Professional Documents
Culture Documents
Neuro Lesions
Uploaded by
kep1313Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Neuro Lesions
Uploaded by
kep1313Copyright:
Available Formats
Neuro: Lesions
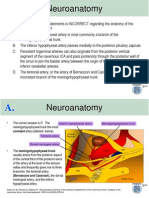
PRINCIPLES SPINAL CORD LESIONS: Can be contralateral, ipsilateral, or bilateral. See figure below. o Total transection Loss of ALL sensation and motor control bilaterally at all levels below the lesion. o Loss of central portion Loss of ALL sensation and motor control bilaterally at every level below the lesion EXCEPT the sacral dermatomes (sacral sparing). o Hemisection Loss of fine touch/propriocep/vibration (DC/ML) ipsilaterally Loss of crude touch/pain/temp (STT) contralaterally at all levels below the lesion. o Loss of white commissure Loss of crude touch, pain, and temp (STT) bilaterally at the level of the lesion but NOT below the lesion. o Loss of dorsal columns Loss of fine touch, proprioception and vibration (DC/ML) bilaterally o Loss of anterolateral system Loss of crude touch, pain, and temp (STT) bilaterally o Loss of spinocerebellar tracts Ataxia BRAIN STEM LESIONS: Can be contralateral or ipsilateral. o Medial Lesions Loss of contralateral motor control (pyramidal tracts). o Lateral Lesions Loss of crude touch, pain, and temp (TTT) in ipsilateral face Loss of fine touch, proprioception, and vibration (DC/ML) in contralateral half of entire body This occurs because the spinothalamic and spinal trigeminal tracts are adjacent in the lateral part of the brainstem. o Vertebrobasiliar Stroke Lesions Three Ds: Contralateral Dysarthria (DC/ML), Ipsilateral Diplopia (CN6), Ipsilateral Dysphagia (CN9 & 10) CEREBRAL LESIONS: Always contralateral. o Internal Capsule Lesion
Loss of ALL sensation and motor control on contralateral half of body (pyramidal and thalamic somatosensory tracts) Muscle weakness on lower quarter of face (corticobulbar tracts) Ventral lesions present with contralateral homonymous hemianopsia IN ADDITION to these sx if optic radiations are affected Trunk ataxia, abnormal eye movements (diplopia) Ipsilateral limb ataxia, intention tremor, fall toward the side of the lesion
CEREBELLAR LESIONS o Vermis o Hemispheres
UMN vs. LMN LESIONS: Everything is lowered in LMN lesion and ramped up in UMN lesions. Note that fasciculations occur with LMN lesions, NOT UMN!
CENTRAL NERVOUS SYSTEM CEREBRUM
Location of Lesion Non-dominant Parietal Lobe Brocas area BROCAS APHASIA Stroke in MCA. Name of Disease SPATIAL NEGLECT SYNDROME Disease Mechanism
Aphasia, Agnosia, Apraxia
Effects (Relative to Location of Lesion) Cognition: Agnosia of the contralateral side of the world.
Cognition: Influent speech with intact understanding.
Brocas area WERNICKES APHASIA Stroke in MCA. Cognition: Fluent speech with impaired understanding.
Thalamus, Caudate, Occipital Lobe
WEBERS SYNDROME
Stroke in PCA.
Contralateral Body: Loss of pain and temperature sensation due to loss of STT, deficits of CN7, CN9 & CN10, hemiparesis and UMN lesion sx, Parkinsonism due to loss of substantia nigra Contralateral Face: Lower face weakness due to loss of corticobulbar tract. Contralateral Eye: Contralateral hemianopia with macular sparing, Ipsilateral Eye: Horners syndrome due to CN3 deficit (ptosis, fixed pupil, down & out gaze).
CENTRAL NERVOUS SYSTEM CEREBELLUM, LIMBIC SYSTEM, DIENCEPHALON, BASAL GANGLIA
Location of Lesion Vermis Hemisphere Cerebellopontine Angle CEREBELLUM Ataxia ACOUSTIC NEURINOMA Tumor spreads from inner ear to the cerebellopontine angle, where CN7 and CN8 exit the brainstem. Tumor compresses CN7 & CN8. Can also compress CN9, CN10 and corticospinal tracts. Name of Disease Disease Mechanism Effects (Relative to Location of Lesion) Axial Muscles: Truncal ataxia, dysarthria. Appendicular Muscles: Body falls toward ipsilateral side. Ipsilateral Ear: Dizziness, pulsating tinnitus deafness. Loss of higher frequencies first. Contrast with Mienieres disease, which loses lower frequencies first. Ipsilateral Face: Paralysis of facial muscles and loss of corneal reflex (efferent arm) due to loss of CN7. Ipsilateral Body: Ataxia due to loss of CN8 and corticospinal tracts. Throat: Hoarseness and trouble swallowing due to loss of CN9 & 10. Tongue: Loss of taste due to loss of CN7. Behavior: Hyperorality, hypersexuality, disinhibited behavior. Memory: Unable to make NEW memories. Old memories are intact. Cognition: Confusion, ophthalmoplegia, ataxia with memory loss, confabulation, personality changes. Arousal: Reduced arousal and wakefulness. Disinhibition of basal ganglia output. Disinhibition of basal ganglia output. Inhibition of basal ganglia output due to destruction of dopaminergic neurons. Contralateral Limb: Wild, flailing involuntary movements. Chorea (sudden, jerky, dancing movements), athetosis (slow, writing, snake-like movements), aggression, depression, dementia. Often initially mistaken for substance abuse. Muscle rigidity (cogwheel rigidity), bradykinesia, resting tremor (pillrolling between thumb and index finger), expressionless face, stooped posture, shuffling gait, postural instability, dementia.
LIMBIC SYSTEM Anterograde Amnesia & Inappropriate Behavior DIENCEPHALON Vegetative States & Endocrine Imbalance BASAL GANGLIA Dyskinesia
Amygdala (Bilat) Hippocampus Mammillary Bodies (Bilat) Reticular Activating System Subthalamic Nucleus Striatum
KLUVER-BUCY SYNDROME ANTEROGRADE AMNESIA WERNICKE-KORSAKOFF SYNDROME COMA HEMIBALLISMUS HUNTINGTONS DISEASE
Associated with HSV-1.
Substantia Nigra
PARKINSONS DISEASE
** Chorea: Sudden, jerky, dancing movements of limbs. ** Athetosis: Slow, writing, snake-like movements of fingers. ** Myoclonus: Sudden, brief muscle contraction (jerk or hiccup). ** Dystonia: Sustained involuntary muscle contraction (writers cramp, blepharospasm). ** Tremor: Rhythmic contraction and relaxation of muscles in one or more body parts (most often the hands).
CENTRAL NERVOUS SYSTEM - BRAINSTEM
Location of Lesion Midbrain (Level of Superior Colliculi) Name of Disease Disease Mechanism Pinealoma impinges on the midbrain. Effects (Relative to Location of Lesion) Eyes: Paralysis of conjugate vertical gaze.
PARINAUD SYNDROME
pg 387 Midbrain (Level of Inferior Colliculi)
Demyelination of superior cerebellar peduncle, CN4, and MLF. Lesions are random and asymmetric. Note that MS can also affect the cervical spinal cord. MULTIPLE SCLEROSIS
Contralateral Limbs: Intention tremor, dysmetria, dysdiadochokinesia due to loss of superior cerebellar peduncle. Contralateral Eye: Unable to depress while adducted due to loss of CN4 nucleus. Ipsilateral Eye: Internuclear ophthalmoplegia (unable to adduct while gazing away from lesion) due to loss of MLF. Both Eyes: Nystagmus and optic neuritis (sudden loss of vision). Can also have scanning speech due to cerebral lesions. Contralateral Limbs: Upper and lower limbs both have weakness, hyperreflexia, positive Babinski sign due to loss of CST, plus loss of fine touch, vibration, and proprioception due to loss of ML. Contralateral Face: Loss of pain sensation due to loss of TTT. Ipsilateral Face: Paralysis of facial muscles due to loss of CN7. Ipsilateral Eye: Esotropia and inability to abduct due to loss of CN6. Inability to adduct during contralateral gaze due to loss of MLF. Both Eyes: Paralysis of ipsilateral gaze (unable to look toward lesion). Ipsilateral Face: No pain due to loss of spinal trigeminal tract. Ipsilateral Pharynx: No gag reflex due to loss of CN10. Ipsilateral Eye: Horner syndrome due to loss of reticular formation. Contralateral Body: No pain due to loss of STT, plus ataxia and dysmetria due to loss of inferior cerebellar peduncle.
pg 387 Caudal Pons Stroke in basilar artery. Affects the brainstem, cerebellum, thalamus, and occipital cortex. Lesions of the corticospinal tract, medial lemniscus, trigeminothalamic tract, parapontine reticular formation, medial longitudinal fasciculus, CN7, and CN6. Symptoms Include the 3 Ds: Dysarthria, Diplopia, Dysphagia.
VERTEBROBASILAR INSUFFICIENCY
pg 384 Stroke in vertebral artery or PICA. Affects the spinal trigeminal tract, the spinothalamic tract, the inferior cerebellar peduncle, reticular formation, and CN10. LATERAL MEDULLARY (WALLENBERG) SYNDROME
Rostral Medulla
pg 383
** Page numbers refer to Basic Clinical Neuroscience, Young & Tolbert, 2 Edition
nd
PERIPHERAL NERVOUS SYSTEM CRANIAL NERVES
Location of Lesion CN12 CN11 CN10 Weakening of muscles from lack of innervation. Bells Palsy is a LMN lesion of the facial nucleus or nerve. Remember that each quadrant of the face has its own LMN. LMNs of the upper half of the face have bilateral UMNs, whereas LMNs of the lower half have only one contralateral UMN. Weakening of muscles from lack of innervation. Name of Disease Disease Mechanism Weakening of muscles from lack of innervation. Weakening of muscles from lack of innervation. Effects Ipsilateral Side of Tongue: Tongue deviates toward the side of the lesion (due to unopposed force from the opposite side of the tongue). Ipsilateral SCM and Trapezius Muscles: Unable to turn head to contralateral side of lesion (SCM). Should droop on ipsilateral side of lesion (trapezius). Ipsilateral Pharynx: Uvula deviates away from side of lesion (since the pharynx muscles on that side collapse). Face: UMN lesion results in paralysis of the contralateral lower quarter of the face. LMN lesion (Bells Palsy) results in paralysis of the ipsilateral half of the face.
CN7
BELLS PALSY
CN5 CN3, CN4, CN6
Ipsilateral Pterygoid Muscle: Jaw deviates toward the side of the lesion (due to unopposed force from the opposite pterygoid muscle).
PERIPHERAL NERVOUS SYSTEM SPINAL CORD
Location of Lesion Any Level of the Cord Name of Disease
LMNs = Flaccid Paralysis (HYPOreflexia & Atrophy), UMNs = Spastic Paralysis (HYPERreflexia w/o Atrophy)
Disease Mechanism nd Damage to white commissure (location of the 2 order neurons of the spinothalamic tract). Caused by syringomyelia (which is associated with type 1 and 2 Chiari malformations) or spinal cord cavitation. Effects are isolated to the same dermatome as the lesion; however, the lesion can expand to affect other tracts. Effects SENSORY - Bilateral Body at Level of Lesion: Loss of pain, temp, and crude touch due to loss of STT. Figure shows effects of commissural syndrome at C5-C7.
COMMISSURAL SYNDROME
FRIEDREICHS ATAXIA
Congenital impairment of mitochondrial functioning due to recessive trinucleotide (GAA) repeat mutation in gene coding for frataxin. Demyelination and degeneration of dorsal columns, lateral corticospinal tracts, and spinocerebellar tracts.
Any Level of the Cord
Hemisection of the spinal cord. Affects anterior horn, lateral corticospinal tract, dorsal column, spinothalamic tract, intermediolateral cell column (sym). If the hemisection occurs ABOVE T1 (in the cervical spinal cord), the patient will present with Horners Syndrome IN ADDITION to all the deficits listed in the next column.
*Remember that STT crosses and exits at TWO LEVELS below its origin in the spinal cord.
BROWN-SEQUARD SYNDROME
SENSORY - Bilateral Body at and Below Lesion: Loss of proprioception, DTRs, and vibration due to loss of DC. MOTOR (UMN) Bilateral Body at and Below Lesion: Ataxia due to loss of spinocerebellar tracts and lateral CST. Also associated with nystagmus, dysarthria, pes cavus (high arch of foot), hypertrophic cardiomyopathy, hammer toes, and kyphoscoliosis (in childhood). MOTOR (UMN+LMN) - Ipsilat Body at 2 Levels* Below Lesion: Loss of all sensation due to loss of DC, uncrossed STT, and crossed STT, plus flaccid paralysis (LMN lesion) due to loss of ventral horn. MOTOR (UMN+LMN) - Ipsilat Body 2+ Levels Below Lesion: Loss of fine touch, proprioception, and vibration due to loss of DC, plus loss of pain, temp, and crude touch due to loss of STT, plus spastic paralysis (UMN lesion) due to loss of CST. MOTOR (LMN) Contralateral Body Below Lesion: Loss of pain, temp, crude touch due to loss of crossed STT.
PERIPHERAL NERVOUS SYSTEM SPINAL CORD
Location of Lesion Anterior Horn Name of Disease POLIOMYELITIS OR SPINAL MUSCULAR DYSTROPHY Cervical & Thoracic Cord
LMNs = Flaccid Paralysis (HYPOreflexia & Atrophy), UMNs = Spastic Paralysis (HYPERreflexia w/o Atrophy)
Disease Mechanism Degeneration of LMNs in anterior horn. Poliomyelitis is acquired (from polio infection) whereas spinal muscular dystrophy (aka Werdnig-Hoffmann Disease) is congenital (SMN1 gene mutation). Infants with spinal muscular dystrophy are known as floppy baby and only survive for 7 months. Demyelination of white matter tracts. Affects posterior and lateral columns of the upper thoracic and cervical spinal cord, plus the peripheral nerves and cerebrum. Impairs the DC/ML and lateral corticospinal tracts. Effects MOTOR (LMN) - Fasciculations, atrophy, weakness, fibrillation, hyporeflexia.
Hyporeflexia
B12 DEFICIENCY
AMYOTROPHIC LATERAL SCLEROSIS (ALS) Lou-Gehrigs Disease Dorsal Columns TABES DORSALIS
Defect in superoxide dismutase I (SODI) causes both LMN and UMN lesions with NO SENSORY DEFICITS. Retrograde degeneration of motor neurons (replaced by gliosis).
MOTOR (LMN & UMN): Fasciculations and atrophy. Progressive and fatal with no sensory, cognitive, or occulomotor deficits.
Tertiary neurosyphilis causes degeneration of dorsal columns and dorsal roots.
SENSORY - Bilateral Body at and Below Lesion: Loss of proprioception and loss of DTRs due to loss of DC, locomotor ataxia due to loss of sensory outflow (dorsal roots). Also associated with Charcots joints, shooting pain, Argyll Robertson pupils (accommodate but do not react), positive Romberg sign, and sensory ataxia at night.
PERIPHERAL NERVOUS SYSTEM SPINAL CORD
Location of Lesion Anywhere along the 3-neuron oculosympathetic pathway between the hypothalamus and the eyes & face (see figures below). Name of Disease
LMNs = Flaccid Paralysis (HYPOreflexia & Atrophy), UMNs = Spastic Paralysis (HYPERreflexia w/o Atrophy)
Disease Mechanism Can be caused by anything that damages the sym pathway to the face, including the hypothalamus, intermediolateral cell column, cervical sym chain, internal carotid, ciliary ganglion, or short ciliary nerve. Diseases that can cause this damage include lateral medullary syndrome, otitis media, Pancoast tumor, MS, thyroid cancer, cavernous sinus thrombosis, syringomyelia, or trauma (brachial plexus injury). Effects Ipsilateral Face: Ptosis due to weakening of superior tarsal muscle, plus anhidrosis, flushing, and miosis (constricted and fixed pupil) due to loss of sympathetic innervation.
HORNERS SYNDROME
You might also like
- Draw It To Know It NotesDocument13 pagesDraw It To Know It Noteskat9210No ratings yet
- NeurologyDocument23 pagesNeurologyAhmad Naufal Basri100% (3)
- Neurology Multiple Choice Questions With Explanations: Volume IIFrom EverandNeurology Multiple Choice Questions With Explanations: Volume IIRating: 5 out of 5 stars5/5 (2)
- Neurology Multiple Choice Questions With Explanations: Volume IFrom EverandNeurology Multiple Choice Questions With Explanations: Volume IRating: 4 out of 5 stars4/5 (7)
- Neurology Multiple Choice Questions With Explanations: Volume IIIFrom EverandNeurology Multiple Choice Questions With Explanations: Volume IIIRating: 4.5 out of 5 stars4.5/5 (6)
- Brainstem & LesionsDocument4 pagesBrainstem & LesionsErnie G. Bautista II, RN, MDNo ratings yet
- Brain + Spinal Cord: Central Nervous System (CNS)Document18 pagesBrain + Spinal Cord: Central Nervous System (CNS)Anna Marthea V.100% (4)
- Neurology MnemonicsDocument2 pagesNeurology MnemonicsJan Taplin100% (1)
- Somatosensory SystemDocument5 pagesSomatosensory Systemaloepathic100% (4)
- Neurology MnemonicsDocument27 pagesNeurology MnemonicsMuhammad Luqman Nul Hakim100% (1)
- Neurology NotesDocument15 pagesNeurology NotesAshley Diane Henry100% (3)
- NeurologyDocument118 pagesNeurologykep1313No ratings yet
- Neuroanatomy Notes 2010Document33 pagesNeuroanatomy Notes 2010Jennifer David InauenNo ratings yet
- BRT Anatomy - NeuroanatomyDocument6 pagesBRT Anatomy - NeuroanatomyNicole Santos100% (3)
- Neurology MnemonicsDocument11 pagesNeurology MnemonicsOstaz100% (1)
- NeuroanatomyDocument72 pagesNeuroanatomyYasar SabirNo ratings yet
- Neuroscience Ii: Summary: Nationality (Will Tell You Incidence, For Example, AsiansDocument29 pagesNeuroscience Ii: Summary: Nationality (Will Tell You Incidence, For Example, AsiansAngelaTrinidad100% (2)
- NeuroTracts - Ascending, Descending, UMN, LMNDocument5 pagesNeuroTracts - Ascending, Descending, UMN, LMNBrandi Allen HensonNo ratings yet
- LocalizationDocument38 pagesLocalizationWilson HannahNo ratings yet
- Comprehensive Neurology Board Review-THIRD EDITIONDocument44 pagesComprehensive Neurology Board Review-THIRD EDITIONDr. Chaim B. Colen50% (4)
- Neurology MnemonicsDocument26 pagesNeurology MnemonicsAnnapurna DangetiNo ratings yet
- Neuroanatomy Notes PDFDocument66 pagesNeuroanatomy Notes PDFfatimaabeer083% (6)
- Neurology ReviewDocument42 pagesNeurology ReviewShahnaaz Shah50% (2)
- Tracts of The Spinal CordDocument21 pagesTracts of The Spinal Corddr.a.k.gupta6924100% (10)
- Neurology Short NotesDocument11 pagesNeurology Short NotesSachin Kumar Rastogi100% (1)
- Spinal Tracts: DR - Krishna Madhukar Dept. of Orthopaedics Bharati HospitalDocument65 pagesSpinal Tracts: DR - Krishna Madhukar Dept. of Orthopaedics Bharati HospitalKrishna Madhukar100% (1)
- Visually Memorable Neuroanatomy for BeginnersFrom EverandVisually Memorable Neuroanatomy for BeginnersRating: 5 out of 5 stars5/5 (1)
- Brainstem MnemonicsDocument2 pagesBrainstem MnemonicsFajar Rudy Qimindra100% (4)
- Neuroanatomy QbankDocument27 pagesNeuroanatomy Qbankbbbanyi67% (3)
- 21-Spinal Cord TractsDocument23 pages21-Spinal Cord TractsALFAHRUL CAHYADINo ratings yet
- Neurology NotesDocument31 pagesNeurology NotesArif Setyawan75% (4)
- Comprehensive Neurology Board Review Flash CardsDocument202 pagesComprehensive Neurology Board Review Flash CardsDr. Chaim B. Colen78% (9)
- Study Guide NeurophysiologyDocument2 pagesStudy Guide NeurophysiologyAndrew MajorNo ratings yet
- Cranial Nerves (Association & Motor Neurons)Document2 pagesCranial Nerves (Association & Motor Neurons)Ernie G. Bautista II, RN, MD100% (3)
- Anatomic LocalizationDocument9 pagesAnatomic Localizationkid100% (1)
- Spinal Cord LesionsDocument110 pagesSpinal Cord Lesionsgtaha80100% (1)
- NeuroanatomyDocument4 pagesNeuroanatomyLouis Fortunato100% (2)
- Neurology Visual ApproachDocument105 pagesNeurology Visual ApproachFrancieudo Sampaio86% (7)
- Neurology NotesDocument87 pagesNeurology Notessuggaplum100% (2)
- High Yield Neuroanatomy 2nd EditionDocument151 pagesHigh Yield Neuroanatomy 2nd Editionppappi1286% (7)
- 14 15 Little Red Book of NeurologyDocument117 pages14 15 Little Red Book of NeurologyeloyNo ratings yet
- 16 Stroke SyndromesDocument32 pages16 Stroke SyndromesRos Potter100% (2)
- Mnemonic For Medical Students For Upper and Lower Motor LesionsDocument1 pageMnemonic For Medical Students For Upper and Lower Motor LesionsLe-Ann Mariamlelue100% (2)
- Neurology NotesDocument1 pageNeurology NotesTharaniNo ratings yet
- NeurologyDocument60 pagesNeurologyniceheir100% (1)
- Cranial NervesDocument9 pagesCranial Nervesangrypandasaredangerous100% (4)
- Stroke Syndromes and Localization 2007Document56 pagesStroke Syndromes and Localization 2007SaintPaul Univ100% (1)
- OSCE Cerebellar Examination PDFDocument6 pagesOSCE Cerebellar Examination PDFriczen vilaNo ratings yet
- Neuroanatomy ReviewDocument107 pagesNeuroanatomy ReviewAlan Magpantay100% (1)
- Essentials of Neurology 2Document153 pagesEssentials of Neurology 2prahul2588100% (7)
- D. Brainstem: PONS (Ventral Metencephalon) 1. External Consideration A. Ventral ViewDocument39 pagesD. Brainstem: PONS (Ventral Metencephalon) 1. External Consideration A. Ventral ViewMarvic SueltoNo ratings yet
- NeuroanatomyDocument3 pagesNeuroanatomyModoro0% (1)
- High-Yield Neuroanatomy - James D. FixDocument145 pagesHigh-Yield Neuroanatomy - James D. FixBahram Dideban100% (2)
- Cranial Nerves SummaryDocument3 pagesCranial Nerves SummaryJoash F. Pacquing75% (4)
- Diploma in Occupational TherapyDocument47 pagesDiploma in Occupational TherapyAzmi Plus100% (2)
- SMP Neuro Lab ManualDocument37 pagesSMP Neuro Lab Manualsas345sas345No ratings yet
- Neuroanatomy Revision Notes PDFDocument7 pagesNeuroanatomy Revision Notes PDFTanya Tanu100% (1)
- Neurology Clerkship Study GuideDocument84 pagesNeurology Clerkship Study GuideHilary Steele100% (1)
- Case Studies 7Document6 pagesCase Studies 7kep1313No ratings yet
- Case Studies 8Document7 pagesCase Studies 8kep1313No ratings yet
- Case Studies 10Document5 pagesCase Studies 10kep1313No ratings yet
- Case Studies 9Document7 pagesCase Studies 9kep1313No ratings yet
- Case Studies 6Document8 pagesCase Studies 6kep1313No ratings yet
- Case Studies 4Document4 pagesCase Studies 4kep1313No ratings yet
- Case Studies 5Document4 pagesCase Studies 5kep1313No ratings yet
- Case 1: Cystic FibrosisDocument5 pagesCase 1: Cystic Fibrosiskep1313No ratings yet
- Psychiatry - BSDocument15 pagesPsychiatry - BSkep1313No ratings yet
- Case Studies 3Document4 pagesCase Studies 3kep1313No ratings yet
- SeizuresDocument3 pagesSeizureskep1313No ratings yet
- Case Studies 1Document11 pagesCase Studies 1kep1313No ratings yet
- Case Studies 2Document4 pagesCase Studies 2kep1313No ratings yet
- Virology 1 3Document5 pagesVirology 1 3kep1313No ratings yet
- Neurology Notes For Clerkship ReviewDocument22 pagesNeurology Notes For Clerkship Reviewkep1313No ratings yet
- Week 2 Learning ObjectivesDocument21 pagesWeek 2 Learning Objectiveskep1313No ratings yet
- Biochem MedicineDocument27 pagesBiochem Medicinekep1313No ratings yet
- Week 4 Learning ObjectivesDocument24 pagesWeek 4 Learning Objectiveskep1313No ratings yet
- Week 3 Learning ObjectivesDocument12 pagesWeek 3 Learning Objectiveskep1313100% (1)
- Preventative Medicine PM - BSDocument22 pagesPreventative Medicine PM - BSkep1313No ratings yet
- Genetics - MMDocument25 pagesGenetics - MMkep1313No ratings yet
- Week 5 Learning ObjectivesDocument34 pagesWeek 5 Learning Objectiveskep1313No ratings yet
- Physiology - BSDocument14 pagesPhysiology - BSkep1313No ratings yet
- Biogenic AminesDocument5 pagesBiogenic Amineskep1313No ratings yet
- 2-5-10 HCT For Immunodeficiency and Autoimmune DisordersDocument2 pages2-5-10 HCT For Immunodeficiency and Autoimmune Disorderskep1313No ratings yet
- Case 1: Cystic FibrosisDocument5 pagesCase 1: Cystic Fibrosiskep1313No ratings yet
- MicroanatomyDocument59 pagesMicroanatomykep1313No ratings yet
- Physiology - BSDocument14 pagesPhysiology - BSkep1313No ratings yet
- Biochem MedicineDocument27 pagesBiochem Medicinekep1313No ratings yet
- 2-5-10 Introduction To Acute LeukemiaDocument3 pages2-5-10 Introduction To Acute Leukemiakep1313No ratings yet
- Laporan Lb1 Puskesmas Berdasarkan Icd-10: Kelompok Usia B L B L B NO Urut PEN Yaki TDocument36 pagesLaporan Lb1 Puskesmas Berdasarkan Icd-10: Kelompok Usia B L B L B NO Urut PEN Yaki TTogi Rut Marlita MarbunNo ratings yet
- Sample Haad Question PDF FreeDocument20 pagesSample Haad Question PDF Freehelen mercyNo ratings yet
- Paediatric Emergencies2Document244 pagesPaediatric Emergencies2Amber MonroeNo ratings yet
- Care of Patient With Musculoskeletal DisordersDocument3 pagesCare of Patient With Musculoskeletal DisordersBryan Mae H. DegorioNo ratings yet
- Module 1 NCM109Document41 pagesModule 1 NCM109AmethystNo ratings yet
- Fork Over Knives 2017 MagazineDocument101 pagesFork Over Knives 2017 Magazinemygacon97% (36)
- Visual Dysfunction in DiabetesDocument395 pagesVisual Dysfunction in DiabetesSergioAcuñaNo ratings yet
- Hypnotism MesmerismDocument32 pagesHypnotism MesmerismMuthu KumarNo ratings yet
- GERIADocument45 pagesGERIAHarry MelanoNo ratings yet
- McDonald Criteria 2005Document2 pagesMcDonald Criteria 2005api-3828181100% (1)
- Psychiatry EORDocument16 pagesPsychiatry EORAndrew BowmanNo ratings yet
- Mnemo CsDocument11 pagesMnemo CsramannishuNo ratings yet
- The Sketch of Indonesia Medicine: Sugma AP, MD, MARSDocument42 pagesThe Sketch of Indonesia Medicine: Sugma AP, MD, MARSRaja Friska YulandaNo ratings yet
- 800 QuestionsDocument77 pages800 QuestionsAtif DogarNo ratings yet
- Duran, Fatima Medriza - MS ModulesDocument130 pagesDuran, Fatima Medriza - MS Modulesnot your medz duranNo ratings yet
- Stenorol® Crypto - OS - Brochure - EN - v01 - 1020 PDFDocument2 pagesStenorol® Crypto - OS - Brochure - EN - v01 - 1020 PDFDrivailaNo ratings yet
- Guarnaccia Et Al. - 1989 - The Multiple Meanings of Ataques de Nervios in TheDocument18 pagesGuarnaccia Et Al. - 1989 - The Multiple Meanings of Ataques de Nervios in TheLaura PalermoNo ratings yet
- OsteoarthritisDocument103 pagesOsteoarthritisDr.sarvar SayyadNo ratings yet
- GH 13 617Document3 pagesGH 13 617Eunice KundimanNo ratings yet
- Third Degree Block After Mi........ Observe The PatientDocument23 pagesThird Degree Block After Mi........ Observe The PatientSunn Ren TeeNo ratings yet
- Sample Disability LTRDocument3 pagesSample Disability LTRbhtdg965940No ratings yet
- Portal HypertensionDocument23 pagesPortal HypertensionSumathi Gopinath100% (1)
- Small Animal Clinical NutritionDocument16 pagesSmall Animal Clinical NutritionJairo Pereira100% (1)
- DRUG STUDY - DexamethasoneDocument26 pagesDRUG STUDY - DexamethasoneChristel Santos100% (5)
- Comment: Pseudomonas Aeruginosa. CFTR Modulator TherapiesDocument2 pagesComment: Pseudomonas Aeruginosa. CFTR Modulator TherapiesBrenda RodriguesNo ratings yet
- Seminar On AsthmaDocument27 pagesSeminar On Asthmalumina.s100% (1)
- Vanderlind - 2021Document14 pagesVanderlind - 2021Sergio GarcíaNo ratings yet
- Bio Words 2010Document6 pagesBio Words 2010TufailAhmedNo ratings yet
- RCL Employment Medical Examination Form A (New-Returning) Revised 2015-03Document2 pagesRCL Employment Medical Examination Form A (New-Returning) Revised 2015-03Ahmad ShodiqNo ratings yet
- BPPV2011Document41 pagesBPPV2011Adimas Ratmanhana KesumaNo ratings yet