaNo ratings yet
- MS4 Midterm NCLEX BurnsDocument5 pagesMS4 Midterm NCLEX BurnsDebbie Dela Cruz100% (5)
- Chronic Renal FailureDocument29 pagesChronic Renal Failuregeorgia.langNo ratings yet
- NCM of Clients With Endocrine DisordersDocument24 pagesNCM of Clients With Endocrine DisordersArgee Alonsabe100% (1)
- NR304 Neurological Study GuideDocument10 pagesNR304 Neurological Study GuideStephanieNo ratings yet
- Neuro Notes #3Document11 pagesNeuro Notes #3Monica JubaneNo ratings yet
- Fluid, Electrolyte, and Acid-BaseDocument6 pagesFluid, Electrolyte, and Acid-BaseRaquel MonsalveNo ratings yet
- The Gastro-Intestinal SystemDocument12 pagesThe Gastro-Intestinal SystemRenelyn ComiaNo ratings yet
- Cancer Types, Causes, Symptoms & TreatmentDocument169 pagesCancer Types, Causes, Symptoms & TreatmentDardarConstantinoNo ratings yet
- MCN II AntepartumDocument28 pagesMCN II AntepartumJharaNo ratings yet
- Completed Concept MapDocument4 pagesCompleted Concept Mapapi-607361848No ratings yet
- Respiratory System DisordersDocument353 pagesRespiratory System Disordersይደግ አብነውNo ratings yet
- Assessment of Digestive and Gastrointestinal FunctionDocument19 pagesAssessment of Digestive and Gastrointestinal Functioncburnett1No ratings yet
- NCLEX - Acid Base Balance Study GuideDocument1 pageNCLEX - Acid Base Balance Study GuideNathalee WalkerNo ratings yet
- IV FluidsDocument17 pagesIV FluidsTiffany NicolèNo ratings yet
- Care of Clients with BurnsDocument3 pagesCare of Clients with BurnsROBERT C. REÑA, BSN, RN, MAN (ue)67% (3)
- Asepsis & Infection ControlDocument8 pagesAsepsis & Infection ControlChutska Jonsewar100% (1)
- Fluid and Electrolyte BalanceDocument257 pagesFluid and Electrolyte BalanceJeth PadillaNo ratings yet
- Neurologic Disorders - NCM 102 LecturesDocument12 pagesNeurologic Disorders - NCM 102 LecturesBernard100% (4)
- Pharmacology Practice Test For NclexDocument10 pagesPharmacology Practice Test For NclexKira99% (96)
- Endocrine System Notes - NCERT BasedDocument8 pagesEndocrine System Notes - NCERT Basedpallab mukherjeeNo ratings yet
- Acid-Base Balance ABGs InterpretationDocument30 pagesAcid-Base Balance ABGs InterpretationQusai IbraheemNo ratings yet
- NoteesDocument177 pagesNoteespearlanne1292100% (1)
- HESI Women's Health:Newborn DrugsDocument8 pagesHESI Women's Health:Newborn Drugsisapatrick8126No ratings yet
- Endocrine Disorders Cont... (For ADRENAL GLAND)Document4 pagesEndocrine Disorders Cont... (For ADRENAL GLAND)Ernie G. Bautista II, RN, MD100% (3)
- Drugs Acting On Respiratory System of AnimalsDocument8 pagesDrugs Acting On Respiratory System of AnimalsSunil100% (4)
- Medsurg 2007Document15 pagesMedsurg 2007WisdomIsMisery100% (1)
- COMPREHENSIVE NURSING ACHIEVEMENT TEST (RN): Passbooks Study GuideFrom EverandCOMPREHENSIVE NURSING ACHIEVEMENT TEST (RN): Passbooks Study GuideNo ratings yet
- Mechanisms of Drug Toxicity: Proceedings of the Third International Pharmacological MeetingFrom EverandMechanisms of Drug Toxicity: Proceedings of the Third International Pharmacological MeetingH. RaškováNo ratings yet
- Nbme 1Document39 pagesNbme 1rockNo ratings yet
- Blank Patient Note For Step2csDocument1 pageBlank Patient Note For Step2csbobiomeNo ratings yet
- Sharma USMLE Study ScheduleDocument10 pagesSharma USMLE Study SchedulebobiomeNo ratings yet
- Pharmacology - Antimicrobial Flash CardsDocument32 pagesPharmacology - Antimicrobial Flash CardsbobiomeNo ratings yet
- Step 1 Physiology Flash CardsDocument22 pagesStep 1 Physiology Flash CardsbobiomeNo ratings yet
- High-Yield Behavioral Science 2nd EdDocument121 pagesHigh-Yield Behavioral Science 2nd Edbobiome100% (2)
- ArenavirusDocument29 pagesArenavirusRamirez GiovarNo ratings yet
- 7 Years - Lukas Graham SBJDocument2 pages7 Years - Lukas Graham SBJScowshNo ratings yet
- Richard CuretonDocument24 pagesRichard CuretonHayk HambardzumyanNo ratings yet
- 5 - Econ - Advanced Economic Theory (Eng)Document1 page5 - Econ - Advanced Economic Theory (Eng)David JackNo ratings yet
- The Human Element is Critical in Personal SellingDocument18 pagesThe Human Element is Critical in Personal SellingArsalan AhmedNo ratings yet
- Introduction To Vitamin C, (Chemistry STPM)Document2 pagesIntroduction To Vitamin C, (Chemistry STPM)NarmeenNirmaNo ratings yet
- Word Formation - ExercisesDocument4 pagesWord Formation - ExercisesAna CiocanNo ratings yet
- Muhammad v. Hall, 10th Cir. (2017)Document12 pagesMuhammad v. Hall, 10th Cir. (2017)Scribd Government DocsNo ratings yet
- People vs. Abad SantosDocument2 pagesPeople vs. Abad SantosTrixie PeraltaNo ratings yet
- Fractional GradingDocument7 pagesFractional Gradingapi-355619062No ratings yet
- The Ontological Argument.: A Basic IntroductionDocument12 pagesThe Ontological Argument.: A Basic IntroductionJas PalNo ratings yet
- Marwar Steel Tubes Pipes StudyDocument39 pagesMarwar Steel Tubes Pipes Studydeepak kumarNo ratings yet
- Benefits and Risks of Dexamethasone in Noncardiac Surgery: Clinical Focus ReviewDocument9 pagesBenefits and Risks of Dexamethasone in Noncardiac Surgery: Clinical Focus ReviewAlejandra VillaNo ratings yet
- Geometry Solving Problems (Circles)Document36 pagesGeometry Solving Problems (Circles)Hero MirasolNo ratings yet
- Vadiyanatha AstakamDocument4 pagesVadiyanatha AstakamRaga MalikaNo ratings yet
- Dwi Athaya Salsabila - Task 4&5Document4 pagesDwi Athaya Salsabila - Task 4&521Dwi Athaya SalsabilaNo ratings yet
- Aiatsoymeo2016t06 SolutionDocument29 pagesAiatsoymeo2016t06 Solutionsanthosh7kumar-24No ratings yet
- Intro To Flight (Modelling) PDFDocument62 pagesIntro To Flight (Modelling) PDFVinoth NagarajNo ratings yet
- AwsDocument8 pagesAwskiranNo ratings yet
- SEO-optimized title for practice test documentDocument4 pagesSEO-optimized title for practice test documentThu GiangNo ratings yet
- MF 04Document21 pagesMF 04Carlos De la CruzNo ratings yet
- Kurukshetra English August '17Document60 pagesKurukshetra English August '17amit2688No ratings yet
- The Sims FreeplayDocument14 pagesThe Sims FreeplayFlorianNo ratings yet
- CBCP Monitor Vol. 17 No. 9Document20 pagesCBCP Monitor Vol. 17 No. 9Areopagus Communications, Inc.No ratings yet
- Christian Appraisal of Feminist Ideologies Among Nigerian Women 2020Document78 pagesChristian Appraisal of Feminist Ideologies Among Nigerian Women 2020Nwaozuru JOHNMAJOR ChinecheremNo ratings yet
- Connectors/Conjunctions: Intermediate English GrammarDocument9 pagesConnectors/Conjunctions: Intermediate English GrammarExe Nif EnsteinNo ratings yet
- Infanrix Hexa RSMKL July 2023Document37 pagesInfanrix Hexa RSMKL July 2023Bayu KurniawanNo ratings yet
- The Pantheon of Greek Gods and GoddessesDocument2 pagesThe Pantheon of Greek Gods and Goddessesapi-226457456No ratings yet
- Ash ContentDocument2 pagesAsh Contentvikasbnsl1No ratings yet
- The Research TeamDocument4 pagesThe Research Teamapi-272078177No ratings yet